Can i spot while pregnant
Bleeding and spotting from the vagina during pregnancy
Bleeding and spotting from the vagina during pregnancy are common
If you bleed or spot during pregnancy, it doesn’t always mean there’s a problem but in some cases they may be signs of a problem for you or your baby’s health
If you have heavy bleeding, call your health care provider right away
Tell your provider about any bleeding or spotting you have during pregnancy
Bleeding and spotting from the vagina during pregnancy are common. Up to 1 out of 4 (up to 25%) of all pregnant women have some bleeding or spotting during their pregnancy.
Bleeding and spotting in pregnancy don’t always mean there’s a problem, but they can be a sign of miscarriage or other serious complications. Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy.
Call your health care provider if you have any bleeding or spotting, even if it stops. It may not be caused by anything serious, but your provider needs to find out what’s causing it.
What’s the difference between bleeding and spotting?
Bleeding or spotting can happen anytime, from the time you get pregnant to right before you give birth. Spotting is light bleeding. It happens when you have a few drops of blood on your underwear. Spotting is so light that the blood wouldn’t cover a panty liner. Bleeding is when the blood flow is heavier, enough that you need a panty liner or pad to keep the blood from soaking your underwear and clothes.
What should you do if you have bleeding or spotting during pregnancy?
Call your health care provider if you have any kind of bleeding during pregnancy and do these things:
- Keep track of how heavy your bleeding is, if it gets heavier or lighter, and how many pads you are using.
- Check the color of the blood. Your provider may want to know. It can be different colors, like brown, dark or bright red.
- Don’t use a tampon, douche or have sex when you’re bleeding.

Call your health care provider right away at any time during pregnancy or go to the emergency room if you have:
- Heavy bleeding
- Bleeding with pain or cramping
- Dizziness and bleeding
- Pain in your belly or pelvis
What causes bleeding or spotting early in pregnancy?
It’s normal to have some spotting or bleeding early in pregnancy. Bleeding or spotting in the first trimester may not be a problem. It can be caused by:
- Having sex
- An infection
- Implantation. When a fertilized egg (embryo) attaches to the lining of the uterus (womb) and begins to grow.
- Hormone changes. Hormones are chemicals made by the body.
- Changes in your cervix. The cervix is opening to the uterus that sits at the top of the vagina.
- Certain types of testing during pregnancy like an amniocentesis or Chorionic villus sampling (CVS). These are tests that are done to check for genetic abnormalities in your baby.
 Genetic abnormalities are changes in the genes that are passed down to a baby from mom or dad. These genetic changes can cause health problems for a baby.
Genetic abnormalities are changes in the genes that are passed down to a baby from mom or dad. These genetic changes can cause health problems for a baby. - Problems related to smoking. If you smoke, it’s best to stop before pregnancy or as soon as you know you’re pregnant.
Sometimes bleeding or spotting in the first trimester is a sign of a serious problem, like:
- Miscarriage. Almost all women who miscarry have bleeding or spotting before the miscarriage.
- Ectopic pregnancy. This is when a fertilized egg implants itself outside of the uterus and begins to grow. An ectopic pregnancy cannot result in the birth of a baby. It can cause serious, dangerous problems for the pregnant woman.
- Molar pregnancy. This is when a mass of tissue forms inside the womb, instead of a baby. Molar pregnancy is rare.
What causes bleeding or spotting later in pregnancy?
Bleeding or spotting later in pregnancy may be caused by:
- Labor
- Having sex
- An internal exam by your health care provider
- Problems with the cervix, like an infection, growths, inflammation or cervical insufficiency.
 This is when a woman’s cervix opens too early. Inflammation of the cervix is when it may be painful, swollen, red or irritated.
This is when a woman’s cervix opens too early. Inflammation of the cervix is when it may be painful, swollen, red or irritated.
Bleeding or spotting later in pregnancy may be a sign of a serious problem, like:
- Preterm labor. This is labor that happens too early, before 37 weeks of pregnancy.
