Cervical test during pregnancy
Cervical screening during pregnancy | Pregnancy Birth and Baby
Cervical screening during pregnancy | Pregnancy Birth and Baby beginning of content5-minute read
Listen
You may be wondering if it’s safe to have a cervical screening test while you’re pregnant, and whether the benefits outweigh any risks. Routine cervical screening is the best way to protect yourself against cervical cancer. Of the 800 women diagnosed with cervical cancer each year in Australia, 1 in 5 were never screened or were not up to date with screening.
What is cervical screening?
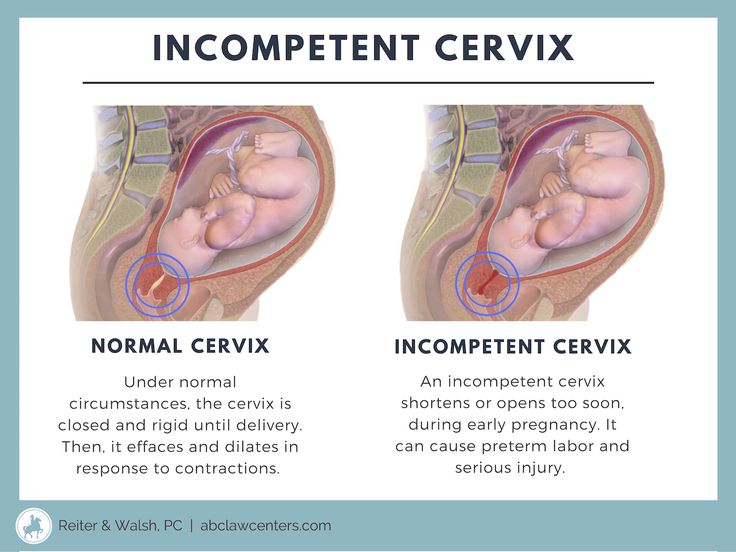
Cervical screening is a simple way to check the health of your cervix. The cervix is the opening of the womb (uterus) at the top of the vagina. The cervical screening test looks for evidence of human papillomavirus (HPV), is a virus that can cause changes to cells in your cervix — which can develop into cervical cancer.
The cervical screening test has replaced the Pap test (or, ‘smear’), which was offered to women every 2 years.
During a cervical screening test, an instrument called a speculum is gently inserted into the vagina, so the health provider performing the screen can see your cervix. A soft spatula or ‘broom’ type brush is then used to collect the sample. The cervical screening test looks and feels the same as the Pap test. The procedure might feel a bit uncomfortable but shouldn’t hurt.
How often should I have a cervical screening test?
Cervical screening can be done every 5 years, if your results are normal. You should have the test if:
- you’re aged between 25 and 74 years
- you have ever been sexually active
- you have a cervix
If you’ve had a Pap test before, your first cervical screening test should be 2 years after your last Pap test.
It’s best to start cervical screening at 25 years of age — studies show there’s no extra benefit to testing women under 25.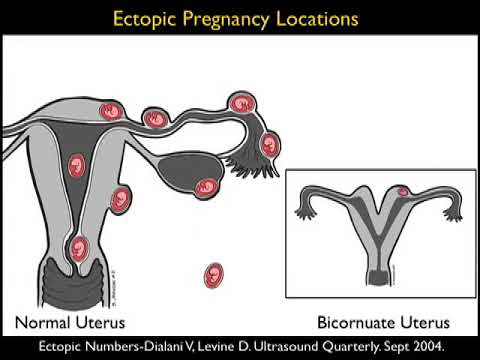 While women under 25 don’t need routine cervical screening, if you have pain during sex, or unusual bleeding or discharge at any age, see your healthcare provider as soon as you can.
While women under 25 don’t need routine cervical screening, if you have pain during sex, or unusual bleeding or discharge at any age, see your healthcare provider as soon as you can.
If you are under 25 years and were previously screened, and received an abnormal test result, you should continue to follow your doctor's advice.
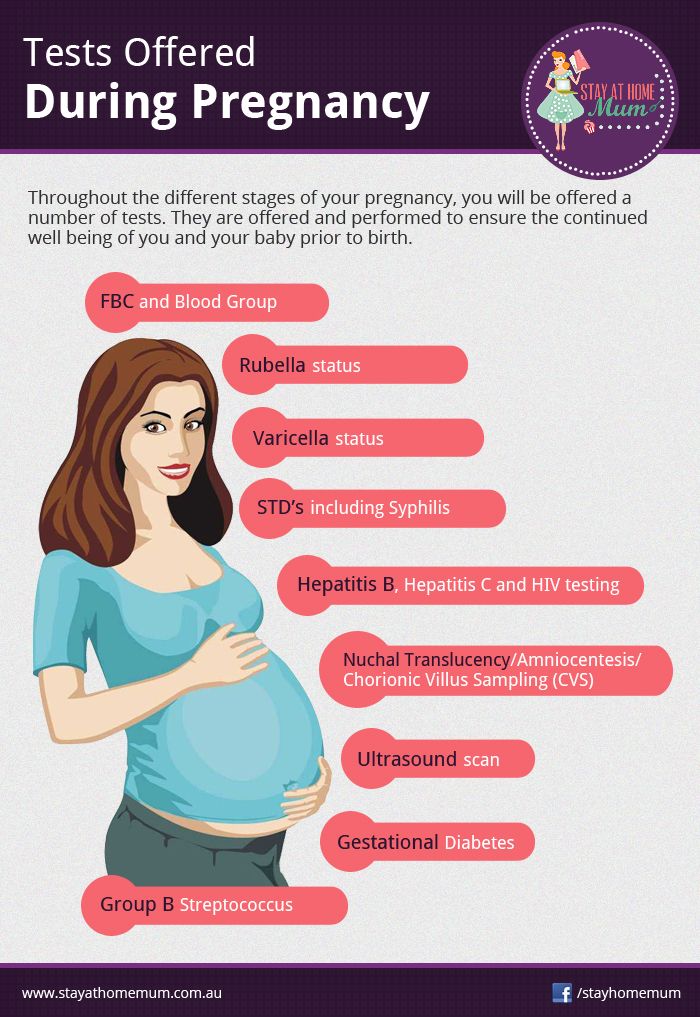
Checkups, scans and tests during pregnancy
Learn more about what checkups, scans and tests you can have during pregnancy.
