Cold sore while breastfeeding
Herpes Simplex Virus (HSV) | Breastfeeding
Herpes simplex virus (HSV) is a lifelong virus that is categorized into two distinct herpesvirus species, herpes simplex virus 1 (HSV-1) and herpes simplex virus 2 (HSV-2). HSV-1 is typically transmitted by oral-oral contact to cause oral herpes but can also cause genital herpes through oral-genital contact. HSV-2 is typically sexually transmitted and causes genital herpes but can also cause infections in the mouth. Importantly, both types of virus can cause herpes disease in newborns and infants and can appear anywhere on the body.
In newborn infants, HSV infections are often severe and result in high rates of mortality and morbidity. Every precaution needs to be taken to prevent infants from being exposed to the herpes virus and appropriate hand hygiene should be done before holding the infant.
Is it safe for a mother to breastfeed if she has active herpetic lesions?
Maybe. Women with herpetic lesions may transmit HSV to their infants by direct or indirect contact with the lesions. Breastfeeding is acceptable if no lesions are present on the breasts and if active lesions elsewhere on the mother are carefully and fully covered. In cases where a mother has herpetic lesions on her breast, the mother should temporarily refrain from breastfeeding her infant from the affected breast or feeding her infant expressed breast milk from the affected breast. She should discard expressed breast milk from the affected side until the lesions have healed. A mother may breastfeed her infant or express milk from the unaffected breast but should ensure that the lesions on the affected breast are completely covered to avoid transmission. Mothers should also follow appropriate hand hygiene practices to avoid transmission of herpes to her infant.
Providers: Lesions on the breast could easily be mistaken for impetigo or eczema. Questionable lesions should be tested promptly for HSV so that if positive, acyclovir (safe to use while breastfeeding) can be administered quickly and breastfeeding can be discontinued until the lesion has healed.
Some mothers may need additional support to maintain their milk production and/or supplement with their expressed human milk (previously expressed milk or expressed milk from the unaffected breast) or formula while herpetic lesions on the breast are healing. Mothers should talk with their physicians to determine if their lesions have healed and they can resume breastfeeding or expressing milk from the affected breast.
Is it safe for a mother to give her infant hand expressed or pumped breast milk if she has active herpetic lesions on her breast?
No. Breast milk can be contaminated if it comes in contact with active herpetic lesions through touching the breast during hand expression or via the pump. Therefore, if a mother has herpetic lesions on her breast, she should discard expressed breast milk from the affected side until the lesions have healed. Expressing breast milk will be important for maintaining milk production while not directly breastfeeding from the affected breast. Mothers should be vigilant about practicing appropriate hand hygiene and cleaning the pump parts thoroughly. Mothers should talk with their healthcare provider to determine if their lesions have healed and they can resume breastfeeding or expressing milk from the affected breast.
Mothers should be vigilant about practicing appropriate hand hygiene and cleaning the pump parts thoroughly. Mothers should talk with their healthcare provider to determine if their lesions have healed and they can resume breastfeeding or expressing milk from the affected breast.
It is safe to use expressed breast milk from the unaffected breast, as long as the mother ensures that the lesions on the affected breast are completely covered to avoid transmission. Appropriate hand hygiene and cleaning the pump parts thoroughly are still important.
For more information about managing breastfeeding with specific medical conditions, read Lawrence RA, Lawrence R. (2016) Breastfeeding: A guide for the medical profession, 8th Edition.
Cold sores in pregnancy | Pregnancy Birth and Baby
Cold sores in pregnancy | Pregnancy Birth and Baby beginning of content6-minute read
Listen
What is HSV?
If you or your partner has the virus that causes cold sores or genital herpes, you might be worried about what could happen when you're pregnant or have a new baby.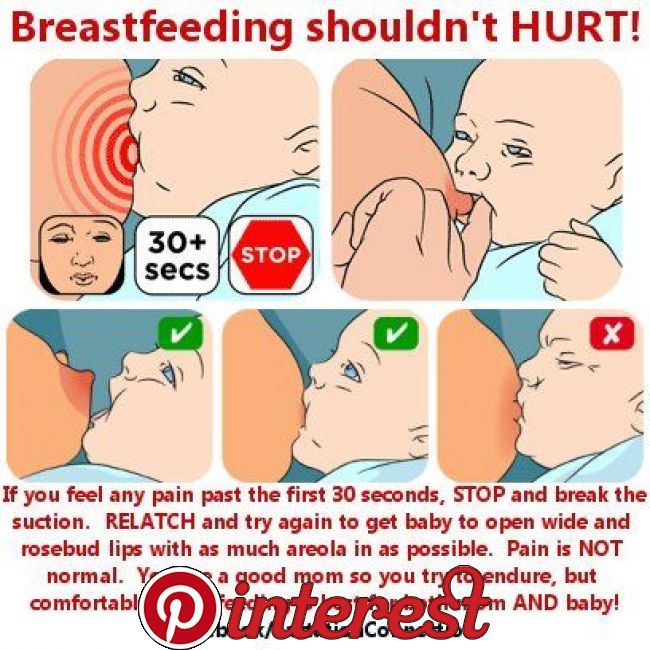 Here's what you need to know about herpes simplex virus (HSV), and how to protect your baby from infection.
