Can you get pregnant at the age of 12
What's the youngest age that a person can get pregnant and give birth?
Lina Medina, the youngest known person to give birth, is pictured here next to one of her doctors and her son. (Image credit: TravelingMan via Flickr; background added (https://creativecommons.org/licenses/by-nc-nd/2.0/))Shortly after the U.S. Supreme Court ruled to overturn Roe v. Wade and eliminate the constitutional right to abortion, news outlets reported the story of a pregnant 10-year-old girl who had to travel from Ohio to Indiana to access abortion care. The story highlighted how young victims of rape will be affected by the court's ruling and jumpstarted a discussion about the risks that pregnancy and childbirth pose to young children.
A pregnant 10-year-old would face significant and potentially life-threatening medical risks in carrying a pregnancy to term — and harrowingly, children even younger than age 10 can become pregnant.
Simply put, pregnancy is possible from the start of ovulation, meaning the point at which the ovaries begin releasing mature eggs, called ova, Dr. Melissa Simon, a professor and obstetrician-gynecologist at the Northwestern University Feinberg School of Medicine in Chicago, told Live Science. It's important to note that "you can start ovulating before you start having your first period," and the release of an egg isn't necessarily accompanied by any obvious physical symptoms, Simon added.
More commonly, ovulation begins after menarche, or a person's first period, according to the medical database StatPearls . According to the latest available data, collected in 2017, menarche typically occurs between age 10 and 16. However, research hints that the age of menarche is trending downward, meaning the number of children who have their first period before age 10 is likely increasing, Simon said.
Related: Why are pregnant women told to sleep on their left side?
ABORTION GUIDANCE AND SUPPORT
—Abortion laws by state: https://reproductiverights.org/maps/abortion-laws-by-state/
—For questions about legal rights and self-managed abortion: www. reprolegalhelpline.org
reprolegalhelpline.org
—To find an abortion clinic in the US: www.ineedanA.com
—Miscarriage & Abortion Hotline operated by doctors who can offer expert medical advice: Available online or at 833-246-2632
—To find practical support accessing abortion: www.apiarycollective.org
"There's a lot of potential dangers of carrying a pregnancy when you're age 9 or 10," Simon said. For example, during pregnancy, the volume of blood in a person's body increases by about 50%, and all that extra fluid can put tremendous strain on a child's heart, Simon said. The child's growing body may also be deprived of critical nutrients, like calcium, as those nutrients get diverted to the developing fetus.
Compared with mothers in their early 20s, mothers aged 10 to 19 face a higher risk of developing dangerously high blood pressure in pregnancy (preeclampsia) that can lead to complications like seizures and coma (eclampsia), according to the World Health Organization (WHO). They also face a heightened risk of systemic infections and infections of the uterine lining (puerperal endometritis), according to the WHO, as well as maternal anemia, where the number of healthy, oxygen-carrying red blood cells in the body significantly declines, according to The New York Times .
They also face a heightened risk of systemic infections and infections of the uterine lining (puerperal endometritis), according to the WHO, as well as maternal anemia, where the number of healthy, oxygen-carrying red blood cells in the body significantly declines, according to The New York Times .
"The complications, the morbidity and the mortality are much higher in girls under 15 than girls 16 to 19, although 16 to 19 has a mortality twice as high as women 20 and above," Dr. Ashok Dyalchand, head of the Institute of Health Management Pachod, a public health organization serving marginalized communities in central India, told The New York Times.
Due to their narrow pelvises, children also face a high risk of obstructed labor, a dangerous complication in which the baby gets stuck in the birth canal during delivery, Simon said. Obstructed labor places pressure on the bladder and urethra and raises the risk of pelvic inflammatory disease, an infection of the reproductive organs, according to The New York Times. In addition, obstructed labor can cause the birth canal to rupture, causing holes to appear between the vagina and bladder or rectum through which urine and feces can leak. These holes, or fistulas, require intensive surgeries to repair, Simon said.
In addition, obstructed labor can cause the birth canal to rupture, causing holes to appear between the vagina and bladder or rectum through which urine and feces can leak. These holes, or fistulas, require intensive surgeries to repair, Simon said.
Due to such risks, pregnant children would typically be recommended to undergo Cesarean sections (C-sections), rather than vaginal deliveries, Simon said. The major surgery comes with its own risks, such as heavy bleeding, infection and bladder and bowel injuries, and depending on the type of incision made, the procedure can increase the likelihood of requiring a C-section in future pregnancies, according to University of Utah Health . Having multiple C-sections raises the risk of "placenta accreta," a life-threatening condition where the placenta implants near the C-section scar.
On top of these medical risks, children who become pregnant also endure significant mental trauma, Simon said. "The mental toll of carrying a baby — I can't even fathom what kind of mental toll that would have on a child," she said.
Related: Why can't babies drink cow's milk?
Lina Medina became the youngest person to give birth in recorded history when she underwent a Cesarean section at the age of 5 years, 7 months and 21 days old, according to the fact-checking website Snopes , which confirmed the validity of this widely cited case in 2004.
