Chlamydia in pregnant women
Chlamydia and pregnancy | Pregnancy Birth and Baby
Chlamydia and pregnancy | Pregnancy Birth and Baby beginning of content3-minute read
Listen
Chlamydia is a bacterial sexually transmitted infection (STI) that affects both men and women. Chlamydia can also cause a number of issues during pregnancy.
Most people with chlamydia are unaware that they have the infection. Left untreated, chlamydia can cause serious complications including infertility and chronic pain. Chlamydia is fairly easy to treat if you know you have it — one course of antibiotics is usually enough.
Causes of chlamydia
Chlamydia is caused by an infection with the bacterium Chlamydia trachomatis. It is spread by unprotected (unsafe) vaginal or anal sex with an infected person.
Chlamydia is the most commonly reported STI in Australia.
What are the symptoms of chlamydia?
Most men and women with chlamydia have no signs or symptoms, which makes it very easy to spread. Some people have the infection for many months or years without knowing it.
Women who get symptoms may have:
- vaginal discharge
- bleeding between periods or after sex
- burning or pain when urinating
- abdominal or pelvic pain
- pain during sex
Men who get symptoms may have some clear discharge from the penis or pain during urination.
In rare cases, people with chlamydia have sore joints (arthritis) or inflammation of the eye (uveitis).
Diagnosing chlamydia
Chlamydia is easily diagnosed. Your doctor may take a sample from the vagina, cervix, anus or penis, and may ask for a urine test. These are sent to a laboratory for testing.
If you think you or your partner have chlamydia, see your doctor or sexual health clinic so you can both be tested. It is important that any sexual partners of people with chlamydia are tested, even if they don’t have symptoms.
It is important that any sexual partners of people with chlamydia are tested, even if they don’t have symptoms.
Treating chlamydia
Treatment for chlamydia is a course of antibiotics. It is important to avoid sex until the full course of treatment is finished, and for at least a week following. You should have another test 3 months after you are treated.
If you have chlamydia, all of your sexual partners should be informed, tested and treated, as they may be infected and can infect you, and others, again after treatment.
If your partner has had a positive test for chlamydia, you should be treated even if you have had a negative test result. As chlamydia infection increases the possibility of contracting other infections, it is important to be tested for other STIs such as gonorrhoea, hepatitis, HIV and syphilis. Using latex condoms and a water-based lubricant is the most effective way to prevent STIs. People who have chlamydia for long periods without treatment risk becoming infertile or developing arthritis. Women can get pelvic inflammatory disease, and men can get epididymitis (a painful infection near the testicle).
Women can get pelvic inflammatory disease, and men can get epididymitis (a painful infection near the testicle).
Chlamydia complications
If chlamydia isn't treated properly, it can cause serious complications. People who have chlamydia for long periods without treatment risk becoming infertile or developing arthritis.
For women, chlamydia can spread into the uterus and fallopian tubes, causing pelvic inflammatory disease. Pelvic inflammatory disease can lead to ectopic pregnancies, chronic pelvic pain and infertility.
In men, chlamydia can cause epididymitis (a painful infection near the testicle) or spread to the prostate gland, and the tubes that carry sperm, which may result in chronic pain and/or fertility problems.
Both men and women can develop arthritis, eye inflammation and inflammation of the rectum.
Chlamydia and pregnancy
Because of this, doctors recommend that pregnant women under the age of 30 should be screened for chlamydia.
Pregnant women who are infected with chlamydia have an increased risk of their waters breaking prematurely, causing the baby to be born early.
If a woman has chlamydia when giving birth, the baby might become infected during delivery. These babies can develop an eye infection (conjunctivitis) or pneumonia, and might need antibiotics. Chlamydia has also been associated with low birthweight.
The antibiotics used to treat chlamydia are safe in pregnancy and are used in pregnant women for many other types of infections.
Sources:
Australian Sexual Health Alliance (STI Management Guidelines for use in primary care; Chlamydia), King Edward Memorial Hospital Women and Newborn Health Service (Chlamydia clinical practice guideline), Lab Tests Online AU (Chlamydia), Melbourne Sexual Health Centre (National Management Guidelines for Sexually Transmissible Infections - Chlamydia), NSW Health (Chlamydia fact sheet)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: November 2020
Back To Top
Related pages
- Routine antenatal tests
- Antenatal care during your pregnancy
Need more information?
