How long does it take for vaccines to be effective
Vaccines - Better Health Channel
COVID-19 vaccines: For information about COVID-19 vaccines please go to the Victorian Government's coronavirus (COVID-19) websiteExternal Link.
About vaccines
Vaccines are clever, they train our bodies into building immunity against infectious diseases, without causing the illness.
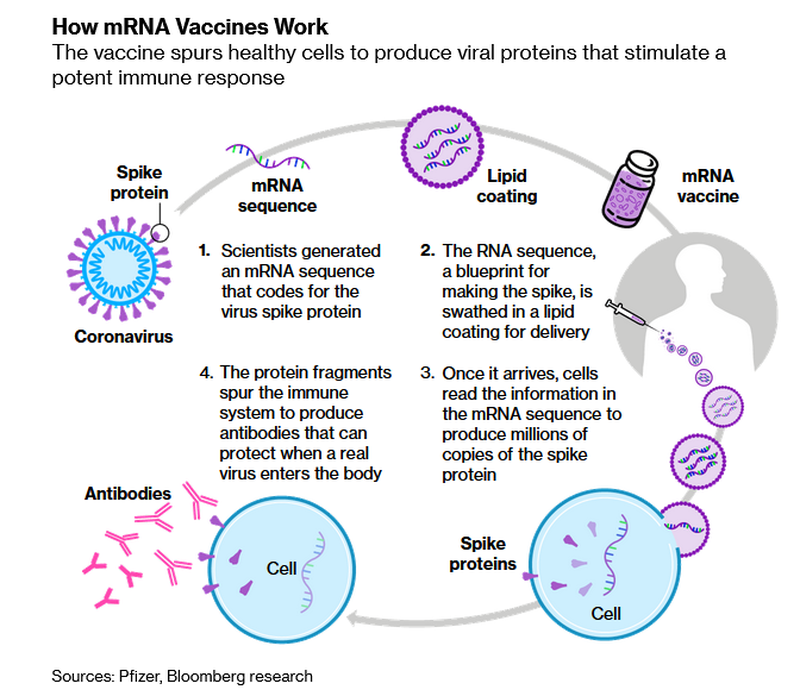
Usually, a dead or weakened version of the disease-causing germ (bacteria or virus) is introduced to our immune system. In some cases, inactivated toxins produced by the germ are used in the vaccine to develop immunity (for example, diphtheria and tetanus vaccines). We call these antigens, and they are the most important ingredient of all vaccines. Alternatively, mRNA vaccines instruct our cells to stimulate an immune response.
Once we’ve been vaccinated, if our immune system encounters the ‘real’ disease-causing germ, it responds quickly and creates antibodies and memory cells to give the body protection.
Immunisation (vaccination) is the most effective preventative measure against serious diseases. Some vaccines offer lifelong immunity. In other cases, ‘catch-ups’ or booster shots are needed.
When were vaccines developed?
Vaccines are not new – immunisation techniques were pioneered over 200 years ago, when smallpox was a feared and deadly disease. An eighteenth-century doctor named Edward Jenner noted that workers on farms who contracted the mild cowpox disease were immune to smallpox.
Jenner guessed that the germ responsible for cowpox was similar enough to the smallpox germ to ‘train’ the immune system to defeat both diseases. He was correct. Immunisation in Australia today relies on similar principles.
How do vaccines work?
Our immune system is made up of special cells and chemicals (called antibodies) that fight infection. We gain immunity against diseases either naturally (by catching an illness), or through immunisation.
Vaccines are made up of a modified version of a disease-causing germ or toxin (known as ‘antigens’). Alternatively mRNA vaccines instruct our cells to stimulate an immune response.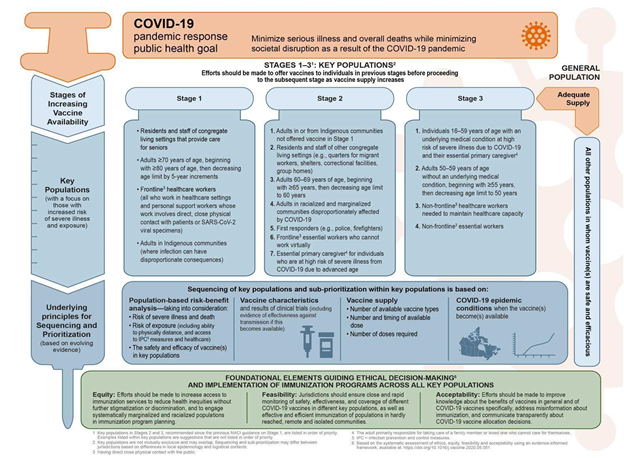 Vaccines are usually given by injection or a small drink that contains the vaccine.
Vaccines are usually given by injection or a small drink that contains the vaccine.
The immune system responds to the weakened, partial or dead germ or inactivated toxin (antigen) as if it was a fully-fledged germ, and makes antibodies to destroy it. These antibodies are made without us catching the illness.
How do vaccines help our immunity?
Our immune system is like a library – it stores information about every germ ever defeated. We sometimes call this immunological memory.
Some antibodies remain ‘on patrol’ in our bloodstream. So if we ever encounter the real germ in the future, our immune system can quickly trigger the memory cells and produce antibodies to defeat it. And this often occurs before we experience any symptoms of illness.
Each vaccine is designed according to how the specific germs make us sick. For example, measles is the result of the body’s reaction to the whole virus and so the vaccine contains a weakened form of the virus. On the other hand, tetanus is caused by the body’s reaction to the toxin produced by the tetanus bacteria and so the vaccine contains inactivated tetanus toxin.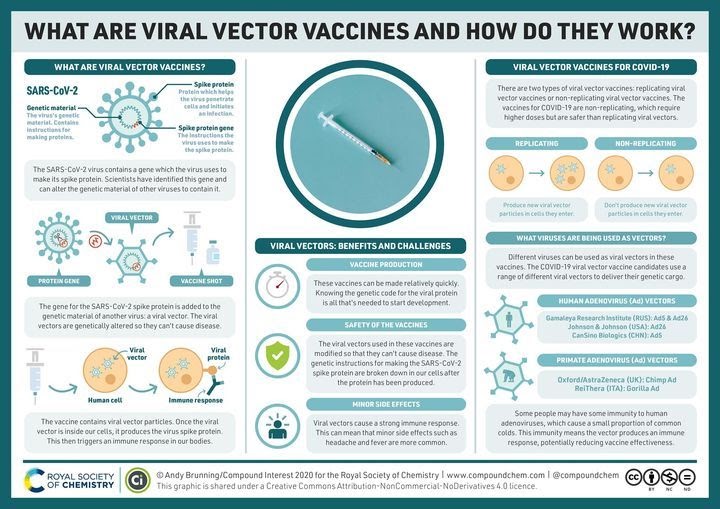
What is in vaccines?
Depending on the infection, ingredients in vaccines can vary. They may also change from year to year as new strains of viruses (such as the flu) appear. Some vaccines may contain a small dose of:
- a live (but weakened) germ
- dead germs
- small parts of germs (for example, a molecule from the surface of a germ)
- inactivated toxins produced by bacteria
- antibiotics or preservatives to stop the vaccine from becoming contaminated or going off
- diluents (such as sterile water or saline).
Alternatively mRNA vaccines teach our cells how to make a protein that stimulates an immune response.
Australia has strict rules on vaccine safety. Before a vaccine is registered by the Therapeutic Goods Administration (TGA)External Link and made available to the public it goes through rigorous testing. And, even when it is used, it is constantly monitored for safety and effectiveness.
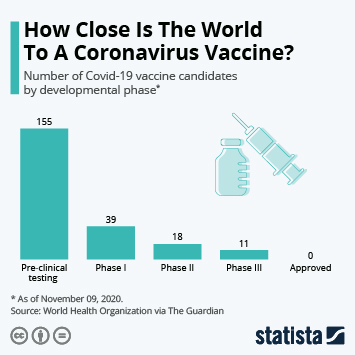
How are new vaccines developed?
It can take a long time to develop a new vaccine.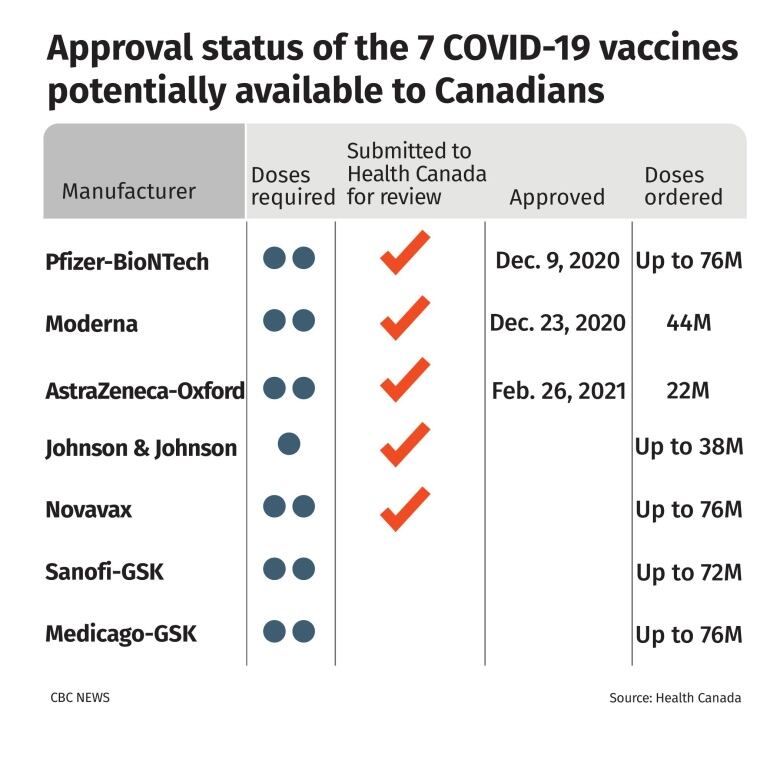 Vaccines go through many phases of development – including research, discovery, pre-clinical testing, clinical testing and regulatory approval. Once the vaccine is approved, the vaccine is then manufactured and shipped to where it’s needed.