Medina lived in Ticrapo, Peru, and in April 1939, her parents brought her to the Hospital of Pisco and expressed concerns that a large tumor was growing in her abdomen. After evaluating Medina, doctors determined that the child was actually about seven months pregnant. The identity of the child's rapist couldn't be confirmed, in part, because the 5-year-old "couldn't give precise responses" to questions about the event, physician-researcher Edmundo Escomel wrote in the May 1939 issue of the French journal La Presse Médicale.
Medina delivered a six-pound (2.7 kilogram) baby boy on May 14, 1939 at a hospital in Lima, the report states. The baby could only be delivered via C-section due to the small size of Medina's pelvis.
The baby could only be delivered via C-section due to the small size of Medina's pelvis.
RELATED MYSTERIES
During the procedure, doctors biopsied a tissue sample from one of Medina's ovaries and found that the tissues resembled those of an adult woman. The child was originally reported to have started menstruating at age 3, but later reports stated that she'd had her first period at 8 months old. In a report published in December 1939 in La Presse Medicale, Escomel theorized that the child started puberty extraordinary early due to some disorder of the pituitary gland — a bean-shaped gland at the base of the brain that directs the body's production of sex hormones.
Editor's note: An earlier version of this article was published in 2011. This new article was published on August 2, 2022 by Live Science staff writer Nicoletta Lanese following the Supreme Court's decision to overturn Roe v. Wade on June 24, 2022. This decision eliminated the constitutional right to abortion that was established by the 1973 court case and later affirmed by a 1992 case called Planned Parenthood of Southeastern Pennsylvania v. Casey.
Casey.
Originally published on Live Science.
Nicoletta Lanese is a staff writer for Live Science covering health and medicine, along with an assortment of biology, animal, environment and climate stories. She holds degrees in neuroscience and dance from the University of Florida and a graduate certificate in science communication from the University of California, Santa Cruz. Her work has appeared in The Scientist Magazine, Science News, The San Jose Mercury News and Mongabay, among other outlets.
What’s Ideal and What Are the Risks?
Childbearing Age: What’s Ideal and What Are the Risks?Medically reviewed by Holly Ernst, PA-C — By Stephanie Watson on June 6, 2018
What’s the childbearing age?
Technically, women can get pregnant and bear children from puberty when they start getting their menstrual period to menopause when they stop getting it. The average woman’s reproductive years are between ages 12 and 51.
Your fertility naturally declines as you get older, which could make it harder for you to conceive. And starting a family later in life could pose greater risks for pregnancy complications.
And starting a family later in life could pose greater risks for pregnancy complications.
Experts say the best time to get pregnant is between your late 20s and early 30s. This age range is associated with the best outcomes for both you and your baby. One study pinpointed the ideal age to give birth to a first child as 30.5.
Your age is just one factor that should go into your decision to get pregnant. You also need to consider your emotional and financial readiness to start a family. That timing is unique for each woman.
How does age affect fertility?
Women are born with all the eggs they’ll ever have — about 2 million of them. Your number of eggs gradually falls over the years.
By age 37, you’ll have about 25,000 eggs left. By age 51, you’ll only have 1,000 eggs left. That might still sound like a lot of eggs, but the quality of your eggs also goes down as you age.
Your risk for developing conditions that can negatively impact fertility, like endometriosis and tubal disease, also increases as you get older.
Because of these factors, your fertility begins to gradually decline at around age 32. Starting between 35 and 37, fertility begins to drop more quickly.
Your chance of getting pregnant decreases as you get older. After three months of trying, your odds of conceiving in during your next cycle are:
- 18 percent at age 25
- 16 percent at age 30
- 12 percent at age 35
- 7 percent at age 40
Other factors may reduce your chances of getting pregnant, including:
- smoking
- cancer treatments such as radiation and chemotherapy
- pelvic infection
What are the benefits of getting pregnant at certain ages?
Women in the United States are waiting longer than ever to get pregnant. The average age of first-time moms is nearly 27, according to the Centers for Disease Control and Prevention. Birth rates have risen among women in their 30s and dropped among those in their 20s.
Benefits of delaying starting a family
Waiting to start a family can have some benefits. You’ll have more time to save up money, establish your relationship, and become more financially secure for your child.
You’ll have more time to save up money, establish your relationship, and become more financially secure for your child.
Age can also bring wisdom and patience. And there’s some evidence that children born to older parents achieve higher levels of education.
Holding off on pregnancy might have advantages for you, as well. A 2012 study suggested that women who gave birth to their last or only child at age 40 or older had a lower risk for uterine cancer.
Benefits of having children at a younger age
Being a younger mother is more beneficial to your baby’s health. Your odds of conceiving are increased in your late 20s or early 30s. Getting pregnant during this time also reduces your chances of having a pregnancy complication.
Risks of getting pregnant at age 35 and older
Starting at age 35, these pregnancy risks become more common:
- gestational diabetes
- high blood pressure
- preeclampsia
- placenta previa
- miscarriage
- premature birth
- stillbirth
- need for a cesarean delivery
- heavy bleeding after delivery
- infant low birth weight
- chromosomal abnormalities such as Down syndrome
When should you see a doctor for fertility questions?