Chlamydia - MyDr.com.au
Chlamydia is a sexually transmitted infection (STI). It affects both men and women, and it's spread by having sex with a person who has the infection.
Read more on myDr website
Chlamydia - Better Health Channel
Chlamydia is often called the 'silent infection' because most people do not realise they have it.
Read more on Better Health Channel website
Chlamydia fact sheet - Fact sheets
Chlamydia is a sexually transmissible infection. Many people who are infected do not have symptoms of infection but can still spread the disease. Chlamydia can lead to infertility, and other complications if not treated.
Many people who are infected do not have symptoms of infection but can still spread the disease. Chlamydia can lead to infertility, and other complications if not treated.
Read more on NSW Health website
Chlamydia | Family Planning NSW
Chlamydia is a common sexually transmitted infection (STI) caused by a bacteria. It affects both men and women. Most people with chlamydia do not have symptoms. This means you can pass the infection to a partner without knowing it. Having a regular sexual health check-up can help you find out if you have chlamydia.
Read more on Family Planning NSW website
Chlamydia treatment for your partner - Play Safe
Did you know it’s possible for your partner to get treated for Chlamydia without ever having to see a GP or go to a sexual health clinic? This is known as Patient Delivered Partner Therapy (PDPT)
Read more on NSW Health website
The facts about Chlamydia, what it is, how to prevent it, and how to treat it
Chlamydia is on the rise in Australia and it’s the most important thing for young people to test for.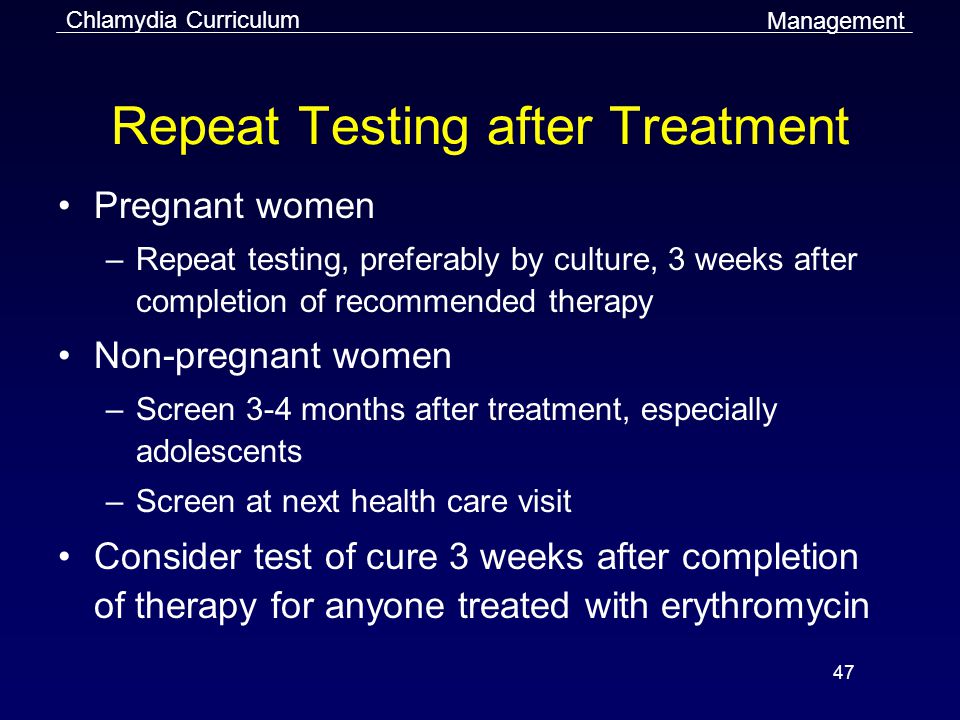 It often doesn’t have any symptoms which means that it’s easy to miss without regular STI testing.
It often doesn’t have any symptoms which means that it’s easy to miss without regular STI testing.
Read more on NSW Health website
Trachoma - Eye Infection
Trachoma is a preventable eye condition caused by repeated infections with eye strains of the bacterium Chlamydia trachomatis that lead to a roughening of the inner surface of the eyelid.
