How to prevent blighted ovum
Blighted Ovum: Symptoms, Causes, and Prevention
When you’re grieving a pregnancy loss, it’s natural to have a lot of questions. Learn what a blighted ovum is, plus get tips for treatment and healing.
Miscarriage is a sensitive topic. One that many people, for a variety of reasons, do not feel comfortable talking about, even though approximately 25 percent of all pregnancies end in miscarriage. And of those miscarriages, 75 percent occur in the first trimester. There are many types of early miscarriage, and a blighted ovum is just one of them.
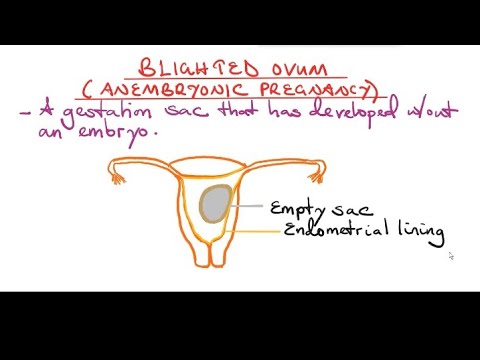
What is a Blighted Ovum?
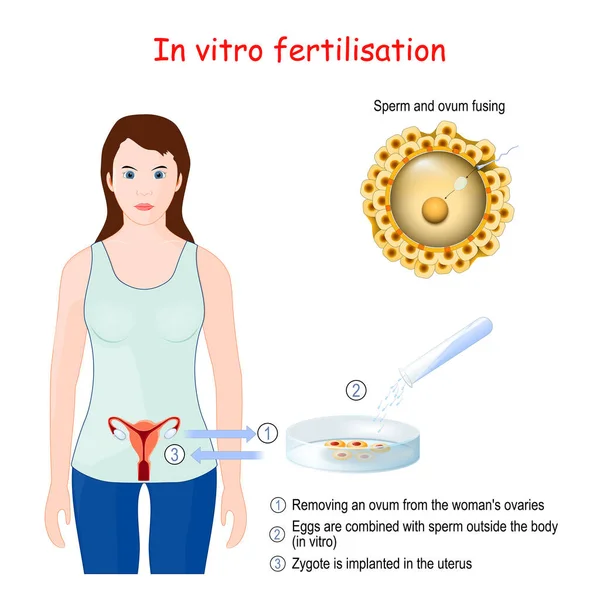
A blighted ovum, also called anembryonic (no embryo) pregnancy or anembryonic gestation, occurs when a fertilized egg stops developing or is reabsorbed during early pregnancy.
Blighted ovum is the most common cause of early miscarriage, occurring in 50 percent of first trimester miscarriages, and usually happens between weeks 8 and 13. It can also happen in the first few weeks of pregnancy before a woman experiences a missed period. (source)
What Causes a Blighted Ovum?
The causes of blighted ovum are generally unknown, but experts believe most cases are due to chromosomal abnormalities in the embryo. (source) Research shows that age and genetic susceptibility may also play a role in early pregnancy miscarriages.
Studies show this particular gene polymorphism could also be the cause if you have repeated blighted ovums.
Though it doesn’t make pregnancy loss any easier, it’s important to know there is nothing you can do to prevent a blighted ovum.
If you have two or more early stage miscarriages you should speak to your doctor about performing tests to rule out any underlying causes. (source)
Blighted Ovum hCG Levels
Though some women may have a blighted ovum miscarriage before they even realized they were pregnant, other women experience early signs of pregnancy. This happens when the fertilized egg causes the body to begin producing human chorionic gonadotropin (hCG).
This happens when the fertilized egg causes the body to begin producing human chorionic gonadotropin (hCG).
Even after the embryo has stopped developing, your body many still produce hCG for a short time.
Since hCG is the hormone detected in at-home pregnancy tests, it is possible to get a positive pregnancy test with a blighted ovum—even after the embryo has stopped developing.
Despite these signs of pregnancy and even a positive pregnancy test, an ultrasound will show an empty gestational sac or a lack of heartbeat. (source)
How is a Blighted Ovum Diagnosed?
Blighted ovums are generally diagnosed during the first ultrasound when there is no embryo and/or no heartbeat. It is almost impossible to diagnose an early blighted ovum without a trip to the doctor for an ultrasound.
