Can you breastfeed with genital herpes
Herpes Simplex Virus (HSV) | Breastfeeding
Herpes simplex virus (HSV) in infants can be severe. Mothers with HSV can continue to breastfeed if no lesions are present on the breasts and if lesions elsewhere on the body are carefully and fully covered. Mothers with active lesions on the breast should temporarily stop breastfeeding from the affected breast and should not feed expressed breast milk from the affected breast.
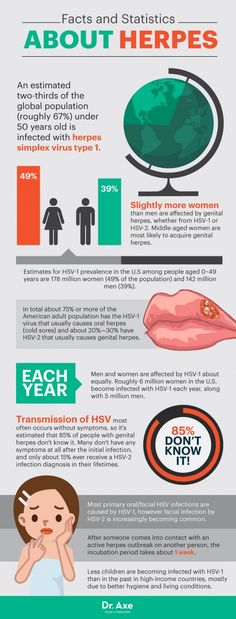
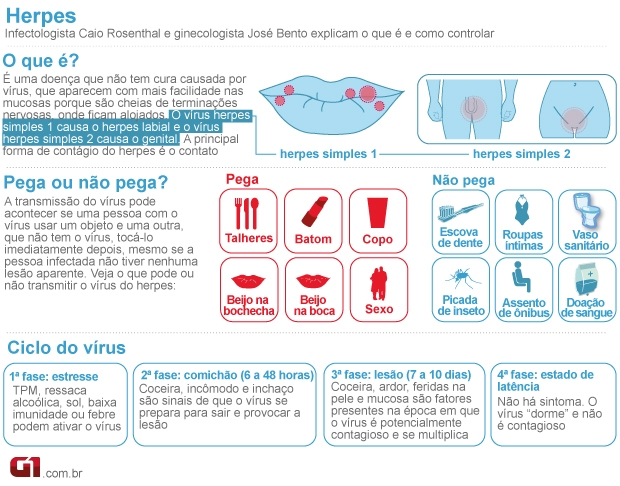
Herpes simplex virus (HSV) is a lifelong virus that is categorized into two distinct herpesvirus species, herpes simplex virus 1 (HSV-1) and herpes simplex virus 2 (HSV-2). HSV-1 is typically transmitted by oral-oral contact to cause oral herpes but can also cause genital herpes through oral-genital contact. HSV-2 is typically sexually transmitted and causes genital herpes but can also cause infections in the mouth. Importantly, both types of virus can cause herpes disease in newborns and infants and can appear anywhere on the body.
In newborn infants, HSV infections are often severe and result in high rates of mortality and morbidity. Every precaution needs to be taken to prevent infants from being exposed to the herpes virus and appropriate hand hygiene should be done before holding the infant.
Is it safe for a mother to breastfeed if she has active herpetic lesions?
Maybe. Women with herpetic lesions may transmit HSV to their infants by direct or indirect contact with the lesions. Breastfeeding is acceptable if no lesions are present on the breasts and if active lesions elsewhere on the mother are carefully and fully covered. In cases where a mother has herpetic lesions on her breast, the mother should temporarily refrain from breastfeeding her infant from the affected breast or feeding her infant expressed breast milk from the affected breast. She should discard expressed breast milk from the affected side until the lesions have healed. A mother may breastfeed her infant or express milk from the unaffected breast but should ensure that the lesions on the affected breast are completely covered to avoid transmission.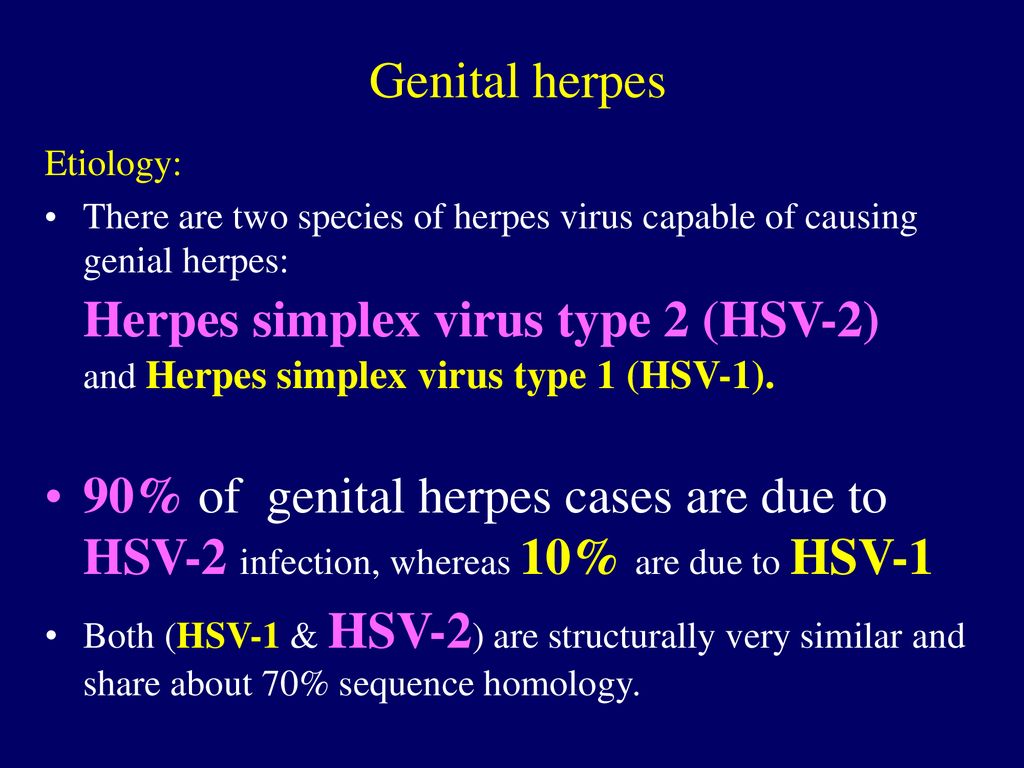 Mothers should also follow appropriate hand hygiene practices to avoid transmission of herpes to her infant.
Mothers should also follow appropriate hand hygiene practices to avoid transmission of herpes to her infant.
Providers: Lesions on the breast could easily be mistaken for impetigo or eczema. Questionable lesions should be tested promptly for HSV so that if positive, acyclovir (safe to use while breastfeeding) can be administered quickly and breastfeeding can be discontinued until the lesion has healed.
Some mothers may need additional support to maintain their milk production and/or supplement with their expressed human milk (previously expressed milk or expressed milk from the unaffected breast) or formula while herpetic lesions on the breast are healing. Mothers should talk with their physicians to determine if their lesions have healed and they can resume breastfeeding or expressing milk from the affected breast.
Is it safe for a mother to give her infant hand expressed or pumped breast milk if she has active herpetic lesions on her breast?
