Cure for eczema on babies
How to treat eczema in babies
Diseases & conditions
- Coronavirus Resource Center
- Acne
- Eczema
- Hair loss
- Psoriasis
- Rosacea
- Skin cancer
- A to Z diseases
- A to Z videos
- DIY acne treatment
- How dermatologists treat
- Skin care: Acne-prone skin
- Causes
- Is it really acne?
- Types & treatments
- Childhood eczema
- Adult eczema
- Insider secrets
- Types of hair loss
- Treatment for hair loss
- Causes of hair loss
- Hair care matters
- Insider secrets
- What is psoriasis
- Diagnosis & treatment
- Skin, hair & nail care
- Triggers
- Insider secrets
- What is rosacea
- Treatment
- Skin care & triggers
- Insider secrets
- Types and treatment
- Find skin cancer
- Prevent skin cancer
- Raise awareness
- Español
Featured
Monkeypox: What you need to knowMonkeypox is a contagious disease that causes a rash. A board-certified dermatologist explains what the rash looks like and when to seek medical care.
This contagious skin disease will usually clear on its own, but sometimes dermatologists recommend treating it. Find out when.
Everyday care
- Skin care basics
- Skin care secrets
- Injured skin
- Itchy skin
- Sun protection
- Hair & scalp care
- Nail care secrets
- Basic skin care
- Dry, oily skin
- Hair removal
- Tattoos and piercings
- Anti-aging skin care
- For your face
- For your skin routine
- Preventing skin problems
- Bites & stings
- Burns, cuts, & other wounds
- Itch relief
- Poison ivy, oak & sumac
- Rashes
- Shade, clothing, and sunscreen
- Sun damage and your skin
- Aprenda a proteger su piel del sol
- Your hair
- Your scalp
- Nail care basics
- Manicures & pedicures
Featured
Practice Safe SunEveryone's at risk for skin cancer. These dermatologists' tips tell you how to protect your skin.
These dermatologists' tips tell you how to protect your skin.
Find out what may be causing the itch and what can bring relief.
Darker Skin Tones
- Skin care secrets
- Hair care
- Hair loss
- Diseases & Conditions
- Acne
- Dark spots
- Dry skin
- Light spots
- Razor bumps
- Caring for Black hair
- Scalp psoriasis
- Weaves & extensions
- Central centrifugal cicatricial alopecia
- Frontal fibrosing alopecia
- Hairstyles that pull can cause hair loss
- Acanthosis nigricans
- Acne keloidalis nuchae
- Hidradenitis suppurativa
- Keloid scars
- Lupus and your skin
- Sarcoidosis and your skin
- Skin cancer
- Vitiligo
- More diseases & conditions
Featured
Fade dark spotsFind out why dark spots appear and what can fade them.
If you have what feels like razor bumps or acne on the back of your neck or scalp, you may have acne keloidalis nuchae. Find out what can help.
Cosmetic treatments
- Your safety
- Age spots & dark marks
- Cellulite & fat removal
- Hair removal
- Scars & stretch marks
- Wrinkles
- Younger-looking skin
Featured
Laser hair removalYou can expect permanent results in all but one area. Do you know which one?
Do you know which one?
If you want to diminish a noticeable scar, know these 10 things before having laser treatment.
BotoxIt can smooth out deep wrinkles and lines, but the results aren’t permanent. Here’s how long botox tends to last.
Public health programs
- Skin cancer awareness
- Free skin cancer screenings
- Kids' camp
- Good Skin Knowledge
- Shade Structure grants
- Skin Cancer, Take a Hike!™
- Awareness campaigns
- Flyers & posters
- Get involved
- Lesson plans and activities
- Community grants
Featured
Free materials to help raise skin cancer awarenessUse these professionally produced online infographics, posters, and videos to help others find and prevent skin cancer.
Free to everyone, these materials teach young people about common skin conditions, which can prevent misunderstanding and bullying.
Find a dermatologist
- Find a dermatologist
- What is a dermatologist?
- FAAD: What it means
- How to select a dermatologist
- Telemedicine appointments
- Prior authorization
- Dermatologists team up to improve patient care
Featured
Find a DermatologistYou can search by location, condition, and procedure to find the dermatologist that’s right for you.
A dermatologist is a medical doctor who specializes in treating the skin, hair, and nails. Dermatologists care for people of all ages.
Baby Eczema Symptoms, Causes, Treatments, Creams, and More
Series Eczema in Babies
Written by WebMD Editorial Contributors
Eczema can show up as crusty, flaky patches on your baby's skin, often during their first few months. It’s common and treatable. Many infants outgrow it.