I'm pregnant — can I have a cervical screening test?
Cervical screening can be performed at any time, including before becoming pregnant and during your pregnancy. Your pregnancy might be the first chance your healthcare provider has to offer you a cervical screening test. Cervical cancer tends to be diagnosed in women who aren’t routinely screened.
Is it part of standard antenatal care?
You may be asked about your cervical screening history during your first antenatal visit, and offered cervical screening if you haven't had one within the recommended time.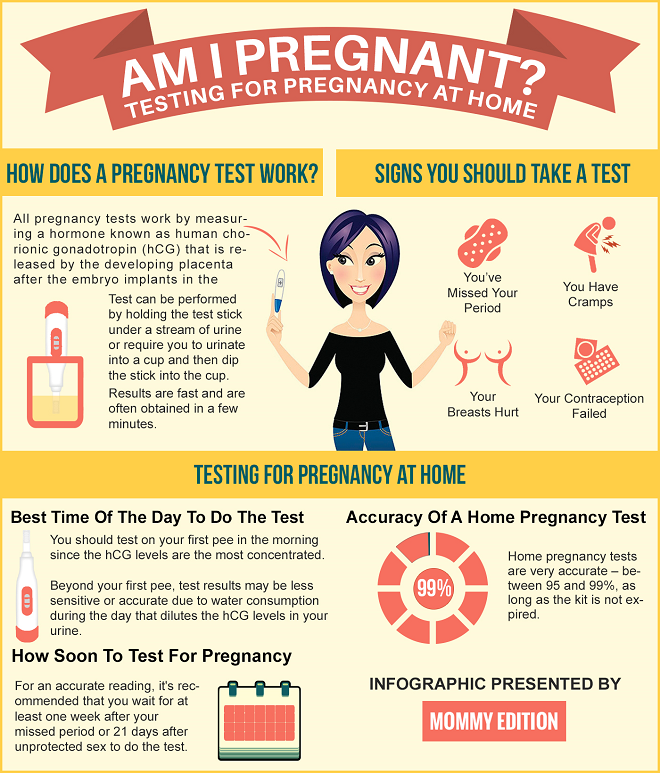 This is an important opportunity to take steps to keep yourself healthy and well, throughout your pregnancy and beyond.
This is an important opportunity to take steps to keep yourself healthy and well, throughout your pregnancy and beyond.
What is 'self-collection' cervical screening and can this be done during pregnancy?
Self-collection is where you are shown how to collect your own sample for cervical screening.
You may be offered the option of self-collection of a vaginal swab for HPV testing. Your healthcare provider should outline the process and discuss the small risk of bleeding or spotting that may occur because of this test.
In some instances, if the test returns a positive result, you may be asked to return to your doctor so they can perform another test.
Is there any danger to the baby?
It’s safe to have a cervical screening test during your pregnancy. The benefits to your health outweigh any risks to your baby.
Whatever the outcome of the screening test, it’s generally safe to continue your pregnancy — since HPV infection during pregnancy doesn’t usually affect the baby.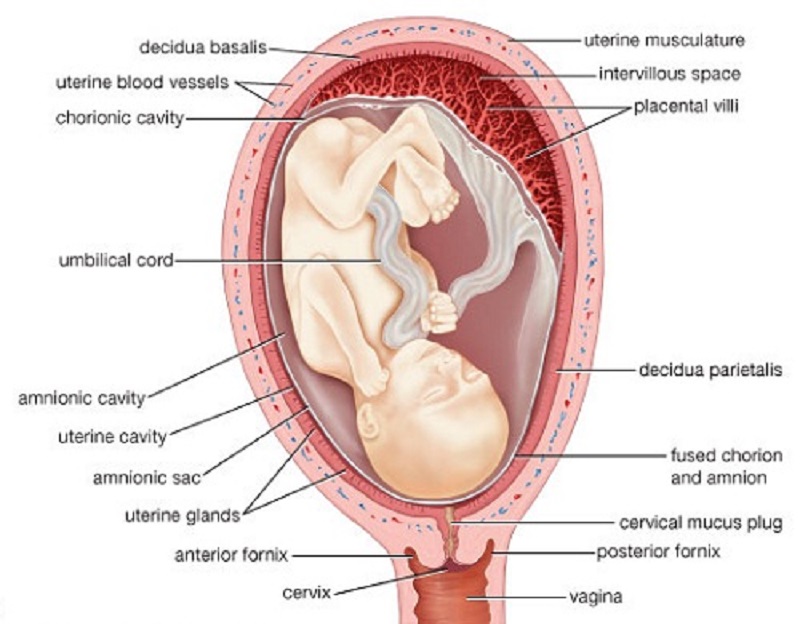 Even if there are abnormal cells on the cervix, it’s very rare for this to progress into cancer during a pregnancy.
Even if there are abnormal cells on the cervix, it’s very rare for this to progress into cancer during a pregnancy.
That’s why, in most cases, your healthcare provider will wait until after your baby is born to do a repeat test and, if necessary, treat cervical cancer.
What happens if the result is not normal?
If your test shows you have HPV, your healthcare provider will monitor the infection and is likely to recommend further tests to better understand the changes to your cervical cells. Even when results show an HPV infection, it normally takes 10 or more years for it to develop into cervical cancer. Only about 1 in 20 pregnant women will have abnormal cervical cells after further investigation.
