Cervix gel to induce labor
Inducing Labor (for Parents) - Nemours KidsHealth
It's common for many pregnant women, especially first-time mothers, to watch their baby's due date come and go without so much as a contraction. The farther away from the expected delivery date (called the EDD) you get, the more anxious you might become. You may start to wonder — is this baby ever going to come?
Late pregnancy can be challenging — you may feel large all over, your feet and back might hurt, you might not have the energy to do much of anything, and you're beyond ready to meet the little one you've nurtured all this time. Which is why waiting a little longer than you'd expected can be particularly hard.
Still, being past your due date doesn't guarantee that your doctor (or other health care provider) will do anything to induce (or artificially start) labor — at least not right away.
What Is It?
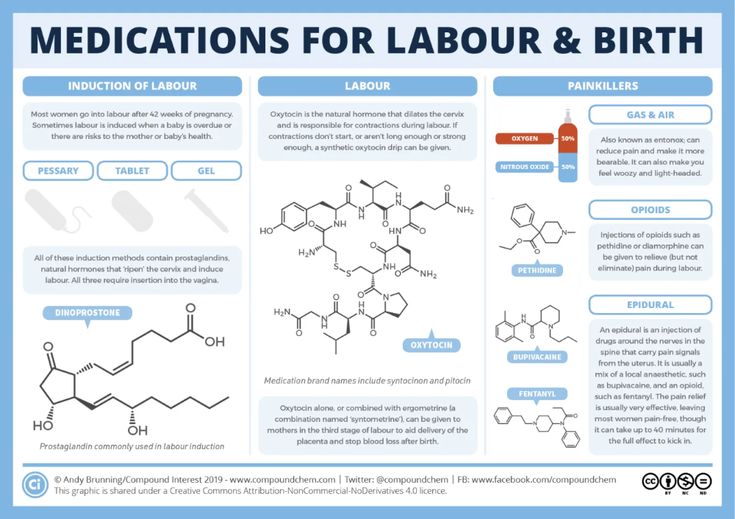
Labor induction is what doctors use to try to help labor along using medications or other medical techniques. Years ago, some doctors routinely induced labor. But now it's not usually done unless there's a true medical need for it. Labor is usually allowed to take its natural course. However, in some situations, a health care provider may recommend induction.
Why It's Done
Your doctor might suggest an induction if:
- your water broke but you are not having contractions
- your baby still hasn't arrived by 2 weeks after the due date (when you're considered post-term — more than 42 weeks into your pregnancy)
- you have an infection in the uterus (called chorioamnionitis)
- you have certain risk factors (e.g., gestational diabetes or high blood pressure)
- there is not enough amniotic fluid
- there is a problem with the placenta
- the baby is not growing appropriately
Induction also can be appropriate under certain circumstances, as with a mother who is full term and has a history of rapid deliveries or lives far from a hospital.
Some mothers request elective inductions for convenience, but these do come with risks. Doctors try to avoid inducing labor early because the due date may be wrong and/or the woman's cervix might not be ready yet.
Page 2
How It's Done
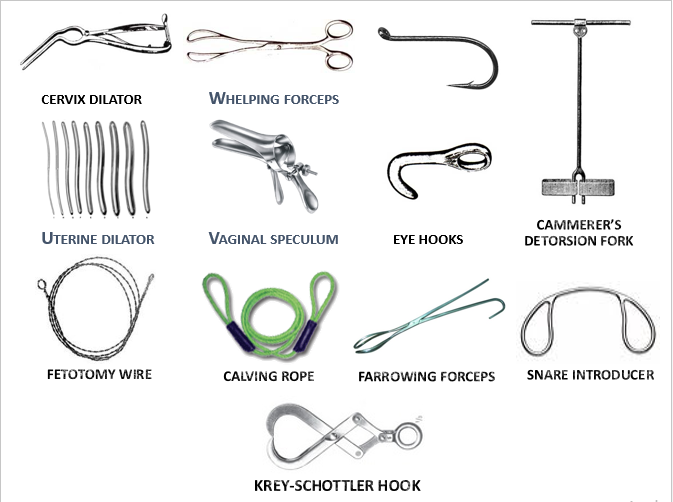
Some methods of induction are less invasive and carry fewer risks than others. Ways that doctors may try to induce labor by getting contractions started include:
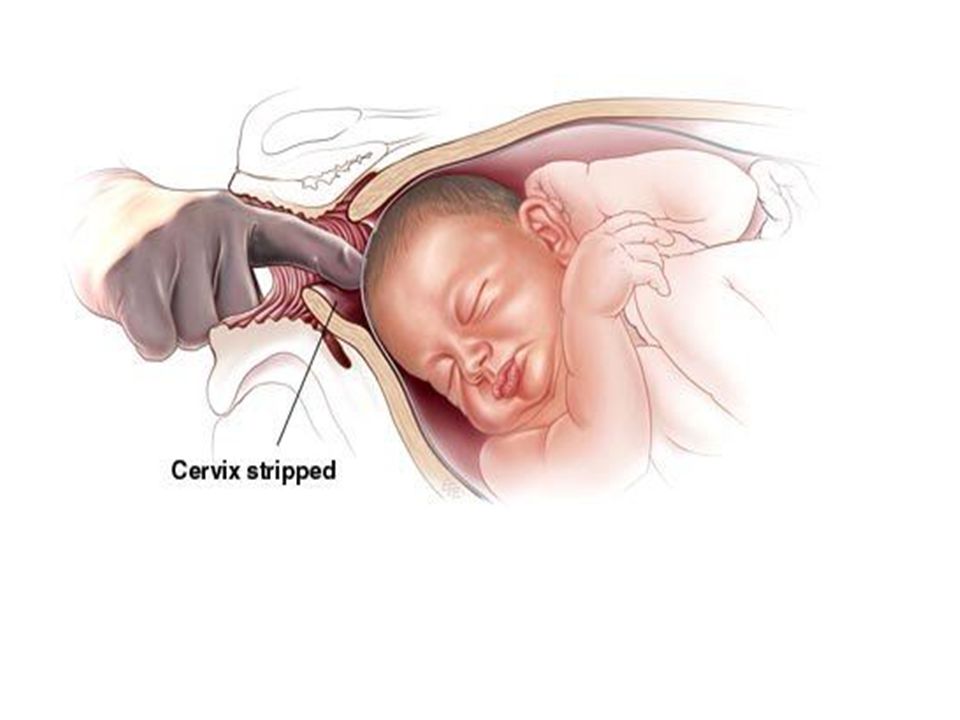
- Stripping the membranes. The doctor puts on a glove and inserts a finger into the vagina and through the cervix (the opening that connects the vagina to the uterus). He or she moves the finger back and forth to separate the thin membrane connecting the amniotic sac (which houses the baby and amniotic fluid) to the wall of the uterus. When the membranes are stripped, the body releases hormones called prostaglandins, which help prepare the cervix for delivery and may bring on contractions. This method works for some women, but not all.