Not sure if your baby's itchy, irritated rash is eczema? Your doctor can tell you for sure. These questions and answers can help you understand what to look for.
What Does Baby Eczema Look Like?
Eczema doesn't look the same on every baby. In babies with light skin, it usually shows up as patches of red skin. In darker-skinned babies, the rash might look purplish, brownish, or grayish. Eczema can be harder to see on babies with dark skin.
These patches are almost always dry, itchy, and rough.
Babies can get the condition just about anywhere on their body. Most often, it affects their cheeks and the joints of their arms and legs.
It’s easy to confuse baby eczema (also called infant eczema or atopic dermatitis) with cradle cap. But there are some key differences.
Cradle cap is much less itchy and irritated. It generally clears up by age 8 months and usually appears on the scalp, sides of the nose, eyelids and eyebrows, and behind the ears. See a photo of what cradle cap looks like.
Causes
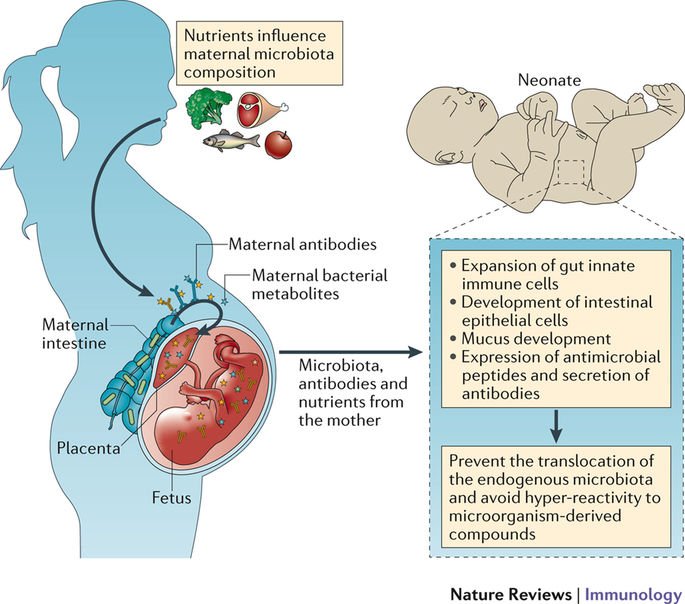
It can run in families. If a parent has eczema, a baby is a lot more likely to get it, too.
Problems in the skin barrier, allowing moisture out and germs in, could also be a cause.
Eczema happens when the body makes too few fatty cells called ceramides. If you don’t have enough of them, your skin will lose water and become very dry. Read more on what causes eczema.
Does Baby Eczema Go Away by Itself?
It often does. Most children outgrow it before they start school.
Most children outgrow it before they start school.
It’s not common, but some kids will have eczema into adulthood. They may have times -- even years -- without the symptoms. But they may still tend to have dry skin. Get more information on kids, allergies, and eczema.
What Can Make It Worse
Each baby is different. But there are some common eczema triggers to avoid, including:
Dry skin. It can make a baby's skin itchier. Low humidity, especially during winter when homes are well-heated and the air is dry, is a cause.
Irritants. Think scratchy wool clothes, polyester, perfumes, body soaps, and laundry soaps. These can all trigger symptoms.
Stress. Children with eczema may react to stress by flushing. That can lead to itchy, irritated skin. And that, in turn, ramps up their eczema symptoms.
Heat and sweat. Both can make the itch of infant eczema worse.
Allergens. It’s not certain, but some experts believe that removing cow’s milk, peanuts, eggs, or certain fruits from a child’s food may help control eczema symptoms. Remember that your baby can get exposed to these foods if their mother eats them before they breastfeed. Find out the connection between food and eczema flares.
Remember that your baby can get exposed to these foods if their mother eats them before they breastfeed. Find out the connection between food and eczema flares.
Home Treatment
Give your little one's skin some TLC. That’s the first step in treating their eczema. Try:
Moisturizers. One with ceramides is the best option. These are available over the counter and by prescription. Otherwise, a good moisturizer, fragrance-free cream, or ointment such as petroleum jelly, when used several times daily, will help your baby's skin retain its natural moisture. Apply immediately after a bath.
A lukewarm bath. This hydrates and cools the skin. It may also ease itching. Make sure the water isn’t too hot! Keep the bath short -- no more than 10 minutes. To soothe itchiness even more, try adding oatmeal soaking products to your baby's tub.
Use mild, unscented body and laundry soaps. Perfumed, deodorant, and antibacterial soaps can be rough on a baby's sensitive skin.
