Child with small bumps on skin
What are those bumps on my child's skin?
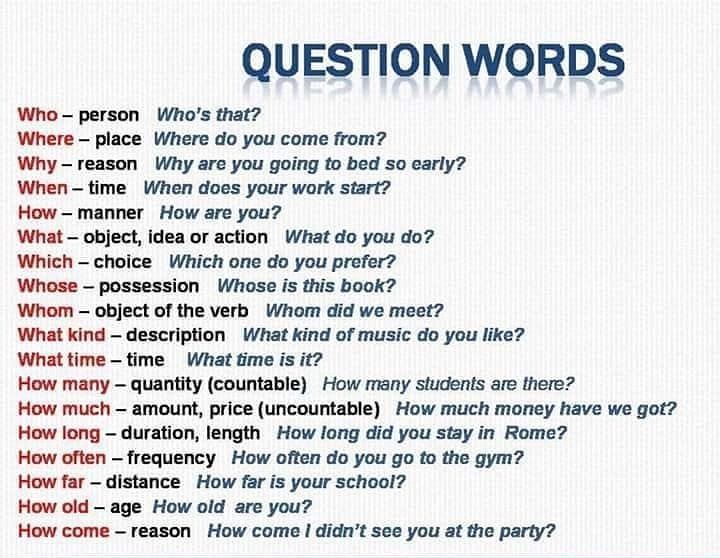
Diseases & conditions
- Coronavirus Resource Center
- Acne
- Eczema
- Hair loss
- Psoriasis
- Rosacea
- Skin cancer
- A to Z diseases
- A to Z videos
- DIY acne treatment
- How dermatologists treat
- Skin care: Acne-prone skin
- Causes
- Is it really acne?
- Types & treatments
- Childhood eczema
- Adult eczema
- Insider secrets
- Types of hair loss
- Treatment for hair loss
- Causes of hair loss
- Hair care matters
- Insider secrets
- What is psoriasis
- Diagnosis & treatment
- Skin, hair & nail care
- Triggers
- Insider secrets
- What is rosacea
- Treatment
- Skin care & triggers
- Insider secrets
- Types and treatment
- Find skin cancer
- Prevent skin cancer
- Raise awareness
- Español
Featured
How Natalie cleared her adult acneNatalie tried many acne products without success. Find out how a board-certified dermatologist helped Natalie see clear skin before her wedding.
JAK inhibitors are helping patients with alopecia areata, eczema/atopic dermatitis, psoriasis, and vitiligo. Here’s what you need to know.
Everyday care
- Skin care basics
- Skin care secrets
- Injured skin
- Itchy skin
- Sun protection
- Hair & scalp care
- Nail care secrets
- Basic skin care
- Dry, oily skin
- Hair removal
- Tattoos and piercings
- Anti-aging skin care
- For your face
- For your skin routine
- Preventing skin problems
- Bites & stings
- Burns, cuts, & other wounds
- Itch relief
- Poison ivy, oak & sumac
- Rashes
- Shade, clothing, and sunscreen
- Sun damage and your skin
- Aprenda a proteger su piel del sol
- Your hair
- Your scalp
- Nail care basics
- Manicures & pedicures
Featured
Practice Safe SunEveryone's at risk for skin cancer. These dermatologists' tips tell you how to protect your skin.
These dermatologists' tips tell you how to protect your skin.
Find out what may be causing the itch and what can bring relief.
Darker Skin Tones
- Skin care secrets
- Hair care
- Hair loss
- Diseases & Conditions
- Acne
- Dark spots
- Dry skin
- Light spots
- Razor bumps
- Caring for Black hair
- Scalp psoriasis
- Weaves & extensions
- Central centrifugal cicatricial alopecia
- Frontal fibrosing alopecia
- Hairstyles that pull can cause hair loss
- Acanthosis nigricans
- Acne keloidalis nuchae
- Hidradenitis suppurativa
- Keloid scars
- Lupus and your skin
- Sarcoidosis and your skin
- Skin cancer
- Vitiligo
- More diseases & conditions
Featured
Fade dark spotsFind out why dark spots appear and what can fade them.
