Can you miscarriage and not know
How to tell if a miscarriage has happened
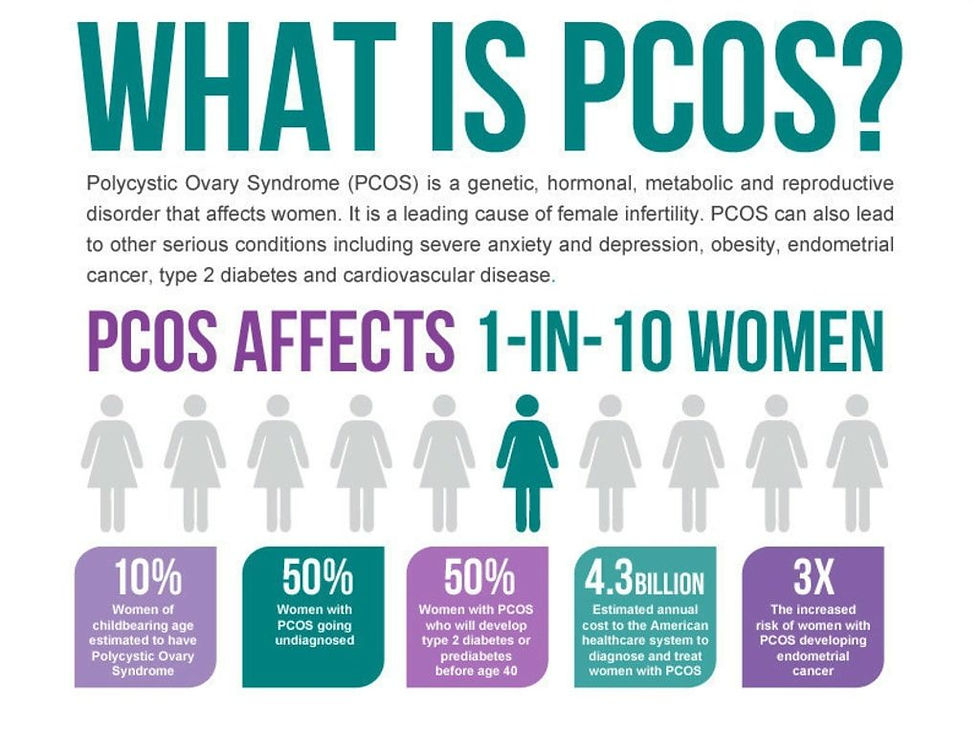
If you’ve heard the term miscarriage, you probably know that it means the loss of a pregnancy before 20 weeks’ gestation. Miscarriage is something that no one wants to think about during early pregnancy, but 10-20% of all known pregnancies end in miscarriage. Being able to recognize miscarriage symptoms and knowing what to do next can help you be more prepared in case one happens.
Miscarriage symptoms
A miscarriage can happen suddenly or gradually, which means that you may not notice any particularly early symptoms of a miscarriage. But no matter how fast it happens, key symptoms include:
- Pink, red or brown vaginal bleeding or spotting
- Cramps or pain in the lower abdomen
- Passing tissue or blood clots from the vagina
Every miscarriage is different. The heaviest bleeding and cramps may be over within a few hours, but bleeding could continue off and on for as long as three weeks. And although most people experience cramps, a miscarriage isn’t always painful.
Both vaginal spotting and mild cramps are common during early pregnancy, so it’s possible to have a miscarriage and not know it. This is why you should call your care provider if you experience any of the above symptoms once you’ve confirmed your pregnancy.
When do miscarriages happen?
Most miscarriages happen during the first trimester, which is the first 12 weeks of pregnancy. If you’re not tracking your menstrual cycle or fertility, it’s possible to mistake an early miscarriage for a period. And although miscarriages can still happen after the first trimester, the chances drop significantly – to around 3-4%. It’s also possible to have a pregnancy loss after 20 weeks, but this is referred to as a stillbirth. It’s treated differently and is much less common than a miscarriage.
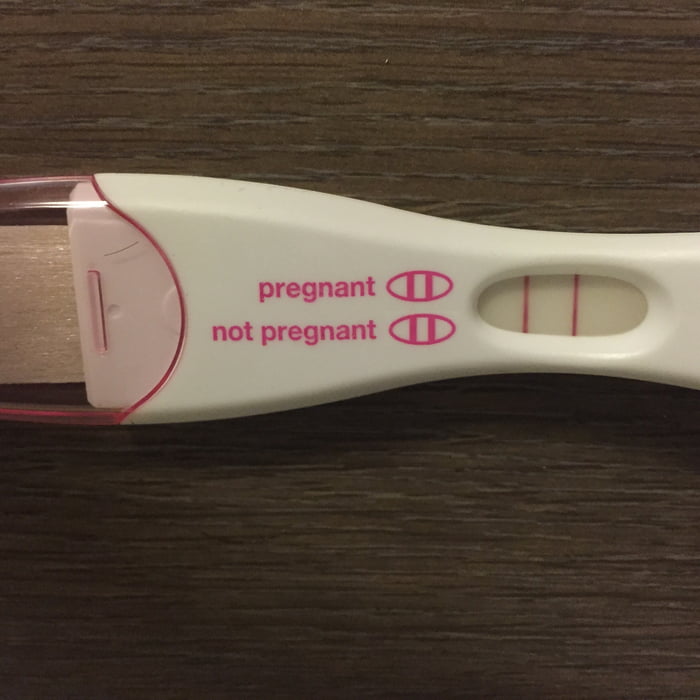
Will a pregnancy test be negative after a miscarriage?