Read more on Queensland Health website
Gonorrhoea | Family Planning NSW
Gonorrhoea is a bacterial sexually transmitted infection (STI). It is spread through vaginal, anal or oral sex, or by the fingers and hands from the genitals to the eyes. It is less common in the general community than other STIs such as chlamydia.
Read more on Family Planning NSW website
Sexually transmitted infections (STIs) | Healthy Male
A sexually transmitted infection (STI) is an infection you get or give during sexual activity. STIs can be caused by viruses (e.g., human immunodeficiency virus, herpes), bacteria (e.g., gonorrhea, syphilis), or parasites (e.g., pubic lice).
STIs can be caused by viruses (e.g., human immunodeficiency virus, herpes), bacteria (e.g., gonorrhea, syphilis), or parasites (e.g., pubic lice).
Read more on Healthy Male - Andrology Australia website
STIs and pregnancy
Sexually transmitted infections (STIs), if left untreated, can cause serious problems for both mother and child.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Chlamydia During Pregnancy - American Pregnancy Association
Navigating pregnancy is difficult enough, but the addition of having a sexually transmitted infection (STI) like chlamydia during pregnancy can add more stress. If you think you may have an STI during your pregnancy, it is crucial that you talk to your healthcare provider and get tested right away. If you think you may have (or have already been diagnosed with chlamydia during your pregnancy), you probably have a lot of questions about how the infection could affect your baby and your prenatal care. Answers to all these questions are presented below!
If you think you may have (or have already been diagnosed with chlamydia during your pregnancy), you probably have a lot of questions about how the infection could affect your baby and your prenatal care. Answers to all these questions are presented below!
Chlamydia is a bacterial infection and is the most commonly reported bacterial STI. It is often symptomless, making it difficult to diagnose without running tests. The Centers for Disease Control (CDC) suggests that all pregnant women be screened at their first prenatal visit, and additionally if any symptoms appear or if risk factors are present.
The CDC estimates that there are 2.86 million infections each year in the USA, with some individuals accounting for multiple cases.
What are the symptoms of chlamydia during pregnancy?
In most cases, there are no symptoms. Some women may experience vaginal discharge and/or pelvic or abdominal pain.
Males usually have pain while urinating and may have a discharge from the penis. If you are pregnant and you notice your partner is experiencing these symptoms, you should both be screened for STIs like chlamydia.
If you are pregnant and you notice your partner is experiencing these symptoms, you should both be screened for STIs like chlamydia.
Am I at risk for contracting chlamydia during my pregnancy?
Anyone who is sexually active (outside of a monogamous relationship where you both have not had previous sexual partners) is at risk for contracting chlamydia via vaginal, anal, or oral sex.
You have the highest risk of contracting chlamydia during your pregnancy if you are sexually active and:
- Have multiple sexual partners,
- Have sex without a condom,
- Have had a previous or current STI, and/or
- Have a partner with an STI.
How will chlamydia affect my pregnancy?
The largest risk to the fetus is if the infection goes untreated. The CDC suggests that all pregnant women be tested at the first prenatal appointment.
If you are at a higher risk for contracting STIs during your pregnancy (i.e. have a new sexual partner or multiple partners), an additional test should be done in the third trimester so that treatment can be started before delivery.
If you have an active or untreated chlamydia infection during delivery, the baby has a chance of contracting the infection that will affect the baby in one of two ways: chlamydial conjunctivitis (18-44% of cases) or chlamydial pneumonia (3-16%).
The CDC also states that an active chlamydia infection during pregnancy increases the risk of preterm delivery.
Can my baby get chlamydia from me?
Yes, chlamydia may be spread from mother to child during birth (perinatal transmission).
The best way to prevent passing chlamydia to your baby during birth is to clear the infection before you are due. This is why first and third trimester screenings are so important, as well as reporting any new symptoms to your doctor.
How is chlamydia diagnosed?
Chlamydia may be diagnosed by your healthcare provider using a lab test to assess the secretions from the infected area which may include the cervix, urethra, anus, or throat. The lab may also use a urine sample for testing.
How is chlamydia treated during pregnancy?
