Blister with red ring around it
Pictures, Causes, Treatment, and Prevention
What are blisters?
A blister, which is also called a vesicle by medical professionals, is a raised portion of skin that is filled with fluid. You’re probably familiar with blisters if you’ve ever worn ill-fitting shoes for too long.
This common cause of blistering produces vesicles when friction between your skin and the shoe results in layers of skin separating and filling with fluid.
Blisters are often annoying, painful, or uncomfortable. But in most cases, they aren’t a symptom of anything serious and will heal without any medical intervention. If you ever have unexplained blistering on your skin, you should see your healthcare provider for a diagnosis.
Blisters can be caused by friction, infection, or, in rare cases, a skin condition. Here are 16 possible causes of blisters.
Warning: Graphic images ahead.
Cold sore
- Red, painful, fluid-filled blister that appears near the mouth and lips
- Affected area will often tingle or burn before the sore is visible
- Outbreaks may also be accompanied by mild, flu-like symptoms such as low fever, body aches, and swollen lymph nodes
Read full article on cold sores.
Herpes simplex
- The viruses HSV-1 and HSV-2 cause oral and genital lesions
- These painful blisters occur alone or in clusters and weep clear yellow fluid and then crust over
- Signs also include mild flu-like symptoms such as fever, fatigue, swollen lymph nodes, headache, body aches, and decreased appetite
- Blisters may reoccur in response to stress, mensturation, illness, or sun exposure
Read full article on herpes simplex.
Genital herpes
- This sexually transmitted disease (STD) is caused by the HSV-2 and HSV-1 viruses.
- It causes herpetic sores, which are painful blisters (fluid-filled bumps) that can break open and ooze fluid.
- The infected site often starts to itch, or tingle, before the actual appearance of blisters.
- Symptoms include swollen lymph nodes, mild fever, headache, and body aches.
Read full article on genital herpes.
Impetigo
- Common in babies and children
- Rash is often located in the area around the mouth, chin, and nose
- Irritating rash and fluid-filled blisters that pop easily and form a honey-colored crust
Read full article on impetigo.
Burns
This condition is considered a medical emergency. Urgent care may be required.
- Burn severity is classified by both depth and size
- First-degree burns: minor swelling and dry, red, tender skin that turns white when pressure is applied
- Second-degree burns: very painful, clear, weeping blisters and skin that appears red or has variable, patchy coloration
- Third-degree burns: white or dark brown/tan in color, with leathery appearance and low or no sensitivity to touch
Read full article on burns.
Contact dermatitis
- Appears hours to days after contact with an allergen
- Rash has visible borders and appears where your skin touched the irritating substance
- Skin is itchy, red, scaly, or raw
- Blisters that weep, ooze, or become crusty
Read full article on contact dermatitis.
Stomatitis
- Stomatitis is a sore or inflammation on the lips or inside of the mouth that can be caused by infection, stress, injury, sensitivity, or other disease.

- The two main forms of stomatitis are herpes stomatitis, also known as a cold sore, and aphthous stomatitis, also known as a canker sore.
- Herpes stomatitis symptoms include fever, body aches, swollen lymph nodes, and painful, fluid-filled blisters on the lips or in the mouth that pop and ulcerate.
- With aphthous stomatitis, ulcers are round or oval with a red, inflamed border and yellow or white center.
Read full article on stomatitis.
Frostbite
This condition is considered a medical emergency. Urgent care may be required.
- Frostbite is caused by extreme cold damage to a body part
- Common locations for frostbite include fingers, toes, nose, ears, cheeks, and chin
- Symptoms include numb, prickly skin that may be white or yellow and feel waxy or hard
- Severe frostbite symptoms include blackening of the skin, complete loss of sensation, and fluid- or blood-filled blisters
Read full article on frostbite.
Shingles
- Very painful rash that may burn, tingle, or itch, even if there are no blisters present
- Rash comprising clusters of fluid-filled blisters that break easily and weep fluid
- Rash emerges in a linear stripe pattern that appears most commonly on the torso, but may occur on other parts of the body, including the face
- Rash may be accompanied by low fever, chills, headache, or fatigue
Read full article on shingles.
Dyshidrotic eczema
- With this skin condition, itchy blisters develop on the soles of the feet or the palms of the hands.
- The cause of this condition is unknown, but it may be related to allergies, like hay fever.