It takes time for your hormones to return to their pre-pregnancy levels after a miscarriage. The amount of the pregnancy hormone human chorionic gonadotropin (hCG) may still be high enough to trigger a positive result on a pregnancy test for several weeks after a miscarriage.
The amount of the pregnancy hormone human chorionic gonadotropin (hCG) may still be high enough to trigger a positive result on a pregnancy test for several weeks after a miscarriage.
What causes miscarriages?
One of the most important things to know about miscarriages is that they’re often caused by things that you have no control over, including:
- Chromosomal abnormalities: This is when a fertilized egg has too many or too few chromosomes. Chromosomal abnormalities account for around half of all miscarriages and are usually random. They can either prevent the embryo from developing or from forming in the first place.
- Uterine or cervical issues: In some cases, conditions related to the uterus or cervix can interfere with embryo development and lead to miscarriage. This includes conditions that create growths or scar tissue in the uterus like endometriosis, pelvic inflammatory disease, and cervical insufficiency – which is when the cervix opens too early, typically in the second trimester.

- Infections: Untreated sexually transmitted infections (STIs) can cause you to miscarry. It’s important to get tested for STIs before you get pregnant, as you can have an infection without symptoms. You may also miscarry if you become infected with listeriosis, which is a type of food poisoning. This is why it’s recommended that you avoid eating certain foods during pregnancy.
In addition to the above, there are other factors that can increase your risk of miscarriage and other pregnancy complications. These risk factors include:
- Age: Pregnancy after age 35 comes with a higher risk of miscarriage. This is because as you age, eggs with extra or missing chromosomes become more common.
- Environmental exposure: Working around or otherwise being exposed to radiation, toxins or contaminants.
- Health conditions: Certain health conditions, like autoimmune disorders, thyroid disorders, severe diabetes and being over- or underweight.

- Lifestyle choices: Smoking, drinking alcohol and using drugs.
- Previous miscarriages: Having two or more miscarriages in a row can be a sign that you have a higher chance of miscarrying in general.
What does NOT cause a miscarriage
Physical activity and sex have not been linked to miscarriage. But if you’re ever unsure about whether something is safe to do during your pregnancy, talk to your care provider.
Some studies have shown that stress or high caffeine intake during pregnancy may increase miscarriage risk. More research is needed, but it’s recommended that you try to manage your stress as best you can, and keep your daily caffeine intake below 200 milligrams.
What to do if you have a miscarriage
Again, if you notice potential symptoms of a miscarriage, call your care provider. They will want to confirm the miscarriage and make sure that you aren’t at risk for heavy blood loss or infection. This is usually done with a pelvic exam and an ultrasound.
Miscarriages frequently resolve on their own without any need for treatment. It may take a few days to pass all of the tissue, and you may have moderate bleeding that lightens over the course of a couple weeks. Seek immediate medical treatment if you have heavy bleeding that does not lighten, fever, weakness or other signs of infection.
Medical treatment for a miscarriage
There’s no treatment that can stop a miscarriage. Instead, miscarriage treatment focuses on preventing excessive blood loss and infection, which can happen if the uterus isn’t completely cleared of tissue. Once a miscarriage has been confirmed, options for treatment may include:
- Medication: Medication can be used to speed up the passing of pregnancy tissue.
- Surgery: If there’s leftover tissue in the uterus or signs of heavy blood loss or infection, a minor surgery called dilation and curettage (D&C) may be performed. In a D&C, the cervix is dilated so that the remaining tissue can be gently removed.
 This option can also be chosen based on preference.
This option can also be chosen based on preference.
Tips for recovering from a miscarriage
- To prevent infection, avoid putting anything in your vagina during a miscarriage, and for two weeks afterwards. This means avoiding sexual intercourse and using pads instead of tampons.
- If you’re having painful cramps during or after a miscarriage, take acetaminophen – follow the label instructions.
- Your iron levels may drop as a result of the bleeding. To offset this and support your body’s blood production, eat a healthy diet that’s high in iron and vitamin C. Iron can be found in red meat, shellfish, beans and leafy green vegetables. Vitamin C can be found in citrus fruit, kiwis, bell peppers and many other vegetables.
- A miscarriage can be an emotionally difficult time, and there’s no right or wrong way to feel. It’s common to experience a variety of emotions, including mood swings, grief, anger and loneliness. Talk with family, friends or a counselor if you’re feeling overwhelmed or need support after a pregnancy loss.
- Be kind to yourself. The physical and emotional toll of a miscarriage can be draining. It’s okay to take a step back from your regular activities if you need to rest and recuperate.
- Once your miscarriage has been confirmed, go to any recommended follow-up appointments, and report new or worsening symptoms to your care provider as soon as possible.
Can you avoid a miscarriage?
After a miscarriage, it’s normal to wonder if you could have done anything differently. Remember, a miscarriage is rarely anyone’s fault, and there’s no sure way to prevent one from happening. That said, there are a few healthy lifestyle choices you can make to minimize your risk:
- If you smoke, drink alcohol or use drugs, quit as soon as possible.
