Cystic fibrosis test prenatal
FAQ: Carrier Testing for Cystic Fibrosis
What is cystic fibrosis?
Cystic fibrosis (CF) is one of the most common life threatening genetic diseases, affecting approximately 1 out of 3,300 people. The severity of CF varies, with some children showing symptoms at birth, and others not diagnosed until they are teenagers or adults.
In people with CF, a defective gene causes the body to produce an abnormally thick, sticky mucus that clogs the lungs and leads to life threatening lung infections. These thick secretions also obstruct the pancreas, preventing digestive enzymes from reaching the intestines to help break down and absorb food.
Cystic fibrosis does not affect intelligence. Most males with the condition are infertile.
Is there treatment for cystic fibrosis?
CF treatment has improved dramatically in the past four decades, although there is no cure. Treatment includes antibiotics, dietary enzyme supplements and physical therapy to help clear the lungs. A lung transplant may be an option for some patients.
In the past, most patients with CF did not reach adulthood. Now most survive into their 30s, with the average life expectancy being about 37 years.
How is cystic fibrosis inherited?
Cystic fibrosis is inherited in an autosomal recessive manner. Our genes come in pairs, with one copy inherited from each parent. Some genes have mutations in them, and do not function properly. A person with one non-functional copy of the gene is a carrier. Carriers for CF have no symptoms, but can pass the non-functioning gene on to their children. An individual must inherit two non-functioning CF genes – one from each parent – to have CF.
If both parents are carriers there is a 1 in 4 (25 percent) chance that both will pass on the non-functioning gene, which would result in a pregnancy affected with cystic fibrosis.
How do I know if I am a carrier of cystic fibrosis?
Carrier testing is available through a simple blood test.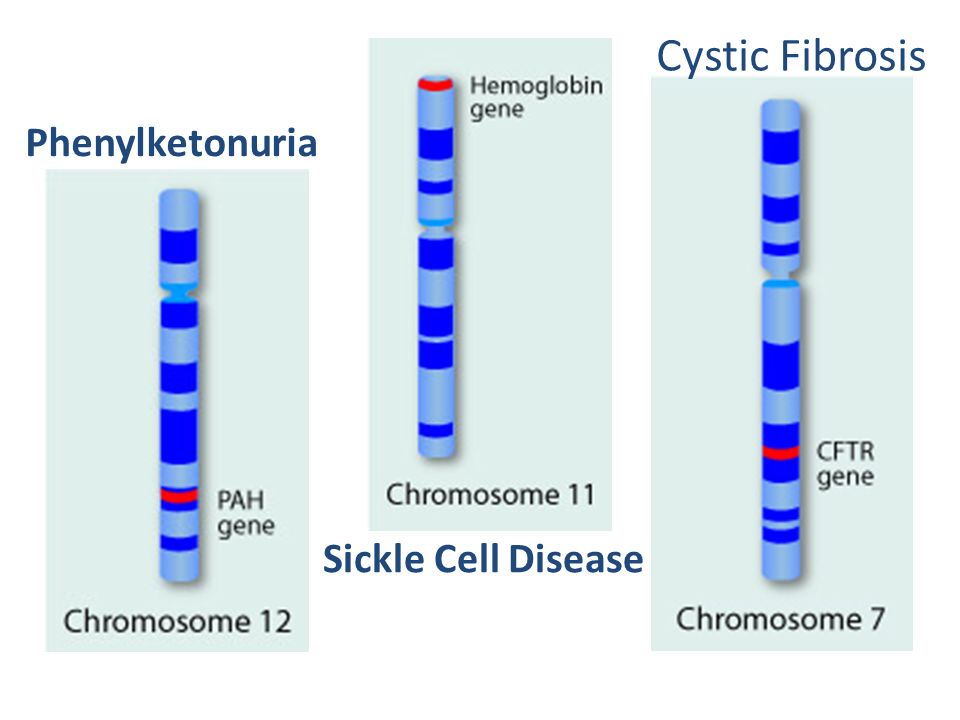 There are over 1,000 mutations that have been found to cause CF. Carrier screening can be done for the most common of these, and will identify about 85 to 90 percent of carriers in the Caucasian population. Carrier testing is also available for other ethnic groups, but the detection rates and carrier frequencies vary.