Vaccines go through many phases of development – including research, discovery, pre-clinical testing, clinical testing and regulatory approval. Once the vaccine is approved, the vaccine is then manufactured and shipped to where it’s needed.
In certain circumstances, increased resources, concurrent clinical trials, and funding can fast-track development, such as in the case of the COVID-19 vaccinesExternal Link.
After vaccines are introduced into immunisation schedules, they are closely monitored through trials and surveillance to see if they are effective and safe. In Australia, there are regional and national surveillance systems actively looking for any adverse events following immunisation. This is necessary, as sometimes unexpected side effects occur after vaccines are registered for use.
Some vaccines, such as the flu, need to be updated every year to respond to changing infection strains and conditions. For these updates, the process is compressed to ensure the vaccine is available as needed.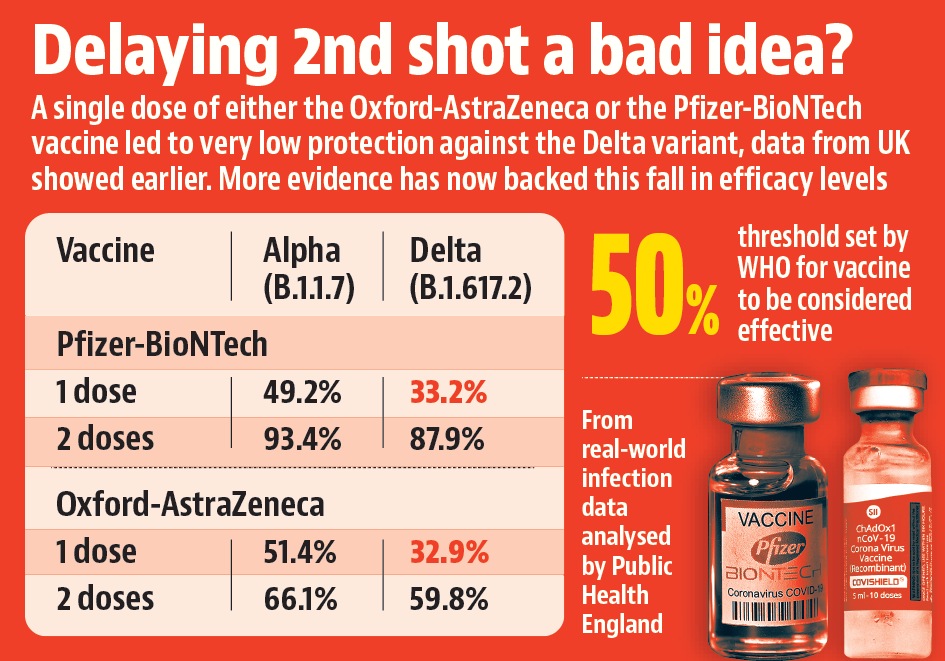
Are vaccines safe?
Millions of people – many of them babies and young children – are immunised every year, with no side effects. Vaccines are much safer than getting sick from a disease. Diseases that can be prevented by vaccines can cause lifelong complications or death – even in normally healthy people.
From time to time, the safety of vaccines has been questioned. Most reactions are mild and usually last one to 2 days. Like any other medication, vaccines carry a small degree of risk, but serious side effects are rare.
The risk of serious side effects must be weighed against the risk of the disease. For example, there is a small risk of developing the rare condition known as idiopathic thrombocytopenic purpura (ITP) after the measles, mumps, rubella and varicella (MMRV) vaccine and the measles, mumps and rubella (MMR) vaccine. However, the risk of developing ITP with measles itself is more than 10 times greater than the risk associated with the vaccine.
How successful are vaccines?
Vaccination is the most effective preventative measure against infectious diseases. Most vaccine-preventable illnesses are highly contagious, spread quickly and can cause severe complications which may impact on our quality of life.
Most vaccine-preventable illnesses are highly contagious, spread quickly and can cause severe complications which may impact on our quality of life.
Vaccines give us immunity without us getting sick. They also protect vulnerable people in our community who cannot be immunised – such as very young children or those who are too sick.
When enough people in the community are vaccinated, the spread of a disease slows down or stops completely. So as long as enough people are vaccinated, diseases will not spread. We call this herd immunity or community immunity. The percentage of people who need to be immune in order to achieve herd immunity varies with each disease. For example:
- Measles, mumps, rubella – 95 out of every 100 people vaccinated will be completely immune.
- Whooping cough – about 85 out of every 100 people vaccinated will be completely immune.
How long does it take for a vaccine to work?
When we receive a vaccine, our immune system gets to work immediately to create antibodies and memory cells to fight the infection.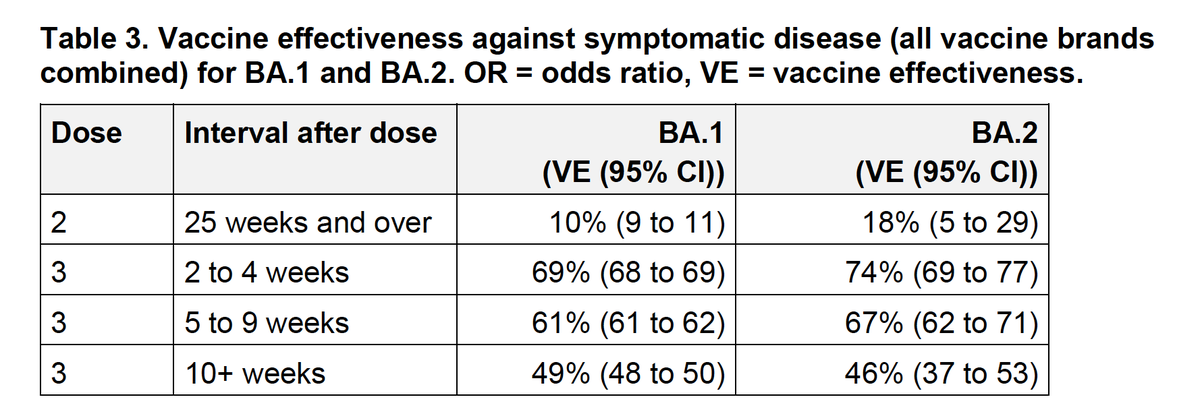 On average, an immune response will take around 7 to 21 days.
On average, an immune response will take around 7 to 21 days.
However, the duration of immunity can depend on a number of factors, such as the nature of vaccine, the timing of dosages, our age, and whether we have had an infection naturally.
To be protected from vaccine-preventable diseases, make sure to stick to the recommended schedulesExternal Link and keep your immunisations up to date.
Which vaccines do we need?
Vaccines not only protect us, but vulnerable people in our community (such as the young, the elderly, or those with weakened immunity).
The vaccines we may need are determined by our health, age, lifestyle and occupation. Together, these factors are known as HALO.
HALO is defined as:
- Health – some people may benefit from additional or more frequent immunisations due to health factors. For example, pregnant women, premature babies, or those with conditions (such as asthma, diabetes, HIV and disorders of the heart, lungs, spleen or kidneys).
- Age – at certain ages, we are more vulnerable to some illnesses. Such as in: childhood, in secondary school and when we are older.
- Lifestyle – some lifestyle choices can put us or the community at risk, such as overseas travel, moving to Australia, becoming a new parent, sexual activity, smoking, or playing contact sport.
- Occupation – some jobs have a higher risk of exposure to infections. Such as those who work in hospitals, childcare and emergency services.
Check your immunisation HALO using the Immunisation for Life infographic.
Remember, if you are not sure about what vaccines you need, talk to your GP (doctor). If you find you are not up to date with your vaccinations, your GP will tell you about catch-ups and boosters.
Australia’s National Immunisation Program Schedule
The National Immunisation Program (NIP) ScheduleExternal Link sets out recommended immunisations for infants, children, older people and other people at risk, such as Aboriginal and Torres Strait Islander people. Most recommended vaccines are available at no cost to these groups.
Most recommended vaccines are available at no cost to these groups.
If you need further information, talk to your GP (doctor) or immunisation provider.
Where to get help
- In an emergency, always call triple zero (000)
- Your GP (doctor)
- Your local council immunisation service – visit Know Your CouncilExternal Link
- Maternal and Child Health Line Tel. 13 22 29 (24 hours, 7 days)
- NURSE-ON-CALL Tel. 1300 60 60 24 – for expert health information and advice (24 hours, 7 days)
- Immunisation Unit, Department of HealthExternal Link, Victorian Government Email: [email protected]
- National Immunisation Information LineExternal Link Tel. 1800 671 811
- Australian Immunisation RegisterExternal Link Tel. 1800 653 809
- Pharmacist
- SAEFVICExternal Link Tel. 1300 882 924 (select option 1)
- Coronavirus (COVID-19) VictoriaExternal Link Tel. 1800 675 398
Vaccines - Better Health Channel
COVID-19 vaccines: For information about COVID-19 vaccines please go to the Victorian Government's coronavirus (COVID-19) websiteExternal Link.
About vaccines
Vaccines are clever, they train our bodies into building immunity against infectious diseases, without causing the illness.
Usually, a dead or weakened version of the disease-causing germ (bacteria or virus) is introduced to our immune system. In some cases, inactivated toxins produced by the germ are used in the vaccine to develop immunity (for example, diphtheria and tetanus vaccines). We call these antigens, and they are the most important ingredient of all vaccines. Alternatively, mRNA vaccines instruct our cells to stimulate an immune response.
Once we’ve been vaccinated, if our immune system encounters the ‘real’ disease-causing germ, it responds quickly and creates antibodies and memory cells to give the body protection.
Immunisation (vaccination) is the most effective preventative measure against serious diseases. Some vaccines offer lifelong immunity. In other cases, ‘catch-ups’ or booster shots are needed.
When were vaccines developed?
Vaccines are not new – immunisation techniques were pioneered over 200 years ago, when smallpox was a feared and deadly disease. An eighteenth-century doctor named Edward Jenner noted that workers on farms who contracted the mild cowpox disease were immune to smallpox.
