What is preeclampsia caused by
Pre-eclampsia - Causes - NHS
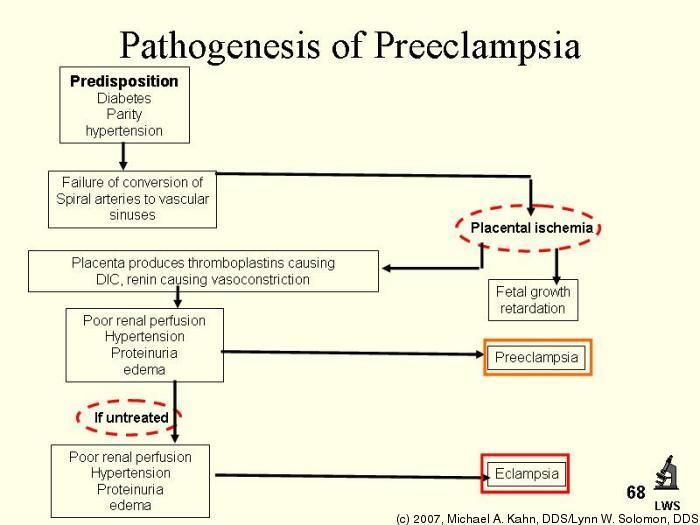
Pre-eclampsia is thought to be caused by the placenta not developing properly due to a problem with the blood vessels supplying it. The exact cause isn't fully understood.
Placenta
The placenta is the organ that links the mother's blood supply to her unborn baby's blood supply.
Food and oxygen pass through the placenta from mother to baby. Waste products can pass from the baby back into the mother.
To support the growing baby, the placenta needs a large and constant supply of blood from the mother.
In pre-eclampsia, the placenta doesn't get enough blood. This could be because the placenta didn't develop properly as it was forming during the first half of the pregnancy.
The problem with the placenta means the blood supply between mother and baby is disrupted.
Signals or substances from the damaged placenta affect the mother's blood vessels, causing high blood pressure (hypertension).
At the same time, problems in the kidneys may cause important proteins that should remain in the mother's blood to leak into her urine, resulting in protein in the urine (proteinuria).
What causes problems with the placenta?
In the initial stages of pregnancy, the fertilised egg implants itself into the wall of the womb (uterus). The womb is the organ a baby grows inside during pregnancy.
The fertilised egg produces root-like growths called villi, which help to anchor it to the lining of the womb.
The villi are fed nutrients through blood vessels in the womb and eventually grow into the placenta.
During the early stages of pregnancy, these blood vessels change shape and become wider.
If the blood vessels don't fully transform, it's likely that the placenta won't develop properly because it won't get enough nutrients. This may lead to pre-eclampsia.
It's still unclear why the blood vessels don't transform as they should.
It's likely that inherited changes in your genes have some sort of role, as the condition often runs in families. But this only explains some cases.
Who's most at risk?
Some factors have been identified that could increase your chances of developing pre-eclampsia.
These include:
- having an existing medical problem – such as diabetes, kidney disease, high blood pressure, lupus or antiphospholipid syndrome
- previously having pre-eclampsia
Some factors also increase your chances by a small amount.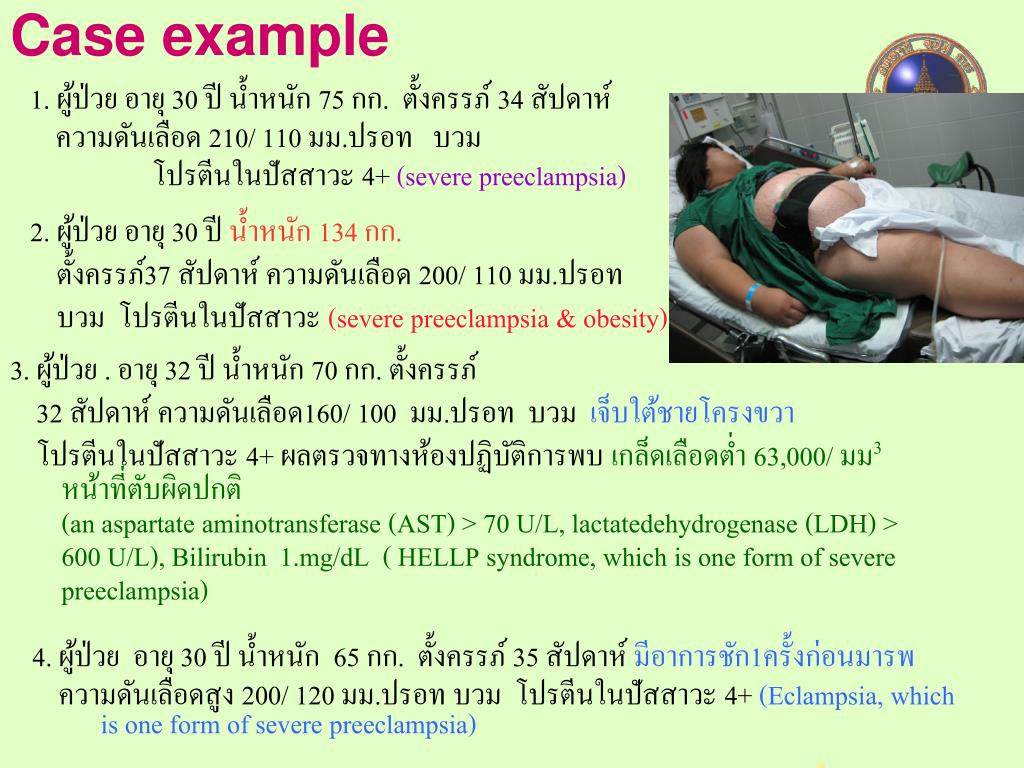
If you have 2 or more of these together, your chances are higher:
- it's your first pregnancy – pre-eclampsia is more likely to happen during the first pregnancy than during any subsequent pregnancies
- it's been at least 10 years since your last pregnancy
- you have a family history of the condition – for example, your mother or sister has had pre-eclampsia
- you're over the age of 40
- you were obese at the start of your pregnancy – meaning you had a body mass index (BMI) of 35 or more
- you're expecting twins or more, such as twins or triplets
If you're considered to be at a high risk of developing pre-eclampsia, you may be advised to take a 75 to 150mg dose of aspirin every day from when you're 12 weeks pregnant until your baby is born.
Evidence suggests this can lower your chances of developing the condition.
Page last reviewed: 28 September 2021
Next review due: 28 September 2024
Preeclampsia - Symptoms and causes
Overview
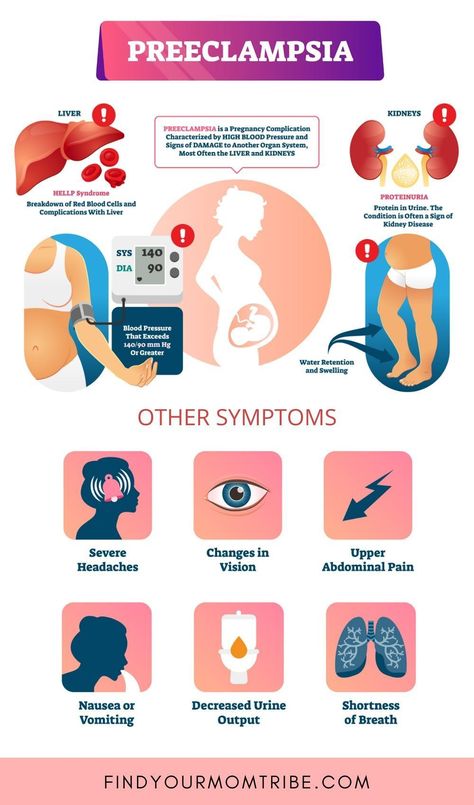
Preeclampsia is a complication of pregnancy. With preeclampsia, you might have high blood pressure, high levels of protein in urine that indicate kidney damage (proteinuria), or other signs of organ damage. Preeclampsia usually begins after 20 weeks of pregnancy in women whose blood pressure had previously been in the standard range.