There are over 1,000 mutations that have been found to cause CF. Carrier screening can be done for the most common of these, and will identify about 85 to 90 percent of carriers in the Caucasian population. Carrier testing is also available for other ethnic groups, but the detection rates and carrier frequencies vary.
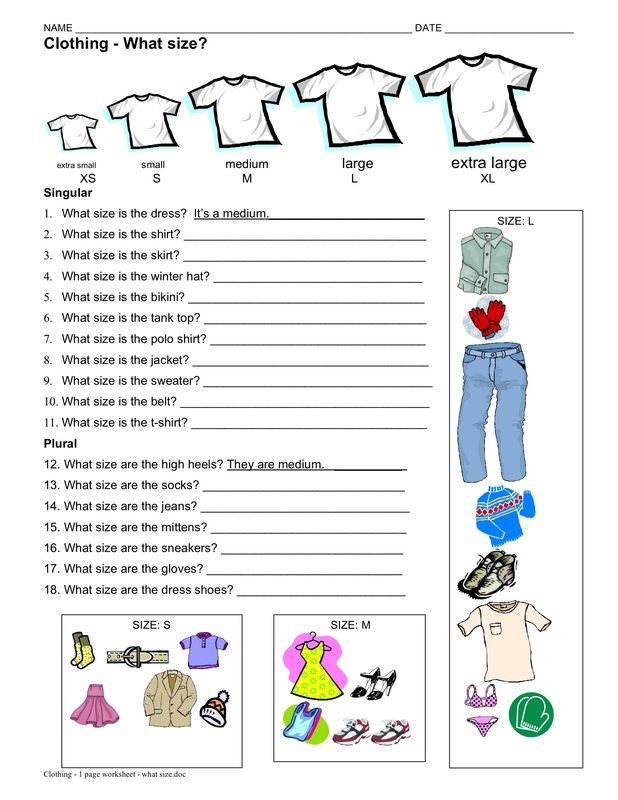
If no one in your family has CF, your chance of being a carrier depends upon your ancestry:
- European Caucasians, Ashkenazi Jews – 1 in 29
- Hispanic Americans – 1 in 46
- African Americans – 1 in 61
- Asian Americans – 1 in 90
If you have a family history of CF, your risk may be higher regardless of your ancestry.
If my test result is normal, can I still be a carrier?
Yes. If you have the test and no CF mutation is identified, your chance of being a CF carrier is reduced but not eliminated. Some people are carriers of a rare CF mutation that cannot be detected by routine screening. There is still a small chance that someone with a negative test result could be a carrier and have a child with CF.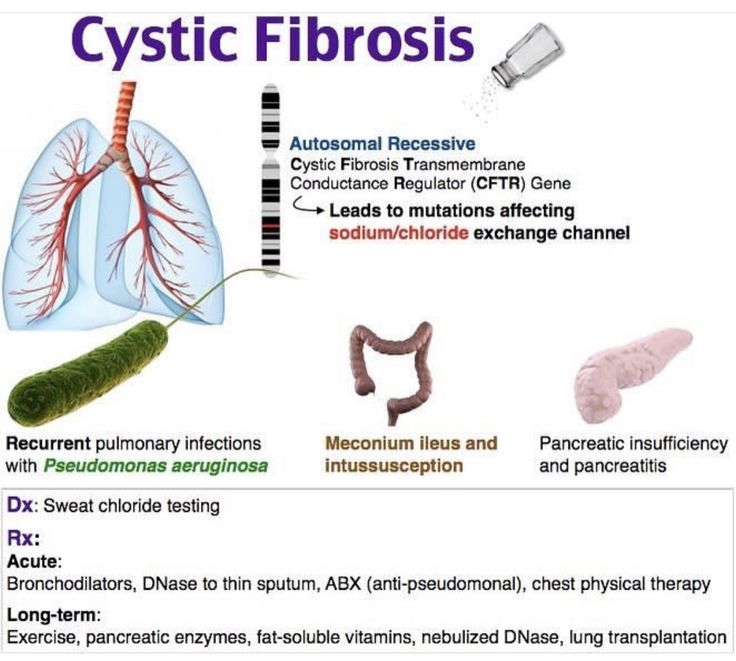
What does it mean if I am a carrier?