- Breaking your water (also called an amniotomy).
 The doctor ruptures the amniotic sac during a vaginal exam using a little plastic hook to break the membranes. If the cervix is ready for labor, amniotomy usually brings on labor in a matter of hours.
The doctor ruptures the amniotic sac during a vaginal exam using a little plastic hook to break the membranes. If the cervix is ready for labor, amniotomy usually brings on labor in a matter of hours. - Giving the hormone prostaglandin to help ripen the cervix. A gel or vaginal insert of prostaglandin is inserted into the vagina or a tablet is given by mouth. This is typically done overnight in the hospital to make the cervix "ripe" (soft, thinned out) for delivery. Administered alone, prostaglandin may induce labor or may be used before giving oxytocin.
- Giving the hormone oxytocin to stimulate contractions. Given continuously through an IV, the drug (Pitocin) is started in a small dose and then increased until labor is progressing well. After it's administered, the fetus and uterus need to be closely monitored. Oxytocin is also frequently used to spur labor that's going slowly or has stalled.
What Will It Feel Like?
Stripping the membranes can be a little painful or uncomfortable, although it usually only takes a minute or so.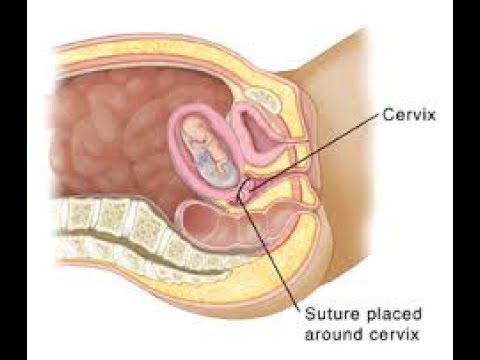 You may also have some intense cramps and spotting for the next day or two.
You may also have some intense cramps and spotting for the next day or two.
It can also be a little uncomfortable to have your water broken. You may feel a tug followed by a warm trickle or gush of fluid.
With prostaglandin, you might have some strong cramping as well. With oxytocin, contractions are usually more frequent and regular than in a labor that starts naturally.
Page 3
Risks and Precautions
Inducing labor is not like turning on a faucet. If the body isn't ready, an induction might fail and, after hours or days of trying, a woman may end up having a cesarean delivery (C-section). This appears to be more likely if the cervix is not yet ripe.
If the doctor ruptures the amniotic sac and labor doesn't begin, another method of inducing labor also might be necessary because there's a risk of infection to both mother and baby if the membranes are ruptured for a long time before the baby is born.
When prostaglandin or oxytocin is used, there is a risk of abnormal contractions developing. In that case, the doctor may remove the vaginal insert or turn the oxytocin dose down. While it is rare, there is an increase in the risk of developing a tear in the uterus (uterine rupture) when these medications are used. Other complications associated with oxytocin use are low blood pressure and low blood sodium (which can cause problems such as seizures).
In that case, the doctor may remove the vaginal insert or turn the oxytocin dose down. While it is rare, there is an increase in the risk of developing a tear in the uterus (uterine rupture) when these medications are used. Other complications associated with oxytocin use are low blood pressure and low blood sodium (which can cause problems such as seizures).
Another potential risk of inducing labor is giving birth to a late pre-term baby (born after 34 and before 37 weeks). Why? Because the due date (EDD) may be wrong. Your due date is 40 weeks from the first day of your last menstrual period (LMP).
Babies born late pre-term are generally healthy but may have temporary problems such as jaundice, trouble feeding, problems with breathing, or difficulty maintaining body temperature. They may also be more likely than full term babies to have developmental or school problems later on.
Even though inductions do come with risks, going beyond 42 weeks of pregnancy can be risky, too. Many babies are born "post-term" without any complications, but concerns include:
Many babies are born "post-term" without any complications, but concerns include:
- A vaginal delivery may become harder as the baby gets bigger. As babies get bigger, the chance of an injury during delivery, such as a broken bone, increases.
- The placenta that helps to provide the baby with nourishment is deteriorating.
- The amniotic fluid can become low or contain meconium — the baby's first feces. If the baby breathes in meconium, it can cause breathing problems.
Old wives' tales abound about ways to induce labor, such as the use of castor oil. It is not safe to try to artificially start labor yourself by taking castor oil, which can lead to nausea, diarrhea, and dehydration. And herbs and herbal supplements meant to induce labor can be harmful. Breast stimulation can cause uterine contractions by causing the release of oxytocin. However, some studies have suggested that the baby might have abnormal heartbeats after breast stimulation. Some women feel that having sex in late pregnancy can induce labor, but there is no conclusion on this yet.
Talk to your doctor before doing anything to try to encourage your little one's arrival. Inducing labor is best left to medical professionals — you may cause more harm than good.
As frustrating as it can be waiting for your baby to finally decide to arrive, letting nature take its course is often best, unless your doctor tells you otherwise. Before you know it, you'll be too busy to remember your baby was ever late at all!
Prostaglandin E2 gel for cervical ripening and induction of labor: a critical analysis
Review
. 1989 Mar;160(3):529-34.
doi: 10.1016/s0002-9378(89)80020-1.
W F Rayburn 1
Affiliations
Affiliation
- 1 Department of Obstetrics and Gynecology, University of Nebraska Medical Center, Omaha 68105.

- PMID: 2648830
- DOI: 10.1016/s0002-9378(89)80020-1
Review
W F Rayburn. Am J Obstet Gynecol. 1989 Mar.
. 1989 Mar;160(3):529-34.
doi: 10.1016/s0002-9378(89)80020-1.
Author
W F Rayburn 1
Affiliation
- 1 Department of Obstetrics and Gynecology, University of Nebraska Medical Center, Omaha 68105.
- PMID: 2648830
- DOI: 10.