- Itchy skin occurs on the hands or feet.
- Fluid-filled blisters appear on the fingers, toes, hands, or feet.
- Dry, red, scaly skin with deep cracks are other symptoms.
Read full article on dyshidrotic eczema.
Pemphigoid
- Pemphigoid is a rare autoimmune disorder caused by a malfunction of the immune system that results in skin rashes and blistering on the legs, arms, mucous membranes, and abdomen.

- There are multiple types of pemphigoid that differ based on where and when the blistering occurs.
- A red rash usually develops before the blisters.
- The blisters are thick, large, and filled with fluid that’s usually clear but may contain some blood.
- Skin around the blisters may appear normal, or slightly red or dark.
- Ruptured blisters are usually sensitive and painful.
Read full article on pemphigoid.
Pemphigus vulgaris
- Pemphigus vulgaris is a rare autoimmune disease
- It affects the skin and mucous membranes of the mouth, throat, nose, eyes, genitals, anus, and lungs
- Painful, itchy skin blisters appear that break and bleed easily
- Blisters in the mouth and throat may cause pain with swallowing and eating
Read full article on pemphigus vulgaris.
Allergic eczema
- May resemble a burn
- Often found on hands and forearms
- Skin is itchy, red, scaly, or raw
- Blisters that weep, ooze, or become crusty
Read full article on allergic eczema.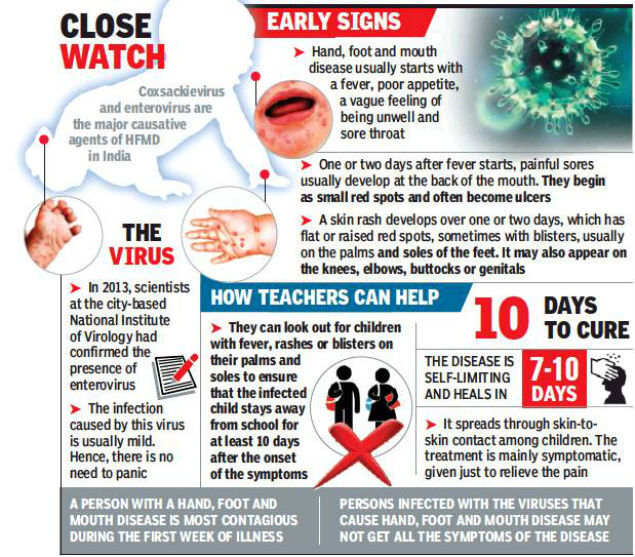
Chickenpox
- Clusters of itchy, red, fluid-filled blisters in various stages of healing all over the body
- Rash is accompanied by fever, body aches, sore throat, and loss of appetite
- Remains contagious until all blisters have crusted over
Read full article on chickenpox.
Erysipelas
- This is a bacterial infection in the upper layer of the skin.
- It’s usually caused by the group A Streptococcus bacterium.
- Symptoms include fever; chills; generally feeling unwell; a red, swollen, and painful area of skin with a raised edge; blisters on the affected area; and swollen glands.
Read full article on erysipelas.
Dermatitis herpetiformis
- Dermatitis herpetiformis is an itchy, blistering, burning skin rash that occurs on the elbows, knees, scalp, back, and buttocks.
- It’s a gluten-related disorder associated with celiac disease.
- Symptoms include extremely itchy bumps that look like pimples filled with clear liquid that form and heal in waxing and waning cycles.

- Symptoms can be controlled by following a gluten-free diet.
Read full article on dermatitis herpetiformis.
There are many temporary causes of blisters. Friction occurs when something rubs against your skin for a prolonged period of time. This happens most commonly on hands and feet.
- Contact dermatitis can also cause blisters. This is a skin reaction to allergens, like poison ivy, latex, adhesives, or irritants like chemicals or pesticides. It can cause red, inflamed skin and blistering.
- Burns, if severe enough, can produce blistering. This includes burns from heat, chemicals, and sunburns.
- Allergic eczema is a skin condition that is caused or worsened by allergens and can produce blisters. Another type of eczema, dyshidrotic eczema, also results in blistering; but its cause is unknown, and it tends to come and go.
- Frostbite is less common, but it can cause blisters on skin that’s exposed to extreme cold for a prolonged period of time.