Clean carefully. Use soap only where your baby may be dirty, such as the genitals, hands, and feet. Simply rinse off the rest of your child's body.
Dry off. Pat skin dry. Don't rub.
Dress for comfy days. To avoid the irritation of clothing rubbing on the skin, your child should wear loose clothes made of cotton.
Always wash new clothes before you put them on your baby. Use a mild, fragrance-free detergent.
To keep your little one comfy, don’t overdress them or use too many blankets. If they get hot and sweaty, that can trigger an eczema flare. Learn more about natural skin care for babies.
What to Do About Itching
Try to keep your baby from scratching their itchy skin. Scratching can make the rash worse, lead to an infection, and cause the irritated skin to get thicker and more leathery.
Trim their nails often, and then take the edge off of them with a file if you can. Some parents also slip "scratch mittens" onto their little one's hands. Others try long socks, tucked in under a long-sleeved shirt, so they're harder for a baby to remove. View a slideshow to get more eczema skin care tips.
Others try long socks, tucked in under a long-sleeved shirt, so they're harder for a baby to remove. View a slideshow to get more eczema skin care tips.
Medicines
Some over-the-counter products, such as hydrocortisone creams and ointments, target itching and inflammation. Check the instructions and don’t use them too long, or they can thin the skin in the affected area.
There are also medicines that need a doctor’s prescription, if other treatments don’t work.
When to Call a Doctor
Make the call if your baby’s eczema doesn’t begin to get better within a week of starting over-the-counter hydrocortisone creams. It may be time for a prescription medicine.
Also check with your doctor if yellow or light brown crust or pus-filled blisters appear on top of the eczema. This could be the sign of a bacterial infection that needs antibiotics.
You should call your doctor if your baby is around anyone who has cold sores or genital herpes. Eczema can make your little one more likely to pick up those germs.
Exacerbation of eczema in children: causes, symptoms, recommendations for care - Care for children and expectant mothers - Blog
Eczema is one of the most common and at the same time the most “mysterious” skin diseases. At the moment, it is diagnosed in 20% of babies, but modern medicine does not have the means to completely cure it. So, faced with eczema in a child, parents will have to constantly pay attention to caring for his skin and closely monitoring the symptoms. nine0003
What is eczema?
Eczema is a non-contagious inflammatory skin disease characterized by various types of rash, burning sensation and itching. Translated from Greek, the word eczema means "boiling": the rash that occurs with some of its types really resembles small air bubbles in boiling water.
In 65% of cases, the symptoms of the disease manifest themselves in infancy (up to a year), and 90% of young patients "outgrow" eczema by the time they reach the age of five.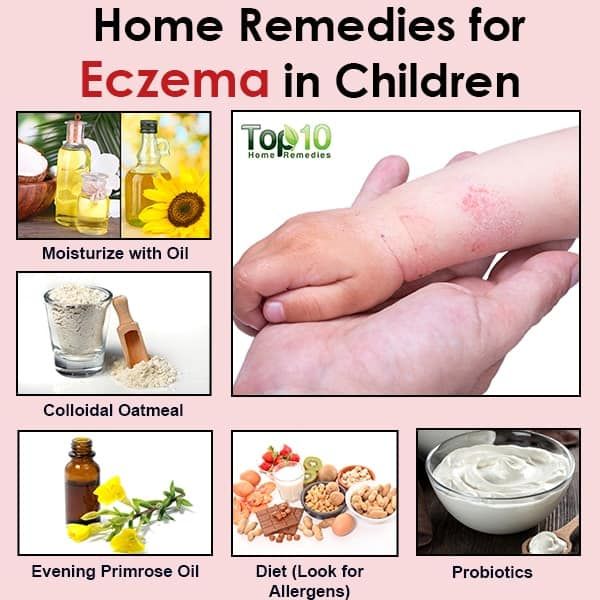 nine0003
nine0003
In order to alleviate the unpleasant symptoms of the disease and make the periods of exacerbation more comfortable and calm for the baby and the whole family, it is important to strictly follow the recommendations of a pediatrician or pediatric dermatologist, as well as adhere to some basic rules in everyday life.
Provoking factors
As we mentioned above, a significant prerequisite for the development of eczema in childhood is a genetic predisposition. Most often, this disease has an allergic nature. nine0003
The main factors that can lead to exacerbation of eczema:
- dry skin
- contact with irritating chemicals (in the composition of soaps, bath foams, washing powders, etc.)