 1016/s0002-9378(89)80020-1
1016/s0002-9378(89)80020-1
Abstract
This report summarizes the cumulative experience of 3313 pregnancies represented in 59 prospective clinical trials in which intracervical or intravaginal prostaglandin E2 gel was used for cervical ripening before induction of labor. Results indicate that local prostaglandin E2 is superior to placebo or no therapy in enhancing cervical effacement and dilation, reducing initial induction failures, shortening the induction-delivery interval, reducing oxytocin use, and lowering the rate of cesarean section because of failure to progress. Certain advantages also exist for labor induction in the presence of a favorable cervical state. Uterine hyperstimulation or pathologic fetal heart rate patterns before oxytocin administration occur in less than 1% of reported cases and are usually dose related, self contained, and reversible with the use of beta-adrenergic tocolytic therapy. Maternal systemic effects in these low doses are negligible. Worldwide clinical experience has clearly demonstrated that prostaglandin E2 gel administered before induction of labor is of major therapeutic benefit and should become commercially available for more than investigational use.
Maternal systemic effects in these low doses are negligible. Worldwide clinical experience has clearly demonstrated that prostaglandin E2 gel administered before induction of labor is of major therapeutic benefit and should become commercially available for more than investigational use.
PIP: Prostaglandin E2 gel is a useful agent for ripening and dilating the cervix. Since it is not available in the US, it must be prepared by thawing and grinding a 20 mg prostaglandin E2 suppository, mixing in a small amount of methylcelulose gel, and blending. The resulting gel is stored frozen in a 3 ml plastic syringe. The gel may be administered intracervically, intravaginally, or extraamniotically. Cervical administration of .5 mg prostaglandin E2 in 2-3 ml of viscous gel is most popular, but intravaginal administration is easiest, although it requires a higher dose (1-5 mg prostaglandin E2 in 2-10 ml of gel). The condition of the cervix is usually favorable for labor induction within 12 hours (range 4-24 hours). 59 clinical trials were conducted among 3313 pregnancies. In patients with unfavorable cervix induction of labor was successful in 83% of those treated with the gel but in only 53% of untreated patients. In women with an unfavorable cervix the gel is more effective if administered intracervically. In patients with favorable cervix, 66% of nulliparas and 82% of multiparas were delivered without oxytocin. Prostaglandin E2 gel has been used successfully even in women with prolonged pregnancy, hypertension, ruptured membranes, and fetal death. It can also be used to induce late 1st trimester abortion. Side effects of the gel are mild and minor. Prostaglandin E2 gel has thus been shown to effect cervical ripening and dilatation, reduce induction failures, shorten the induction-delivery interval, reduce oxytocin use, and lower the need for cesarean sections. Prefabricated prostaglandin E2 delivery systems should be approved by the Food and Drug Administration for commercial use.
59 clinical trials were conducted among 3313 pregnancies. In patients with unfavorable cervix induction of labor was successful in 83% of those treated with the gel but in only 53% of untreated patients. In women with an unfavorable cervix the gel is more effective if administered intracervically. In patients with favorable cervix, 66% of nulliparas and 82% of multiparas were delivered without oxytocin. Prostaglandin E2 gel has been used successfully even in women with prolonged pregnancy, hypertension, ruptured membranes, and fetal death. It can also be used to induce late 1st trimester abortion. Side effects of the gel are mild and minor. Prostaglandin E2 gel has thus been shown to effect cervical ripening and dilatation, reduce induction failures, shorten the induction-delivery interval, reduce oxytocin use, and lower the need for cesarean sections. Prefabricated prostaglandin E2 delivery systems should be approved by the Food and Drug Administration for commercial use.
Similar articles
-
Misoprostol: an effective agent for cervical ripening and labor induction.
Wing DA, Rahall A, Jones MM, Goodwin TM, Paul RH. Wing DA, et al. Am J Obstet Gynecol. 1995 Jun;172(6):1811-6. doi: 10.1016/0002-9378(95)91416-1. Am J Obstet Gynecol. 1995. PMID: 7778637 Clinical Trial.
-
Ripening of the uterine cervix and induction of labour at term with prostaglandin E2 in viscous gel.
Wingerup L, Andersson KE, Ulmsten U. Wingerup L, et al. Acta Obstet Gynecol Scand. 1978;57(5):403-6. doi: 10.3109/00016347809156519. Acta Obstet Gynecol Scand. 1978. PMID: 364917 Clinical Trial.
-
Cervical ripening and labor induction with prostaglandin E2 gel: a placebo-controlled study.
Bernstein P, Leyland N, Gurland P, Gare D. Bernstein P, et al. Am J Obstet Gynecol.
 1987 Feb;156(2):336-40. doi: 10.1016/0002-9378(87)90279-1. Am J Obstet Gynecol. 1987. PMID: 3548368 Clinical Trial.
1987 Feb;156(2):336-40. doi: 10.1016/0002-9378(87)90279-1. Am J Obstet Gynecol. 1987. PMID: 3548368 Clinical Trial. -
[The use of prostaglandin E2 to induce labor and abortion in the second trimester].
Khadzhiev A. Khadzhiev A. Akush Ginekol (Sofiia). 1991;30(1):39-45. Akush Ginekol (Sofiia). 1991. PMID: 1793135 Review. Bulgarian.
-
Therapeutic considerations for preinduction cervical ripening with intracervical prostaglandin E2 gel.
Bernstein EP. Bernstein EP. J Reprod Med. 1993 Jan;38(1 Suppl):73-7. J Reprod Med. 1993. PMID: 8429530 Review.
See all similar articles
Cited by
-
Human Chorionic Gonadotropin Modulates the Transcriptome of the Myometrium and Cervix in Late Gestation.

Motomura K, Romero R, Galaz J, Miller D, Done B, Arenas-Hernandez M, Garcia-Flores V, Tao L, Tarca AL, Gomez-Lopez N. Motomura K, et al. Reprod Sci. 2021 Aug;28(8):2246-2260. doi: 10.1007/s43032-020-00454-6. Epub 2021 Mar 1. Reprod Sci. 2021. PMID: 33650091 Free PMC article.
-
Obstetric and perinatal outcome in anti-Ro/SSA-positive pregnant women: a prospective cohort study.
Martínez-Sánchez N, Pérez-Pinto S, Robles-Marhuenda Á, Arnalich-Fernández F, Martín Cameán M, Hueso Zalvide E, Bartha JL. Martínez-Sánchez N, et al. Immunol Res. 2017 Apr;65(2):487-494. doi: 10.1007/s12026-016-8888-5. Immunol Res. 2017. PMID: 28138914
-
INDUCTION OF LABOUR WITH MISOPROSTOL - A PROSTAGLANDIN E1 ANALOGUE.
Kumar S, Awasthi RT, Kapur A, Srinivas S, Parikh H, Sarkar S.
 Kumar S, et al. Med J Armed Forces India. 2001 Apr;57(2):107-9. doi: 10.1016/S0377-1237(01)80125-8. Epub 2011 Jul 21. Med J Armed Forces India. 2001. PMID: 27407309 Free PMC article.