Since a blighted ovum can occur so early in pregnancy that a woman thinks the miscarriage is simply the arrival of her period, some blighted ovums go undiagnosed.

If not diagnosed by an ultrasound, you may suspect a blighted ovum if early pregnancy signs subside or if you experience heavier than normal bleeding. Call your doctor or midwife with any concerns.
Can the Diagnosis Be Wrong?
It is possible that the date of conception could be wrong. If you conceived later than you originally thought, it is possible, although unusual, that an ultrasound was simply too early to see any fetal development. According to Dr. Judith Reichman, many doctors and midwives will not make a final diagnosis of a blighted ovum until hormone levels are checked and a second ultrasound is performed a week later to check if the sac remains empty.
There is a small (about 1 in 250 or 0.4%) chance that a tubal or ectopic pregnancy may be misdiagnosed as a blighted ovum. (source) Ectopic pregnancy is not viable and is a very serious condition that requires medical treatment. A follow-up ultrasound a few weeks after a diagnosis of a blighted ovum, especially if a natural passing of the baby has not occurred, is important to rule out ectopic or tubal pregnancy.
Treatment for Blighted Ovum
Expectant management
Expectant Management is simply letting nature take its course. This treatment plan, which essentially waits for the body to naturally miscarry, is for women who are at 13 weeks or earlier in pregnancy.
Research suggests that 80 percent of women can have a natural miscarriage without complications.
There are several natural remedies to support this process:
- Castor Oil Packs: A piece of cloth soaked in castor oil applied topically (externally) to the pelvic area where the uterus is located can help ease cramps. Though research is fairly limited, there are some studies that suggest ingesting castor oil is an effective way to stimulate labor.
- Red Light Therapy: Red light therapy, or low-level laser therapy (LLLT), is a non-invasive treatment that employs low energy lasers or light emitting diodes (LEDs). (source) Exposure to this form of light has been shown to improve skin conditions and some research suggests it can even promote healing and provide pain relief.
 (source) It is a non-invasive, safe, and relatively budget-friendly option available at some spas and dermatology offices.
(source) It is a non-invasive, safe, and relatively budget-friendly option available at some spas and dermatology offices. - Rest: This may sound simple, but one of the most important things you can do for your body when it has experienced trauma is to rest. Even if you are not feeling a lot of pain, your body is healing and you may also be dealing with emotional trauma as well. It’s ok to take a step back from commitments and even take a few days off from work to support the healing process.
What If I Don’t Want to or Can’t Miscarry Naturally?
After 10 weeks gestation, the chance of incomplete miscarriage (and resulting infection) goes up, but you may still be able to pass the tissue on your own. Some women may feel a medically assisted miscarriage is safe or will help provide closure. Always consult with your healthcare provider about what’s right for you. (source)
When Is a D&C Necessary?
If the bleeding and cramping last longer than 2 weeks, you may need to consider medical help, like prescription misoprostol (similar to what they use for induction) to avoid infection or hemorrhage.
A more invasive option is a D&C. This is a surgical procedure to remove conception tissue after a pregnancy loss. Although sometimes medically necessary, there are risks associated with a D&C, which is why they are not recommended in early miscarriages. Studies suggest risks include:
- Hemorrhage or heavy bleeding
- Infection in the uterus or other pelvic organs
- Perforation or puncture to the uterus
- Laceration or weakening of the cervix
- Scarring of the uterus or cervix, which may require further treatment
- Incomplete procedure that requires another procedure to be performed
You can read more about D&Cs in this post.
Is There Anything I Can Do to Prevent a Blighted Ovum?
The short answer is no. Blighted Ovum is generally believed to be due to chromosomal abnormalities that are not due to underlying health issues.
However, you could focus on improving your egg quality (and your partner’s sperm quality) by making these lifestyle changes:
- Go organic.
 Pesticides and healthy sperm don’t mix. In one study men who ate more than 1.5 servings of fruits and vegetables with pesticides residue had 49 percent lower sperm count and 32 percent lower percentage of normal sperm than men who ate less than 0.5 serving per day. They also had a lower sperm counts, lower ejaculate volumes, and lower percentages of normal sperm.