Fertility issues are very common. More than 12 percent of women have difficulties getting pregnant. If you haven’t been able to get pregnant, a fertility specialist can do tests to see why you’re not conceiving and offer treatments to improve your odds of a pregnancy.
More than 12 percent of women have difficulties getting pregnant. If you haven’t been able to get pregnant, a fertility specialist can do tests to see why you’re not conceiving and offer treatments to improve your odds of a pregnancy.
See a fertility specialist if:
- You’re age 35 or younger and you’ve been trying to get pregnant for a year.
- You’re over age 35 and you’ve been trying for more than 6 months.
- You’re over age 40 and you’d like to start a family.
The fertility treatment your doctor recommends depends on factors like the cause of your fertility issues, your age, and your preferences. Options include:
- fertility drugs to stimulate ovulation
- surgery to fix a uterine condition, such as endometriosis, fibroids, or blocked fallopian tubes
- intrauterine insemination, where sperm is placed directly into your uterus during ovulation
- in vitro fertilization, where sperm and egg are placed together in a lab until they form an embryo, which is then implanted into your uterus
- zygote intrafallopian transfer and gamete intrafallopian transfer, where the sperm and egg or a fertilized egg is placed into your fallopian tube
Tips for conception
If you’re ready to start trying for a baby, here are a few things you can do to help make parenthood a reality:
- Get to a healthy weight.
 An ideal body mass index is between 19 and 24. Being overweight or underweight can affect your ability to ovulate.
An ideal body mass index is between 19 and 24. Being overweight or underweight can affect your ability to ovulate. - Quit smoking. Smoking can damage your egg supply and make you more likely to miscarry if you do get pregnant.
- Watch your diet. Eating a high-fat diet can contribute to weight gain and disrupt your reproductive cycle.
- Limit caffeine and alcohol. Research has linked excess amounts of caffeine (more than two or three cups of coffee daily) with miscarriage. Frequent alcohol use can prolong the time it takes you to get pregnant and is harmful to fetal development.
You can increase your chances of having a healthy baby by following these tips:
- Treat any conditions that could make pregnancy risky, including diabetes and high blood pressure.
- See your obstetrician for a preconception visit to make sure you’re healthy enough to get pregnant. Then, keep up with all of your scheduled pregnancy visits.
 Seeing you regularly will let your doctor monitor your and your baby’s health and address any problems that arise.
Seeing you regularly will let your doctor monitor your and your baby’s health and address any problems that arise. - Take good care of your body. Don’t smoke or drink alcohol, follow a healthy eating plan, exercise often, and get enough sleep.
The takeaway
You’ll have the best odds of getting pregnant and having a healthy baby if you start trying in your 20s or 30s, but that scenario isn’t right for every woman. When deciding to start a family, you also need to consider whether you’re:
- in a solid relationship or have the support system to have a child on your own
- ready to temporarily put your career on hold
- financially secure enough to support a child
If you have any concerns about your ability to get pregnant, see your gynecologist or visit a fertility specialist.
Last medically reviewed on June 6, 2018
- Parenthood
- Pregnancy
How we vetted this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Age and fertility. (n.d.).
pregnancy.sogc.org/fertility-and-reproduction/age-and-fertility - Alcohol and fertility. (n.d.).
yourfertility.org.au/for-women/alcohol-and-fertility/ - Barclay K. (2016). Advanced maternal age and offspring outcomes: Reproductive aging and counterbalancing period trends. DOI:
10.1111/j.1728-4457.2016.00105.x - Births and natality. (2017).
cdc.gov/nchs/fastats/births.htm - Births in the United States, 2016. (2017).
cdc.gov/nchs/products/databriefs/db287.htm - Dietl A, et al. (2015). Pregnancy and obstetrical outcomes in women over 40 years of age. DOI:
10.1055/s-0035-1546109 - Female age-related fertility decline. (2014).
acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Gynecologic-Practice/Female-Age-Related-Fertility-Decline - Having a baby after age 35.
 (2017).
(2017).
acog.org/Patients/FAQs/Having-a-Baby-After-Age-35 - Infertility. (2016).
cdc.gov/nchs/fastats/infertility.htm - Lyngsø J, et al. (2017). Association between coffee or caffeine consumption and fecundity and fertility: A systematic review and dose-response meta-analysis. DOI:
10.2147/CLEP.S146496 - Mayo Clinic Staff. (2018). Infertility.
mayoclinic.org/diseases-conditions/infertility/diagnosis-treatment/drc-20354322 - Menopause 101: A primer for the perimenopausal. (n.d.).
menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/menopause-101-a-primer-for-the-perimenopausal - Mirowsky J. (2002). Parenthood and health: The pivotal and optimal age at first birth. DOI:
10.1353/sof.2002.0055 - Periods. (2016).
nhs.uk/conditions/periods - Setiawan VW, et al. (2012). Age at last birth in relation to risk of endometrial cancer: pooled analysis in the epidemiology of endometrial cancer consortium.