Left untreated, preeclampsia can lead to serious — even fatal — complications for both the mother and baby.
Early delivery of the baby is often recommended. The timing of delivery depends on how severe the preeclampsia is and how many weeks pregnant you are. Before delivery, preeclampsia treatment includes careful monitoring and medications to lower blood pressure and manage complications.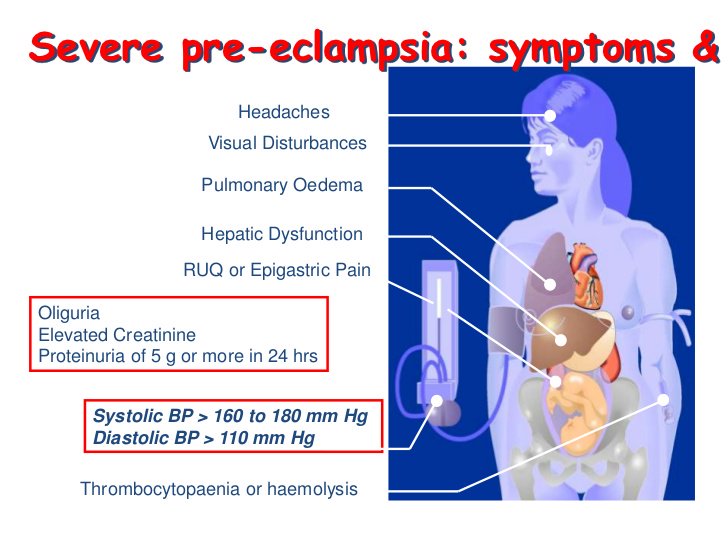
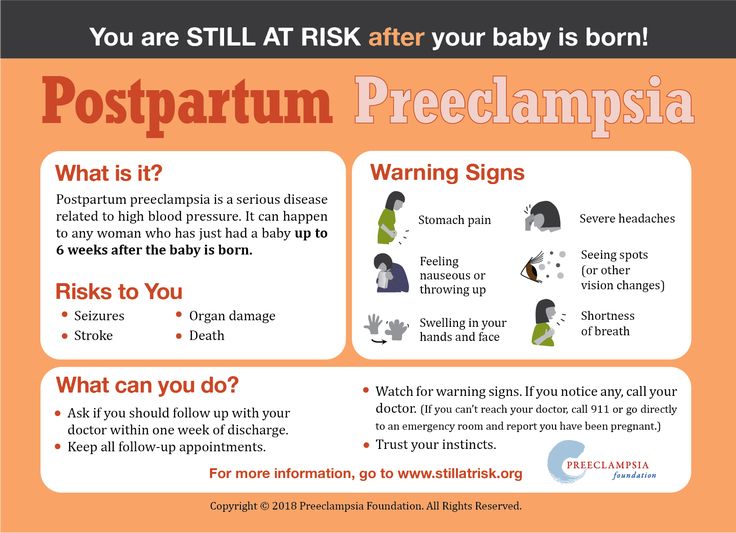
Preeclampsia may develop after delivery of a baby, a condition known as postpartum preeclampsia.
Products & Services
- Book: Mayo Clinic Guide to a Healthy Pregnancy
Symptoms
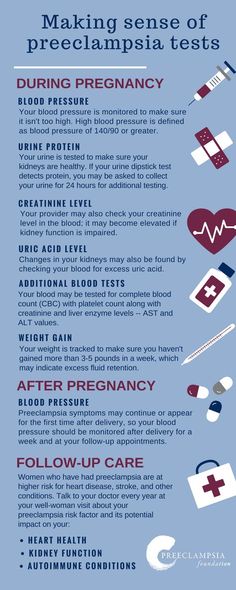
The defining feature of preeclampsia is high blood pressure, proteinuria, or other signs of damage to the kidneys or other organs. You may have no noticeable symptoms. The first signs of preeclampsia are often detected during routine prenatal visits with a health care provider.
Along with high blood pressure, preeclampsia signs and symptoms may include:
- Excess protein in urine (proteinuria) or other signs of kidney problems
- Decreased levels of platelets in blood (thrombocytopenia)
- Increased liver enzymes that indicate liver problems
- Severe headaches
- Changes in vision, including temporary loss of vision, blurred vision or light sensitivity
- Shortness of breath, caused by fluid in the lungs
- Pain in the upper belly, usually under the ribs on the right side
- Nausea or vomiting
Weight gain and swelling (edema) are typical during healthy pregnancies. However, sudden weight gain or a sudden appearance of edema — particularly in your face and hands — may be a sign of preeclampsia.
However, sudden weight gain or a sudden appearance of edema — particularly in your face and hands — may be a sign of preeclampsia.
When to see a doctor
Make sure you attend your prenatal visits so that your health care provider can monitor your blood pressure. Contact your provider immediately or go to an emergency room if you have severe headaches, blurred vision or other visual disturbances, severe belly pain, or severe shortness of breath.
Because headaches, nausea, and aches and pains are common pregnancy complaints, it's difficult to know when new symptoms are simply part of being pregnant and when they may indicate a serious problem — especially if it's your first pregnancy. If you're concerned about your symptoms, contact your doctor.
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.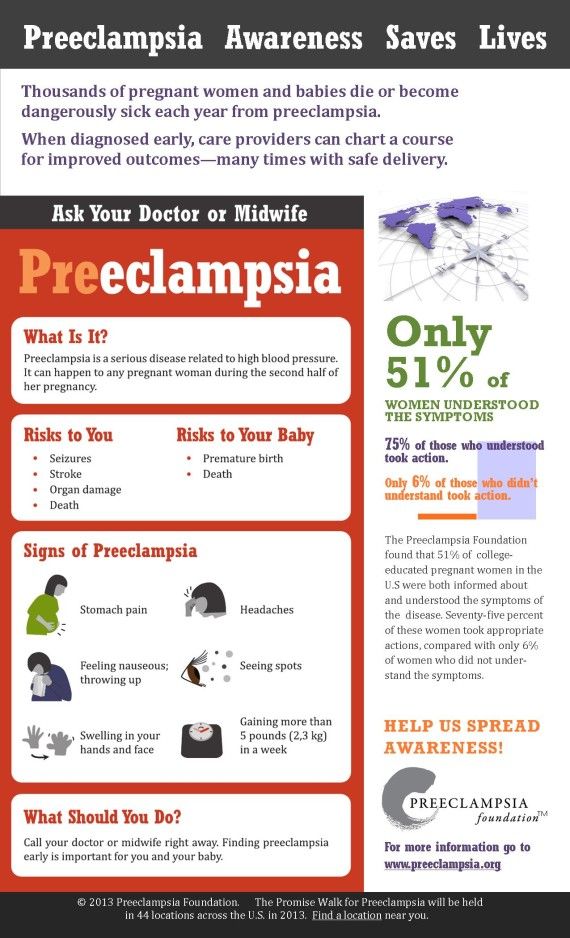 Click here for an email preview.
Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
The exact cause of preeclampsia likely involves several factors. Experts believe it begins in the placenta — the organ that nourishes the fetus throughout pregnancy.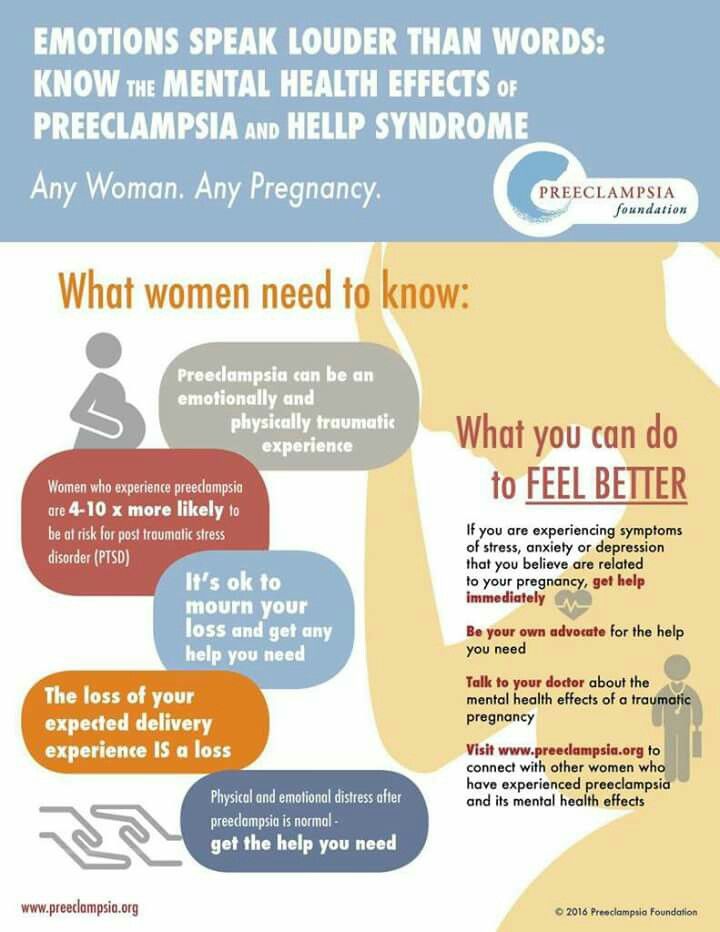 Early in a pregnancy, new blood vessels develop and evolve to supply oxygen and nutrients to the placenta.
Early in a pregnancy, new blood vessels develop and evolve to supply oxygen and nutrients to the placenta.
In women with preeclampsia, these blood vessels don't seem to develop or work properly. Problems with how well blood circulates in the placenta may lead to the irregular regulation of blood pressure in the mother.
Other high blood pressure disorders during pregnancy
Preeclampsia is one high blood pressure (hypertension) disorder that can occur during pregnancy. Other disorders can happen, too:
- Gestational hypertension is high blood pressure that begins after 20 weeks without problems in the kidneys or other organs. Some women with gestational hypertension may develop preeclampsia.
- Chronic hypertension is high blood pressure that was present before pregnancy or that occurs before 20 weeks of pregnancy. High blood pressure that continues more than three months after a pregnancy also is called chronic hypertension.
- Chronic hypertension with superimposed preeclampsia occurs in women diagnosed with chronic high blood pressure before pregnancy, who then develop worsening high blood pressure and protein in the urine or other health complications during pregnancy.
Risk factors
Conditions that are linked to a higher risk of preeclampsia include:
- Preeclampsia in a previous pregnancy
- Being pregnant with more than one baby
- Chronic high blood pressure (hypertension)
- Type 1 or type 2 diabetes before pregnancy
- Kidney disease
- Autoimmune disorders
- Use of in vitro fertilization
Conditions that are associated with a moderate risk of developing preeclampsia include:
- First pregnancy with current partner
- Obesity
- Family history of preeclampsia
- Maternal age of 35 or older
- Complications in a previous pregnancy
- More than 10 years since previous pregnancy
Other risk factors
Several studies have shown a greater risk of preeclampsia among Black women compared with other women.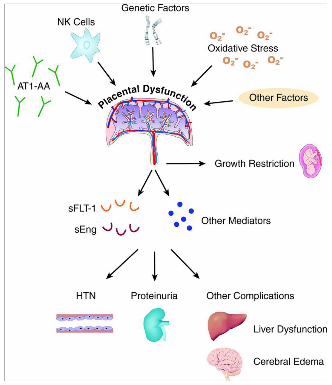 There's also some evidence of an increased risk among indigenous women in North America.
There's also some evidence of an increased risk among indigenous women in North America.
A growing body of evidence suggests that these differences in risk may not necessarily be based on biology. A greater risk may be related to inequities in access to prenatal care and health care in general, as well as social inequities and chronic stressors that affect health and well-being.
Lower income also is associated with a greater risk of preeclampsia likely because of access to health care and social factors affecting health.
For the purposes of making decisions about prevention strategies, a Black woman or a woman with a low income has a moderately increased risk of developing preeclampsia.
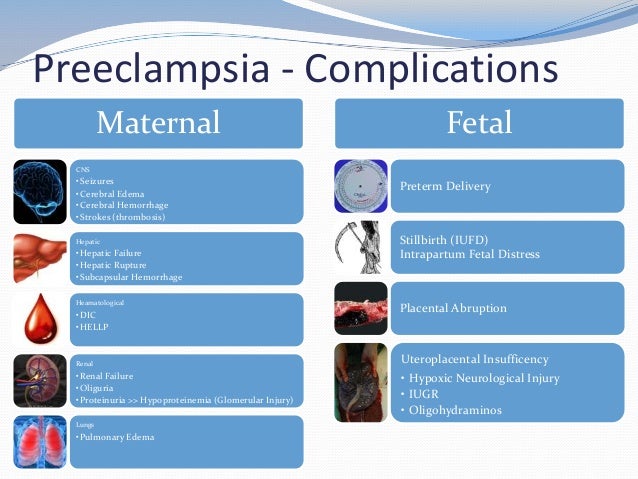
Complications
Complications of preeclampsia may include:
- Fetal growth restriction. Preeclampsia affects the arteries carrying blood to the placenta. If the placenta doesn't get enough blood, the baby may receive inadequate blood and oxygen and fewer nutrients.
 This can lead to slow growth known as fetal growth restriction.
This can lead to slow growth known as fetal growth restriction. - Preterm birth. Preeclampsia may lead to an unplanned preterm birth — delivery before 37 weeks. Also, planned preterm birth is a primary treatment for preeclampsia. A baby born prematurely has increased risk of breathing and feeding difficulties, vision or hearing problems, developmental delays, and cerebral palsy. Treatments before preterm delivery may decrease some risks.
- Placental abruption. Preeclampsia increases your risk of placental abruption. With this condition, the placenta separates from the inner wall of the uterus before delivery. Severe abruption can cause heavy bleeding, which can be life-threatening for both the mother and baby.
-
HELLP syndrome. HELLP stands for hemolysis (the destruction of red blood cells), elevated liver enzymes and low platelet count.
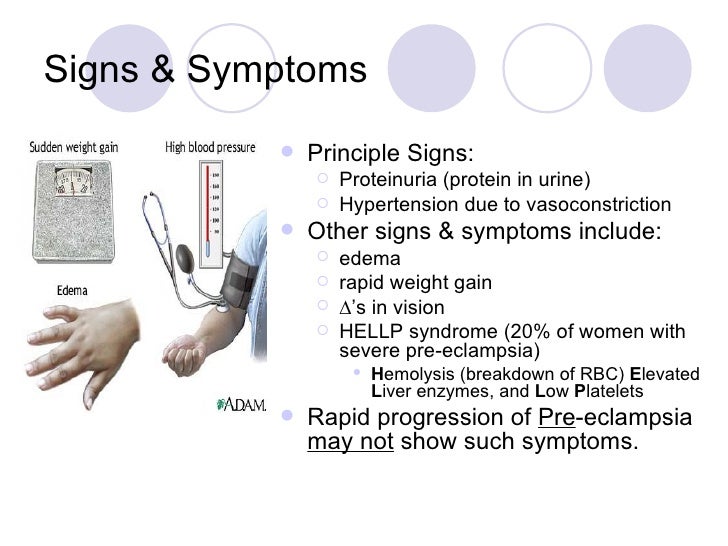 This severe form of preeclampsia affects several organ systems. HELLP syndrome is life-threatening to the mother and baby, and it may cause lifelong health problems for the mother.
This severe form of preeclampsia affects several organ systems. HELLP syndrome is life-threatening to the mother and baby, and it may cause lifelong health problems for the mother.Signs and symptoms include nausea and vomiting, headache, upper right belly pain, and a general feeling of illness or being unwell. Sometimes, it develops suddenly, even before high blood pressure is detected. It also may develop without any symptoms.