Pesticides and healthy sperm don’t mix. In one study men who ate more than 1.5 servings of fruits and vegetables with pesticides residue had 49 percent lower sperm count and 32 percent lower percentage of normal sperm than men who ate less than 0.5 serving per day. They also had a lower sperm counts, lower ejaculate volumes, and lower percentages of normal sperm. - Be sure to eat a well-balanced and high-variety diet. Get all of your macro and micronutrients in each day. Or consider taking a prenatal now as extra insurance.
- Try strategic supplementation. In studies, DHEA and CoQ10 improved egg quality and/or pregnancy outcome. Good food sources include: yam, soy, eggs, and salmon.
- Reduce stress. In one study, women with high stress levels were 12 percent less likely to conceive than counterparts with lower stress levels.
- Get enough sleep: There are a number of studies that suggest there may be a correlation between sleep disturbances and reproductive health.
 In one study, women with diminished ovarian reserve were found to be 30 times more likely to have disturbed sleep.
In one study, women with diminished ovarian reserve were found to be 30 times more likely to have disturbed sleep. - Do moderate exercises. Research suggests fertility rates are slightly higher in women who engage in moderate activities—walking or yoga, for example—for any length of time.
Healing After a Blighted Ovum
Any miscarriage, even in the first few weeks of pregnancy, is a loss. If you are reading this article because you have personally experienced this, I am so sorry for your loss. Despite the early gestational age, it is natural to grieve the loss of your baby. I know I did.
If you are struggling with the feelings of loss after an early miscarriage, talk to someone about it. It can be your partner, a friend, a family member, or a mental health professional. You do not have to deal with the grief of a miscarriage on your own. (Click here for more suggestions.)
Trying Again
As long as you feel emotionally and physically ready, there is no reason to wait. You can begin trying to conceive again the first cycle after a miscarriage due to a blighted ovum. (Source)
You can begin trying to conceive again the first cycle after a miscarriage due to a blighted ovum. (Source)
Most women who experience a blighted ovum go on to have later successful pregnancies. In fact, a subsequent pregnancy after experiencing a blighted ovum is no more likely to result in a miscarriage than any other normal pregnancy. (source)
If you run into trouble conceiving, you may want to check out this post for ways to increase your fertility and, of course, always work with your healthcare provider.
How About You?
If you feel comfortable, please help us support each other and share your experiences below.
Treatment, Symptoms, Causes, and Outlook
Blighted Ovum: Treatment, Symptoms, Causes, and Outlook- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Debra Rose Wilson, Ph. D., MSN, R.N., IBCLC, AHN-BC, CHT — By Corey Whelan on December 13, 2017
D., MSN, R.N., IBCLC, AHN-BC, CHT — By Corey Whelan on December 13, 2017
What is a blighted ovum?
A blighted ovum is a fertilized egg that implants itself in the uterus but doesn’t become an embryo. The placenta and embryonic sac form, but remain empty. There’s no growing baby. It’s also known as anembryonic gestation or anembryonic pregnancy.
Even though there’s no embryo, the placenta still produces human chorionic gonadotropin (hCG). This is a hormone designed to support pregnancy. Blood and urine pregnancy tests look for hCG, so blighted ovum can result in a positive pregnancy test even though the pregnancy isn’t actually proceeding. Pregnancy-related symptoms, such as sore breasts and nausea, may also occur.
A blighted ovum eventually leads to miscarriage. It’s not able to turn into a viable pregnancy.