- Get tested for STIs.
- Talk to a medical professional about any health conditions you haven’t had treatment for.
- Stick to any treatment plans or other methods you’ve already been given for managing health conditions.
- Get enough physical activity.
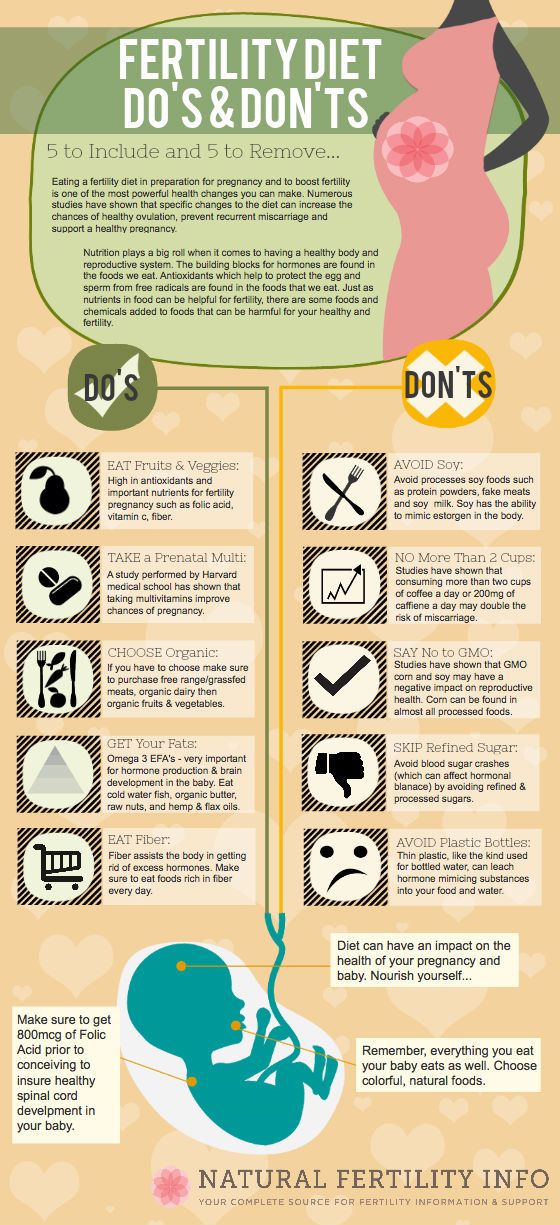
- Eat a balanced diet.
Keep your risk low
If you aren’t pregnant yet, one of the best things you can do to minimize your risk of miscarriage and other complications is to make a preconception appointment. This is an opportunity for your care provider to review your medical and lifestyle histories, and make recommendations that can give your pregnancy the healthiest possible start.
And if you’re already pregnant, stick to your prenatal appointment schedule. Your prenatal appointments ensure that you and your little one are getting all the care you need. Plus, these appointments give your care team the chance to catch signs and symptoms of complications before they affect your pregnancy.
Make a preconception appointment or a prenatal appointment.
Can a woman have a miscarriage without knowing it? - Healthcare Wellness Blogs
Miscarriages are relatively common and it is possible to have a miscarriage without bleeding or cramping.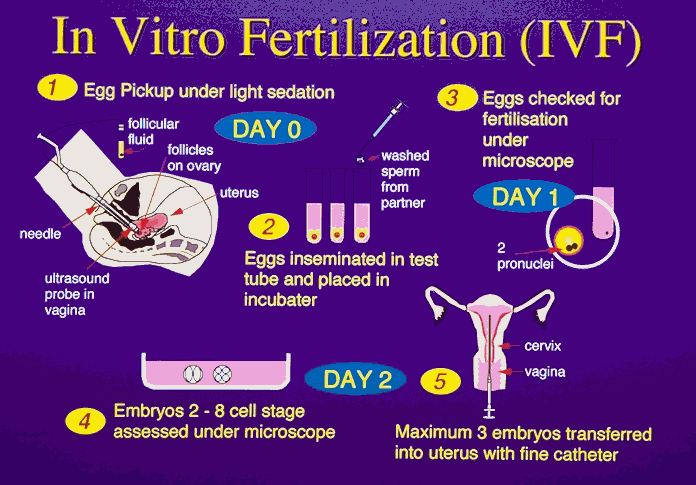 The missed miscarriage is also known as “silent miscarriage”. It is called as “missed” because the body has not yet recognized that the woman is no longer pregnant. Around 50% of all pregnancies end up in some sort of miscarriage. This happens mostly in early pregnancy and most women feel that it is just a heavy menses. You may think that your period is a day or two late. The chance of miscarriage becomes 15% once the pregnancy goes beyond a month or so and you still might not have known. You may get to know it only when you go for an ultrasound and find there is no fetal heartbeat. This happens because of an event that happens inside the womb and the embryo stops developing due to it. It often causes cramping and bleeding, but sometimes it can also go unnoticed for several weeks. To avoid or to be on the safer side it is advised to visit the doctor for regular checkups & consult with the best gynecologist in Bangalore at Ovum Hospitals.