An eighteenth-century doctor named Edward Jenner noted that workers on farms who contracted the mild cowpox disease were immune to smallpox.
Jenner guessed that the germ responsible for cowpox was similar enough to the smallpox germ to ‘train’ the immune system to defeat both diseases. He was correct. Immunisation in Australia today relies on similar principles.
How do vaccines work?
Our immune system is made up of special cells and chemicals (called antibodies) that fight infection. We gain immunity against diseases either naturally (by catching an illness), or through immunisation.
Vaccines are made up of a modified version of a disease-causing germ or toxin (known as ‘antigens’). Alternatively mRNA vaccines instruct our cells to stimulate an immune response. Vaccines are usually given by injection or a small drink that contains the vaccine.
The immune system responds to the weakened, partial or dead germ or inactivated toxin (antigen) as if it was a fully-fledged germ, and makes antibodies to destroy it.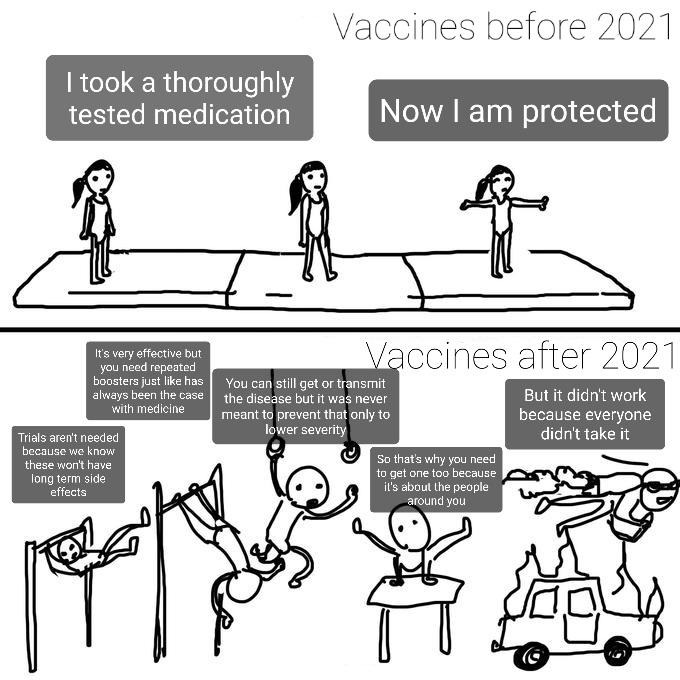 These antibodies are made without us catching the illness.
These antibodies are made without us catching the illness.
How do vaccines help our immunity?
Our immune system is like a library – it stores information about every germ ever defeated. We sometimes call this immunological memory.
Some antibodies remain ‘on patrol’ in our bloodstream. So if we ever encounter the real germ in the future, our immune system can quickly trigger the memory cells and produce antibodies to defeat it. And this often occurs before we experience any symptoms of illness.
Each vaccine is designed according to how the specific germs make us sick. For example, measles is the result of the body’s reaction to the whole virus and so the vaccine contains a weakened form of the virus. On the other hand, tetanus is caused by the body’s reaction to the toxin produced by the tetanus bacteria and so the vaccine contains inactivated tetanus toxin.
What is in vaccines?
Depending on the infection, ingredients in vaccines can vary. They may also change from year to year as new strains of viruses (such as the flu) appear. Some vaccines may contain a small dose of:
Some vaccines may contain a small dose of:
- a live (but weakened) germ
- dead germs
- small parts of germs (for example, a molecule from the surface of a germ)
- inactivated toxins produced by bacteria
- antibiotics or preservatives to stop the vaccine from becoming contaminated or going off
- diluents (such as sterile water or saline).
Alternatively mRNA vaccines teach our cells how to make a protein that stimulates an immune response.
Australia has strict rules on vaccine safety. Before a vaccine is registered by the Therapeutic Goods Administration (TGA)External Link and made available to the public it goes through rigorous testing. And, even when it is used, it is constantly monitored for safety and effectiveness.
How are new vaccines developed?
It can take a long time to develop a new vaccine. Vaccines go through many phases of development – including research, discovery, pre-clinical testing, clinical testing and regulatory approval. Once the vaccine is approved, the vaccine is then manufactured and shipped to where it’s needed.
Once the vaccine is approved, the vaccine is then manufactured and shipped to where it’s needed.
In certain circumstances, increased resources, concurrent clinical trials, and funding can fast-track development, such as in the case of the COVID-19 vaccinesExternal Link.
After vaccines are introduced into immunisation schedules, they are closely monitored through trials and surveillance to see if they are effective and safe. In Australia, there are regional and national surveillance systems actively looking for any adverse events following immunisation. This is necessary, as sometimes unexpected side effects occur after vaccines are registered for use.
Some vaccines, such as the flu, need to be updated every year to respond to changing infection strains and conditions. For these updates, the process is compressed to ensure the vaccine is available as needed.
Are vaccines safe?
Millions of people – many of them babies and young children – are immunised every year, with no side effects.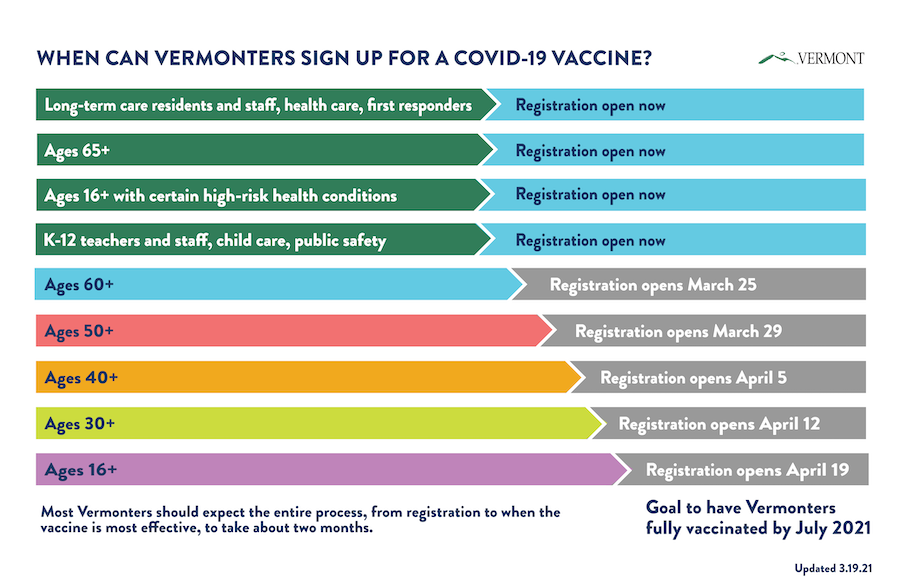 Vaccines are much safer than getting sick from a disease. Diseases that can be prevented by vaccines can cause lifelong complications or death – even in normally healthy people.
Vaccines are much safer than getting sick from a disease. Diseases that can be prevented by vaccines can cause lifelong complications or death – even in normally healthy people.
From time to time, the safety of vaccines has been questioned. Most reactions are mild and usually last one to 2 days. Like any other medication, vaccines carry a small degree of risk, but serious side effects are rare.
The risk of serious side effects must be weighed against the risk of the disease. For example, there is a small risk of developing the rare condition known as idiopathic thrombocytopenic purpura (ITP) after the measles, mumps, rubella and varicella (MMRV) vaccine and the measles, mumps and rubella (MMR) vaccine. However, the risk of developing ITP with measles itself is more than 10 times greater than the risk associated with the vaccine.
How successful are vaccines?
Vaccination is the most effective preventative measure against infectious diseases. Most vaccine-preventable illnesses are highly contagious, spread quickly and can cause severe complications which may impact on our quality of life.
Vaccines give us immunity without us getting sick. They also protect vulnerable people in our community who cannot be immunised – such as very young children or those who are too sick.
When enough people in the community are vaccinated, the spread of a disease slows down or stops completely. So as long as enough people are vaccinated, diseases will not spread. We call this herd immunity or community immunity. The percentage of people who need to be immune in order to achieve herd immunity varies with each disease. For example:
- Measles, mumps, rubella – 95 out of every 100 people vaccinated will be completely immune.
- Whooping cough – about 85 out of every 100 people vaccinated will be completely immune.
How long does it take for a vaccine to work?
When we receive a vaccine, our immune system gets to work immediately to create antibodies and memory cells to fight the infection. On average, an immune response will take around 7 to 21 days.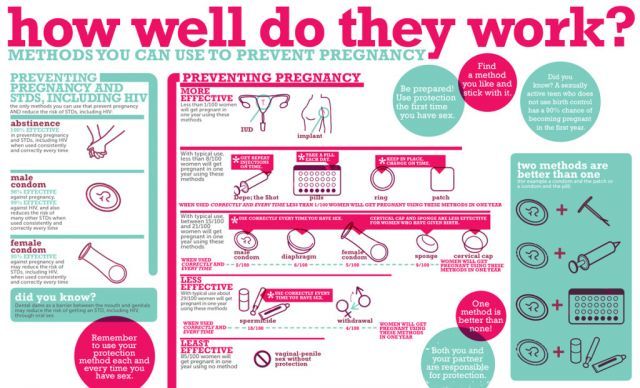
However, the duration of immunity can depend on a number of factors, such as the nature of vaccine, the timing of dosages, our age, and whether we have had an infection naturally.
To be protected from vaccine-preventable diseases, make sure to stick to the recommended schedulesExternal Link and keep your immunisations up to date.
Which vaccines do we need?
Vaccines not only protect us, but vulnerable people in our community (such as the young, the elderly, or those with weakened immunity).
The vaccines we may need are determined by our health, age, lifestyle and occupation. Together, these factors are known as HALO.
HALO is defined as:
- Health – some people may benefit from additional or more frequent immunisations due to health factors. For example, pregnant women, premature babies, or those with conditions (such as asthma, diabetes, HIV and disorders of the heart, lungs, spleen or kidneys).