- eating or contact with foods to which the child is allergic
- contact with plant pollen, house dust, animal hair, dust mite faeces
- contact with woolen or synthetic fabrics
- Ambient temperature too high or too low
- transferred stress
Signs and symptoms
Manifestations of eczema vary in different age periods:
In infants, it usually occurs between 3 and 6 months of age and is a small red spot that is dry and rough to the touch. As the disease develops, their number increases, and the surface is covered with bubbles with a clear liquid. If their integrity is violated (independently or due to scratching), the surface of the skin becomes wet, wet. nine0003
As the disease develops, their number increases, and the surface is covered with bubbles with a clear liquid. If their integrity is violated (independently or due to scratching), the surface of the skin becomes wet, wet. nine0003
At this age, foci of inflammation are located on the cheeks and limbs, less often on the body. Since the child's immunity is weak and fragile, in the first months of life, eczema is often accompanied by a secondary infection.
Upon reaching one and a half to two years, rashes on the cheeks are less common, gradually moving to the limbs. The foci of damage are often the wrists and hands, bends of the elbows and knees. Excessive surface moisture is less typical, on the contrary, the skin becomes excessively dry, painful cracks may appear. The picture is aggravated by constant scratching, which is difficult for the child to control. nine0003
By adolescence, the symptoms of eczema can completely disappear: the body gets stronger, the immune system begins to work normally, and the child "outgrows" the disease. If this does not happen, foci of inflammation, manifested in the form of red scaly areas, a blistering rash and weeping spots, can appear on the wrists and hands, cheeks, forehead and chin, on the chest and between the shoulder blades, on the bends of the elbows and knees.
If this does not happen, foci of inflammation, manifested in the form of red scaly areas, a blistering rash and weeping spots, can appear on the wrists and hands, cheeks, forehead and chin, on the chest and between the shoulder blades, on the bends of the elbows and knees.
Eczema in children is manifested by symptoms of true, seborrheic and microbial eczema. nine0003
- True eczema is a reddening of the skin that does not have distinct boundaries. Accompanied by peeling, rash in the form of bubbles. For children, especially characteristic is the separation of fluid, "wetting" the surface of inflammation. Yellowish-brown crusts may also occur. As a rule, it primarily affects the cheeks and forehead (bypassing the nasolabial triangle), subsequently spreading to the scalp, auricles, neck, torso, folds of the limbs and buttocks. Its appearance is most often associated with the nutrition of the child. Moreover, the reaction can be caused by both the introduction of complementary foods and a change in the composition of breast milk.
 nine0022
nine0022 - Seborrheic eczema is characterized by dry, red, scaly patches covered with greasy, white or yellow scales. They appear in places where the sebaceous glands accumulate: on the scalp, forehead, cheeks, auricles, behind the ear and neck folds.
- Microbial eczema manifests itself in the form of asymmetric rashes provoked by the ingress of microbes into wounds, abrasions, scratches or burns on the skin. The lesions have clear boundaries, often located on the arms and legs. nine0022
Any form of eczema is also characterized by itching and burning - depending on the degree of damage, their intensity may vary, but almost always they cause discomfort to the child, he becomes capricious and irritable, cannot sleep.
Stages of development of eczema
By identifying the symptoms of eczema in the early stages, treatment is much easier. As the disease progresses, the likelihood of complications, microbial and infectious inflammation increases. nine0003
nine0003
| Stage | Characteristic |
| 1. Erythrematous | Extensive reddening of the skin. Area of irritated skin without clear boundaries. | nine0081
| 2. Papular | A nodule-like rash is added. Small foci can merge with each other, forming plaques. Increased swelling. |
| 3. Vesicular | Nodules transform into vesicles with clear or whitish fluid. nine0003 |
| 4. | Vesicles burst, leaving areas of damaged skin exuding fluid (serous wells) in their place. |
| 5. Crustose | As the liquid dries, crusts form on the surface of the skin. nine0003 |
| 6. Squamous | Dried crusts peel off, forming whitish scales. |
Basic recommendations for eczema in a child
Eczema is one of the chronic diseases that cannot be completely cured. However, a combination of drug treatment, physiotherapy and basic home care can significantly alleviate the condition and practically nullify the symptoms and bring the disease into remission. nine0003
nine0003
Consultation with a specialist: eczema is easily confused with other conditions: diaper rash, white lichen, ichthyosis, etc. All these diseases require a different approach to treatment, so when the first symptoms appear, you should contact your pediatrician and get the doctor's recommendations. He will be able to determine the nature of the disease and the factors provoking its exacerbation of the disease and select the appropriate treatment.