Sources:
National Cervical Screening Program (Self-collection and the Cervical National Screening Test: Factsheet), National Cervical Screening Program (About the test), The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Cervical screening in Australia), National Cervical Screening Program (Guidelines for the management of screen-detected abnormalities, screening in specific populations and investigation of abnormal vaginal bleeding. Screening in Pregnancy Screening in Pregnancy), Australian Government Department of Health (Pregnancy Care Guidelines: Antenatal Visits), Cancer Council Australia (Cervical cancer screening: summary of recommendations)
Screening in Pregnancy Screening in Pregnancy), Australian Government Department of Health (Pregnancy Care Guidelines: Antenatal Visits), Cancer Council Australia (Cervical cancer screening: summary of recommendations) Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Your first antenatal visit
- Routine antenatal tests
- Check-ups, tests and scans available during your pregnancy
- Antenatal care during your pregnancy
Need more information?
Understanding your Pap test or cervical screening test results | Cancer Council
The Pap test (sometimes called the Pap smear) has changed to the cervical screening test. Find out about how the changes impact you here
Find out about how the changes impact you here
Read more on Cancer Council Australia website
Pap smear tests - MyDr.com.au
Pap smear tests are currently used in Australia as a screening test for cervical cancer. A Pap smear test can detect changes in the cells of the cervix that may develop into cancer.
Read more on myDr website
Cervical Screening | Pap Smear | Jean Hailes
All you need to know about cervical screening tests and how they differ from pap smears. Learn why and when you should have one and how they work.
Read more on Jean Hailes for Women's Health website
Pap Smear Tests | Cervical Screening Tests - Sexual Health Victoria
Cervical Screening (formerly Pap Smear or Pap Test) is a 5-yearly test for those between the ages of 25 – 74 years, to check cervical health.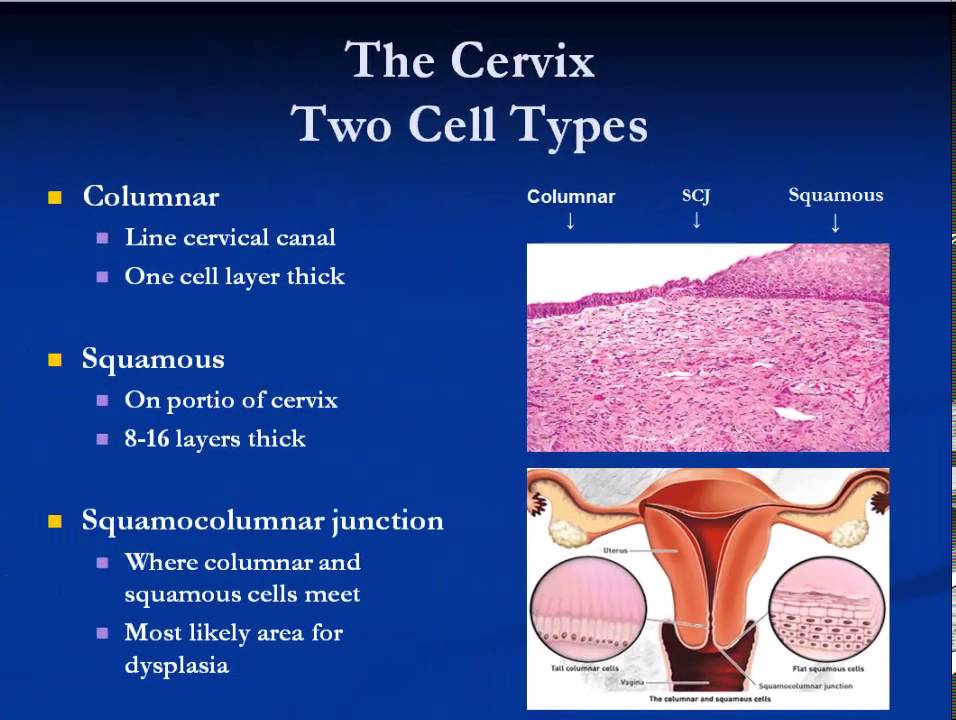 Book an appointmen
Book an appointmen
Read more on Sexual Health Victoria website
Your questions answered on cervical screening tests | Know Pathology Know Healthcare
A cytologist answers questions about cervical cancer screening and why you should get up to date
Read more on Know Pathology Know Healthcare website
Cervical Cancer - Frequently Asked Questions
Frequently asked questions of the Australian Cervical Cancer Foundation. FAQ
Read more on Australian Cervical Cancer Foundation website
Cervical cancer screening | Cancer Council
Read about the cervical screening program designed to work together with the HPV vaccination program, to help reduce the incidence of cervical cancer
Read more on Cancer Council Australia website
What happens if your cervical screening test is positive? | Know Pathology Know Healthcare
Find out how cervical screening tests are performed and what happens when a cervical screening test is positive for HPV
Read more on Know Pathology Know Healthcare website
Cervical screening: what health professionals wish you knew | Know Pathology Know Healthcare
The people who perform your tests told us their messages to women about cervical screening, cancer and why vaccinated and young women still need the test
Read more on Know Pathology Know Healthcare website
Samantha’s story - Surviving HPV related cancer | Australian Government Department of Health and Aged Care
Samantha survived a rare but aggressive form of cervical cancer that her doctor said was highly likely caused by human papillomavirus (HPV). She urges all parents to sign the consent form so their child can be protected against HPV related disease as part of the school based immunisation program.
She urges all parents to sign the consent form so their child can be protected against HPV related disease as part of the school based immunisation program.
