Cold and flu pregnant
Pregnancy and the flu: MedlinePlus Medical Encyclopedia
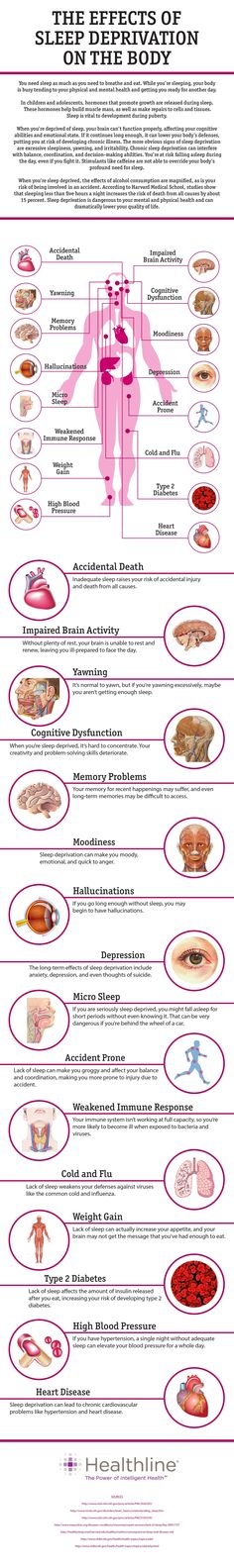
During pregnancy, it is harder for a woman's immune system to fight infections. This makes a pregnant woman more likely to get the flu and other diseases.
Pregnant women are more likely than nonpregnant women their age to become very ill if they get the flu. If you are pregnant, you need to take special steps to stay healthy during the flu season.
This article gives you information about the flu and pregnancy. It is not a substitute for medical advice from your health care provider. If you think you have the flu, you should contact your provider's office right away.
WHAT ARE THE SYMPTOMS OF FLU DURING PREGNANCY?
Flu symptoms are the same for everyone and include:
- Cough
- Sore throat
- Runny nose
- Fever of 100°F (37.8°C) or higher
Other symptoms may include:
- Body aches
- Headache
- Fatigue
- Vomiting, and diarrhea
SHOULD I GET THE FLU VACCINE IF I AM PREGNANT?
If you are pregnant or thinking about becoming pregnant, you should get the flu vaccine. The Centers for Disease Control and Prevention (CDC) considers pregnant women at a higher risk for getting the flu and developing flu-related complications.
Pregnant women who get the flu vaccine get sick less often. Getting a mild case of the flu is often not harmful. However, the flu vaccine can prevent the severe cases of the flu that can harm mother and baby.
Flu vaccines are available at most provider offices and health clinics. There are two types of flu vaccines: the flu shot and a nose-spray vaccine.
- The flu shot is recommended for pregnant women. It contains killed (inactive) viruses. You cannot get the flu from this vaccine.
- The nasal spray-type flu vaccine is not approved for pregnant women.
It is OK for a pregnant woman to be around somebody who has received the nasal flu vaccine.
WILL THE VACCINE HARM MY BABY?
A small amount of mercury (called thimerosal) is a common preservative in multidose vaccines. Despite some concerns, vaccines that contain this substance have NOT been shown to cause autism or attention deficit hyperactivity disorder.
If you have concerns about mercury, ask your provider about a preservative-free vaccine. All routine vaccines are also available without added thimerosal. The CDC says pregnant women may get flu vaccines either with or without thimerosal.
WHAT ABOUT SIDE EFFECTS OF THE VACCINE?
Common side effects of the flu vaccine are mild, but can include:
- Redness or tenderness where the shot was given
- Headache
- Muscle aches
- Fever
- Nausea and vomiting
If side effects occur, they most often begin soon after the shot. They may last as long as 1 to 2 days. If they last longer than 2 days, you should call your provider.
HOW DO I TREAT THE FLU IF I'M PREGNANT?
Experts recommend treating pregnant women with flu-like illness as soon as possible after they develop symptoms.
- Testing is not needed for most people. Providers should not wait for results of testing before treating pregnant women. Rapid tests are often available in urgent care clinics and provider's offices.

- It is best to start antiviral medicines within the first 48 hours of developing symptoms, but antivirals can also be used after this time period. A 75 mg capsule of oseltamivir (Tamiflu) twice per day for 5 days is the recommended first choice antiviral.
