Cervical pictures during pregnancy
What Does A Cervix Look Like? 7 Cervix Pictures, Explained
Think of your cervix as the gatekeeper to your uterus. Lots of things—like tampons, fingers, penises, sex toys, and other germ-carrying items—can get to your cervix, but they aren't getting past it. Your cervix, in its 24/7 role of keeping your uterus happy and healthy, won't let that happen.
Likewise, there are things—like mucous, menstrual blood, and the occasional baby—that need to get out of your uterus. Your cervix is the bouncer, deciding what and when things go in and come out of the most vital piece of your reproductive system. Yet, despite benefiting from its work, day in and day out, chances are you don't know much about it.
So...what does a cervix even look like?
Great Q! Your cervix is the "neck" of your uterus, positioned at the top of your vaginal canal. Because of its location, seeing your cervix isn't as easy as squatting over a hand mirror, like you would if you were examining your other lady bits, but it is possible with the right tools.
All you need is a flashlight, a mirror, a retractable speculum, and a little courage. If you don't have a speculum just lying around your bathroom (and if you do, we want to hear that story!) you can buy a starter kit for $22.95 from the Beautiful Cervix Project. It even comes with a handy map to guide you through your own nethers. Once there you can admire the beauty of your own, unique cervix and even snap some cervix pictures if you're so inclined. (Use this handy video guide for tips on getting a good picture of your vaginal canal and cervix.)
The Beautiful Cervix Project is a movement to better understand and appreciate the awesomeness of the underrated cervix. O’Nell Starkey started it as a project for midwifery school, with her husband taking snaps of her cervix throughout her cycle. She quickly discovered, as she's put it, “Cervices are amazing!”
After sharing her images with the world, she found that other women also wanted to see their own cervices (that's plural for cervix!), leading her to start the Beautiful Cervix Project, as well as live workshops dedicated to helping women learn about and appreciate their bodies.
"What I have learned by creating this website is that people from all over the world are curious about their bodies, cervices, and the menstrual cycle—everyone from newly menstruating teens, pregnant people, medical students, people with abnormal Paps, to people trying to conceive, artists, educators, and the list goes on," Starkey says. "Cervical self-exam is about educating and empowering people by contradicting some of the shame and under-education we have about our bodies and menstrual cycles.
The Beautiful Cervix Project is dedicated to people working to reclaim their entire bodies as beautiful and lovable. The more we know about ourselves, the more we feel confident to advocate and care for ourselves."
While each cervix is slightly different (which is why we recommend checking out your own cervix!), they all go through similar changes during your monthly cycle, when you're pregnant, during labor and delivery, and after giving birth. Curious? Starkey was kind enough to share some cervix pictures to help you see what your cervix is up to...right now.
Curious? Starkey was kind enough to share some cervix pictures to help you see what your cervix is up to...right now.
During the Follicular Phase
When your cervix is just hanging out, the visible part of the cervix protrudes into the vaginal canal and is covered by smooth, pink, squamous epithelium, says Kim Thornton, M.D., a reproductive endocrinologist at Boston IVF. In this picture, the cervix is preparing for ovulation by preparing more fluid.
During Ovulation
The cervix looks a little bit like a donut. When it's closed, the hole looks like a dimple, but it opens during ovulation to let sperm in, explains Ronald D. Blatt, M.D., gynecologist and chief surgeon and medical director of the Manhattan Center for Vaginal Surgery.
During the Luteal Phase
After ovulation, the cervix prepares for menstruation. In this picture the cervix is just doing its thing, waiting for either a pregnancy or shark week to happen. The average cervix measures 3 to 5 centimeters in length and 2 to 3 centimeters in diameter, Thornton says.
The average cervix measures 3 to 5 centimeters in length and 2 to 3 centimeters in diameter, Thornton says.
During Menstruation
When your flow comes to visit, you know the blood is coming from somewhere up in there, but this picture shows exactly how it comes out of your cervix. Again, the dimple in the center—called the os—is in the open position to release menstrual fluids, Blatt says.
During Sex
This is a picture of the cervix just minutes after the woman had an orgasm during sex (you can even see the semen pooled around the bottom). Depending on the size of you and your partner's anatomy, the penis can bump into the cervix during sex. Some women find the sensation enjoyable and may even orgasm from it, according to a study published in the journal Hormones and Behavior. Others find repeated thrusting into the cervix to be incredibly painful and it can cause bruising or even tearing of your cervical tissue.