Blistering can also be a symptom of certain infections, including the following:
- Impetigo, a bacterial infection of the skin that can occur in both children and adults, may cause blisters.
- Chickenpox, an infection caused by a virus, produces itchy spots and often blisters on the skin.
- The same virus that causes chickenpox also causes shingles, or herpes zoster. The virus reappears in some people later in life and produces a skin rash with fluid vesicles that can rupture.
- Herpes and the resulting cold sores can lead to skin blistering.
- Stomatitis is a sore inside the mouth that can be caused by herpes simplex 1.
- Genital herpes can also result in blisters around the genital region.
- Erysipelas is an infection caused by the Streptococcus group of bacteria, which produces skin blisters as a symptom.
More rarely, blisters are the result of a skin condition. For many of these rare conditions, the cause is unknown. A few skin conditions that cause blisters include:
A few skin conditions that cause blisters include:
- porphyrias
- pemphigus
- pemphigoid
- dermatitis herpetiformis
- epidermolysis bullosa
Most blisters require no treatment. If you leave them alone, they will go away, and the top skin layers prevent will infection.
If you know the cause of your blister, you may be able to treat it by covering it with bandages to keep it protected. Eventually the fluids will seep back into the tissue, and the blister will disappear.
You shouldn’t puncture a blister unless it is very painful, as the skin over the fluid protects you from infection. Blisters caused by friction, allergens, and burns are temporary reactions to stimuli. In these cases, the best treatment is to avoid what is causing your skin to blister.
The blisters caused by infections are also temporary, but they may require treatment. If you suspect you have some type of infection, you should see your healthcare provider.
In addition to medication for the infection, your healthcare provider may be able to give you something to treat the symptoms. If there is a known cause for the blisters, such as contact with a certain chemical or use of a drug, discontinue use of that product.
If there is a known cause for the blisters, such as contact with a certain chemical or use of a drug, discontinue use of that product.
Some conditions that can cause blisters, such as pemphigus, don’t have a cure. Your healthcare provider can prescribe treatments that will help you manage symptoms. This may include steroid creams to relieve skin rashes or antibiotics to cure skin infections.
In most cases, blisters aren’t part of a life-threatening condition. Most will go away without treatment, but may cause you pain and discomfort in the meantime.
The quantity of blisters you have, and whether these have ruptured or have become infected, is important in the outlook of your condition. If you treat an infection that is causing blisters, your outlook is good. For rare skin conditions, how well treatments work will depend on the individual situation.
For the most common of blisters — those caused by friction on the skin of your feet — you can practice basic preventive measures:
- Always wear comfortable, well-fitting shoes.

- If you will be walking for a long period of time, use thickly cushioned socks to reduce friction.
- As you walk, you may feel a blister beginning to form. Stop and protect this area of skin with a bandage to prevent further friction.
Read this article in Spanish.
Blisters with Water: Causes, Treatment, Draining, Prevention
Blisters with Water: Causes, Treatment, Draining, PreventionMedically reviewed by Alana Biggers, M.D., MPH — By Scott Frothingham — Updated on January 25, 2019
Blisters with water
Water blisters — fluid-filled sacs on your skin — are relatively common.
Referred to as vesicles (small blisters) and bullae (larger blisters), blisters are often simple to treat. It can also be comparatively uncomplicated to identify the cause of a water blister.
When the outer layer of your skin is damaged, your body sends blood to heal and cool the injured area.
Part of that process is the formation of protective pads comprised of blood serum (without the clotting agents and blood cells). These serum pads are water blisters.
These serum pads are water blisters.
Some common reasons water blisters occur are:
- friction
- burns from heat, chemicals, or the sun
- contact dermatitis
- eczema
- an allergic reaction
- poison ivy, poison oak, or poison sumac
- viral infections such as herpes, chickenpox, and shingles
- skin infections such as impetigo
- frostbite
Blisters will usually heal on their own with the skin over the blister helping to keep out infection while new skin is formed underneath and the fluid is absorbed.
To keep a blister clean and to protect it from friction, you can cover it with a bandage.
Contact your doctor if:
- the blister shows signs of infection such as pus, or the area around the blister becomes swollen, red, warm, or painful
- you develop a fever
- you have several blisters and you can’t identify what’s causing them
- you continue to see drainage after you’ve drained the blister
- you have poor circulation or diabetes
If your blister is large, painful, or likely to be aggravated and pop on its own, you might consider draining it.