The missed miscarriage is also known as “silent miscarriage”. It is called as “missed” because the body has not yet recognized that the woman is no longer pregnant. Around 50% of all pregnancies end up in some sort of miscarriage. This happens mostly in early pregnancy and most women feel that it is just a heavy menses. You may think that your period is a day or two late. The chance of miscarriage becomes 15% once the pregnancy goes beyond a month or so and you still might not have known. You may get to know it only when you go for an ultrasound and find there is no fetal heartbeat. This happens because of an event that happens inside the womb and the embryo stops developing due to it. It often causes cramping and bleeding, but sometimes it can also go unnoticed for several weeks. To avoid or to be on the safer side it is advised to visit the doctor for regular checkups & consult with the best gynecologist in Bangalore at Ovum Hospitals.
Signs of miscarriage-
Most miscarriages happen in the 1st trimester and the symptoms are different for everyone. Not every miscarriage is associated with pain. But most common ones are
Not every miscarriage is associated with pain. But most common ones are
- Vaginal bleeding and cramps – you may feel like bad menstrual cramps
- Large blood clots up to the size of lemon will pass.
- Abdominal pain
- Fever
- Weakness
- Back pain
Common causes of miscarriage –
Most of the women think that miscarriage happened because of themselves or their lifestyle. But, in fact, you have done nothing to cause it. You cannot prevent it from happening. Miscarriage cannot just happen because of mild exercises, or by drinking tea or coffee. The most common cause is a genetic abnormality in the embryo. Other problems that miscarriage include:
- Chromosome problems- in the process of fertilization, the egg and sperm each bring 23 chromosomes together to make 23 perfect pairs of chromosomes. This is a very complex process and any minor disturbance can result in genetic abnormality that stops the embryo from developing.

- Hormone imbalance – many miscarriages happen due to hormone imbalance such as insufficient progesterone levels that prevent your fertilized egg from implanting in the uterus.
- Thyroid disorders – thyroid problems may lead to infertility or cause recurrent miscarriages
- Diabetes
- High fever- if you fall sick and develop a high fever in your first trimester, you may experience a miscarriage.
- Chronic illness – autoimmune diseases like lupus, heart problems, kidney, and liver may cause miscarriage.
How to prevent miscarriage?
Miscarriage cannot be prevented in most cases. But you can take some measures to reduce the risk. These include- avoid smoking and drinking alcohol, maintain a healthy weight, maintain proper hygiene, eat a healthy diet, don’t do strenuous exercises, take enough rest, take precautions against infections, consult your doctor if you already have any chronic diseases.
Miscarriage, how to avoid - Planning and management of pregnancy in the gynecology of the Literary Fund polyclinic after a miscarriage
- Gallery
- News
- Blog
- Reviews
- Jobs
- Licenses
- Insurance partners
- Controlling organizations
- Schedule of reception of citizens on personal appeals
- What you need to know about coronavirus infection? nine0004
- Rules for patients
- Online doctor's consultation
- to corporative clients
- The documents
A miscarriage is always associated with severe consequences for the whole body of a woman and for her reproductive organs in particular, it also affects the family situation, disrupts the woman's work schedule. An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child. nine0033
An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child. nine0033
Any competent gynecologist will tell you that the problem of miscarriage can be solved. With proper preparation for pregnancy and its management, the next time you will have a successful pregnancy. Most girls after a miscarriage go to extremes: they try to get pregnant again as soon as possible. And if this succeeds, then the miscarriage is very often repeated. And you need to give the body a rest for 2-3 months, then identify and eliminate the cause. And only then try.
Causes of miscarriage
Many are convinced that miscarriages are due to a fall, bruise, or some other physical shock. Any woman who has had a miscarriage can remember that not long before she either fell or lifted something heavy. And I am sure that she lost her unborn child precisely because of this. However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same. nine0033
However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same. nine0033
The woman's body is almost always to blame for the other half of miscarriages. They are caused by various known and unknown factors, such as: acute infectious diseases suffered in the first trimester of pregnancy, poor environment or difficult working conditions, excessive psychological or physical stress, abnormal development of the uterus, radiation, alcohol, smoking and certain types of drugs.
The causes of early and late miscarriage may differ, although they may overlap. The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss. nine0033
The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss. nine0033
Miscarriage
Miscarriage statistics also include “missed pregnancy”. Sometimes it happens that the embryo dies and lingers in the uterine cavity. Most often, this fact is detected by ultrasound. The dead fetus may begin to decompose, and this, thereby, will lead to poisoning of the mother's body.
Doctors resort to surgical curettage, which is associated with a risk of inflammation and complications. With such a miscarriage, the next pregnancy is planned after the body is fully restored - not earlier than a year. During this year, you will have to find out the cause of the missed pregnancy and treat it. nine0033
Miscarriage up to 6 weeks
The main causes of miscarriage on this line are malformations of the embryo itself. Statistics say that from 70-90% of embryos had chromosomal abnormalities: they are random and will not occur in other pregnancies. You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
The human body is perfect and finds a way to correct the situation by miscarriage. Today is a tragedy for you. The real tragedy would be the preservation and birth of a sick, non-viable child. So don’t cry and understand: everything is for the best, you won’t help grief with tears ... And after three months, try again - it will almost certainly turn out to be successful. nine0033
It should also be noted that the fact of a miscarriage does not mean that you have lost something. So for a period of 7-8 weeks, the absence of an embryo in the fetal egg is found - "anembryony". It is believed that in 80-90% of cases, miscarriages are undiagnosed non-developing pregnancies.