Here's what you need to know about herpes simplex virus (HSV), and how to protect your baby from infection.
The herpes simplex virus is a very common virus carried by most people. Sometimes it causes cold sores or genital herpes.
Cold sores are blisters that form on the lips, around the mouth and nose. Genital herpes is blisters or sores around the genitals or anus. The blisters may form a crust after about 3 days. The sores go away by themselves within 2 weeks.
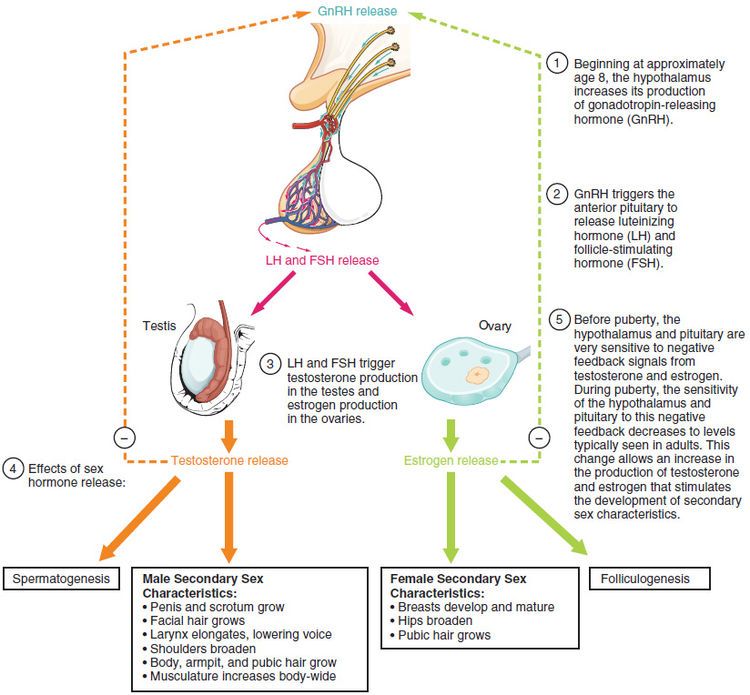
There are two main types of HSV:
- HSV-1 causes mostly cold sores on the face and lips, and sometimes on the genitals
- HSV-2 causes mostly genital herpes
Both viruses are transferred though contact of the skin, saliva or genitals, and the viruses stay in the body for life. The viruses do not always cause symptoms, so you can carry the virus without knowing it.
HSV-1 is very common, with about 8 in 10 Australians carrying it in their bloodstream. But only 1 in 3 people with the virus has ever had a cold sore. HSV-2 is less common.
HSV-2 is less common.
It is common for women who have had cold sores in the past to experience an outbreak while pregnant.
What happens if I get cold sores or genital herpes during pregnancy?
Having the HSV virus does not affect your chance of becoming pregnant.
It is quite common for women to have a cold sore during their pregnancy, even if they haven’t had one for a long time. Cold sores should not affect your unborn baby. But they are infectious, so it’s a good idea to treat them.
Genital herpes should not affect the baby if you have your first outbreak or it comes back in the first 34 weeks. But it can be transferred to your baby during the birth, especially if it’s your first outbreak.
If you've ever had a cold sore or genital herpes and you become pregnant, or you develop these conditions during pregnancy, it's important to tell your doctor or midwife about it. Together you can make a plan for managing herpes during pregnancy and birth.
How is HSV treated during pregnancy or breastfeeding?
You can treat cold sores and genital herpes with:
- aciclovir cream, available from a pharmacist without prescription
- aciclovir or valaciclovir tablets, for which you need a prescription
These 'antiviral' drugs are known to be safe for pregnant and breastfeeding women and are effective most of the time.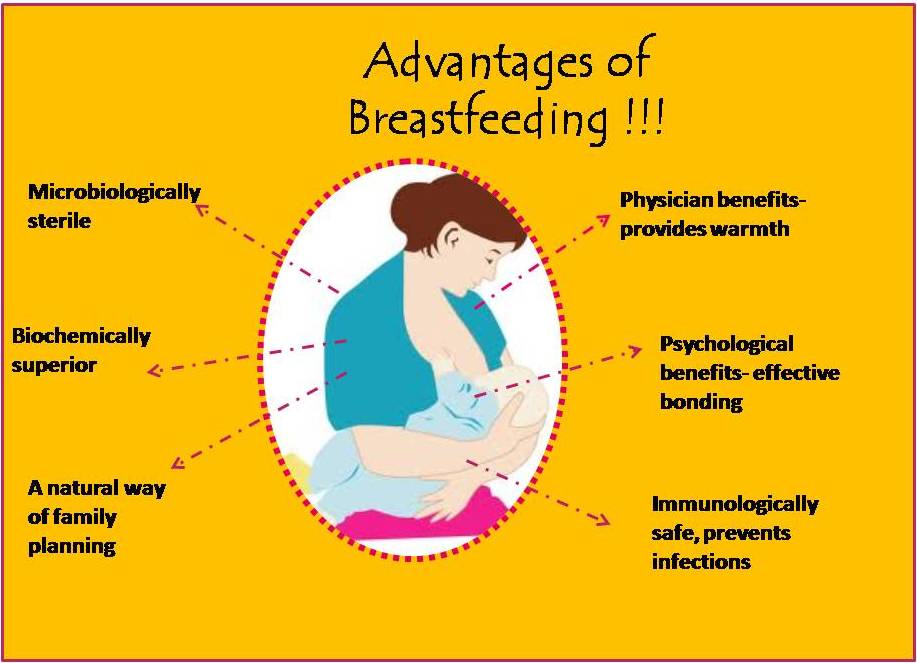
Famciclovir tablets are not recommended to take during pregnancy. Speak to your doctor if the cold sore is severe.