WILL ANTIVIRAL MEDICINES HARM MY BABY?
You may be worried about the medicines harming your baby. However, it is important to realize there are severe risks if you do not get treatment:
- In past flu outbreaks, pregnant women who were otherwise healthy were more likely than those who were not pregnant to become very sick or even die.
- This does not mean that all pregnant women will have a severe infection, but it is hard to predict who will become very ill. Women who become more ill with the flu will have mild symptoms at first.
- Pregnant women can become very sick very fast, even if the symptoms are not bad at first.
- Women who develop a high fever or pneumonia are at higher risk for early labor or delivery and other harm.

DO I NEED AN ANTIVIRAL DRUG IF I HAVE BEEN AROUND SOMEONE WITH THE FLU?
You are more likely to get the flu if you have close contact with someone who already has it.
Close contact means:
- Eating or drinking with the same utensils
- Caring for children who are sick with the flu
- Being near the droplets or secretions from someone who sneezes, coughs, or has a runny nose
If you have been around someone who has the flu, ask your provider if you need an antiviral drug.
WHAT TYPES OF COLD MEDICINE CAN I TAKE FOR THE FLU IF I'M PREGNANT?
Many cold medicines contain more than one type of medicine. Some may be safer than others, but none are proven 100% safe. It is best to avoid cold medicines, if possible, especially during the first 3 to 4 months of pregnancy.
The best self-care steps for taking care of yourself when you have the flu include rest and drinking plenty of liquids, especially water. Tylenol is most often safe in standard doses to relieve pain or discomfort. It is best to talk to your provider before taking any cold medicines while you are pregnant.
It is best to talk to your provider before taking any cold medicines while you are pregnant.
WHAT ELSE CAN I DO TO PROTECT MYSELF AND MY BABY FROM THE FLU?
There are many things you can do to help protect yourself and your unborn child from the flu.
- You should avoid sharing food, utensils, or cups with others.
- Avoid touching your eyes, nose, and throat.
- Wash your hands often, using soap and warm water.
Carry hand sanitizer with you, and use it when you are unable to wash with soap and water.
Which Cold & Flu Medication Is Safe to Take During Pregnancy? | UNM Health Blog
By Maria Montoya, MD | February 04, 2022
You are pregnant and start feeling sick. Before you reach for that bottle of cold or flu medicine, are you certain it is safe for your baby?
When you are pregnant, your baby will be exposed to everything you are exposed to. This means that when you are sick with a cold or flu your baby will not only be exposed to the cold or flu virus, but also any medication you may take.
Typically, with most viruses, you must wait for your immune system to fight the infection. Over-the-counter medications can help soothe your symptoms while you wait.
However, not all over-the-counter medicines are safe to take during pregnancy. Certain medications may hurt the baby or cause problems for you, such as increasing your blood pressure.
Use this quick list of pregnancy-safe natural cold and flu remedies and over-the-counter medications as a starting point. Remember, read the directions on the package for any medication you might take. It’s also a good idea to talk with your doctor or midwife before taking a cold or flu medication.
Natural, Pregnancy-Safe Remedies
Before you try any medications, there are natural remedies you may find adequate relief from first. Here are a couple of safe, natural remedies to try:
- Gargle warm salt water
- Get as much restful sleep as possible
- Sip honey in hot water
- Stay well hydrated
- Use nasal saline sprays
- Try a humidifier
While not all herbs and supplements are safe in pregnancy. You may be able to safely take:
You may be able to safely take:
- Vitamin C
- Zinc
- Manuka Honey
- Elderberry
Talk with your doctor or midwife before taking any supplements or trying at-home remedies or essential oils during pregnancy.
If natural remedies don’t provide enough relief, consider these pregnancy-safe medications.
Pregnancy-Safe Cold & Flu Medication
It is best to avoid taking medications when possible. If you do need to take something, follow the package directions carefully. Talk with your doctor or midwife before taking medication during pregnancy.
These over-the-counter medications are considered safe for most pregnant patients:
- Acetaminophen (Tylenol)
- Safe during the entire pregnancy.
- Take only as needed.
- Try to limit regular exposure.
- Not safe if you are allergic to it or have liver problems.