Miscarriage between 6 and 12 weeks
Miscarriage in this period is also considered early. Its most common causes are:
Endocrine disorders
Endocrine disorders, when the ovaries do not synthesize enough hormones to keep the fetus in the womb, or the amount of male sex hormones is increased, is one of the most common causes of miscarriage and miscarriage.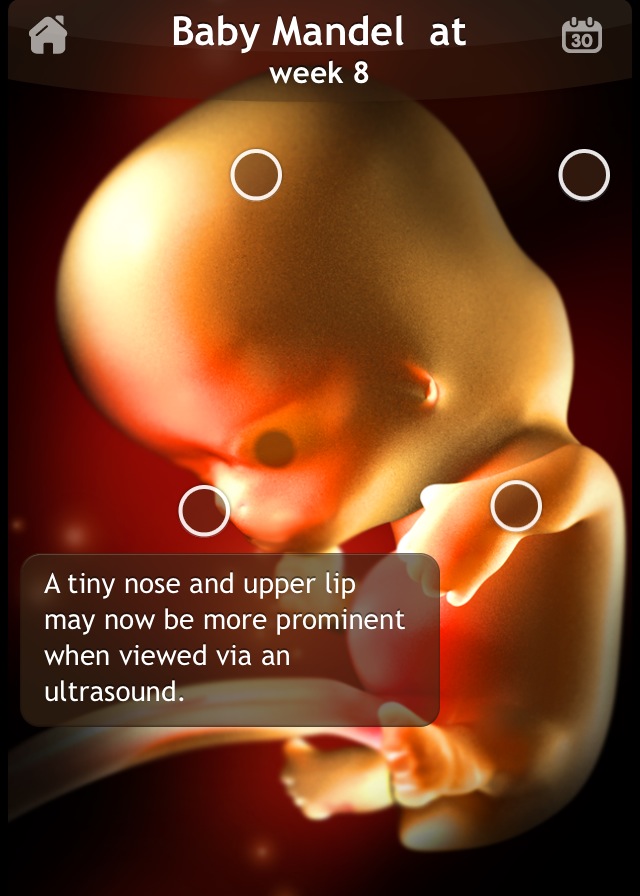 nine0033
nine0033
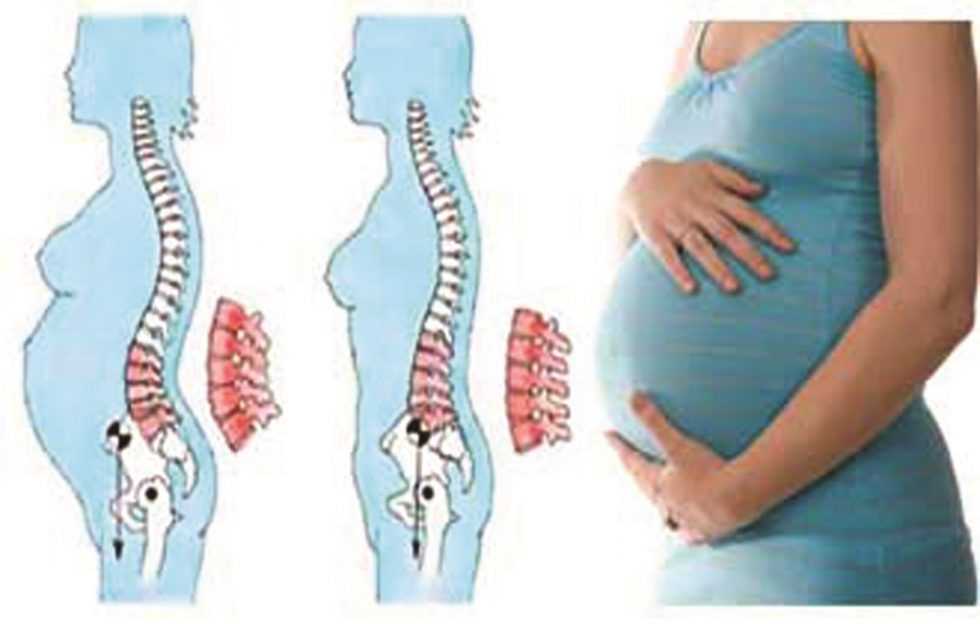
Imbalance of hormones in a woman's body is very likely to lead to an early termination of pregnancy. With a lack of the main hormone progesterone produced by the ovaries, this happens most often. Another hormonal problem is an increase in the tone of the uterus, which provokes the expulsion of the fetus.
Progesterone prepares the uterine mucosa for implantation and is the hormone for maintaining pregnancy in the first months. If conception occurs, the fetus cannot properly establish itself in the uterus. As a result, the fertilized egg is rejected. But pregnancy can be saved with the help of progesterone preparations if this problem is detected in time. nine0033
An excess of male sex hormones that suppress the production of estrogen and progesterone can also be the cause of an early miscarriage. Often, the cause of recurrent miscarriages are androgens that affect the formation and development of pregnancy; as well as thyroid and adrenal hormones. Therefore, a change in the function of these glands can lead to miscarriage.