How is genital herpes treated during pregnancy?
You should take acyclovir or valaciclovir tablets, as above.
If it's your first outbreak of genital herpes, your baby may be more at risk because you haven't had time to develop immune protection against the virus, which also helps protect the baby.
Some women experiencing an outbreak of genital herpes might be advised to have a caesarean. This would prevent the herpes virus passing from mother to baby during a vaginal birth. But most women in Australia with genital herpes do give birth safely to healthy babies vaginally.
It's often recommended that women who have ever had genital herpes take antiviral tablets prior to the birth, even if the herpes isn't active at the time.
Talk to your doctor or midwife about the best course of action for your situation.
How do I protect my baby from herpes?
Herpes can cause serious problems in a baby, such as infections to the eyes and throat, brain damage and even death.
A newborn baby can catch HSV-1 and HSV-2 from being kissed or touched by someone with cold sores, or during childbirth.
Fortunately, most babies born to women who carry the virus are not affected. But if you or your partner has a cold sore or genital herpes, talk to your doctor about keeping it under control during the pregnancy and after the birth. It is also important to treat these conditions aggressively while you are breastfeeding.
It's important to maintain strict hygiene habits when caring for a new baby if you, or anyone in close contact with the baby, have cold sores.
If you have cold sores, you should:
- cover cold sores when you're around the baby
- avoid kissing your baby until the sores are completely healed
- avoid touching the cold sores then touching your baby
- wash your hands thoroughly before touching your baby
What if I have a cold sore while breastfeeding?
If you have cold sores, it is safe to breastfeed your baby as long as the cold sores are not on the breast or nipple.
If they are, it may be wise to breastfeed from the unaffected nipple only until the lesions have cleared up. You would express and dispose of breastmilk from the affected nipple. Breastmilk itself doesn't contain the herpes virus but it can be contaminated through the skin lesions.
Talk to your doctor or midwife as soon as you notice any cold sores on your breast or nipple.
What happens if my baby gets herpes?
It is very important that herpes in a newborn is recognised and treated by a doctor in hospital immediately. Signs of herpes in a newborn include:
- blisters on the skin
- fever
- irritability
- tiredness
- lack of appetite
If you think your baby might have the herpes virus, don't wait to see if they get better — seek medical help. Tell medical staff if you or your partner carry the herpes virus.
Resource and Support
If you are worried about your baby, see a doctor or midwife, or take them to the hospital.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
If you're not sure what to do or want more information, you call Pregnancy Birth Baby on 1800 882 436 to speak with a maternal child nurse.
Sources:
Family Planning NSW (Genital herpes), The Royal Woman’s Hospital (Genital herpes), Mothersafe (Cold sores in pregnancy and breastfeeding), Queensland Government Health (Genital Herpes and Pregnancy), SA Health (Cold sores (herpes simplex type 1) - including symptoms, treatment and prevention), Safer Care Victoria (Herpes simplex virus in neonates)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2021
Back To Top
Need more information?
Genital Herpes (HSV) | Body Talk
Genital herpes is a common STI caused by the Herpes Simplex Virus (HSV). Find out all the facts about Genital Herpes here.
Find out all the facts about Genital Herpes here.
Read more on Body Talk website
Cold sores - Better Health Channel
Cold sores are blisters around the mouth and nose, caused by the herpes simplex virus.
Read more on Better Health Channel website
Cold sores overview - MyDr.com.au
A cold sore is a skin infection that is caused by the herpes simplex virus (HSV). Cold sores usually occur on or around the lips or nose and are very common. They have nothing to do with colds.