- Placenta previa. This is when the placenta lies very low in the uterus and covers all or part of the cervix.
- Placenta accreta. This is when the placenta grows into the wall of the uterus too deeply.
- Placental abruption. This is when the placenta separates from the wall of the uterus before birth.
- Uterine rupture. This is when the uterus tears during labor. This happens very rarely. It can happen if you have a scar in the uterus from a prior cesarean birth (also called c-section) or another kind of surgery on the uterus.
 A c-section is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus.
A c-section is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus.
How are bleeding and spotting treated?
Your treatment depends on what caused your bleeding. You may need a medical exam and tests.
Most of the time, treatment for bleeding or spotting is rest. Your provider may also suggest treatments like:
- Take time off from work and stay off your feet for a little while
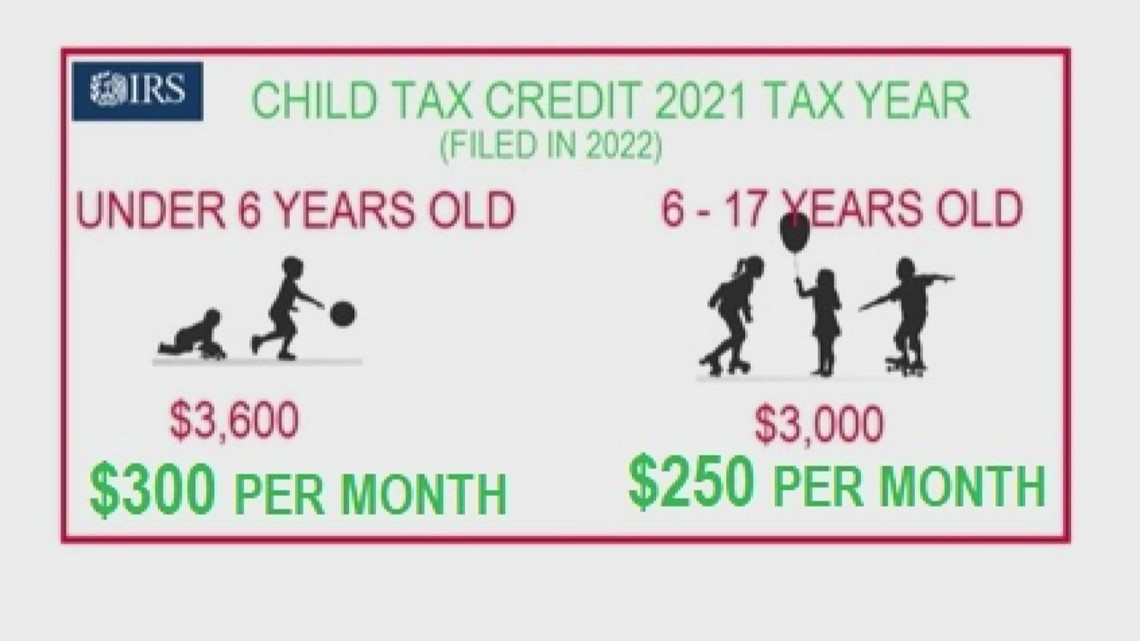
- You may need medicine to help protect your baby from Rh disease. Rh disease is when your blood and baby’s blood are incompatible (can’t be together). This disease can cause serious problems — even death — for your baby.
- Don’t have sex, douche or use tampons
- If you have heavy bleeding, you may need a hospital stay or surgery
Last reviewed April 2020
Spotting During Pregnancy | American Pregnancy Association
Spotting is when you see a light or trace amount of pink, red or dark brown blood. It will be lighter than your menstrual period and there won’t be enough blood to cover a panty line. Spotting during pregnancy isn’t always a sign that something is wrong. It’s actually a common concern that many pregnant women experience during their first 12 weeks of pregnancy. The majority of women who experiencing spotting during pregnancy go on to have a healthy pregnancy and baby.