- Age – at certain ages, we are more vulnerable to some illnesses.
 Such as in: childhood, in secondary school and when we are older.
Such as in: childhood, in secondary school and when we are older. - Lifestyle – some lifestyle choices can put us or the community at risk, such as overseas travel, moving to Australia, becoming a new parent, sexual activity, smoking, or playing contact sport.
- Occupation – some jobs have a higher risk of exposure to infections. Such as those who work in hospitals, childcare and emergency services.
Check your immunisation HALO using the Immunisation for Life infographic.
Remember, if you are not sure about what vaccines you need, talk to your GP (doctor). If you find you are not up to date with your vaccinations, your GP will tell you about catch-ups and boosters.
Australia’s National Immunisation Program Schedule
The National Immunisation Program (NIP) ScheduleExternal Link sets out recommended immunisations for infants, children, older people and other people at risk, such as Aboriginal and Torres Strait Islander people.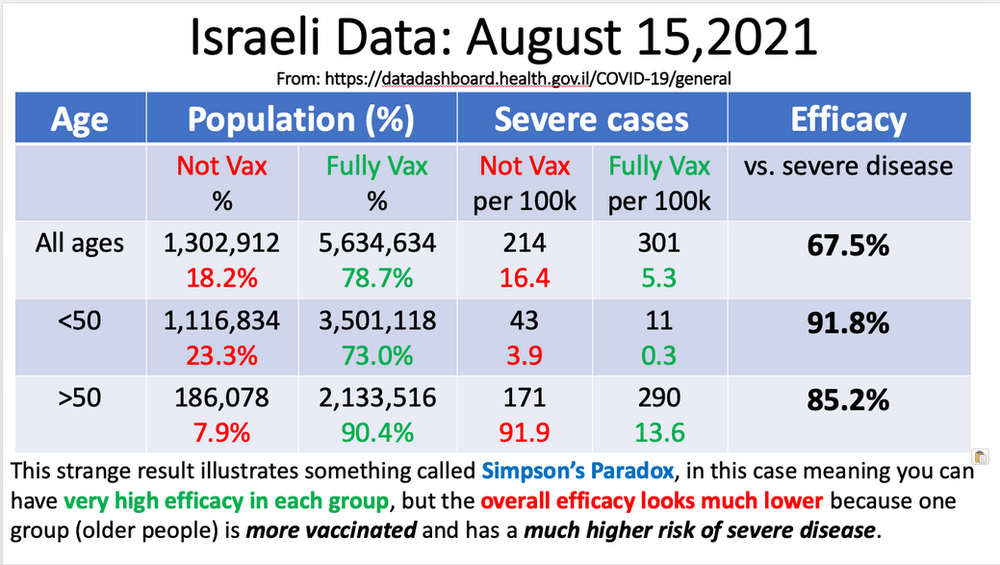 Most recommended vaccines are available at no cost to these groups.
Most recommended vaccines are available at no cost to these groups.
If you need further information, talk to your GP (doctor) or immunisation provider.
Where to get help
- In an emergency, always call triple zero (000)
- Your GP (doctor)
- Your local council immunisation service – visit Know Your CouncilExternal Link
- Maternal and Child Health Line Tel. 13 22 29 (24 hours, 7 days)
- NURSE-ON-CALL Tel. 1300 60 60 24 – for expert health information and advice (24 hours, 7 days)
- Immunisation Unit, Department of HealthExternal Link, Victorian Government Email: [email protected]
- National Immunisation Information LineExternal Link Tel. 1800 671 811
- Australian Immunisation RegisterExternal Link Tel. 1800 653 809
- Pharmacist
- SAEFVICExternal Link Tel. 1300 882 924 (select option 1)
- Coronavirus (COVID-19) VictoriaExternal Link Tel. 1800 675 398
How long does the COVID-19 vaccine last? Is it possible to live like before after vaccination? Will it protect against new strains? Here's what we know about vaccine immunity right now
Spencer Platt / Getty Images
There are already at least five vaccines against SARS-CoV-2 in the world, the effectiveness of which has been shown quite reliably in large-scale studies. But the most important question remains: how long will vaccine immunity last, will it not be necessary to vaccinate again every year? The experience of other diseases suggests that in the general case it is impossible to predict the duration of immunity (for example, by the level of antibodies) - the situation develops differently for different diseases and different components of the immune system are important. Despite this, it is already becoming clear that in the case of covid with immunity itself, most likely, everything will be in order: the main problem is not "falling antibodies", but new strains of the virus that have already learned how to deceive the body's defense system.
But the most important question remains: how long will vaccine immunity last, will it not be necessary to vaccinate again every year? The experience of other diseases suggests that in the general case it is impossible to predict the duration of immunity (for example, by the level of antibodies) - the situation develops differently for different diseases and different components of the immune system are important. Despite this, it is already becoming clear that in the case of covid with immunity itself, most likely, everything will be in order: the main problem is not "falling antibodies", but new strains of the virus that have already learned how to deceive the body's defense system.
When does the vaccine start to work?
All coronavirus vaccines for which there is data today begin to work approximately two to three weeks after the first injection. This is clearly seen simply from the incidence graphs among vaccinated and unvaccinated groups in clinical studies: for about two weeks, the sick accumulate in both groups at the same rate, and then an inflection occurs in the vaccinated group and people begin to get sick much less often.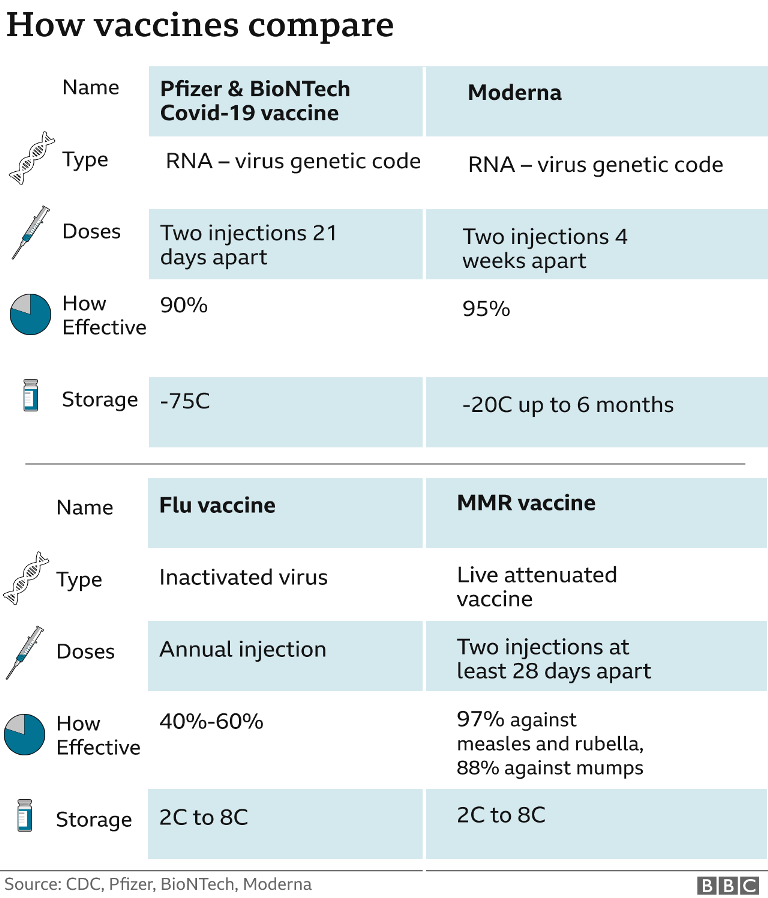 This period (two to three weeks) corresponds to the average time during which antibodies have time to develop in a significant amount during vaccination, which indirectly confirms the importance of antibodies in protecting against the disease.
This period (two to three weeks) corresponds to the average time during which antibodies have time to develop in a significant amount during vaccination, which indirectly confirms the importance of antibodies in protecting against the disease.
These schedules are available for Moderna, Pfizer/BioNTech, J&J, and Sputnik V vaccines. They look very similar to each other, with the possible exception of a slight difference in which day this inflection falls on. Differences between vaccines may have some interesting immunological explanation (for example, related to the difference between vaccine carriers - mRNA or adenovirus), but in practical terms, they are insignificant: it cannot be said that on the 18th day all vaccinated people experience what - some qualitative changes in immunity, a kind of "turning on the protection toggle switch." It’s just that, on average, it is at this moment that the likelihood of getting sick decreases.
Although this is not visible in the pictures, it is important to keep in mind that they are all based on these people who received both the first and second injections. We do not see any traces of enhanced protection after the second injection (second bend), but this does not mean that the second injection is not needed. Firstly, it is not clear what the graph would look like without it - although theoretically for Sputnik V it should reproduce the corresponding graph (.pdf, p. 60) for the J&J vaccine, because it is very similar to the first component of Sputnik V. Secondly, the maturation of antibodies and a change in the immune response after the second (booster) vaccination may have delayed consequences not now, but in a year or two - after all, it is known that in some other diseases, without booster vaccination, immune memory can be unstable.
We do not see any traces of enhanced protection after the second injection (second bend), but this does not mean that the second injection is not needed. Firstly, it is not clear what the graph would look like without it - although theoretically for Sputnik V it should reproduce the corresponding graph (.pdf, p. 60) for the J&J vaccine, because it is very similar to the first component of Sputnik V. Secondly, the maturation of antibodies and a change in the immune response after the second (booster) vaccination may have delayed consequences not now, but in a year or two - after all, it is known that in some other diseases, without booster vaccination, immune memory can be unstable.
Is it possible to get infected between the first and second injections? And get sick after the second?
Both are possible. None of today's vaccines is 100% effective, which means that you can get sick even after vaccination, only with a lower probability. For a vaccine with 90% effectiveness, this probability is ten times less than the probability of getting sick without vaccination, for a vaccine with 95% effectiveness, it is 20 times less, and so on.
