Cmv test pregnancy
CMV In Pregnancy: What Should I Know?
Cytomegalovirus (CMV) is the most common virus most people have never heard of! It is the most common congenitally acquired virus, and about 1 out of every 100 to 150 newborns is born congenitally infected with CMV. It is common in both children and adults. Between 50 to 80 percent of women of childbearing age have caught CMV and between 1 and 5 percent of pregnant women will catch CMV for the first time during their pregnancy. Most CMV infections are "silent" and harmless, but in pregnant women, CMV can be transmitted to the fetus, with sometimes devastating effects to the unborn baby and newborn. Therefore, it is important if you are pregnant, or know someone who is pregnant, to be "CMV Aware" and "CMV Cautious". Women who are pregnant should discuss CMV with their obstetrician. Testing for CMV infection is a simple blood test. And, there are interventions available to help. Unfortunately, studies have shown most women of childbearing age and surprisingly, many obstetricians, are not aware of the most recent advances in management of CMV infection in pregnancy. Because many of the questions I received from my first blog post were about CMV infection during pregnancy, I decided to post some basic information that I hope you find helpful:
What are the signs and symptoms of CMV during pregnancy?
Most CMV infections in pregnant women are "silent" and cause no symptoms. When symptoms do occur, they most commonly are fever, sore throat, swollen lymph glands and extreme fatigue. Rarely, a rash, cough or diarrhea may occur. These symptoms are not specific for CMV infection and may be cause by other conditions. And, unfortunately, often the first time a pregnant woman is aware of CMV is when she has a baby who is diagnosed with congenital CMV infection. Therefore, blood tests are needed to accurately diagnose a CMV infection during pregnancy.
Is CMV infection common in pregnancy?
Approximately 1-4% of all pregnant women will experience a primary CMV infection during their pregnancy.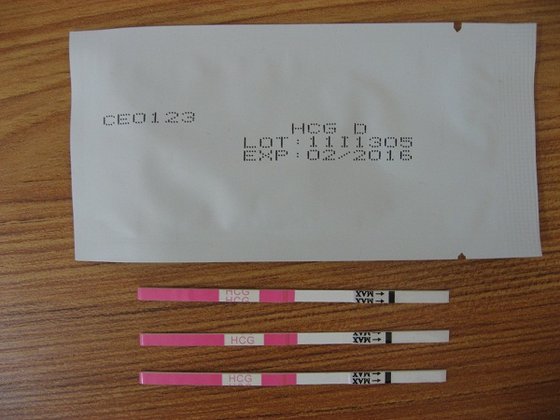 If you work in a child care setting, the risk increases to approximately 10%. If you have a toddler at home who is actively infected with CMV and shedding CMV in their saliva or urine, the risk is even higher, approaching 50% in some studies.
If you work in a child care setting, the risk increases to approximately 10%. If you have a toddler at home who is actively infected with CMV and shedding CMV in their saliva or urine, the risk is even higher, approaching 50% in some studies.
What is the risk to my baby if I have a CMV infection during pregnancy?
CMV infections in pregnancy may be primary (first infection with CMV) or recurrent (infection with a second strain of CMV or reactivation of your own CMV strain). Approximately 40% of women who experience a primary CMV infection during pregnancy will transmit the CMV infection to their baby, and approximately 60% will not. The reason why some women transmit CMV to their baby and some women do not is not known. Most babies born congenitally infected with CMV will appear normal at birth. However, approximately 10% of babies born congenitally infected as a result of their mother's primary CMV infection during pregnancy will have symptoms in the womb or at birth. Newborns with symptomatic congenital CMV disease at birth may have a variety of signs and symptoms in many organ systems, and also may experience disabilities long term in hearing, vision, cognition and motor development. In some babies with severe congenital CMV disease, the congenital CMV infection is fatal. Therefore a maternal primary CMV infection may carry a significant risk to the unborn baby. Women who experience a recurrent CMV infection also may transmit CMV to their baby, but the occurrence is much, much lower ( 0.1% or less) than after a primary CMV infection (40%), and serious symptoms rarely occur in the fetus or newborn born congenitally infected as a result of a maternal recurrent infection.
Newborns with symptomatic congenital CMV disease at birth may have a variety of signs and symptoms in many organ systems, and also may experience disabilities long term in hearing, vision, cognition and motor development. In some babies with severe congenital CMV disease, the congenital CMV infection is fatal. Therefore a maternal primary CMV infection may carry a significant risk to the unborn baby. Women who experience a recurrent CMV infection also may transmit CMV to their baby, but the occurrence is much, much lower ( 0.1% or less) than after a primary CMV infection (40%), and serious symptoms rarely occur in the fetus or newborn born congenitally infected as a result of a maternal recurrent infection.
How do you test for CMV during pregnancy?
Testing for CMV infection is a simple blood test, called a CMV IgG antibody. It will determine if a pregnant woman has had CMV. A positive result indicates a current or past CMV infection. A second blood test, called CMV IgM antibody will help determine if the CMV infection is current or past. If positive, the infection may be current, usually sometime within the last 4 months. CMV IgM antibody in some women may remain positive for over 4 months (sometimes up to a year or more) or may be a false positive result. Therefore, a third CMV antibody test may be performed, called CMV IgG avidity index. A low CMV IgG avidity index indicates the primary CMV infection occurred less than 4 months prior to the blood test, and a high CMV IgG avidity index indicates a CMV infection occurred 4 months ago or longer. A CMV IgG avidity test is not recommended if the CMV IgM antibody is negative, and the test cannot be performed if the CMV IgG antibody is negative.
A positive result indicates a current or past CMV infection. A second blood test, called CMV IgM antibody will help determine if the CMV infection is current or past. If positive, the infection may be current, usually sometime within the last 4 months. CMV IgM antibody in some women may remain positive for over 4 months (sometimes up to a year or more) or may be a false positive result. Therefore, a third CMV antibody test may be performed, called CMV IgG avidity index. A low CMV IgG avidity index indicates the primary CMV infection occurred less than 4 months prior to the blood test, and a high CMV IgG avidity index indicates a CMV infection occurred 4 months ago or longer. A CMV IgG avidity test is not recommended if the CMV IgM antibody is negative, and the test cannot be performed if the CMV IgG antibody is negative.
What can be done if I catch CMV during my pregnancy?
If you experience a CMV infection during your pregnancy, your obstetrician should follow the growth and development of your fetus carefully with serial fetal ultrasound examinations and other tests. In addition, consultation with a maternal-fetal medicine specialist or a specialist in high risk obstetrics may be indicated, especially if the effects of in utero CMV are seen in the fetus. At Texas Children’s Hospital Pavilion for Women consultations with a maternal fetal medicine specialist may be requested through this website. Prenatal treatment of the pregnant mother with CMV hyperimmune globulin (CMV enriched antibody) may reduce the transmission of CMV to the fetus and reduce or reverse some of the effects of CMV on the fetus. If you have experienced a primary CMV infection during pregnancy, please consult with your obstetrician or maternal-fetal medicine specialist about whether or not CMV hyperimmune globulin treatment is right for you and your baby, in addition to following the health and well-being of your baby while still in the womb. A national randomized clinical trial is also underway in the United States (and also possibly in other countries in Europe) to more carefully study the potential benefits of this treatment.
In addition, consultation with a maternal-fetal medicine specialist or a specialist in high risk obstetrics may be indicated, especially if the effects of in utero CMV are seen in the fetus. At Texas Children’s Hospital Pavilion for Women consultations with a maternal fetal medicine specialist may be requested through this website. Prenatal treatment of the pregnant mother with CMV hyperimmune globulin (CMV enriched antibody) may reduce the transmission of CMV to the fetus and reduce or reverse some of the effects of CMV on the fetus. If you have experienced a primary CMV infection during pregnancy, please consult with your obstetrician or maternal-fetal medicine specialist about whether or not CMV hyperimmune globulin treatment is right for you and your baby, in addition to following the health and well-being of your baby while still in the womb. A national randomized clinical trial is also underway in the United States (and also possibly in other countries in Europe) to more carefully study the potential benefits of this treatment. More information may be available as well at https://www.clinicaltrials.gov. What if I am pregnant and CMV antibody negative? If you are CMV IgG and CMV IgM antibody negative and pregnant, then you have never had a CMV infection, and are therefore vulnerable to catching CMV for the first time during your pregnancy. By knowing you are CMV negative, and by knowing about the CMV precautions recommended in my first blog post, you may take steps to reduce your CMV risk during pregnancy.
More information may be available as well at https://www.clinicaltrials.gov. What if I am pregnant and CMV antibody negative? If you are CMV IgG and CMV IgM antibody negative and pregnant, then you have never had a CMV infection, and are therefore vulnerable to catching CMV for the first time during your pregnancy. By knowing you are CMV negative, and by knowing about the CMV precautions recommended in my first blog post, you may take steps to reduce your CMV risk during pregnancy.
Cytomegalovirus and pregnancy
What is cytomegalovirus?
Cytomegalovirus (also called CMV) is a common virus that infects people of all ages. More than half of adults in the United States become infected with CMV by age 40. Once CMV is in your body, you have it for the rest of your life. The virus can reactivate and cause another infection. You can also be re-infected with a different strain (variety) of the virus.