-
Eclampsia. Eclampsia is the onset of seizures or coma with signs or symptoms of preeclampsia. It is very difficult to predict whether a patient with preeclampsia will develop eclampsia. Eclampsia can happen without any previously observed signs or symptoms of preeclampsia.
Signs and symptoms that may appear before seizures include severe headaches, vision problems, mental confusion or altered behaviors.
 But, there are often no symptoms or warning signs. Eclampsia may occur before, during or after delivery.
But, there are often no symptoms or warning signs. Eclampsia may occur before, during or after delivery. - Other organ damage. Preeclampsia may result in damage to the kidneys, liver, lung, heart, or eyes, and may cause a stroke or other brain injury. The amount of injury to other organs depends on how severe the preeclampsia is.
- Cardiovascular disease. Having preeclampsia may increase your risk of future heart and blood vessel (cardiovascular) disease. The risk is even greater if you've had preeclampsia more than once or you've had a preterm delivery.
Prevention
Medication
The best clinical evidence for prevention of preeclampsia is the use of low-dose aspirin. Your primary care provider may recommend taking an 81-milligram aspirin tablet daily after 12 weeks of pregnancy if you have one high-risk factor for preeclampsia or more than one moderate-risk factor.
It's important that you talk with your provider before taking any medications, vitamins or supplements to make sure it's safe for you.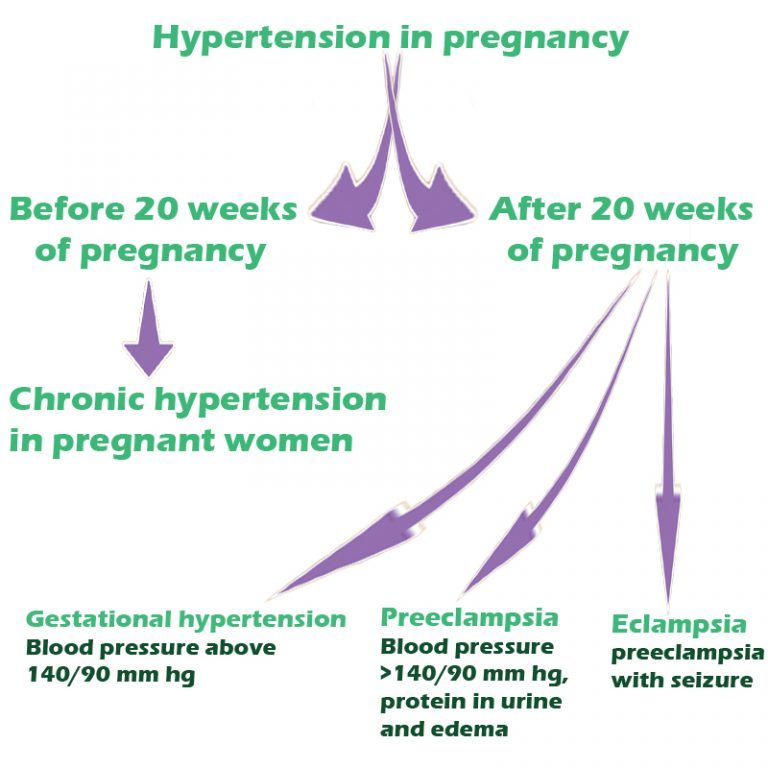
Lifestyle and healthy choices
Before you become pregnant, especially if you've had preeclampsia before, it's a good idea to be as healthy as you can be. Talk to your provider about managing any conditions that increase the risk of preeclampsia.
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
Preeclampsia and pregnancy | Ida-Tallinna Keskaigla
Preeclampsia and pregnancy
The purpose of this information leaflet is to provide the patient with information about the nature, occurrence, risk factors, symptoms and treatment of preeclampsia.
What is preeclampsia?
Pre-eclampsia is a disease that occurs during pregnancy and is characterized by high blood pressure and protein in the urine. Preeclampsia is one of the most common complications of pregnancy. Epilepsy-like seizures occur in severe preeclampsia and are life-threatening.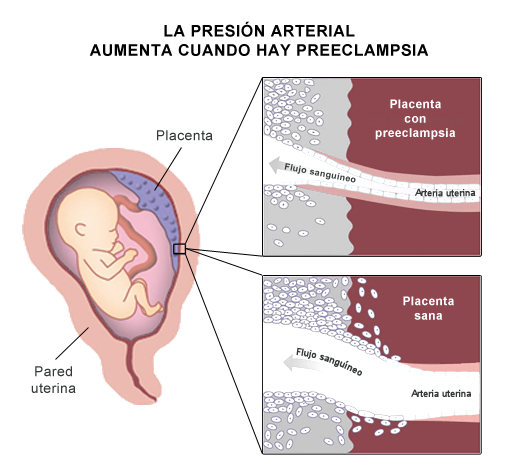
What symptoms may indicate the development of preeclampsia?
High blood pressure - blood pressure values are 140/90 mmHg. Art. or higher. If systolic (upper) or diastolic (lower) blood pressure rises by 30 mm Hg. Art. or more, then such an increase cannot be ignored.
Protein in urine - 300 mg in urine collected over 24 hours, or +1 value on a rapid test.
Swelling of the arms, legs or face , especially under the eyes or if the skin is pitted when pressed. Edema can occur in all pregnant women and is generally harmless, but rapidly developing edema should be taken into account.
Headache that does not improve after taking pain medication.
Visual disturbances - double vision or blurred vision, dots or flashes before the eyes, auras.
Nausea or pain in the upper abdomen - These symptoms are often mistaken for indigestion or gallbladder pain.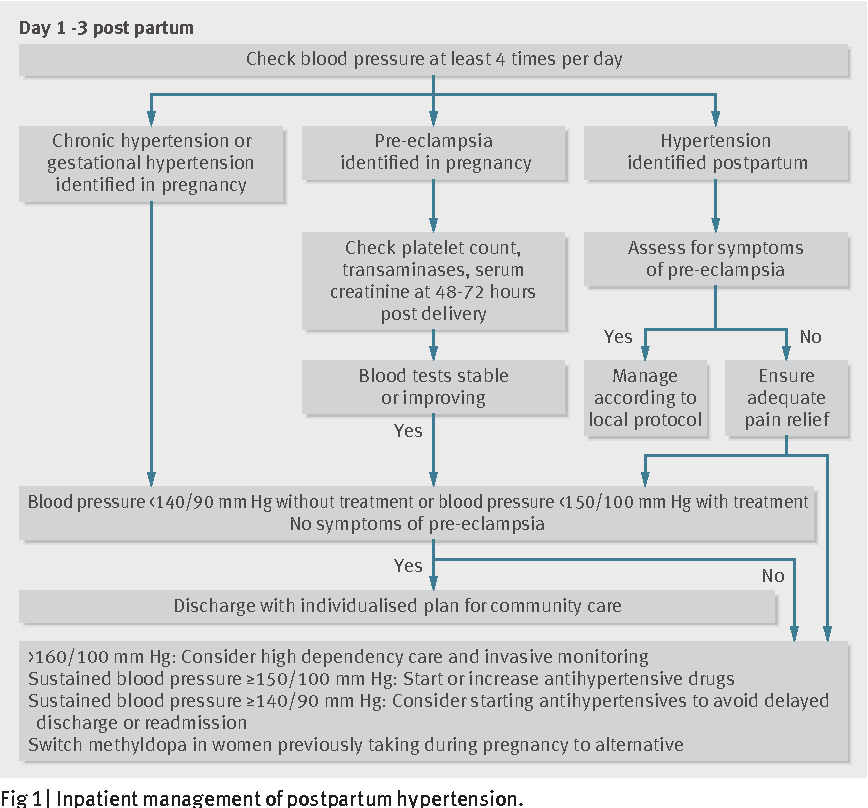 Nausea in the second half of pregnancy is not normal.
Nausea in the second half of pregnancy is not normal.