If you are a carrier, there is no impact on your health. However, there is a chance that you could have a child with CF. Your partner should undergo carrier screening if this has not already been performed.
If only one of you is found to be a carrier, the chance that you will have a child with CF is very low, although not completely eliminated. If you are both carriers, each pregnancy will have a 1 in 4, or 25 percent chance of being affected with cystic fibrosis.
Is prenatal testing available?
If both partners are carriers of cystic fibrosis, prenatal testing is available. Chorionic villus sampling (CVS) at 10 to 14 weeks or amniocentesis at 16 to 20 weeks can be performed to determine if the fetus has inherited two copies of the cystic fibrosis gene mutation.
If you and your partner are both carriers and you are thinking of becoming pregnant, there are other options available. You can meet with a genetic counselor to discuss these issues.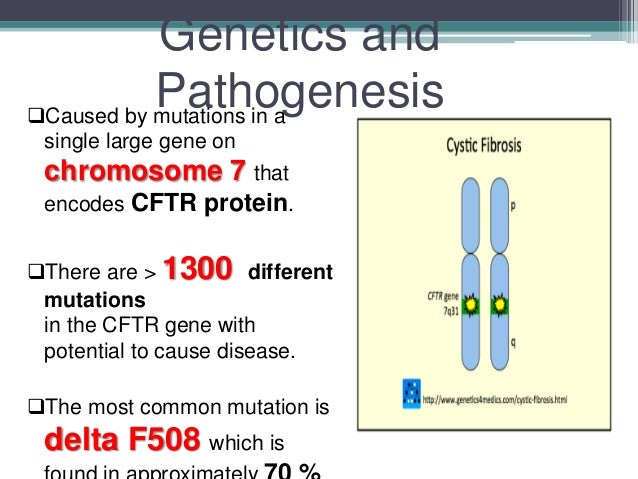
Is cystic fibrosis tested on the newborn screen?
Yes. Before your baby leaves the hospital, his or her blood sample will be collected on a piece of filter paper with a simple heel stick. Your baby will be tested for several different conditions, including cystic fibrosis.
For more information about cystic fibrosis, genetic counseling, or to arrange carrier or prenatal testing, please contact the Prenatal Diagnostic Center.
Cystic Fibrosis: Prenatal Screening and Diagnosis
Amniocentesis: A procedure in which amniotic fluid and cells are taken from the uterus for testing. The procedure uses a needle to withdraw fluid and cells from the sac that holds the fetus.
Amniotic Fluid: Fluid in the sac that holds the fetus.
Carrier: A person who shows no signs of a disorder but could pass the gene to their children.
Carrier Screening: A test done on a person without signs or symptoms to find out whether he or she carries a gene for a genetic disorder.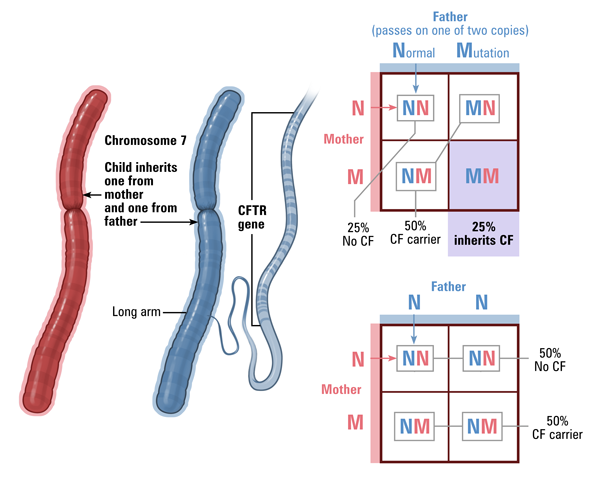
Chorionic Villus Sampling (CVS): A procedure in which a small sample of cells is taken from the placenta and tested.
Cystic Fibrosis (CF): An inherited disorder that causes problems with breathing and digestion.
Diagnostic Test: A test that looks for a disease or cause of a disease.
Embryo: The stage of development that starts at fertilization (joining of an egg and sperm) and lasts up to 8 weeks.