To properly drain the fluid while leaving the top skin in place for shielding, there are specific steps you should take. These include:
- Wash the blister, the area around it, and your hands with warm water and soap.
- Use an absorbent pad to apply iodine to the blister and surrounding area.
- Wipe a sharp needle with rubbing alcohol to sterilize it.
- Aiming for spots near the blister’s edge, puncture it a few times with the needle.
- Allow the fluid to drain, while leaving the overlying skin in place.
- Spread the blister area with petroleum jelly or a similar ointment.
- Cover the blister with a non-stick gauze bandage.
Follow-up care
- Check for any signs of infection daily.
- After a few days, using small, sharp scissors and tweezers — wiped with rubbing alcohol to sterilize — cut away all the dead skin.
- Apply more ointment and cover the area with a bandage.
The general rule of blister prevention is to stay away from whatever caused the blister.
It’s overly simple, but it also makes sense: If you got blisters from getting a sunburn, spend less time in the sun (or wear more protective clothing and sunscreen).
For specific body parts, here are a few prevention tips to keep in mind:
Feet
- Wear shoes that fit properly.
- Wear moisture-wicking socks.
- Attach moleskin to the inside of your shoe where it rubs against your foot.
- Put powder in your socks just prior to putting them on.
Hands
- Wear gloves.
- Put powder in your gloves just prior to putting them on.
Body, arms, and legs
- Avoid wearing clothing thatcauses chafing.
- Wear moisture-wicking clothing.
- Apply petroleum jelly to areas that are rubbed by other body parts or clothing.
Water blisters are common and, if left alone, will typically heal on their own.
If a blister grows, becomes painful, or seems likely to be irritated, you might consider draining it using proper sterilization steps and bandaging the open wound. There are steps you can take to prevent blisters, including shoe, sock, and clothing choices.
There are steps you can take to prevent blisters, including shoe, sock, and clothing choices.
If you can’t determine the origin of a blister, blister drainage continues after it’s been drained, or if a blister shows signs of infection, contact your doctor.
Last medically reviewed on October 12, 2018
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- 5 ways to avoid blisters and the best way to treat them. (2015).
health.clevelandclinic.org/5-ways-to-avoid-blisters-and-the-best-ways-treat-them/ - American Academy of Dermatology. (n.d.). How to prevent and treat blisters.
aad.org/public/skin-hair-nails/injured-skin/blisters - Mayo Clinic Staff.
 (2018). Blisters: First aid.
(2018). Blisters: First aid.
mayoclinic.org/first-aid/first-aid-blisters/basics/art-20056691 - U.S. National Library of Medicine. (2016). Blisters.
medlineplus.gov/blisters.html
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Share this article
Medically reviewed by Alana Biggers, M.D., MPH — By Scott Frothingham — Updated on January 25, 2019
Read this next
Blisters
Medically reviewed by University of Illinois
A blister, or vesicle, is a raised portion of skin that is filled with fluid. You’re probably familiar with blisters if you’ve ever worn ill-fitting…
READ MORE
How Do I Know If My Blister’s Infected?
Medically reviewed by Jill Seladi-Schulman, Ph.D.
Everyone gets a blister from time to time.
 Blisters are your body’s natural way of protecting itself from further friction and damage. They can also…
Blisters are your body’s natural way of protecting itself from further friction and damage. They can also…READ MORE
Why Are Blisters Forming Between My Toes and How Do I Treat Them?
Medically reviewed by Stacy Sampson, D.O.
If you routinely get blisters on or between your toes, there are a few steps you can take to prevent future recurrences. Sometimes, blisters can be a…
READ MORE
When and How to Pop a Blister
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
You’ve probably heard that it’s best to leave blisters alone. While this is true, it’s not always practical. Read on to learn how to tell when it…
READ MORE
How to Use Moleskin for Blisters
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Moleskin is a type of durable bandage made out of cotton that’s often used to protect and prevent blisters.
 We’ll go over how to use moleskin for…
We’ll go over how to use moleskin for…READ MORE
Hypertrophic Scars and Keloids: Similarities and Differences
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Keloids and hypertrophic scars are similar in many ways but differ in their risk factors, treatment, and outlook.
READ MORE
Latisse for Eyebrows: Is It Safe to Use?