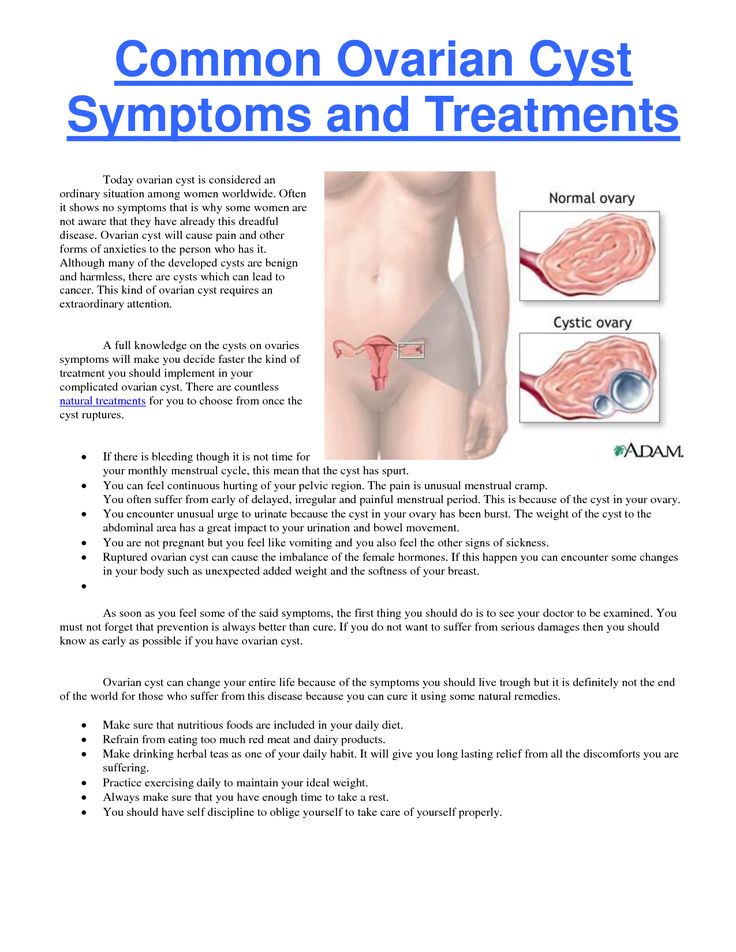
What are the symptoms?
A blighted ovum sometimes ends before you realize you’re pregnant. When this happens, you may just think you’re having a heavier-than-normal menstrual period.
A blighted ovum may have the same symptoms associated with pregnancy, such as:
- a positive pregnancy test
- sore breasts
- a missed period
As the pregnancy ends, symptoms may include those of miscarriage. These can include:
- vaginal spotting or bleeding
- abdominal cramping
- disappearance of breast soreness
Pregnancy tests measure hCG levels, so a blighted ovum can continue to result in positive test results before the tissues are passed.
What are the causes?
This condition isn’t caused by anything that you did or didn’t do, either during or before your pregnancy.
The exact cause of blighted ovum isn’t known. It’s thought to be caused by chromosomal abnormalities occurring within the fertilized egg. This may be the result of genetics, or of poor-quality eggs or sperm.
Blighted ovum may be linked to abnormalities within chromosome 9. If you have repeated blighted ovum pregnancies, consider talking to your doctor about a chromosomal analysis of your embryos.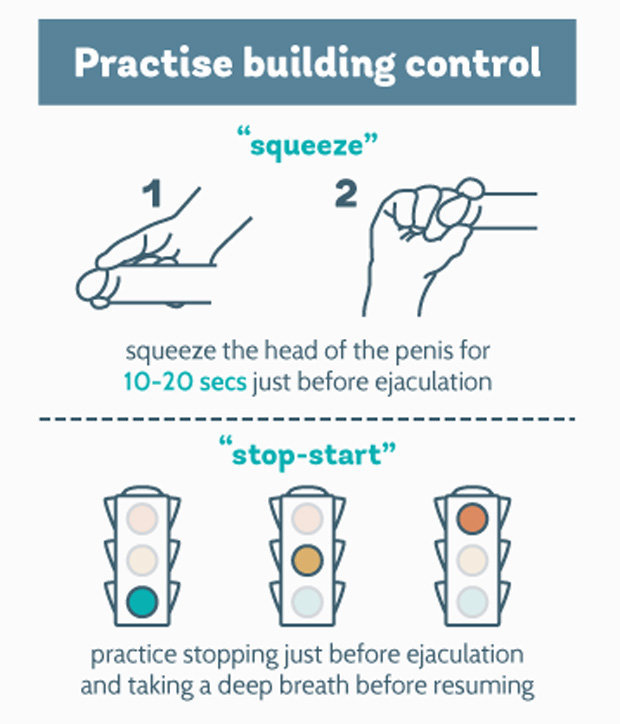
You may be at a significantly higher risk of blighted ovum than the general population if your partner is biologically related to you.
A blighted ovum can occur so early that it goes unrecognized. However, many women who receive a diagnosis of this condition go on to have subsequent healthy pregnancies. It’s not clear if blighted ovum occurs most typically in first-time pregnancies or if they sometimes occur more than once. Most women who have a blighted ovum do go on to have successful pregnancies and healthy babies.
How is this diagnosed?