As for the period between injections, for the vast majority of vaccines it is so short (21 or 28 days) that it is easier to assume that there is no immunity at all until the second injection. This will be some simplification of reality (the second vaccination almost, but not quite, coincides with the beginning of the inflection in the graphs above), but in a practical sense it is quite reasonable.
Is it true that even after vaccination, safety measures must be observed? Masks are terribly tired!
Restrictions when they make no practical sense are really unpleasant. Note, however, that what we know about vaccine effectiveness today only refers to the reduction in chance of disease, not the chance of infection - which are two different things.
Even after vaccination, it is still possible to become an asymptomatic carrier of the infection, not notice it and infect someone else. It is really known about some vaccines (for example, polio, measles, rubella) that they create not only protective, but also sterilizing immunity - in this case, when it enters the human body, the virus does not multiply and cannot be transmitted from this person to others.
But this scenario is the exception rather than the rule in the vaccine world. Whether anti-covid vaccines fall into the list of such happy exceptions that create sterilizing immunity, we do not know now. Research on this issue is being actively pursued. Apparently, quite soon, scientists will accurately measure how much the probability of infection for a vaccinated person decreases compared to those who have not been vaccinated, and it is quite possible that this decrease will be very strong - but we still have to live until this moment.
In the meantime, when making decisions, one should be guided not by the fact of vaccination itself, but by the number of potentially dangerous contacts and possible consequences: even if you have been vaccinated for a long time, you should not visit your grandmother if you recently attended a concert.
I have been vaccinated and my antibody level is high. So everything is ok?
We have already written that it is not necessary to do an antibody test after vaccination.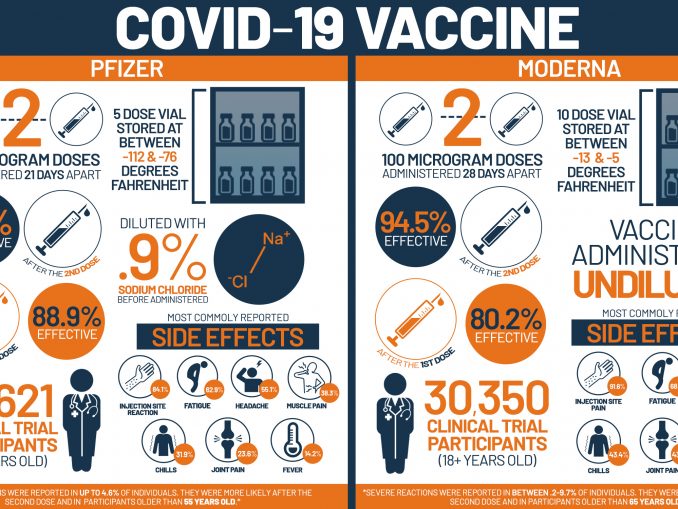 We can only repeat: if you were vaccinated, then the vaccine most likely worked and no test will add anything to this fact. The clause “most likely” here reflects the personal characteristics of the immune system, which you probably know about yourself (immunodeficiency, immunosuppressive therapy, etc.).
We can only repeat: if you were vaccinated, then the vaccine most likely worked and no test will add anything to this fact. The clause “most likely” here reflects the personal characteristics of the immune system, which you probably know about yourself (immunodeficiency, immunosuppressive therapy, etc.).
Given the fact that some of those who are vaccinated do get sick, of course, it would be great to have some kind of test that will immediately tell if you can be among the sick or are completely protected. But to do this, scientists first need to establish exactly what exactly distinguishes the diseased vaccinated from the unaffected: whether it is a low level of antibodies or, perhaps, their poor “quality”. Or even some special history of previous infections.
One way or another, so far, scientists have not found such “correlates of protection”, that is, features that indicate the likelihood of a disease, for coronavirus vaccines. The search for these correlates is actively underway - but so far we have to admit that even for old, well-known diseases, knowledge about such correlates is very superficial and far from complete.
If antibodies don't guarantee protection, what does?
The level of antibodies is, of course, related to the level of protection. But this connection, like everything in immunology, is not as simple as it seems. There is a whole separate area of \u200b\u200bthis science - the study of correlates of protection - within which scientists are trying to establish what exactly in the immune system allows us to predict that a person will not get sick when faced with this or that pathogen. And in what cases the disease still develops, even if the person had the experience of encountering the pathogen. Stanley Plotkin, the author of one of the classic textbooks on vaccinology, calls this area "one of the most controversial in infectious medicine", while it is his reviews of protection correlates that are the most cited, and they can be recommended for introduction to the topic of correlates.
Yes, one of the main correlates of protection is antibodies, they play an important role in most known infections. Sometimes a high level of antibodies in itself (for example, obtained during a blood serum transfusion) is enough and nothing additional is required. In this case, the threshold of the amount of antibodies is usually known, after which the disease does not occur.
Sometimes a high level of antibodies in itself (for example, obtained during a blood serum transfusion) is enough and nothing additional is required. In this case, the threshold of the amount of antibodies is usually known, after which the disease does not occur.
Thus, for hepatitis A, it is known that at a blood plasma antibody level of 10 international units per milliliter (10 mIU/mL), the disease is almost excluded. And this is a fairly low level - after vaccination against this disease, the level of antibodies is usually hundreds of times higher than this threshold level. The protective level of antibodies was also established, for example, when testing (not very successfully) a vaccine against Lyme disease: then scientists determined that everyone who was vaccinated, but still got sick, had an antibody level significantly below the average of 1100 units, then there is in their case, the vaccine did not work. There was no other significant difference between the sick and the non-ill, which is why it was concluded that the matter was exclusively in antibodies.
But the more scientists investigate the correlates of protection, the more complex the picture becomes. Often, the total level of antibodies alone is not enough to predict the presence or absence of protection. For example, for influenza, it has long been believed that with a total antibody titer of 1:40 and above, the disease usually does not occur. However, antibodies against the virus can be of different types, they can be present in the blood or in the mucous membranes, and it is not always possible to guess which of them is “more important”.
Just in the case of influenza, this difference between antibody types has been shown to have a significant impact on the incidence. So, in a study on children who were given a live influenza vaccine, in those who had absolutely no specific antibodies before vaccination, the attenuated vaccine virus multiplied in the upper respiratory tract in 63% of cases (children did not get sick, it was just about virus multiplication) . Among those who had only IgG immunoglobulins in their blood at the time of vaccination, the virus multiplied in 15%, and those who were positive for IgA antibodies in mucosal secretions, this proportion was 19%. However, if both types of antibodies were present in a child, even not in very large quantities, they gave a synergistic effect: only 3% of such children did not have sterilizing immunity, that is, it allowed the virus to multiply. If a similar picture is observed in the case of a new disease, then a general analysis for antibodies will not be very informative - after all, it is the breakdown by antibody classes, supplemented by the way these data are interpreted, that will be important to determine the correlate of protection.
However, if both types of antibodies were present in a child, even not in very large quantities, they gave a synergistic effect: only 3% of such children did not have sterilizing immunity, that is, it allowed the virus to multiply. If a similar picture is observed in the case of a new disease, then a general analysis for antibodies will not be very informative - after all, it is the breakdown by antibody classes, supplemented by the way these data are interpreted, that will be important to determine the correlate of protection.
And this is just a single example of important differences that tests do not capture, within the only potential correlate of immune protection - the total level of antibodies. But in addition to them, the state of memory B-cells, which store information about antibodies and produce them during repeated infection, and T-cells of various classes that help or directly participate in the destruction of virus-infected cells of the body play a crucial role in predicting the fate of infection. Well, and other components of immunity, including innate. In addition, the very amount of the virus that enters the body often plays a critical role in the fate of the infection - this is, for example, established in the case of polio.
Well, and other components of immunity, including innate. In addition, the very amount of the virus that enters the body often plays a critical role in the fate of the infection - this is, for example, established in the case of polio.
In general, all this suggests that in immunology, unfortunately, there is no single and universal parameter, the measurement of which would be sufficient to predict whether a person currently has sufficient immunity to prevent disease or not. Although for individual diseases (for example, the same hepatitis A), long-term observations make it possible to make some reliable predictions about whether a person will get sick, but in general terms, for a new disease like COVID-19, this problem has no solution. To date, the most reliable data on a new infection is data from vaccine efficacy trials. They, of course, do not provide any information on each person separately, but allow us to state that on average vaccinated people are much less likely to get sick than unvaccinated people.
But do vaccines protect at least against a severe course of the disease?
Yes. It’s quite simple here - in all published studies among those vaccinated (and this is about 175 thousand people) there were no cases of hospitalizations and deaths associated with covid (figures can be viewed, for example, here). Of course, deaths in such large groups were recorded, but these deaths were not associated with coronavirus infection. The level of immune response in different people was very different, but since in any case it was enough to prevent severe covid, such protection can be expected to last for a long time.
So why is immunity sometimes lifelong and sometimes not?
How long immunity to a pathogen can last after illness or vaccination depends on two very different things: the stability of immune memory and the rate of evolutionary change of the pathogen itself. This can be easily illustrated by the example of the same flu.
Back in 2008, a group of American infectious disease specialists showed that immune memory can last a very long time and be actually lifelong even in the case of such a seemingly "ephemeral" disease as the flu. Some time before, other researchers had reconstructed the genome sequence of the Spanish flu (it caused the legendary pandemic of 1918), which made it possible to create test systems that detect the presence of antibodies specifically to this type of influenza. The authors of the article then found 32 people born before 1915, analyzed their blood and showed that literally each of them at the time of the study had antibodies to the Spanish flu in the blood, although the virus itself had disappeared from the human population for 90 years. Chemically, these antibodies, of course, were not the same proteins that were developed sometime at the beginning of the 20th century: the half-life of the antibodies themselves as protein molecules is short and is approximately 21 days. Those antibodies that were found in 2008 were synthesized in the body of recovered centenarians shortly before the experiment itself by memory cells. They retained their specificity to the Spanish flu and worked, apparently, throughout their lives, although they did not encounter the virus and could not be reactivated by it for almost a century.