Chlamydia may be treated and cured with antibiotics administered orally. This may be either a single dose or a 7-day course. The antibiotics used are typically safe during pregnancy.
If you continue seeing symptoms after a few days into the antibiotic treatment, you should return to your doctor for another evaluation. The CDC suggests that pregnant women who are treated for chlamydia infection should be retested at 3 weeks and 3 months post-treatment since reinfection is somewhat common.
How can I prevent getting chlamydia during pregnancy?
There are only two 100% effective ways to prevent chlamydia. The first is to refrain from sexual contact of any kind. The second is to be in a long-term monogamous relationship such as marriage in which both of you test negative for STIs.
According to the Sexuality Information and Education Council of the United States (SIECUS), the consistent and correct use of condoms can decrease the risk of contracting chlamydia during vaginal, oral, or anal intercourse by only 60%.
Compiled using information from the following sources:
1. Centers for Disease Control and Prevention (CDC)
https://www.cdc.gov/std/chlamydia/stdfact-chlamydia-detailed.htm
2. Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/chlamydia-trachomatis/symptoms-causes/dxc-20315310
3. Sexuality Information and Education Council of the United States (SIECUS)
Chlamydia and pregnancy
Their favorite habitat is the cervix (more precisely, the mucous membrane of the cervical canal). It is there that they are located in colonies, i.e. are not found throughout. Such frequent cases are associated with this fact, when one doctor takes a smear from the cervical canal and chlamydia is found in it, and the other one also takes a smear a day later, but chlamydia is not found again. That is why the diagnostic value of swabs for chlamydia is quite low - about 30%.
How chlamydia manifests itself
During an exacerbation of the infectious process, women's complaints may be different, depending on the level of chlamydia spread.
When chlamydia is found in the cervix, there may be slight discharge from the vagina, accompanied by moderate pulling pains in the lower abdomen, which is typical with local exacerbation of the process (there are practically no complaints in the chronic form). If the infection spreads higher (uterine cavity, tubes), then the complaints are more pronounced, because, for example, inflammation of the appendages may begin.
Exacerbation of chlamydial infection is especially dangerous during pregnancy, as it can lead to various complications.
Possible complications:
- early miscarriages are possible,
- late term premature amniotic fluid and preterm labor,
- in childbirth, there is a high probability of infection of the fetus (conjunctivitis, pharyngitis, otitis and even pneumonia).
Chlamydia diagnostics
The most informative method is a blood test for antibodies (immunoglobulins) to chlamydia. If a small concentration of these antibodies is detected, then they speak of a chronic carriage of chlamydia. If the concentration is high, there is an exacerbation of chlamydial infection.
If a small concentration of these antibodies is detected, then they speak of a chronic carriage of chlamydia. If the concentration is high, there is an exacerbation of chlamydial infection.
The diagnosis of "chlamydia" is legitimate when it is confirmed by two fundamentally different diagnostic methods: smear (microscopy) and blood for antibodies to chlamydia (biochemical method). Only when the titer (concentration) of antibodies is high and / or in the presence of complaints specific to this infection, a course of treatment is indicated.
Digits must be multiples, i.e. more or less than twice, from the previous one (IgA 1:40 and IgG 1:80). Titers of 1:5 and less are doubtful and negative. Elevated IgG numbers indicate that the process is chronic. In this case, treatment is indicated if there are certain complaints, or if before that, the person has never been treated for this infection. High numbers of IgA are mainly found in an acute process (primary infection) or during an exacerbation of a chronic one that needs treatment.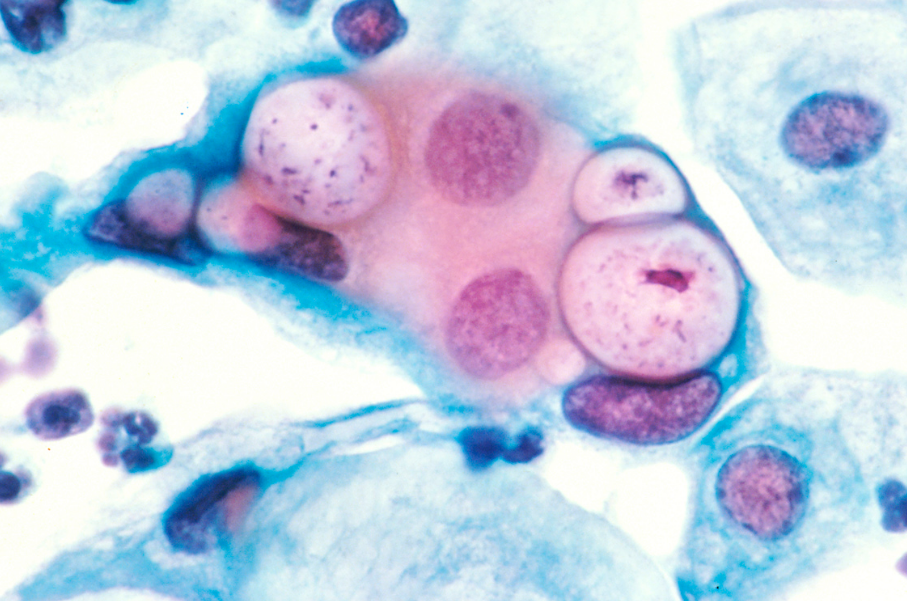
What to do if the test is positive?