A blighted ovum is often discovered on the first ultrasound given during a prenatal appointment. The sonogram will show the placenta and empty embryonic sac. A blighted ovum usually occurs between the 8th and 13th weeks of pregnancy.
What are the treatment options?
If blighted ovum is discovered during a prenatal appointment, your doctor will discuss treatment options with you. These may include:
- waiting for miscarriage symptoms to occur naturally
- taking medication, such as misoprostol (Cytotec), to bring on a miscarriage
- having a D and C (dilation and curettage) surgical procedure to remove the placental tissues from the uterus
The length of your pregnancy, medical history, and emotional state will all be taken into account when you and your doctor are deciding upon a treatment option. You’ll want to discuss the side effects and the standard risks associated with any type of medication or surgical procedure, including a D and C.
You’ll want to discuss the side effects and the standard risks associated with any type of medication or surgical procedure, including a D and C.
Even though there wasn’t a baby, there has been a loss of a pregnancy. Miscarriages can be emotionally difficult, and waiting for the pregnancy to end can take longer than anticipated. For this reason, some women decide to terminate surgically or with medication. Other women are uncomfortable with these choices and prefer to let the miscarriage happen on its own.
Discuss all of your options with your doctor. Let them know if you’re uncomfortable with any of the options available to you.
Can this be prevented?
A blighted ovum can’t be prevented.
If you’re concerned about this condition, talk to your doctor about possible genetic causes and testing procedures, which might help you avoid it. Also discuss with your doctor about exposure to toxins in the environment. It may be linked to blighted ovum and miscarriage.
Are there any complications with future pregnancies?
Just as with any miscarriage, your body and emotional well-being need time to heal. It’s important to remember that most women who go through a blighted ovum go on to have successful pregnancies.
You and your doctor will discuss how long you should wait before trying to conceive again. It’s typically recommended that you wait three full menstrual cycles so that your body has time to recuperate fully and is ready to support pregnancy. During this time, focus on healthy lifestyle habits for your body and mental health, such as:
- eating well
- keeping stress at bay
- exercising
- taking a daily prenatal supplement that contains folate
Having a blighted ovum once doesn’t mean you’re destined to have another one. However, there are factors associated with this type of miscarriage that you should discuss with your doctor. These factors include genetics, egg quality, and sperm quality. Your doctor may recommend testing for these types of conditions. Tests may include:
Your doctor may recommend testing for these types of conditions. Tests may include:
- preimplantation genetic screening (PGS), a genetic analysis of embryos that can be done prior to implantation into the uterus
- semen analysis, which is used to determine sperm quality
- follicle stimulating hormone (FSH) or anti-mullerian hormone (AMH) tests, which can be used to help improve egg quality
The takeaway
The specific cause of blighted ovum is unknown, but chromosomal anomalies appear to be a main factor. Having a blighted ovum doesn’t mean you’ll have another one. Most women who experience this go on to have healthy pregnancies.
Last medically reviewed on December 13, 2017
- Parenthood
- Pregnancy
- Pregnancy Health
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Baghbani F, et al. (2014). Association of heteromorphism of chromosome 9 and recurrent abortion (ultrasound diagnosed blighted ovum): A case report.
ncbi.nlm.nih.gov/pmc/articles/PMC4094662/ - Balanced translocations. (2014).
rarechromo.org/information/Other/Balanced%20translocations%20FTNP.pdf - Blighted ovum. (2016).
pregnancybirthbaby.org.au/blighted-ovum - de La Rochebrochard E, et al. (2002). Paternal age and maternal age are risk factors for miscarriage; results of a muticentre European study. DOI:
10.1093/humrep/17.6.1649 - Overcoming a ‘pseudo pregnancy’: Blighted ovums can cause miscarriage. (n.d.).
doctorsthatdo.org/overcoming-a-pseudo-pregnancy - Shekoohi S, et al. (2013). Chromosomal study of couples with a history of recurrent spontaneous abortions with diagnosed blighted ovum.
ncbi.nlm.nih.gov/pmc/articles/PMC3927383/ - Tobah YB. (2016). What causes a blighted ovum? What symptoms can I expect?
mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/expert-answers/blighted-ovum/faq-20057783 - When is the best time for pregnancy after miscarriage? (2016).
mayoclinic.org/healthy-lifestyle/getting-pregnant/in-depth/pregnancy-after-miscarriage/art-20044134?pg=2
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Dec 13, 2017
Written By
Corey Whelan
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Share this article
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Corey Whelan on December 13, 2017
related stories
How Long Does a Miscarriage Last?