Most people with CMV infection have no symptoms and aren’t aware that they have been infected.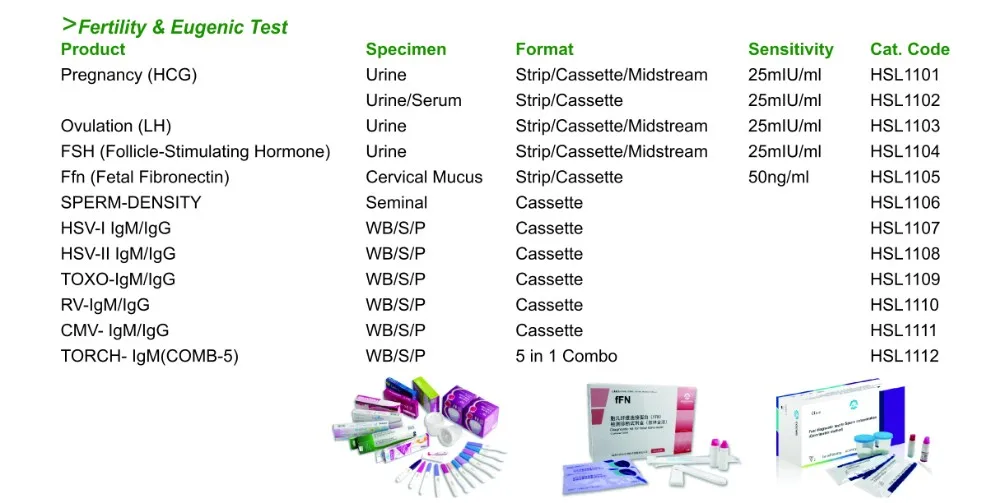 CMV infection usually isn’t harmful in healthy adults or children because their immune system protects their bodies from infection. But CMV can cause serious health problems for some, including:
CMV infection usually isn’t harmful in healthy adults or children because their immune system protects their bodies from infection. But CMV can cause serious health problems for some, including:
- Babies who get infected before birth
- Preterm babies (babies born before 37 weeks of pregnancy) or low birthweight babies (babies born weighing less than 5 pounds, 8 ounces)
- People with weakened immune systems. People with weak immune systems include people living with a serious illness, like HIV, people getting treatment for cancer and people who’ve had a bone marrow or organ transplant.
CMV is the most common infection passed from pregnant people to babies during pregnancy. One in 3 pregnant people passes the infection on to their babies. If you have CMV during pregnancy, the virus in your blood can pass through the placenta to your baby. The placenta supplies the baby with food and oxygen through the umbilical cord. It’s possible for CMV to cause the death of a baby during pregnancy (pregnancy loss).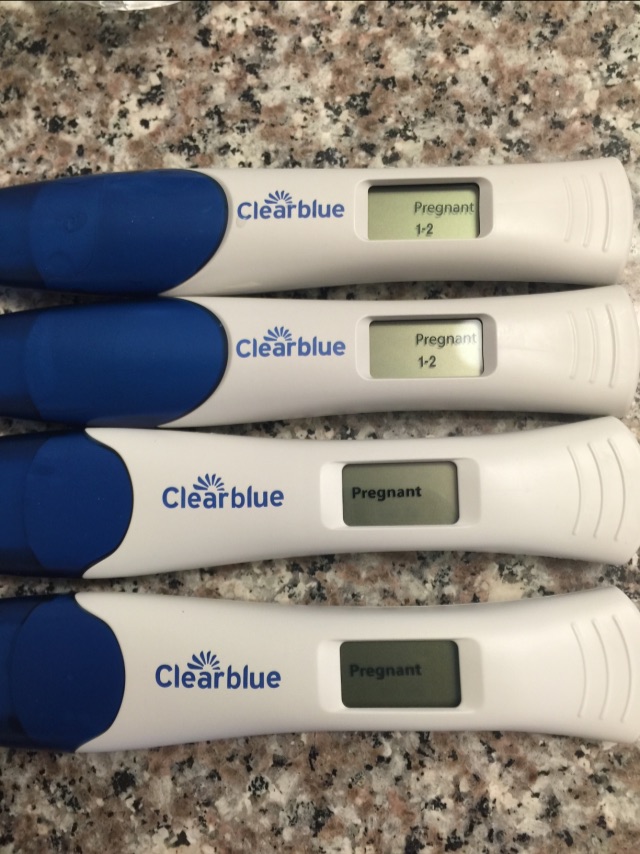
When a baby gets CMV during pregnancy, it’s called congenital CMV. Congenital means that it’s present at birth. One in 200 babies in the U.S. is born with CMV. Most babies with congenital CMV don’t have problems, but some get sick or have long-term health problems. A baby also may get infected after birth if they come in contact with infected body fluids.
There’s no cure for CMV, but medicines can help treat CMV in newborns and people with weak immune systems.
CMV is part of the family of herpes viruses. It’s related to the viruses that cause chickenpox, herpes simplex (also called HSV) and mononucleosis (also called mono). Once you’re infected with CMV, it stays in your body for life. If you’re healthy, CMV usually stays inactive but it can become active again, especially if you get a disease or take medicine that weakens your immune system. You also can get infected again with a different strain of the virus.
What are the signs and symptoms of CMV?
Most people with CMV don’t know they have the infection because they don’t have signs or symptoms. Signs and symptoms of CMV can be different in healthy people, babies and people with weak immune systems.
Signs and symptoms of CMV can be different in healthy people, babies and people with weak immune systems.
Signs and symptoms of CMV in healthy people may include:
- Chills and/or sweats
- Decreased appetite
- Fatigue (being very tired and having little energy)
- Fever
- Headache
- Muscle aches
- Sore throat
- Swollen glands
CMV sometimes can cause hepatitis and mononucleosis (mono). Hepatitis is a disease caused by a virus that attacks the liver. Mono is a disease that can cause extreme fatigue, head and body aches, sore throat, swollen lymph nodes and swollen spleen or liver.
People with weakened immune systems who get CMV can have more serious problems that can affect the eyes, lungs, liver, esophagus, stomach and intestines. The esophagus is the tube that connects the mouth and stomach. The intestines are long tubes that help your body break down (digest) food.
People who are more likely to have the signs and symptoms of CMV include:
- Babies who became infected with CMV before they are born (congenital CMV).

- Babies who become infected during birth or shortly after (perinatal CMV). This group includes babies infected while nursing.
- People who have weakened immune systems, such as those who have had an organ, bone marrow or stem cell transplant, or those who are infected with HIV.
Contact your health care provider if you have the symptoms of mono while pregnant. These include:
- Extreme fatigue
- Head and body aches
- Sore throat
- Swollen lymph nodes
- Swollen spleen or liver.
How does CMV spread?
You get CMV by coming in direct contact with body fluids from a person who’s infected with CMV. Body fluids that can contain CMV include:
- Blood
- Breast milk
- Saliva
- Semen
- Tears
- Urine
- Vaginal fluids
CMV spreads in several ways:
- Passing it to your baby during pregnancy, labor, birth, or nursing
- Touching your eyes or the inside of your mouth or nose after direct contact with an infected person’s body fluids, including saliva, urine, blood, tears, semen and human milk.
- Having sexual contact or kissing an infected person
- Getting an organ, bone marrow or stem cell transplant or blood transfusion
Adults usually get CMV by having sex with someone who has CMV or by having contact with young children who have CMV.
You may be more likely than other people to get CMV if you:
- Have young children. CMV often spreads during diaper changes, bathing and other close contact with babies and young children. Children can get infected with CMV at child care or school and pass it on to their families, caregivers and other children.
- Work with young children. For example, you’re a child care worker or a teacher. CMV spreads easily in child care centers or preschools where children share toys that may carry CMV.
- Have sex with someone who has CMV.
- Work in a health care setting, like a health care provider’s office or a laboratory, where you may have contact with infected body fluids.

- Have a blood transfusion or organ transplant. A blood transfusion is when you have new blood put into your body. An organ transplant is when you have a new organ, like a heart or kidney, put into your body.
Can I give CMV to my baby?
You’re more likely to pass CMV to your baby if you get infected during pregnancy than if you had an infection before you got pregnant. If you have a CMV infection during pregnancy, you have a 1-in-3 chance (33 percent) of passing it to your baby. If you were infected with CMV before you got pregnant, the chance of passing it to your baby drops to about 1 in 100.
More than half of adults have had a CMV infection by the time they are 40 years old, and about 1 to 4 in 100 people (1 to 4 percent) get infected with CMV for the first time during pregnancy.
You can pass CMV to your baby at any time during pregnancy. But you are more likely to pass it on if you get infected for the first time during pregnancy or if a past CMV infection becomes active again, especially in the third trimester. You also can pass CMV to your baby during labor and birth, or while nursing. If your baby gets the virus during these times and was born at a healthy weight, they probably won’t have health problems. Preterm babies (babies born before 37 weeks of pregnancy) and low-birthweight babies (babies born weighing less than 5 pounds, 8 ounces) may get sick if they’re infected during birth or while you’re nursing.
You also can pass CMV to your baby during labor and birth, or while nursing. If your baby gets the virus during these times and was born at a healthy weight, they probably won’t have health problems. Preterm babies (babies born before 37 weeks of pregnancy) and low-birthweight babies (babies born weighing less than 5 pounds, 8 ounces) may get sick if they’re infected during birth or while you’re nursing.
If you had a CMV infection before you got pregnant, you can still pass it to your baby, but this is rare.
How does CMV affect babies?
Most babies born with CMV never show signs of the disease and don’t have health problems.
However, babies who are infected with CMV at birth may have long-term health problems, including:
- Hearing loss
- Intellectual and developmental disabilities. These are problems with how the brain works that can cause a person to have trouble or delays in physical development, learning, communicating, taking care of themselves or getting along with others.

- Coordination issues or muscle weakness
- Smaller than expected head (called microcephaly)
- Seizures or convulsions
- Vision loss
Some babies with congenital CMV who don’t show the signs of the disease at birth may still have or develop hearing loss. It may affect one ear or both ears. Sometimes hearing loss can get worse as a baby grows up.