No.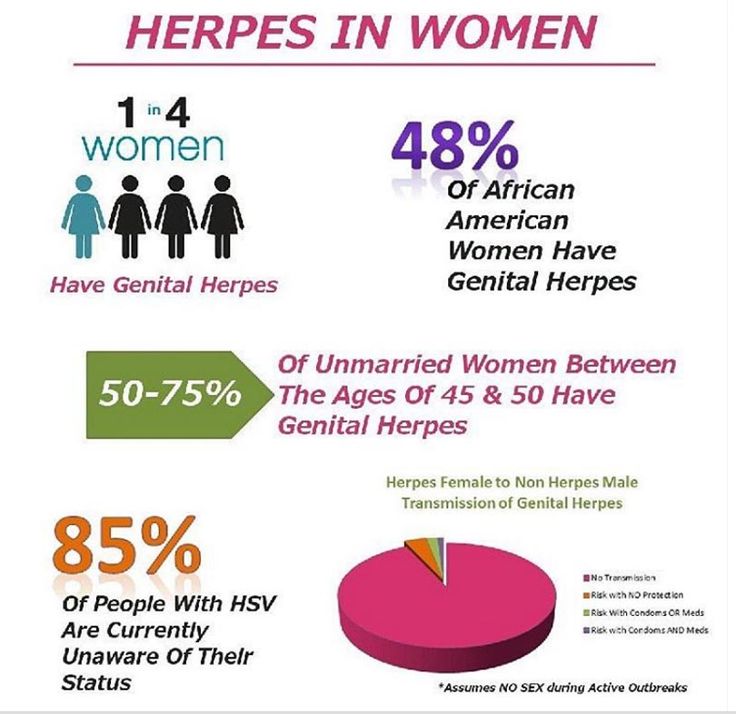 Breast milk can be contaminated if it comes in contact with active herpetic lesions through touching the breast during hand expression or via the pump. Therefore, if a mother has herpetic lesions on her breast, she should discard expressed breast milk from the affected side until the lesions have healed. Expressing breast milk will be important for maintaining milk production while not directly breastfeeding from the affected breast. Mothers should be vigilant about practicing appropriate hand hygiene and cleaning the pump parts thoroughly. Mothers should talk with their healthcare provider to determine if their lesions have healed and they can resume breastfeeding or expressing milk from the affected breast.
Breast milk can be contaminated if it comes in contact with active herpetic lesions through touching the breast during hand expression or via the pump. Therefore, if a mother has herpetic lesions on her breast, she should discard expressed breast milk from the affected side until the lesions have healed. Expressing breast milk will be important for maintaining milk production while not directly breastfeeding from the affected breast. Mothers should be vigilant about practicing appropriate hand hygiene and cleaning the pump parts thoroughly. Mothers should talk with their healthcare provider to determine if their lesions have healed and they can resume breastfeeding or expressing milk from the affected breast.
It is safe to use expressed breast milk from the unaffected breast, as long as the mother ensures that the lesions on the affected breast are completely covered to avoid transmission. Appropriate hand hygiene and cleaning the pump parts thoroughly are still important.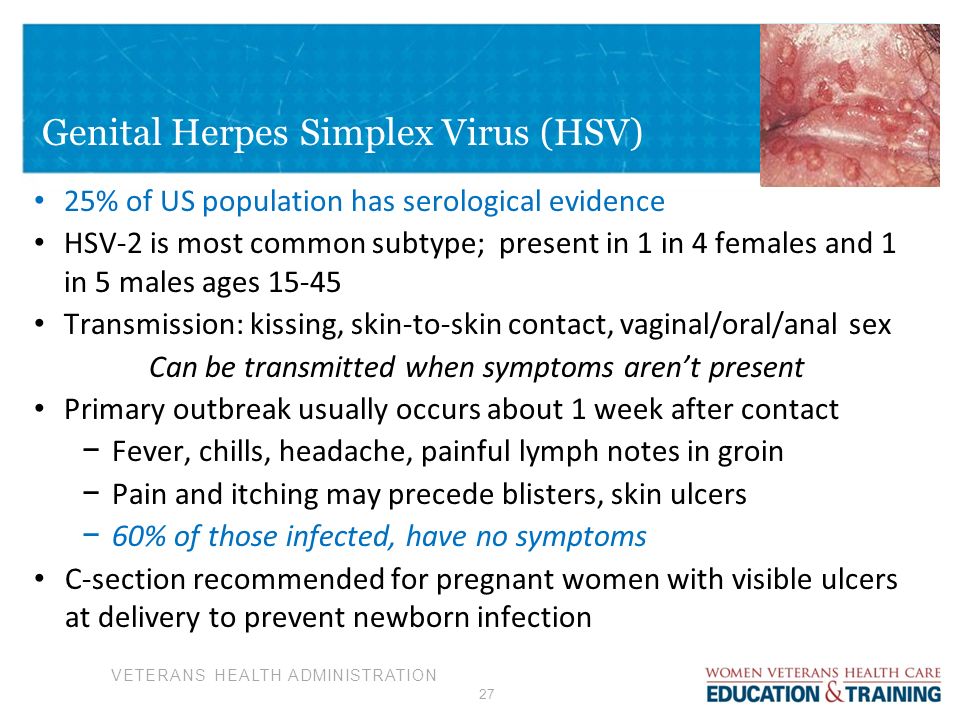
For more information about managing breastfeeding with specific medical conditions, read Lawrence RA, Lawrence R. (2016) Breastfeeding: A guide for the medical profession, 8th Edition.
Herpes and Breastfeeding - Breastfeeding Support
The herpesvirus family includes herpes simplex virus and varicella-zoster virus. An infection with herpes simplex virus is commonly known as herpes and varicella-zoster virus causes chicken pox and shingles. Symptoms of a herpesvirus infection include outbreaks of little blisters or sores on the skin which could include the breasts or nipples. If you think you might have one of these infections, consult with your doctor to get a positive diagnosis as blisters on nipples can have other causes. This article looks at frequently asked questions if you are breastfeeding and have herpes simplex virus or varicella-zoster virus.
Sign Up to the Newsletter
Get breastfeeding articles in your inbox
Herpes simplex virus
There are two herpes simplex viruses; type 1 (HSV-1) and type 2 (HSV-2).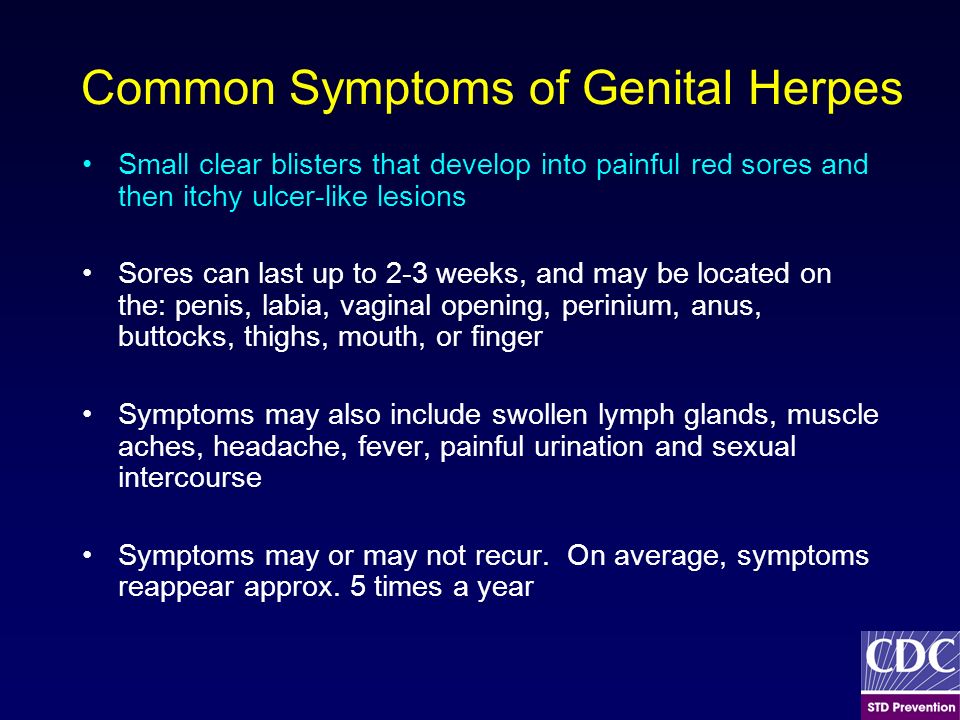 An infection with herpes simplex 1 usually appears as an open sore (known as a cold sore) or small blisters (fever blisters) in the mouth area causing oral herpes but HSV-1 can also cause genital herpes. HSV-2 is almost exclusively transmitted through sexual contact, producing blisters on the skin and the moist lining of the genital or anal organs (genital herpes).1 The small, painful, red-rimmed blisters containing viral material dry and form a scab after a few days (similar to chicken pox lesions). The blisters can appear anywhere on the body including the breast.