Proper nutrition: try to eliminate potential allergens from the baby's (or mother's, if breastfeeding) diet. Your doctor will also help you develop a safe diet. nine0003
Regular cleansing: Bathing daily is an easy way to help partially relieve rashes and other symptoms of eczema. An important nuance: you should not use hot water, as it, in fact, dries fragile skin even more.
Natural fabrics: It is best if the child's clothes and bedding are made of cotton or other soft natural materials. Cotton mittens and socks will also help to solve the problem of combing.
Cotton mittens and socks will also help to solve the problem of combing.
Maintain optimal humidity: dry air in a heated room can lead to excessive dryness of the skin, which in turn increases irritation and itching. It is a good idea to put a humidifier in the children's room to maintain optimal moisture levels. And if you need to calm the itching urgently, you can attach a soft towel moistened with cool water to the dry area for several minutes. nine0003
Baby skin care for eczema
Bathing
To soften crusts and prevent discomfort from contact with water, a special moisturizing oil can be applied shortly before bathing.
Gentle almond oil spray with vitamin E for babies from the first days of life, 75 ml
Nourishes the skin, suitable for massage nine0003
570 ₽ -fifty% 1140 ₽
Buy nine0003
12345
nine0166 Emollient bath and shower oil for dry and atopic skin of babies, children and adults AP+, 200 mlGENTLE CLEANSING AND SOFTENING DRY SKIN
948 ₽ -twenty% 1185 ₽
nine0168 Buy12345
Products used to cleanse sensitive skin of a child must not contain soap and aggressive surfactants. Also avoid excessive exposure to water - during prolonged contact with water, lipids are washed out of the skin, leading to a decrease in its barrier function.
Also avoid excessive exposure to water - during prolonged contact with water, lipids are washed out of the skin, leading to a decrease in its barrier function.
Cleansing foaming cream for children and newborns 1 l
Gentle cleansing for delicate skin. gives softness and elasticity nine0003
2250 ₽ -thirty% 3215 ₽
Buy nine0003
12345
nine0166 Cleansing gel for face and body, 200 mlGENTLY CLEANSES, DOES NOT CAUSE IRRITATION, REDUCES SKIN REACTIVITY
859 ₽ -thirty% 1227 ₽
nine0168 Buy12345
nine0166 Washing gel for babies from the first days of life 500 mlCAREFULLY CLEANSES, SOFTENES AND MOISTURIZES BABY'S TENDER SKIN
1241 ₽ -thirty% 1773 ₽
nine0168 Buy12345
Use a soft towel to dry off, dabbing lightly on the skin.
Moisturizing and softening
Use lotions and emollient creams to prevent drying of the skin after bathing and relieve the discomfort caused by dryness. They should be applied in a thick layer with light circular movements, without rubbing, so as not to disturb the integrity of fragile skin.
nine0166 Stelatopia Emollient cream 200 mlProvides long lasting moisturizing effect
1480 ₽ -thirty% 2115 ₽
nine0168 Receipt expected nine0166 Nourishing protective body milk, 350 mlMoisturizes and nourishes baby's skin
1087 ₽ -fifty% 2175 ₽
nine0168 Receipt expected nine0166 Cold cream body 200 mlNOURISHES, SOFTENS AND PROTECTS BABY'S SKIN
1485 ₽ -thirty% 2122 ₽
nine0168 Buy12345
Protection against negative environmental factors
Exposure to cold and wind can cause skin dryness and flaking. Special protective creams will help strengthen the barrier function of the skin.
Special protective creams will help strengthen the barrier function of the skin.
nine0003
Cream for sensitive skin 0+, 100 g
Soothes, moisturizes, relieves itching
756 ₽
Buy nine0003
123
nine0166 Nutri-Protectrice Cold Cream, 50 mlnourishes and protects dry and sensitive skin from wind and frost
367 ₽ -fifty% 735 ₽
nine0168 Receipt expected Despite the chronic, relapse-prone nature of the disease, with timely and proper treatment, it will not cause discomfort to the child. Tracking and eliminating irritating factors will not allow irritation to spread, and complex therapy that combines delicate care, daily application of moisturizers and proper hygiene can almost completely get rid of the unpleasant symptoms of eczema. nine0003
Tracking and eliminating irritating factors will not allow irritation to spread, and complex therapy that combines delicate care, daily application of moisturizers and proper hygiene can almost completely get rid of the unpleasant symptoms of eczema. nine0003
90,000 is useful to know about EKSEM (EKSEM)
It is useful to know about eczema ( EKSEM)
Useful information about the Norwegian Union of Astmatics and Allergies 9021?