Ethnic-Based Screening: Screening recommended for people who belong to an ethnic group or race that has a high rate of carriers of a specific genetic disorder.
Expanded Carrier Screening: A blood test to screen for a large number of genetic disorders.
Fetus: The stage of human development beyond 8 completed weeks after fertilization.
Gene: A segment of DNA that contains instructions for the development of a person’s physical traits and control of the processes in the body.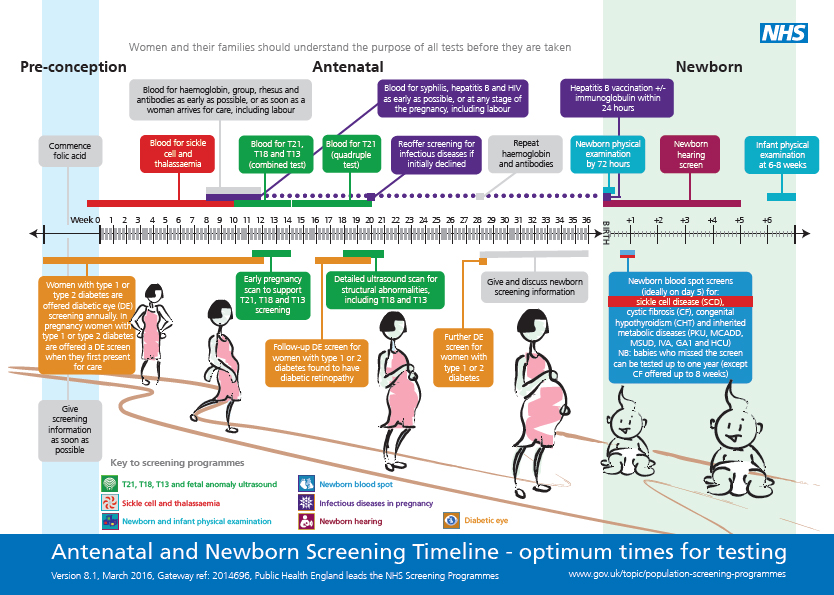 The gene is the basic unit of heredity and can be passed from parent to child.
The gene is the basic unit of heredity and can be passed from parent to child.
Genetic Counselor: A health care professional with special training in genetics who can provide expert advice about genetic disorders and prenatal testing.
Genetic Disorder: A disorder caused by a change in genes or chromosomes.
In Vitro Fertilization (IVF): A procedure in which an egg is removed from a woman’s ovary, fertilized in a laboratory with the man’s sperm, and then transferred to the woman’s uterus to achieve a pregnancy.
Mutation: A change in a gene that can be passed from parent to child.
Obstetric Care Provider: A health care professional who cares for a woman during pregnancy, labor, and delivery. These professionals include obstetrician– gynecologists (ob-gyns), certified nurse–midwives (CNMs), maternal–fetal medicine specialists (MFMs), and family practice doctors with experience in maternal care.
Obstetrician–Gynecologist (Ob-Gyn): A doctor with special training and education in women’s health.
Placenta: An organ that provides nutrients to and takes waste away from the fetus.
Preimplantation Genetic Testing: A type of genetic testing that can be done during in vitro fertilization. Tests are done on the fertilized egg before it is transferred to the uterus.
Sperm: A cell made in the male testicles that can fertilize a female egg.
Diagnosis of cystic fibrosis during pregnancy
Recently, the world began to carry out genetic tests to determine cystic fibrosis in infants. A blood test is taken from the child, if it turns out that the level of immunoreactive trypsin is at high levels, the newborn is at risk. But, to confirm the disease or its absence, an additional study of salts in the sweat fluid is carried out. Some parents ask: why is it necessary to undergo a study with a confirmed disease? To answer this question, it is necessary to consider this disease in more detail and find out what it can lead to. nine0003
nine0003
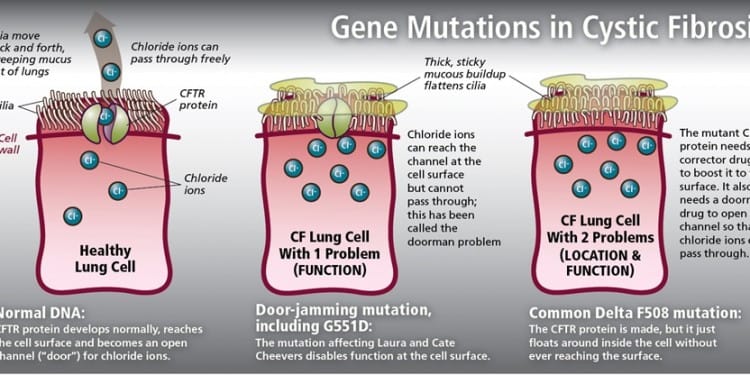
Cystic fibrosis is a severe genetic disease caused by a mutation of the CFTR gene on the seventh chromosome, which cannot be cured. The mutation leads to the fact that the protein that regulates the movement of electrolytes through the cell structure is produced in small quantities or ceases to be produced at all.