How is CMV diagnosed during pregnancy?
You typically won’t be tested for CMV during prenatal testing. Tell your health care provider if you think you may have CMV or you think you may have been exposed to CMV. Your provider can give you a blood test or test other body fluids to see if you’re infected. Blood tests can help you know whether you have a new infection or if you had a past infection.
Can a baby get tested for CMV before birth?
Yes. If a blood test shows you have a new CMV infection during pregnancy, your provider may recommend testing your baby for the virus using amniocentesis (also called amnio).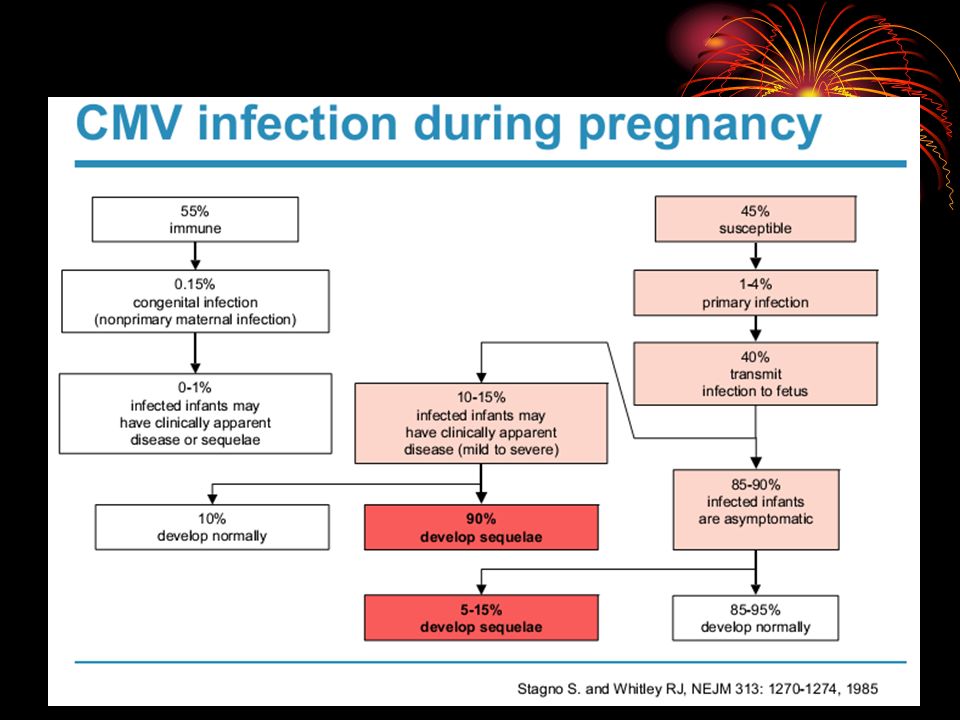 An amniocentesis is a test that takes some amniotic fluid from around your baby before they are born to check for birth defects and genetic conditions in your baby. You can get this test at 15 to 20 weeks of pregnancy. Your provider also may use ultrasound to check for physical signs that your baby has CMV. An ultrasound (also called sonogram) uses sound waves to show a picture of your baby before they are born. If your provider thinks that your baby may have CMV, your baby’s urine and saliva may be tested to check for the virus.
An amniocentesis is a test that takes some amniotic fluid from around your baby before they are born to check for birth defects and genetic conditions in your baby. You can get this test at 15 to 20 weeks of pregnancy. Your provider also may use ultrasound to check for physical signs that your baby has CMV. An ultrasound (also called sonogram) uses sound waves to show a picture of your baby before they are born. If your provider thinks that your baby may have CMV, your baby’s urine and saliva may be tested to check for the virus.
How is CMV treated during pregnancy?
There is no cure for CMV, but medications can control infections. Most healthy adults with CMV don’t need treatment. This includes during pregnancy.
People with weakened immune systems may need treatment with an antiviral medicine. These medicines kill infections caused by viruses. Medicines used to treat CMV include ganciclovir, valganciclovir, cidofovir and foscarnet.
How are babies diagnosed with CMV after birth?
About 1 in 200 babies (less than 1 percent) is born with congenital CMV in this country each year. Your baby’s provider can diagnose CMV infection by testing your newborn baby’s saliva, urine or blood. Testing should be done within 2 to 3 weeks after your baby is born to confirm that your baby has congenital CMV.
Your baby’s provider can diagnose CMV infection by testing your newborn baby’s saliva, urine or blood. Testing should be done within 2 to 3 weeks after your baby is born to confirm that your baby has congenital CMV.
Most babies with congenital CMV don’t have health problems, but about 1 in 5 babies with congenital CMV can get sick from the virus or have long-term health problems.
Some babies born with CMV have signs and symptoms, including:
- Hearing loss. This is the most common health problem in babies born with CMV. A baby may have hearing loss at birth or it may develop later in childhood.
- Eye damage
- Problems with the spleen, liver or lungs. The spleen is an organ that filters blood in your body and fights infection.
- Jaundice. Jaundice is when a baby’s eyes and skin look yellow. A baby has jaundice when their liver isn’t fully developed or isn’t working well.
- Low birth weight (less than 5 pounds, 8 ounces)
- Smaller than expected head (called microcephaly)
- Neurologic problems, including seizures or convulsions
- Pneumonia
- Preterm birth
- Skin rash or purple splotches on the skin
- Swollen lymph nodes
How is CMV treated after birth?
Babies who show the signs of CMV at birth may be treated with antiviral medications. Antiviral medication may lower your baby’s risk of developing health problems and hearing loss. These medications can include ganciclovir or valganciclovir. However, both can cause serious side effects. More research about using antiviral medications on babies is needed.
Antiviral medication may lower your baby’s risk of developing health problems and hearing loss. These medications can include ganciclovir or valganciclovir. However, both can cause serious side effects. More research about using antiviral medications on babies is needed.
Using antivirals to treat babies with congenital CMV who have no signs at birth is not currently recommended.
Babies with congenital CMV, with or without signs at birth, should have regular hearing checks. If your baby has a hearing issue, the earlier it’s detected, the more your baby can benefit from treatment. You should also follow up regularly with your baby’s doctor to discuss any care or additional services that your baby may need. This may include speech services or occupational therapy.
Can I nurse my baby if I have CMV?
CMV can be transmitted to your baby through breast milk while nursing. If you have CMV, you can nurse your baby if they were full term at birth. However, if your baby was born before 30 weeks of pregnancy and weighs less than 3. 3 pounds (1,500 grams), talk to your provider before nursing. Some preterm and low birthweight babies can get sick from infected breast milk. Freezing and pasteurizing (heating) breast milk can decrease the risk of transmission. However, freezing does not make nursing completely safe for your baby.
3 pounds (1,500 grams), talk to your provider before nursing. Some preterm and low birthweight babies can get sick from infected breast milk. Freezing and pasteurizing (heating) breast milk can decrease the risk of transmission. However, freezing does not make nursing completely safe for your baby.
How can you protect yourself from CMV?
Here are some things you can do:
- Wash your hands often with soap and water, especially after being in contact with body fluids from babies or children. Carefully throw away used diapers and tissues. Wash your hands after changing diapers, feeding a child, wiping noses and picking up toys.
- Avoid contact with tears or saliva if you kiss a child, especially if you’re pregnant. Kiss babies and children on the cheek or head instead of on the lips.
- Don’t share toothbrushes, food, drinks, cups, straws, forks or other utensils with young children or with anyone who may have CMV.
 Don’t put a baby’s pacifier in your mouth.
Don’t put a baby’s pacifier in your mouth. - Clean toys and countertops often.
- If your partner has CMV, use a latex condom during sex.
- If you’re a health care worker in contact with people who have CMV, including newborns, follow workplace safety rules to protect yourself from infection. Wash your hands often and wear gloves.
Scientists are working to develop vaccines for CMV. Vaccines make you immune to certain diseases. These vaccines may help prevent CMV infection in pregnant people and babies, and they may help reduce the chance that a baby born to an infected person will have health problems.
For more information
- nationalcmv.org
- stopcmv.org
- CDC.gov
Last reviewed: August 2021
The question is asked by Irina, - a question-answer from the specialists of the clinic "Mother and Child"
irina:
10/23/2014
gestational age 23 weeks, age 31, first pregnancy. on the 9th week - October 20, an analysis was taken for cytomegalovirus-antibody Ig G detected - the number was not indicated, the avidity index was 50 (in decoding - primary infection, on Wednesday 3-5 months ago, if the avidity index was more than 50 percent, then in decoding these are highly avid bodies), from the 3rd week of pregnancy, the subfebrile temperature of 37.2 lasted more than 5 weeks, the throat hurt (plugs, white plaque), severe runny nose, pulling pains in the muscles of the legs, ached eyes. herpes popped up on the lip. at 11 weeks, the analysis for CMV was again passed, the result of Ig G 10me \ ml-immunocab (positive from 1 me \ lm), Ig M-not detected, two weeks later, the result of which cytomegalovirus-anti was tested for control Ig G bodies were detected, the avidity index was already 62%. I did not donate blood before pregnancy, I did it by PCR (scraping of the cervical canal epithelium) on June 24, DNA was not detected. Streptococcus genus was found in a normal throat culture molytic grade 3, at first they wanted to prescribe antibiotics but sent for a blood test, it wasn’t found there, she was treated with bioparox, nothing was found on the next smear.