- Pseudoephedrine (Sudafed)
- Safe in the second and third trimester
- Not safe in the first trimester due to a small risk of abdominal wall birth defects
- Not safe if you have high blood pressure (hypertension) or a history of heart disease
- Chlorpheniramine (Chlor-Trimeton)
- Safe during pregnancy.

- Not safe while breastfeeding.
- Safe during pregnancy.
- Diphenhydramine (Benadryl)
- Safe throughout pregnancy.
Watch out for extra ingredients. Many cold and flu medications treat more symptoms than you may be experiencing. For example, Tylenol Cold Multi-Symptom treats headaches, fever, body aches, cough, chest congestion, stuffy nose, and more. If you just have a stuffy nose, this is more medication than you need.
A word about antibiotics. Some sinus infections are treated with antibiotics. In general, pregnant patients should not take antibiotics unless it is necessary. Make sure your health care provider knows you are pregnant if they prescribe antibiotics.
The dangers of high blood pressure in pregnancy
How to spot symptoms and get help
Read More
Medications to Avoid in Pregnancy
Nonsteroidal anti-inflammatory (NSAID) medications can hurt your developing baby. Do not take NSAIDs such as these when you are pregnant:
Do not take NSAIDs such as these when you are pregnant:
- Ibuprofen (Advil, Motrin)
- Naproxen (Aleve, Midol)
- Celecoxib (Celebrex)
- Aspirin (Bayer), unless your doctor or midwife prescribes daily low-dose aspirin.
Do not take these medications during pregnancy. These drugs can hurt the developing baby:
- Benzocaine (throat lozenges/throat sprays)
- Codeine (a pain and cough medication)
- Phenylephrine (i.e., Sudafed PE): it not considered safe while pregnant because studies with animals showed adverse effects to the fetus.
When you don’t feel well, the last thing you might want to do is read a medication label. However, it is worth taking a few extra moments to read the label and avoid additional risks. If you’re not sure what medicine is safe to take, call us. We are always here to help you.
To find out whether you or a loved one might benefit from Ob/Gyn care
Call 505-272-2245.
Categories: Women's Health
Colds during pregnancy: how to treat?
Any cold or respiratory disease in early pregnancy, during the primary formation of the fetus, can lead to unpredictable consequences and complications. The matter is complicated by the fact that most medications are absolutely contraindicated for use during gestation.
In this regard, the treatment and prevention of colds in pregnant women is an important issue, which should be approached especially responsibly! The main thesis is: be careful with medicines and apply mild preventive measures based on alternative medicine methods to avoid respiratory diseases and flu.
"One for two - immunity"
This is a very fragile system, it is not necessary to interfere in its work, but it is necessary to support and strengthen it. Pregnancy belongs to the category of special, albeit temporary, conditions during which a woman needs additional protection.
This issue will help simple recommendations that are available to everyone:
• During the period of frequent weather changes, it is necessary to dress warmer, paying special attention to footwear.
• During an epidemic, it is better for a pregnant woman to refrain from being in crowded places - transport, metro, shops and hospitals. If there is an urgent need, to prevent possible infection, a protective respiratory mask should be worn before leaving the house.
• Be especially careful about hygiene after visiting the street and public places. Upon returning home, the first thing to do is wash your hands thoroughly.
Interesting: More than 90% of all acute respiratory infections are caused by viruses, about 10% are bacteria and other pathogens. Accordingly, any soap can be used, not necessarily antibacterial.
• Before going outside, you can lubricate the nasal mucosa with oxolinic ointment. Upon returning home, flush the upper respiratory tract with soda solution.
• Rationalization of nutrition and intake of vitamins will strengthen the immune defense. It is especially useful to eat fruits and vegetables that are enriched with vitamins and have not undergone heat treatment.
Interesting: our grandmothers used to say: in order not to get sick, you need to drink chicken broth! Strange, but until recently, scientists did not attach much importance to this prophylactic. Pulmonologist Stefan Rennard decided to find out if this was true or not. The professor conducted a study and proved that the use of chicken broth affects the mobility of neutrophils, leukocytes that protect the body from infections and activate the immune system.
- Vitamins can be taken using ready-made pharmaceutical multivitamin complexes. Before choosing a drug, you should consult your doctor.