An infection with herpes simplex 1 usually appears as an open sore (known as a cold sore) or small blisters (fever blisters) in the mouth area causing oral herpes but HSV-1 can also cause genital herpes. HSV-2 is almost exclusively transmitted through sexual contact, producing blisters on the skin and the moist lining of the genital or anal organs (genital herpes).1 The small, painful, red-rimmed blisters containing viral material dry and form a scab after a few days (similar to chicken pox lesions). The blisters can appear anywhere on the body including the breast.
Can I breastfeed with herpes?
If a mother has herpes simplex virus, she can still breastfeed as long as the following precautions are observed:
#1 Prevent baby from touching the sores
As these viruses are spread by simply touching the sores, it is important that your baby doesn’t come into skin-to-skin contact with any of the herpes lesions. Sores should be completely covered so the baby cannot touch them.2
Sores should be completely covered so the baby cannot touch them.2
#2 Observe strict hygiene
Observing strict hygiene by washing hands thoroughly with soap before breastfeeding and sterilising breast pump parts after each use will help prevent spreading the infection.3
#3 Seek medical advice for babies under three weeks of age
Herpes can be very dangerous and life threatening for a newborn baby up to three weeks of age. A mother should speak to her healthcare provider for the latest recommendations and precautions if she has a very young baby and suspects she has herpes or has recurrent herpes.4
#4 Avoid kissing your baby if you have oral lesions
A mother with a cold sore on her lip can breastfeed but should be warned not to kiss her newborn and to wash her hands often and be very careful about hygiene precautions while the sore is active (Lawrence and Lawrence, 2016).
Can I breastfeed if herpes sores are on the breast or nipple?
If active herpes sores are on a breast or nipple, mothers are advised not to breastfeed from that breast until the lesions have dried.56 Mohrbacher clarifies that breastfeeding can continue if it is possible to cover all the sores so the baby does not come into any contact with them otherwise breastfeeding could continue on the other breast if there are no lesions on that breast (Mohrbacher, 2020 p731). Treatment with antiviral medications may reduce the period of active herpes lesions (Lawrence and Lawrence, 2016).
The breast milk from a breast with an active herpes lesion will need to be expressed to maintain the mother’s milk supply and prevent engorgement or mastitis. If this milk can be expressed without it coming into any contact with a herpes sore (or any breast pump part or hand that has been in contact with a sore), the expressed milk can be given to the baby. However if the milk has been in contact with a sore it should be thrown away (Mohrbacher, 2020, p731).
If this milk can be expressed without it coming into any contact with a herpes sore (or any breast pump part or hand that has been in contact with a sore), the expressed milk can be given to the baby. However if the milk has been in contact with a sore it should be thrown away (Mohrbacher, 2020, p731).
Can I breastfeed a toddler who has oral herpes?
If a breastfed toddler has oral herpes there is a risk of transferring HSV-1 from the child’s mouth to the mother’s nipples by breastfeeding.7 However by the time the mother is aware that her little one has sores on their lips or in their mouth it is likely that she will have already been exposed to the virus because cold sores/herpes ulcers in the mouth are contagious for a day or two before the lesions appear.89 Many people carry the herpes simplex virus without having any symptoms10 which will make it difficult for a mother to gauge her risk of getting the infection if she doesn’t have a history of herpes.
Jack Newman, a Canadian paediatrician and breastfeeding expert, says that a child with herpes ulcers in the mouth (herpes stomatitis) can carry on breastfeeding as the mother will have already been infected a few days before the sores appeared.11 Newman adds that if the mother does develop sores on her nipple she can continue breastfeeding if she is able to, but if the sores make breastfeeding too painful, hand expressing breast milk for the toddler is likely to be more comfortable than pumping until the sores heal. The mother should discuss her situation with her healthcare provider for the latest medical advice including whether antiviral medication is recommended (see below).
The mother should discuss her situation with her healthcare provider for the latest medical advice including whether antiviral medication is recommended (see below).
Is herpes passed on through breast milk?
The risk of catching herpes from breast milk is very low. Authors Wambach & Spencer state it is “doubtful” that HSV infection can be transmitted via human milk. Transmission during lactation is more likely to occur with direct contact with an active lesion or blister.12
The following paper also states the risk of viral transmission via breast milk is very low and that breastfeeding ought not be interrupted unless the sores are on the breasts:
Excerpt From
Recommendations for breastfeeding during maternal infections J Pediatr (Rio J), Lamounier et al, 2004
It is important that baby doesn’t come into skin-to-skin contact with any herpes lesionsThe risk of viral transmission via breast milk is very low. In nursing mothers with herpes, breastfeeding should not be interrupted, except when the herpetic vesicles are located on the breasts.
Active lesions in other body parts should be covered, and the nursing mother’s hygiene should not be overlooked so that breastfeeding can be maintained.
Herpes treatment and breastfeeding
Although there is not a cure for herpes, antiviral treatments (drugs and topical creams) focus on relieving symptoms and preventing the spread of HSV (Wambach and Spencer, 2020). Lawrence and Lawrence 13 state that oral or IV acyclovir (Zovirax) and valacyclovir (Valtrex) are compatible with breastfeeding. For the latest information on compatibility of antiviral drugs with breastfeeding refer to the resources listed in Medications and Breastfeeding, e.g. Hale’s Medications and Mothers’ Milk [paywall], Lactmed or e-lactancia.
Varicella-zoster virus
Varicella-zoster virus also belongs to the herpesvirus family, it affects the central nervous system and an infection can cause chickenpox (varicella) and shingles (zoster).
Breastfeeding and chickenpox
Chickenpox is generally a mild contagious childhood illness.14 Most adults will have immunity to it as they will already have had it as a child or been immunised against it in some countries.
Can I breastfeed with chickenpox?