Sudden weight gain - 2 kg or more per week.
As a rule, there is a mild course of the disease that occurs at the end of pregnancy and has a good prognosis. Sometimes, preeclampsia can worsen quickly and be dangerous to both mother and fetus. In such cases, rapid diagnosis and careful monitoring of the mother and child are of paramount importance.
Unfortunately, most women develop symptoms in the final stages of the disease. If you experience any of the above symptoms, you should contact your midwife, gynecologist, or the Women's Clinic emergency department.
Is preeclampsia called toxemia of pregnancy?
Previously, pre-eclampsia was really called toxicosis, or toxemia, since it was believed that the cause of the disease was toxins, that is, poisons in the blood of a pregnant woman.
What is the difference between preeclampsia and gestational hypertension?
Pregnancy hypertension is an increase in blood pressure above normal after the 20th week of pregnancy. With hypertension of pregnant women, protein in the urine is not observed.
With hypertension of pregnant women, protein in the urine is not observed.
What is HELLP syndrome?
HELLP syndrome is one of the most severe forms of preeclampsia. HELLP syndrome is rare and sometimes develops before symptoms of preeclampsia appear. Sometimes the syndrome is difficult to diagnose, as the symptoms resemble gallbladder colic or a cold.
When does preeclampsia occur?
Preeclampsia usually occurs after the 20th week of pregnancy. As a rule, preeclampsia goes away after delivery, but complications can occur up to six weeks after delivery, during which careful monitoring of the condition is necessary. If by the sixth week after birth, blood pressure does not return to normal, then you need to contact a cardiologist, who will begin treatment against hypertension.
What is the cause of preeclampsia?
The causes of the disease are still not clear, there are only unproven hypotheses.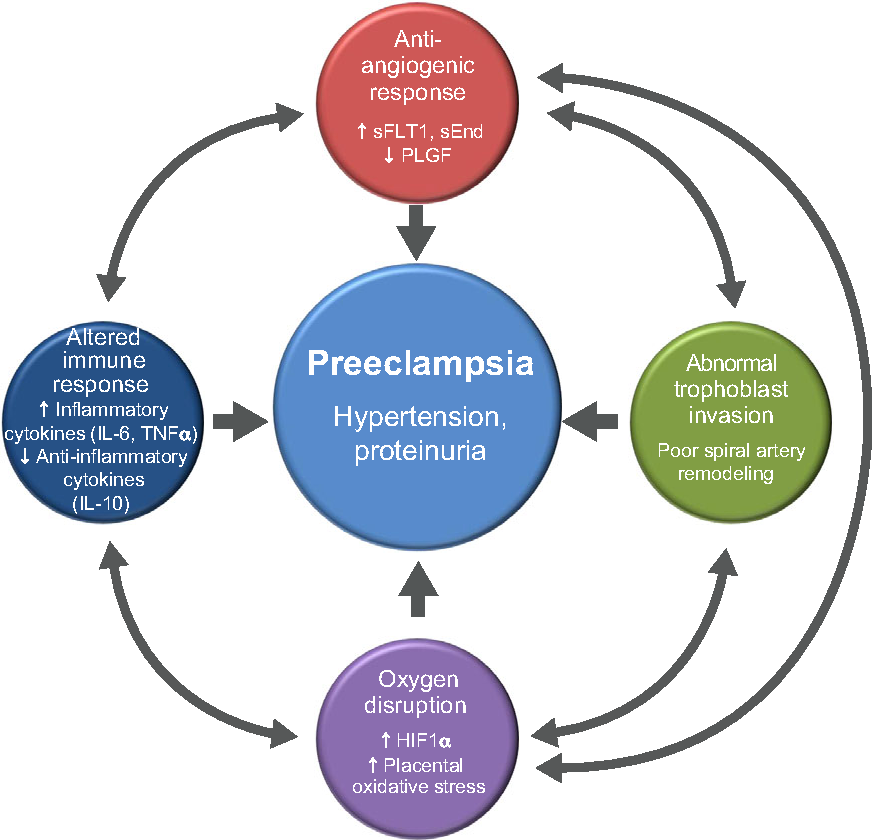
How does the disease affect pregnant women and pregnancy?
Most preeclamptic pregnancies have a favorable outcome and a healthy baby is born. However, the disease is very serious and is one of the most common causes of death of the child and mother. Preeclampsia affects a woman's kidneys, liver, and other vital organs, and if left untreated, it can cause seizures (eclampsia), cerebral hemorrhage, multiple organ failure, and death.
How does the disease affect the fetus?
In preeclampsia, the fetus does not receive enough oxygen and nutrients to grow, and intrauterine growth retardation may occur. In addition, the placenta may separate from the uterine wall before the baby is born. Since the only treatment for preeclampsia is childbirth, sometimes a pregnancy has to be terminated prematurely. Until the 34th week of pregnancy, the lungs of the fetus have not yet matured, and steroid hormones are injected intramuscularly into the pregnant woman to prepare his lungs.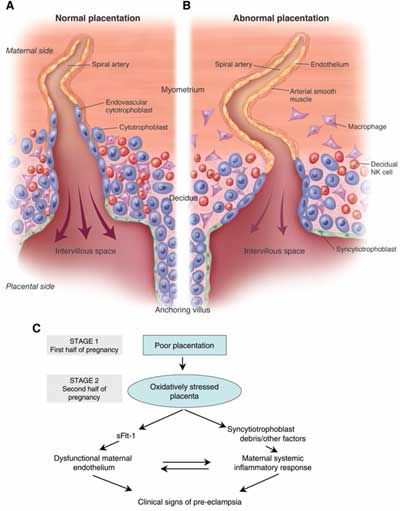 In addition to the immaturity of the lungs, the health of a premature baby is threatened by many other diseases.
In addition to the immaturity of the lungs, the health of a premature baby is threatened by many other diseases.
Who is at risk of developing preeclampsia?
Preeclampsia occurs in approximately 8% of pregnant women, many of whom have no known risk factors.
What are the risk factors for preeclampsia?
Patient-related risk factors
- First pregnancy
- Pre-eclampsia during a previous pregnancy
- Age over 40 or under 18
- High blood pressure before pregnancy
- Diabetes before or during pregnancy
- Multiple pregnancy
- Overweight (BMI> 30)
- Systemic lupus erythematosus or other autoimmune disease
- Polycystic ovary syndrome
- Long interval between two pregnancies
Risk factors associated with the patient's family
- Pre-eclampsia in the mother's or father's family
- Parental high blood pressure or heart disease
- Diabetes mellitus
What is the prevention and treatment of preeclampsia
The first trimester screening or Oscar test also calculates the risk of preeclampsia in addition to the most common chromosomal disorders.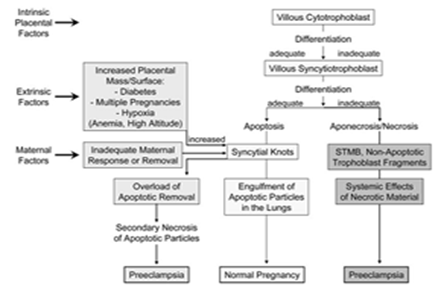 In case of high risk, pregnant women are advised to take aspirin (acetylsalicylic acid) at a dose of 150 mg in the evenings until the 36th week of pregnancy. This helps reduce the chance of preeclampsia by the 34th week of pregnancy by up to 80%.
In case of high risk, pregnant women are advised to take aspirin (acetylsalicylic acid) at a dose of 150 mg in the evenings until the 36th week of pregnancy. This helps reduce the chance of preeclampsia by the 34th week of pregnancy by up to 80%.
Childbirth is the only treatment for preeclampsia. Sometimes a child can be born naturally, but sometimes, if the disease is very acute, an emergency caesarean section is necessary. The best time to have a baby is after the 37th week of pregnancy. Bed rest, medications, and, if necessary, hospitalization can sometimes help bring the condition under control and prolong the pregnancy. Often, a doctor will refer a woman with preeclampsia to the hospital for observation, as the condition of the fetus and pregnant woman may suddenly worsen.