Undertreated sexual infections
This problem must be solved before conception. Often the cause of miscarriage is sexually transmitted infections: syphilis, trichomoniasis, toxoplasmosis, chlamydia, cytomegalovirus and herpetic infections. Their effect on the fetus and the course of pregnancy is different for each woman and depends on the timing of infection, the activity of the microorganism, the degree of immune protection and the presence of other adverse factors. Depending on the situation, they can lead to the formation of fetal malformations, intrauterine infection, feto-placental insufficiency, early miscarriage or premature birth. Infection of the fetus and damage to the membrane of the fetus leads to miscarriage. To avoid this, infections should be treated before pregnancy. The use of therapy is possible during pregnancy as prescribed by a doctor. nine0033
Viral infections and other diseases
Any disease accompanied by intoxication and fever above 38 about C can lead to a miscarriage. Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections. nine0033
Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections. nine0033
Extremely dangerous during pregnancy rubella - it leads to severe fetal malformations, so infection during pregnancy is an indication for medical abortion.
Any disease during pregnancy can lead to non-viability of the fetus. And the body, through a miscarriage, insures you against unwanted offspring. With such a miscarriage, the next pregnancy has every chance of going well.
Immune causes of miscarriage
Sometimes antibodies that are hostile to the fetus are formed in the blood of a pregnant woman. This cause can be predicted and eliminated in advance. Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect. nine0033
Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect. nine0033
Reduced immunity
Reduced immunity during pregnancy also refers to immune causes. The body is simply not able to grow a new life in itself. You need to take care of yourself and recover before the next conception.
Anatomical causes of miscarriage
Anatomical causes of miscarriage are the most intractable. Malformations of the uterus are a serious reason for miscarriage. Sometimes you just have to deal with it.
Miscarriage between 12 and 22 weeks
Such a miscarriage is considered late. Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
At this time, miscarriage also occurs due to isthmic-cervical insufficiency - a weak cervix cannot hold the fetus and opens. For this reason, a miscarriage can occur in the 2nd or 3rd trimester. Isthmic-cervical insufficiency is observed in 15.0-42.7% of women suffering from miscarriage. Careful monitoring of the pregnant woman allows you to identify the problem in time and make surgical correction of the cervix before the onset of childbirth. nine0033
In isthmic-cervical insufficiency, there is only one method of treatment - mechanical narrowing of the cervical canal. To do this, the neck is either sewn up or a special ring is put on it. However, the latter method is less efficient, because the ring can easily slide off the neck, then it will no longer hold back the process of opening it.
After suturing, if necessary, it is possible to use antibiotics and drugs that normalize the microflora of the vagina. The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor. nine0033
The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor. nine0033
Isthmic-cervical insufficiency may be primary (for no apparent reason), may be the result of abortion or hormonal disorders (increased levels of androgens - male sex hormones or their precursors).
Miscarriage after 22 weeks
Such a loss is hard to forget. Obstetricians talk about premature birth after the 28th week of pregnancy. Traditionally, a child born after this period is considered viable. But medicine knows many cases when it was possible to save the life of earlier children. nine0033
We recommend that you be carefully examined for miscarriage, check the above factors. In addition to them, the cause of a miscarriage can be antiphospholipid syndrome, while the woman's body perceives the child as something alien and rejects it. This disease, like the others listed, can be corrected; you have a very real chance of bearing a child.
Miscarriages due to hemostasis disorders
All of the above causes account for only 30-40%. Up to 70% of miscarriages are caused by disorders in the blood coagulation system (hemostasis). nine0033
Blood coagulation disorders leading to pregnancy loss can be divided into thrombophilic (increased clotting) and hemorrhagic (bleeding tendencies). Both of these extremes are dangerous to the fetus. Various disorders leading to the formation of small blood clots lead to the fact that the fetus loses sufficient blood supply, development is disturbed and the fetus is rejected.
The main hemorrhagic changes can appear even in childhood in the form of increased bleeding during cuts, tooth extractions, the onset of menstruation. But sometimes they declare themselves only during pregnancy and are the cause of a miscarriage. Bleeding in the early stages and detachment of the chorion is difficult to stop. nine0033
You may not guess, but incomprehensible headaches, weakness, fatigue, temporary loss of smell or hearing may be symptoms of disorders in the blood coagulation system.
When planning a pregnancy, a genetic examination should be carried out and, if necessary, treatment should be started.
It is advisable to be examined for hidden hemostasis defects even for those who consider themselves healthy. This will allow you to predict the occurrence of complications and prevent loss. Early therapy can prevent miscarriage at 98% of cases. If defects in hemostasis are already detected during pregnancy, it can be difficult to maintain it.
What to do after a miscarriage?
Find the cause! The ideal option is to be examined by future parents: it is much more reasonable to postpone conception and spend two or three months to identify the causes than to risk getting pregnant again, spend two months waiting, and then lose everything again and still go to the doctors.