How to Tell if You’re Having a Miscarriage Without Bleeding
What I’ve Learned from Counseling Couples Through Miscarriage
7 Causes for a False-Positive Pregnancy Test
What’s a Chemical Pregnancy?
Read this next
How Long Does a Miscarriage Last?
Medically reviewed by Holly Ernst, PA-C
The loss of a pregnancy before 20 weeks is considered a miscarriage.
 The length of time a miscarriage lasts varies from woman to woman, as do the risk…
The length of time a miscarriage lasts varies from woman to woman, as do the risk…READ MORE
How to Tell if You’re Having a Miscarriage Without Bleeding
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
A miscarriage is also known as a pregnancy loss. These are the symptoms, causes, and a look at how to move forward.
READ MORE
What I’ve Learned from Counseling Couples Through Miscarriage
Most women tell me it doesn’t get better, but it does get easier.
READ MORE
7 Causes for a False-Positive Pregnancy Test
Reputable home pregnancy tests can be accurate, but they aren’t foolproof and can cause confusion. Here are 7 reasons you may receive a false-positive…
READ MORE
What’s a Chemical Pregnancy?
Medically reviewed by Debra Rose Wilson, Ph.
 D., MSN, R.N., IBCLC, AHN-BC, CHT
D., MSN, R.N., IBCLC, AHN-BC, CHTA chemical pregnancy is an early pregnancy loss that occurs shortly after implantation. Chemical pregnancies may account for 50 to 75 percent of all…
READ MORE
Orgasm During Pregnancy: Why It’s Fine (and How It’s Different)
If you're wondering if a pregnant orgasm feels different, here's why.
READ MORE
Joy Is Our Birthright: Striving for Black Maternal Health Equity
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Black Maternal Health Week was created to reduce disparities Black women and birthing people face today. Here are 5 solutions that can help.
READ MORE
Anemia in Pregnancy: What It Is and How to Prevent It
Anemia is common during pregnancy. Here’s how to prevent and treat anemia in pregnancy with healthy foods, supplements, and more.
READ MORE
How to Support Black Mothers and Parents with Postpartum Depression
Medically reviewed by Mia Armstrong, MD
Due to medical and social biases, Black mothers are more likely to experience postpartum depression than any other group. Let's look at why and how to…
READ MORE
The Best Gift for New Dads Just in Time for Father's Day
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
It's not usually dad who is showered with gifts when a new baby comes, but why not? He deserves appreciation too! Here are our picks of the best new…
READ MORE
Freezing of eggs (oocytes), cryopreservation, cost
Frozen young eggs can be stored for decades without being subjected to aging and harmful effects along with the whole body. They will not lose quality and will not disappear. This will be a "golden reserve" that will allow a woman to quietly make a career, meet a man, start a family and give birth to a child at the most convenient time for this closer to 40 and even after 50 (although in the latter case, you may have to resort to surrogate mother service). Frozen eggs will also be a safety net in case of early menopause or a disease that can adversely affect reproductive function.
They will not lose quality and will not disappear. This will be a "golden reserve" that will allow a woman to quietly make a career, meet a man, start a family and give birth to a child at the most convenient time for this closer to 40 and even after 50 (although in the latter case, you may have to resort to surrogate mother service). Frozen eggs will also be a safety net in case of early menopause or a disease that can adversely affect reproductive function.
Natural egg reserve or ovarian reserve is an individual indicator for each woman. It is genetically determined and is laid in the womb. With each year of life, the number of eggs decreases. This process cannot be stopped, and the losses cannot be replenished.
Digits:
by the 20th week of pregnancy, the number of follicles in a female fetus is about 6-7 million,
by the time of birth - about 1-1.5 million,
by the period of menarche (first menstruation) - about 300 thousand,
after 37 years - about 25 thousand,
by the beginning of menopause - about 1 thousand.
Menopause usually occurs closer to 50-55 years, but maybe earlier - up to 40 years.
During the entire reproductive period of a woman's life, mature eggs are formed from only 400-500 follicles. The remaining primary follicles die. This process is called follicular atresia.