Does bed rest help?
Sometimes bed rest is enough to control mild preeclampsia. In this case, the patient often visits a doctor who measures blood pressure, does blood and urine tests, and monitors the course of the disease.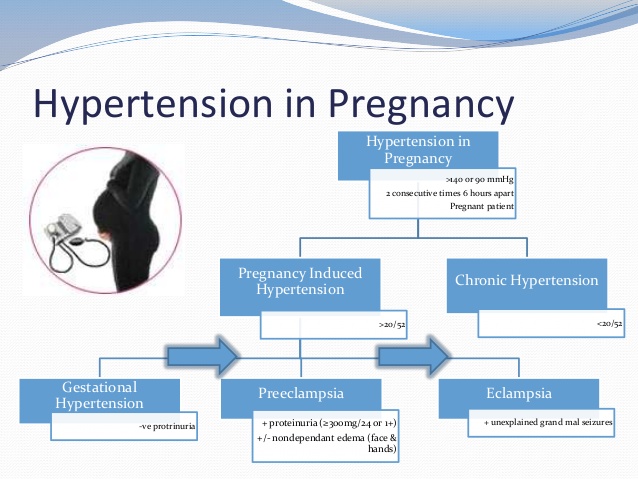 The condition of the fetus is also often examined using a cardiotocogram (CTG) and ultrasound.
The condition of the fetus is also often examined using a cardiotocogram (CTG) and ultrasound.
Are drugs used to treat preeclampsia?
High blood pressure sometimes requires medication. The medications used have few side effects, the drugs prescribed do not have much effect on the fetus, but are very important in the treatment of maternal high blood pressure.
Seizures are a rare but very serious complication of preeclampsia. Magnesium sulfate is sometimes given intravenously to prevent seizures in a pregnant woman with preeclampsia both during and after childbirth. It is safe for the fetus, but the mother may experience side effects such as hot flashes, sweating, thirst, visual disturbances, mild confusion, muscle weakness, and shortness of breath. All these side effects disappear when the drug is discontinued.
Can preeclampsia recur?
Preeclampsia does not necessarily recur in the next pregnancy, but the main risk factor for preeclampsia is the presence of preeclampsia in a previous pregnancy(s).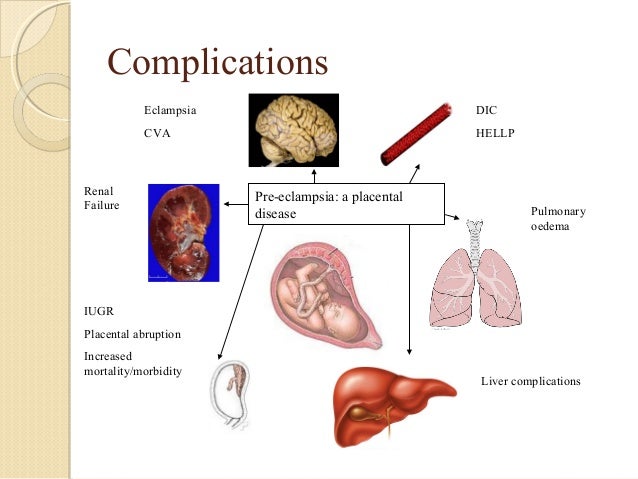 Risk factors for relapse include the severity of the previous case and the woman's overall health during pregnancy. A woman who has previously had preeclampsia should consult a gynecologist during a new pregnancy or when planning a pregnancy.
Risk factors for relapse include the severity of the previous case and the woman's overall health during pregnancy. A woman who has previously had preeclampsia should consult a gynecologist during a new pregnancy or when planning a pregnancy.
ITK1013
The information material was approved by the Health Care Quality Committee of East-Tallinn Central Hospital on 11/30/2022 (Minutes No. 18-22).
Postpartum management of preeclampsia
HEALTH OF WOMAN. 2019.9(145): 8–13; doi 10.15574/HW.2019.145.8
I.V. Lakhno
Kharkiv Medical Academy of Postgraduate Education
Preeclampsia occurs only in humans during the second half of pregnancy and in the postpartum period, is characterized by the development of multiple organ arterial hypertension and leads to multiple organ failure syndrome. It is known that almost a third of cases of eclampsia occurs in the postoperative period. Patients with preeclampsia require careful monitoring of blood pressure and the appointment of antihypertensive drugs after delivery.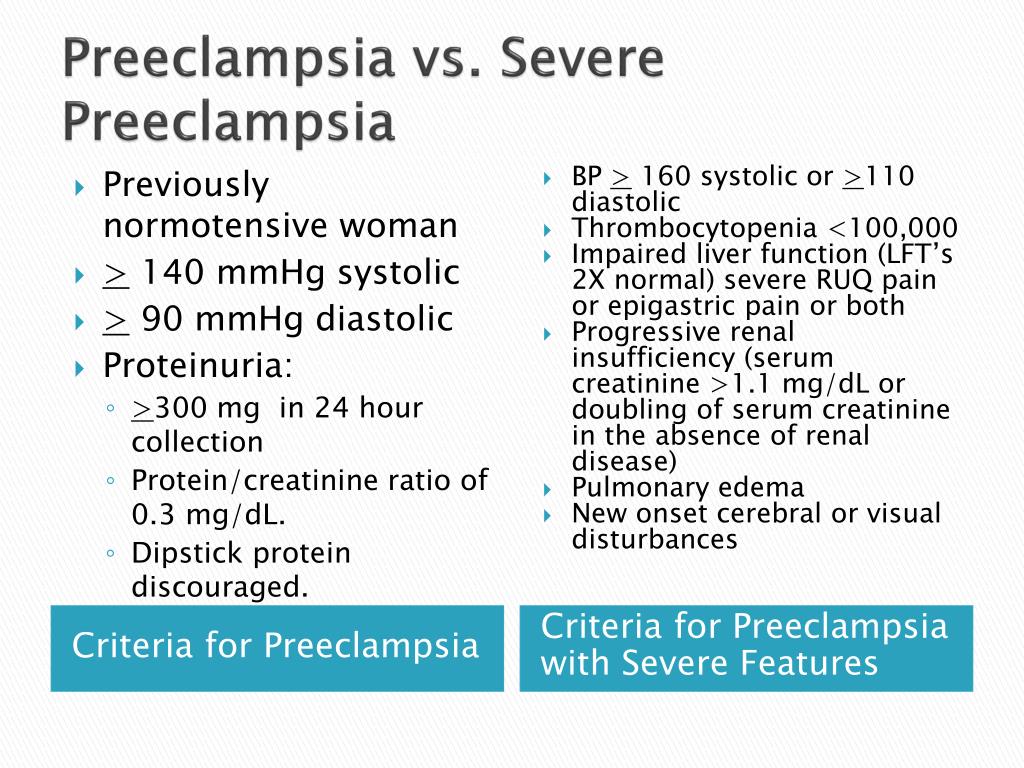
The pathogenesis and tactics of managing women in labor with preeclampsia that arose in de novo puerperia are not well understood. The greatest risk of stroke after childbirth remains within 10 days. During the manifestation of preeclampsia after childbirth, it is very important to start the use of antihypertensive drugs. First-line drugs should be used within 30 to 60 minutes of the diagnosis of severe preeclampsia to prevent cerebral hemorrhage. Labetalol or hydralazine are used to quickly lower blood pressure. Sublingual nifedipine can also be considered first-line therapy. The use of magnesium sulfate is necessary for the prevention of seizures in patients with severe preeclampsia. Against the background of an attack of eclampsia, a solution of magnesium sulfate is started to be administered intravenously at a dose of 4-5 g for 15-20 minutes, and then the infusion administration is continued at a dose of 1 g per hour during the day.