on the 9th week - October 20, an analysis was taken for cytomegalovirus-antibody Ig G detected - the number was not indicated, the avidity index was 50 (in decoding - primary infection, on Wednesday 3-5 months ago, if the avidity index was more than 50 percent, then in decoding these are highly avid bodies), from the 3rd week of pregnancy, the subfebrile temperature of 37.2 lasted more than 5 weeks, the throat hurt (plugs, white plaque), severe runny nose, pulling pains in the muscles of the legs, ached eyes. herpes popped up on the lip. at 11 weeks, the analysis for CMV was again passed, the result of Ig G 10me \ ml-immunocab (positive from 1 me \ lm), Ig M-not detected, two weeks later, the result of which cytomegalovirus-anti was tested for control Ig G bodies were detected, the avidity index was already 62%. I did not donate blood before pregnancy, I did it by PCR (scraping of the cervical canal epithelium) on June 24, DNA was not detected. Streptococcus genus was found in a normal throat culture molytic grade 3, at first they wanted to prescribe antibiotics but sent for a blood test, it wasn’t found there, she was treated with bioparox, nothing was found on the next smear.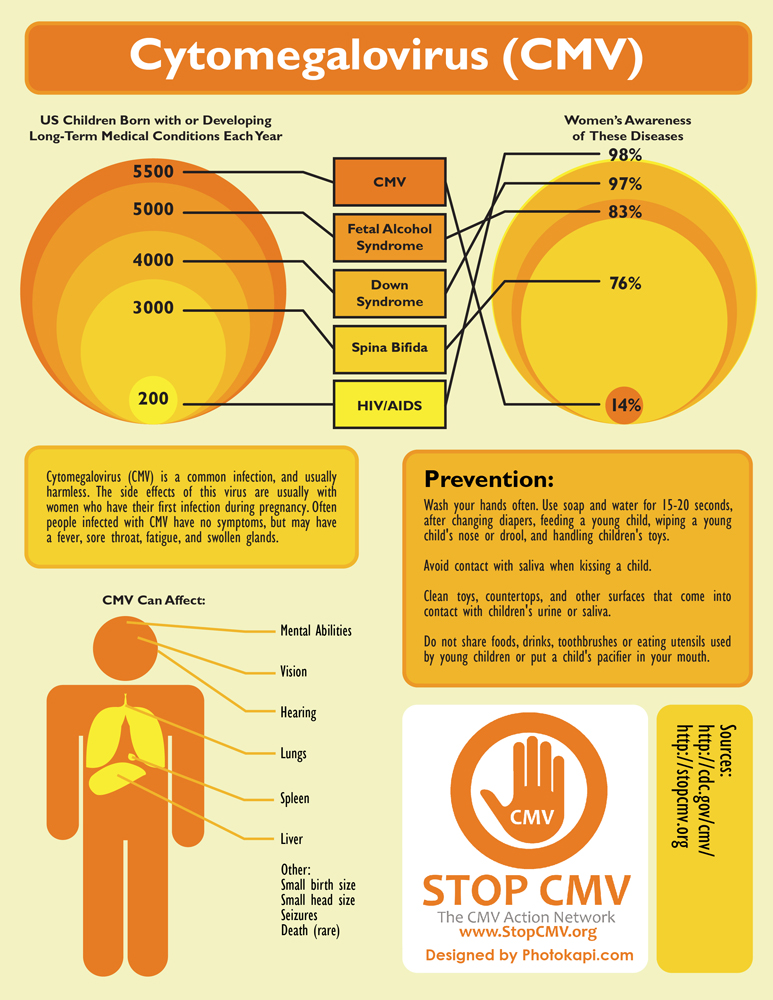 Then, on November 25, blood was donated - immunoglobulin M to CMV was not detected, avidity 62 percent, December 12 - avidity 74 percent, M-negative. On December 27, I was tested in another laboratory for CMV-Ig M-not detected, Ig G 100, avidity index for CMV-99 percent. From January 16, smears were taken - scraping of the epithelium of the cervical canal, DNA of the pathogen, the result of a PCR study - CMV - DNA was not detected, Herpes type 1 and 2 DNA was not detected, and in the blood by the Ifa method of January 27, CMV-Ig M-not detected, Ig G 140, Herpes simplex virus 1,2 type Ig M-not detected, Ig Gk HSV 1 type 100, HSV 2 type Ig G not detected, avidity to HSV-98.9%. tell me, please, they didn’t take blood from me by PCR for CMV, I just now asked the doctor, on the advice of a laboratory assistant, who said that CMV and herpes can be a cross reaction. If I now donate blood by PCR for CMV, then a positive result will indicate an acute process? and how long the M titers to CMV are in the blood, which indicate an acute process.
Then, on November 25, blood was donated - immunoglobulin M to CMV was not detected, avidity 62 percent, December 12 - avidity 74 percent, M-negative. On December 27, I was tested in another laboratory for CMV-Ig M-not detected, Ig G 100, avidity index for CMV-99 percent. From January 16, smears were taken - scraping of the epithelium of the cervical canal, DNA of the pathogen, the result of a PCR study - CMV - DNA was not detected, Herpes type 1 and 2 DNA was not detected, and in the blood by the Ifa method of January 27, CMV-Ig M-not detected, Ig G 140, Herpes simplex virus 1,2 type Ig M-not detected, Ig Gk HSV 1 type 100, HSV 2 type Ig G not detected, avidity to HSV-98.9%. tell me, please, they didn’t take blood from me by PCR for CMV, I just now asked the doctor, on the advice of a laboratory assistant, who said that CMV and herpes can be a cross reaction. If I now donate blood by PCR for CMV, then a positive result will indicate an acute process? and how long the M titers to CMV are in the blood, which indicate an acute process.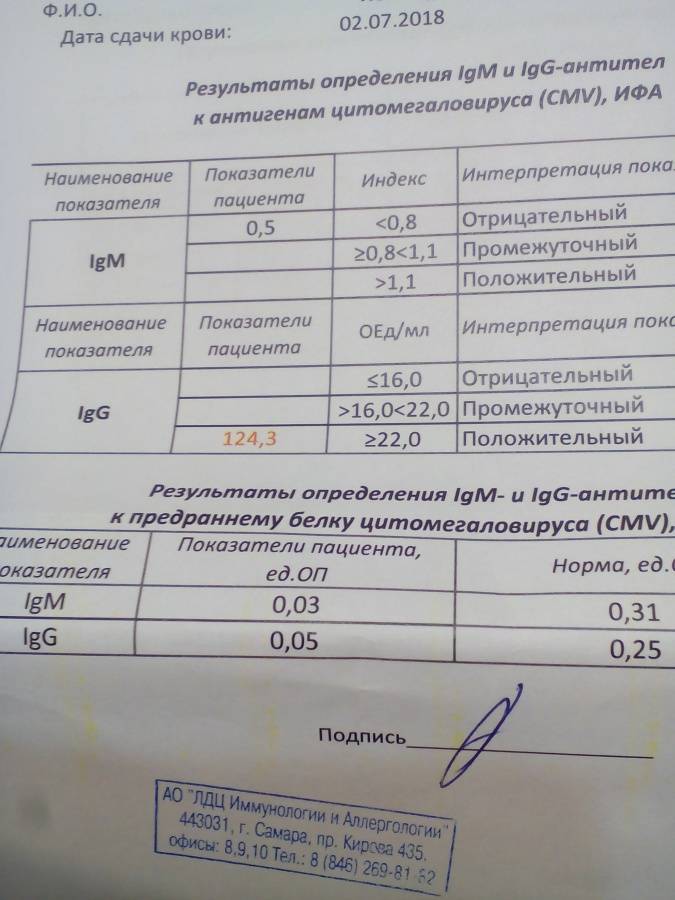 I also know that a fourfold increase in G indicates an acute process, but I can’t compare the analysis from November and December, and the doctor does not answer anything. I’m going to do it at 24 weeks ultrasound, afp at 17 weeks below the norm - 0.6 mom, norm 20.9-59.9 I have 17.8 beta hcg and free estriol is normal.
I also know that a fourfold increase in G indicates an acute process, but I can’t compare the analysis from November and December, and the doctor does not answer anything. I’m going to do it at 24 weeks ultrasound, afp at 17 weeks below the norm - 0.6 mom, norm 20.9-59.9 I have 17.8 beta hcg and free estriol is normal.
MD GROUP Clinical Hospital:
01/26/2021
Virus carriers are not yet sick. The vast majority of people do not even know that they are infected. Infection and real disease are by no means the same thing. IgM antibodies may indicate either a primary infection or an exacerbation of a chronic infection. The presence of specific. IgM increase shortly after the onset of the disease, reach a peak by 1-4 weeks, exist in the blood for 30-60 days after the initial infection with the virus, and then disappear. You have never had IgM during pregnancy, apparently there was no exacerbation of the infection, or there was no acute process, but it is possible that you had CMV infection immediately before pregnancy.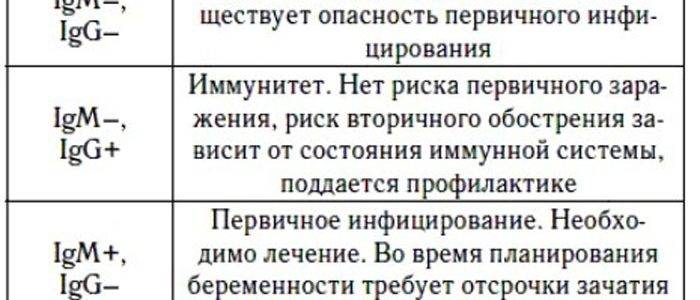 IgG are determined a little later (not earlier than 2 weeks after the onset of the disease), their levels rise more slowly than IgM, but they also remain much longer (for some infections, throughout life). An increase in the level of IgG suggests that the body has already met with this infection. If you are pregnant and have positive IgG antibodies against cytomegalovirus, then the chance of transmitting the virus from you to the fetus is negligible if you did not become infected with CMV in the months preceding pregnancy. In your case, this is likely (clinical manifestations at the beginning of pregnancy, low-avid IgG antibodies). If the mother has antibodies to CMV, congenital infection is observed in 1.4-1.9% of newborns. When a mother is infected with CMV for the first time during pregnancy, up to 46-50% of fetuses are infected in utero. It is necessary for you to consult in the herpetic center. If you become infected with cytomegalovirus during pregnancy, this does not mean at all that the unborn child will be infected.