Until you understand the reason, it will not evaporate. In most cases, the answers lie on the surface. Take care of your health and your future baby. nine0033
Sign up for a consultation with an obstetrician-gynecologist by phone +7 (495) 150-60-01
Tyan Oksana Alexandrovna
Head of the department, obstetrician-gynecologist Doctor of the highest category Work experience: 26 years
Volkova Polina Dmitrievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the highest category Experience: 35 years
Postnikova Nadezhda Anatolyevna
Obstetrician-gynecologist, ultrasound specialist Work experience: 35 years
Moiseeva Alla Vitalievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the first category Work experience: 37 years
Zabolotnova Olga Valentinovna
Obstetrician-gynecologist Doctor of the first category Experience: 26 years
Shchelokova Elena Nikolaevna
Obstetrician-gynecologist Doctor of the highest category Experience: 38 years
Maksimova Tamara Anatolyevna
Obstetrician-gynecologist Work experience: 7 years
Pass or medical card number:
Contact phone: *
Select the day of your appointment:
Additional information: nine0033
I am not a robot
By clicking the "Submit Application" button, you agree to the terms Privacy Policy and User Agreement
Why is it so important for us to talk about the loss of a child
Why is it so important for us to talk about the loss of a child?- Health »
- A
- B
- C
- D
- E 9Ol000
- c
- h 9000 Popular Topics
- Air pollution
- Coronavirus disease (COVID-19))
- Hepatitis
- Data and statistics »
- Newsletter
- The facts are clear
- Publications
- Find the country »
- A
- B
- B
- g
- D
- E
- and 9000 H
- O
- P
- R
- C
- T
- U x
- C hours
- Sh
- E
- I
- I
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean nine0004
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Highlights "
- About WHO »
- General director
- About WHO
- WHO activities
- Where does WHO work?
nine0031 - Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Spotlight /
- Why is it so important for us to talk about the loss of a child
Why is it important for us to talk about the loss of a child
WHO/M. Purdie
Purdie
© A photo
The loss of a child during pregnancy due to miscarriage or stillbirth is still a taboo topic around the world, which is associated with condemnation or a sense of shame. Many women who lose a child during pregnancy or childbirth continue to receive neither the proper care nor the respect they deserve. nine0084 In this material we want to share stories told by women from different countries.
Miscarriage is the most common cause of pregnancy loss. Estimates of the prevalence of this phenomenon vary somewhat, although according to the March of Dimes Foundation, an organization dedicated to maternal and child health, the prevalence of miscarriage in women who knew they were pregnant is 10-15%. Different countries around the world use different definitions of pregnancy loss, but as a rule, the death of a child before 28 weeks of gestation is considered a miscarriage, and death at or after 28 completed gestational weeks is considered a stillbirth. There are 2.6 million stillborn babies born each year, and many of these deaths could have been prevented. However, even in developed countries, miscarriages and stillbirths are not systematically recorded, so the actual figures may be even higher. nine0033
There are 2.6 million stillborn babies born each year, and many of these deaths could have been prevented. However, even in developed countries, miscarriages and stillbirths are not systematically recorded, so the actual figures may be even higher. nine0033
Worldwide, women's access to health services varies by country of residence, with hospitals and outpatient facilities very often under-resourced and understaffed in many countries. As varied as the experience of bereaved women, stigma, guilt and shame are common themes around the world. Women who have lost their children have shared personal experiences that they felt they had to keep their grief quiet, either because miscarriages or stillbirths remain common or because people perceive them as inevitable. nine0033
Jessica Zucker, Clinical Psychologist and Writer, USA
“I am a clinical psychologist specializing in mental health issues related to reproduction and motherhood. I have been doing this for over ten years. But when I myself had a miscarriage at 16 weeks, only then could I truly feel that heartache, that re-experienced feeling of grief and loss that my patients have been telling me about for so many years.
Jessica's story
All this has a very hard effect on women. Many women who lose a child during pregnancy may develop mental health problems that last for months or years, even if they later have healthy children.
Cultural and social views on the loss of a child in different parts of the world can be very different from each other. Thus, in sub-Saharan Africa, the prevailing opinion is that a baby can be born dead because of witchcraft or the machinations of evil spirits. nine0191
Larai, 44, pharmacist, Nigeria
“I took everything that happened after my miscarriage very hard. This was greatly facilitated by the medical workers themselves, despite the fact that I am also a doctor. Another issue is cultural representations. Here, the loss of a child brings shame to the woman, because there is a perception that if a woman has lost a child several times, something is wrong with her, and that she may have had extramarital affairs, and the loss of a child in that case, God's punishment. nine0033
nine0033
Larai's story
There are many possible causes for miscarriages or stillbirths, from fetal abnormalities to maternal age to infections, many of which (such as malaria and syphilis) are preventable, although identifying the exact cause is often difficult.
General recommendations for preventing miscarriage include a healthy diet, physical activity, avoidance of smoking, drug and alcohol use, limiting caffeine intake, managing stress, and maintaining a normal body weight. This approach focuses on lifestyle factors, and in the absence of specific explanations for what happened, this can lead to women feeling guilty that it was their behavior that caused the miscarriage. nine0033
Lisa, 40, Marketing Manager, UK
“I've had four miscarriages. Every time this happens, a part of you dies. The first time was the hardest. It was my very first pregnancy. We were so happy that we will soon have a baby. But when we went to our local hospital in the southeast of England at week 12 for a routine ultrasound, I was told that I had a miscarriage, or miscarriage, which meant that my baby had died long ago, although I did not feel no signs. " nine0033
" nine0033
Lisa's story
As with some other medical topics, such as mental health, which remain a huge taboo, many women report that, regardless of their cultural background, education and upbringing, their friends and families don't want to talk about their loss. Apparently, this is due to the general tradition to surround any grief with a veil of silence.