 DOI:
DOI:
10.1093/aje/kws129 - Sozou PD. (2012). Time to pregnancy: A computational method for using the duration of non-conception for predicting conception. DOI:
10.1371/journal.pone.0046544 - When to see a fertility specialist. (n.d.).
fertility.womenandinfants.org/services/see-fertility-specialist
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Share this article
Medically reviewed by Holly Ernst, PA-C — By Stephanie Watson on June 6, 2018
Read this next
How Long Does It Take to Get Pregnant?
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Getting pregnant can take longer than expected. Many couples also struggle with infertility. Learn how long it typically takes to conceive after sex…
READ MORE
How Much of Infertility Is Genetic?
From health conditions to hormonal imbalances, it can seem that there are so many possible causes of infertility.
 Find out whether genetics play a…
Find out whether genetics play a…READ MORE
10 Thoughtful Gifts for Women Going Through IVF
Medically reviewed by Karen Gill, M.D.
In vitro fertilization is a tough journey. Let your friend know you’re there for them. Here are our top picks of gifts that anyone going through IVF…
READ MORE
How Fertility Treatment May Affect Your Mental Health
Medically reviewed by Joslyn Jelinek, LCSW
Infertility can affect your mental health. We explore the impact of infertility on your mental health and ways to feel better.
READ MORE
What’s the Infertility Journey Like for Non-Carrying Partners?
Fertility treatments take a toll on nonpregnant partners, too. We discuss their journey and provide expert advice on finding support.

READ MORE
Teenage pregnancies
Magnitude of the problem
Approximately 21 million pregnancies occur each year among girls aged 15-19 in developing countries, and approximately 12 million of them end in childbirth 1 . At least 777,000 births in developing countries registered among adolescent girls under the age of 15 2 .
An estimated 11.6% decline in adolescent birth rates worldwide over the past 20 years 5 . At the same time, there are large differences in this indicator between regions. For example, the adolescent birth rate is 7.1 in the countries of East Asia, and in the countries of Central Africa it reaches 129.5 5 .
There are also huge differences within regions. In 2018, the total adolescent birth rate in Southeast Asia was 33 6 . At the same time, the value of this indicator fluctuated from 0.3 in the Democratic People's Republic of Korea Republic to 83 in Bangladesh 5 .
Huge differences exist even within countries. For example, in Ethiopia, the total fertility rate ranges from 1.8 in Addis Ababa to 7.2 in the Somali region, with the proportion of women aged 15-19 years having a first birth ranging from 3% in Addis Ababa to 23% in Afar district 7 .
Although the adolescent birth rate is estimated to be declining worldwide, the actual number of adolescent births is not declining due to a large – and in some parts of the world increasing – the number of young women aged 15-19years 8 . The largest number of births occur in East Asia (95,153) and West Africa (70,423) 9
Overview
Teenage pregnancy is a global problem affecting high, middle and low income countries. Globally, however, teenage pregnancy is more likely to occur in marginalized populations and is often due to poverty, lack of education and employment opportunities 10 .
Several factors contribute to the occurrence of teenage pregnancies and births. In many societies, girls are forced to marry early and have children 11,12,13 . In the least developed countries, at least 39% of girls go married before the age of 18, and 12% before the age of 15 14 . In many places, girls choose to become pregnant due to limited educational or employment opportunities. In such societies, motherhood importance is attached to which marriage or union and childbearing may be the best limited option available 12 .
In many societies, girls are forced to marry early and have children 11,12,13 . In the least developed countries, at least 39% of girls go married before the age of 18, and 12% before the age of 15 14 . In many places, girls choose to become pregnant due to limited educational or employment opportunities. In such societies, motherhood importance is attached to which marriage or union and childbearing may be the best limited option available 12 .
Adolescents who would like to avoid pregnancy may be unable to do so due to lack of knowledge and misconceptions about where they can get contraceptives and how to use them15. Teenagers face barriers in access to contraceptives, including restrictive laws and policies regarding the provision of contraceptives based on age or marital status, biased attitudes by health care workers and/or reluctance to recognize the sexual health needs of adolescents, and due to adolescents' own inability to access contraceptives as a result of lack of knowledge, lack of transportation and financial constraints. In addition, teenagers may not have the capacity or discretion to ensure the correct and consistent use of contraceptive methods. There are at least 10 million unwanted pregnancies among adolescent girls every year in developing countries aged 15-19years 1 .
In addition, teenagers may not have the capacity or discretion to ensure the correct and consistent use of contraceptive methods. There are at least 10 million unwanted pregnancies among adolescent girls every year in developing countries aged 15-19years 1 .
Another cause of unwanted pregnancies is sexual violence, which is widespread with over a third of girls in some countries reporting that their first sexual experience was coerced 16 .
Health implications
Early teenage pregnancy has serious health implications for teenage mothers and their children. Complications of pregnancy and childbirth are the leading cause of death among girls aged 15-19years worldwide, with low- and middle-income countries accounting for 99% of the world's maternal deaths among women aged 15-49 3 . Adolescent mothers (aged 10-19 years) are at higher risk of eclampsia, postpartum endometritis and systemic infections than women aged 20-24 years 4 . In addition, adolescent girls aged 15-19 experience approximately 3.9 million unsafe abortions each year, contributing to maternal mortality, morbidity and long-term ill health 1 .