It must be remembered that today there are almost no 100% reliable methods, including the ELISA method (enzymatic immunoassay) is no exception. Quite often there are “false positive” results - you have to do either repeated tests or use other, fundamentally different methods.
These can be:
- taking smears for the PIF method (examination with a luminescent microscope) - where there may also be “false positive” answers,
- PCR blood test (based on the principle of genetic engineering, the study of DNA or its fragments) - today, its reliability is very high.
In the search for the truth of the diagnosis, quite often, everything can rest either on the financial capabilities of patients, or on the insufficient equipment of a particular laboratory. The better the body's defenses, the less likely it is to contract chlamydia. In which case, only “carriage” threatens you, it is not dangerous for you (only IgG, in low titers, will be determined in the blood test).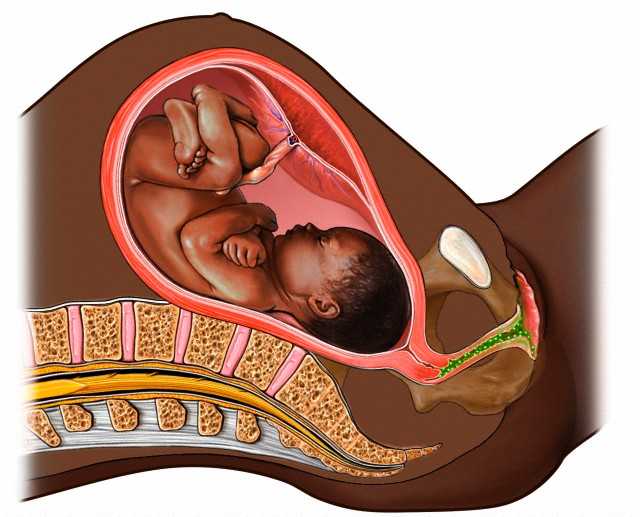
It is considered optimal if the whole family is examined at the same time (all interested persons, including children), because in this case, it is possible to identify who is at what stage and monitor the effectiveness of treatment.
In most cases, the pathogens of ureplasmosis and mycoplasmosis do not manifest themselves (hidden bacteriocarrier), and only when the process is exacerbated, they cause pregnancy complications similar to chlamydia and infection of the fetus. Therefore, when examining women who have had the above problems in the past, swabs and blood are taken at least immediately for these three pathogens. By the way, studies have shown that taking hormonal birth control pills reduces the risk of chlamydia infection, this effect is associated with an increase in the protective properties of cervical mucus (its permeability to bacteria decreases). As mentioned above, chlamydia is dangerous for pregnant women.
What to do?
But what to do if, after all, doctors found chlamydia in the acute stage in the expectant mother?
The placenta can be thought of as a mesh filter through which large molecules cannot pass (they remain in the mother's body). Therefore, in the treatment of a pregnant woman, antibiotics are used that are harmless to the fetus (i.e. those that do not pass through the placenta). These include drugs whose molecular weight is greater than the "capacity" of the capillaries. However, when taking these drugs, the effect on the fetus is still possible. The antibiotic acts primarily on the mother's body, however, during the period of treatment, it changes the metabolism in the body, which in turn affects the metabolism of the fetus. Antibiotics are always prescribed in short courses so that the effects are minimal.