- Compliance with the regimen and duration of sleep - at least 9 hours a day. The possibility of psychotraumatic situations should be minimized.
- Maintaining cleanliness in the living quarters (ventilation, wet cleaning).
- Air humidification is an important aspect in the prevention of influenza and respiratory diseases. If air conditioners or heaters are used in the house of a pregnant woman, it would be best to purchase a mechanical humidifier.

Medications for prevention
- Grippferon - a drug in the form of drops for the nose, which provides prevention and treatment of influenza, is not contraindicated for pregnant and lactating women. The medicine stimulates an increase in immunity, has a pronounced antiviral effect that can protect against colds, infections and influenza varieties.
- Ascorbic acid - can be used as a separate source of vitamin C in a synthetic version, with a reduced daily intake from food. Ascorbic acid not only prevents infection, but also fights viruses that have already entered the body of a woman.
- Viferon - nasal ointment, which is prescribed for the prevention of influenza and respiratory infections during an epidemic. The ointment has protective and immunomodulatory effects, and also allows you to deal with disorders that are already occurring in the body at the time of use. Viferon in the form of a nasal ointment has no contraindications for use in pregnant women at any time, including the first trimester.

- Aquamaris is a natural drug in the form of a nasal spray that allows you to moisturize the nasal mucosa, thereby reducing the risk of influenza viruses entering the nasal cavity.
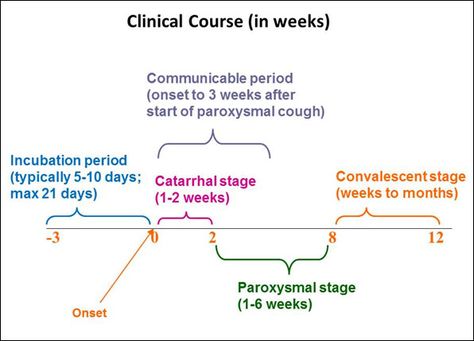
I would like to say a few words about such a method of prevention as vaccination. Most often, the expectant mother may be at risk of infection due to the annual influenza epidemic. This disease is dangerous for a pregnant woman precisely because of its complications: pneumonia, bronchitis, otitis media. Influenza in a pregnant woman can also affect the health of the fetus. Most of all, it is dangerous in the early stages of pregnancy, when the tissues and organs of the human embryo are laid and formed. Viral intoxication or drug exposure can lead to pathology of the child's organs. In later pregnancy, there is a risk of infection of the fetus.
The most dangerous consequence of influenza in a pregnant woman is threatened miscarriage or premature birth!
It is quite natural that expectant mothers often wonder whether or not to vaccinate.
Studies have concluded that the use of inactivated ("killed") influenza vaccines does not have a teratogenic effect on the fetus and does not harm the health of a pregnant woman. After consulting with your doctor about such an inoculation, you can come to an optimal solution. If an influenza epidemic is inevitable, and the pregnant woman has no contraindications, then the vaccine should be given. If a pregnant woman has a negligible risk of infection, she does not come into contact with a large number of people, or is opposed to vaccination, then you can not do it. According to research, it is known that vaccination of mothers reduces the risk of influenza infection of a born child by 63%. Seasonal influenza prevention is carried out in September, October. Vaccinations for pregnant women are recommended from the second trimester of pregnancy.
In the period of a planned pregnancy, a flu shot is given 1 month before it: the formation of immunity occurs 2-4 weeks. Protection after vaccination lasts about a year.
Protection after vaccination lasts about a year.
If infection does occur, action should be taken immediately if at least one symptom of the disease is detected. The health of a pregnant woman and her unborn child depends entirely on her responsibility and respect for her own body.
Proven folk remedies will be used first. Since pregnant women cannot steam their legs, steam their hands, and this will facilitate nasal breathing. Bundle up, put on woolen socks and crawl under the covers: warmth, peace and sleep are good for colds. Do not forget to drink plenty of water - hot green tea with lemon and honey, lime blossom tea, cranberry juice, rosehip broth, dried fruit compote. Ginger in the form of tea also helps, not only with catarrhal symptoms, but with nausea in the morning.