Read more on myDr website
Cold sores: self-care - MyDr.com.au
Cold sores are caused by the herpes simplex type 1 virus. Most people carry this virus in their bodies.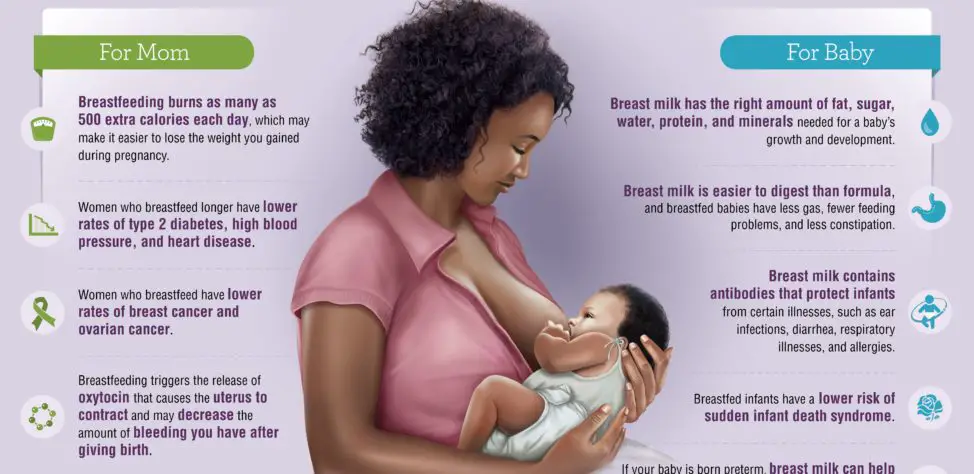 Find out what products are available for cold sores.
Find out what products are available for cold sores.
Read more on myDr website
Cold sores | SA Health
Herpes simplex virus type 1 (HSV1) causes cold sores on the face or lips - it is spread by skin or mucous membrane contact with infected saliva
Read more on SA Health website
Cold sore infections - MyDr.com.au
Find the answers to common questions about cold sores, irritating blisters which are caused by the herpes simplex type 1 virus and can be triggered by stress, fatigue or exposure to sunlight.
Read more on myDr website
Cold sores: children & teens | Raising Children Network
Cold sores are quite common in older children and teenagers. Cold sores usually clear up by themselves, but see your GP if you’re concerned.
Cold sores usually clear up by themselves, but see your GP if you’re concerned.
Read more on raisingchildren.net.au website
Genital Herpes | Family Planning NSW
Genital herpes is a common sexually transmitted infection (STI) caused by the herpes simplex virus (HSV). There are two types of herpes simplex virus.
Read more on Family Planning Australia website
Genital Herpes and Pregnancy
If you are pregnant and you get genital herpes, it is important to tell your midwife or obstetrician.
Read more on Queensland Health website
Genital herpes
Genital herpes is a sexually transmitted infection (STI) which shows as blisters or sores on the genitals. This is caused by the herpes simplex virus (HSV).
This is caused by the herpes simplex virus (HSV).
Read more on WA Health website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.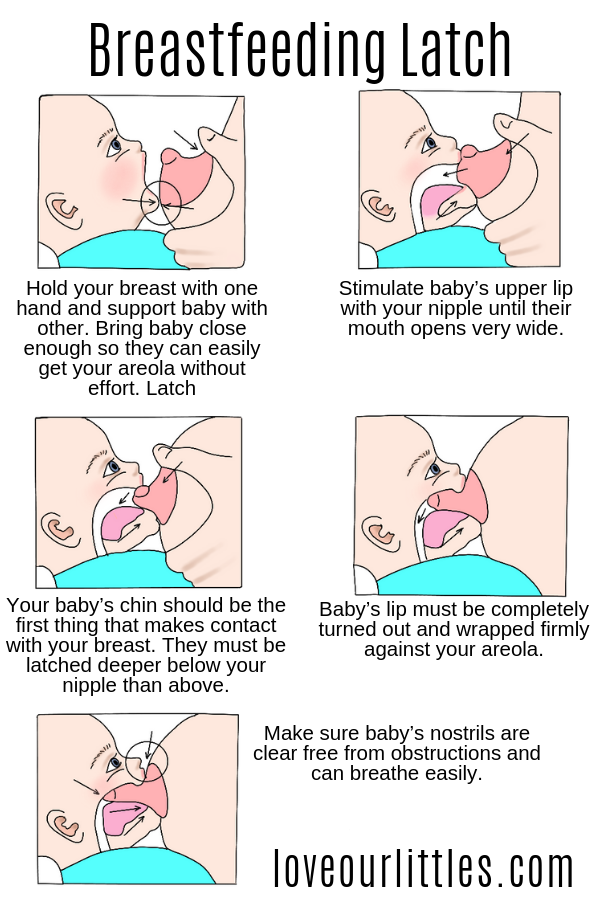
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care.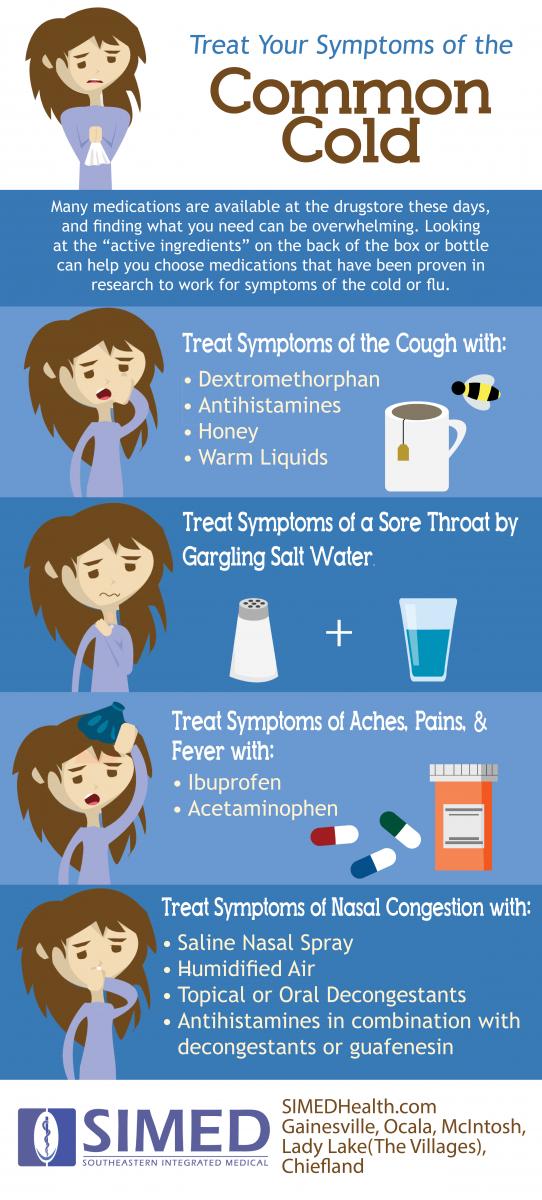 If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Use and safety Acyclovir for pregnant and lactating women: can it be taken during pregnancy and breastfeeding