Bad habits (smoking, drug use, alcohol), stress, unhealthy diet, poor environment, as well as hormonal disorders, certain types of surgical interventions, and heredity contribute to a decrease in the number and quality of eggs.
In women after 35 years, even a regular menstrual cycle does not guarantee the possibility of conceiving a child. The follicle may mature, but the egg may not be in it - this phenomenon is called "empty follicle syndrome". As women age, the risk of fetal malformations and genetic syndromes increases.Frequency of chromosomal abnormalities in women of different age groups:
20-25 years is 1:1300,
30 years is 1:750,
35 years is 1:300.
40 years is 1:80,
45 years is 1:5.Birth rate of babies with Down syndrome:
25 years - 1 in 1250 births,
35 years - 1 case per 400 births,
older than 40 years - 1 case per 30 births.
If a woman at 45 looks 30, but feels 25, leads an active and RIGHT lifestyle, then this still does not affect the quality and quantity of eggs - they age with the body, which increases the risks of late motherhood.
Therefore, if you are not in a hurry with the birth of a child, then hurry up to evaluate your ovarian reserve and, if indicated, use the cryopreservation service.
Start with a visit to a reproductive specialist - this should be done before the age of 34.
Your specialist will assess your ovarian reserve.
1) will conduct an ultrasound. The method allows you to determine the size of the ovaries and the state of blood flow, count the number of antral follicles (their size is up to 8 mm).
2) prescribe laboratory tests:
- for FSH (follicle-stimulating hormone)
- on AMH (anti-mullerian hormone).
An AMH between 5 and 10 is an indicator that the egg supply is good.
AMH less than one indicates that the ovarian reserve is practically depleted.
Based on the results, the doctor will make a prognosis for the onset of menopause. If the ovarian reserve is low, and pregnancy is planned only after a few years, then there are indications for cryopreservation of eggs.
To obtain eggs, the ovaries are stimulated with hormonal preparations. At the same time, several follicles mature in one cycle and from 10 to 20 eggs can be obtained. Follicle growth is monitored by ultrasound. Typically, mild (sparing) stimulation of ovulation with small doses of hormonal drugs is used. This reduces the risk of side effects.
The accumulation of eggs can be produced in a natural cycle, but they will be much less than in the case of cycles with stimulation.And the fewer eggs, the less chance of IVF success - after all, there will also be few embryos.
Before the procedure for obtaining eggs for cryopreservation, a woman undergoes an examination, the purpose of which is to identify and correct conditions that may adversely affect the quality of the eggs. Based on the diagnostic results, the doctor develops an individual stimulation scheme. The examination includes tests, incl. for urogenital infections, hormones, as well as ultrasound of the pelvic organs, mammary glands. The list of studies can be expanded taking into account individual indications.
The egg retrieval procedure (puncture) is carried out under ultrasound guidance. With the help of special equipment, the follicular fluid containing the eggs is aspirated. Then they go to the embryological laboratory, where they are evaluated, prepared for freezing and directly frozen.
In clinics "Genome" the technology of ultrafast freezing - vitrification is applied.At the same time, ice crystals do not have time to form, so the cell is practically not injured. Frozen eggs are stored in liquid nitrogen at a temperature of minus 196°C. At the same time, their quality and all genetic information is intact. Thawed eggs are fertilized with the same frequency as "fresh".
For your information. At the age of 40, the probability of conception with the help of young frozen eggs is 50%, with your own fresh egg - about 15%.
Numbers that speak for themselves
Probability of pregnancy within 1 year of regular sexual activity in women of different age groups:
up to 25 years - 85%
25-35 years old - about 45%;
after 35 years - 25%;
after 40 - about 10%.
Vitrified donor egg
Achievements of modern medicine have made it possible to use for IVF not only native (untreated) germ cells, but also cryopreserved ones. Vitrification is the most progressive and highly effective way of freezing biological material. It is she who is preferred to be used for cryopreservation of donor eggs all over the world, including in ICLINIC. After all, this technology allows for a long time to keep germ cells outside the body of a woman without losing their quality and ability to fertilize.
What is a vitrified donor egg?