Eczema is the general term for various itchy skin conditions. The most common forms of eczema are atopic, occupational (contact), seborrheic, and childhood. Atopy means "difference". In this case, it refers to differences in skin properties and describes hereditary allergic eczema. nine0003
Eczema may be chronic ie. with a long, or acute form of the course of the disease and in most cases is characterized by improvement in the summer and deterioration in winter. The chronic form is characterized by the appearance of a rash with itching. The result of scratching is often the formation of thickened areas of the skin that crack easily. Acute eczema is characterized by itching, redness and swelling of the skin with the possible formation of watery blisters.
The chronic form is characterized by the appearance of a rash with itching. The result of scratching is often the formation of thickened areas of the skin that crack easily. Acute eczema is characterized by itching, redness and swelling of the skin with the possible formation of watery blisters.
In eczema, there is a deterioration in the body's defense against infections, which easily leads to infectious inflammation, which can lead to a worsening of eczema.
Symptoms of eczema
Atopic eczema results in itchy, dry skin.
New or recurrent contact eczema is characterized by itching, redness and swelling of the skin with the formation of small and large blisters, as well as wet sores in places of direct exposure to the allergen. With prolonged contact eczema, the skin becomes increasingly dry and cracked. Severe itching is common. In the initial stage, eczema is observed only on the area of \u200b\u200bthe skin that was exposed to the allergen, but then the rash can spread to other areas. nine0003
nine0003
With seborrheic eczema in infants, there is the formation of oily, red skin covered with greasy crusts on the forehead, head, face, and also in the folds of the skin on the neck and in the perineum. In adults, it appears as scaly, red, oily skin on the central areas of the face, on the head, behind the ears, and on the chest.
Baby eczema is accompanied by the formation of red, smooth, sometimes wet areas of the skin in diaper wear areas. nine0003
Who can get eczema?
Atopic eczema primarily affects young children. It is estimated that about 15% of Norwegian children suffer from eczema. Often the disease occurs in children in the first months of life, in 60% of them it disappears by the age of four. However, recurrence of the disease may occur in adolescence or adulthood.
Contact eczema is rare in young children, but its occurrence is becoming more common from school age. Ear piercings, body piercings and base metal contact with the skin are responsible for a significant increase in nickel contact allergies.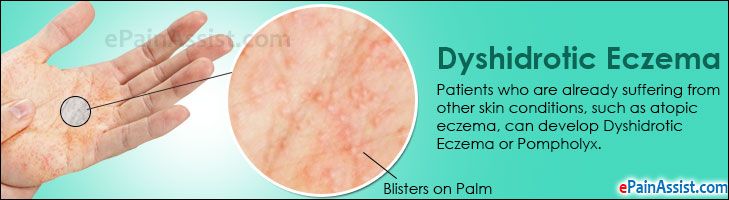 Getting a tattoo can lead to allergic contact eczema, which can occur weeks or even months after getting a tattoo. Hair coloring is also an increasingly common cause of eczema, especially as more and more young people dye their hair. nine0003
Getting a tattoo can lead to allergic contact eczema, which can occur weeks or even months after getting a tattoo. Hair coloring is also an increasingly common cause of eczema, especially as more and more young people dye their hair. nine0003
Seborrheic eczema is relatively common. Eczema can appear as early as the first months of life, but usually occurs in adults.
Causes of eczema
The cause of atopic eczema is unknown. Allergies can play a role, but only in conjunction with other factors. The disease has a connection with heredity and the environment. The presence of atopic diseases in other family members (asthma, eczema or allergic rhinitis) is common. In 20-30% of patients, allergies can be detected, which for some of them may be the cause of eczema. Food allergies are never the only cause of eczema. nine0003
Seborrheic eczema is not caused by hypersensitivity, but by a painful reaction in the sebaceous glands, possibly caused by a specific yeast usually found on the surface of the skin.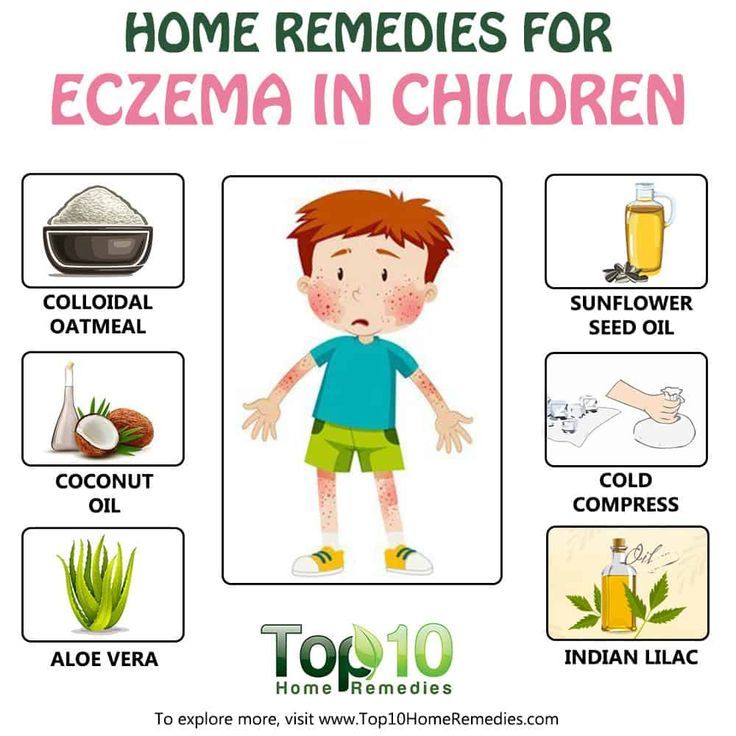 This form of eczema is especially prone to people with oily skin and increased productivity of the sebaceous glands.