If a mother develops chickenpox for the first time while breastfeeding, she can continue to breastfeed because her baby will have already been exposed to the infection before the blisters came out, and immune factors in breast milk can help the baby’s recovery.151617
Caution for the newborn baby
Note, if a mother develops chickenpox for the first time up to five days before or two days after her baby’s birth (Wambach and Spencer, 2020; e-lactancia, 2020), this could be very dangerous for her baby and she should seek urgent medical advice from her health professionals.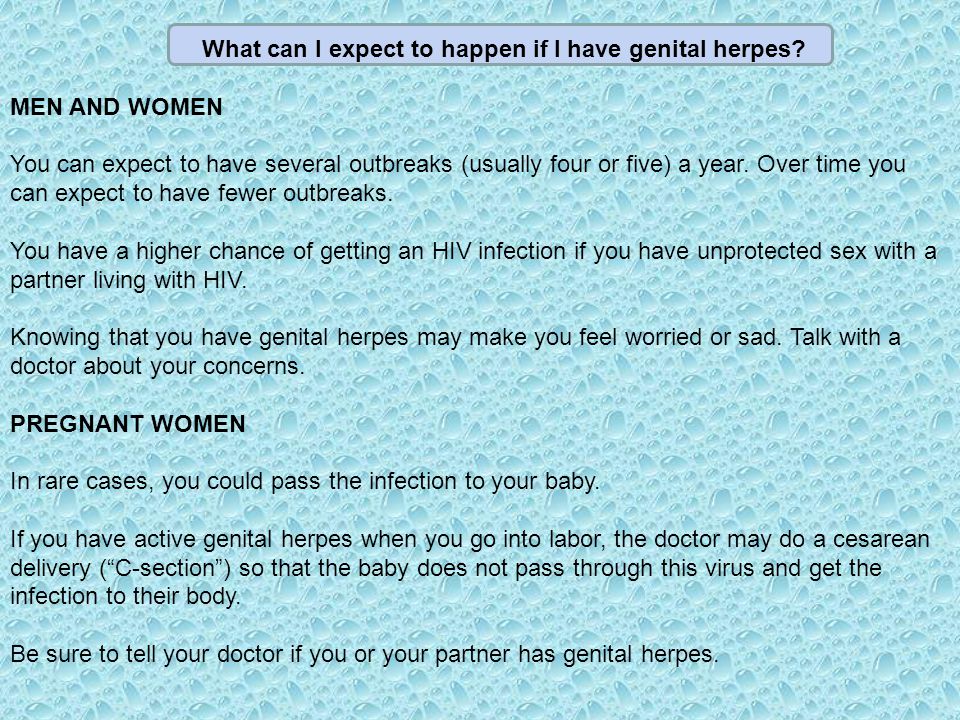 18 Breastfeeding can continue in this situation, but the baby will require treatment against the virus and the mother is advised to take special hygiene precautions, and avoid her baby being in contact with any skin lesions until they are fully crusted.1920 Paediatrician Jack Newman explains:
18 Breastfeeding can continue in this situation, but the baby will require treatment against the virus and the mother is advised to take special hygiene precautions, and avoid her baby being in contact with any skin lesions until they are fully crusted.1920 Paediatrician Jack Newman explains:
Excerpt from
Dr. Jack Newman’s Guide to Breastfeeding (updated edition), Jack Newman and Teresa Pitman, 2014
Infected babies should be given zoster immune globulin (antibodies against the virus) immediately at birth and acyclovir or a similar drug to prevent the baby from getting very sick. The baby and mother should not be separated. The baby should be breastfed to get the immune factors present in the milk that will help protect his mucous membranes from invasion by the virus.
For more information about symptoms and treatments see Chickenpox and Breastfeeding, Breastfeeding Network, 2019.
Speak to a health professional if you think you have herpes or chicken pox and your baby is newly bornShingles and breastfeeding
If you have already had chickenpox, the virus can sometimes flare up again years later as shingles (herpes zoster virus). It causes a painful rash that develops into blisters usually affecting just one area of the body which may include the breast. It is possible to catch chickenpox from someone with shingles if you have not had it before—by skin-to-skin contact with the blisters.
Can I breastfeed with shingles?
Doctor Jack Newman explains that the baby of a mother with shingles will already have some immunity to chickenpox from his mother and breastfeeding can continue:
Excerpt from
Dr. Jack Newman’s Guide to Breastfeeding (updated edition), Jack Newman and Teresa Pitman, 2014
So, if the mother gets shingles, should she stop breastfeeding? Absolutely not.
She is immune. She had chicken pox in the past and the baby got antibodies from her during pregnancy. These antibodies remain in the baby’s blood for about six months; plus, he will receive immunity through breastfeeding. If the mother is treated with acyclovir or a similar drug and painkillers, she does not have to interrupt breastfeeding.
Lesions on the breast?
The Academy of Breastfeeding Medicine advises against breastfeeding from a breast with shingles lesions until they have healed:
Excerpt from
ABM Clinical Protocol #26: Persistent Pain with Breastfeeding, Academy of Breastfeeding Medicine, 2016
Exposure to these [shingles] lesions can result in chicken pox (varicella zoster) in unimmunized infants. In most situations, it should be treated similarly to a Herpes simplex infection and women should not breastfeed or use expressed breast milk from an affected breast until the lesions have healed. Infants may be given Zoster immunoglobulin if appropriate.
Cover lesions
The Breastfeeding Network indicates if the lesions can be covered there is little risk of passing on the infection:
Excerpt from
Shingles and Breastfeeding, Breastfeeding Network, 2019
If the rash is only on your body and can be covered by clothing, there’s little risk of passing the infection on to others even before the lesions have dried.
Summary
If a mother has herpes simplex virus she can continue to breastfeed as long as any herpes lesions are covered so that her baby has no contact with the sores. If active lesions are on a breast/nipple, breastfeeding will need to be interrupted from that breast until the sores heal. Contact with herpes can be very dangerous for a baby under three weeks of age and a mother should contact her doctor for advice if she suspects she might have herpes in the early weeks after birth. Breastfeeding can continue if a mother has chicken pox for the first time while she is breastfeeding, but again this can be dangerous for a newborn baby in their first week of life, and a health professional should be consulted so that appropriate precautions can be taken. Shingles is compatible with breastfeeding, the recommendation being to cover all lesions so that baby has no direct contact with any active sores.
Shingles is compatible with breastfeeding, the recommendation being to cover all lesions so that baby has no direct contact with any active sores.
This article should not be considered a substitute for advice from your health professionals. Any medical concerns about yours and your baby’s welfare should be discussed with your doctor, paediatrician or health care provider.
Footnotes & References
-
Herpes Simplex Virus. World Health Organisation. 2020
-
Mohrbacher. Breastfeeding Answers A Guide for Helping Families. 2020. p822
-
Breastfeeding and Human Lactation 6e, Wambach and Spencer. 2021. p 164
-
Mohrbacher. Breastfeeding Answers A Guide for Helping Families. 2020. p731
-
ABM Clinical Protocol #26: Persistent Pain with Breastfeeding, Academy of Breastfeeding Medicine, 2016
-
Breastfeeding, A Guide for the Medical Profession, 8e, Lawrence and Lawrence, 2016
-
Sealander and Kerr.
 Herpes simplex of the nipple: infant-to-mother transmission. Am Fam Physician. 1989
Herpes simplex of the nipple: infant-to-mother transmission. Am Fam Physician. 1989 -
Cold sores. NHS. 2020
-
Newman. Breastfeeding and Maternal Illness Part 2. updated 2020 [accessed 10 November 2020]
-
Globally, an estimated two-thirds of the population under 50 are infected with herpes simplex virus type 1. WHO. 2015
-
Newman. Breastfeeding and Maternal Illness Part 2. updated 2020 [accessed 10 November 2020]
-
Breastfeeding and Human Lactation 6e, Wambach and Spencer. 2021. p 163
-
Breastfeeding, A Guide for the Medical Profession, 8e, Lawrence and Lawrence, 2016
-
Chickenpox, National Health Service (NHS), 2017
-
Breastfeeding and Human Lactation, Wambach and Spencer, 2021
-
Dr Jack Newman’s Guide to Breastfeeding, Jack Newman and Teresa Pitman, 2014
-
Varicella-Zoster Virus, e-lactancia, 2020
-
Chickenpox and Breastfeeding, Breastfeeding Network, 2019
-
Breastfeeding and Human Lactation, Wambach and Spencer, 2020
-
Varicella-Zoster Virus, e-lactancia, 2020
Mother with genital herpes: is it possible to breastfeed
Genital herpes during breastfeeding is not a contraindication. Moreover, along with milk, the child will receive protective antibodies.
Moreover, along with milk, the child will receive protective antibodies.
However, during this period, you should be very careful, because there is a high risk of infection of the baby. And only in some cases it is recommended to stop HB for the duration of treatment.
In this article you will learn:
- Symptoms
- How to prevent infection in your baby
- Why is herpes dangerous for a child
- Can I breastfeed if I have herpes?
- Feeding rules
- Precautions
- How to strengthen the immune system?
- Diagnosis of genital herpes in a nursing mother
- Treatment of the disease during lactation
- How is genital herpes treated after childbirth
Symptoms
Herpes in a nursing mother can appear on any part of the body. Depending on the type of pathology, the following symptoms are distinguished:
- The first type of herpes. Most often, rashes appear on the lips, but can be localized on the cheeks or on the nose.