If you have what feels like razor bumps or acne on the back of your neck or scalp, you may have acne keloidalis nuchae. Find out what can help.
Cosmetic treatments
- Your safety
- Age spots & dark marks
- Cellulite & fat removal
- Hair removal
- Scars & stretch marks
- Wrinkles
- Younger-looking skin
Featured
Laser hair removalYou can expect permanent results in all but one area. Do you know which one?
Do you know which one?
If you want to diminish a noticeable scar, know these 10 things before having laser treatment.
BotoxIt can smooth out deep wrinkles and lines, but the results aren’t permanent. Here’s how long botox tends to last.
Public health programs
- Skin cancer awareness
- Free skin cancer screenings
- Kids' camp
- Good Skin Knowledge
- Shade Structure grants
- Skin Cancer, Take a Hike!™
- Awareness campaigns
- Flyers & posters
- Get involved
- Lesson plans and activities
- Community grants
Featured
Free materials to help raise skin cancer awarenessUse these professionally produced online infographics, posters, and videos to help others find and prevent skin cancer.
Free to everyone, these materials teach young people about common skin conditions, which can prevent misunderstanding and bullying.
Find a dermatologist
- Find a dermatologist
- What is a dermatologist?
- FAAD: What it means
- How to select a dermatologist
- Telemedicine appointments
- Prior authorization
- Dermatologists team up to improve patient care
Featured
Find a DermatologistYou can search by location, condition, and procedure to find the dermatologist that’s right for you.
A dermatologist is a medical doctor who specializes in treating the skin, hair, and nails. Dermatologists care for people of all ages.
Molluscum Contagiosum in Children | Cedars-Sinai
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is molluscum contagiosum in children?
Molluscum contagiosum is a viral skin disease that causes small pink or skin-colored bumps on your child’s skin. It is not harmful and usually does not have any other symptoms. The virus is inside the bumps and is mildly contagious. These bumps usually clear over time.What causes molluscum contagiosum in a child??
Molluscum contagiosum is caused by a virus called the poxvirus. It is very common in children and adolescents.Which children are at risk for molluscum contagiosum?
Children can get molluscum contagiosum by skin-to-skin contact with a person who has it. The problem is found worldwide but is thought to be more common in hot, humid environments.What are the symptoms of molluscum contagiosum in a child?
The bumps are small and are usually pink or skin-colored. Eventually, the bumps tend to have a small sunken center. The bumps can show up alone or in clusters. They are not harmful, but they may make your child feel self-conscious if they appear on the face or other visible areas.How is molluscum contagiosum diagnosed in a child?
The bumps are unique and are usually diagnosed on physical exam. The healthcare provider will also take your child’s health history. Additional tests are not routinely ordered.How is molluscum contagiosum treated in a child?
Treatment will depend on your child's symptoms, age, and general health. It will also depend on how severe the condition is.
In most cases, the bumps will heal without treatment over a period of 6 to 12 months. The virus can last up to 4 years and leave scars. Additional treatment choices may include:
- Removing the bumps by freezing them, using lasers, or cutting them out with a special instrument
- Using medicines on the skin to help the bumps go away faster
Some treatments sold on the Internet may not work and may be harmful, according to the CDC. For your child’s safety, talk with your child's healthcare provider before trying any alternative treatments.
What can I do to prevent molluscum contagiosum in my child?
The virus inside the bump is only mildly contagious. It can be spread to other children who directly touch the bumps. The best prevention is to avoid contact with the bumps.How can I help my child live with molluscum contagiosum?
The virus will gradually disappear on its own.When should I call my child’s healthcare provider?
If you think your child has molluscum contagiosum, talk with your child’s healthcare provider about treatment choices.Key points about molluscum contagiosum in children
- Molluscum contagiosum is a viral skin disease that causes small pink or skin-colored bumps on your child’s skin.