Kumar S, et al. Med J Armed Forces India. 2001 Apr;57(2):107-9. doi: 10.1016/S0377-1237(01)80125-8. Epub 2011 Jul 21. Med J Armed Forces India. 2001. PMID: 27407309 Free PMC article. -
Genome-wide analysis of DNA methylation in human amnion.
Kim J, Pitlick MM, Christine PJ, Schaefer AR, Saleme C, Comas B, Cosentino V, Gadow E, Murray JC. Kim J, et al. ScientificWorldJournal. 2013;2013:678156. doi: 10.1155/2013/678156. Epub 2013 Feb 19. ScientificWorldJournal. 2013. PMID: 23533356 Free PMC article.
-
Maternal intravaginal prostaglandin E2 gel before elective caesarean section at term to induce catecholamine surge in cord blood: randomised, placebo controlled study.
Singh M, Patole S, Rane A, Naidoo D, Buettner P.
 Singh M, et al. Arch Dis Child Fetal Neonatal Ed. 2004 Mar;89(2):F131-5. doi: 10.1136/adc.2002.025957. Arch Dis Child Fetal Neonatal Ed. 2004. PMID: 14977896 Free PMC article. Clinical Trial.
Singh M, et al. Arch Dis Child Fetal Neonatal Ed. 2004 Mar;89(2):F131-5. doi: 10.1136/adc.2002.025957. Arch Dis Child Fetal Neonatal Ed. 2004. PMID: 14977896 Free PMC article. Clinical Trial.
See all "Cited by" articles
Publication types
MeSH terms
Substances
Makarov I.O. • Modern methods of preparing the body for childbirth, labor induction and labor stimulation
RS80 ultrasound scanner
The standard of new standards! Unprecedented clarity, resolution, ultra-fast data processing, and a comprehensive suite of state-of-the-art ultrasound technologies to meet the most demanding diagnostic challenges.
Modern principles of preparation for childbirth and their management should ensure the birth of not only a live, but also a healthy child.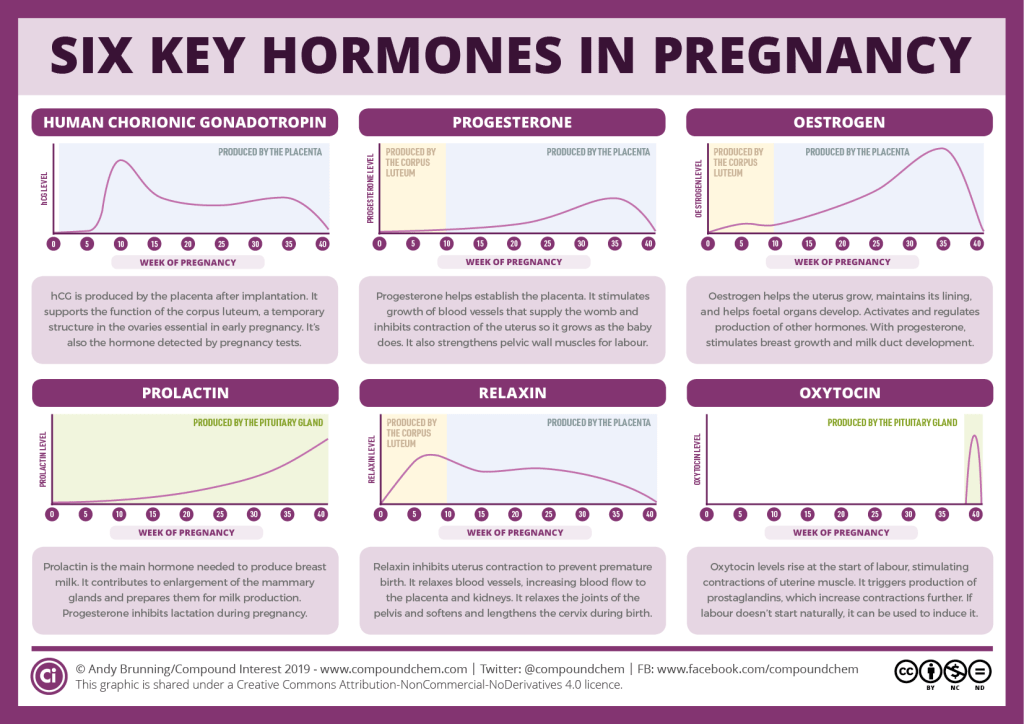 Accordingly, the further physical development and health of the child largely depends on the success of the preparation for childbirth and the quality of their conduct. For the effective onset and further progression of normal labor activity, one of the important conditions is the presence of a "mature" cervix, which reflects the readiness of the mother's body and the fetus for childbirth. With an "immature" cervix, labor induction and intensification of labor cannot be carried out because of the danger of a violation of the contractile activity of the uterus, the occurrence of hypoxia and fetal injury.
Accordingly, the further physical development and health of the child largely depends on the success of the preparation for childbirth and the quality of their conduct. For the effective onset and further progression of normal labor activity, one of the important conditions is the presence of a "mature" cervix, which reflects the readiness of the mother's body and the fetus for childbirth. With an "immature" cervix, labor induction and intensification of labor cannot be carried out because of the danger of a violation of the contractile activity of the uterus, the occurrence of hypoxia and fetal injury.
Prostaglandins
According to modern concepts, the preparation of the cervix for childbirth occurs not only under the influence of hormones, but primarily under the action of substances called prostaglandins. In this case, we are talking about two types: prostaglandin E2 and F2α. So, in particular, prostaglandin E2 is produced by the fetal part of the placenta, in the body of the fetus, and also in the tissues of the cervix.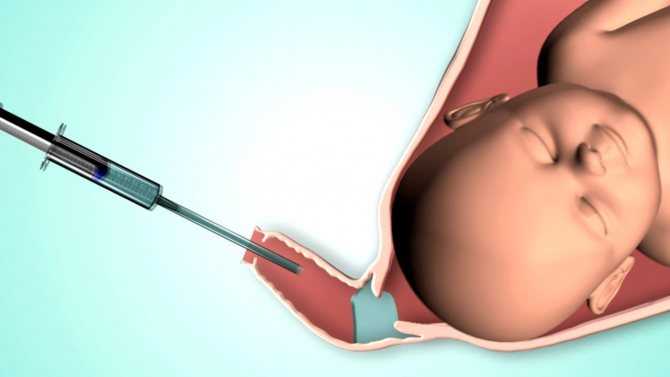 It helps to change the structure of the tissues of the cervix, ensuring its maturation, and also has a certain relaxing effect on the isthmus, cervix and lower segment of the uterus. Upon reaching the proper degree of maturation of the cervix, under the influence of prostaglandin E2, the development of labor activity gradually begins. Therefore, it is prostaglandin E2 that plays the starting role of the onset of labor. Prostaglandin F2α is produced in the maternal part of the placenta and in the walls of the uterus. It supports the labor activity that has already begun, providing the strongest and most effective reducing effect, helps to limit blood loss during childbirth.