 The first symptoms of the disease are characterized by the appearance of itching and burning in the area where pimples appear after a few hours. Gradually, they will increase in size and merge with each other. The blisters are filled with a fluid that contains a "concentrate" of the virus. When the bubbles burst, weeping sores form in their place. As they dry, a crust forms, which comes off on its own.
The first symptoms of the disease are characterized by the appearance of itching and burning in the area where pimples appear after a few hours. Gradually, they will increase in size and merge with each other. The blisters are filled with a fluid that contains a "concentrate" of the virus. When the bubbles burst, weeping sores form in their place. As they dry, a crust forms, which comes off on its own. - Genital herpes, or type 2. In women, the skin in the vulva, perineum, anus and vagina turns red. Hyperemic mucosa swells. All this is accompanied by severe itching. Additionally, herpes in a nursing mother can provoke frequent urination, heaviness in the abdomen (below), headache, irritability, nausea, or fever. The affected area is covered with vesicles that are filled with a cloudy liquid. When pimples burst, sores appear in their place. They are covered with a yellow purulent coating (read more here).
- Herpes zoster (type 3). Initially, a woman experiences general signs of malaise.
 At the end of the promoral period, there is a sensation of itching and burning in the direction of the peripheral nerves. A rash will soon form on this part of the body. Pimples do not merge with each other. From the inside they are filled with serous fluid. Rashes are localized along the dorsal nerve ganglia. Bilateral involvement is rare.
At the end of the promoral period, there is a sensation of itching and burning in the direction of the peripheral nerves. A rash will soon form on this part of the body. Pimples do not merge with each other. From the inside they are filled with serous fluid. Rashes are localized along the dorsal nerve ganglia. Bilateral involvement is rare.
How to prevent infection of the baby
After the birth of a child, a woman's body experiences increased stress, as a result of which the immune system is significantly weakened. Therefore, very often it is during this important period that many ailments worsen, especially genital herpes. This may be the first episode or recurrence of the disease.
Genital herpes is characterized by the appearance of rashes on the external and internal genital organs. These vesicles contain active virus. Therefore, a woman must take all possible measures to prevent its spread and protect the child. To do this, you must strictly adhere to certain rules:
- Breastfeeding during genital herpes does not need to stop.
 After all, the child does not come into contact with rashes, so there is no direct risk for infection. The only exception is when herpetic vesicles appear on the nipples. Therefore, it is strictly forbidden to feed the baby with a sick breast. The second mammary gland can be given, but strictly ensure that the child does not touch the patient.
After all, the child does not come into contact with rashes, so there is no direct risk for infection. The only exception is when herpetic vesicles appear on the nipples. Therefore, it is strictly forbidden to feed the baby with a sick breast. The second mammary gland can be given, but strictly ensure that the child does not touch the patient. - Personal hygiene. In no case should the crumbs be allowed to come into contact with the rashes. After carrying out water procedures or treating the skin and mucous membranes, a woman must wash her hands well with soap and water. After all, there is a high risk of damage to the bubbles and the virus getting on the skin. If there is a baby in the house, you need to wash your hands every time you go to the baby, change the diaper, feed, etc. This simple rule will minimize the risk of infection.
- For hygienic procedures, use towels and other accessories specially allocated for this purpose.
Why is herpes dangerous for a child? It remains for life, "lives" in the cells of peripheral nerves.
 In a normal state of immunity, there are no clinical manifestations of the disease. If for one reason or another the immune system weakens, an exacerbation occurs. In many women, they occur at fairly short intervals, which creates problems when breastfeeding.
In a normal state of immunity, there are no clinical manifestations of the disease. If for one reason or another the immune system weakens, an exacerbation occurs. In many women, they occur at fairly short intervals, which creates problems when breastfeeding. Is herpes dangerous for a baby during lactation? Infection with the virus occurs through direct contact with the affected areas of the skin. If the child does not come into contact with them, infection will not occur. In addition, in the breast milk of a mother during an exacerbation there are many protective antibodies. They enter the body of the baby, create additional protection. First of all, this applies to herpes zoster. After all, the same virus causes chickenpox in children.
Proper breastfeeding of a child with herpes The only case when herpes is really dangerous for infants is its localization on the nipples. Then the probability of infection is really high and there is a question about the compatibility of herpes and breastfeeding.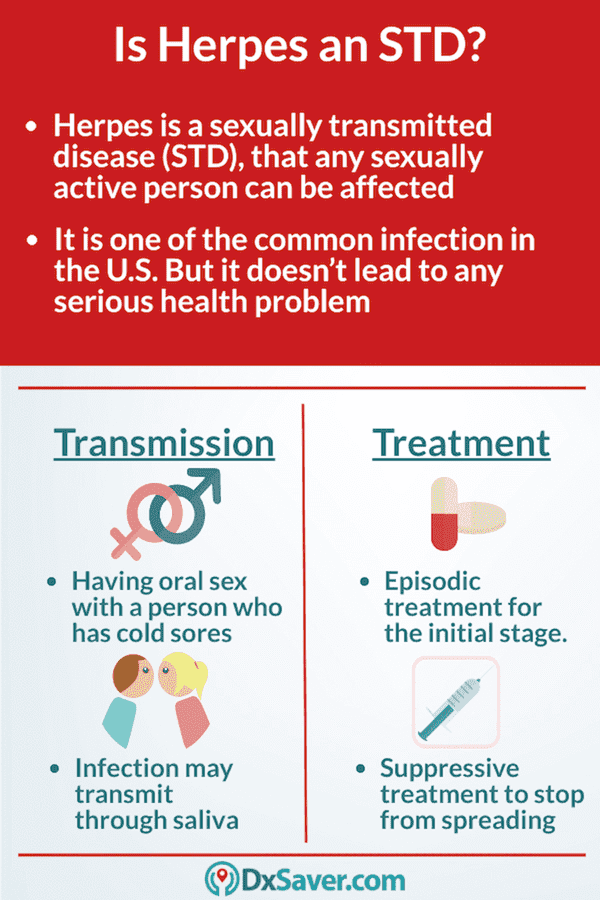 Doctors recommend temporarily stopping it until the treatment is over and the rashes go away.
Doctors recommend temporarily stopping it until the treatment is over and the rashes go away.
Herpetic infection in children is much more severe than in adults. When infected with herpes of the first type, painful aphthae appear in the mouth, the temperature rises, the child refuses to eat. Chicken pox in infants is accompanied by generalized rashes, severe body condition, and fever. Fortunately, maternal antibodies protect babies and infection is rare if all prevention rules are followed.
Can I breastfeed if I have herpes?
Breastfeeding is considered to prevent infection in the baby. If a woman is infected with an infection, during breastfeeding, the production of specific antibodies that inhibit the activity of herpes is activated. It takes 3-4 days to block the exacerbation. The produced antibodies penetrate into breast milk and are transmitted to the baby, thereby preventing the infection of the child - antibodies form immunity against infection.
If the child does not come into contact with inflamed tissue, the risk of infection is less than 0.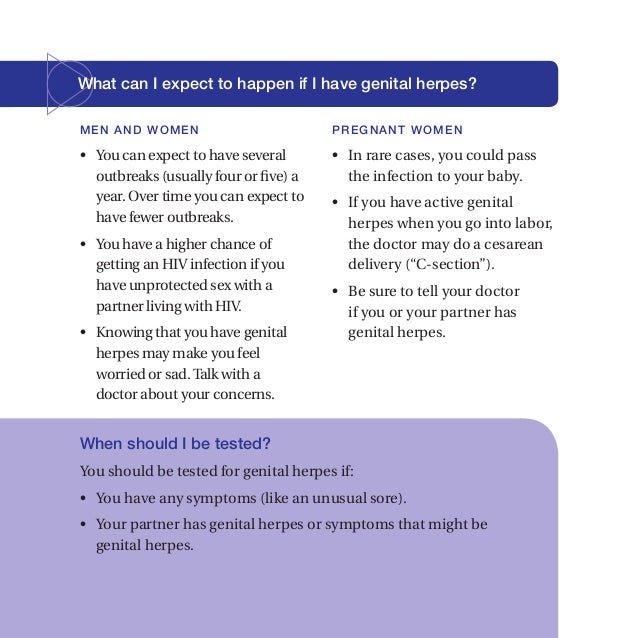 1%. But at the same time, it is important to follow strict rules that will protect the baby from infection.