Can acyclovir be used during pregnancy to treat herpes and possible risks to the fetus
Acyclovir belongs to a class of antiviral drugs called synthetic nucleoside analogues. It works by stopping the spread of the herpes virus in the body. Used to reduce pain and speed up the healing of sores or blisters in people with chickenpox (chickenpox), shingles, a rash that can occur in people who have had chickenpox in the past, and outbreaks of genital herpes (occasionally causes ulcers around genitals and rectum).
It works by stopping the spread of the herpes virus in the body. Used to reduce pain and speed up the healing of sores or blisters in people with chickenpox (chickenpox), shingles, a rash that can occur in people who have had chickenpox in the past, and outbreaks of genital herpes (occasionally causes ulcers around genitals and rectum).
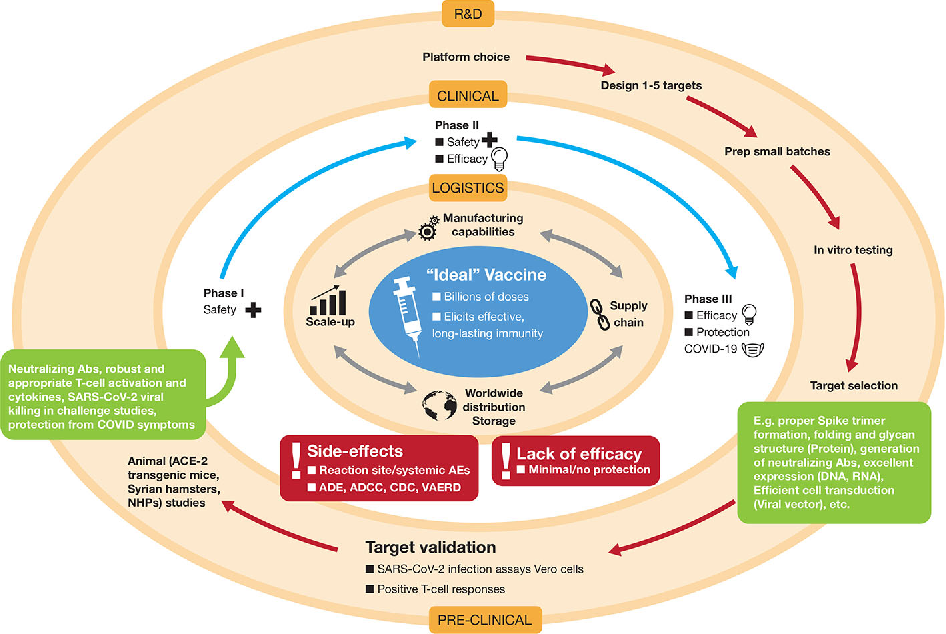
In a study by the Centers for Disease Control and Prevention (CDC), aciclovir was found to cross the placenta, but teratogenicity (birth defects) was not observed, but there are still insufficient data to assess the risk of less common defects or to obtain reliable or final conclusions regarding the safety of this drug during pregnancy.
According to research by the Food and Drug Administration (FDA), it was noted that women taking acyclovir for the treatment of herpes simplex, even during the first trimester of pregnancy, did not demonstrate a risk to the fetus.
The Australian Medicines Administration (AU TGA) has studied a limited number of pregnant women and women of childbearing age who have taken oral acyclovir and found that it did not increase the incidence of malformations or other direct or indirect harmful effects on the mother's fetus. Animal studies have shown an increased incidence of fetal injury, the significance of which in humans is uncertain.
Animal studies have shown an increased incidence of fetal injury, the significance of which in humans is uncertain.