Uterine curettage is also a possible treatment for lowering blood pressure in women with preeclampsia.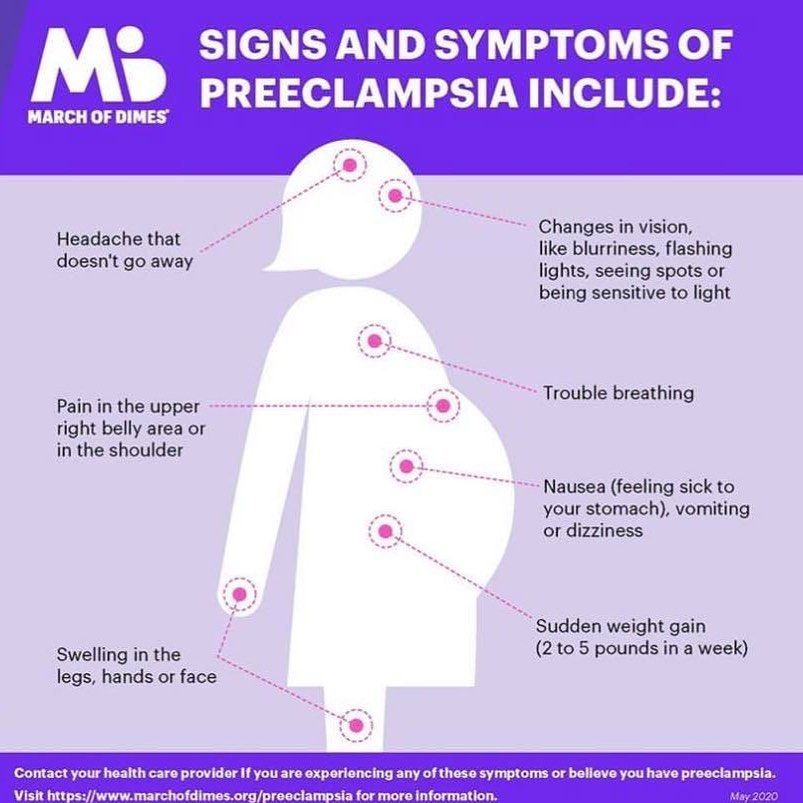 To date, there is not enough data on the safety of its use in terms of the risks associated with anesthesia, possible perforation of the uterus and the spread of infection against the background of endometritis. But curettage should be performed during caesarean section for women with preeclampsia.
To date, there is not enough data on the safety of its use in terms of the risks associated with anesthesia, possible perforation of the uterus and the spread of infection against the background of endometritis. But curettage should be performed during caesarean section for women with preeclampsia.
The article presents its own observation of the systemic inflammatory response syndrome, which arose in a woman with initial mild preeclampsia after childbirth. Postpartum endomyometritis, which was caused by group B streptococcus, was supposed to play a triggering role in the progression of preeclampsia. The problem of polychemoresistance has led to the inability of traditional antimicrobial agents to prevent dissemination of infection after curettage. The systemic inflammatory response syndrome caused an increase in the severity of preeclampsia and the development of multiple organ failure.
Keywords: preeclampsia, postpartum period, antihypertensive drugs.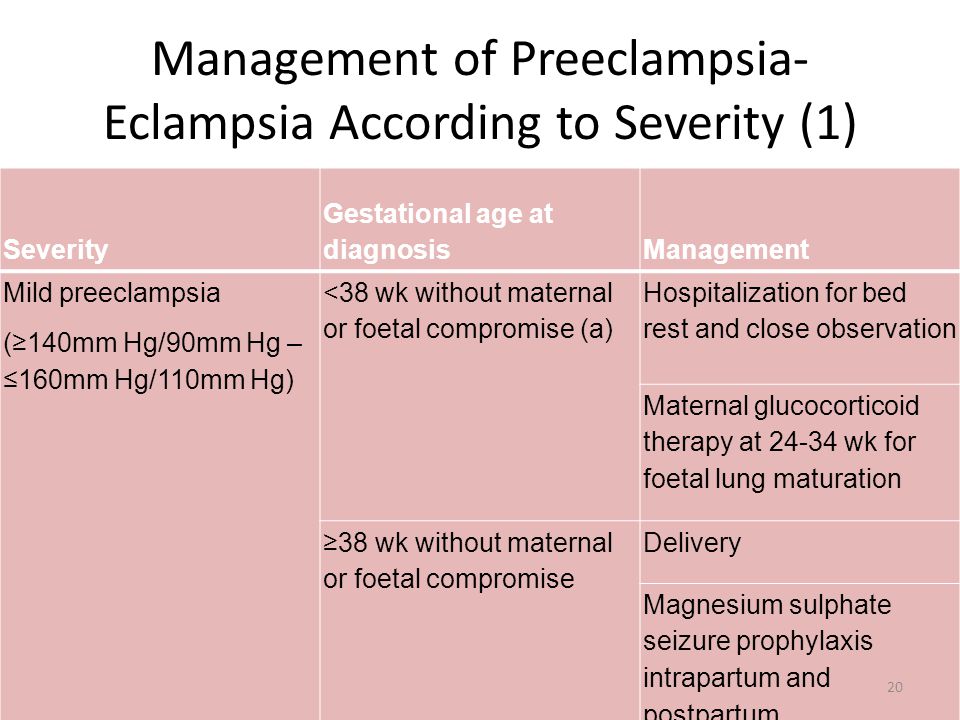
BIBLIOGRAPHY
1. ACOG Committee Opinion No. 767 Summary: Emergent Therapy for Acute-Onset, Severe Hypertension During Pregnancy and the Postpartum Period. Obstet Gynecol. 2019; 133(2):409-412. https://doi.org/10.1097/AOG.0000000000003082; PMid:30681541
2. Al-Safi Z, Imudia AN, Filetti LC, Hobson DT, Bahado-Singh RO, Awonuga AO. Delayed postpartum preeclampsia and eclampsia: demographics, clinical course, and complications. Obstet Gynecol. 2011; 118(5):1102–7. https://doi.org/10.1097/AOG.0b013e318231934c; PMid:21979459
3. American College of Obstetricians and Gynecologists, Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013; 122(5):1122–31.
4. Ann-Charlotte I. Inflammatory mechanisms in preeclampsia. Pregnancy Hypertens. 2013 ;3(2):58. https://doi.org/10.1016/j.preghy.2013.04.005; PMid:26105840
https://doi.org/10.1016/j.preghy.2013.04.005; PMid:26105840
5. Bigelow CA, Pereira GA, Warmsley A, Cohen J, Getrajdman C, Moshier E, Paris J, Bianco A, Factor SH, Stone J. Risk factors for new-onset late postpartum preeclampsia in women without a history of preeclampsia. Am J Obstet Gynecol. 2014; 210(4):338 e1–8. https://doi.org/10.1016/j.ajog.2013.11.004; PMid:24211478
6. Brien ME, Boufaied I, Soglio DD, Rey E, Leduc L, Girard S. Distinct inflammatory profile in preeclampsia and postpartum preeclampsia reveal unique mechanisms. Biol Reprod. 2019;100(1):187-194. https://doi.org/10.1093/biolre/ioy164; PMid:30010720
7. Burgess A, McDowell W, Ebersold S. Association Between Lactation and Postpartum Blood Pressure in Women with Preeclampsia. MCN Am J Matern Child Nurs. 2019;44(2):86-93. https://doi.org/10.1097/NMC.0000000000000502; PMid:30688668
8. Cairns AE, Pealing L, Duffy JMN, et al. Postpartum management of hypertensive disorders of pregnancy: Late postpartum eclampsia. J Obstet Gynaecol. 2012; 32(3):264–6. a systematic review. BMJ Open 2017;7:e018696. https://doi.org/10.1136/bmjopen-2017-018696; PMID:29187414 PMCid:PMC5719299
J Obstet Gynaecol. 2012; 32(3):264–6. a systematic review. BMJ Open 2017;7:e018696. https://doi.org/10.1136/bmjopen-2017-018696; PMID:29187414 PMCid:PMC5719299
9. Clark T.P. Late-onset postpartum preeclampsia: a case study. The nurse practitioner. 2014; 39(7): 34–42. https://doi.org/10.1097/01.NPR.0000443230.18099.e9; PMid:24932793
10. Cohen J, Vaiman D, Sibai BM, Haddad B. Blood pressure changes during the first stage of labor and for the prediction of early postpartum preeclampsia: a prospective study. European journal of obstetrics, gynecology, and reproductive biology. 2015; 184:103-7. https://doi.org/10.1016/j.ejogrb.2014.11.020; PMid:25483991
11. Ditisheim A, Sibai B, Tatevian N. Placental Findings in Postpartum Preeclampsia: A Comparative Retrospective Study. Am J Perinatol. 2019 Jul 2. https://doi.org/10.1055/s-0039-1692716; PMCid:PMC7008975. [Epub ahead of print].