- It is not harmful, does not have any other symptoms, and is only mildly contagious.
- It is very common in children and adolescents.
- In most cases, the bumps will heal without treatment over a period of 6 to 12 months.
- You should discuss treatment options with your child’s healthcare provider.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
- Know the reason for the visit and what you want to happen.
- Before your visit, write down questions you want answered.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
- Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
- Ask if your child’s condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if your child does not take the medicine or have the test or procedure.
- If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
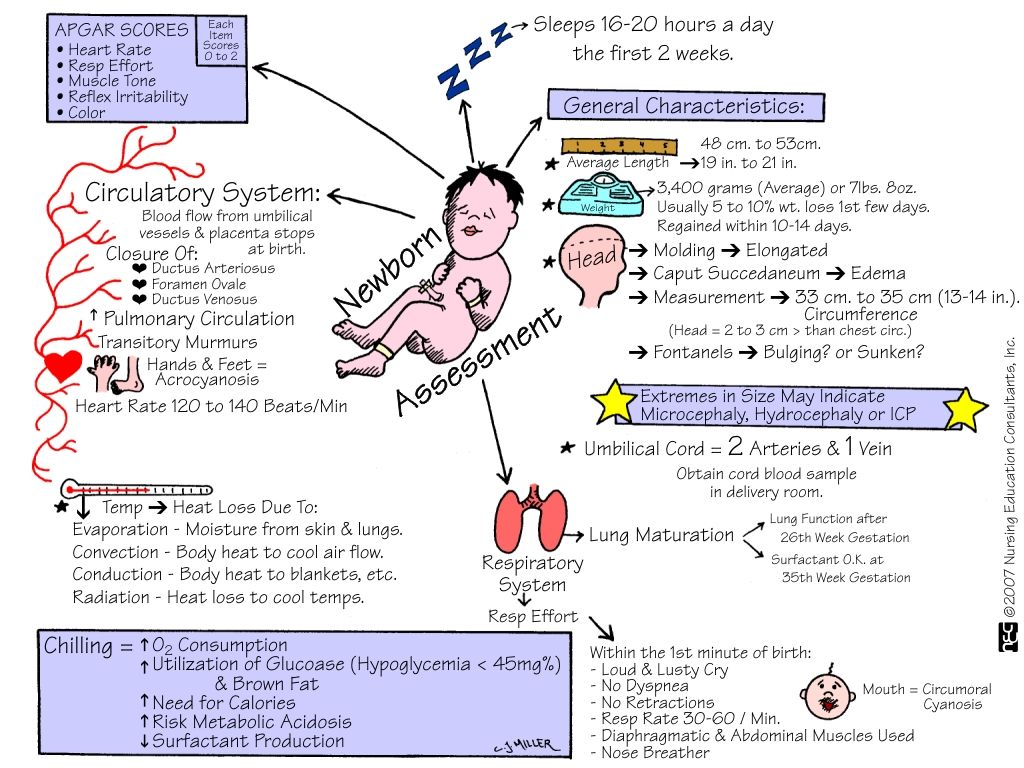
Cephalhematoma in newborns - GBUZ YNAO
It only seems that when the baby is born, the baby slowly and leisurely leaves the mother's womb. In fact, in order to be born, the child has to make corkscrew, pendulum and other active movements of the body. Therefore, in the process of passing through the birth canal, the baby often gets injured.
Neonatal cephalohematoma refers to birth trauma to the head and is a small tumor that occurs as a result of rupture of blood vessels. This leads to the fact that between the bones of the skull and the periosteum begins to accumulate blood. Since the blood of newborns is characterized by low coagulability, the formation continues to increase in size within 2-3 days after birth.
Cephalhematoma occurs in 0.1 to 1.8% of newborns.
Causes of cephalohematoma in newborns As a result, the brain is compressed, and the child's head is slightly deformed. However, you should not worry about this - within a few days after the birth, the bones of the cranium return to their places.