As a result of impaired function of the synthesized protein, the mucus produced by the respiratory organs, as well as the gastrointestinal tract, becomes viscous, thick, which leads to damage to these organs and sclerotic changes develop in them. It is impossible to get infected with cystic fibrosis, since people are already born with this disease, and the disease affects both girls and boys with the same frequency. nine0003
Patients often get sick with bronchitis, pneumonia, cirrhosis of the liver or cholelithiasis caused by bile stasis can also develop.
Common manifestations (symptoms of the disease) include:
- chronic wet cough;
- audible rales in the lungs;
- recurring illnesses like SARS, pneumonia and bronchitis;
- weakness and lethargy.
People who have only one defective gene are called carriers. In a child, during examination, this disease can be detected only if the parents are carriers of mutations. nine0003
Non-invasive prenatal DNA testing and early detection of cystic fibrosis
Carriers of the defective gene have a 25% increased risk of having a child diagnosed with cystic fibrosis with each subsequent pregnancy. To prevent this from happening, it is necessary to identify which defect in the CFTR gene provoked the disease in the child.
The easiest and cheapest way is to be tested for various types of mutation, of which there are about thirty. If the test reveals a single defect, the entire gene sequence will need to be analyzed by sequencing. This test allows you to identify all existing mutations. nine0008
This must be done in order to know which type of mutations the parents are and, if necessary, during pregnancy or in vitro fertilization, examine the fetus for their presence.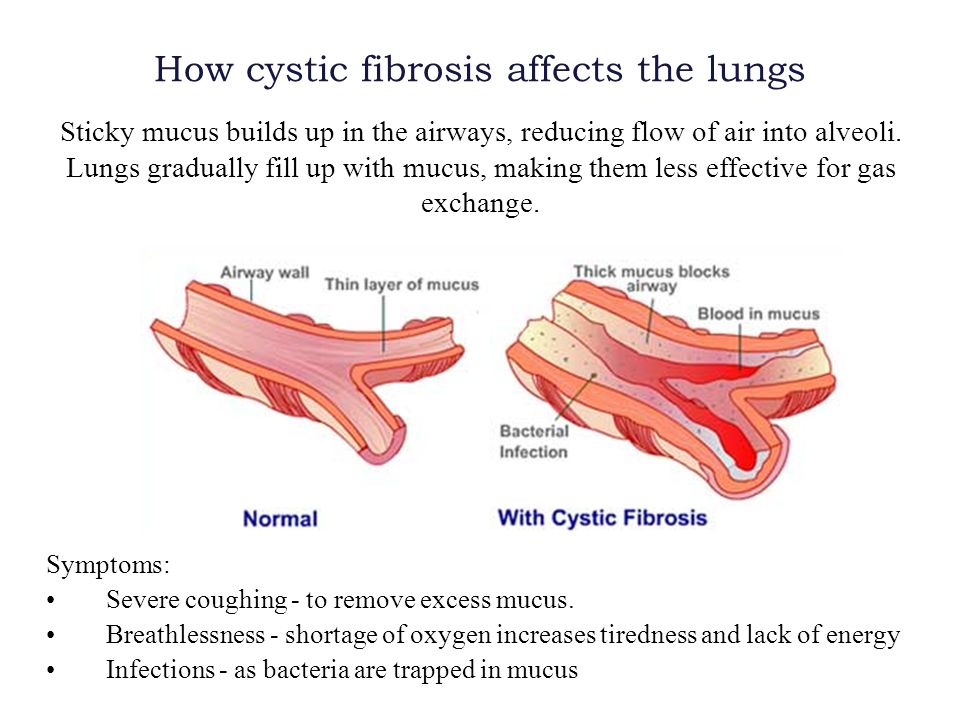 There are several methods for diagnosing monogenic diseases, including cystic fibrosis:
There are several methods for diagnosing monogenic diseases, including cystic fibrosis:
— Before pregnancy, women are advised to do preimplantation genetic diagnosis in the IVF cycle (PGD).