The American College of Obstetricians and Gynecologists (ACOG) recommends taking aciclovir for the treatment of genital herpes, especially recurrent ones, from the 36th week of pregnancy to avoid infection of the newborn baby. But since, as a result of not multiple studies, little information has been provided about it, it is advised to use it with extreme caution, strictly according to the doctor's prescription in the exact minimum dosage indicated as soon as possible.
Information was also provided to ACOG that suppressive therapy in late pregnancy reduces the rate of caesarean section in women with recurrent genital herpes by reducing the rate of recurrence during pregnancy, but such treatment may not protect against transmission of the viral infection to the newborn in all cases .
Centers for Disease Control and Prevention (CDC) in 2015 concluded that this drug can be used to treat herpetic lesions in women at all stages of pregnancy, but under the strict supervision of a doctor, following all his prescriptions for prescribed doses, frequency and duration of administration, as well as in case of the most urgent need and, as a rule, the benefit to the mother should exceed the risk to the fetus.
Breastfeeding use of acyclovir and exposure to infants
Food and Drug Administration (FDA) studies of acyclovir use in breastfeeding women have found that it passes into breast milk, but even at the most At high maternal doses, the concentration of acyclovir in milk is only about 1% of the typical pediatric dose and is not expected to cause any side effects in breastfed infants. Local application of acyclovir to small areas of the mother's body away from the breast does not pose a risk to the infant.
As a result of maternal herpesvirus infection of the infant during pregnancy, newborns are given aciclovir at doses of 20 to 30 mg/kg intravenously daily according to the CDC. Dosages obtained in breast milk at high maternal doses are only about 3-5% of this dose. Because the infant receives oral doses of breast milk and aciclovir is only about 20% orally bioavailable, the systemic dose received by the nursing infant is 1% or less of the typical pediatric dose, resulting in no reported adverse reactions in infants.
Several cases of oral aciclovir in breastfeeding mothers have also been reported to the CDC and FDA:
-
The mother of a 4-month-old infant did not notice any side effects in her breastfed infant when she took aciclovir 800 mg orally 5 times a day;
- 90,004 a woman who was 6 weeks postpartum received acyclovir 300 mg (5 mg/kg) intravenously three times a day for 5 days. Milk samples were taken every 6 hours after the last dose. The peak level was 7.3 mg/L and the drug was detectable in milk up to 88 hours after the last dose. 6 hours after the last dose, the breast-fed child received a daily dose of 1.1 mg / kg of acyclovir through mother's milk, in the case of such therapy in the mother during lactation, there were also no negative effects in the infant.
As a result of these studies, the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA) have concluded that aciclovir for lactating women is considered acceptable but should not be taken. uncontrolled, the dose and duration of treatment with acyclovir should be determined by the doctor, with a mandatory comparison of the benefits for the mother and the possible risks for the newborn.
uncontrolled, the dose and duration of treatment with acyclovir should be determined by the doctor, with a mandatory comparison of the benefits for the mother and the possible risks for the newborn.
Herpes during breastfeeding in a nursing mother: on the lip, chest, genital
The herpes virus is known to almost everyone. Statistics show that only 10% of the world's inhabitants are not among those infected with any of the forms of herpes. If it once appeared in the body, the risk of relapse persists throughout life, but there is a reliable barrier that keeps it - immunity. It depends on the state of the immune system how often you will observe familiar symptoms.
Herpes only appears when the immune system is weakened. The cause may be illness, hypothermia, stressContents
- 1. Varieties of herpes
- 1.1. On the lips
- 1.2. On the genitals
- 1.3. Herpes zoster
- 2.
Do I need to change my feeding regimen?
- 3. Treatment of herpes on the lips
- 4. Drugs for the treatment of other forms of herpes
- 5. Video on the topic of the article
- 6. Questions from readers and answers from an expert
Varieties of herpes
During breastfeeding, as you know, immunity decreases, and if at this time you are even a little overcooled, the disease can immediately make itself felt. It manifests itself in different ways, since the types of the causative agent of the disease also differ.
Herpes during breastfeeding can be:
- on the lips;
- on the genitals;
- zoster.
On the lips
Herpes on the lips - the first type of virus - the most common. It is transmitted in a domestic way, that is, through dishes, towels, etc. A small child from a nursing mother can get it through kisses.
First, redness and swelling appear on or near the lips, as well as on the wings of the nose, which are necessarily accompanied by itching. Then small bubbles begin to appear with a clear liquid inside, which, bursting, contribute to the emergence of new ones - already more numerous.
Then small bubbles begin to appear with a clear liquid inside, which, bursting, contribute to the emergence of new ones - already more numerous.
If herpes first appeared, other cold symptoms may be added - fever, general weakness and malaise. With relapses, such signs usually do not happen.
Herpes on the lips is the most common and familiar to almost everyone: according to statistics, about 90% of the world's population are its carriersTreatment in this case will be local. The main thing is to start it immediately when the slightest redness appears. In this case, it is good to have some kind of external remedy in your first-aid kit, and if it is not available, immediately purchase it. Then you have the right to count on a quick solution to the problem. If the bubbles have already appeared, it will take longer to be treated.