It will be lighter than your menstrual period and there won’t be enough blood to cover a panty line. Spotting during pregnancy isn’t always a sign that something is wrong. It’s actually a common concern that many pregnant women experience during their first 12 weeks of pregnancy. The majority of women who experiencing spotting during pregnancy go on to have a healthy pregnancy and baby.
Spotting During Pregnancy Versus Bleeding
Vaginal bleeding during pregnancy is any discharge of blood from the vagina. It can happen anytime from conception (when the egg is fertilized) to the end of pregnancy.
Light bleeding, or spotting, during pregnancy is common, especially during the first trimester. It is considered spotting when you notice a few drops of blood occasionally in your underwear, or if you wipe yourself with tissue and see a little blood on the paper. There should not be enough blood to fill a panty liner.
Bleeding is a heavier flow of blood. With bleeding, you will need a liner or pad to keep the blood from soaking your clothes. Whether you are bleeding or spotting, it is best to contact your healthcare provider and describe what you are experiencing.
Whether you are bleeding or spotting, it is best to contact your healthcare provider and describe what you are experiencing.
What Causes Spotting During Pregnancy?
Implantation bleeding is a common cause of spotting early on in pregnancy. Implantation bleeding happens when the fertilized egg attaches to the uterine lining. This can trigger a few days of light bleeding or spotting. This spotting occurs before a woman even knows she is pregnant and is often mistaken as a pending period. Bleeding that occurs after the day a woman expects her period is typically too late to be considered implantation bleeding, and is more likely related to early pregnancy in general.
Another common cause of spotting is a cervical polyp (a harmless growth on the cervix), which is more likely to bleed during pregnancy due to higher estrogen levels. This may occur because there is an increased number of blood vessels in the tissue around the cervix during pregnancy. As a result, contact with this area (through sexual intercourse or a gynecological exam, for example) can cause bleeding.
Even without the presence of a cervical polyp, there are a few things that may cause some spotting in the couple days after:
- Sexual intercourse
- Gynecological exam, such as a vaginal ultrasound
- Heavy lifting/excessive exercise
When to Worry About Spotting During Pregnancy?
Spotting or bleeding during pregnancy is not expected and may be abnormal, but it is not always a cause for concern. However, it is important to contact your healthcare provider to discuss the symptoms you are experiencing. The good news is that 50% of women with bleeding during pregnancy go on to have a healthy pregnancy and a healthy baby.
Any spotting or bleeding in the second or third trimesters should be reported to your healthcare provider immediately. In the first trimester, spotting is somewhat more common, but should also be reported to your doctor or midwife.
Call your obstetrician especially if you notice heavy bleeding similar to a menstrual period to make sure the bleeding is not a result of pregnancy complications, such as an ectopic pregnancy. Abnormal bleeding in late pregnancy may be more serious because it can signal a complication with you or your baby. Call your doctor as soon as possible if you experience any bleeding in your second or third trimester. Your healthcare provider will most likely check for cervical polyps, and make sure your cervix is closed.
Abnormal bleeding in late pregnancy may be more serious because it can signal a complication with you or your baby. Call your doctor as soon as possible if you experience any bleeding in your second or third trimester. Your healthcare provider will most likely check for cervical polyps, and make sure your cervix is closed.
To help manage your spotting during pregnancy and to increase the probability of continuing with a healthy pregnancy, your healthcare provider may encourage you to do the following:
- Bed rest or more naps
- More time off your feet
- Staying well hydrated
- Limit your physical activity
- Elevate your feet when possible
- Avoid lifting items over 10 pounds
Remember, the good news is the majority of women who experience spotting during pregnancy go on to have a healthy pregnancy. However, do not let this fact keep you from contacting your healthcare provider. It is important to discuss spotting and bleeding with your doctor.
Want to Know More?