Meanwhile, the scalp is displaced along with the periosteum, thereby provoking vascular rupture. Most often this happens if the newborn suffers from a deficiency of vitamins K, C, PP. The blood flowing from the damaged capillaries begins to accumulate in the pocket between the flat bone of the skull and the periosteum, forming a tumor.
Other causes of cephalohematoma in newborns:
Large fetus with narrow birth canal;
Breech, parietal or facial presentation;
Rapid or, conversely, too slow delivery;
Postterm pregnancy;
Malformations and pathologies of fetal development;
A woman's narrow pelvis or past trauma that deformed the pelvic bones.
Also among the factors contributing to the formation of cephalohematoma in newborns, one can name chronic intrauterine fetal hypoxia. It can occur as a result of entanglement or squeezing of the umbilical cord. In addition, hemorrhages can be the result of the actions of obstetricians if forceps or vacuum are used in complicated births.
Treatment of cephalohematoma in newborns
A cephalohematoma can be located in different parts of the head, but most often it occurs in the region of the crown, less often in the occipital, frontal or temporal regions. The boundaries of the tumor usually do not go beyond the sutures of the skull, where the periosteum is tightly fused with the bones. The blood in the cephalohematoma remains liquid for a long time, does not clot, so the formation is initially elastic in consistency. On palpation, you can feel the movement of fluid inside.
If the amount of blood in the cephalohematoma in newborns is small, then after a few days it begins to decrease in size and dissolve. The tumor disappears completely in about one and a half to two months without any intervention. If there was a significant hemorrhage, then resorption may take a longer period of time.
Small cephalohematomas in newborns usually do not require treatment. Doctors observe the child, sometimes they prescribe vitamin K, which increases blood clotting. This is done in order to stop the leakage of blood and the increase in the size of the tumor. To avoid complications, it is recommended to feed the baby with breast milk, which contains maternal antibodies and contributes to the formation of his own immunity.
If the size of the hemorrhage is significant, a puncture of the cephalohematoma is performed, but not earlier than 10 days of life, due to the high probability of rebleeding. With a special needle, punctures are made in the periosteum, through which the contents of the formation are sucked out. Then a pressure bandage is applied to the damaged area.
If there is inflammation of the cephalohematoma, its redness, swelling, increase in body temperature, then there is infection and suppuration. In this case, instead of puncture of cephalohematoma in newborns, surgical intervention is required. The skin at the site of the formation of the tumor is cut, after which the blood accumulated there is removed and the edges of the wound are sutured. Further antibiotic therapy is carried out. After the operation, the child is under the supervision of doctors for several months.
Consequences of cephalohematoma in newborns
Anemia resulting from blood loss;
Jaundice (increased bilirubin), which develops as a result of tumor resorption, which is accompanied by the breakdown of hemoglobin and the entry of its products into the bloodstream;
Extremely rare:
Suppuration of cephalohematoma, development of an inflammatory process;
Ossification or ossification of the mass, resulting in a deformity of the skull.
Prevention of cephalohematoma in newborns consists in maintaining a healthy lifestyle for a pregnant woman and avoiding the use of drugs that can affect the development of the fetus.
Mycosis of the skin: symptoms, treatment, diagnosis of the disease
Mycoses are an extensive group of diseases united by one symptom - they are all caused by pathogenic fungi that parasitize on the skin, mucous membranes and other human tissues. Among all skin infections, they rank first in terms of prevalence, but despite this, many sick people cannot recognize the disease in time and consult a doctor, which is why dermatologists often have to deal with advanced forms of pathology.
Disease types
Currently, about four hundred different types of fungi are known that can be pathogenic to humans under certain conditions. According to the type of tissues affected, mycoses are distinguished:
- superficial, affecting the skin and mucous membranes:
- deep, the affected area of which is the subcutaneous tissue;
- visceral, which parasitize on the internal organs.