Susan, 34, writer, USA
“I've been dealing with infertility for almost five years now. After I decided to try IVF, I actually managed to get pregnant, but after a few weeks the baby stopped growing. It took doctors two and a half weeks to confirm this. It took another two weeks before I had a miscarriage that lasted 19days. I could not imagine that it could be so painful, for so long and with such heavy bleeding.
Susan's story
Stillbirths occur later in pregnancy, namely after 28 gestational weeks, as defined by WHO. About 98% of stillbirths occur in low- and middle-income countries. Lack of proper care and supervision during labor results in one in two stillbirths occurring during delivery, many of which could have been prevented with quality care and proper supervision of the woman in labour. nine0033
Lack of proper care and supervision during labor results in one in two stillbirths occurring during delivery, many of which could have been prevented with quality care and proper supervision of the woman in labour. nine0033
Better care during pregnancy and childbirth could prevent more than half a million stillbirths globally. Even in high-income countries, non-compliance with standards of care is an important cause of stillbirths.
There are clear ways to reduce the number of children who die during pregnancy, namely: improving access to antenatal care (in some parts of the world, women do not see a health worker until they are several months pregnant), introducing continuous care models, provided by midwives, as well as community care where possible. Integrating infection management during pregnancy, fetal heart rate monitoring and birth monitoring into a comprehensive care package could save 1.3 million lives of otherwise stillborn babies. nine0033
Emilia, 36, shopkeeper, Colombia
“When my baby was stillborn at 32 weeks, we already gave him a name. The doctor referred me for an ultrasound examination, during which he told me that the child was not showing signs of life. I knew right away that my baby was dead. I know this could have been avoided. If from the very beginning I had been told everything about my condition in more detail, if the doctors had treated me more attentively during the critical periods of my pregnancy, my child could have been saved. nine0033
The doctor referred me for an ultrasound examination, during which he told me that the child was not showing signs of life. I knew right away that my baby was dead. I know this could have been avoided. If from the very beginning I had been told everything about my condition in more detail, if the doctors had treated me more attentively during the critical periods of my pregnancy, my child could have been saved. nine0033
Emilia's story
The attitude towards women during pregnancy is related to the extent to which their sexual and reproductive rights are generally realized; many women around the world do not have the ability to make autonomous decisions in this area.
In many parts of the world, the pressure of public opinion is forcing women to become pregnant when they are not yet physically or psychologically ready for it. Even in 2019, 200 million women who want to avoid pregnancy do not have access to modern methods of contraception. And when pregnancy does occur, 30 million women are forced to give birth outside of health facilities, and 45 million women do not receive adequate antenatal care or no antenatal care at all, greatly increasing the risk of complications and death for both the mother and the mother. child. nine0033
child. nine0033
Cultural practices, such as ritual female genital mutilation and child marriage, cause great harm to girls' sexual and reproductive health and the health of their children. Having children at a young age can be dangerous for both mother and child. Adolescent girls (aged 10–19 years) are significantly more likely to have eclampsia or intrauterine infections than women aged 20–24 years, increasing the risk of stillbirth in this age group. In addition, babies born to women younger than 20 are more likely to have low birth weight, prematurity, or severe health problems in the first month of life, which also increases the risk of stillbirth. nine0033
Female genital mutilation increases a woman's risk of protracted or difficult labour, bleeding, severe tears and increases the frequency of instrumental use in childbirth. At the same time, children of such mothers are much more likely to need resuscitation during childbirth and increase the risk of death during childbirth or after birth.
Putting women at the center of care is critical to creating a positive pregnancy experience—the biomedical and physiological aspects of health services need to be complemented by social, cultural, emotional and psychological support. nine0033
However, many women, even those living in developed countries with access to the best health care systems, do not receive adequate care after the loss of a child. Even the language used by medical professionals in relation to miscarriage and stillbirth can be traumatic in itself: the use of terms such as "cervical failure" or "dead gestational sac" can be painful.
Andrea, 28, stylist and singer, Colombia
“When I was 12 weeks pregnant, I went to a scheduled appointment with the doctor, where I had an ultrasound. The doctor told me that I was not doing well, but did not specify what exactly was wrong. The next day, when I woke up, I noticed blood stains on the sheets. I didn't get any information about why I had a miscarriage. My doctor was very kind to me, but he didn't explain anything to me. But the nurses were completely indifferent and unfriendly and behaved as if I had undergone an ordinary medical procedure, and nothing more. No one gave me any support." nine0033
My doctor was very kind to me, but he didn't explain anything to me. But the nurses were completely indifferent and unfriendly and behaved as if I had undergone an ordinary medical procedure, and nothing more. No one gave me any support." nine0033
Depending on the rules of the particular medical facility, stillborn bodies may be treated as clinical waste and incinerated. It happens that when a woman learns that her child has died, she is forced to continue to carry the dead baby for several weeks before she can give birth. Even if this delay may be clinically justified, this situation is excruciating for both the woman and her partner. Even in developed countries, women may be forced to give birth to their dead babies in maternity wards, surrounded by women who have healthy children, which is very difficult from a psychological point of view and reminds the woman of her loss. nine0033
Not all inpatient or outpatient facilities can adopt a new care strategy or provide more services.