Before transferring an embryo into the uterine cavity, some of its cells are examined for the presence of genetic diseases. After the diagnosis, a conclusion is issued on the suitability of the transfer of the examined embryo. nine0003
- During pregnancy. In case of serious abnormalities in the fetus due to chromosomal abnormalities, at the tenth to twelfth week of pregnancy, the placenta is taken by puncture of the anterior abdominal cavity.
Further, the material is checked for the carriage of gene mutations, if they are not detected or one mutation is detected, you can not be afraid that the child will be born sick. In a situation where two defective genes are identified, the diagnosis is considered confirmed, and parents are faced with the choice of having a child with cystic fibrosis or terminating the pregnancy.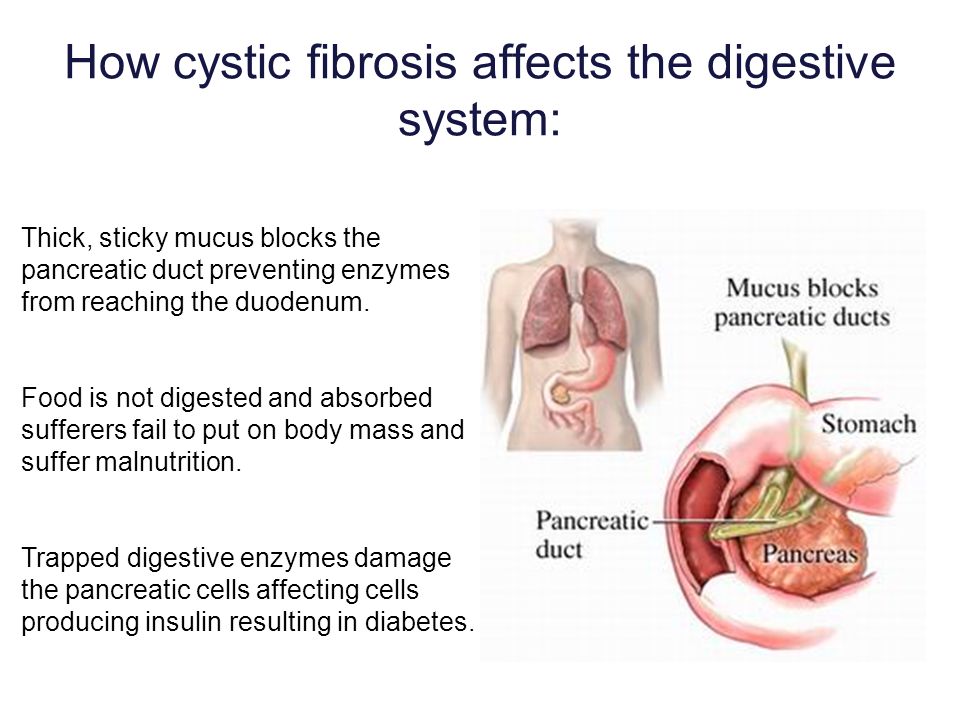 nine0003
nine0003
- During pregnancy, safe option. There is also a safe and absolutely non-traumatic method for studying the genetic health of the unborn child during pregnancy - a non-invasive prenatal test.
In Russia, only one European test examines fetal DNA for 100 monogenic diseases, this is the VERAgene test, manufactured in Cyprus.
The test is carried out as early as 10 weeks of gestation and only maternal venous blood is required for the test. The accuracy of the study is the same as with invasive procedures. nine0003
We sincerely hope that over time new drugs will appear that can regulate the work of genes, and the prescription of the drug will depend on what type of gene mutation the child has.
To take the VERAgene test, contact the Medical Genomics laboratory. Also, in case of a positive result, there will be an opportunity to consult with a practicing geneticist of our medical center for free.