On the genitals
The second type of virus causes genital herpes. To the main reason for the exacerbation (decreased immunity), another one is added - the activation of the virus in the husband.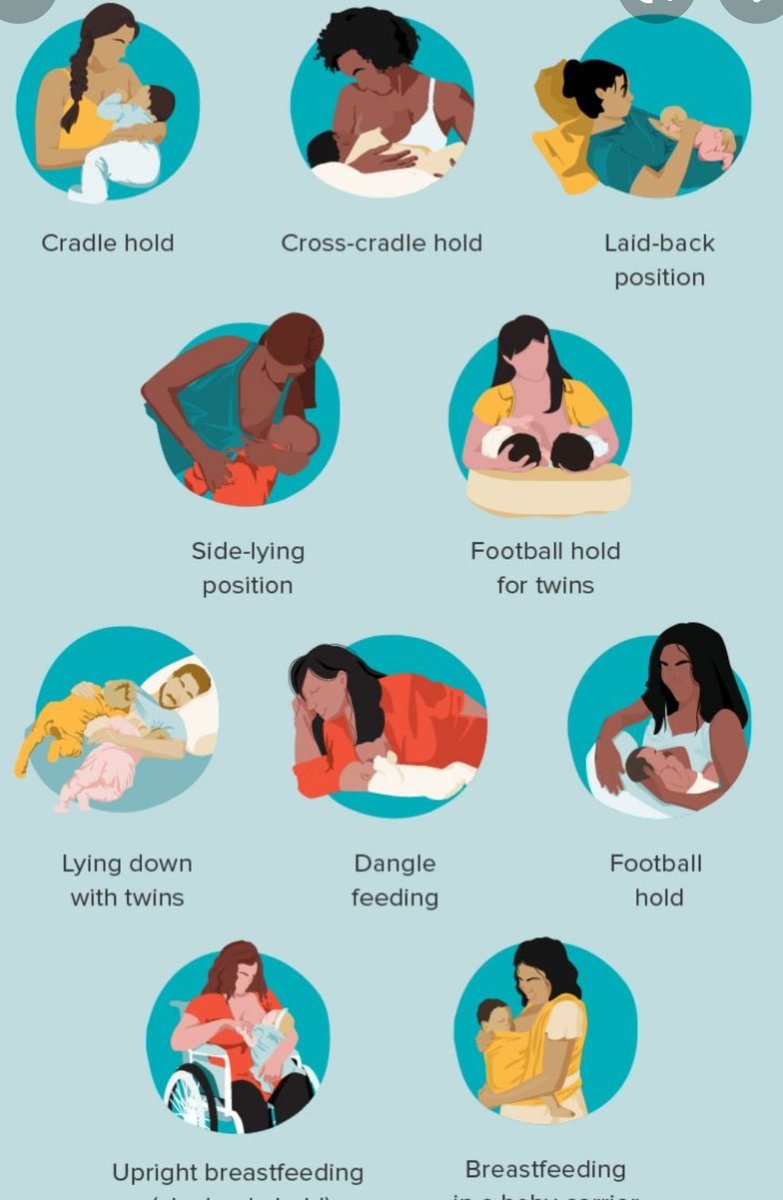 The first symptoms in this case will be similar to the common cold - chills, fever, general weakness. Obstetrician-gynecologist Nana Ordzhonikidze advises to pay close attention to the initial signs of the disease, which can easily be confusing, and only a characteristic rash that appears later will tell about the presence of an infection.
The first symptoms in this case will be similar to the common cold - chills, fever, general weakness. Obstetrician-gynecologist Nana Ordzhonikidze advises to pay close attention to the initial signs of the disease, which can easily be confusing, and only a characteristic rash that appears later will tell about the presence of an infection.
If the diagnosis is confirmed and small watery vesicles appear, they will cover the entire perineum, pubis, inner thighs and mucous membrane of the labia. They will be present even on the mucous membrane of the vagina and cervix, but only a gynecologist can detect them during examination. Another characteristic sign - severe itching - will worsen, and urination will become painful, as the bubbles will begin to burst and urine will fall into microcracks and wounds.
Treatment of genital herpes is more complicated. You will need a mandatory consultation with a gynecologist or dermatovenereologist. It is dangerous to engage in self-medication, since when prescribing it is necessary to take into account an important factor - the period of breastfeeding.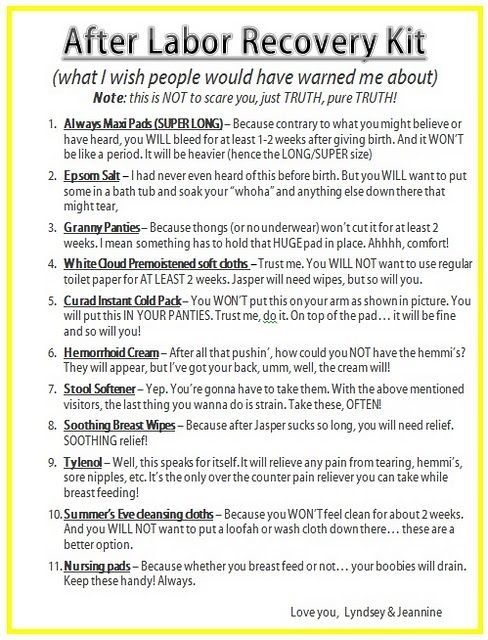 As in the previous case, the sooner treatment is started, the more successful it will be.