Read more on Department of Health and Aged Care website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.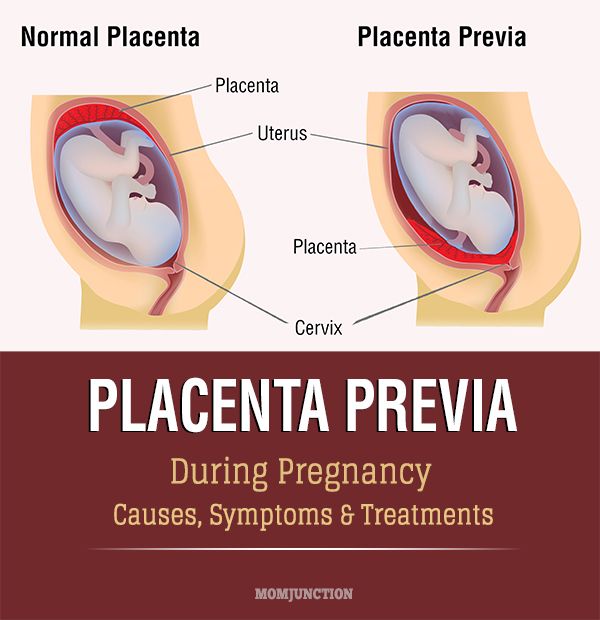
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Pregnancy and abnormal cervical cells | Cervical cancer
Before you become pregnant you should check that you are up to date with your cervical screening.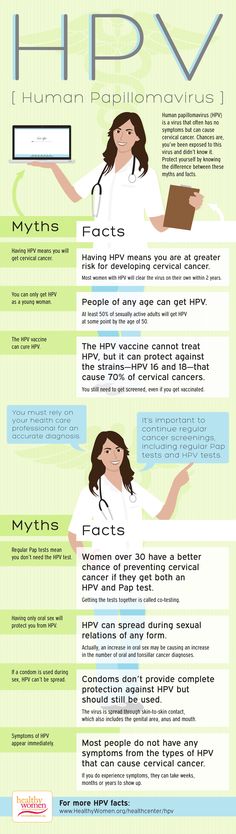 If you are already pregnant you can usually wait and have the test 3 months after you have had your baby.
If you are already pregnant you can usually wait and have the test 3 months after you have had your baby.
For women who are pregnant and have an abnormal screening test it will depend on the result of your test as to what happens next.
Most women can have a normal pregnancy after treatment for abnormal cells but rarely there are problems. You might need treatment to keep future pregnancies safe.
The NHS cervical screening programme say that routine cervical screening tests can usually be delayed in pregnant women until after they have had their baby. Pregnancy can make the result of the test harder to interpret and could be inaccurate.
Planning to become pregnant
If you're planning to become pregnant, it's a good idea to check with your GP that you are up to date with your cervical screening. Then you can have the test and if you need treatment you can have it before you become pregnant.
Already pregnant
If you are already pregnant, and are due to have a cervical screening test, you can usually wait to have the test until 3 months after your baby is born. When you are invited for your test, you should let your GP or clinic know that you are pregnant. They can then delay the test.
When you are invited for your test, you should let your GP or clinic know that you are pregnant. They can then delay the test.
If you've previously had an abnormal result from a cervical screening test, or you haven't had a screening test in the last 3 to 5 years, you may need to have a screening test while you are pregnant. Your GP or midwife might ask you to have the test at your first antenatal appointment. This test is safe to have when you are pregnant.
If the results come back abnormal, or if a test you had just before you became pregnant shows abnormal results, you don't need to worry. This doesn't mean that you have cancer, but that there are some abnormal cells that can be easily treated a few months after the birth.
You may need to have a colposcopy (a close examination of your cervix and vagina) while you are pregnant. This is safe to have during pregnancy, and your doctor can see how much the cells on your cervix have changed.
Treatment for abnormal cells during pregnancy
Remember that if your doctor tells you that you have abnormal cervical cells (or CIN 1, 2 or 3), you don't have cervical cancer.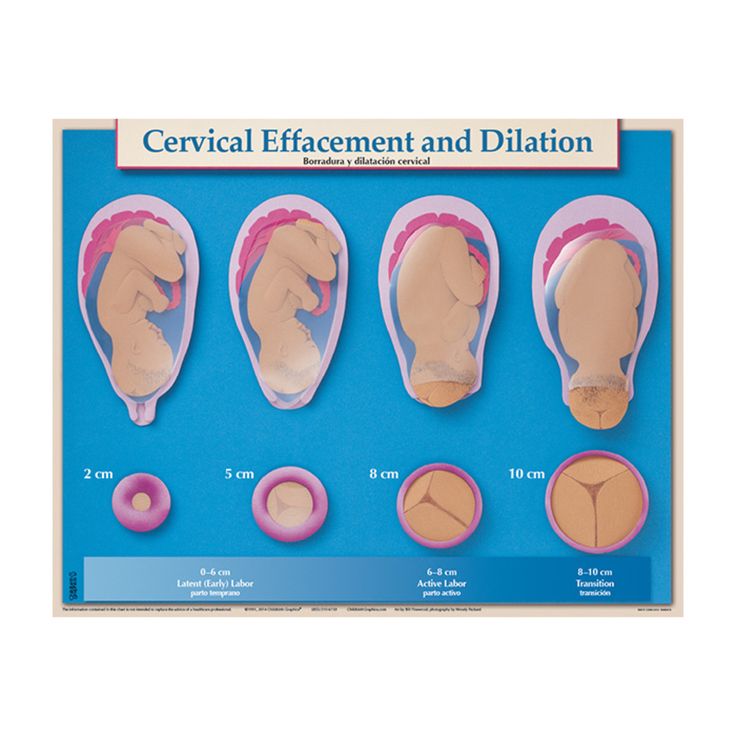 Some of the abnormal cells could eventually turn into cancer if left untreated.
Some of the abnormal cells could eventually turn into cancer if left untreated.
Before giving birth
If you only have mild changes to the cells on your cervix (CIN 1), you won't need to have any treatment until around 3 months after your baby is born. After that, you may have another colposcopy to check the cervical cells again. In many women with mild changes, they go back to normal without any treatment.