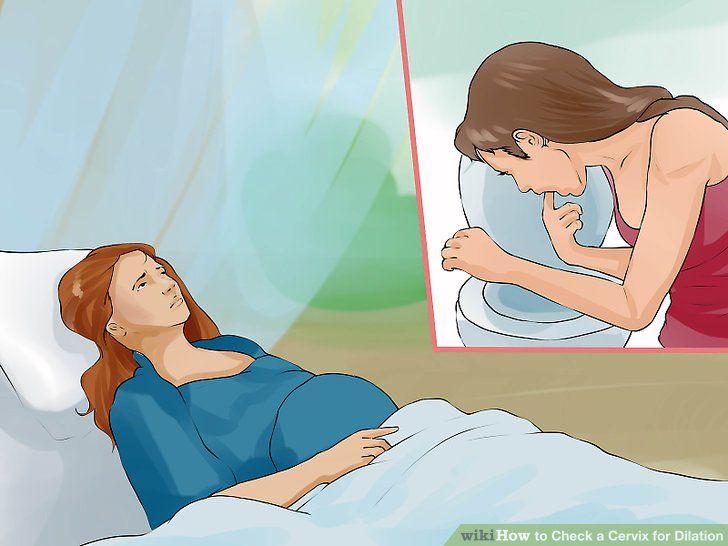
During Pregnancy
Your sex life and monthly cycle may keep your cervix busy, but the real work happens during pregnancy and delivery. In this picture, the woman is about two months pregnant. The white goo, called leukorrhea, is very common type of vaginal discharge that can occur during pregnancy and is nothing to worry about, Starkey says.
During a Pap Smear
Getting swabbed for a Pap smear and HPV test isn't anyone's idea of a good time but it's a necessary evil to catch cervical cancer and other diseases before they can cause more harm. But you don't have to do them every year, says Devorah Daley, M.D., ob-gyn at Weill Cornell Medicine and NewYork-Presbyterian. "The recommendation is to have your first Pap smear at age 21—it does not matter when sexual activity has started," she says. "After that, for younger women, every other year is sufficient. Starting at age 30, we recommend every three years if you're doing just the Pap. "
"
If, however, you get co-tested—meaning your Pap and HPV tests are collected at the same time—Dr. Daley says you can stretch that time frame out to five years. "Even if you were to leave the office and come in contact with [HPV], it doesn't cause initial problems for about five years," she says.
It's believed that more than 90 percent of cervical cancer cases are caused by HPV, according to the Centers for Disease Control and Prevention, with higher incidence rates among Black and Hispanic people. However, it's hard to know whether that prevalence is due to socioeconomic factors (such as access to health care) or other variables.
Amy Wilkinson
Amy Wilkinson is an entertainment editor who also specializes in health and wellness. When not editing or writing, she can be found teaching Pilates as a comprehensively certified instructor.
Age 25 – Entire Cycle
This 25 year old woman has never given birth and has no history of STIs. Each photo was taken at approximately 10:00 pm every day starting the first day of her menstrual cycle. For the duration of this project, she used condoms as her birth control method so as not to introduce semenal fluid into the photoshoot. She did not use tampons or mooncups during her menstruation either.
Each photo was taken at approximately 10:00 pm every day starting the first day of her menstrual cycle. For the duration of this project, she used condoms as her birth control method so as not to introduce semenal fluid into the photoshoot. She did not use tampons or mooncups during her menstruation either.
This cycle is of normal/average length for her, about 33 days. Her cycle’s follicular phase (variable number of days preovulation) lasts until about day 20 or 21. Her fertile phase lasts from days 13 to 21 with ovulation on day 20. Her luteal (postovulation) phase is 13 days long (12-16 days is the norm and is not variable in a normal cycle).
This is a graph of her basal body temperature for this cycle. As you can see, after ovulation on about day 20, her temperature began to rise due to the heat-inducing hormone progesterone produced by the corpus luteum. This temperature shift signifies that ovulation has already occurred. The coverline would be drawn at 97. 4 F. Check out more information about the Fertility Awareness Method of birth control to learn more about cyclical temperature changes.