When and why are genetic tests needed if a child has cystic fibrosis?| Center for Genetics and Reproductive Medicine Genetico
November 21, 2016
In many countries, all newborns are now screened for cystic fibrosis.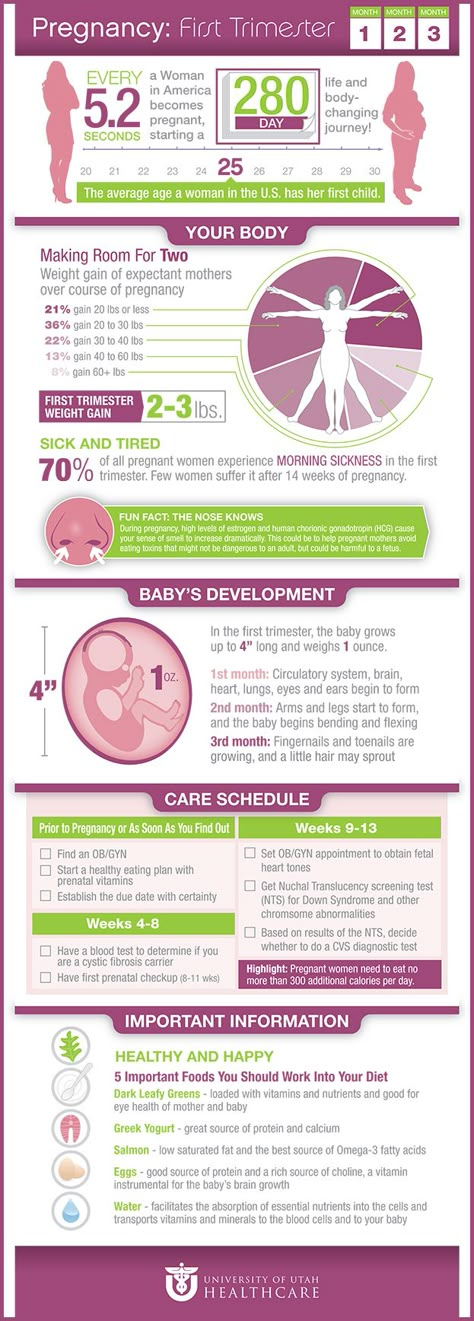 If an elevated level of immunoreactive trypsin is detected in the blood of a child, he is referred to the risk group, and the final diagnosis is established (or excluded) based on the study of salts (chlorides) in sweat fluid. Many parents may have a natural question: why undergo a genetic test if the child's diagnosis has already been confirmed? Let's figure it out. nine0003
If an elevated level of immunoreactive trypsin is detected in the blood of a child, he is referred to the risk group, and the final diagnosis is established (or excluded) based on the study of salts (chlorides) in sweat fluid. Many parents may have a natural question: why undergo a genetic test if the child's diagnosis has already been confirmed? Let's figure it out. nine0003
Cystic fibrosis is a hereditary disease. And it is associated with a malfunction of the CFTR gene on chromosome 7. This gene produces a special protein in all healthy people, which is necessary to maintain the low viscosity of the mucus produced by various hollow organs (mainly in the respiratory and digestive systems). If a given gene carries a mutation (breakdown/defect) on both 7th chromosomes (received from both mother and father), its protein is not produced or produced in very small quantities. If the mutation is present only on one of the 7 chromosomes, this does not manifest itself in any way and is called “carriage”.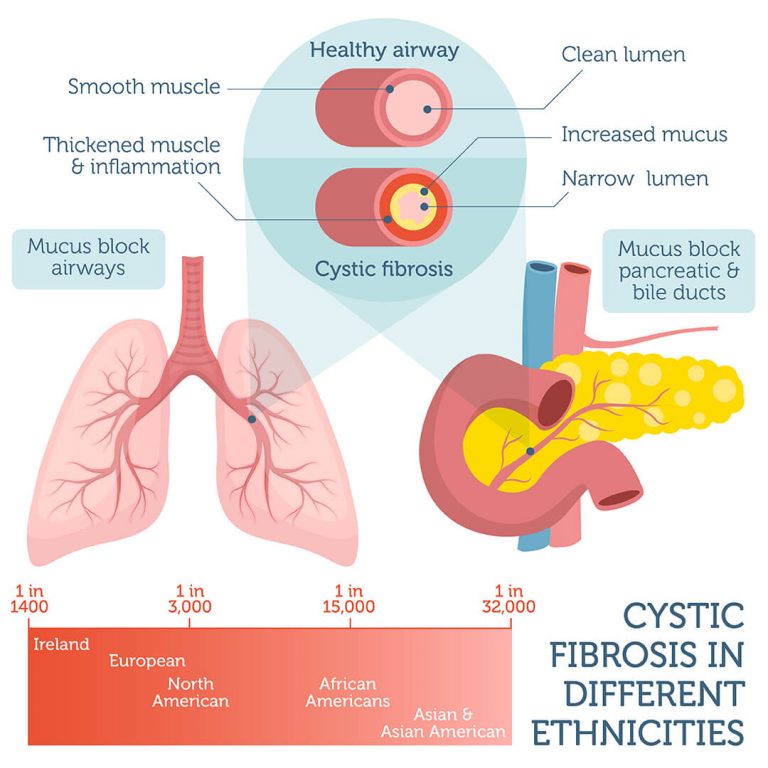 Thus, if your child is diagnosed with cystic fibrosis, you and your spouse both carry mutations in the CFTR gene. nine0003
Thus, if your child is diagnosed with cystic fibrosis, you and your spouse both carry mutations in the CFTR gene. nine0003