It helps to change the structure of the tissues of the cervix, ensuring its maturation, and also has a certain relaxing effect on the isthmus, cervix and lower segment of the uterus. Upon reaching the proper degree of maturation of the cervix, under the influence of prostaglandin E2, the development of labor activity gradually begins. Therefore, it is prostaglandin E2 that plays the starting role of the onset of labor. Prostaglandin F2α is produced in the maternal part of the placenta and in the walls of the uterus. It supports the labor activity that has already begun, providing the strongest and most effective reducing effect, helps to limit blood loss during childbirth.
The topical application of prostaglandins became widespread after the development of special gels containing the required dose of the drug. Usually, to achieve sufficient maturity of the cervix and prepare it for childbirth, prostaglandin gel is injected into the cervical canal. For the successful use of the drug and the prevention of possible complications when using it, a number of conditions must be observed, as well as adhere to the relevant indications and contraindications.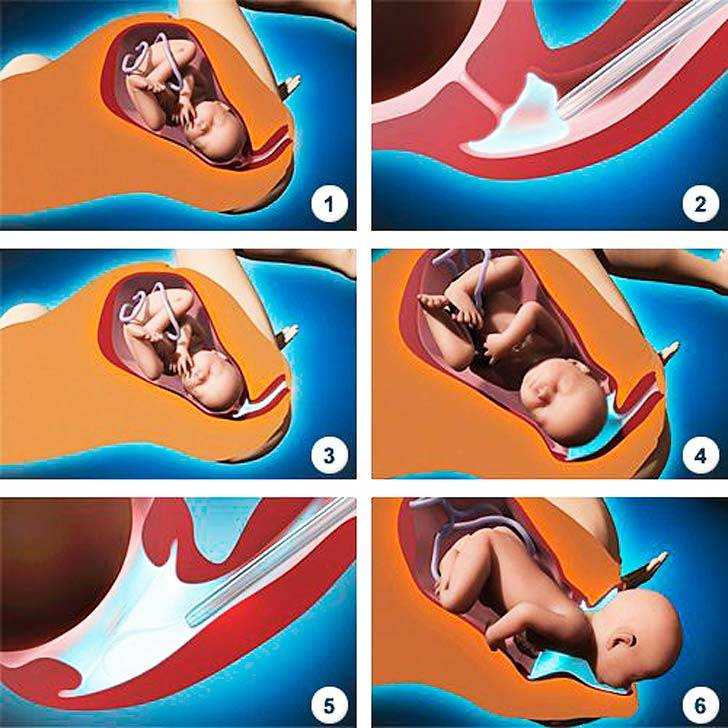 Thus, the need to use a prostaglandin gel to prepare the cervix arises in the absence of the biological readiness of the body for childbirth (immature cervix) and there are indications for urgent delivery in case of various obstetric or other complications (for example, in the case of prolonged pregnancy, preeclampsia, fetoplacental insufficiency, etc.). ).
Thus, the need to use a prostaglandin gel to prepare the cervix arises in the absence of the biological readiness of the body for childbirth (immature cervix) and there are indications for urgent delivery in case of various obstetric or other complications (for example, in the case of prolonged pregnancy, preeclampsia, fetoplacental insufficiency, etc.). ).
Contraindications for the use of the drug are: the presence of a scar on the uterus after caesarean section or after other operations on the uterus; placenta previa; multiple pregnancy; pronounced signs of violation of the condition of the fetus; narrow pelvis; leakage of amniotic fluid; allergy to prostaglandins; asthma; increased intraocular pressure. Prostaglandin gel is used only in a hospital in the following cases: the presence of an immature or insufficiently mature cervix; a whole fetal bladder; absence of contraindications for childbirth through the natural birth canal.
Labor induction, preparation of the cervix
Before using the drug, it is necessary to determine the condition of the cervix, pulse and respiration rate, blood pressure, as well as assess the condition of the fetus and the contractile activity of the uterus.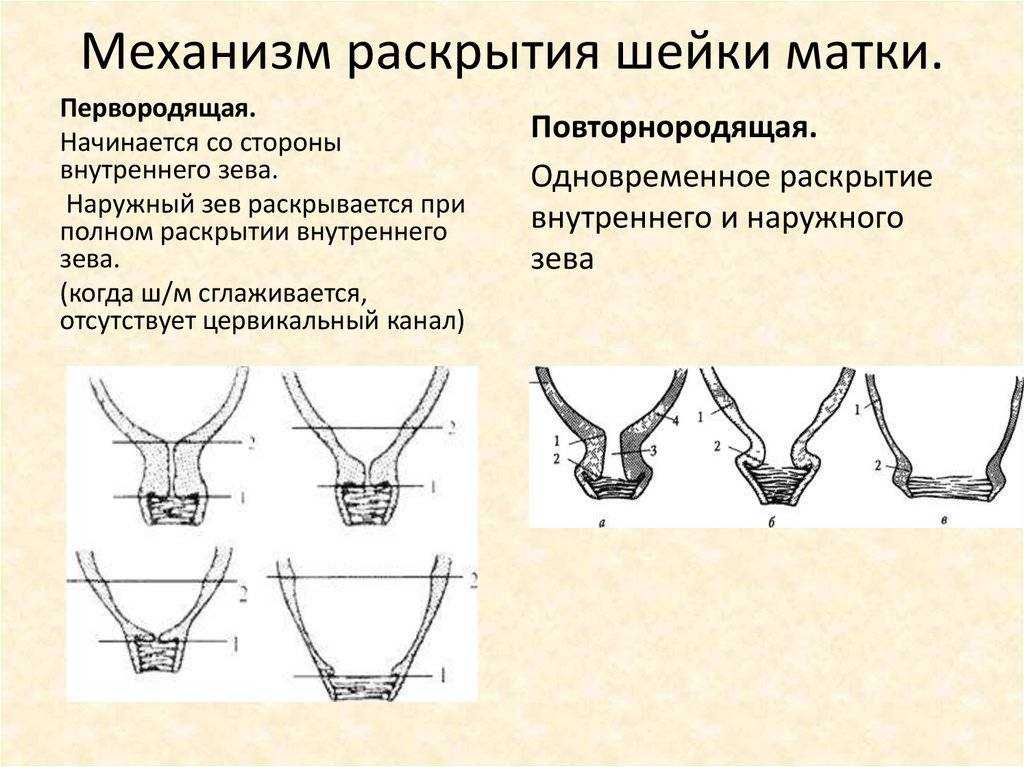 The gel is injected into the cervical canal in the position of the pregnant woman on her back, under the control of mirrors. To prevent leakage of the gel, the pregnant woman is left in the supine position for 30 minutes.