1%. But at the same time, it is important to follow strict rules that will protect the baby from infection.
Feeding rules
- Avoid contact of the baby with infected tissue.
- Hand sanitizer before every feeding.
- Do not interrupt the course of treatment before the term prescribed by the doctor.
Stopping breastfeeding is recommended only in cases of herpes rash in the nipple area. At the same time, if one gland is affected, only healthy ones are used for feeding. With the defeat of any other part of the body, HB continues.
Precautions
Maternal chipes and breastfeeding are compatible. But women should take precautions to ensure that the baby does not contract the virus. How can a mother protect her child from infection?
To do this, she should avoid direct contact of the affected areas with the delicate, receptive skin of the baby, wear a gauze bandage during feeding and strictly observe the rules of personal hygiene.
How to strengthen immunity?
It must be understood that in case of viral infections we take drugs that suppress the reproduction of the virus, but the main role is still played by the state of the patient's immunity. Immune cells secrete antibodies that destroy viruses and prevent them from spreading in the body. Therefore, supporting our defenses is no less important point of treatment than taking antiviral drugs.
If genital herpes is exacerbated by breastfeeding, a young mother needs to ensure that her diet is rich in proteins, because it is from them that immune cells produce antibodies. If a woman has strictly limited her diet and, for example, eats only buckwheat and apples, it is difficult to expect effective protection from her immune system. Recall that most often a strict diet during breastfeeding is not needed.
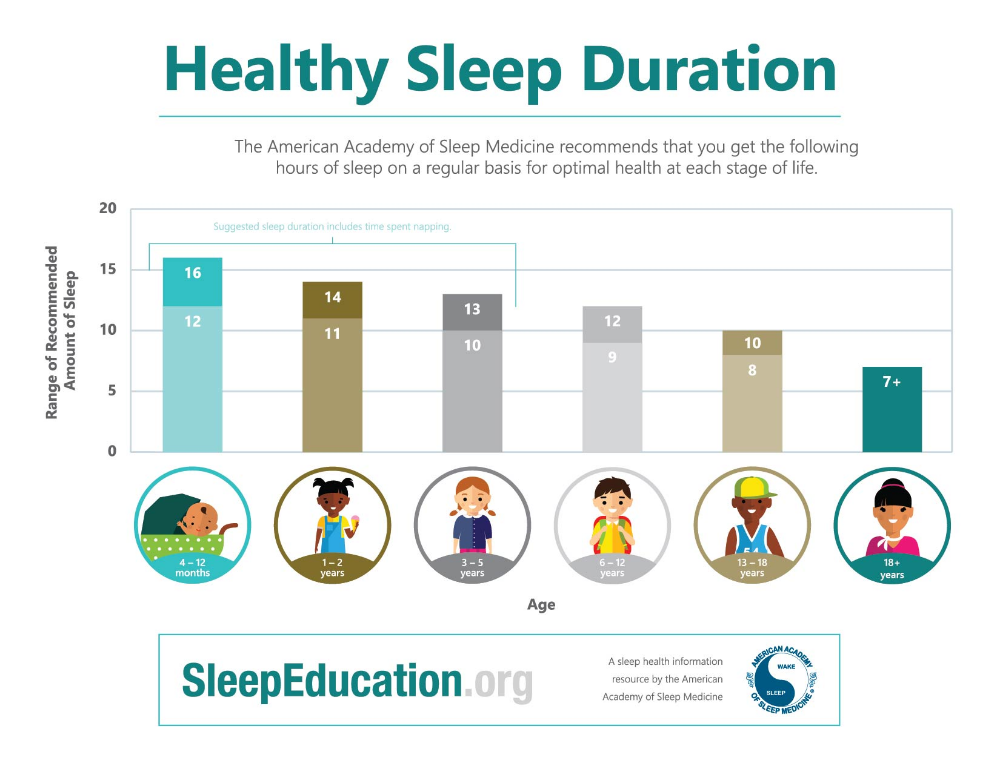
It is equally important to get enough sleep and rest. Nursing mothers often perceive this advice as an impossible condition. But maybe try to explain to relatives that if a woman goes to the hospital, it won’t make anyone feel better, and it’s better to help her now and give her time to rest than to stay at home alone with a baby later.
But maybe try to explain to relatives that if a woman goes to the hospital, it won’t make anyone feel better, and it’s better to help her now and give her time to rest than to stay at home alone with a baby later.
Sometimes immunomodulatory drugs are used to treat herpes (for example, suppositories "Kipferon", "Viferon"), but you cannot prescribe drugs of this group to yourself. Not all of them are compatible with HB, and besides, their thoughtless use can affect immunity in the most unpredictable way.
Diagnosis of genital herpes in a breastfeeding mother
For a breastfeeding mother to be diagnosed, a doctor should be consulted. The specialist will be able to diagnose genital herpes during the initial examination. To determine the exact diagnosis, the patient is sent for laboratory tests.
To identify the type of causative agent of the disease, a smear is taken from the affected area, after which sowing is carried out. But tank culture is not always an informative study: the results of the analysis can be false negative.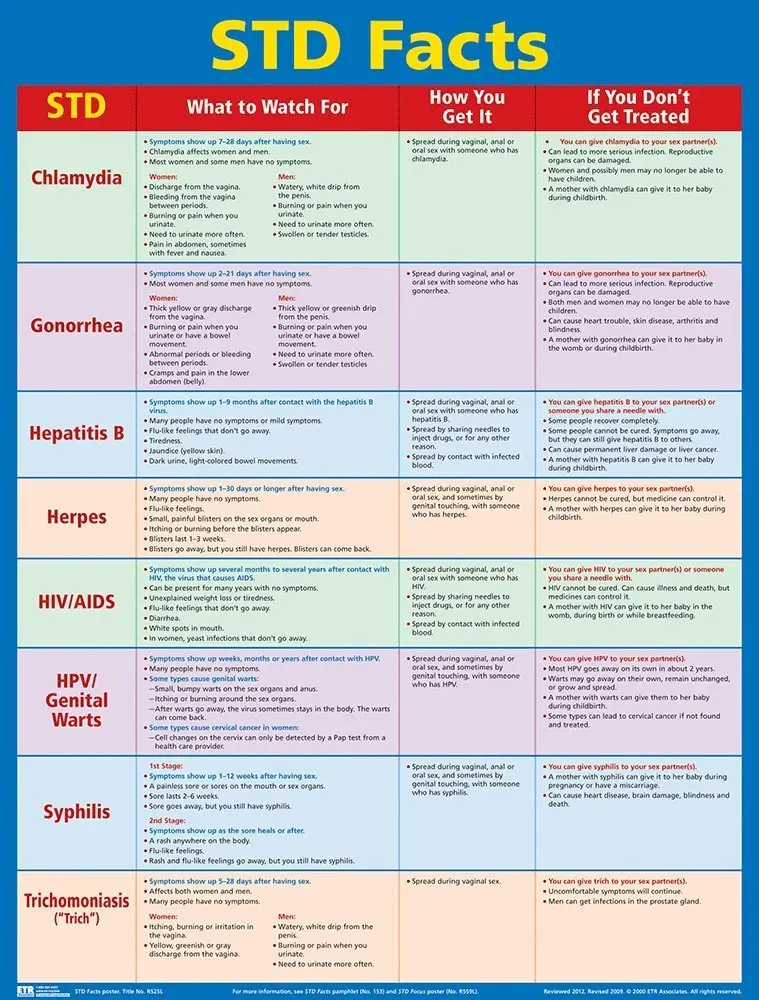 Therefore, it is recommended to conduct this study a few days after the appearance of signs of genital herpes in a nursing mother.