Therefore, in the treatment of a pregnant woman, antibiotics are used that are harmless to the fetus (i.e. those that do not pass through the placenta). These include drugs whose molecular weight is greater than the "capacity" of the capillaries. However, when taking these drugs, the effect on the fetus is still possible. The antibiotic acts primarily on the mother's body, however, during the period of treatment, it changes the metabolism in the body, which in turn affects the metabolism of the fetus. Antibiotics are always prescribed in short courses so that the effects are minimal.
References
- Zofkie AC., Fomina YY., Roberts SW., McIntire DD., Nelson DB., Adhikari EH. Effectiveness of Chlamydia Trachomatis expedited partner therapy in pregnancy. // Am J Obstet Gynecol - 2021 - Vol - NNULL - p.; PMID:33894150
- Zofkie AC., Fomina YY., Roberts SW., McIntire DD., Nelson DB., Adhikari EH. Effectiveness of Chlamydia Trachomatis expedited partner therapy in pregnancy.
 // Am J Obstet Gynecol - 2021 - Vol - NNULL - p.; PMID:33894147
// Am J Obstet Gynecol - 2021 - Vol - NNULL - p.; PMID:33894147 - Shilling HS., Garland SM., Costa AM., Marceglia A., Fethers K., Danielewski J., Murray G., Bradshaw C., Vodstrcil L., Hocking JS., Kaldor J., Guy R., Machalek D.A. Chlamydia trachomatis and Mycoplasma genitalium prevalence and associated factors among women presenting to a pregnancy termination and contraception clinic, 2009-2019. // Sex Transm Infect - 2021 - Vol - NNULL - p.; PMID:33782146
- Vercruysse J., Mekasha S., Stropp LM., Moroney J., He X., Liang Y., Vragovic O., Valle E., Ballard J., Pudney J., Kuohung W., Ingalls RR. Chlamydia trachomatis Infection, when Treated during Pregnancy, Is Not Associated with Preterm Birth in an Urban Safety-Net Hospital. // Infect Dis Obstet Gynecol - 2020 - Vol2020 - NNULL - p.8890619; PMID:33082702
- Olaleye AO., Babah OA., Osuagwu CS., Ogunsola FT., Afolabi BB. Sexually transmitted infections in pregnancy - An update on Chlamydia trachomatis and Neisseria gonorrhoeae.
 // Eur J Obstet Gynecol Reprod Biol - 2020 - Vol255 - NNULL - p.1-12; PMID:33059307
// Eur J Obstet Gynecol Reprod Biol - 2020 - Vol255 - NNULL - p.1-12; PMID:33059307 - Hoenderboom BM., van Bergen JEAM., Dukers-Muijrers NHTM., Götz HM., Hoebe CJPA., de Vries HJC., van den Broek IVF., de Vries F., Land JA., van der Sande MAB., Morré SA., van Benthem BHB. Pregnancies and Time to Pregnancy in Women With and Without a Previous Chlamydia trachomatis Infection. // Sex Transm Dis - 2020 - Vol47 - N11 - p.739-747; PMID:32701764
- He W., Jin Y., Zhu H., Zheng Y., Qian J. Effect of Chlamydia trachomatis on adverse pregnancy outcomes: a meta-analysis. // Arch Gynecol Obstet - 2020 - Vol302 - N3 - p.553-567; PMID:32643040
- Freeman J., Pettit J., Howe C. Chlamydia test-of-cure in pregnancy. // Can Fam Physician - 2020 - Vol66 - N6 - p.427-428; PMID:32532724
- Rajabpour M., Emamie AD., Pourmand MR., Goodarzi NN., Asbagh FA., Whiley DM. Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis among women with genitourinary infection and pregnancy-related complications in Tehran: A cross-sectional study.
 // Int J STD AIDS - 2020 - Vol31 - N8 - p.773-780; PMID:32517577
// Int J STD AIDS - 2020 - Vol31 - N8 - p.773-780; PMID:32517577 - Goggins ER., Chamberlain AT., Kim TG., Young MR., Jamieson DJ., Haddad LB. Patterns of Screening, Infection, and Treatment of Chlamydia trachomatis and Neisseria gonorrhea in Pregnancy. // Obstet Gynecol - 2020 - Vol135 - N4 - p.799-807; PMID:32168225
Chlamydia - KVD №2
What is chlamydia?