The gel is injected into the cervical canal in the position of the pregnant woman on her back, under the control of mirrors. To prevent leakage of the gel, the pregnant woman is left in the supine position for 30 minutes.
During the subsequent observation of the patient, monitoring of the contractile activity of the uterus and the condition of the fetus is carried out. Assess the condition of the cervix (every 2-3 hours), pulse, blood pressure and respiratory rate. Under the influence of the drug, not only the maturation of the cervix occurs, labor can begin. In this case, after reaching a sufficient degree of maturity and opening the cervix by at least 4 cm, the fetal bladder is opened if it has not opened on its own before. Most often, after the application of a prostaglandin gel in the first 3-4 hours, more than half of the patients already have noticeable changes in the condition of the cervix. At the same time, it shortens and softens, located along the axis of the pelvis. In the next 3 hours (6 hours after the injection of the gel), a mature cervix is observed in another 1/3 of the patients. In many patients, on average after 9-10 hour labor activity develops. In the event that after applying the gel for 6 hours, the cervix remains immature, the drug is administered again at the same dose.
In the next 3 hours (6 hours after the injection of the gel), a mature cervix is observed in another 1/3 of the patients. In many patients, on average after 9-10 hour labor activity develops. In the event that after applying the gel for 6 hours, the cervix remains immature, the drug is administered again at the same dose.
A maximum of three injections of gel within 24 hours. With prenatal or early rupture of amniotic fluid, repeated administration of the gel is contraindicated, and further childbirth is carried out depending on the obstetric situation. Effective use of the gel is considered when a sufficient degree of maturity of the cervix is reached within 12 hours, and the onset of labor within 24 hours from the moment of its introduction. Usually, after applying the gel, the contractile activity of the uterus is normal, while there are no pathological changes in blood pressure and pulse rate in the mother, and there are no signs of fetal disorders.
For induction of labor with a sufficient degree of maturity of the cervix, it is advisable to use a gel containing prostaglandin E2 in the vagina.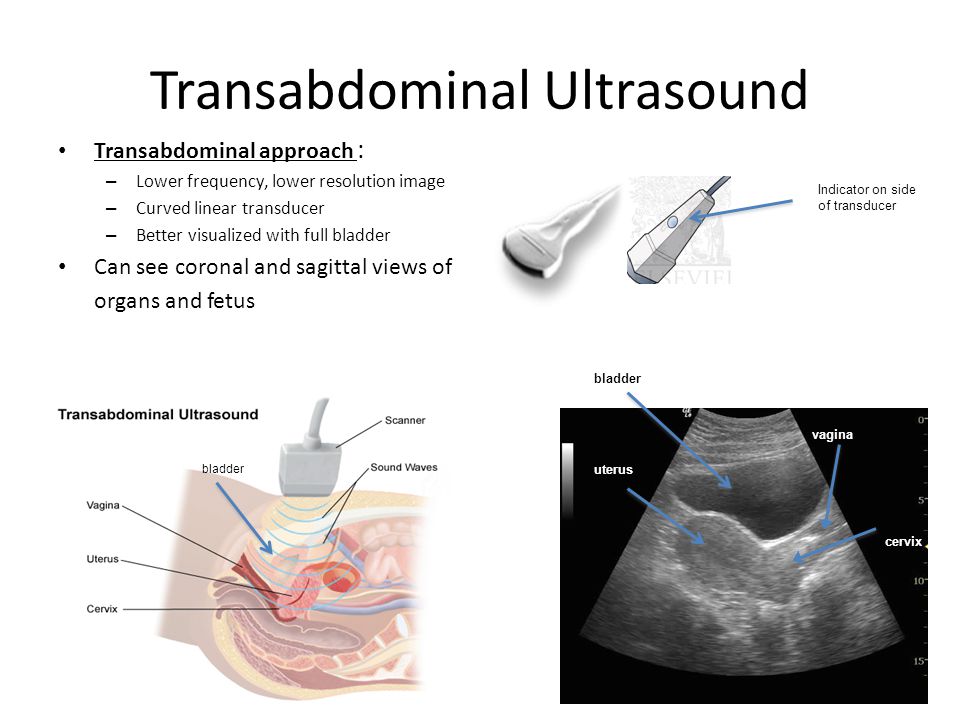 The drug is used in cases where there is a need for urgent delivery due to obstetric or some other complications. Conditions and contraindications for the use of vaginal gel are the same as for the use of prostaglandin gel for insertion into the cervical canal.
The drug is used in cases where there is a need for urgent delivery due to obstetric or some other complications. Conditions and contraindications for the use of vaginal gel are the same as for the use of prostaglandin gel for insertion into the cervical canal.