In addition, adolescent girls aged 15-19 experience approximately 3.9 million unsafe abortions each year, contributing to maternal mortality, morbidity and long-term ill health 1 .
Childbirth at an early age increases the risk for both mothers and their newborns. Children born before age 20 are at higher risk of low birth weight, prematurity and severe neonatal illness 4 . In some countries, frequent pregnancy at a young age is of great concern, as it creates additional health risks for both mother and child 17 .
Socio-economic impact
Social consequences for unmarried pregnant adolescents may include stigmatization, social rejection or violence from partners, parents and peers. Girls who become pregnant before the age of 18 are more likely to experience marital or partner violence 16 . Pregnancy and childbirth during adolescence often causes girls to drop out of school. Although efforts are being made in a number of countries to allow them to return to work after the birth of a child, this may seriously limit their future educational and employment opportunities 19 .
WHO activities
In the early stages of achieving the Millennium Development Goals, prevention of teenage pregnancy and its associated mortality and morbidity, as well as the prevention of HIV infection and HIV-related mortality among adolescents and young people, was not given sufficient attention due to presence of competing priorities 20 . During this period, WHO collaborated with partners to raise awareness of adolescent issues, expand the body of evidence and the epidemiological basis for action, including the development of WHO guidance on the prevention of early pregnancy and adverse outcomes in adolescents in developing countries 21 , developing and testing program support tools, capacity building and pilot initiatives in a small but growing number of countries that recognize the need to address adolescent health concerns. As the world moves towards achieving the Sustainable Development Goals, adolescents are placed at the center of the global health and development agenda 21 .
While WHO continues its advocacy, evidence-gathering, tool development and capacity-building efforts, the focus is now on scaling up activities at the country level. WHO is working closely with partners within and outside the United Nations system to contribute to efforts around the world to prevent children from becoming wives and mothers. WHO's work is aimed at expanding the evidence base for action and supporting the use of evidence in well-designed and effectively implemented programs at the national and subnational levels. For example, WHO is collaborating closely with UNICEF, UNFPA and UN Women on a global program to accelerate action against child marriage 22 . WHO is also collaborating with the Family Planning 2020 global partnership, which aims to ensure that 120 million additional women and girls have access to contraception by 2020.
Nongovernmental organizations play a leading role in preventing teenage pregnancy in many countries carrying out bold and innovative projects. The number of successful national programs led by governments, for example in Chile, Ethiopia and the United Kingdom, is currently small but growing 23 . These countries show what can be achieved with sound scientific knowledge combined with strong leadership, management and perseverance. They set an example and inspire other countries to urgently achieve realistic goals and take necessary actions.
The number of successful national programs led by governments, for example in Chile, Ethiopia and the United Kingdom, is currently small but growing 23 . These countries show what can be achieved with sound scientific knowledge combined with strong leadership, management and perseverance. They set an example and inspire other countries to urgently achieve realistic goals and take necessary actions.
Bibliography
(1) Darroch J, Woog V, Bankole A, Ashford LS. Adding it up: Costs and benefits of meeting the contraceptive needs of adolescents. New York: Guttmacher Institute; 2016.
(2) UNFPA. Girlhood, not motherhood: Preventing adolescent pregnancy. New York: UNFPA; 2015.
(3) Neal S, Matthews Z, Frost M, et al. Childbearing in adolescents aged 12–15 years in low resource countries: a neglected issue. New estimates from demographic and household surveys in 42 countries. Acta Obstet Gynecol Scand 2012;91: 1114–18. Every Woman Every Child. The Global Strategy for Women`s, Children`s and Adolescents` Health (2016-2030). Geneva: Every Woman Every Child, 2015.
Every Woman Every Child. The Global Strategy for Women`s, Children`s and Adolescents` Health (2016-2030). Geneva: Every Woman Every Child, 2015.
(4) WHO. Global health estimates 2015: deaths by cause, age, sex, by country and by region, 2000–2015. Geneva: WHO; 2016.
(5) Ganchimeg T, et al. Pregnancy and childbirth outcomes among adolescent mothers: a World Health Organization multicountry study. bjog. 2014;121(S Suppl 1):40-8.
(6) UN DESA, Population Division. World Population Prospects: The 2017 Revision, DVD Edition. New York: UN DESA; 2017 UNDESA, Population Division. World Population Prospects, the 2015 Revision (DVD edition). New York: UNDESA, Population Division, 2015.
(7) UNFPA. Adolescent pregnancy: A review of the evidence. New York: UNFPA, 2013.
(8) UN DESA, Statistics Division. SDG Indicators: Global Database. New York: UN DESA: 2017.
(9) Every Woman Every Child. The Global Strategy for Women`s, Children`s and Adolescents` Health (2016-2030). Geneva: Every Woman Every Child; 2015.