Various hot milk drinks are also suitable. Honey can be added to milk, and it is best to boil it on onions. It must be emphasized right away that not all herbs for colds during pregnancy can be used.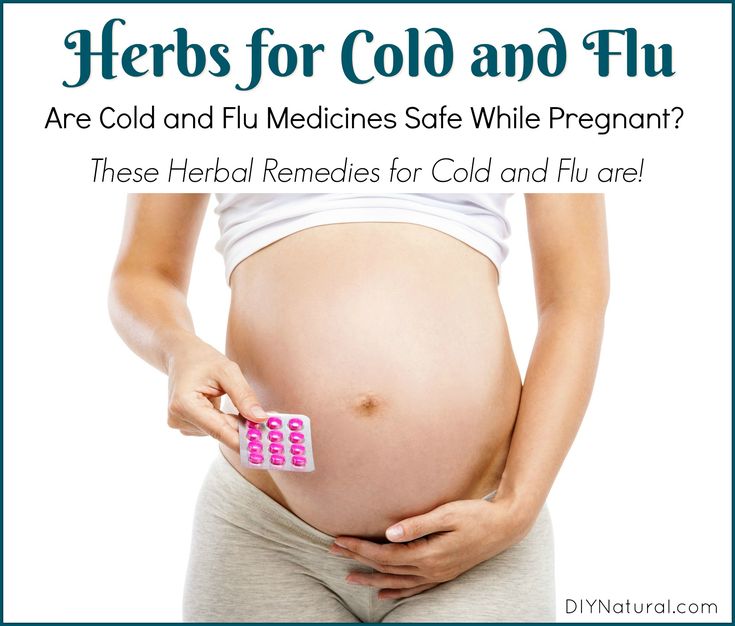 Here is a list of medicinal plants that are contraindicated: aloe, anise, barberry, elecampane (grass and root), sweet clover, oregano, St. John's wort, strawberries (leaves), viburnum (berries), raspberries (leaves), lemon balm, lovage, wormwood, licorice root), celandine, sage. Accordingly, preparations containing these plants should not be taken.
Here is a list of medicinal plants that are contraindicated: aloe, anise, barberry, elecampane (grass and root), sweet clover, oregano, St. John's wort, strawberries (leaves), viburnum (berries), raspberries (leaves), lemon balm, lovage, wormwood, licorice root), celandine, sage. Accordingly, preparations containing these plants should not be taken.
The use of medicines for colds during pregnancy must be treated with great care!
It is contraindicated to use the following drugs : Pertussin, Tussin plus, Joset, Glycodin, Ascoril, Travisil, Broncholitin, ACC, Grippeks, Codelac, Terpinkod. Do not use lozenges and lozenges for sore throat or cough are also undesirable due to the likelihood of allergic reactions.
Spray Pinosol, judging by the components indicated in the instructions, is not dangerous during pregnancy. However, the essential oils contained in the preparation - pine, peppermint, eucalyptus, thymol, guaiazulene (wormwood oil) - can lead to an allergic reaction with swelling of the nasal mucosa.
Viferon suppositories are allowed to be used only after 14 weeks from the start of conception. This drug contains recombinant human interferon alpha-2, ascorbic acid and alpha-tocopherol acetate and has antiviral, immunomodulatory and antiproliferative effects. It is used in the treatment of various infectious and inflammatory diseases in adults and children (including newborns). In the form of an ointment, Viferon is used to treat herpetic lesions of the skin and mucous membranes. The ointment is applied in a thin layer to the affected areas of the skin 3-4 times a day for 5-7 days.
The homeopathic preparation Stodal, which includes predominantly herbal ingredients, acts on various types of cough and has an expectorant and bronchodilator effect.
Viburkol - homeopathic suppositories - have analgesic, anti-inflammatory, sedative, antispasmodic action. They are prescribed in the complex therapy of acute respiratory viral infections and other uncomplicated infections (including in newborns), as well as in inflammatory processes of the upper respiratory tract and inflammatory diseases of the genitourinary system.
So, you can try to eliminate a slight ailment on your own, but there are conditions under which you need to call a doctor at home:
- Prolonged fever;
- Myalgia, fatigue, fatigue, general malaise;
- Difficulty breathing, nasopharyngeal lumps and dry or wet barking cough;
- A pregnant woman is troubled by severe pressing headache.