- Sharp Pain During Pregnancy
- 7 Common Discomforts of Pregnancy
- Warning Signs of Miscarriage
Compiled using information from the following sources:
1. Mayo Clinic Guide to a Healthy Pregnancy, New York, NY: HarperCollins Publishers Inc.
2. Obstetrics and Gynecology: The Essentials of Clinical Care. New York, NY: Thieme New York
3. Danforth’s Obstetrics and Gynecology, Ninth Ed. Scott, James et al., Ch. 17
4. Williams Obstetrics, Twenty-Second Ed. Cunningham, F. Gary et al., Ch. 51
advice from a genetics doctor - Amurskaya Pravda
An early visit to the doctor will help to avoid the birth of a sick baby
Health "Pregnancy comes like a war - in the morning and unexpectedly." This is exactly what Annunciation obstetricians have been saying lately about a significant part of their pregnant patients. According to doctors, pregnancy should be planned, and an early visit to the doctor will help to avoid some fetal diseases. Vladimir Samokhvalov, Director of the Center for Family Health and Reproduction, told the Presidential Administration why it is important to do an ultrasound scan in each trimester of pregnancy and what will reveal an ultrasound examination.
According to doctors, pregnancy should be planned, and an early visit to the doctor will help to avoid some fetal diseases. Vladimir Samokhvalov, Director of the Center for Family Health and Reproduction, told the Presidential Administration why it is important to do an ultrasound scan in each trimester of pregnancy and what will reveal an ultrasound examination.
The first ultrasound is the most important
Prenatal diagnosis is the determination of the condition of the fetus in the womb. In modern medicine, there are methods that can make a diagnosis for the fetus and determine the health status of the unborn child. The most common is ultrasound diagnostics. A pregnant woman must undergo it at least three times: from the 12th to the 14th week, in the 20th and 30th weeks. Ultrasound in the first trimester is very important, because it is during this period that gross fetal malformations can be detected: the absence of limbs, anencephaly, a two-chambered heart, etc.
If a pregnant woman is over 35 years old and she is registered after 14 weeks of pregnancy, then it is impossible to perform an objective examination of the fetus for chromosomal diseases. Therefore, a prerequisite for diagnosing these diseases is a puncture and sampling from the placenta.
“During this period, early prenatal screening is done, or it is also called combined screening,” said Vladimir Samokhvalov. - During an ultrasound examination, special measurements are taken for possible chromosomal abnormalities, one of which is Down's disease. At the same time, blood is taken for biochemical markers of fetal pathology. In addition to the ultrasound result and the level of biochemical markers, a lot of data is entered into the memory of special equipment: nationality, age, diseases, bad habits, such as smoking. The analyzer compares the information and gives a percentage of the risk of having a baby with chromosomal diseases. It is important to remember: based on the results of screening, they do not make a diagnosis, but only calculate the possibility of having a child with a chromosomal pathology.
Prenatal ultrasound screening is carried out by a doctor-expert of the Fetal Medicine Foundation, who has a special certificate - a conclusion on permission to work in this field. The specialist passes the exams in London online, after the positive results of which he is assigned an identification number. It is needed for the operation of the analyzer, which, without the registration number of the doctor's certificate, will not diagnose fetal pathology. There are such certified specialists in Blagoveshchensk, Belogorsk, Tynda, Zeya and Svobodny.
If the calculation on the analyzer shows a high risk of fetal chromosomal pathology, the woman is prescribed additional research methods - prenatal karyotyping. This is a puncture and collection of fetal cells from the placenta under ultrasound control and a cytogenetic study to exclude such serious diseases as Down syndrome, Patau, Klinefelter, etc. Last year, thanks to this method, the birth of 20 children with Down's disease was prevented. It is important to conduct such a study before 14 weeks: chromosomal disorders are sensitive to biochemistry and ultrasound only during this period of pregnancy.
It is important to conduct such a study before 14 weeks: chromosomal disorders are sensitive to biochemistry and ultrasound only during this period of pregnancy.
According to doctors, Down's disease is not an anomaly for the Amur Region. The main reason is fresh mutations in the sex cells of the spouses. The older the woman, the higher the probability of giving birth to a child with Down syndrome: for a woman at the age of 25, it is 1:1040, and for a fifty-year-old - 1:5.