This means that with each subsequent pregnancy you have a high risk that the baby will also be sick with cystic fibrosis. This risk is 25%.
If you want to protect yourself from having a child with cystic fibrosis again, you must first find out which mutations (defects) in the CFTR gene caused the disease in your child. The simplest and least expensive test is a test for mutations that occur most often. There are about 30 of them, and all can be tested at the same time. If, however, no mutations are detected, or only one is detected, the entire gene sequence will have to be tested to search for rarer ones. This test is called sequencing. It will identify all mutations that may not have been previously described in any patient with cystic fibrosis in the world. nine0003
When you know which mutations you and your husband are carriers of, you can test them on the fetus (in the presence of pregnancy) or the embryo (in the event of conception with the help of IVF).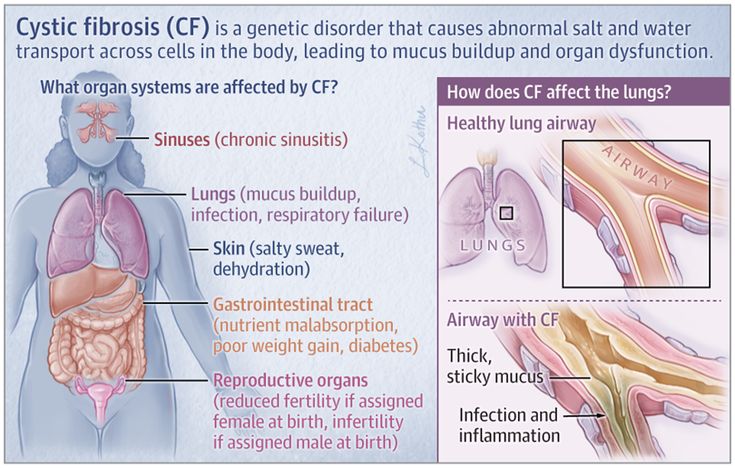
Now the most common prenatal diagnosis is when during pregnancy at a period of 10-12 weeks the fetal material (placenta) is taken through a puncture of the anterior abdominal wall. The resulting material is examined for the carriage of already known mutations. If no mutations are found, or only one mutation is found, the child will be healthy. If 2 mutations are found, then the diagnosis of cystic fibrosis can be considered established and the family faces a difficult decision to keep the pregnancy in order to give birth to a child with a hereditary disease, or to interrupt. nine0003
Preimplantation genetic diagnosis (PGD) is a better option for prenatal diagnosis. PGD allows you to examine the genetic status of an embryo obtained through in vitro fertilization (IVF) before it enters the uterine cavity and pregnancy occurs. In this case, you will not face the moral problem of terminating a pregnancy and at the same time you will know for sure that your unborn child will not suffer from cystic fibrosis.