IgG are determined a little later (not earlier than 2 weeks after the onset of the disease), their levels rise more slowly than IgM, but they also remain much longer (for some infections, throughout life). An increase in the level of IgG suggests that the body has already met with this infection. If you are pregnant and have positive IgG antibodies against cytomegalovirus, then the chance of transmitting the virus from you to the fetus is negligible if you did not become infected with CMV in the months preceding pregnancy. In your case, this is likely (clinical manifestations at the beginning of pregnancy, low-avid IgG antibodies). If the mother has antibodies to CMV, congenital infection is observed in 1.4-1.9% of newborns. When a mother is infected with CMV for the first time during pregnancy, up to 46-50% of fetuses are infected in utero. It is necessary for you to consult in the herpetic center. If you become infected with cytomegalovirus during pregnancy, this does not mean at all that the unborn child will be infected.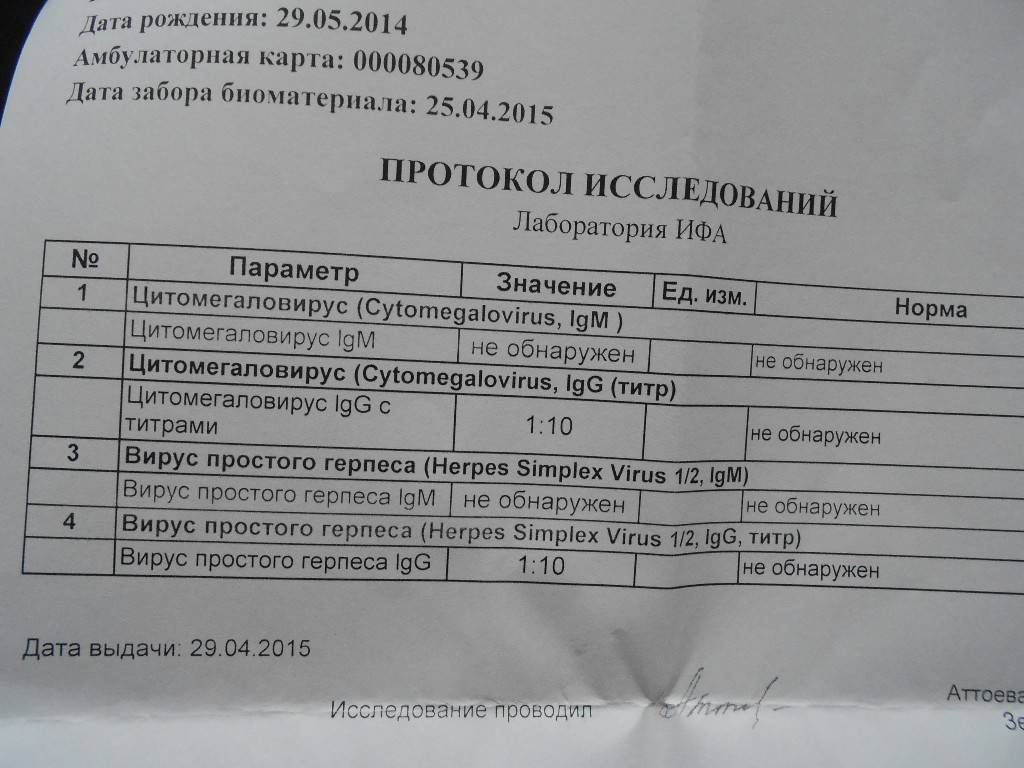 In these cases, it is necessary to monitor the condition of the fetus (ultrasound in qualified medical centers), it is possible to conduct more thorough examinations (amniocentesis) in order to find out if it is infected fetus or not. In the vast majority of cases, children born with CMV develop normally. Agranovskaya A.V., obstetrician-gynecologist, Ph.D.
In these cases, it is necessary to monitor the condition of the fetus (ultrasound in qualified medical centers), it is possible to conduct more thorough examinations (amniocentesis) in order to find out if it is infected fetus or not. In the vast majority of cases, children born with CMV develop normally. Agranovskaya A.V., obstetrician-gynecologist, Ph.D.
Cytomegalovirus infection and pregnancy
Cytomegalovirus (CMV) is the causative agent of one of the most common viral infections in the world, which is usually asymptomatic [1]. Clinical manifestation of the disease with the possible development of extremely severe forms occurs very rarely and only in patients with acquired immunodeficiency states (AIDS, cytostatic, immunosuppressive therapy, etc.) or physiological nature, which is typical, for example, for newborns. It is this last circumstance that determines the special interest in the problem of CMV infection during pregnancy [2].
Etiology and pathogenesis
CMV is a DNA-containing virus of the Herpesviridae family, which also includes herpes simplex viruses types 1 and 2, varicella-zoster virus, and Epstein-Barr virus. The main biological feature of these viruses is their lifelong persistence and possible reactivation in the body of an infected person.
The main biological feature of these viruses is their lifelong persistence and possible reactivation in the body of an infected person.
During reproduction, CMV acts cytopathically with the formation of giant cells with typical intranuclear and cytoplasmic inclusions [1]. For the first time, these cells were found in the kidneys of a stillborn and described by the German pathologist H. Ribbert in 1881. Subsequently, other researchers identified similar cells in the lungs, liver, salivary glands and other organs in fetuses who died in utero, but the cause of their occurrence remained unknown for a long time. Therefore, in the 20s of the last century, taking into account the characteristic features of the affected cells, it was proposed to call this condition cytomegaly. Later, with the advent of electron microscopy, it was suggested that the cause of giant cell changes is a viral infection. The virus itself, named cytomegalovirus, was isolated in 1956 M. Smith [1].
Epidemiology
According to the latest epidemiological data [3, 4], 65-70% of people become infected with CMV during their lifetime. At the same time, the frequency of infection development varies in different populations depending on a number of geographical, ethnic, age and socio-economic factors. So, in the UK and the USA among the adult population of the middle and high socioeconomic levels, 40-60% are seropositive, and in the population with a low social status - 80%. In developing countries, the prevalence of CMV infection is even higher - 80% of children and almost the entire adult population [5-7]. Among pregnant women, specific antibodies to CMV are determined in 40% in economically developed countries and in 100% in developing countries (Table 1).
At the same time, the frequency of infection development varies in different populations depending on a number of geographical, ethnic, age and socio-economic factors. So, in the UK and the USA among the adult population of the middle and high socioeconomic levels, 40-60% are seropositive, and in the population with a low social status - 80%. In developing countries, the prevalence of CMV infection is even higher - 80% of children and almost the entire adult population [5-7]. Among pregnant women, specific antibodies to CMV are determined in 40% in economically developed countries and in 100% in developing countries (Table 1).
Table 1. Prevalence of CMV infection among women, %
Although CMV is a common pathogen and most people become infected with it at some stage in their lives, the virus is not highly contagious and transmission requires close or intimate contact between infected people (transmission of the virus through blood, urine, saliva, semen, cervical discharge, etc. ) [3]. It is believed that 43-53% of CMV cases in adults are infected children who shed the virus in urine and saliva for many years. Therefore, women working with children in kindergartens and other preschool institutions are at increased risk of infection. In the United States, the annual incidence of CMV infection in such groups is 8–40%, while in the general population it is 3–5%. Other ways of transmission of infection among adults: through sexual intercourse, transfusion of blood products, transplantation of organs and tissues [3].
) [3]. It is believed that 43-53% of CMV cases in adults are infected children who shed the virus in urine and saliva for many years. Therefore, women working with children in kindergartens and other preschool institutions are at increased risk of infection. In the United States, the annual incidence of CMV infection in such groups is 8–40%, while in the general population it is 3–5%. Other ways of transmission of infection among adults: through sexual intercourse, transfusion of blood products, transplantation of organs and tissues [3].
Course of CMV infection in pregnant women
Primary CMV infection during pregnancy, when a seronegative pregnant woman first becomes infected with CMV and seroconverts, occurs in 1-2% of cases [7]. However, this situation is most dangerous in relation to intrauterine transmission of the infection to the fetus (see below). Another 13–14% of seropositive women are susceptible to secondary infection during pregnancy, which can be either activation of a latent infection (relapse) or reinfection with a new virus strain [6, 7].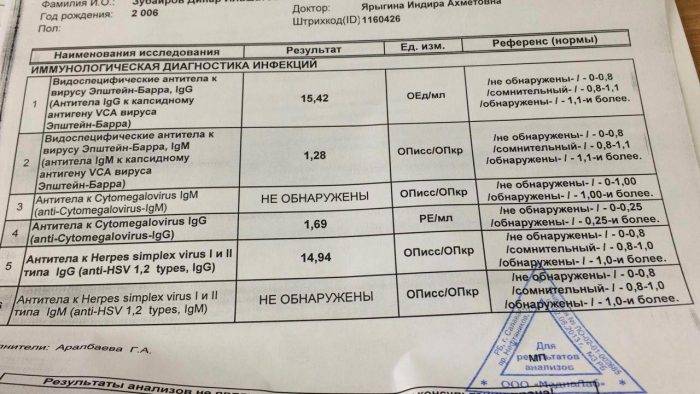
In more than 90% of cases, clinical manifestations of the disease are absent. However, some patients may experience symptoms characteristic of infectious mononucleosis (subfebrile temperature, weakness, headache, myalgia, cough, sore throat, nausea, diarrhea, lymphadenopathy, rarely hepatosplenomegaly and rash) [8]. In a laboratory blood test, a slight increase in the level of hepatic transaminases, lymphopenia or lymphocytosis with atypical lymphocytes in a peripheral blood smear, and thrombocytopenia are noted. The duration of manifestations is 1–2 weeks in mild cases and up to 6 weeks in severe cases [8]. Rarely, with severe immunosuppression, severe complications are possible: interstitial pneumonia, hepatitis, meningoencephalitis, myocarditis, hemolytic anemia [8].