Medically reviewed by Cynthia Cobb, DNP, APRN, WHNP-BC, FAANP
If you’re experiencing eyebrow hair loss or simply have sparse eyebrows, Latisse is one option to consider. Learn more about its benefits, how to use…
READ MORE
Erythema annulare: symptoms, treatment, diagnosis of the disease
Dermatovenereologist
Khasanova
Alina Rashidovna
Experience 10 years
Make an appointment
Erythema annulare is a multiform lesion of the skin, a characteristic feature of which is the appearance of ring-shaped spots and rashes on the skin. The color of the skin of the affected areas changes and becomes red, hot pink or bluish. Depending on the causes of the disease, edema, local fever and other manifestations of the disease can be observed. A change in skin color occurs due to the expansion of the lumen of the blood capillaries penetrating the connective tissue, and the blood stagnation associated with it. nine0003
The color of the skin of the affected areas changes and becomes red, hot pink or bluish. Depending on the causes of the disease, edema, local fever and other manifestations of the disease can be observed. A change in skin color occurs due to the expansion of the lumen of the blood capillaries penetrating the connective tissue, and the blood stagnation associated with it. nine0003
Varieties of pathology
Doctors distinguish several types of annular erythema, depending on the causes of the disease:
- Darya centrifugal erythema - most often affecting middle-aged men, less often - children and the elderly, related to infectious-allergic manifestations;
- migratory - a disease of an infectious nature resulting from the bite of a tick infected with Borrelia;
- rheumatic, or annular erythema, is one of the symptoms that accompany rheumatism, characteristic of children and adolescents.
According to external signs, ring erythema can occur:
- in scaly form - with desquamation of dead skin along the edges or the entire surface of the spots;
- in vesicular form - with the appearance of small fluid-filled vesicles along the edge or the entire surface of the spots;
- in a garland-like form - with the mildest course, which is characterized by pale pink spots arranged in chains or garlands and disappearing after a few days; nine0020
- in microgarland-like form - with small spots, up to 1 cm in diameter, sometimes accompanied by peeling or blistering, with a long course.

The medical literature also mentions other, very rare types of annular erythema - telangiectatic, purpuric or indurated.
Symptoms
The main manifestation of the disease is the appearance on the skin of characteristic rashes in the form of irregular rings with a bright border raised above the surface of the skin. With centrifugal erythema of Dardieu, they appear, as a rule, on areas of the skin, usually covered with clothing - on the back, abdomen and chest, forearms. Erythema annulare after a midge bite is a single spot spreading from the site of infection, and in its final form it can reach 20-25 cm in diameter. The spots may be accompanied by itching or burning. In the rheumatic form of the pathology, there are no unpleasant sensations. nine0003
Causes of disease
There are many diseases and conditions that can cause erythema annulare, since it is not an independent disease and always occurs against the background of some pathological process.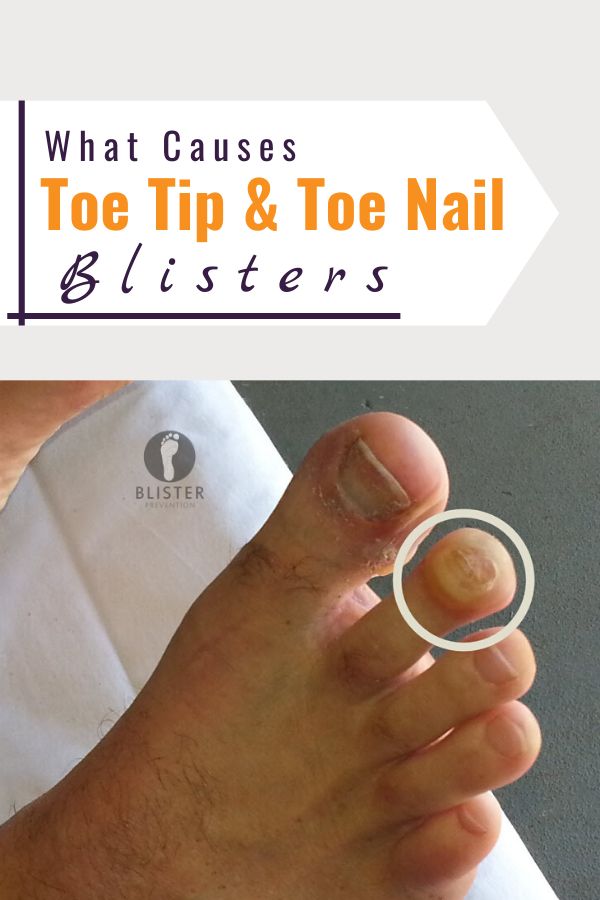 Skin manifestations most often develop against the background of:
Skin manifestations most often develop against the background of:
- accumulation of toxins in the body;
- rheumatism;
- fungal, viral or bacterial infections; nine0019 chronic inflammatory diseases;
- endocrine gland dysfunctions;
- tuberculosis;
- borreliosis;
- reduce the protective function of the immune system;
- allergic reaction;
- cancer;
- helminthic infestation;
- taking certain medications.