The main purpose of the introduction of this drug is, first of all, the development of labor. As an additional effect, its positive effect on the process of maturation of the cervix with its insufficient readiness for childbirth is noted. In the subsequent observation and management of patients, the following principles must be observed: every 3 hours after the introduction of the vaginal gel, the condition of the cervix is assessed. If the opening of the cervix occurs less than 3 cm after 6 hours from the moment of gel administration, or there is no regular labor activity during this period of time, then the drug is administered again 1 or 2 more times, also with an interval of 6 hours. If spontaneous opening of the membranes occurs before the expiration of 6 hours from the moment of the last administration of the gel, the drug is no longer administered.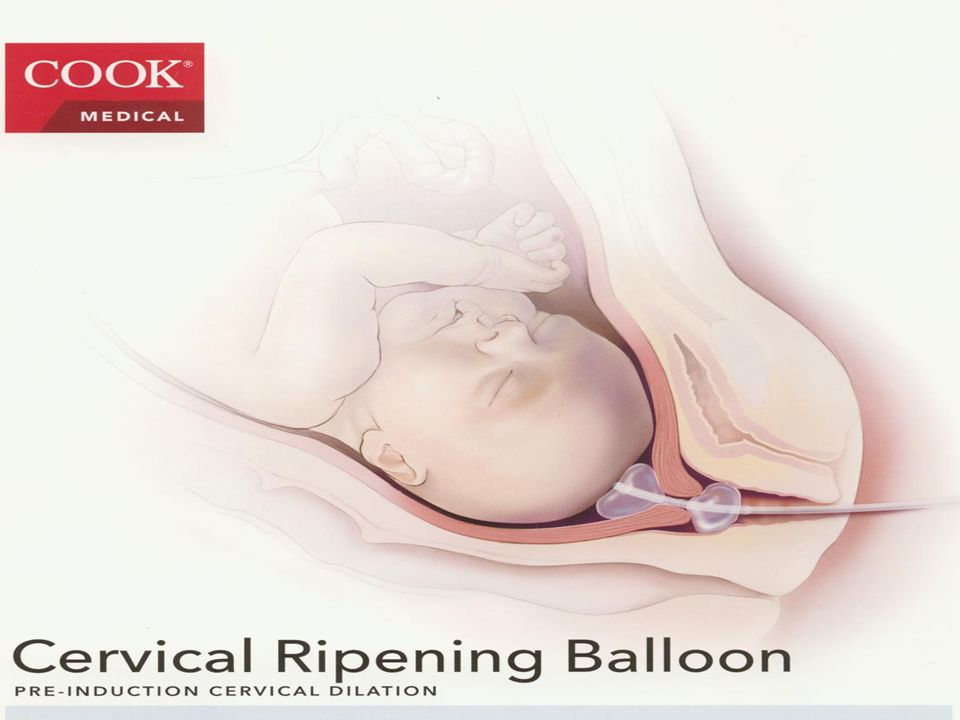 If, after the administration of the drug, the cervix opens by at least 4 cm with regular labor, it is possible to open the fetal bladder, but not earlier than 6 hours after the administration of the gel. If necessary, it is possible to administer oxytocin intravenously for rhodostimulation, however, not earlier than 6 hours after the injection of the gel.
If, after the administration of the drug, the cervix opens by at least 4 cm with regular labor, it is possible to open the fetal bladder, but not earlier than 6 hours after the administration of the gel. If necessary, it is possible to administer oxytocin intravenously for rhodostimulation, however, not earlier than 6 hours after the injection of the gel.
In the process of monitoring a woman in labor, monitor control of the fetus, contractile activity of the uterus, control pulse, blood pressure and respiratory rate. Correction of weak contractile activity of the uterus and ineffective labor activity should include the use of the most effective medications in accordance with scientific data on the mechanisms of development of labor activity.
In obstetric practice, to enhance the contractile activity of the uterus in case of weakness of labor forces, various drugs are used that are administered intravenously. The most popular among them is still oxytocin. However, in some cases, for example, with an insufficiently mature cervix and prenatal rupture of amniotic fluid, it is possible to use an intravenous drip of a drug containing prostaglandin E2.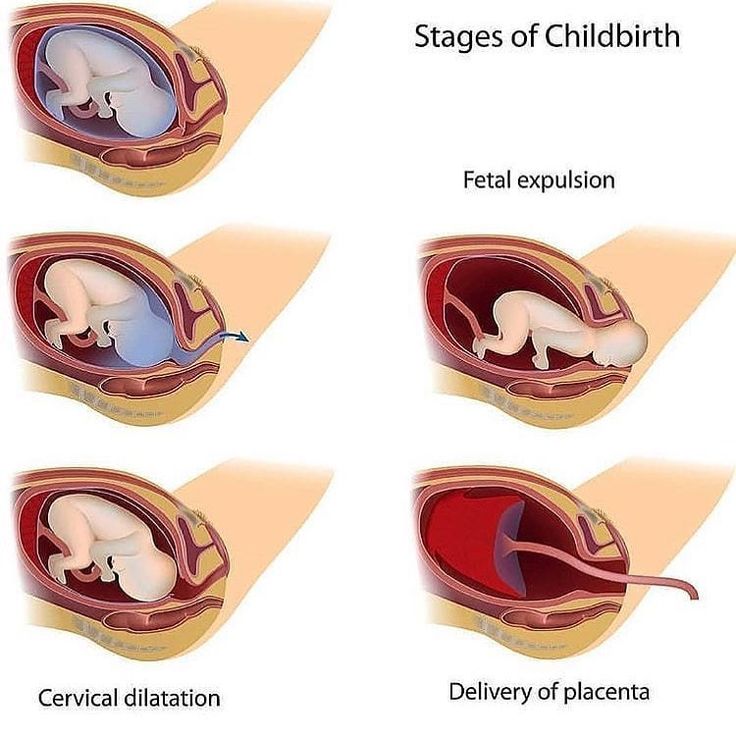 And with the primary weakness of labor, it is advisable to intravenously drip the drug containing prostaglandin F2α.
And with the primary weakness of labor, it is advisable to intravenously drip the drug containing prostaglandin F2α.
Features of the use of oxytocin
The results of the studies indicate that in the process of artificial strengthening of the contractile activity of the uterus, the anti-stress resistance of the fetus decreases, and its protective and adaptive capabilities are suppressed. At the same time, the use of oxytocin to enhance labor activity has the least favorable effect on the course of labor, the condition of the fetus and newborn in comparison with drugs containing prostaglandins E2 and F2α, which are used for the same purpose and in a similar obstetric situation.
The adverse effect of oxytocin can be especially pronounced in cases where the fetus experienced hypoxia even before the onset of labor, and the administration of oxytocin lasted more than 3 hours. The findings highlight the high health risk of the newborn with long-term use of oxytocin. The combined intravenous use of a solution containing prostaglandin F2α and oxytocin at half the dosage has a milder effect on the fetus, and is appropriate if it is necessary to increase contractions in the active phase of labor.
The combined intravenous use of a solution containing prostaglandin F2α and oxytocin at half the dosage has a milder effect on the fetus, and is appropriate if it is necessary to increase contractions in the active phase of labor.
Labor stimulation
Labor stimulation with drugs containing prostaglandin E2 allows you to achieve the best effect in case of primary weakness of labor, insufficient cervical maturity and prenatal rupture of amniotic fluid. To achieve the best effect from the introduction of drugs to correct the weakness of labor, certain principles and conditions must be observed. So, before rhodostimulation, it is important to exclude a narrow pelvis, inferiority of the uterine wall due to numerous or complicated induced abortions or inflammatory processes.
The use of labor stimulation is contraindicated in the presence of a scar on the uterus after caesarean section or other operations, as well as in the unsatisfactory condition of the fetus. Labor stimulation should, as it were, imitate the natural development of labor in order to achieve the physiological rate of labor. In the process of rhodostimulation, constant monitoring of the condition of the fetus and the contractile activity of the uterus is carried out. The duration of rhodostimulation should not exceed 3-4 hours. If excessive contractile activity of the uterus occurs or if the condition of the fetus worsens against the background of the administration of drugs, rhodostimulation is stopped.