As in the previous case, the sooner treatment is started, the more successful it will be.
READ ALSO: How to treat a cold while breastfeeding?
Shingles
The third type of herpes virus causes even more serious diseases - shingles, chicken pox, chicken pox. This virus is localized in the nerve endings, so the exacerbation is accompanied by itching and pain, which are the main symptoms in relapses. When the disease appears, as in the two cases described above, there is an increase in temperature and general malaise. The rash is found in the area of nerve endings and quickly occupies large areas on the skin, accompanied by severe pain.
Therapist prescribes the treatment. Only local remedies like ointments and gels are indispensable here. You will need antiviral pills, which must be selected taking into account the fact that the woman is breastfeeding.
Herpes zoster is accompanied by itching, but this is too common a symptom - only a specialist should make a diagnosisShould I change the feeding regimen?
Many doctors believe that it is better for a woman to stop breastfeeding while she is ill, but the WHO states that there is no reason for this.
There is a document (Complete List of Medical Reasons for Using Breastmilk Substitutes 2009) which states that breastfeeding is not acceptable only if the baby is HIV-infected, and also if the baby suffers from one of the two serious diseases - galactosemia or phenylketonuria. In all other cases, including herpes, it is even necessary to continue lactation.
You just have to follow the rules of hygiene. Additional measures will also be needed:
- HB must be continued, as the activation of the virus contributes to the production of antibodies against the disease.
 Antibodies immediately pass into breast milk and provide the baby with protection by blocking the activity of the virus on the third to fifth day.
Antibodies immediately pass into breast milk and provide the baby with protection by blocking the activity of the virus on the third to fifth day. - Even if rashes appear on the body, breastfeeding should be interrupted only when they have affected the skin of the nipples. In other cases - on the lips, genitals, or even with herpes zoster, the rash is not a reason to suspend or completely stop breastfeeding. If the rash is only on one breast, you can feed the baby on the other.
- At the same time, it is necessary to carefully monitor that the child does not have contact with the affected areas of the skin on the mother's body. Herpes is transmitted by household means, so the baby must be protected in every possible way from infection. If the virus appeared on the lips, of course, there can be no question of any kisses.
- Personal hygiene needs to be monitored more carefully than usual. Regardless of which part of the body is affected by herpes, it is necessary to wash your hands with soap as often as possible: do this before you start feeding or just pick up the baby, and also after washing or eating.

Maintaining cleanliness and good hygiene can cure the virus faster or prevent infection altogether. Cleanliness is the key to health, it is not for nothing that experts have been talking about this for many years.
Treatment of herpes on the lips
Treatment of herpes on the lips is easier than other types of the virus. The first thing to do is not to ignore the problem or procrastinate, but to take action quickly. The virus can be dealt with at the very beginning of the development of the disease, preventing it from reaching an advanced stage. The second important rule is to use local remedies (ointments, creams, gels). The concentration of active substances in them is low and, as a rule, they do not pass into breast milk. Lactation at this time should not be interrupted.
Local remedies for herpes help, but they must be used systematically and according to the instructionsPreparations for the treatment of other forms of herpes
Genital and herpes zoster are more severe, and therefore more difficult to treat. It is necessary to act on them in a complex way, that is, to use external agents and antiviral tablets.
It is necessary to act on them in a complex way, that is, to use external agents and antiviral tablets.
Despite the fact that there are enough drugs for oral administration, manufacturers in the instructions for use limit their use during lactation or recommend interrupting breastfeeding while the mother is being treated. It is useful to study the list of funds, but we advise you not to prescribe the funds yourself, but be sure to visit a doctor. Only a competent specialist will do this with minimal damage to the health of the child.
READ ALSO: treatment of the common cold during breastfeeding
Consider the most well-known and effective drugs:
- Acyclovir (Acyclovir, Zovirax) is considered a highly effective remedy for the treatment of herpes of the first and third types. Available in the form of tablets, powder, cream and ointment.
- Valaciclovir (Valvir, Valtrex) is a next-generation tablet after acyclovir. They are used to treat all types of herpes.

- Penciclovir (Fenistil Pencivir) - topical (cream). Despite external use, it is recommended to use it during lactation very carefully, only if the expected benefit outweighs the potential harm to the child. Although the latest data from the E-LACTANCIA guideline states that when applied topically, the drug is not detected in blood plasma and therefore does not penetrate into breast milk, when applied to the body, care must be taken that the child does not have contact with the treated areas of the skin, and before feeding the breast should be washed thoroughly with soap.
If the immune system is weak, the doctor may prescribe additional drugs to increase immunity. These are preparations with interferon ("Viferon", "Kipferon"), produced in the form of candles.
Folk remedies for the treatment of herpes are used only as an auxiliary during remission.