In addition, in many cases, Darier's annular erythema occurs for no apparent reason in perfectly healthy people. nine0003
Diagnostics
When erythema annulare appears, the diagnosis is based on dermatological examination data and history taking. The main task of the examination is to determine the cause that caused pathological changes in the skin. For this, the patient is prescribed:
- skin scraping test for fungus;
- clinical blood test;
- testing for treponematosis;
- skin biopsy for histological analysis; nine0020
- serological examination of blood;
- allergy tests.

Based on the results obtained, specific studies can be prescribed to determine the state of certain organs and identify the underlying disease.
Treatment
The main principle of the treatment of erythema annulare is to stop the action of the factor that provokes the pathology. Depending on the results of the diagnosis, the patient may be prescribed drugs for oral administration: nine0003
- antibiotics, antivirals for the treatment of infection;
- antiallergic and hyposensitizing agents;
- cytostatics;
- deworming agents;
- glucocorticoids.
In addition, external agents may be useful - antihistamine, steroid or zinc-containing ointments to reduce discomfort and reduce symptoms. With erythema annulare, clinical recommendations may include limiting certain foods that cause an allergic reaction: confectionery, mushrooms, nuts, canned food, smoked meats, citrus fruits, etc. You should be prepared for the fact that the treatment process will last several months, as well as the possibility relapses. nine0003
You should be prepared for the fact that the treatment process will last several months, as well as the possibility relapses. nine0003
Diagnostics and treatment of annular erythema in Moscow
The clinic of JSC "Medicina" conducts effective diagnostics and treatment of erythema annulare in Moscow. We have a powerful laboratory and diagnostic base that allows us to perform the most modern and informative types of analyzes and diagnostic procedures. Consultations are conducted by experienced doctors of the highest category. Make an appointment online or by phone at a convenient time for you.
Questions and answers
Which doctor treats erythema annulare?
If you suspect an annular erythema, you should immediately contact a dermatologist who will conduct an appropriate diagnosis and prescribe treatment based on its results. In the future, you may need to consult an allergist, rheumatologist, oncologist or other specialists, depending on the cause that caused the appearance of red spots on the skin.
Ring erythema - is it contagious? nine0003
No, this pathology is not transmitted to other people even in cases where it is caused by an infectious disease.
How dangerous is erythema annulare?
By itself, ring erythema does not pose a great danger. With timely started adequate treatment, the patient is guaranteed to recover. However, it should not be neglected: if left untreated, the disease becomes chronic with constant relapses. Skin manifestations indicate the presence of health problems, therefore, when they appear, it is necessary to contact a qualified dermatologist without delay. nine0003
Erythrasma - Symptoms, treatment - AMC Medical Directory
Erythrasma is a disease that affects the human skin (except nails and scalp). Its development is caused by the bacterium Corynebacterium minutissimum. The rashes are strictly defined and look like red spots under the microscope. The most common pathology occurs in men.
Erythrasma in most cases is a consequence of increased sweating, changes in the acid-base balance of the skin, or a violation of the integrity of the skin. nine0003
Pathogenic bacteria can live on human skin for a long time without causing a pathological process. However, if a nutrient medium is created for reproduction and entry of the pathogen into the skin, inflammation begins.
Erythrasma is transmitted from person to person. The most likely way of infection is the use of someone else's clothes and towels. Transmission of the pathogen from a sick person is possible on the beach, in the pool or through close contact.
Consult a dermatovenereologist
Do not delay treatment
Enroll
I accept the terms of the user agreement and agree to the processing of personal data in accordance with the requirements of "152-FZ"
Symptoms of erythrasma
The development of pathology causes increased sweating. Therefore, due to physiological characteristics, the disease is most common in representatives of the strong half of humanity.