Therefore, it is recommended to conduct this study a few days after the appearance of signs of genital herpes in a nursing mother.
In case of a recurrent form, it is possible to identify the pathogen with a probability of no more than 30%. Another way to make a diagnosis is the chain reaction method. For its implementation, a sample of the material of the affected area is required. The most reliable method for determining the presence of the virus in the body of a nursing mother is blood tests.
An enzyme-linked immunosorbent assay is carried out, during which it is possible to study the level of antibodies in the body of a nursing mother. Enzyme immunoassay can be quantitative, which allows you to detect the level of antibodies. If a large number of antibodies are found, this indicates a recent recurrence of genital herpes. Qualitative enzyme immunoassay is aimed at studying the type of virus.
Treatment of lactation disease
The appearance of signs of genital herpes requires immediate medical attention.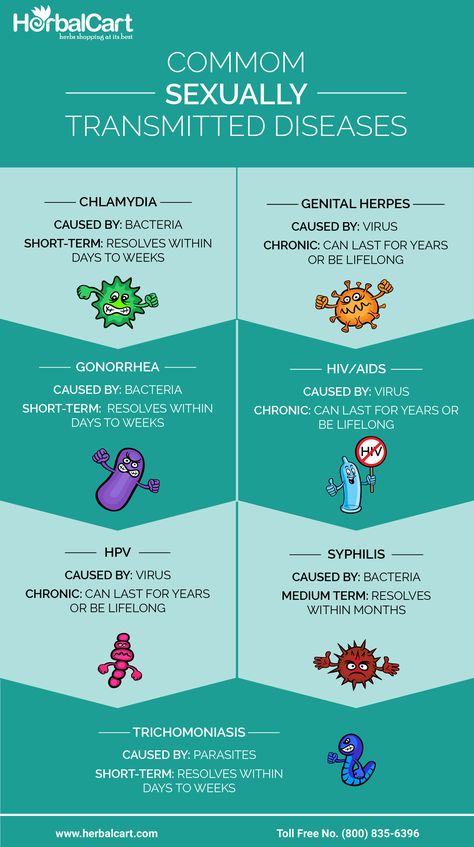 This is necessary in order to make sure of the diagnosis, especially if this is a first episode. After all, there are many varieties of infectious and other ailments, accompanied by the appearance of a rash in the genital area.
This is necessary in order to make sure of the diagnosis, especially if this is a first episode. After all, there are many varieties of infectious and other ailments, accompanied by the appearance of a rash in the genital area.
In addition, herpesvirus infection is accompanied by the occurrence of pain, itching, swelling of tissues, mucous membranes and other unpleasant sensations, which lead to a significant deterioration in well-being. In some cases, chills, severe weakness, drowsiness, aching bones and muscles, and fever may occur. This threatens to reduce the amount of milk produced and even successful breastfeeding.
Only a doctor can prescribe treatment for herpes. After all, the bulk of pharmacological preparations is strictly prohibited for use during lactation. This is due to the fact that antiviral components are able to penetrate into breast milk and thus affect the baby.
Based on the examination of the patient, the doctor develops an individual treatment plan.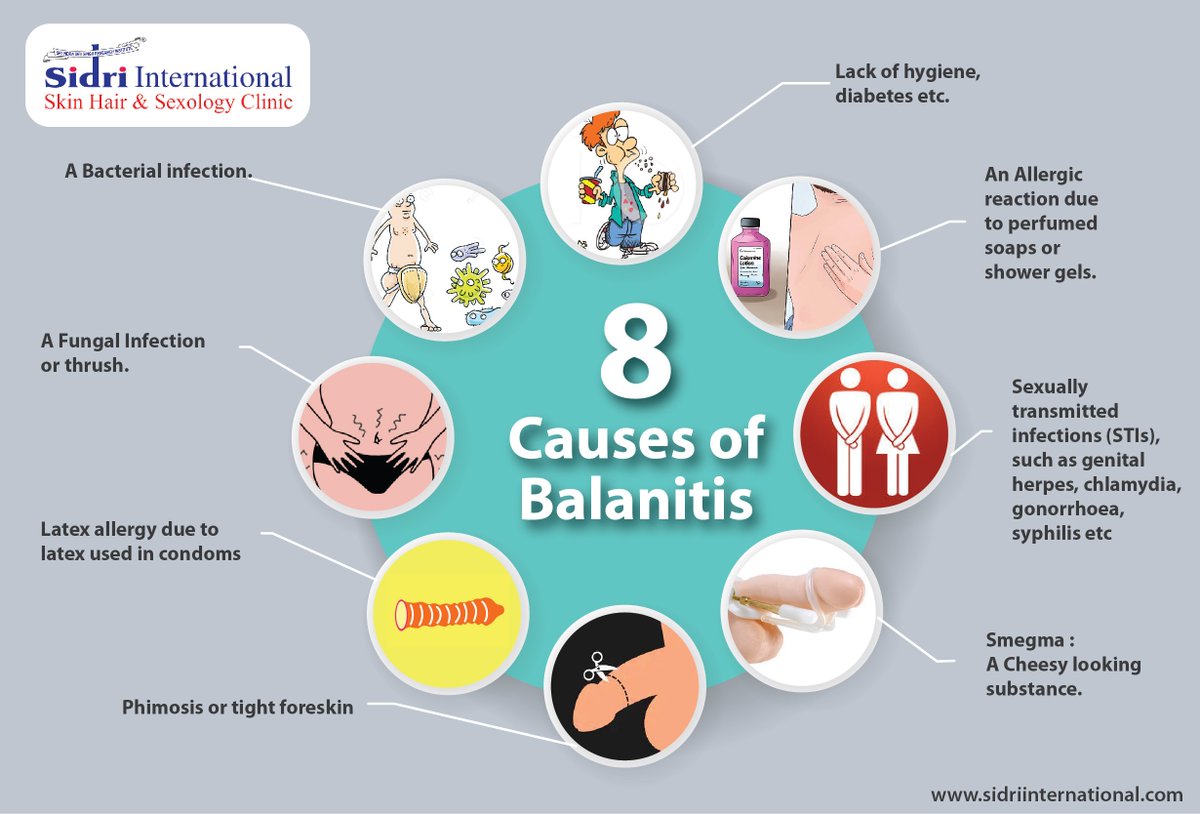 Depending on the severity of clinical manifestations, especially if it is a first-time genital herpes infection, a decision may be made on the need to temporarily stop HB.
Depending on the severity of clinical manifestations, especially if it is a first-time genital herpes infection, a decision may be made on the need to temporarily stop HB.
This requires powerful antiviral and immunomodulatory therapy, which is absolutely incompatible with breastfeeding. At this time, the child must be transferred to artificial mixtures. After the end of the course of treatment, lactation can be resumed, especially if, while taking medications, the young mother regularly expressed herself so that the body would constantly produce milk.
If a recurrence occurs, especially if there are no other symptoms of herpes infection other than the appearance of a rash, topical treatment may be used. In this case, the woman can safely continue breastfeeding. An experienced doctor will select drugs that act only at the site of application and do not penetrate into the systemic circulation.