The Global Strategy for Women`s, Children`s and Adolescents` Health (2016-2030). Geneva: Every Woman Every Child; 2015.
(10) UNICEF. Ending child marriage: Progress and prospects. New York: UNICEF, 2013
(11) WHO. Global and regional estimates on violence against women: Prevalence and health effects of intimate partner violence and non-partner sexual violence. Geneva: WHO; 2013.
(12) WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Trends in maternal mortality: 1990 to 2015: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: WHO; 2015. Filippi V, Chou D, Ronsmans C, et al. Levels and Causes of Maternal Mortality and Morbidity. In: Black RE, Laxminarayan R, Temmerman M, et al., editors. Reproductive, Maternal, Newborn, and Child Health: Disease Control Priorities, Third Edition (Volume 2). Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2016 Apr 5. Chapter 3.
Chapter 3.
(13) Kozuki N, Lee A, Silveira M, et al. The associations of birth intervals with small-for-gestational-age, preterm, and neonatal and infant mortality: A meta-analysis. BMC Public Health 2013;13(Suppl. 3):S3.
(14) World Bank. Economic impacts of child marriage: Global synthesis report. Washington, DC: World Bank; 2017.
(15) WHO. Preventing early pregnancy and poor reproductive outcomes among adolescents in developing countries. Geneva: WHO; 2011.
(16) Raj A, Boehmer U. Girl child marriage and its association with national rates of HIV, maternal health, and infant mortality across 97 countries. Violence Against Women 2013;19(4).
(17) WHO. Making health services adolescent friendly: Developing national quality standards for adolescent friendly health services. Geneva: WHO; 2012.
(18) WHO. Global Accelerated Action for the Health of Adolescents (AA-HA!): Guidance to support country implementation. Geneva: WHO; 2017.
Geneva: WHO; 2017.
(19) WHO. Global standards for quality health care services for adolescents. Geneva: WHO; 2015.
(20) WHO. Core competencies in adolescent health and development for primary care providers: including a tool to assess the adolescent health and development component in pre-service education of health-care providers. Geneva: WHO; 2015.
(21) UNESCO. International Technical Guidance on Sexuality Education: An evidence-informed approach for schools, teachers and health educators. Paris: UNESCO; 2009.
(22) UNESCO. Early and Unintended Pregnancy & the Education Sector: Evidence Review and Recommendations. Paris: UNESCO; 2017.
(23) United Nations General Assembly. Resolution adopted by the General Assembly on 25 September 2015: Transforming our world: the 2030 Agenda for Sustainable Development. New York: United Nations; 2015.
Early teenage pregnancy and childbirth
For inquiries please contact:
Kyiv (Poznyaki)
st. A. Akhmatova 31
A. Akhmatova 31
+38(096) 683-06-18
+38(063) 217-14-64
Sign up for a consultation
General information. In medical practice, there are episodes when young pregnant women need obstetric care (a primipara is called young if she gave birth before the age of 18). Her pregnancy proceeds, undoubtedly, in unusual conditions associated with the immaturity of adaptive mechanisms.
The heavy burden on the immature, fragile body due to pregnancy is a serious test.
Pregnancy in girls under 8 years of age becomes possible in case of accelerated puberty. At the age of 9 to 16 years, pregnancy can occur even in cases where the dynamics of puberty is not ahead of the norm.
Classification of pregnancy. A distinction is made between pregnancy that occurred before puberty (violent ovulation occurs long before puberty) and pregnancy in a woman who has already entered puberty. In these two groups, the features of the course of pregnancy and childbirth and, of course, the tactics of their management differ significantly. In particular, during pregnancy and childbirth during puberty, there are fewer complications than at a younger age.
In particular, during pregnancy and childbirth during puberty, there are fewer complications than at a younger age.
In addition, cases of pregnancy that occur in girls without signs of precocious puberty (on the one hand) and those who have them (on the other) are to be distinguished. With premature puberty, pregnancy often occurs with its true variant than with pathological (on the basis of a tumor, etc.).
The influence of pregnancy on the body of a girl. There is no doubt that pregnancy, if it occurs at a young age, accelerates the processes of somatic and puberty. The secretion of estrogen and progesterone is not inferior to that of adult pregnant women.
Changes in the bone pelvis are especially evident, which during pregnancy in 13-15-year-olds can reach the size characteristic of 16-18 years old. However, the outer conjugate increases more slowly than the other outer dimensions. Of the young primiparous, 10.7% of births proceed in the presence of an anatomically narrowed pelvis; at the same time, to a greater extent than in adult women, hydrophilicity and elasticity of the ligamentous apparatus, symphysis and cartilaginous zones are expressed. All this provides some flexibility of the bone ring.
All this provides some flexibility of the bone ring.
We have to observe how in a girl without pronounced secondary sexual characteristics before pregnancy, they appear even if the pregnancy was terminated at an early date.
As for the mental reactions of young pregnant women, according to our observations, they correspond to age, but do not outstrip it. Psychopathies and psychoses are rare, mostly with rape (reactive psychosis). A number of character traits revealed in this group are explained by the shortcomings of education. So, after polling 79underage pregnant women, they stated the predominance of their independent character, a tendency to experiment, impracticality, poverty of the emotional world, bad manners.