In conclusion, I would like to emphasize the importance of treating chronic diseases before pregnancy, a healthy lifestyle during childbearing and following all doctor's orders.
I wish expectant mothers and their loved ones to try to maintain a good mood: optimists live longer and happier, they are more productive. Remember your victories and pleasant moments more often and everything will be fine!
Influenza and SARS in pregnant women
HomeFor patientsInformation Influenza and SARS in pregnant women
Viral infections are now regarded as one of the main causes of reproductive losses. On the one hand, the infectious agent has a direct damaging effect on the fetus, and on the other hand, causing significant changes in the immune responses of the mother's body, leads to a complicated course of pregnancy. A special place among infectious diseases of pregnant women is occupied by influenza and other acute respiratory viral infections transmitted by airborne droplets.
On the one hand, the infectious agent has a direct damaging effect on the fetus, and on the other hand, causing significant changes in the immune responses of the mother's body, leads to a complicated course of pregnancy. A special place among infectious diseases of pregnant women is occupied by influenza and other acute respiratory viral infections transmitted by airborne droplets.
The urgency of the problem of acute respiratory diseases of a viral nature is determined by their prevalence, uncontrollability, high contagiousness, allergization and the development of secondary immunodeficiency states after an illness.
The ecological features of modern urbanization provide a real basis for the frequent encounter of women with various respiratory viruses during the entire period of pregnancy. In extragenital pathology of pregnant women, acute respiratory infections occupy the first place in terms of prevalence - more than 2/3 of the total incidence of acute infections. This is due to the high susceptibility of pregnant women to viral infections, the tendency to chronicity of pathological processes, which is due to the peculiarities of the immunity of pregnant women.
The impact of viral infection on the course of pregnancy and the condition of the fetus is characterized by two main mechanisms. Firstly, the possible infection of the placenta, amniotic membranes, as well as the fetus itself, teratogenic (causing malformations) effect on the embryo and fetus, the development of local lesions of the fetus, as well as infection of the fetus with clinical manifestations in the postnatal period (after birth). Secondly, a possible indirect effect as a result of the development of a pregnant fever, a violation of homeostasis (balance, constancy) in the body, etc. , and the fetus.
The main links in the pathogenesis of a viral infection in a pregnant woman, which determine the high risk of perinatal pathology, are:
Activation of the blood coagulation system by the toxic effect of the virus on the vascular wall;
Pathological changes in the immune system resulting from a viral infection;
Activation of chronic intrauterine infection.
The possibility of transmission of respiratory group viruses, which include viruses that cause ARVI, through the placenta from a sick mother to a fetus has been proven, which leads to the involvement of all three components of the "mother-placenta-fetus" system in the infectious process.
Modern researchers consider gestosis (toxicosis of the second half of pregnancy), including its severe forms, as a causal factor of placental insufficiency (PI), a direct relationship between the severity of late gestosis and the severity of PI has been proven. Recent studies have confirmed the assumption that the placenta serves as a kind of "reservoir" in the process of intrauterine infection, as it has been proven that under the influence of viruses, some structures of the placenta change, and viruses reproduce in them.
Specific prophylaxis of influenza does not eliminate the problem of respiratory viral infections, since the proportion of ARVI of non-influenza etiology is up to 75% even during influenza epidemic periods. In addition, the physiological changes in the immune system that occur in the body of pregnant women do not allow them to use vaccine preparations to prevent infectious diseases.
In addition, the physiological changes in the immune system that occur in the body of pregnant women do not allow them to use vaccine preparations to prevent infectious diseases.
The risk group for ARVI infection includes women in whom the incidence of these infections occurred more than three times in the previous year of pregnancy. This sign is a classic confirmation of immunological deficiency in the patient. They are characterized by: a protracted, recurrent course of diseases (rhinitis, pharyngitis, laryngotracheitis, bronchitis), the presence of foci of chronic infection (chronic tonsillitis, sinusitis). In the pathological process in such patients, to one degree or another, other body systems are also involved, which ensure its protection when it encounters the external environment. The most common pathology of the digestive tract: from dysfunctions and dysbiosis to chronic colitis, enteritis, enterocolitis, pancreatitis and cholecystitis.