In the process of rhodostimulation, constant monitoring of the condition of the fetus and the contractile activity of the uterus is carried out. The duration of rhodostimulation should not exceed 3-4 hours. If excessive contractile activity of the uterus occurs or if the condition of the fetus worsens against the background of the administration of drugs, rhodostimulation is stopped.
RS80 ultrasound scanner
Setting new standards! Unprecedented clarity, resolution, ultra-fast data processing, and a comprehensive suite of state-of-the-art ultrasound technologies to meet the most demanding diagnostic challenges.
Induction of labor or induction of labor
The purpose of this information material is to familiarize the patient with the induction of labor procedure and to provide information on how and why it is performed.
In most cases, labor begins between the 37th and 42nd weeks of pregnancy. Such births are called spontaneous. If drugs or medical devices are used before the onset of spontaneous labor, then the terms "stimulated" or "induced" labor are used in this case.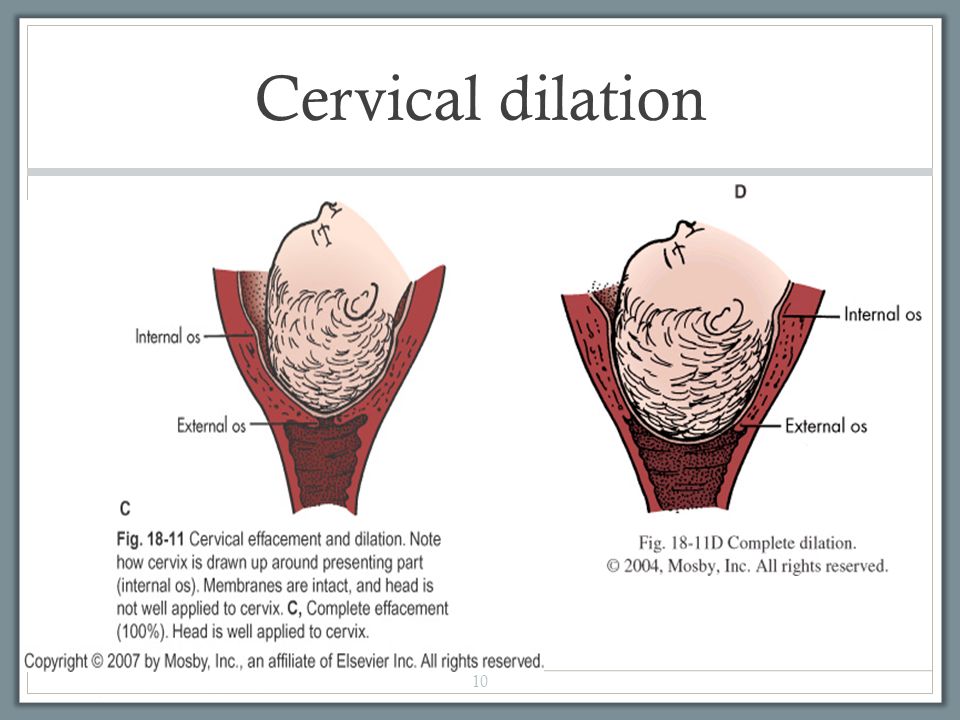
Labor should be induced when further pregnancy is for some reason unsafe for the mother or baby and it is not possible to wait for spontaneous labor to begin.
The goal of stimulation is to start labor by stimulating uterine contractions.
When inducing labor, the patient must be in the hospital so that both mother and baby can be closely monitored.
Labor induction methods
The choice of labor induction method depends on the maturity of the cervix in the patient, which is assessed according to the Bishop scale (when viewed through the vagina, the position of the cervix, the degree of its dilatation, consistency, length, position of the presenting part of the fetus in the area pelvis). Also important is the medical history (medical history) of the patient, for example, a past caesarean section or operations on the uterus.
The following methods are used to induce labor:
- Oral misoprostol is a drug that is a synthetic analogue of prostaglandins found in the body.
 It prepares the body for childbirth, under its action the cervix becomes softer and begins to open.
It prepares the body for childbirth, under its action the cervix becomes softer and begins to open. - Balloon Catheter – A small tube is placed in the cervix and the balloon attached to the end is filled with fluid to apply mechanical pressure to the cervix. When using this method, the cervix becomes softer and begins to open. The balloon catheter is kept inside until it spontaneously exits or until the next gynecological examination.
- Amniotomy or opening of the fetal bladder - in this case, during a gynecological examination, when the cervix has already sufficiently dilated, the fetal bladder is artificially opened. When the amniotic fluid breaks, spontaneous uterine contractions will begin, or intravenous medication may be used to stimulate them.
- Intravenously administered synthetic oxytocin - acts similarly to the hormone of the same name produced in the body. The drug is given by intravenous infusion when the cervix has already dilated (to support uterine contractions).
 The dose of the drug can be increased as needed to achieve regular uterine contractions.
The dose of the drug can be increased as needed to achieve regular uterine contractions.
When is it necessary to induce labor?
Labor induction is recommended when the benefits outweigh the risks.
Induction of labor may be indicated in the following cases:
- The patient has a comorbid condition complicating pregnancy (eg, high blood pressure, diabetes mellitus, preeclampsia, or some other condition).
- The duration of pregnancy is already exceeding the norm - the probability of intrauterine death of the fetus increases after the 42nd week of pregnancy.
- Fetal-related problems, eg, problems with fetal development, abnormal amount of amniotic fluid, changes in fetal condition, various fetal disorders.
- If the amniotic fluid has broken and uterine contractions have not started within the next 24 hours, there is an increased risk of inflammation in both the mother and the fetus. This indication does not apply in case of preterm labor, when preparation of the baby's lungs with a special medicine is necessary before delivery.
- Intrauterine fetal death.
What are the risks associated with labor induction?
Labor induction is not usually associated with significant complications.
Occasionally, after receiving misoprostol, the patient may develop fever, chills, vomiting, diarrhea, and too frequent uterine contractions (tachysystole). In case of too frequent contractions to relax the uterus, the patient is injected intravenously relaxing muscles uterus medicine. It is not safe to use misoprostol if you have had a previous caesarean section as there is a risk of rupture of the uterine scar.
The use of a balloon catheter increases the risk of inflammation inside the uterus.
When using oxytocin, the patient may rarely experience a decrease in blood pressure, tachycardia (rapid heartbeat), hyponatremia (lack of sodium in the blood), which may result in headache, loss of appetite, nausea, vomiting, abdominal pain, depression strength and sleepiness.