Chlamydia is a common sexually transmitted infection (STI). The disease is caused by the bacterium Chlamydia trachomatis (Chlamydia trachomatis), which affects the female genital area and is the cause of non-gonococcal urethritis in men. Manifestations of chlamydia are usually minor or absent, but serious complications develop. Complications can cause irreparable damage to the body, including infertility - all this proceeds very secretly.
Chlamydia also causes penile discharge in infected men.
Ways of transmission of chlamydia
Chlamydia can be transmitted through:
- vaginal or anal contact with an infected partner;
- less common with oral sex;
- use of sex toys with an infected partner;
- infection of a newborn during childbirth from a sick mother.

Absolutely all sexually active people can get chlamydia. The greater the number of sexual partners, the greater the risk of infection. The risk of infection is especially high in girls, because their cervix is not fully formed. About 75% of new cases occur in women under 25 years of age. By the age of 30, approximately 50% of sexually active women have had chlamydia. In sexually active men, the risk of infection is highest between the ages of 20 and 24.
You cannot get chlamydia through kisses, hugs, dishes, baths, towels.
Manifestations of chlamydia
Chlamydia is very secretive. About 75% of infected women and 50% of infected men are asymptomatic. If manifestations of the disease develop, then this occurs approximately 1 to 3 weeks after infection.
In women, chlamydia first affects the cervix and urethra (urinary canal).
Manifestations:
- unusual vaginal discharge;
- pain or discomfort when urinating;
If the infection penetrates to the appendages, manifestations are possible:
- pain in the lower abdomen;
- pain in the lumbar region;
- nausea;
- slight increase in temperature;
- pain during intercourse or bleeding after it;
- bleeding between periods.

Symptoms in men:
- clear or cloudy discharge from the penis;
- pain or discomfort when urinating;
- there may be burning and itching in the area of the outlet of the urethra;
- rarely pain and/or swelling of the testicles.
Men or women who have anal sex with an infected partner can infect the rectum, resulting in inflammation, pain, discharge, or bleeding from the rectum.
Chlamydia can cause sore throat (pharyngitis) in men and women who have oral contact with an infected partner.
What complications can develop if chlamydia is not treated?
If the disease is not treated, serious short-term and persistent complications develop. Like the disease itself, complications often occur insidiously.
In women with untreated chlamydia, the infection can spread from the urethra to the fallopian tubes (the tubes that carry the egg from the ovaries to the uterus) - this causes (in 40% of cases) the development of pelvic inflammatory disease (PID).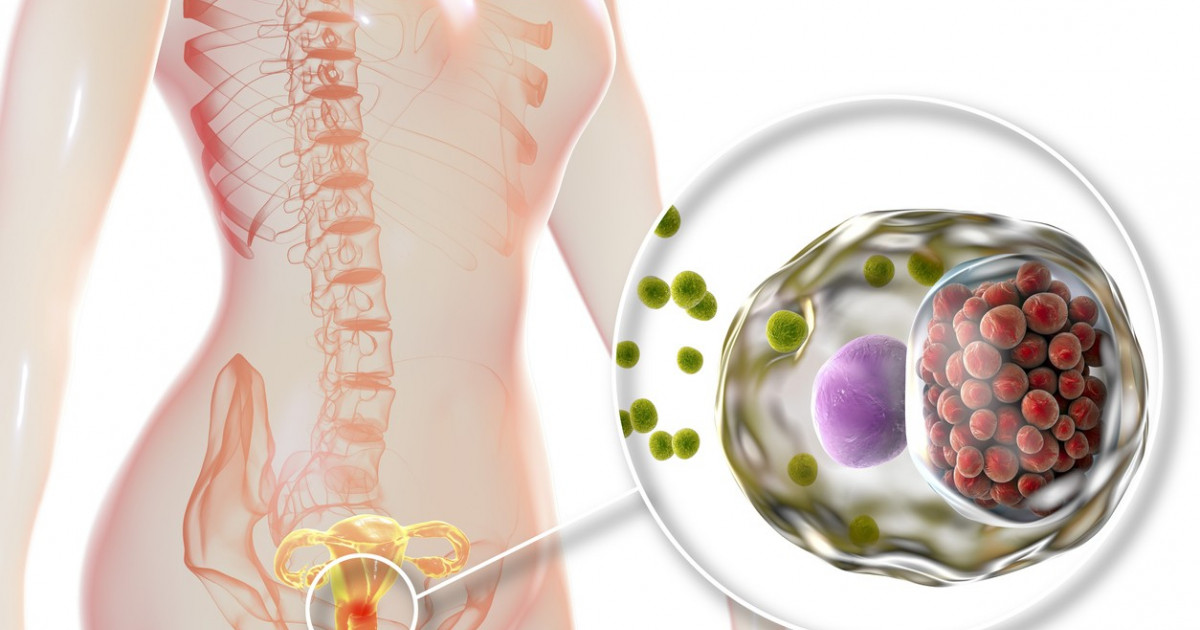 PID causes permanent damage to the fallopian tubes, uterus, and surrounding tissues. Chronic pelvic pain, infertility and ectopic pregnancy are the result of PID.