If the cells are more abnormal (CIN 2 or 3), your doctor may ask you to have another colposcopy when you are about 6 months pregnant to keep an eye on them. The abnormal cells are not likely to change much over the time of your pregnancy.
If you are pregnant and your colposcopy shows that the cell changes have started to turn into cancer, your doctor will need to take a tissue sample. This is probably by a procedure called LLETZ (large loop excision of the transformation zone). But your specialist will not do this unless it's absolutely necessary.
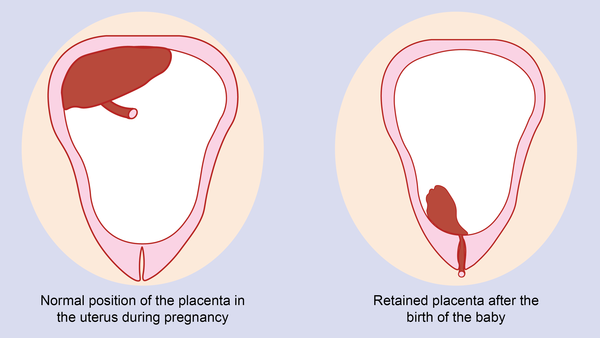
After giving birth
If the cells on your cervix have not gone back to normal after you have given birth, you may then have treatment to remove them.
You can discuss your treatment options and any worries you have with your GP or midwife, or your doctor or specialist nurse at the colposcopy clinic.
It's important to make sure that you go to all of your follow up appointments after you've had your baby.
Pregnancy after a cone biopsy
A cone biopsy removes a cone shaped wedge of tissue from your cervix. It can cause particular problems with future pregnancies. But these are not common.
Ask your doctor how much tissue was removed. If less than 10mm (1cm) was removed then it shouldn't cause problems. If more than 10mm was removed, then in pregnany they can monitor your cervix.
Narrowing of the cervix
After a cone biopsy there is a very small chance that the cervix can narrow. This is called cervical stenosis. The cervix might become so tightly closed that sperm can't get in. If this happened, you wouldn't be able to get pregnant naturally.
If you're having periods after a cone biopsy you have not got complete cervical stenosis. If the lining of the womb can get out when it is shed as a period, then sperm can get in.
If the lining of the womb can get out when it is shed as a period, then sperm can get in.
Some women may need surgery to stretch (dilate) the cervical opening.
Future pregnancies
Some treatments for CIN or very early stage cancer (stage 1A) can lead to a small risk of complications in future pregnancies. Women who have had a cone biopsy have:
- a higher chance of their babies being born before 37 weeks (preterm delivery)
- a higher risk of a baby that weighs less than 2.5kg (low birthweight)
- an increase in birth by caesarean section
You may have an increased risk of early birth because the cone biopsy has weakened your cervix. The cervix is really a muscle that keeps the entrance to the womb closed unless you are in labour.
In some women who have had a cone biopsy, there is a risk that the cervix may start to open too soon because of the weight of the growing baby. Serious problems can usually be prevented.
If your doctor thinks your cervix may start to open too soon, you can have a sort of running stitch put around it to hold it shut.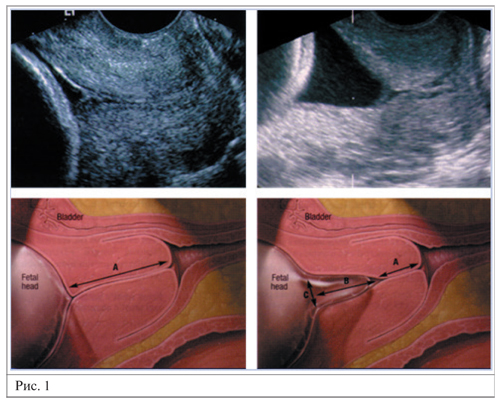 Your doctor may call this a purse string suture. The stitch is cut before you go into labour, usually at about week 37 of your pregnancy. The cervix can then open normally for the baby to come out.
Your doctor may call this a purse string suture. The stitch is cut before you go into labour, usually at about week 37 of your pregnancy. The cervix can then open normally for the baby to come out.
Pregnancy after other treatment
It's very unlikely that any other treatment for abnormal cells, such as laser therapy, cold coagulation or cryotherapy will affect your ability to get pregnant in the future.
The most likely way that these treatments can affect your ability to get pregnant, is if you get an infection after treatment which spreads into your fallopian tubes.
Infection in the fallopian tubes can cause them to become blocked. If both your tubes are blocked, then your eggs can't travel down the tubes into your womb. This would mean that you couldn't get pregnant naturally.