This form of eczema is especially prone to people with oily skin and increased productivity of the sebaceous glands.
Contact eczema occurs when the skin reacts to contact with certain substances. The reaction may be allergic or non-allergic. A non-allergic reaction occurs in direct contact with skin irritating substances such as detergents or disinfectants. An allergic reaction is caused by allergenic substances such as nickel, chromium, rubber, formaldehyde and perfumes. Paraphenylenediamine (PPD) is one of the substances frequently associated with allergic contact eczema. PPD is found in many types of hair dye. nine0003
Children's eczema is caused by irritants found in urine and feces.
Treatment of eczema
In the treatment of eczema, hygiene, the systematic use of creams and ointments to prevent drying of the skin, refraining from scratching, reducing exposure to irritants, and refraining from eating foods known to be allergic, are the most important. Sunlight and salt baths work well for mild to moderate eczema. Regular bathing with calcium permanganates gives a good preventive effect. nine0003
Sunlight and salt baths work well for mild to moderate eczema. Regular bathing with calcium permanganates gives a good preventive effect. nine0003
However, in most cases a cortisone ointment is necessary. The indicated treatment will give the desired result, provided that the correct drug is applied to the appropriate area of \u200b\u200bthe body at the prescribed frequency. Once control of eczema is established, it is important to reduce the concentration of cortisone ointment, and, if necessary, increase the intervals between applications of the ointment. Proper use of cortisone ointment does not lead to negative effects. The attending physician will give you the necessary recommendations for the use and reduction of the concentration of the drug. nine0003
In general terms, it can be said that it is necessary to use strong drugs for a sufficiently long period of time. By opting for weaker drugs, you will not be able to get eczema under control. In this case, the whole process of cortisone treatment may be in vain. Often this leads to increased eczema. It is important to remember that the poor effect of cortisone ointment is due to infection in the eczema itself, which should be treated with antibiotics, both locally and in general. nine0003
Often this leads to increased eczema. It is important to remember that the poor effect of cortisone ointment is due to infection in the eczema itself, which should be treated with antibiotics, both locally and in general. nine0003
In the event of a new flare-up of eczema in a child with a history of the condition, treatment may be initiated with cortisone group 2 or 3. Once the condition has stabilized, the application may be made less frequently (at intervals of 2-3 days). With further improvement in the condition, you can switch to a weaker ointment in order to eventually switch to applying the drug with an interval of 2-3 days.