12. Jääskeläinen T, Heinonen S, Hämäläinen E, Pulkki K, Romppanen J, Laivuori H; FINNPEC.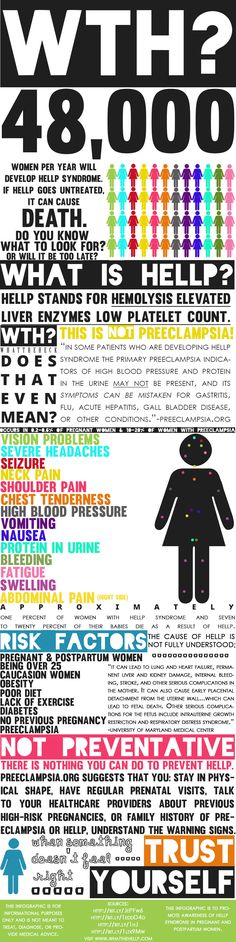 Impact of obesity on angiogenic and inflammatory markers in the Finnish Genetics of Pre-eclampsia Consortium (FINNPEC) cohort. Int J Obes (Lond). 2019;43(5):1070-1081. https://doi.org/10.1038/s41366-018-0217-8; PMid:30254363
Impact of obesity on angiogenic and inflammatory markers in the Finnish Genetics of Pre-eclampsia Consortium (FINNPEC) cohort. Int J Obes (Lond). 2019;43(5):1070-1081. https://doi.org/10.1038/s41366-018-0217-8; PMid:30254363
13. Janzarik WG, Jacob J, Katagis E, Markfeld-Erol F, Sommerlade L, Wuttke M, Reinhard M. Preeclampsia postpartum: Impairment of cerebral autoregulation and reversible cerebral hyperperfusion. Pregnancy Hypertens. 2019;17:121-126. https://doi.org/10.1016/j.preghy.2019.05.019; PMid:31487628
14. Kalafat E, Thilaganathan B. Cardiovascular origins of preeclampsia. Curr Opin Obstet Gynecol. 2017;29(6):383-389. https://doi.org/10.1097/GCO.0000000000000419; PMid:28961633
15. Lakhno IV. Systemic Inflammatory Response Syndrome as a Reason for the Multiple Organ Failure in a Postpartum Pre-eclamptic Patient. J South Asian Feder Obst Gynae 2018;10(3):215-217. https://doi.org/10.5005/jp-journals-10006-1592
16. Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol. 2004; 190(5):1464–6. https://doi.org/10.1016/j.ajog.2004.02.037; PMid:15167870
Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol. 2004; 190(5):1464–6. https://doi.org/10.1016/j.ajog.2004.02.037; PMid:15167870
17. Mc Lean G, Reyes O, Velarde R. Effects of postpartum uterine curettage in the recovery from Preeclampsia/Eclampsia. A randomized, controlled trial. Pregnancy Hypertens. 2017;10:64-69. https://doi.org/10.1016/j.preghy.2017.06.001; PMid:29153692
18. Odigboegwu O, Pan LJ, Chatterjee P. Use of Antihypertensive Drugs During Preeclampsia. Front Cardiovasc Med. 2018;5:50. https://doi.org/10.3389/fcvm.2018.00050; PMID:29896480 PMCid:PMC5987086
19. Skurnik G, Hurwitz S, McElrath TF, Tsen LC, Duey S, Saxena AR, Karumanchi A, Rich-Edwards JW, Seely EW. Labor therapeutics and BMI as risk factors for postpartum preeclampsia: A case-control study. Pregnancy Hypertens. 2017;10:177-181. https://doi.org/10.1016/j.preghy.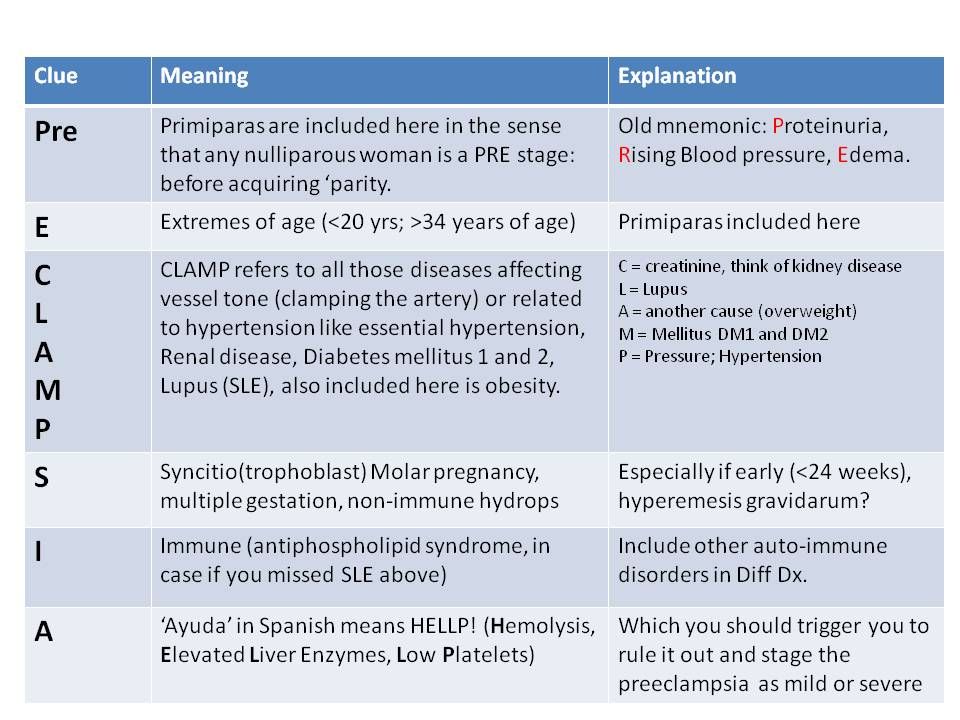 2017.07.142; PMid:29153674 PMCid:PMC5747249
2017.07.142; PMid:29153674 PMCid:PMC5747249
20. Smith GN, Pudwell J, Saade GR. Impact of the New American Hypertension Guidelines on the Prevalence of Postpartum Hypertension. Am J Perinatol. 2019;36(4):440-442. https://doi.org/10.1055/s-0038-1669441; PMid:30170330
21. Takaoka S, Ishii K, Taguchi T, Kakubari R, Muto H, Mabuchi A, Yamamoto R, Hayashi S, Mitsuda N. Clinical features and antenatal risk factors for postpartum-onset hypertensive disorders. Hypertens Pregnancy. 2016:1–10. https://doi.org/10.3109/10641955.2015.1100308; PMid:26828093
22. Too G, Wen T, Boehme AK, Miller EC, Leffert LR, Attenello FJ, Mack WJ, DʼAlton ME, Friedman AM. Timing and Risk Factors of Postpartum Stroke. Obstet Gynecol. 2018;131(1):70-78. https://doi.org/10.1097/AOG.0000000000002372; PMID:29215510 PMCid:PMC6402829
23. Verhaegen J, Peeters F, Debois P, Jacquemyn Y. Posterior reversible encephalopathy syndrome as a complication of pre-eclampsia in the early postpartum period.