Such a severe infection is unlikely after treatment for abnormal cells. See your GP straight away if you have any symptoms of infection. These can include:
- heavy bleeding, especially if it's more than during a period
- a vaginal discharge that smells or is green or yellow in colour
- period like pains that last more than a day or two
- a high temperature (fever)
LLETZ
As with cone biopsy, studies looking at pregnancy after LLETZ show that there is a small rise in risk of birth before 37 weeks and having a low birth weight baby.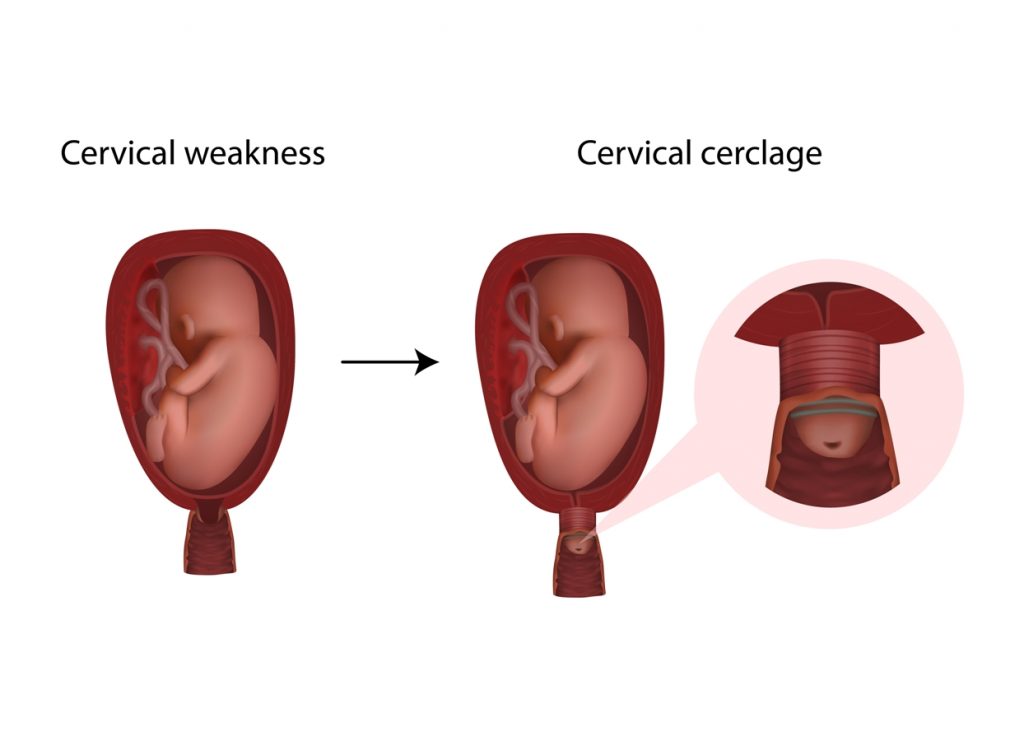 This risk can depend on the amount of cervical tissue that has been removed.
This risk can depend on the amount of cervical tissue that has been removed.
There is also a slight increase in the risk of your waters breaking early (premature rupture of membranes) if you've had treatment with LLETZ.
If you are pregnant, you should let your midwife or doctor know if you have had treatment for abnormal cervical cells.
What to remember
You may feel worried about these risks, but remember:
- the risk of developing serious side effects during pregnancy is small
- if you have cervical abnormalities, having treatment is very important
- your doctor will talk through the treatment options, and discuss any potential risks to future pregnancies
-
NHS Cervical Screening Programme: Colposcopy and Programme Management, 3rd edition
Public Health England, 2016 (Updated Feb 2020). -
Adverse obstetric outcomes after local treatment for cervical pre invasive and early invasive disease according to cone depth: systematic review and meta analysis
M Kyrgiou and others
BMJ, 2016. Volume 354, Issue 3633
Volume 354, Issue 3633 -
The risk of preterm birth following treatment for precancerous changes in the cervix: a systematic review and meta-analysis
F Bruinsma and M Quinn
BJOG: An International Journal of Obstetrics and Gynaecology, 2011. Volume 118, Issue 9 -
Risk of preterm birth after treatment for cervical intraepithelial neoplasia among women attending colposcopy in England: retrospective-prospective cohort study
A Castanon and others
BMJ, 2012. Volume 345, Issue 5174
Last reviewed:
10 Mar 2020
Next review due:
10 Mar 2023
Print page
Changes in the cervix during pregnancy
Pregnancy is always pleasant, but sometimes not planned. And not all women have time to prepare for it, to be fully examined before its onset. And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.
And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.
The cervix is the lower segment of the uterus in the form of a cylinder or cone. In the center is the cervical canal, one end of which opens into the uterine cavity, and the other into the vagina. On average, the length of the cervix is 3–4 cm, the diameter is about 2.5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
Outside, the surface of the cervix has a pinkish tint, it is smooth and shiny, durable, and from the inside it is bright pink, velvety and loose.