4 F. Check out more information about the Fertility Awareness Method of birth control to learn more about cyclical temperature changes.
You may notice on the right side of some photos, some jagged looking skin, which is the remnants of her hymenal ring. Her os (opening in the cervix) is round because she has never given birth; the os becomes more of a slit after childbirth. On the sides of the photos, you can see her vaginal rugae, which are the ridges that make the elastic muscular canal of the vagina able to open/expand dramatically during arousal and childbirth.
She also tracked the depth/movement of her cervix in her vagina. These gradual shifts are not really distinguishable in the photos, but was a tangible change as the depth she needed to reach a finger inside to touch her own cervix varied slightly each day. She also noted the firmness of the cervix and openness of the os – again a change she was feeling with her finger.
Her uterus is tipped backward (retroflexed), so you may notice that the cervix is pointing upwards in some photos.:strip_icc():format(jpeg)/kly-media-production/medias/2785562/original/028627600_1556001360-shutterstock_1019963743.jpg) The body of the uterus lies more towards her back than over her bladder as it does in most women. Much scientific literature states that a retroflexed uterus is an anatomical variation that is present in about 20-30% of the population, and sometimes considered a genetic trait. Another perspective is that proper alignment of all the pelvic organs can help tonify a woman’s fertility, ease menstrual cramps, and allow the proper flow of blood, lymph, nerve & chi energy. Attention to posture, Mayan abdominal massage, and addressing underlying inflammation or injuries might help right the uterus into an anteverted position.
The body of the uterus lies more towards her back than over her bladder as it does in most women. Much scientific literature states that a retroflexed uterus is an anatomical variation that is present in about 20-30% of the population, and sometimes considered a genetic trait. Another perspective is that proper alignment of all the pelvic organs can help tonify a woman’s fertility, ease menstrual cramps, and allow the proper flow of blood, lymph, nerve & chi energy. Attention to posture, Mayan abdominal massage, and addressing underlying inflammation or injuries might help right the uterus into an anteverted position.
Day One
Blood – red , clotty and heavy flow
Cramps – mild
Breasts – de-swelling
Feeling – very sexual and tender
Day Two
Blood – Dark red, medium/light flow
Breasts – normal
Basal body temperature – 97. 2 F (and remains between 97 F and 97.4 F until day 20)
2 F (and remains between 97 F and 97.4 F until day 20)
Day Three
Blood – Brown and watery dark red, low flow
Day Four
Brown Spotting with some dark red flecks (note fresh blood at os)
Day Five
Light brown discharge; very low flow
Tender, heart-achey
Tired
Day Six
Very light brown discharge
Sticky cervical fluid when touched between fingers
Day Seven
Cervix in low closed position
Cervical fluid sticky
Day Eight
Cervix low and closed/firm
Cervical fluid white and sticky
Day Nine
Cervix low and closed
Dry sensation
Day Ten
Cervix low and closed
Notice blood spot near os and brown clot near cervix (right). This is not mid-cycle spotting as she is not ovulating yet. This woman has been diagnosed with an endometrial polyp that occasionally causes bleeding mid-cycle, usually unrelated to intercourse.
This is not mid-cycle spotting as she is not ovulating yet. This woman has been diagnosed with an endometrial polyp that occasionally causes bleeding mid-cycle, usually unrelated to intercourse.
Day Eleven
Cervical fluid is creamy
Day Twelve
Cervical fluid white and wet, milky
Feeling particularly sexual
Day Thirteen
Copious watery cervical fluid
Cervix softening and moving upwards
Day Fourteen
White/clear watery cervical fluid, dripping
Day Fifteen
Cervical fluid changed to more eggwhite texture
Cervix is soft, open and high
Day Sixteen
Cervical fluid alternately wet and eggwhite consistency
Cervix soft and high
Day Seventeen
Cervical fluid is very gelatainous (here seen covering os) and streaked with whitish yellow
Sensitive, sensual breasts (not painfully tender)
Stringy Fluid when stretched between fingers (above)
Day Eighteen
Eggwhite fluid
Day Nineteen
More white-tinged eggwhite fluid
Very stretchy and strong Fluid (above)
Day Twenty
Mild back pain and cramp on left side (mittelschmerz)
Ovulation suspected!