Some time before, other researchers had reconstructed the genome sequence of the Spanish flu (it caused the legendary pandemic of 1918), which made it possible to create test systems that detect the presence of antibodies specifically to this type of influenza. The authors of the article then found 32 people born before 1915, analyzed their blood and showed that literally each of them at the time of the study had antibodies to the Spanish flu in the blood, although the virus itself had disappeared from the human population for 90 years. Chemically, these antibodies, of course, were not the same proteins that were developed sometime at the beginning of the 20th century: the half-life of the antibodies themselves as protein molecules is short and is approximately 21 days. Those antibodies that were found in 2008 were synthesized in the body of recovered centenarians shortly before the experiment itself by memory cells. They retained their specificity to the Spanish flu and worked, apparently, throughout their lives, although they did not encounter the virus and could not be reactivated by it for almost a century.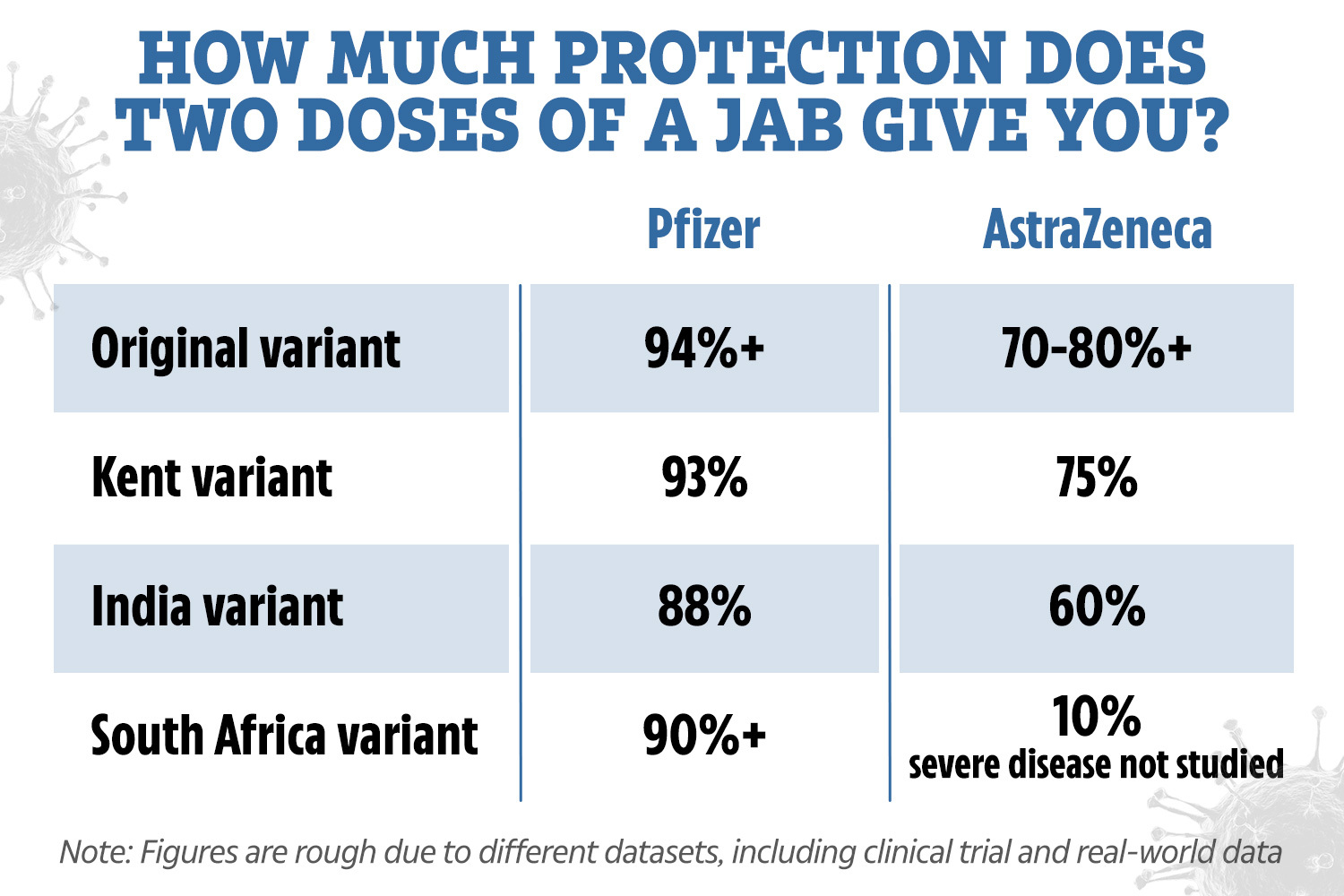 Nevertheless, the emergence of new flu variants requires annual vaccination, but this has nothing to do with the fact that immunity to influenza suddenly disappears on its own.
Nevertheless, the emergence of new flu variants requires annual vaccination, but this has nothing to do with the fact that immunity to influenza suddenly disappears on its own.
And this is no exception - similar work has been done for smallpox, so, in general, the possibility of lifelong immunity does not cause concern among scientists. Of course, there are cases when even in those who have been ill, a second infection becomes possible with the same pathogen as the first time, but this is always the exception, not the rule. For example, the meningococcal vaccine does not normally need to be repeated, but in some immunosuppressed populations, the same vaccine needs to be re-administered every five years or even more frequently.
Be that as it may, the rule is that the immune memory to a particular pathogen usually remains long and often lifelong, but the pathogen can change and move away from the immune response.
Eloisa Lopez / Reuters / Scanpix / LETA
And what is the situation with covid? If re-infections are possible in those who have been ill, does it mean that vaccines are useless?
No, it doesn't. With immunity, most likely, everything will be in order - at least in the future for six months - a year. What will happen next, scientists do not want to predict, but from general considerations, we know that if problems arise, then almost certainly they will not be associated with poor immune memory, but with a change in the virus itself.
With immunity, most likely, everything will be in order - at least in the future for six months - a year. What will happen next, scientists do not want to predict, but from general considerations, we know that if problems arise, then almost certainly they will not be associated with poor immune memory, but with a change in the virus itself.
Now more. The level of antibodies to SARS-CoV-2 does indeed gradually decrease over time. This has already been shown in several studies (for example, 1, 2, 3, 4, 5), where scientists have been monitoring the dynamics of the immune response in recovered patients for several months. There are no such studies on vaccinated people, simply because not much time has passed since the start of vaccination. However, as a first approximation, we can assume that their immunity will behave the same or even more actively: firstly, this is true for many other infections, and secondly, in 100% of those vaccinated against SARS-CoV-2 with Pfizer / BioNTech vaccines , Moderna and Sputnik V, antibody production is observed, and often in larger quantities than in those who have been ill.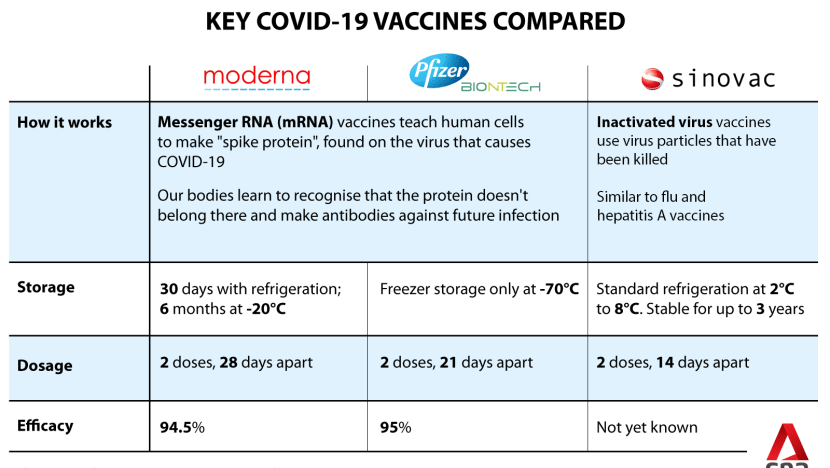
One of the most detailed studies of this kind on immunity duration was recently published by Shine Croty's group at the University of California in Science. In it, unlike several previous ones, scientists followed the evolution of not only antibodies, but also the four most important types of immunity for six months or more (antibodies in plasma, memory B-cells, killer T-cells that directly destroy virus-infected body cells, helper T cells that regulate this process, helping killer T cells).
Two important facts emerge from this study.
- Firstly, scientists have confirmed and clearly shown that the reaction to covid in different people differs much more than the state of immunity in the same person immediately after infection or many (up to eight) months later. These are both qualitative and quantitative differences: T-killers are strongly activated in someone, more antibodies are produced in someone, but in general, almost everyone reacts to all the studied branches of immune defense and this reaction does not suddenly disappear on its own after six months - at 95% of those who recovered by the end of the study "worked" at least three lines of defense.
- Secondly, it turned out that despite a small but noticeable drop in both antibodies and T-cells, the level of B-cells does not decrease - the very ones that are able to reactivate upon a new encounter with infection. In the studied time scale, there are only more of them. This means that there is simply no objective reason to believe that immunity to SARS-CoV-2 can suddenly disappear on its own. Moreover, covid, as the authors emphasize, refers to rather slowly occurring infections, which means that when re-infected, B-cells will have quite enough time to reactivate and produce a large number of antibodies. If you look at a completely different part of immunity - the half-life of T-killers - then it does not give cause for concern: a certain half-life is less than for smallpox, but very similar to the corresponding parameter for yellow fever (and the vaccine against this virus gives lifelong immunity).
In conclusion, the authors stipulate that since the very “correlates of protection” mentioned above have not yet been established for COVID-19, formally reliable conclusions about the future of immunity for recovered patients cannot be made. However, it is clear that the overall picture is not much different from other viral infections, the immunity to which is lifelong, so that “strong immunity against a secondary disease of COVID-19 is possible in most people,” the researchers conclude.
However, it is clear that the overall picture is not much different from other viral infections, the immunity to which is lifelong, so that “strong immunity against a secondary disease of COVID-19 is possible in most people,” the researchers conclude.