After healing of eczema, it is recommended to continue applying the drug 1-2 times a week for at least 2-4 weeks, in order to achieve the best result. It is also recommended to use a moisturizer in the morning and evening, as well as every time after taking a bath or shower, even during periods without eczema. nine0003
Children suffering from eczema that regularly flares up and worsens benefit from calcium permanganate baths even during good times.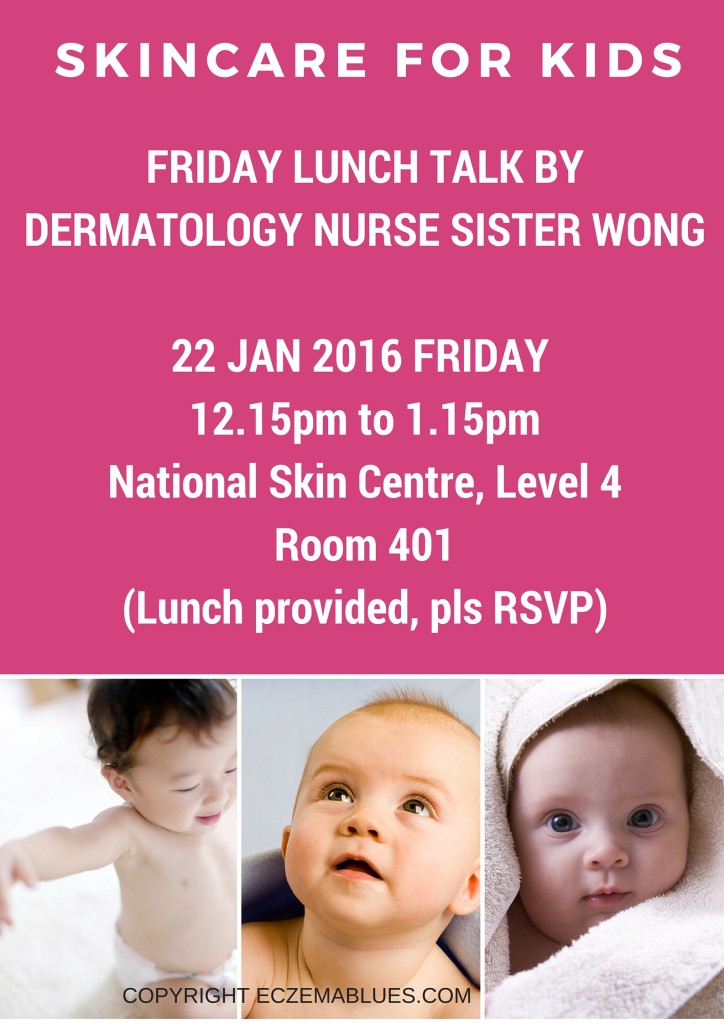 During periods of active eczema, baths with calcium permanganate can be done every day or every other day.
During periods of active eczema, baths with calcium permanganate can be done every day or every other day.
Cortisone-free anti-eczema ointments (Elidel®, Protopic®) are good alternatives to try for chronic eczema. These ointments are applied daily, twice a day. The advantage of these ointments is that they do not affect the thickness of the skin even with prolonged use, and also that they can be used in cases where treatment with cortisone ointments does not lead to the desired result and control of eczema is not established by treatment with cortisone ointments without risk. side effects. nine0003
For skin infections, the infection itself must be treated first, and then the above remedies should be applied.
Medical light or climate treatments for eczema may work. However, some patients may experience a temporary increase in eczema, which is probably due to sweat irritation. In addition, such treatment requires a lot of money and time, which makes it unacceptable for school-age children. This treatment is carried out exclusively by doctors specializing in skin diseases. nine0003
This treatment is carried out exclusively by doctors specializing in skin diseases. nine0003
Achieving positive results depends on how well the patient is informed about the treatment. Eczema can be a very debilitating disease, but early treatment can in most cases bring it under control. Fortunately, the disease eventually subsides on its own, and 80% of patients recover by the age of 18. There is evidence to suggest that quality treatment of eczema leads to an improved prognosis.
Aggravating factors
Rough, tight clothing, rough wools, polyester, heavily dyed fabrics, humidity, stress, infections, food, chlorinated water, tobacco smoke, perfumes, allergies, alkaloid soaps, degreasing chemicals and exposure to heat.
The child knows what clothes cause itching!
Prevention of eczema
Prevention of eczema by controlling the mother's diet during pregnancy, or after the birth of the child, has no effect on the development of atopic eczema in the child. Research shows that symptoms of atopic eczema may be delayed in some cases in children who are breastfed for the first four to six months of life. nine0003
Research shows that symptoms of atopic eczema may be delayed in some cases in children who are breastfed for the first four to six months of life. nine0003
Where to get help
For mild sporadic eczema in children, getting advice from a nurse may be enough. In more complex cases, you should contact your doctor, who, if necessary, will write a referral to a specialist. The hospital free choice system in Norway allows for informed choice. On the Internet site www.frittsykehusvalg.no and free of charge on 800 41 004, you can find out about available eczema treatment sites and your rights in choosing a hospital. nine0003
People suffering from eczema and other skin diseases, as well as people who work with this group of patients, can communicate with specialists at the skin disease clinic, Villa Derma, Oslo University Hospital, by contacting the “skin phone” 23075803 , open for calls three hours a week according to the following schedule: Tuesday and Friday from 8 am to 9 am, Thursday from 12 am to 1 pm (check that this schedule is correct!).
 Wet
Wet