Feeling very sexual
Cervical Fluid gelatinous and egg-white (right)
Os very open
Day Twenty One
Drier/chunkier cervical fluid – drying up pattern
Nipples very tender and painful
Basal Body temperature beginning to rise, today 97. 7 F, confirming ovulaiton
7 F, confirming ovulaiton
Day Twenty-Two
Tender nipples
Cervical position is middle
Day Twenty-Three
Very tender nipples
Dry feeling
Day Twenty-Four
Very tender nipples
Dry feeling
Cervix feels hard and high again
Day Twenty-Five
Headache and tired
Dry/tacky
Day Twenty-Six
Breasts swelling
Tacky cervical fluid
Basal Body temperature now very noticeably higher than preovulation by about 1 degree Farenheit. It is now 98.1 F and ranges from 98.1 F to 98.6 F for the rest of this of cycle
It is now 98.1 F and ranges from 98.1 F to 98.6 F for the rest of this of cycle
Day Twenty-Seven
Tender nipples, swollen breasts
Tacky cervical fluid
Day Twenty-Eight
Dry feeling
Day Twenty-Nine
Dry feeling
Day Thirty
Dry feeling
Breasts feel heavy
Day Thirty-One
Feeling bloated
Dry fluid (note fresh blood at os, sign of impending menses)
Feeling emotionally tender
Day Thirty-Two
Very light brown spotting
Cervix low and open
Feeling tired
Day Thirty-Three
Pink spotting
Lower back ache
Menses begins tomorrow upon waking, 13 days after ovulation (luteal phase)
Feel free to comment below. Please know that we ‘censor’ the comments, so you needn’t bother saying something mean, derogatory, pornographic, or sexist as posting such comments does not further the vision of this project or the health of the world.
Please know that we ‘censor’ the comments, so you needn’t bother saying something mean, derogatory, pornographic, or sexist as posting such comments does not further the vision of this project or the health of the world.
Changes in the cervix during pregnancy
Pregnancy is always pleasant, but sometimes not planned. And not all women have time to prepare for it, to be fully examined before its onset. And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.
The cervix is the lower segment of the uterus in the form of a cylinder or cone. In the center is the cervical canal, one end of which opens into the uterine cavity, and the other into the vagina. On average, the length of the cervix is 3–4 cm, the diameter is about 2.5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
Outside, the surface of the cervix has a pinkish tint, it is smooth and shiny, durable, and from the inside it is bright pink, velvety and loose.
The cervix during pregnancy is an important organ, both in anatomical and functional terms. It must be remembered that it promotes the process of fertilization, prevents infection from entering the uterine cavity and appendages, helps to "endure" the baby and participates in childbirth. That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary.
During pregnancy, a number of physiological changes occur in this organ. For example, a short time after fertilization, its color changes: it becomes cyanotic. The reason for this is the extensive vascular network and its blood supply. Due to the action of estriol and progesterone, the tissue of the cervix becomes soft. During pregnancy, the cervical glands expand and become more branched.
Screening examination of the cervix during pregnancy includes: cytological examination, smears for flora and detection of infections. Cytological examination is often the first key step in the examination of the cervix, since it allows to detect very early pathological changes that occur at the cellular level, including in the absence of visible changes in the cervical epithelium. The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
During pregnancy, in addition to physiological changes in the cervix, some borderline and pathological processes may occur.
Under the influence of hormonal changes that occur in a woman's body during the menstrual cycle, cyclic changes also occur in the cells of the epithelium of the cervical canal. During the period of ovulation, the secretion of mucus by the glands of the cervical canal increases, and its qualitative characteristics change. With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
Quite often, in pregnant women, during a mirror examination of the vaginal part, polyps cervix. The occurrence of polyps is most often associated with a chronic inflammatory process. As a result, a focal proliferation of the mucosa is formed, sometimes with the involvement of muscle tissue and the formation of a pedicle. They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
The most common pathology of the cervix in women is erosion . Erosion is a defect in the mucous membrane. True erosion is not very common. The most common pseudo-erosion (ectopia) is a pathological lesion of the cervical mucosa, in which the usual flat stratified epithelium of the outer part of the cervix is replaced by cylindrical cells from the cervical canal. Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease. The reasons may be:
Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease. The reasons may be:
- genital infections, vaginal dysbacteriosis and inflammatory diseases of the female genital area;
- is an early onset of sexual activity and a frequent change of sexual partners. The mucous membrane of the female genital organs finally matures by the age of 20-23. If an infection interferes with this delicate process, erosion is practically unavoidable;
- is an injury to the cervix. The main cause of such injuries is, of course, childbirth and abortion;
- hormonal disorders;
- , cervical pathology may also occur with a decrease in the protective functions of immunity.