Will vaccines work against new variants of SARS-CoV-2?
Unfortunately not equally effective against everyone. Meduza wrote about new variants of the coronavirus not so long ago, and the main thing that is said there still remains relevant: now there are indeed several variants of SARS-CoV-2 that have been proven to have special properties, including greater infectivity, increased lethality and the ability to partially escape immunity. The main and most studied are British (B.1.1.7), South African (B.1.351) and Brazilian (P.1) variants. Although now others are constantly being registered, somewhat similar to these three lines of evolution of the virus (you can see the current infographic here).
There are several studies in which the activity of antibodies produced in response to existing vaccines is tested against new variants of the virus (1, 2, 3). For the British version, scientists do not observe a decrease in the ability to "bind" the virus, however, in the case of the South African and Brazilian, such a decrease is quite significant. The latter variants are similar to each other in the presence of the E484K mutation, which, apparently, is of key importance for the ability to evade antibodies to the classic coronavirus. Its independent occurrence has already been shown in several lines.
For the British version, scientists do not observe a decrease in the ability to "bind" the virus, however, in the case of the South African and Brazilian, such a decrease is quite significant. The latter variants are similar to each other in the presence of the E484K mutation, which, apparently, is of key importance for the ability to evade antibodies to the classic coronavirus. Its independent occurrence has already been shown in several lines.
So, in a recent work by Oxford immunologists, published in Cell, scientists for the first time directly compared the antibody titers needed to neutralize the virus in those vaccinated with two vaccines: Pfizer/BioNTech and AstraZeneca. It turned out that against the South African one, at least 7.6 or even 9 times more neutralizing antibodies are needed (for vaccinated Pfizer/BioNTech and AstraZeneca, respectively) than against the “normal”, Wuhan variant of the virus. It is impossible to translate this decrease in the effectiveness of antibodies into a decrease in the effectiveness of the vaccines themselves according to some formula - as we have already said, due to gaps in knowledge about the correlates of protection for covid.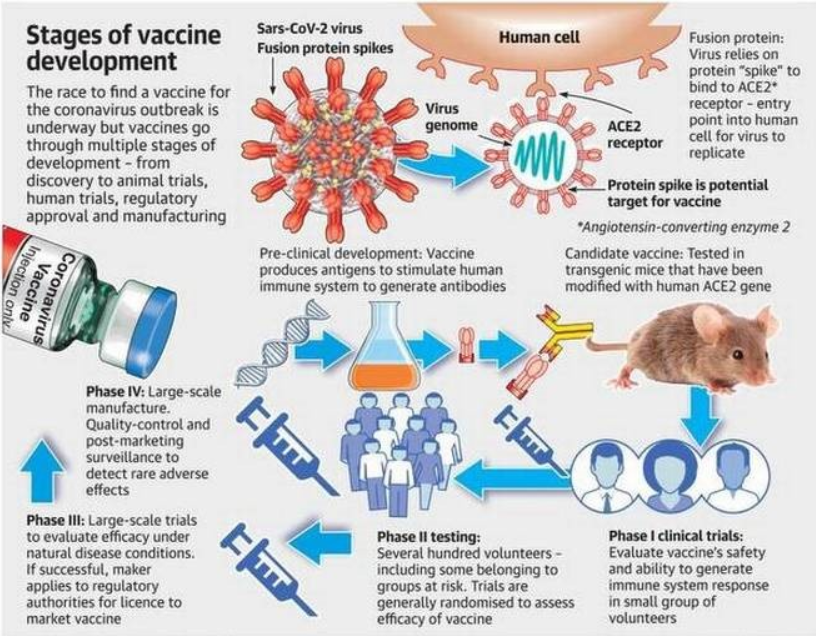 However, it is reasonable to assume that this explains the low effectiveness of the AstraZeneca vaccine, which it showed in South Africa.
However, it is reasonable to assume that this explains the low effectiveness of the AstraZeneca vaccine, which it showed in South Africa.
Now one can hope that even in the case of infection with a new strain, the old vaccine will protect a person from a severe course of the disease. However, there is no reliable data that speaks of this yet. In any case, vaccine manufacturers are already preparing for the spread of new mutations and are working on mechanisms to accelerate the renewal of their drugs.
And what is the result?
Today we know that the level of antibodies to coronavirus infection after the disease does drop over time (although not very quickly), but the memory cells that can respond to re-infection remain. Re-infections are already known but still very rare. With a long and detailed study of the reaction of the immune system, scientists see a response very similar to the one that accompanies the reaction to other viruses, immunity to which is lifelong. That is, potentially vaccine immunity can be very long - but it will depend not on the vaccines themselves, but on how the virus changes.
That is, potentially vaccine immunity can be very long - but it will depend not on the vaccines themselves, but on how the virus changes.
And indeed, already now there are several variants of SARS-CoV-2, which partially "leave" immunity - it is much weaker if it encounters these new variants. Vaccine manufacturers are starting to take this into account and are preparing "updates" of their vaccines. The further development of the pandemic will depend on what happens faster: universal vaccination or the emergence of new variants of SARS-CoV-2 that move away from existing vaccines. In any case, this is an additional argument in favor of maximizing the speed of vaccination, and for people to comply with at least part of the restrictions even after vaccination, which may not work against new options.
Alexander Ershov
Coronavirus vaccination in Russia: a year later
What is known about domestic vaccines, who can be vaccinated and how to prepare for the procedure
Universal vaccination against coronavirus in Russia started on January 18, 2021. Now almost 50% of the population in the country are fully vaccinated, and 51% have received at least one component of the vaccine. 10.6 million were revaccinated. According to Deputy Prime Minister Tatyana Golikova, at least 80% must be vaccinated to achieve herd immunity. This figure has so far been achieved in four regions - Sevastopol, St. Petersburg, Karelia and the Chukotka Autonomous Okrug.
Now almost 50% of the population in the country are fully vaccinated, and 51% have received at least one component of the vaccine. 10.6 million were revaccinated. According to Deputy Prime Minister Tatyana Golikova, at least 80% must be vaccinated to achieve herd immunity. This figure has so far been achieved in four regions - Sevastopol, St. Petersburg, Karelia and the Chukotka Autonomous Okrug.
What vaccines can be vaccinated in Russia?
Now there are five vaccines in civilian circulation - Sputnik V (Gam-COVID-Vak), Sputnik Light, Sputnik M, Epivaccorona and Kovivak.
The first two were created by the Center. Gamaleya by vector technology. It is also used in several foreign vaccines, such as Vaxzevria (formerly AstraZeneca) and Ad26.COV2.S from Johnson & Johnson. Previously, a vaccine against the Ebola virus was developed using the same technology at the Gamaleya Center.
Sputnik V is injected into a small number of body cells with harmless virus-like particles - vectors. They carry with them the "instruction" by which our cells assemble the spike protein of the coronavirus. Auxiliary cells recognize this protein as foreign, and B-lymphocytes remember it and create antibodies specially tailored against it. "Sputnik V" consists of two doses with two different vectors - this is necessary in order to strengthen the immune response. "Sputnik Light" is the first dose of "Sputnik V", it is used for revaccination.
They carry with them the "instruction" by which our cells assemble the spike protein of the coronavirus. Auxiliary cells recognize this protein as foreign, and B-lymphocytes remember it and create antibodies specially tailored against it. "Sputnik V" consists of two doses with two different vectors - this is necessary in order to strengthen the immune response. "Sputnik Light" is the first dose of "Sputnik V", it is used for revaccination.
Epivaccorona is a peptide vaccine developed by the Vector Center. The peptides in its composition are artificially synthesized fragments of the proteins that make up the coronavirus. They are selected so that the body's immune system reacts to them and creates antibodies. The virus itself is not in the vaccine. Two doses are also required to consolidate the effect. It is the only peptide vaccine in the world.
"Kovivak" is an inactivated vaccine created at the Chumakov Institute. Inactivated vaccines are among the most widely used in the world. For production in the laboratory, a specially isolated strain of the virus multiplies. Then it is chemically neutralized, leaving the protein structure intact. Once in the body, these viral remains attract immune cells (for this they use an irritant substance - an adjuvant), and they produce antibodies.
The Sputnik M vaccine is also registered in Russia for adolescents aged 12–17. In terms of composition, this is the same Sputnik V, but adapted for a younger organism. The first batches were released into civilian circulation at the end of December.
What is known about the safety of vaccines?
All vaccines went through several stages of testing before being released into civilian circulation. They were first tested in animals to rule out serious adverse reactions, such as mutagenicity, a threat to fertility and fetal health during pregnancy. They were then administered to a small group of people and finally to thousands of volunteers. Data on undesirable effects are also collected after the registration of vaccines.
Most data on the safety of Sputnik V - the vaccine was registered first, and in addition, it was studied in other countries (Argentina, San Marino, UAE). In Russia, almost 70 million people completed the full course, and another 100 million abroad.
During testing, side effects were observed in more than half of the cases, but most often - pain at the injection site, weakness, fever. In the elderly, the risk of adverse reactions is significantly less; women are also known to report side effects more often than men.
According to the report of the Ministry of Health of Argentina, after vaccinating 11 million people with Sputnik V, only 2% experienced severe (requiring hospitalization) side effects. Among the rare reactions are an increase in lymph nodes (0.83 cases per 100 thousand), anaphylaxis (0.1 per 100 thousand), a metallic taste in the mouth (0.08 per 100 thousand).
There were no deaths directly related to vaccination.
The creators of "Epivaccorona" position it as a "soft" vaccine, from which there are almost no side effects. They explain this by the fact that the vaccine does not contain a live virus, its components do not penetrate into the cells, and therefore do not cause a strong reaction of the immune system. More than 1 million people received the full course of Epivacorona.
During clinical trials, the vaccine showed no side effects, except for minor and short-term (one to two days) soreness at the injection site in several people. According to Rinat Maksyutov, director general of the Vector center that developed the vaccine, pain at the injection site and fever are the only side effects that have been identified after vaccinating a million people.