Inflammations appear in the folds of the skin, where there is a favorable environment for the reproduction of bacteria. Usually the disease begins on the inner thighs, armpits or groin. Also, pathology can develop between the fingers or on the stomach. If the disease affects a woman, then rashes may appear under the breast. nine0003
Erythrasma is rare in young people. More often it affects the older generation.
The main symptom of erythrasma is the characteristic rash. They are spots with a well-defined border. The color of inflammation can be from dark brown to light pink.
The size of the affected area is from a point to 10 centimeters in diameter. The rashes are usually round in shape with brightly marked edges. With the progression of the disease, the spots merge into one large area affected by bacteria. nine0003
Pathology begins with a slight peeling. In this case, the person does not feel discomfort. Spots are found randomly.
If the pathology is not treated, it is possible to attach a secondary infection. Then there is itching and pain. The transition of the disease to a chronic form is also likely in case of violation of the therapeutic regimen.
Then there is itching and pain. The transition of the disease to a chronic form is also likely in case of violation of the therapeutic regimen.
Chronic erythrasma has periods of calm and exacerbation. Most often, new rashes appear in the warm season. During this period, a person begins to sweat more, which creates favorable conditions for the reproduction of bacteria. nine0003
How is erythrasma diagnosed
Making a diagnosis is not difficult. Usually, a full-time examination of the patient and transillumination of the rash with a Wood's lamp is usually sufficient. If, under the light of a lamp, the affected areas of the skin turn red, then there is usually no doubt. This feature usually arises from the release of water-soluble porphyrins by pathogens.
However, before resorting to diagnosis with a Wood's lamp, it is worth making sure that the patient has not treated the rash with anything. Otherwise, the coloring pigment may wash off and an incorrect diagnosis will be made. nine0003
nine0003
The inguinal form of the disease has characteristic features. The rashes are distinguished by protrusions along the edges, maceration and vesicles. However, erythrasma is very easily confused with rubromycosis of the groin. These two pathologies have similar symptoms. When diagnosing, special attention should be paid to the edges of the inflamed areas. With rubromycosis, they will be intermittent, and erythrasma will have a continuous, pronounced edge.
Treatment of erythrasma
Since inflammation is caused by pathogens, antibacterial ointments are used to treat pathology. Often, the affected areas are treated with erythromycin or sulfur-tar ointment. nine0003
Therapy usually takes at least a week. It is necessary to treat the rashes twice a day, each time removing the remnants of the old ointment.
If a secondary infection joins the underlying disease, areas of the affected skin are lubricated with salicylic alcohol or iodine. In advanced cases and with large rashes, systemic antibiotics are prescribed.
In order to maximize the effect of the treatment of the disease, patients are recommended to take sun ointments or undergo a course of UV radiation. The procedure will help dry the skin in the affected area and get rid of the pathology faster. nine0003
When a doctor makes a diagnosis of erythrasma, it is necessary to disinfect all personal belongings of the patient. Bed linen, all towels and clothes are subject to processing.
Until the course of therapy is completed, the clothes of a sick person should be changed daily, washed and ironed on both sides. At the end of treatment, all areas of the skin where there were rashes for a month are treated daily with salicylic alcohol and sprinkled with talc.
Erythrasma prophylaxis
The main measure to prevent this contagious disease is hygiene. In order not to create a favorable environment for the reproduction of microorganisms on the skin, you should regularly take a shower and wipe the skin folds dry. Especially the armpits, groin, neck and abdomen.
Especially the armpits, groin, neck and abdomen.
One of the important preventive measures is to reduce sweating. This is achieved by changing synthetic clothing to natural, using deodorants, and daily hygiene procedures.
It is also worth remembering that all new clothes must be washed and ironed before being worn.
Make an appointment with a dermatovenereologist
Do not delay treatment
Enroll
I accept the terms of the user agreement and agree to the processing of personal data in accordance with the requirements of "152-FZ"
Why Choose American Medical Clinic?
- Team of professionals. Candidates and doctors of medical sciences, professors and associate professors of departments of leading universities, doctors of the first and highest qualification category work in the clinic 24 hours a day, 7 days a week. We work without holidays and weekends so that you are healthy and happy.
- Regular professional development.