The presence of erosion does not affect pregnancy in any way, as well as pregnancy on erosion. Treatment during pregnancy consists in the use of general and local anti-inflammatory drugs for inflammatory diseases of the vagina and cervix.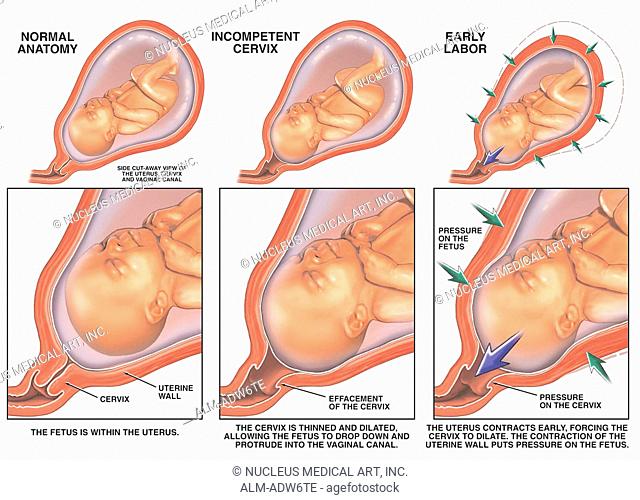 And in most cases, just dynamic observation is enough. Surgical treatment is not carried out throughout the entire pregnancy, since the excess of risks and benefits is significant, and after treatment during childbirth, there may be problems with opening the cervix.
And in most cases, just dynamic observation is enough. Surgical treatment is not carried out throughout the entire pregnancy, since the excess of risks and benefits is significant, and after treatment during childbirth, there may be problems with opening the cervix.
Almost all women with various diseases of the cervix safely bear and happily give birth to beautiful babies!
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
Clinical Hospital of IDKClinic "Mother and Child" Entuziastov Samara
All directionsSpecialist consultations (adults)Specialist consultations (children's)Laboratory of molecular geneticsGeneral clinical examinationsProcedural roomOther gynecological operationsTelemedicine for adultsTherapeutic examinationsUltrasound examinations for adults
01.
Specialist consultations (adults)
02.
Specialist consultations (children)
03.
Laboratory of molecular genetics
04.
General studies
05.
Procedure cabinet
06.
other gynecological operations
07.
Telemedicine for adults
08. examinations
09.
Adult ultrasound examinations
Nothing found
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of the tests by calling
FIRST SIGNS OF PREGNANCY
All girls have heard about the first signs of pregnancy, the so-called discharge .
How else can you tell if you are pregnant or not? Let's say you had a long delay in your menstrual cycle. Time flies, and menstrual bleeding does not start. In this case, you will systematically feel nausea, while the mammary glands will seem heavy to you.
In this case, you will systematically feel nausea, while the mammary glands will seem heavy to you.
In addition to discharge, another sign of pregnancy is the constant thirst for sleep. The everyday activities of the people around you are annoying, and besides, you become very nervous about the presence of certain smells.
In addition to discharge, the first sign of pregnancy is an increase in appetite. Food begins to evaporate from your refrigerator at an astonishing rate and in a variety of combinations of ingredients. At the same time, saliva may still flow, and the number of midnight trips to the toilet will also increase. During the day, you can’t walk for a long time either, this is problematic because of the constant desire to urinate.
All of these discharges and other signs may be present both together and separately. Often a woman talks about a delay in the menstrual cycle in the absence of any deviations in her state of health.
There is an accessible and easy way to clarify these facts. Of course, no method will give you 100% guarantees. You can get a reliable 100% conclusion only after an examination by a gynecologist and a special diagnosis (examination). However, when the first signs of pregnancy appear (discharge, etc.) in the initial 10-12 days of the deviation of the menstrual cycle from the chronology, even in a good clinic you will not be able to guarantee the results of studies to determine pregnancy.