Vitrification is a special high-tech method of ultra-fast deep cryopreservation (freezing) of living cells at -196°C using liquid nitrogen. At the same time, their cytoplasm almost instantly passes into a glassy state, bypassing the crystallization phase. This is precisely the key advantage of the technique over the earlier method of slow controlled freezing. Attempts to cryopreserve germ cells and embryos have been made since the 1940s. The technique was gradually improved, but for a long time it was not possible to achieve sufficient survival of eggs sensitive to external influences. From 19In 1998–1999, reports of successful vitrifications began to appear, but they were sporadic. In 2000, the Japanese professor Masashige Kuwayama (M.Kuwayama) announced the method of vitrification developed by him on cryotopes. He also created the world's first donor egg bank. Subsequently, the method was improved and began to be actively used in world reproduction. Thanks to vitrification, it was possible to achieve a very high survival rate of oocytes after freezing, which made it possible to create banks of donor eggs. The same technology has become the basis for delayed motherhood, when women decide to cryopreserve their own oocytes at an increased risk of early loss of fertility.
When you need donor eggs
On the territory of the Russian Federation, the procedure for cryopreservation (including vitrification) of eggs is regulated by the current order of the Ministry of Health of the Russian Federation No. 107n dated August 30, 2012. Indications for the use of donor oocytes include:
- Loss of fertility in a woman. This may be due to premature ovarian failure (genetically determined or caused by the use of hormonal drugs), surgical, radiation or chemical castration of a woman.
- The patient has severe genetic diseases with a high risk of inheritance.
- Poor quality of own eggs, which leads to repeated failures in IVF/ICSI cycles. Conducting protocols with vitrified donor eggs (oocytes) significantly expands the possibilities of treating infertility with a pronounced female factor.
How vitrified oocytes are obtained
Vitrified oocytes require special equipment to obtain and store vitrified eggs. The process of such cryopreservation includes:
- Collection of mature oocytes by transvaginal puncture of ovarian follicles. Donor eggs are obtained after drug stimulation of the ovaries for the maturation of several follicles and eggs.
- Isolation of an oocyte from aspirated fluid and its purification from accompanying oocyte-cumulus complexes. They include cells of the radiant crown (corona radiata) and follicular oviferous tubercle (cumulus oophorus). For this, washing and enzymatic processing methods are used. At the same stage, the degree of maturity and the prospects of the obtained donor eggs are visually assessed.
- Placement of oocytes in a special cryoprotective solution. This prevents the destruction of cell membranes and makes the process of subsequent rapid freezing uniform.
- Instant immersion of prepared donor eggs in nitrogen, the temperature of which is maintained at -196°C. The rate of freezing occurring in this case is -180°C/min.
- Storage of vitrified eggs in liquid nitrogen by placing them in Dewars. A stable environment is automatically maintained in cryocontainers, which ensures a predictable result of cryopreservation.
Donor eggs can be vitrified only after the written consent of the donor woman for their processing, storage and further anonymous use in various reproductive protocols. This is discussed in the Agreement drawn up in advance.
What are the benefits of vitrified oocytes
- Vitrified oocytes have an average survival rate of 90-99%. Whereas, when using classical slow freezing, no more than 55–60% of oocytes are suitable for further use.
- The effectiveness of IVF with vitrified eggs is comparable to the efficiency of protocols with native material. This has been proven by numerous clinical studies.
- Using the IVF protocol with vitrified donor eggs avoids the need to synchronize the cycles of the donor and the recipient woman. And this reduces the hormonal load on the body of the expectant mother and makes it possible to choose the appropriate cycle for embryo transfer.
- The shelf life of vitrified oocytes is practically unlimited.
- The possibility of transporting vitrified eggs from the cryobank to other clinics (in special cryocontainers, subject to the necessary conditions). This expands the possibilities of using donor programs.
In addition, vitrification is not only planned. With the consent of the woman, emergency cryopreservation of oocytes is possible if the current IVF protocol failed to obtain sperm for fertilization in a timely manner, as well as for patients with cancer before chemotherapy or radiation therapy.
Vitrification – a progressive but not universally used method
Vitrification of oocytes requires the clinic to have special expensive modern equipment, an organized cryobank and a qualified embryologist with the appropriate certificate and work experience. Therefore, not all IVF centers can provide such a service to their patients. The ICLINIC Reproductive Medicine Clinic has its own regularly replenished donor bank. Moreover, it is possible to carry out IVF/ICSI with both native and vitrified eggs. The appropriateness of using different protocols is determined by the doctor, taking into account the specific clinical situation.