Features of the course of acute respiratory viral infections in pregnant women
Pregnant women are characterized by a protracted course of acute respiratory viral infections in the absence of severe clinical manifestations. This is due to the ability of respiratory group viruses to reproduce in the placenta, as well as the peculiarity of the immune system of the pregnant woman (a state of physiological immunodeficiency).
The main clinical symptoms of acute respiratory infections: symptoms of general intoxication (malaise, weakness, increased fatigue, etc.) against the background of subfebrile or normal temperature, symptoms of rhinitis or nasopharyngitis.
The most typical ARVI clinic for pregnant women is often the reason for insufficient attention to the very fact of the disease, both on the part of doctors and the woman herself, however, ARVI leads to a breakdown in physiological immune mechanisms and does not exclude the possibility of complications during pregnancy.
Features of pregnancy after SARS. Influence of acute respiratory viral infections in pregnant women on the health of their newborns
The most characteristic complications of pregnancy after acute respiratory viral infections are:
- more than double the incidence of placental insufficiency;
- increase in cases of early onset of preeclampsia;
- oligohydramnios - as a concomitant sign of placental insufficiency, as well as a manifestation of a viral lesion of the fetoplacental complex;
- the threat of premature termination of pregnancy is more common in the 2nd trimester, namely at 17-26 weeks, for pregnant women after ARVI, a constant course of the threat of termination of pregnancy is characteristic, insensitive to the ongoing standard therapy;
- intrauterine growth retardation and intrauterine fetal hypoxia;
- increase in neonatal morbidity:
- hypoxic lesion of the central nervous system is most characteristic of acute respiratory viral infections in the 2nd trimester;
- chronic placental insufficiency (inflammatory and degenerative changes in the placenta, impaired differentiation of placental tissue, suppression of compensatory-adaptive vascular reactions of chorionic villi).
Characteristics of the state of the immune system of pregnant women after SARS
When studying the state of systemic immunity in pregnant women who had ARVI, depending on the duration of pregnancy, in comparison with similar indicators in healthy pregnant women, the following patterns were revealed.
Past ARVI causes changes in the immune status, is characterized, as a rule, by changes in the content of leukocytes and lymphocytes and their populations. A characteristic sign of the immunogram of pregnant women who have had ARVI is lymphocytopenia (destruction of lymphocytes), while during the physiological development of pregnancy, an increase in the total number of leukocytes occurs. Lymphocytopenia can be explained by the direct damaging effect of respiratory viruses on lymphoid cells, its degree depends both on the virulent properties of the viral pathogen and on the adaptive capabilities of the organism.
The effect of viruses on immunological reactivity lies in the fact that in the course of infection, not one, but a series of indicators characterizing the immune response of the organism affected by the virus to foreign antigens changes. There is a disorder of immunological reactivity, caused by a violation of all the functions of immunocompetent cells as a result of the reproduction of the virus.
The occurrence of defects in immunological reactivity should be considered as an essential element of the pathogenesis of ARVI. The presence of these defects does not prevent the formation of specific immunity against the homologous virus.
Methods of prevention and treatment of acute respiratory viral infections in pregnant women
It is known that the specific prevention of influenza and acute respiratory viral infections by vaccine preparations is contraindicated during pregnancy. Researchers both here and abroad pay attention to the search and implementation in practice of methods of non-specific protection of the population from respiratory viral infections. It should be noted that one of the most promising methods of viral infection tactics is immunocorrection. From this point of view, the use of modern immunobiological preparations, adaptogens and eubiotics, is promising.
Therapeutic measures with the use of immunotropic drugs are carried out after ARVI in the 2nd - 3rd trimesters of pregnancy, as well as 10-14 days before the expected date of delivery in the following groups of patients:
- diseases more than 3 times in the previous year of pregnancy;
- pregnant women who had ARVI with a complicated course of pregnancy;
- in the presence of a positive prognosis for the development of perinatal pathology.
Preventive measures
All pregnant women should refrain as much as possible from visiting public places with a large crowd of people in case of a threat and the occurrence of an epidemic of influenza and SARS.
Pregnant women with acute respiratory infections three or more times a year prior to pregnancy should be classified as a high risk group for the development of complications.
This group of patients, as well as all pregnant women with the threat and occurrence of an epidemic of influenza and SARS, need to undergo a course of non-specific prophylaxis.