In studies in people over 60 years of age, after the first vaccination, local reactions were noted in 1.3%, after the second - in 0.6%. Most often it was pain at the injection site, in a few people - a short-term fever.
No vaccination-related deaths were recorded. No one needed hospitalization either.
Ilya Gomyranov
27 years old, biologist
Many people around me got sick, some died
During the first lockdown, more than a quarter of people in my circle already got sick. Some have died. Due to both the specifics of the work and my personal desire, I do not want to limit myself in my travels and refuse to meet. So I decided to indulge. I would advise everyone to take an antibody test to exclude the possibility of an asymptomatic course of the disease at the moment. Well, it’s better to get vaccinated before the day off, so that in case of poor health, you can lie down
Ilya Gomyranov
27 years old, biologist
Data on "Kovivak" is still the least. To date, only the results of preclinical trials have been published - on mice and guinea pigs. No pathological changes after the injection were found in them. The instructions for the drug say that the most frequent reactions during the tests were local reactions: pain at the injection site (15% of cases), headache (2%), induration at the injection site (1%) and short-term fever (1%). The testers did not reveal any severe systemic reactions.
Can everyone be vaccinated?
Initially, vaccines had a fairly wide range of contraindications. The effect of drugs has not yet been sufficiently studied (eg, in pregnant and lactating women, children, people with chronic diseases). Gradually, some of the bans were lifted.
Now the fewest contraindications for "Sputnik V". In the list for "withdrawal" - hypersensitivity to the components of the vaccine, severe allergic reactions in the past, infectious diseases or exacerbations of chronic diseases at the time of vaccination, a severe reaction to the first component.
In the summer of 2021, the Ministry of Health allowed pregnant women to be vaccinated "when the expected benefit to the mother outweighs the potential risk to the fetus." We are talking about those who have an increased risk of a severe course of the disease, and the gestational age is at least 22 weeks. In October, the Ministry of Health lifted the ban on breastfeeding women. At the same time, there was a reservation that there is no data on whether the active substances in the composition of the vaccine can penetrate into breast milk.
Inoculation with Sputnik V is allowed, including cancer patients, but no later than two weeks before the start of treatment or surgery. Those who have autoimmune diseases should consult a doctor to make a decision. The Ministry of Health also issued a clarification that HIV-positive status is not a contraindication for vaccination.
Kovivak has the same contraindications as Sputnik V, but it should not be administered during pregnancy and breastfeeding, as well as people over 60 years of age. It is recommended with caution in chronic diseases, in patients taking immunosuppressive drugs, in blood diseases.
Epivaccorona has the most contraindications: in addition to the same as Sputnik, the instructions also indicate primary immunodeficiency, malignant blood diseases and neoplasms, pregnancy and the period of breastfeeding. But it can be administered to older people.
All vaccines listed are contraindicated under 18 years of age. At the same time, on November 24, the Ministry of Health registered a vaccine for adolescents 12-17 years old - Sputnik M. Its contraindications are generally the same as those of "Sputnik V" (including it can be used during pregnancy after consulting a doctor).
How well do vaccines protect? Why is the pandemic still not over?
No vaccine provides 100% protection against infection. The chance of getting infected after vaccination depends on several factors.
How well did the vaccine work? Even 20% of those who have been ill do not develop immunity to the coronavirus, and they can become infected again. After vaccination, this figure can reach up to 10%. At the same time, experts advise not to judge only by the level of antibodies, since cellular immunity can also provide protection.
How long have you been vaccinated . Six months after vaccination, the quantity and quality of antibodies are reduced. Therefore, the Ministry of Health recommends revaccination every six months.
Are you exposed to high doses of the virus. If large concentrations of viral particles enter the body, they can break through the defense.
Which variant of the virus is spread around you . The delta and omicron variants are notorious for being less defensive against them than against the original Wuhan variant. For example, in those revaccinated with Sputnik V, after two or three months, the level of neutralizing antibodies against Omicron decreased by 7.13 times.
But data from trials and mass use of vaccines suggests that they can avoid hospitalization and death and significantly reduce the risk of infection.
Most efficiency data is available from Sputnik V. The vaccine was 91.6% effective in Phase 3 trials and 100% effective against moderate to severe COVID-19. In older people, the vaccine was 78.6% effective against infection, 87.6% against hospitalization, and 84.8% against death.
Additional studies have shown that Sputnik V is effective against other variants of coronavirus, including against the delta variant (the study was carried out before the discovery of the omicron variant). According to Argentine doctors, vaccination with two components of Sputnik V is more effective against the delta strain than drugs from AstraZeneca and Sinopharm.
According to the head of the Center. Gamalei Alexander Gintsburg, the effectiveness of Sputnik V against the omicron variant is 75%.
The effectiveness of "Sputnik Light" according to the results of the research was 79.4%.
So far, only immunological efficacy is known for "Epivaccorone" - the percentage of those vaccinated who have formed antibodies. According to the test results, it is 79%. At the same time, according to the statements of the deputy head of the Vector center, Tatiana Nepomnyashchikh, after being vaccinated with Epivacorona, only 1% become ill with coronavirus. Later, the deputy director for scientific work of the Central Research Institute of Epidemiology of Rospotrebnadzor, Alexander Gorelov, estimated the effectiveness of the vaccine at 90%.
Kovivak also has immunological efficacy data only. According to preliminary data, antibodies were formed in 80% of the study participants. Later, the quality director of the center Alexandra Sinyugina reported that the vaccine protects against infection by 98.4% and from a severe form of the disease by 99.1%.
How to prepare for vaccination? How to behave during the procedure and after it?
There is no need for special examination before injection, although it is worth consulting with your doctor if you are at risk. A few days before vaccination, you should exclude alcohol, avoid serious physical exertion, stress and hypothermia, do not smoke and do not eat fatty and fried foods, and do not take medications that suppress the activity of the immune system. During the first days after vaccination, the recommendations are the same.
The drug is administered intramuscularly - in the upper arm or thigh. Before the procedure, you will be examined by a doctor, and after it you will need to stay in the clinic for some time - in case of unforeseen reactions.
Rospotrebnadzor recommends self-isolation and all precautions between two doses, as the disease may affect the effect of the vaccine. After the first dose of the vaccine, there is still no stable immunity and a high risk of infection remains.
Vladislav Rusakov
33 years old, power engineer
I want to live a fuller life
When every person coughing next to me causes anxiety, I want to do something about it already.
Live life to the fullest, without looking back at the pandemic. I work in the energy sector: when I found out that vaccination for our category would begin on Monday, I immediately signed up on the government services portal. I already get a flu shot every year, so all this is familiar to me
Vladislav Rusakov
33 years old, power engineer
How long does the protection last? When should you revaccinate?
So far, it is reliably known that immunity from the vaccine of the Center. Gamaleya is preserved for six months. At the same time, the antibody titer naturally decreases, but immunological memory is preserved - cells that, upon a new encounter with infection, can quickly create a new supply of antibodies.
According to Denis Logunov, deputy director of the Gamaleya Center, there is no specific antibody titer that could protect the body from infection with the coronavirus. However, in his opinion, titers that provide a "substantial level of protection" (about 80-90%) and protect against the average course of the disease are of the order of 200-300 BAU / ml.
Doctor-infectionist, candidate of medical sciences Ekaterina Stepanova believes that about 1.5 thousand BAU/ml is needed to protect against the "delta" variant. At the same time, she stressed that there is no “dangerous” (too high) antibody titer and it is possible to be vaccinated even if you have immunity after an illness.
When does the protection start?
According to the data of the third phase of the tests, which are given by the specialists of the Center. Gamaleya, already three weeks after receiving the first dose of the vaccine, the probability of getting sick is reduced by 90%. Full protection occurs three weeks after the second immunization. According to the Vector Center, sufficient protection against the vaccine produced by it is formed starting from the 21st day after the first injection. You can find out if an immune response has formed by the results of an antibody test.
Pavel Skrylnikov
29 years old, journalist
I wanted to participate in the fight against the pandemic
Back in the spring of 2020, I registered as a volunteer to help the elderly, but the application remained unclaimed. And I wanted to participate in the fight against the pandemic at least somehow. Therefore, as soon as I learned that a vaccine would be tested on volunteers in Moscow, I immediately signed up. A year later, I still had the coronavirus. I think if I hadn’t been grafted, I might not have pulled out
Pavel Skrylnikov
29 years old, journalist
Can I not wear a mask and keep my distance after vaccination?
Since the vaccine does not provide 100% protection against infection, you must continue to follow preventive measures - wear a mask, wash your hands more often and avoid crowds. After all, even if you do not have symptoms, you can still be a carrier of the virus. It should be borne in mind that the risk of infection increases if the body experiences a large viral load (for example, you are among the infected for a long time).
When, where and who can be vaccinated? What does vaccinated status give?
You can get vaccinated at special points for vaccination based on city clinics. Vaccination is completely voluntary and free of charge for Russian citizens. You can also sign up online through the portal "Gosuslugi".
After vaccination, a certificate is issued for a period of six months. Now the presentation of a certificate of vaccination in different regions is required when attending sports and physical education, as well as congress and exhibition events with more than 40 people; visits to swimming pools and fitness clubs; visiting theaters, cinemas, concert halls, circuses, museums and exhibitions; accommodation in hotels and hotels, rest houses; attending the solemn ceremony of marriage in the registry office.
Now each region imposes restrictions based on its own situation.
Russian vaccination certificates are recognized in several dozen countries around the world, including Australia, Armenia, Egypt, Israel, Moldova, Turkey, Croatia and Montenegro. In a number of countries, only a vaccination given 14 days before the date of arrival is recognized.
Are foreign vaccines available in Russia? How are things going with the recognition of certificates?
Pfizer announced its readiness to consider registration of its own vaccine in Russia. In Russia, a vaccine from the Chinese company Livzon Mabpharm Inc is being tested, as a result of which it can be registered. However, no foreign vaccine has been registered in Russia so far. Those vaccinated with foreign vaccines do not receive certificates and related rights.
There are contraindications, specialist advice is required.