Of course, no method will give you 100% guarantees. You can get a reliable 100% conclusion only after an examination by a gynecologist and a special diagnosis (examination). However, when the first signs of pregnancy appear (discharge, etc.) in the initial 10-12 days of the deviation of the menstrual cycle from the chronology, even in a good clinic you will not be able to guarantee the results of studies to determine pregnancy.
If menstruation does not start at the expected time, then after waiting for the morning, measure the body temperature in the rectum. An ordinary thermometer (medical, of course) is inserted into the rectum as soon as you wake up. Do not get out of bed while performing this operation. Doctors advise to prepare a thermometer in the evening and put it near the bed.
Need more than 6 hours of sleep. The thermometer is inserted behind the muscle that compresses the anus. The insertion depth of the thermometer is 2 centimeters, and the measurement time is from five to seven minutes. Record the measurement results. Measure body temperature every day for 7-10 days. If the temperature is most often more than 37 C, then this indicates the presence of the first signs of pregnancy.
Record the measurement results. Measure body temperature every day for 7-10 days. If the temperature is most often more than 37 C, then this indicates the presence of the first signs of pregnancy.
In the absence of menstruation for 3 or more days, as well as in the presence of the first signs of pregnancy (discharge), gynecologists recommend doing a test to determine early pregnancy (most of the tests that are commercially available detect the presence of pregnancy already on the 1st day of delay !). They are easy to use and quite reliable.
The confidence probability of the test turns out to be much greater if it is carried out two or three times.
Outwardly, these tests are all different, but they are based on one chemical reaction to a specific hormone called human chorionic gonadotropin. This hormone is produced during pregnancy. The breakdown products of the hormone are excreted in the urine. The chemical reagent that drinks the dough plate interacts with these products.
Check that the test has not expired. For the experiment, the purpose of which are the first signs of pregnancy (discharge, etc.) it is better to use morning urine. After sleep, the content of the hormone and its decay products in the female body increases. This means that the probability that the tester will detect this increases. If you are a person who does not trust such tests, then as an option, you can do a urine test to quantify the content of hCG. Although, this analysis is carried out by far not every medical and diagnostic center.
Suppose 3-4 weeks have passed, the temperature in the rectum is systematically over 37 degrees, and the test for determining signs of pregnancy gave a positive result 2 times. At the same time, you feel great, there are no subjective disorders and you are full of energy. There may even be an emotional upsurge. Do you need a women's consultation to determine the first signs of pregnancy? Need. To begin with, to confirm that the pregnancy is uterine, and also that the fetal egg was formed precisely in the uterine cavity.
In the normal course of pregnancy, fertilization occurs in the uterine cavity itself. After all, a fertilized egg must reach the site of implantation (through the fallopian tube). If there are any obstacles in the way of the fetal egg (narrowing in the fallopian tube or in the tubal angle of the uterus), and also if the fertilized egg moves for a very long time, or the egg is too large to pass the fallopian tube, then such an egg will not enter the uterine cavity.
In this case, an ectopic or ectopic pregnancy may occur and develop. Remember that an ectopic pregnancy in the earliest period shows the same qualitative reactions as the uterine one. In general, the first signs of pregnancy, discharge for example, are universal for pregnancy in the general case.
A gynecologist can detect only indirect first signs of pregnancy, such as plethora of the external genital organs, discoloration of the mucous membrane of the cervix and vagina. It turns blue (acquires a cyanotic hue). In addition, softening of the isthmus (the place where the body of the uterus and its cervix connects) may be noted.
In addition, softening of the isthmus (the place where the body of the uterus and its cervix connects) may be noted.
In general, the body of the uterus may be quite large and soft, and may also appear asymmetrical due to swelling at the site of implantation of the ovum.
The uterine appendages are palpated (felt) by a gynecologist. Sometimes it happens that during a normally developing pregnancy, growths are found in the places where the appendages of the cervix are projected. These changes are usually reversible and the normal structure of the ovary is gradually restored. Such growths may appear as corpus luteum or corpus luteum cysts. However, these formations can also be pathological.
To find out if this is the case, you need to resort to other methods of determining the presence of discharge and other first signs of pregnancy.
Ultrasound of the pelvic organs is the safest method. Depending on which research method is chosen (transvaginal or transabdominal), already three weeks after conception, you can get information about the fact of pregnancy, as well as its localization.