They can reduce the manifestations of the disease, prevent the further spread of the rash, block the reproduction of the virus in the vesicles and alleviate the clinical manifestations.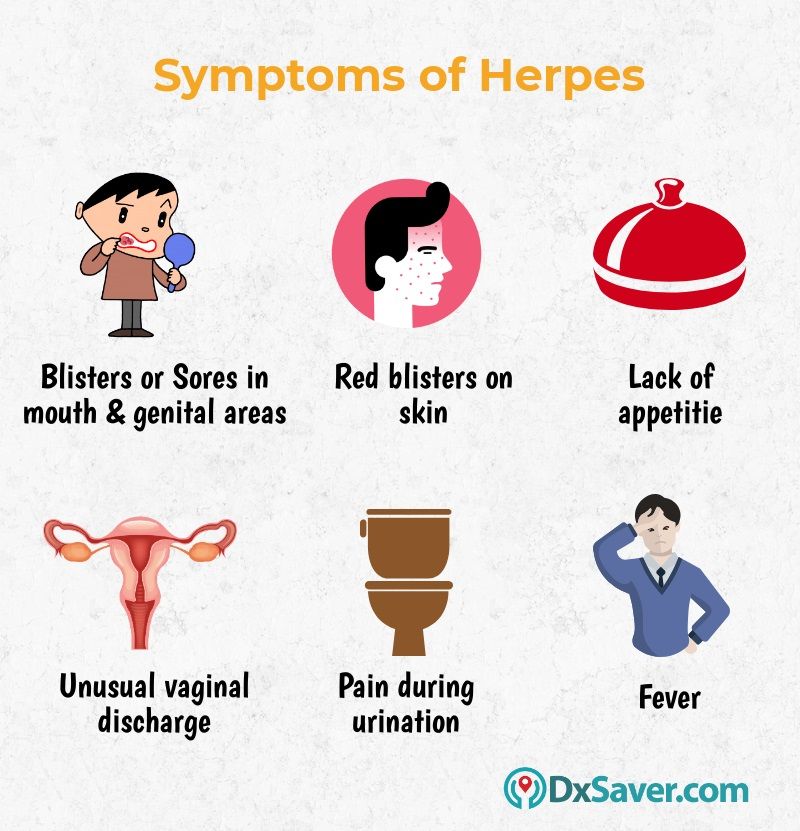 Antiviral ointments or creams will shorten the period of rashes and speed up the recovery of the patient. Breastfeeding women can safely use preparations based on acyclovir, etc. A doctor will help you choose the right one and describe the treatment regimen.
Antiviral ointments or creams will shorten the period of rashes and speed up the recovery of the patient. Breastfeeding women can safely use preparations based on acyclovir, etc. A doctor will help you choose the right one and describe the treatment regimen.
As a general rule, antiviral ointments should be applied to the affected area up to 4-5 times a day. Processing should be done only after hygiene procedures, and it is advisable to apply the product with gloves or a special fingertip. If the manipulation was carried out by hand, then they should be washed well with soap and water.
How to treat genital herpes that remained after childbirth
If genital herpes appears after childbirth, then its treatment is carried out with local drugs: Zovirax, Acyclovir, etc., which lubricate the vaginal wall. These drugs should be used 3 times a day.
In addition, you need to watch your diet, take vitamins and maintain immunity. If the disease is not treated, another genital infection may join it.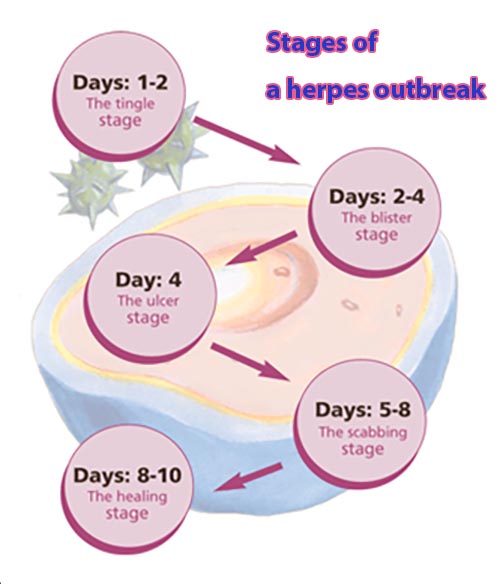 At this time, you need to refrain from sexual intimacy with a partner, as the virus can easily be transmitted to him.
At this time, you need to refrain from sexual intimacy with a partner, as the virus can easily be transmitted to him.
Use and safety Aciclovir for pregnant and lactating women: can it be taken during pregnancy and breastfeeding
Can aciclovir be used during pregnancy to treat herpes and possible risks to the fetus
Aciclovir belongs to a class of antiviral drugs called synthetic nucleoside analogs. It works by stopping the spread of the herpes virus in the body. Used to reduce pain and speed up the healing of sores or blisters in people with chickenpox (chickenpox), shingles, a rash that can occur in people who have had chickenpox in the past, and outbreaks of genital herpes (occasionally causes ulcers around genitals and rectum).
In a study by the Centers for Disease Control and Prevention (CDC), aciclovir was found to cross the placenta, but teratogenicity (birth defects) was not observed, but there is still insufficient data to assess the risk of less common defects or to obtain reliable or final conclusions regarding the safety of this drug during pregnancy.
According to research by the Food and Drug Administration (FDA), it was noted that women taking acyclovir for the treatment of herpes simplex, even during the first trimester of pregnancy, did not demonstrate a risk to the fetus.
The Australian Medicines Administration (AU TGA) has studied a limited number of pregnant women and women of childbearing age who have taken oral acyclovir and found that it did not increase the incidence of malformations or other direct or indirect harmful effects on the mother's fetus. Animal studies have shown an increased incidence of fetal injury, the significance of which in humans is uncertain.
The American College of Obstetricians and Gynecologists (ACOG) recommends taking aciclovir for the treatment of genital herpes, especially recurrent ones, from the 36th week of pregnancy to avoid infection of the newborn baby. But since, as a result of not multiple studies, little information has been provided about it, it is advised to use it with extreme caution, strictly according to the doctor's prescription in the exact minimum dosage indicated as soon as possible.
Information was also provided to ACOG that suppressive therapy in late pregnancy reduces the rate of caesarean section in women with recurrent genital herpes by reducing the rate of relapse during pregnancy, but such treatment may not protect against transmission of the viral infection to the newborn in all cases .
The Centers for Disease Control and Prevention (CDC) in 2015 concluded that this drug can be used to treat herpetic lesions in women at all stages of pregnancy, but under the strict supervision of a doctor, following all his prescriptions for prescribed doses, frequency and duration of administration, as well as in case of the most urgent need and, as a rule, the benefit to the mother should exceed the risk to the fetus.
Breastfeeding use of acyclovir and exposure to infants
Food and Drug Administration (FDA) studies of the use of acyclovir in breastfeeding women found that it passes into breast milk, but even at the most At high maternal doses, the concentration of acyclovir in milk is only about 1% of the typical pediatric dose and is not expected to cause any side effects in breastfed infants. Local application of acyclovir to small areas of the mother's body away from the breast does not pose a risk to the infant.
As a result of maternal herpesvirus infection of the infant during pregnancy, newborns are given aciclovir at doses of 20 to 30 mg/kg IV daily according to the CDC. Dosages obtained in breast milk at high maternal doses are only about 3-5% of this dose. Because the infant receives oral doses of breast milk and aciclovir is only about 20% orally bioavailable, the systemic dose received by the nursing infant is 1% or less of the typical pediatric dose, resulting in no reported adverse reactions in infants.
Several cases of oral aciclovir in breastfeeding mothers have also been reported to the CDC and FDA:
-
The mother of a 4-month-old infant did not notice any side effects in her breastfed infant when she took aciclovir 800 mg orally 5 times a day;
- 90,002 women who were 6 weeks postpartum received acyclovir 300 mg (5 mg/kg) intravenously three times a day for 5 days.