In accordance with the varieties of fungi that parasitize on humans, the following diseases are the most common.
- Rubrophytia. The fungus rubrum trichophyton affects the interdigital spaces, feet, less often settles in the skin folds and on the head. The skin at the site of the lesion turns red and flaky, nodules and small tubercles appear on it. When the skin of the trunk is affected, it forms large patches of reddened skin with bright red concentric ridges.
- Microsporia. As a rule, the fungus is transmitted from sick cats or dogs and affects the fluffy hair on the body, less often - the skin with the formation of a focus of inflamed skin with peeling and vesicles, surrounded by a roller. Microspores are resistant to external influences.
- Trichophytosis. The trichophyton fungus parasitizes on the skin, affecting mainly open areas of the body - the face, hands. It is highly contagious. In humans, outbreaks of the disease are most often recorded in late summer and autumn during field work, when people come into contact with hay and straw, on which the infection was left by sick rodents.
- Lichen versicolor. The cause of the common mycosis of smooth skin is Malassezia furfur. Foci, as a rule, form on the chest and abdomen, less often on other parts of the body: small pink spots appear, the color of which then changes to yellow or brown. They are covered with coarse scales that look like bran. Multiple spots soon merge into large formations.
- Seborrheic dermatitis. This is a common mycosis of the scalp, affecting the scalp, including the skin of the eyebrows, eyelashes, mustache and beard, caused by pityrosporum ovale. A variety of pityrosporum orbicularare parasitizes the smooth skin of the trunk. These are lipophilic fungi that feed on sebum. The affected areas of the skin are marked by inflammation and flaky crusts.
- Candidiasis. Candida yeast-like fungi settle in the skin folds, on the mucous membranes and form reddish spots covered with small bubbles. After a while, eroded areas of bright red color appear in place of the bubbles.
There are many types of mycosis of the skin, subcutaneous tissues and internal organs, which are much less common than the listed types.
Symptoms
It is possible to speak about the symptoms of mycosis only in general terms, since each variety has its own manifestations, which only an experienced dermatologist can recognize. With skin lesions, as a rule, appear:
- reddened and scaly patches of skin;
- severe itching in places affected by the fungus;
- diaper rash in skin folds and interdigital areas;
- small blisters that burst and dry out after a while;
- white, yellow or brownish crusts over inflamed skin.
With mycosis of the extremities, as a rule, the nails also suffer - they become brittle, delaminate, then gradually become cloudy and dark.
Deep mycoses, as a rule, proceed with the formation of deep ulcers, purulent inflammations, fistulas, etc. They are most common in countries with a hot climate, and are extremely rare in Russia. Visceral, depending on the location and degree of damage, can cause dysfunction of the organs on which the fungi parasitize - pulmonary diseases, digestive disorders, etc.
Reasons for the development of pathology
The main cause of mycosis is infection with a pathogenic fungus. At the same time, many types of fungi are constantly present in the body, and their growth is usually restrained by the immune system. With a decrease in control, the fungus begins to grow on the skin or tissues of internal organs. This is often due to:
- chronic disease that weakens the body;
- non-compliance with hygiene rules;
- insufficient or unbalanced nutrition;
- smoking and alcohol abuse;
- exposure to external factors that weaken the body - hypothermia, excess ultraviolet radiation, poisoning, radiation damage, etc.;
- long-term use of antibiotics or certain other medicines.
The only exception here is the so-called fungal mycosis, which is not a fungal disease. This is an oncological tumor pathology, which is based on the degeneration of T-lymphocytes into a malignant form.
Transmission routes
There are many ways to get infected with fungal diseases. Most often this happens:
- in direct contact with the affected skin of another person;
- when sharing towels, slippers, personal hygiene items;
- through a contaminated manicure instrument;
- through contaminated clothing and shoes;
- through the soil, especially in the presence of skin microtraumas;
- in contact with pets.