Features of the course of pregnancy in adolescence. Pregnancy proceeds, as a rule, favorably. Its duration is 38 ± 0.9 weeks, i.e., slightly less than in adult women. Prematurity is 3%. Overlapping is almost not observed. Multiple pregnancy in young is less common (1: 100) than in older age groups.
Early toxicosis was diagnosed by us in isolated cases. Complication of pregnancy by late toxicosis is observed, according to our data, in 0.5%, which is 20 times less than usual. In the literature, there are completely different figures for the frequency of late toxicosis: 46-65.29%.
According to the opinion of the cited authors, pregnancy at a young age is generally complicated by 40-70%. This is significantly different from our data (no more than 5%), as well as from the opinion of W. Stockel, M. Shash and L. Kovacs (1967). Such a significant difference in the nature of the course of pregnancy is undoubtedly due to different tactics of management, in particular, the regular medical supervision adopted in the IMMI clinic throughout pregnancy and carefully observed preventive hospitalization.
Diagnosis of early pregnancy. Diagnosis of pregnancy at a young age is based on the identification of the same supposed, probable and undoubted signs as in adult women, however, the diagnosis is often established with a delay, that is, with the appearance of precisely reliable signs.
The main obstacle to correct and timely diagnosis is the young pregnant woman herself, who, due to a number of circumstances, either does not suspect pregnancy or hides the appearance of dubious (subjective) signs of pregnancy. Sometimes a person whom the girl especially trusts learns about pregnancy for the first time: a school teacher, a pioneer leader, etc.
Often, the first diagnosis of pregnancy is made by the district pediatrician during examination and palpation of the abdomen.
Diagnostic errors in establishing pregnancy at a young age are a fairly common phenomenon. Even at the stage of acquaintance with the anamnesis, the assurances of the relatives accompanying the girl that "pregnancy is impossible here" lead to a medical error.
The integrity of the hymen or the absence of its integrity is not of decisive diagnostic value. Characteristically, in the first trimester of pregnancy, there is insufficient softening of the uterus, some lag in its size from the timing of the delay in menstruation, and a moderate severity of a group of probable signs based on ascertaining softening of the isthmus.
In addition to the generally accepted clinical diagnostic methods, one should not forget about the existence of such additional methods as the determination of placental lactogen, chorionic gonadotropin, abdominal radiography, ultrasound diagnostics, phono- and electrocardiography of the fetus.
In the process of differential diagnosis, it becomes necessary to distinguish pregnancy from the following diseases: anomalies in the development of the uterus, kidney prolapse, tumors of the small pelvis or abdominal cavity, obesity (often accompanied by amenorrhea), primary ectopic pregnancy (often in the right fallopian tube).
Pregnancy management. The very fact of establishing a pregnancy diagnosis imposes additional responsibility on the doctor for the fate of a young mother and her child. First of all, we have to resolve the issue of the possibility of carrying pregnancy and giving birth with minimal damage to health. The decision must be strictly individual. The age of the girl and the gestational age are decisive. Stereotypical decisions aimed at, say, unconditional termination of pregnancy can be harmful, as there are situations, especially in the second trimester, in which the risk associated with termination outweighs the health damage from the burden of pregnancy and childbirth.
The age of the girl and the gestational age are decisive. Stereotypical decisions aimed at, say, unconditional termination of pregnancy can be harmful, as there are situations, especially in the second trimester, in which the risk associated with termination outweighs the health damage from the burden of pregnancy and childbirth.
In healthy girls of 15-17 years of age in the first trimester, a positive decision on the issue of leaving the pregnancy is preferable, because pregnancy and childbirth are usually successful. At the same time, the risk of complications associated with induced abortion at a young age is greater than in adult women. In the presence of serious illnesses or the occurrence of complications that threaten health, an abortion is undertaken according to the relevant indications.
If a schoolgirl has a full term pregnancy, then school attendance is undesirable for ethical and pedagogical reasons. In addition, the study load adversely affects the formation of gestational dominance and can be an etiological moment in the development of late toxicosis of pregnant women. We must not forget that the need for frequent hospitalization also does not favor the continuation of studies.
We must not forget that the need for frequent hospitalization also does not favor the continuation of studies.
The girl is registered at the antenatal clinic and periodically (at least 3 times during pregnancy) goes to the antenatal department, where an in-depth monitoring of her health and the development of the fetus is carried out. Preventive or curative measures are taken as needed; in particular, foci of latent infection are eliminated and the vagina is sanitized. Particular attention in the hospital is given to physio-psycho-prophylactic preparation for childbirth, since it is difficult to do this in the antenatal clinic.
Given that at a young age, childbirth occurs 1-2 weeks earlier than in adult women, the last admission to the hospital should be made no later than 36-37 weeks of pregnancy. During this time, the next examination is carried out, preparations for childbirth are carried out and a plan for their maintenance is drawn up.