PID causes permanent damage to the fallopian tubes, uterus, and surrounding tissues. Chronic pelvic pain, infertility and ectopic pregnancy are the result of PID.
Women with chlamydia are more susceptible to HIV infection, the risk increases by almost 5 times.
To prevent serious consequences of chlamydia, an annual chlamydia screening is required for all sexually active women 25 years of age and younger. An annual examination is necessary for women over 25 who are at risk (new sexual partner, multiple sexual partners). All pregnant women should be screened for chlamydia.
Complications of chlamydia are rare in men. The infection sometimes extends to the epididymis and causes pain, fever, and, rarely, male infertility (sterility).
Rarely, chlamydial infection can cause inflammation of the joints in combination with skin lesions, inflammation of the eyes and urinary tract - this is the so-called Reiter's syndrome.
The effect of chlamydia on a pregnant woman and her child
Chlamydia in pregnant women increases the risk of miscarriage, premature detachment of the placenta. Newborns from infected mothers can get eye and lung infections. A lung infection (pneumonia) can be fatal to a newborn.
Newborns from infected mothers can get eye and lung infections. A lung infection (pneumonia) can be fatal to a newborn.
Diagnosis of chlamydia
Diagnosis includes observation of the patient's clinical symptoms, testing for chlamydia smears from the cervix, scraping from the urinary canal, the first morning portion of urine. Most often, the study is carried out by PCR (polymerase chain reaction). Swabs and scrapings may cause minor discomfort.
Additionally, a blood test is performed by ELISA (enzyme-linked immunosorbent assay) for the presence of immunity to chlamydia, this auxiliary test often helps to establish an accurate diagnosis.
Treatment of chlamydia
Treatment of chlamydia is with oral antibiotics. To prevent re-infection, all sexual partners must be found, examined and treated. Patients with chlamydia should refrain from unprotected sex during treatment, otherwise it is possible to re-infect the sexual partner. Unfortunately, after successful treatment, re-infection with chlamydia is possible, since a strong immunity to this microorganism does not develop. Repeated infection of women with chlamydia leads to a significant increase in the risk of serious complications, including infertility. A re-examination is carried out 4 weeks after treatment.
Repeated infection of women with chlamydia leads to a significant increase in the risk of serious complications, including infertility. A re-examination is carried out 4 weeks after treatment.
Chlamydia prevention
The best way to prevent sexually transmitted infections is through long-term sexual contact with one healthy sexual partner. Latex male condoms, when used correctly, drastically reduce the risk of transmission.
Annual chlamydia screening required for all sexually active women aged 25 and under. An annual examination is also necessary for women over 25 who are at risk (new sexual partner, multiple sexual partners). All pregnant women should be screened for chlamydia.
Any manifestations, such as pain or discomfort when urinating, unusual rash, discharge are a signal to stop sexual intercourse and immediately examine in a specialized clinic - KVD. If the patient is found to have chlamydia (or any other STI), he must inform his sexual partners so that they also undergo a full examination and appropriate treatment.