Course of CMV infection in the fetus and newborn
CMV infection is the most common congenital infection identified to date and a well-known cause of fetal and neonatal pathology. Infection of the fetus is possible both in utero, with transplacental transmission of the virus from the mother, and during childbirth when passing through an infected birth canal [9]. In the postnatal period, CMV is most often transmitted to the newborn through breast milk or blood transfusion. The number of cases of intrauterine transmission of CMV fluctuates between 0.2-2.2%, averaging 1% in the population. Intranatal and postnatal infection during the first 6 months of life occurs in another 1-15% of all newborns (Table 2) [9].
Infection of the fetus is possible both in utero, with transplacental transmission of the virus from the mother, and during childbirth when passing through an infected birth canal [9]. In the postnatal period, CMV is most often transmitted to the newborn through breast milk or blood transfusion. The number of cases of intrauterine transmission of CMV fluctuates between 0.2-2.2%, averaging 1% in the population. Intranatal and postnatal infection during the first 6 months of life occurs in another 1-15% of all newborns (Table 2) [9].
Table 2. Modes of transmission and incidence of CMV infection in the fetus and newborn
Congenital CMV infection. Most often, intrauterine infection of the fetus occurs during primary CMV infection in pregnant women - in 30-40% of cases (Table 3) [10]. However, unlike most other viruses, CMV can also be transmitted from mother to fetus during recurrent infection (reactivation or reinfection), although this occurs much less frequently - 1–2% [10].
Table 3. The number of cases of CMV infection in pregnant women and the risk of intrauterine infection
CMV infection is transmitted to the fetus transplacentally, with primary infection of the placental tissue with subsequent penetration of the virus into the amniotic cells. In the future, the fetus swallows infected amniotic fluid. Transmission of CMV to the fetus is possible with the same frequency in any trimester of pregnancy, increasing as its duration increases [8–10]. There are suggestions that intrauterine CMV infection may be accompanied by spontaneous miscarriages or antenatal fetal death [11].
In 90-95% of newborns, intrauterine CMV infection is asymptomatic (see figure). Thus, clinical manifestations at birth are present in only 5-10% of prenatally infected children and are most often characterized by hepatosplenomegaly (75%), petechiae (65-80%), growth retardation (70%), jaundice (65%), microcephaly ( 45-50%) and periventricular calcification of the brain (45%) [3, 8, 12-15].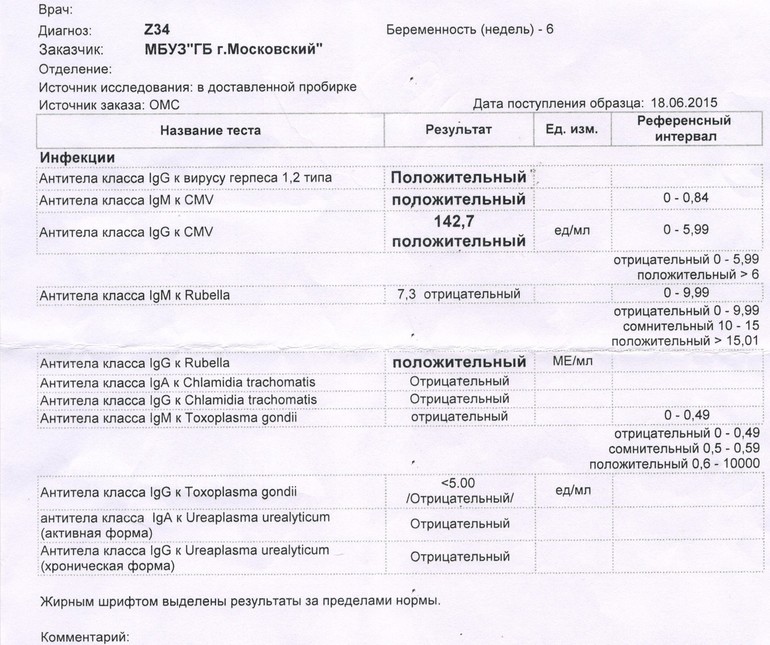 Due to the high tropism of CMV to the central nervous system, 70–90% of these children in the future may have severe long-term consequences — hearing loss, visual impairment, mental retardation, and cerebral palsy [12, 15]. The likelihood of developing severe forms of the disease increases significantly with primary CMV infection in the mother, especially if the virus enters the fetus in the first half of pregnancy. Mortality in severe forms of the disease is 30% [15, 16].
Due to the high tropism of CMV to the central nervous system, 70–90% of these children in the future may have severe long-term consequences — hearing loss, visual impairment, mental retardation, and cerebral palsy [12, 15]. The likelihood of developing severe forms of the disease increases significantly with primary CMV infection in the mother, especially if the virus enters the fetus in the first half of pregnancy. Mortality in severe forms of the disease is 30% [15, 16].
Congenital CMV infection.
Most children infected with CMV in utero, born without clinical manifestations of the disease, develop absolutely normally. However, in 5-10% of them, some neurological disorders are subsequently likely, among which sensorineural deafness is the most common. Other long-term consequences include cerebral palsy, epilepsy, psychomotor retardation, and chorioretinitis [3, 14, 16, 17].
Sensorineural deafness. CMV, which can damage various structures of the inner ear, is one of the main causes of hearing loss in children. Hearing loss occurs in 5–11% of infected neonates and may be unilateral or bilateral. Many researchers note that this disease is more common in patients with symptomatic intrauterine CMV infection - 23-58% than in children without symptoms of the disease - 4-15%. At the same time, in the 1st group of children, the disease manifests itself in more severe forms [5, 18].
Hearing loss occurs in 5–11% of infected neonates and may be unilateral or bilateral. Many researchers note that this disease is more common in patients with symptomatic intrauterine CMV infection - 23-58% than in children without symptoms of the disease - 4-15%. At the same time, in the 1st group of children, the disease manifests itself in more severe forms [5, 18].
Anecdotal evidence suggests that, unfortunately, hearing screening in newborns detects less than half of cases of CMV-induced sensorineural deafness, as this disease may present later in life. Moreover, it is impossible to identify among newborns a risk group for the development of late sensorineural deafness, since in many of them intrauterine CMV infection is asymptomatic [5, 18, 19].
Chorioretinitis. Retinitis develops in 10-15% of newborns with symptomatic intrauterine CMV infection. As long-term observations have shown, such children have a high probability of mental retardation in the future (almost 100%) [18, 19].
Microcephaly. Microcephaly, which occurs in 50% to 70% of symptomatic neonates, is also a predictor of delayed neurological disorders, although the risk is not as high as in retinitis.
In addition, other neurological abnormalities (hypotension, drowsiness, convulsions, weak sucking reflex) found in children during examination during the first year of life may indicate a possible mental retardation, although their diagnostic value has not been clearly established [20, 21] .
Periventricular calcification of the brain. Periventricular calcifications in the brain, which are also characteristic of intrauterine CMV infection, are detected by computed tomography in 70% of newborns with symptomatic disease. These findings are significant, since many of these children subsequently experience hearing loss or may have problems learning at school (IQ < 70 - low intelligence index when tested) [8, 20, 21].
CMV infection in newborns (intra- and postnatal infection). Like congenital, this form of CMV infection is most often asymptomatic and is accompanied by a long-term (for several years) shedding of the virus. The main source of infection is breast milk, less often intrapartum infection occurs when passing through an infected birth canal. Even more rarely (about 5%), CMV transmission is observed during the transfusion of blood components. The incubation period is 4-12 weeks.
Like congenital, this form of CMV infection is most often asymptomatic and is accompanied by a long-term (for several years) shedding of the virus. The main source of infection is breast milk, less often intrapartum infection occurs when passing through an infected birth canal. Even more rarely (about 5%), CMV transmission is observed during the transfusion of blood components. The incubation period is 4-12 weeks.
Intra- and postnatal CMV infection in term newborns is not usually associated with adverse outcomes. Premature babies can have serious problems, especially when they receive infected blood. That is why, if necessary, they should be transfused with blood previously tested for the presence of CMV [22].
Diagnosis of CMV infection
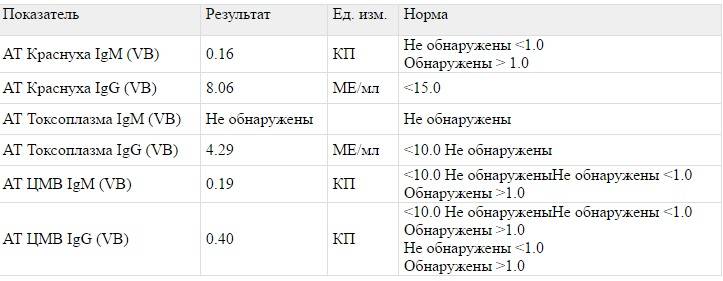
Pregnant. Since in most cases there are no clinical manifestations of CMV infection, laboratory methods of examination are of primary diagnostic value. Serological tests that detect specific IgG and IgM antibodies to CMV are currently widely used among them [7].