The cervix during pregnancy is an important organ, both in anatomical and functional terms. It must be remembered that it promotes the process of fertilization, prevents infection from entering the uterine cavity and appendages, helps to "endure" the baby and participates in childbirth. That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary.
During pregnancy, a number of physiological changes occur in this organ. For example, a short time after fertilization, its color changes: it becomes cyanotic. The reason for this is the extensive vascular network and its blood supply. Due to the action of estriol and progesterone, the tissue of the cervix becomes soft. During pregnancy, the cervical glands expand and become more branched.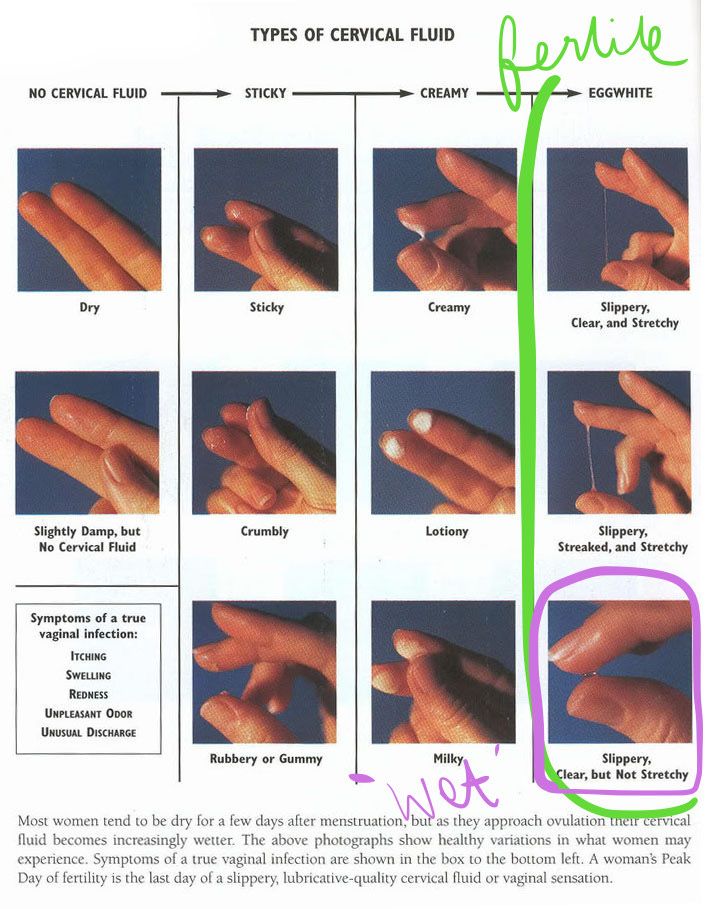
Screening examination of the cervix during pregnancy includes: cytological examination, smears for flora and detection of infections. Cytological examination is often the first key step in the examination of the cervix, since it allows to detect very early pathological changes that occur at the cellular level, including in the absence of visible changes in the cervical epithelium. The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.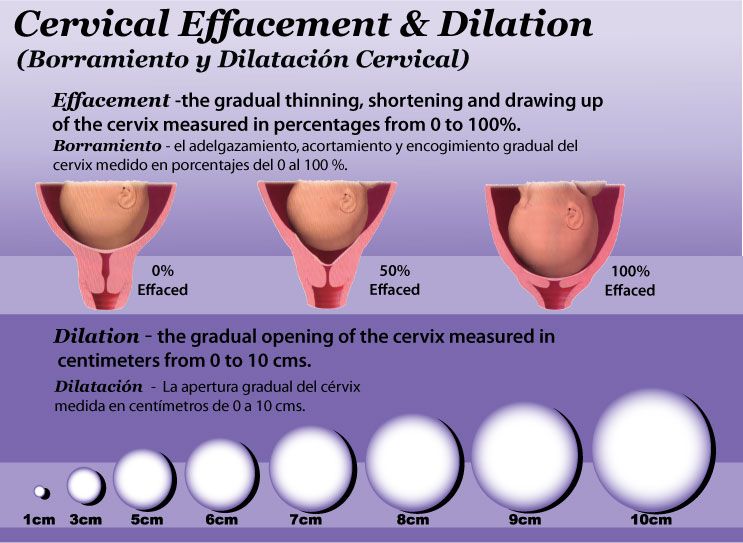
During pregnancy, in addition to physiological changes in the cervix, some borderline and pathological processes may occur.
Under the influence of hormonal changes that occur in a woman's body during the menstrual cycle, cyclic changes also occur in the cells of the epithelium of the cervical canal. During the period of ovulation, the secretion of mucus by the glands of the cervical canal increases, and its qualitative characteristics change. With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
Quite often, in pregnant women, during a mirror examination of the vaginal part, polyps cervix. The occurrence of polyps is most often associated with a chronic inflammatory process. As a result, a focal proliferation of the mucosa is formed, sometimes with the involvement of muscle tissue and the formation of a pedicle. They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows.
The occurrence of polyps is most often associated with a chronic inflammatory process. As a result, a focal proliferation of the mucosa is formed, sometimes with the involvement of muscle tissue and the formation of a pedicle. They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows.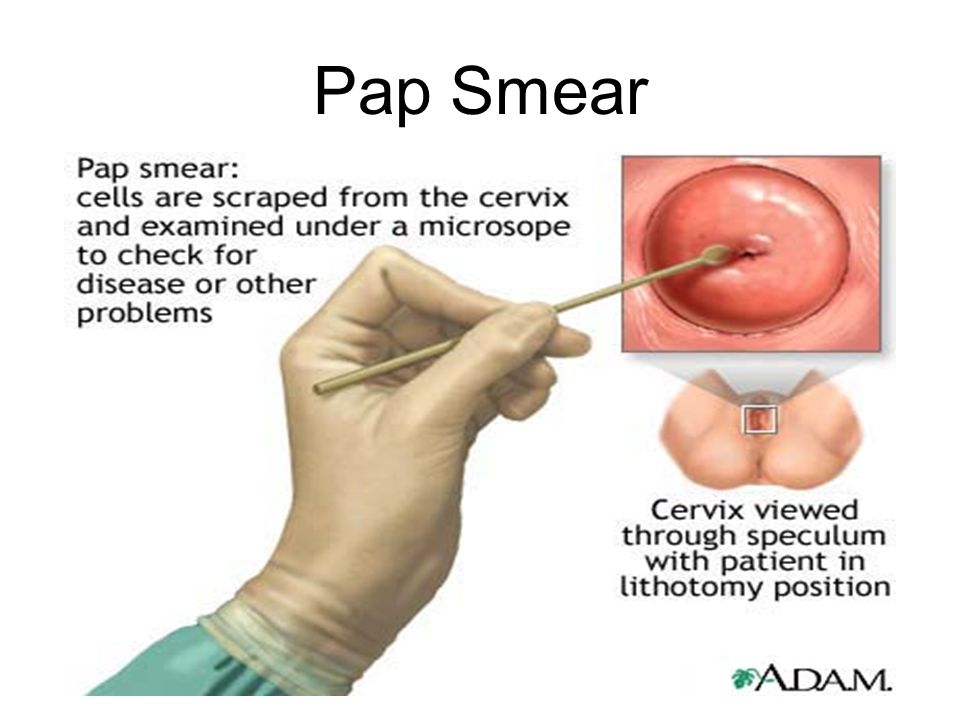 The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
The most common pathology of the cervix in women is erosion . Erosion is a defect in the mucous membrane. True erosion is not very common. The most common pseudo-erosion (ectopia) is a pathological lesion of the cervical mucosa, in which the usual flat stratified epithelium of the outer part of the cervix is replaced by cylindrical cells from the cervical canal. Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease. The reasons may be:
- genital infections, vaginal dysbacteriosis and inflammatory diseases of the female genital area;
- is an early onset of sexual activity and a frequent change of sexual partners.