Often, skin mycoses develop in people who visit swimming pools, saunas, showers at sports clubs, etc. Infection is all the more likely, the worse the human immune system works.
Diagnostic methods
As part of the diagnosis of mycoses, studies of scrapings of the skin and nail formations, sputum, blood, hair, scrapings of mucous membranes, feces and other biomaterials can be performed, depending on the type and location of the lesion. For skin diseases, they usually perform:
- dermatoscopy - examination of affected areas of the skin, hair or nails to identify characteristic signs;
- microscopic examination of a scraping to detect fungal mycelium;
- bakposev on nutrient media, which allows you to identify not only the type of fungi, but also the optimal drug for treatment;
- serological examination of blood;
- PCR test for fungal genome detection.
Some types of fungi are quite easily diagnosed using UV radiation, which is generated using a Wood's lamp.
Simultaneously with determining the type of fungus, the patient is given a general examination to identify the cause of weakened immunity, which led to infection.
Treatment
Currently, there are many means and methods for the treatment of mycosis of almost all types. The main method is drug therapy, which includes drugs of general action and local remedies, which are selected depending on the type of fungus, the degree of damage, the duration of the disease, the patient's health and other factors. Mycoses of the skin and mucous membranes are best treated: if the doctor's recommendations are followed, the disease can be eliminated within two to three weeks, and sometimes in just a few days.
With damage to the nails, the course of therapy is several months, and combined treatment is required: local preparations are combined with systemic agents. Local dosage forms are extremely diverse: these are creams, ointments, gels, sprays, nail polishes, powders, drops. Systemic antimycotics are usually available in the form of tablets or capsules. In some cases, complete removal of the affected nail is required.
When choosing drugs, a dermatologist must take into account the individual sensitivity of the pathogen to a particular agent. Self-administration of certain drugs often does not bring the desired result, since before starting treatment it is necessary to determine the type of pathogen. In certain fungal infections, the diet of the patient is important. So, during the treatment of yeast and mold fungi, it is necessary to exclude foods that contain fast carbohydrates (sweets, flour products), fermented foods, alcohol and potatoes.
Prevention
To avoid mycosis, you must:
- observe the rules of hygiene, especially in public areas;
- avoid contact with stray animals;
- monitor the disinfection of instruments in hairdressing, beauty salons, manicure rooms;
- do not use other people's clothes and shoes.
With prolonged use of antibiotics, corticosteroids and immunosuppressants, it is necessary to take antimycotics at the same time.
Diagnosis and treatment of mycosis in Moscow
The clinic of JSC "Medicina" offers reliable, comfortable and high-quality treatment of mycosis. We employ qualified dermatologists with many years of practical experience, the latest medical equipment is used for diagnostics. Modern medical procedures allow you to quickly and reliably cleanse the body of a fungal infection. Call us to make an appointment or register online on our website.
Questions and answers
Which doctor treats mycosis?
For the diagnosis and treatment of mycosis, it is necessary to contact a specialized specialist - a mycologist. However, this medical specialty is quite rare, and in the absence of such a specialist in the clinic, you should visit a dermatologist.
Mycosis - what kind of disease and why is it dangerous?
Mycosis is a fungal infection caused by microscopic fungi. Settling on the tissues of the human body, they feed on them, at the same time destroying what they parasitize - skin, hair, nails, internal organs. At the same time, parasites inhibit the microflora of the body, adjust metabolic processes for themselves and poison the body with waste products of their vital activity. As a result, a person constantly feels unwell, his immune system is weakened, he is easily infected with pathogenic viruses and bacteria, and some people even develop cancer.
How to treat mycosis at home?
There are many traditional medicine recipes for the treatment of fungal infections. They can be used as supplements to fight fungus, but only after the approval of the attending physician. The most effective are baths and compresses with apple cider vinegar, alcohol tincture on pine cones, tea tree oil, garlic vegetable oil, birch tar, propolis. However, all these remedies by themselves do not completely eliminate the fungus. They are used only in combination with antimycotic drugs.