It is known that during pregnancy the greatest danger is the primary CMV infection, in which the risk of infection of the fetus is high. This diagnosis in the mother can only be established if IgG seroconversion is detected, i.e., when specific IgG antibodies to CMV appear, which were previously absent. A certain diagnostic value is also an increase in the titer of IgG antibodies (4 times or more). However, these changes cannot be unambiguously interpreted as a manifestation of primary infection, since they only confirm the recent activity of the infectious process, which means that they can also occur during relapses of CMV infection. The same applies to specific IgM antibodies, the presence of which, as a rule, indicates a recent or current infection. But, unfortunately, it is also impossible to differentiate between primary and recurrent infection, since in almost 25% of people during primary infection IgM antibodies to CMV are not detected, and about 10% of women during relapse, on the contrary, may be their carriers. In addition, during primary infection, IgM antibodies can persist in the blood in high titers from several weeks to many years [4], i.e., infection can occur even before the onset of pregnancy. Therefore, the detection of IgM, even in a high titer, is not the only criterion for a recent CMV infection, and a positive serological test should be considered only as one of the diagnostic steps [4, 7, 23].
In addition, during primary infection, IgM antibodies can persist in the blood in high titers from several weeks to many years [4], i.e., infection can occur even before the onset of pregnancy. Therefore, the detection of IgM, even in a high titer, is not the only criterion for a recent CMV infection, and a positive serological test should be considered only as one of the diagnostic steps [4, 7, 23].
Commercial diagnostic kits used in most laboratories to detect IgG antibodies to CMV have a fairly high sensitivity (99%) and specificity (95%). At the same time, test systems for the detection of IgM antibodies, the sensitivity of which is 75%, are less valuable due to the large number of false positive results associated with cross-reactions (with other viruses of the Herpesviridae family). In this case, the determination of IgG avidity can help in establishing the statute of limitations for CMV infection [14]. Avidity is the strength of an antigen-antibody bond. A high degree of avidity indicates that the infection most likely occurred more than 3 months ago, which may help to exclude a primary infection during pregnancy. The problem of diagnosing a primary infection can also be solved by recently developed and, therefore, serological diagnostic kits with recombinant CMV antigens, which are still little available for practical use.
The problem of diagnosing a primary infection can also be solved by recently developed and, therefore, serological diagnostic kits with recombinant CMV antigens, which are still little available for practical use.
There is another group of diagnostic tests that detect CMV antigens or DNA in the blood of pregnant women using immunological methods or polymerase chain reaction (PCR). But due to the lack of correlation between antigen-(DNA)-emia and an increased risk of intrauterine transmission of the virus, many researchers point to the low diagnostic value of these methods [7].
Another method for diagnosing CMV infection is a virological study [4], which allows the culture method to isolate the virus and type it. In the active stage, CMV can be found in urine, saliva, cervical mucus and vaginal contents, amniotic fluid, blood, and milk. Usually, the virus quickly disappears from the blood, and continues to stand out in other biological fluids for several months. In practice, virological diagnosis of CMV infection in pregnant women is used extremely rarely, since this is a long, expensive study that cannot differentiate between primary and recurrent infection.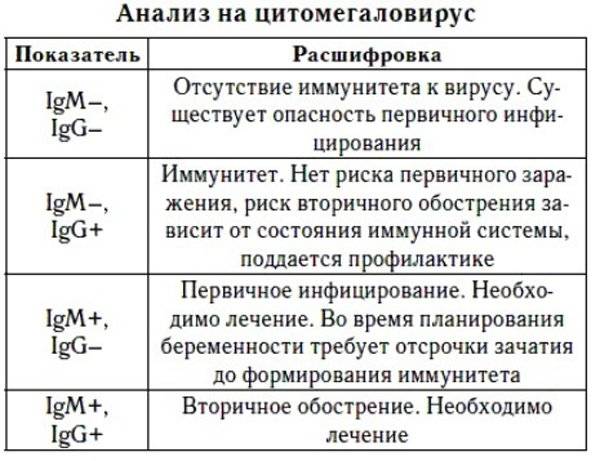 However, virus isolation is of particular interest in those situations where it is necessary to distinguish the asymptomatic form of the disease from the carriage of antibodies to CMV (for example, in newborns with suspected intrauterine CMV infection). Thus, common commercial diagnostics cannot always reliably detect pregnant women with primary CMV infection, in which the risk of intrauterine transmission of the virus is high.
However, virus isolation is of particular interest in those situations where it is necessary to distinguish the asymptomatic form of the disease from the carriage of antibodies to CMV (for example, in newborns with suspected intrauterine CMV infection). Thus, common commercial diagnostics cannot always reliably detect pregnant women with primary CMV infection, in which the risk of intrauterine transmission of the virus is high.
Fetus and newborn. Prenatal screening ultrasound examination of the fetus sometimes suggests the presence of intrauterine CMV infection during pregnancy [10]. At the same time, many or oligohydramnios, fetal growth retardation, microcephaly, hydrocephalus, hepatosplenomegaly, pseudomeconial ileus, ascites, hydrothorax and hydropericardium are often found; in more severe cases, fetal dropsy [10, 20, 21, 24]. However, these ultrasound signs are nonspecific and can occur [10, 20, 21, 24] not only in CMV infection, but also in toxoplasmosis, rubella, syphilis and other infections, as well as in some genetic diseases and metabolic disorders. In such situations, additional examination is required for differential diagnosis.
In such situations, additional examination is required for differential diagnosis.
Amniocentesis is recommended as a prenatal diagnosis of intrauterine CMV infection [25, 26]. Its results are of fundamental importance, since if symptomatic CMV infection is established in the fetus, abortion is possible for medical reasons. Due to the fact that amniocentesis is an invasive manipulation, it is necessary to compare its benefits and the risk of possible complications. Therefore, according to general recommendations, it is desirable to carry out amniocentesis in the presence of the above ultrasound signs of fetal pathology and primary CMV infection or viremia detected in the pregnant woman in the first half of pregnancy. The optimal gestational age for amniocentesis and detection of CMV in the amniotic fluid is 21 weeks of gestation. This is due to a number of circumstances:
- before this period, false-negative results are possible, since the kidneys of the infected fetus, releasing the virus into the amniotic fluid, begin to fully function only by 20-21 weeks;
- in most cases, the virus enters the amniotic fluid after 6-9 weeks from the moment of infection of the pregnant woman, and infection is most dangerous for the fetus before 12 weeks of pregnancy.
On the other hand, in countries where termination of pregnancy after 20 weeks is not allowed, amniocentesis should be performed earlier, but taking into account the lower sensitivity of the test.
PCR or virological testing is used to detect CMV in amniotic fluid. Both of these methods are quite informative, but still not without drawbacks: in the first case, the probability of overdiagnosis is high, and in the second, it is often not possible to isolate the virus.
Relatively recently, the advisability of prenatal diagnosis (amniocentesis) for all pregnant women with primary CMV infection has been discussed. The problem is that intrauterine infection, which is detected in almost 30% of the examined, does not necessarily mean the development of complications in the fetus. Thus, the question arises of how to identify fetuses at risk for developing complications associated with CMV. In clinical practice, they are usually detected during routine ultrasound examination of pregnant women.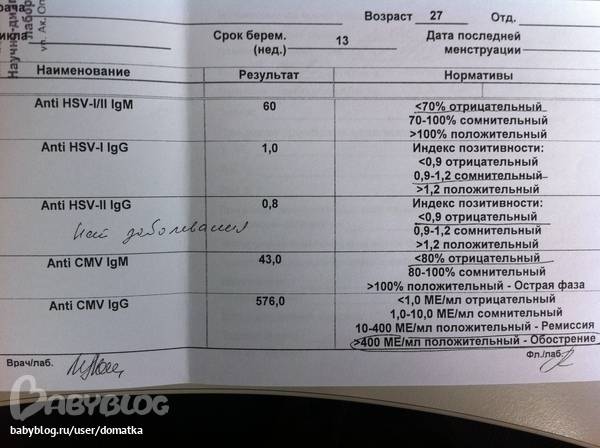 But, according to some authors [25], in many cases, ultrasound signs of intrauterine infection appear too late to allow abortion. Therefore, for the purpose of early detection of this risk group in case of established CMV infection of the fetus, they propose to determine the virus titer in the amniotic fluid by a quantitative PCR method.
But, according to some authors [25], in many cases, ultrasound signs of intrauterine infection appear too late to allow abortion. Therefore, for the purpose of early detection of this risk group in case of established CMV infection of the fetus, they propose to determine the virus titer in the amniotic fluid by a quantitative PCR method.
The serological method is considered an aid in the diagnosis of intrauterine CMV infection and is used extremely rarely. The presence of specific IgM antibodies in cord blood samples is a reliable sign of fetal infection. But with negative results, this method, having low sensitivity (20-75% depending on the diagnostics and the gestational age, since full-fledged immunity in the fetus is formed no earlier than 22 weeks), cannot exclude the possibility of intrauterine CMV infection. In addition, it should be taken into account that it is often technically difficult to perform cordocentesis [25].