The course of childbirth. The course and outcomes of childbirth significantly depend on the girl's belonging to a certain age group. If at the age of 14 and younger the percentage of severe complications is high (15), then in the group of 15-17 years the percentage of complications decreases sharply (1-2).
The course and outcomes of childbirth significantly depend on the girl's belonging to a certain age group. If at the age of 14 and younger the percentage of severe complications is high (15), then in the group of 15-17 years the percentage of complications decreases sharply (1-2).
In women under the age of 14, the following structure of the main complications in childbirth can be outlined:
a) clinical discrepancy between the fetal head and the mother's pelvis,
b) weakness of labor activity,
c) injuries of the birth canal,
d) hypotonic bleeding (listed in descending order).
At the same time, in women in labor 15-17 years old, the structure of complications is somewhat different:
a) rapid delivery,
b) primary weakness of labor,
c) rupture of the cervix and perineum,
d) hypotonic bleeding.
Thus, most of the complications owe their genesis to a violation of the contractility of the uterus, due to both the immaturity of the regulatory links and the inferiority of the executive tissues (myometrium).
Birth management. Delivery of young pregnant women should be carried out in highly qualified institutions, preferably those with specialists with relevant experience and round-the-clock anesthesia and pediatric services. The doctor and midwife require a special approach to the young woman in labor, dictated by the need to reckon with the unusual position, emotional lability, low threshold of pain sensitivity and the constant threat of complications for the mother and fetus.
In the first stage of labor, in parallel with careful monitoring of the dynamics of structural changes in the cervix (external methods are preferred, for example, the Rogovin method), it is necessary to prescribe antispasmodic agents, thereby reducing pain.
The use of anesthesia is based on a sufficient choice of means. The widespread use of painkillers is not justified in cases where there is a high possibility of a clinical discrepancy between the fetal head and the mother's pelvis. For the same reasons, the appointment of strong uterine stimulants is contraindicated.
Surgical interventions among young women in labor are undertaken no more often than usual in clinical practice: perineotomy - in 12%, obstetric forceps - in 1%, caesarean section - in 0.5%. Vacuum extraction of the fetus is not used at all. Those authors who point to a high incidence of late toxicosis in young pregnant women, naturally, give a high percentage of operative delivery (17-22%).
In pregnant women under the age of 14 years (especially younger than 12), it is more likely than at an older age to tend to delivery by caesarean section in a planned manner at term 39-40 weeks. The determining circumstances are the size of the pelvis, the nature of the presentation, the estimated weight of the fetus and the state of health of the girl. 1-3 hours before the production of caesarean section, the fetal bladder is opened. This achieves gradual emptying of the uterus and, consequently, the prevention of hypotonic bleeding and lochiometers.
If the doctor has a hope for a spontaneous completion of labor, then at first he conducts labor conservatively; in the future, the appearance of complications makes it necessary to proceed with operative delivery.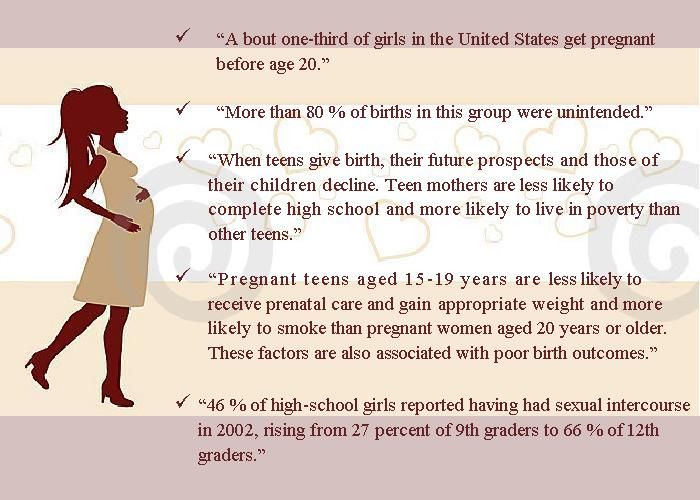 With modern anesthesia, a caesarean section poses no greater risk for a pregnant woman under 14 years of age than, for example, delivery per vias naturales or a fetus-destroying operation. In addition, during the abdominal surgery, it is possible to revise the pelvic organs, in particular, to assess the condition of the ovaries.
With modern anesthesia, a caesarean section poses no greater risk for a pregnant woman under 14 years of age than, for example, delivery per vias naturales or a fetus-destroying operation. In addition, during the abdominal surgery, it is possible to revise the pelvic organs, in particular, to assess the condition of the ovaries.
Transfer to the postpartum department after spontaneous delivery and examination of the soft birth canal is usually carried out not after 2-4 hours, but after 10-12 hours due to fear of not noticing the onset of hypotonic bleeding.
In the postpartum period, the issue of breastfeeding is solved in different ways, depending on the plans of the guardians, the adoptive parents of the child. In relation to women in childbirth under the age of 14 and older who refuse children, measures are taken to stop lactation. Subsequently, a visit by a girl to the same group of students, obviously, cannot be considered justified from a pedagogical point of view.