 The mucous membrane of the female genital organs finally matures by the age of 20-23. If an infection interferes with this delicate process, erosion is practically unavoidable;
The mucous membrane of the female genital organs finally matures by the age of 20-23. If an infection interferes with this delicate process, erosion is practically unavoidable; - is an injury to the cervix. The main cause of such injuries is, of course, childbirth and abortion;
- hormonal disorders;
- , cervical pathology may also occur with a decrease in the protective functions of immunity.
The presence of erosion does not affect pregnancy in any way, as well as pregnancy on erosion. Treatment during pregnancy consists in the use of general and local anti-inflammatory drugs for inflammatory diseases of the vagina and cervix. And in most cases, just dynamic observation is enough. Surgical treatment is not carried out throughout the entire pregnancy, since the excess of risks and benefits is significant, and after treatment during childbirth, there may be problems with opening the cervix.
Almost all women with various diseases of the cervix safely bear and happily give birth to beautiful babies!
Attention! Prices for services in different clinics may vary. To clarify the current cost, select the clinic
To clarify the current cost, select the clinic
The administration of the clinic takes all measures to update the prices for programs in a timely manner, however, in order to avoid possible misunderstandings, we recommend that you check the cost of services by phone / with the managers of the clinic
Clinical Hospital IDKMother and Child Clinic Enthusiastov Samara
All directionsSpecialist consultations (adults)Specialist consultations (children)Molecular genetics laboratoryGeneral clinical examinationsProcedural roomOther gynecological operationsTelemedicine for adultsTherapeutic examinationsAdult ultrasound examinations
01.
Specialist consultations (adults)
02.
Consultations of specialists (children's)
03.
Laboratory of molecular genetics
04.
Adult Telemedicine
08.
Therapeutic Research
09.
Adult Ultrasound
Nothing found
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of the tests by calling
Cervicometry (ultrasound of the cervix) - Reproductive medicine, gynecology, pregnancy monitoring, urology
Cervicometry is an ultrasound examination of the cervix, which allows you to determine in advance the risk of spontaneous abortion or other pathologies of gestation and prevent the problem in a timely manner.
Brief description of the procedure
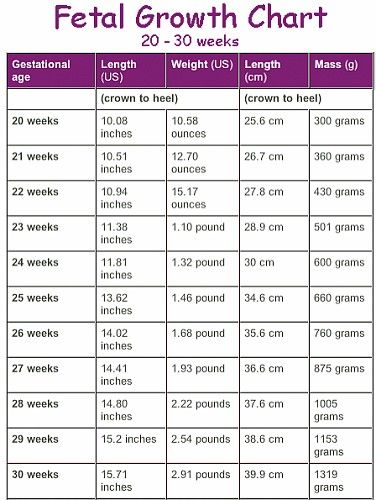
Ultrasound of the cervix during pregnancy is done at different times. As a rule, the procedure is prescribed for a period of 12-22 weeks. But if a woman already had problems with bearing or a multiple pregnancy, then cervicometry is prescribed until the 15th week, and at the 20th week of gestation it is recommended to undergo a second examination.
Cervicometry is performed using a special transfuser, which is inserted into the woman's birth canal. This allows you to comprehensively assess the condition of the neck of the organ, measure its length and inspect the inner surface of the cervical canal.
Ultrasound of the cervix during pregnancy is safe not only for the woman, but also for the unborn child. The channel is measured both externally and internally. More objective data is obtained by measuring the channel from the inside.
Who should be screened
Cervicometry is recommended for women during gestation if:
- a multiple pregnancy is diagnosed;
- before conception, an operation was performed on the reproductive organs;
- was previously diagnosed with isthmic-cervical insufficiency;
- the cervix is shortened.
When analyzing the results, the doctor compares the results obtained with the reference and gives a conclusion about the risk of miscarriage.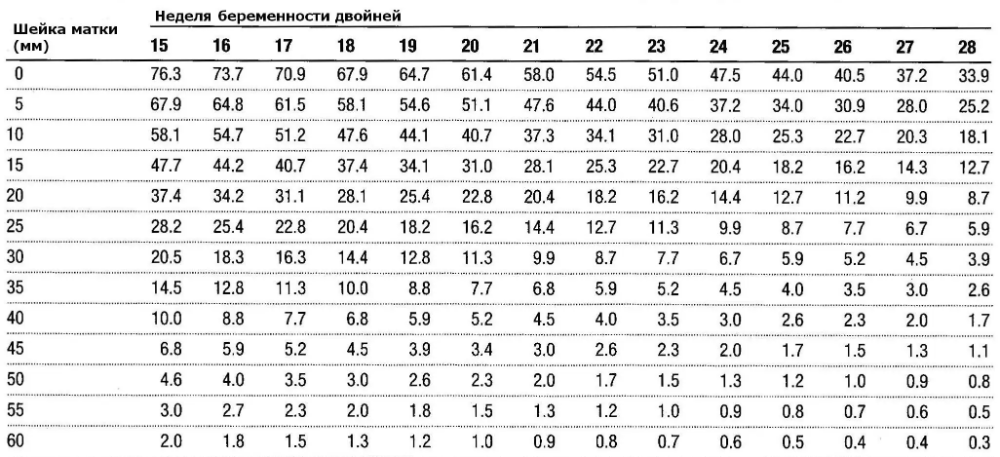
Pre-laboratory preparation
Preparation for ultrasound does not differ from similar studies of other organs of the reproductive system, except for one point - for examination, the woman's bladder must be emptied of the contents, since the full bladder does not allow visualization of the cervix. It is also desirable that the intestines be empty and not gassed, for which it is allowed to take Espumizan or Almagel the day before.
Reference values and interpretation of indicators
Ultrasound of the cervix during pregnancy shows changes in canal length at different gestational ages:
| Gestational timing (weeks) | Length of cervical canal (mm) |
| 16-20 | 40-45 |
| 24 | ~37 |
| 25-28 | 35-40 |
| 32-36 | 30-35 |
If the length is less than the reference values, then the risk of miscarriage is very high.