The "gold standard" in the diagnosis of intrauterine CMV infection in newborns is a molecular biological urine test (PCR) during the first 3 weeks of life [19].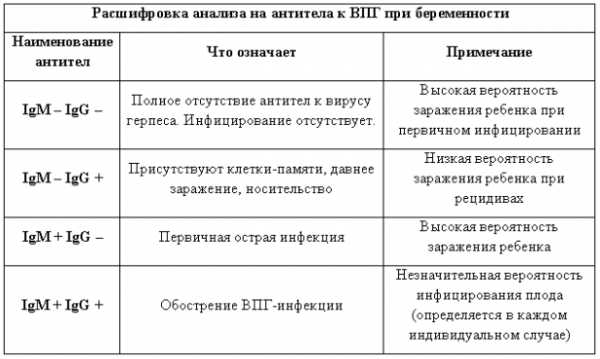 Detection by PCR of CMV DNA in the blood, urine and cerebrospinal fluid of newborns makes it possible to diagnose intrauterine infection with high reliability. The detection of specific IgM antibodies at birth has a certain diagnostic value. However, this method is considered less sensitive. In addition, for the differential diagnosis of intrauterine infection and the carriage of maternal antibodies, a repeated serological examination of the newborn is required after 4-6 months. Unfortunately, molecular biological (PCR) and serological research methods performed later than 3 weeks of life do not distinguish between intrauterine and postnatal CMV infection. In these cases, the diagnosis should rely on the clinical symptoms of the disease [19].
Detection by PCR of CMV DNA in the blood, urine and cerebrospinal fluid of newborns makes it possible to diagnose intrauterine infection with high reliability. The detection of specific IgM antibodies at birth has a certain diagnostic value. However, this method is considered less sensitive. In addition, for the differential diagnosis of intrauterine infection and the carriage of maternal antibodies, a repeated serological examination of the newborn is required after 4-6 months. Unfortunately, molecular biological (PCR) and serological research methods performed later than 3 weeks of life do not distinguish between intrauterine and postnatal CMV infection. In these cases, the diagnosis should rely on the clinical symptoms of the disease [19].
Case management
Antenatal period. There are currently no recommended treatments for primary or recurrent CMV infection during pregnancy. The exception is extremely rare severe forms of the disease (pneumonia, hepatitis, myocarditis, meningoencephalitis) in patients with immunodeficiency states.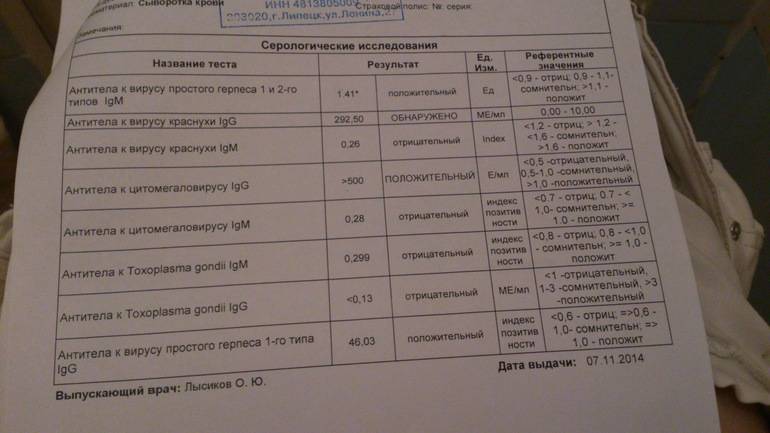 In this case, specific chemotherapy with ganciclovir, foscarnet, cidofovir is used [17, 27].
In this case, specific chemotherapy with ganciclovir, foscarnet, cidofovir is used [17, 27].
The use of drugs from the arsenal of immunotherapeutic agents (various "immunomodulators", "inducers of interferonogenesis", "nonspecific immunoglobulins", etc.) should be considered absolutely unreasonable, since there is no convincing evidence of the effectiveness of this "therapy". Active immunization of women is also impossible, since there are still no licensed CMV vaccines [28-30].
There are currently few studies on the use of cytomegalovirus hyperimmune globulin to prevent vertical transmission of CMV in women with confirmed primary CMV infection. However, these studies are not randomized, and the experience of using the drug is so small that it is not yet possible to recommend it for practical use [13, 31–34].
Termination of pregnancy is indicated before 22 weeks of gestation in case of confirmed symptomatic CMV infection in the fetus. However, in practice, the solution of this issue is extremely difficult.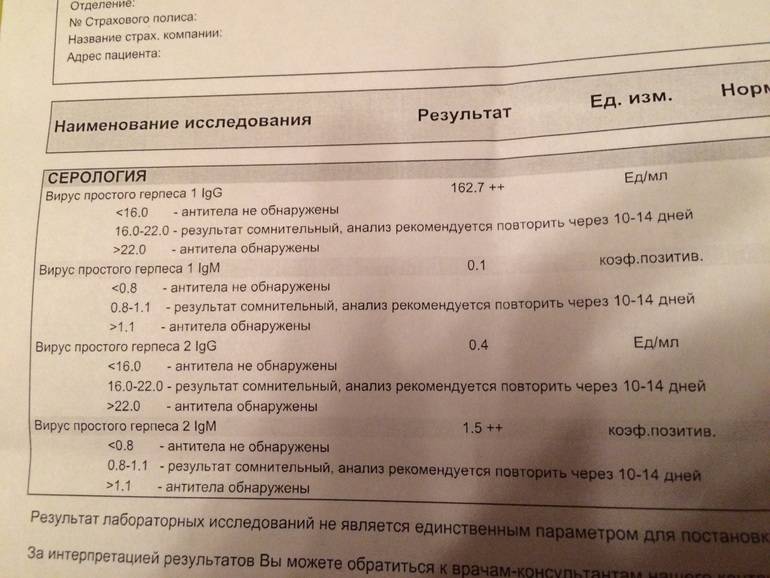 The combination of primary CMV infection in the mother in the first half of pregnancy, nonspecific ultrasound signs of fetal pathology, and positive samples during amniocentesis is extremely rare and has the character of random findings. Namely, the combination of these three parameters allows us to speak with a sufficient degree of accuracy about severe fetal pathology. In other situations, even if intrauterine infection of the fetus was established during amniocentesis, it is impossible to accurately assess the risk of developing clinically pronounced forms of the disease, since in 95% of them CMV infection is asymptomatic [13, 17, 23].
The combination of primary CMV infection in the mother in the first half of pregnancy, nonspecific ultrasound signs of fetal pathology, and positive samples during amniocentesis is extremely rare and has the character of random findings. Namely, the combination of these three parameters allows us to speak with a sufficient degree of accuracy about severe fetal pathology. In other situations, even if intrauterine infection of the fetus was established during amniocentesis, it is impossible to accurately assess the risk of developing clinically pronounced forms of the disease, since in 95% of them CMV infection is asymptomatic [13, 17, 23].
Neonatal period. There is currently no safe and effective treatment for neonatal CMV infection. Currently, a multicenter study is underway in the United States to evaluate the effectiveness of one of the antiviral drugs, ganciclovir, in the treatment of CMV infection in newborns. Preliminary evidence suggests that treatment with ganciclovir improves immediate prognosis, but it is not yet known whether antiviral therapy reduces the risk of long-term hearing loss and psychomotor impairment.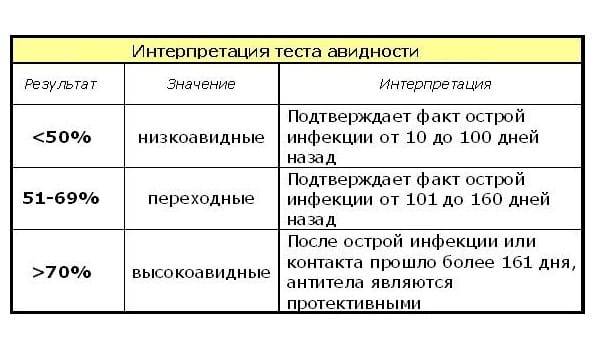 In addition, the high toxicity of ganciclovir makes it incredibly difficult to select the optimal therapeutic dose. Relatively recently, data have appeared on the possibility of passive immunization of the fetus and newborn with the help of specific CMV hyperimmunoglobulin. In addition, the prospects for the use of new-generation antiviral drugs, benzimadazole-ribonucleosides, with high bioavailability and minimal toxicity, are discussed. However, based on a small number of preliminary studies, it is not yet possible to speak about the effectiveness of this therapy [13].
In addition, the high toxicity of ganciclovir makes it incredibly difficult to select the optimal therapeutic dose. Relatively recently, data have appeared on the possibility of passive immunization of the fetus and newborn with the help of specific CMV hyperimmunoglobulin. In addition, the prospects for the use of new-generation antiviral drugs, benzimadazole-ribonucleosides, with high bioavailability and minimal toxicity, are discussed. However, based on a small number of preliminary studies, it is not yet possible to speak about the effectiveness of this therapy [13].
Prevention of CMV infection
Antenatal screening. Screening of pregnant women for CMV infection is not currently meaningful. Firstly, intrauterine infection can be observed both with primary and recurrent CMV infection in the mother, and it is extremely difficult to assess the risk of transmission of the virus to the fetus, and even more so the development of clinically pronounced forms of the disease in each case. Secondly, there is no specific therapy for intrauterine CMV infection [17].
Secondly, there is no specific therapy for intrauterine CMV infection [17].
Health education. During pregnancy, hygiene precautions are of particular importance to reduce the possible risk of CMV infection [3, 35]. These include thorough handwashing and advice to avoid contact with various biological secretions, in particular saliva and urine. Compliance with hygiene measures is especially important for those who work with children, who can often shed the virus into the environment during asymptomatic CMV infection. In the work of C. Vauloup-Fellous et al. [36] confirmed the effectiveness of sanitary and hygienic measures. In this study, 2500 seronegative women before 12 weeks of gestation were instructed on the rules of conduct to prevent CMV infection. The seroconversion rate in these pregnant women at 36 weeks of gestation was only 0.2% [36].
Nosocomial infection. There are isolated reports of nosocomial infection in newborns. This is usually associated with blood transfusion or the use of contaminated donor breast milk.