We exclude fetal defects in the second trimester of pregnancy
The main task of second trimester ultrasound is to exclude fetal malformation. It is at this stage that congenital heart defects and tumors of internal organs and the skeletal system are already visible. Every week, when examining pregnant women in the area in the perinatal center, at least one case of congenital fetal pathology is detected.
Among diagnosed congenital malformations, heart defects are the most common. To determine the tactics of pregnancy management and the prognosis of the health of the unborn child, a woman is consulted by specialized specialists - surgeons, cardiac surgeons, neurosurgeons. Spouses are informed about the condition of the fetus and a decision is made on the advisability of bearing a child. With a positive decision on gestation, the institution in which the woman will give birth and the surgical tactics for treating the fetus are determined. In cases requiring very complex surgical interventions, the pregnant woman is sent for delivery to central clinics, where surgical treatment will be performed on the child immediately after birth. If the malformation is incompatible with life or leads to severe disability, by decision of the council, the pregnant woman is recommended to terminate the pregnancy. But the final decision on carrying a pregnancy remains with the spouses.
To determine the tactics of pregnancy management and the prognosis of the health of the unborn child, a woman is consulted by specialized specialists - surgeons, cardiac surgeons, neurosurgeons. Spouses are informed about the condition of the fetus and a decision is made on the advisability of bearing a child. With a positive decision on gestation, the institution in which the woman will give birth and the surgical tactics for treating the fetus are determined. In cases requiring very complex surgical interventions, the pregnant woman is sent for delivery to central clinics, where surgical treatment will be performed on the child immediately after birth. If the malformation is incompatible with life or leads to severe disability, by decision of the council, the pregnant woman is recommended to terminate the pregnancy. But the final decision on carrying a pregnancy remains with the spouses.
For 9 months at the Center for Family Health and Reproduction of the Amur Regional Clinical Hospital, 47 congenital malformations and 16 fetal chromosomal diseases were diagnosed in utero.
Vladimir Aleksandrovich cites a recent clinical case: a congenital defect of the aorta was found in the fetus, and in order for the child to live fully, its prosthesis is necessary. The operation is possible only in large specialized centers of the country. The tragedy is that this born person is doomed to lifelong surgical procedures. With age, the prosthesis will need to be changed due to the growth of the child and take drugs for the whole life to prevent thrombosis.
Third ultrasound - getting ready for childbirth
In the last trimester, an ultrasound examination assesses the growth rate of the child and its proportions, assesses the amount of amniotic fluid and the condition of the placenta, and excludes malformations that are manifested by a violation of the anatomical structure of individual organs and systems of the fetus. Also, the doctor of ultrasound diagnostics determines how ready the woman's organs are for childbirth and how the fetus is located.
It is possible to determine the disease of a child by the blood of the mother
More recently, in Moscow, commercial medical centers have a new opportunity to determine the genetic information about a child using fetal DNA. During pregnancy, a small amount of the baby's DNA circulates in the mother's bloodstream, and with the help of modern technology, they can be "caught" and a number of severe fetal chromosomal diseases can be determined - by the mother's blood.
IMPORTANT!
One of the main conditions for the birth of a healthy child is registration in the antenatal clinic before 12 weeks of pregnancy!
Age category of materials: 18+
Materials on topic
“I didn’t even have time to get confused”: a student of the medical academy, working on an ambulance, took birth at the Annunciation woman At Epiphany, ambulance doctors took birth at the Annunciation woman Two 49-year-old Amur women became the oldest mothers in the region in 2020 In Blagoveshchensk, an anesthesiologist took money from a woman in labor for a free procedure A mother with a newborn child was found dead in Zeya 09/20/2018, 17:46 Young mother and grandmother: Amur women are not afraid to give birth after forty In the Amur region, almost a third of women became pregnant after IVF Dad can: heroic husbands remembered how their spouses survived the pregnancy| Vladimir Samokhvalov, Director of the Center for Family Health and Reproduction, geneticist |
Screening tests for Down syndrome in the first 24 weeks of pregnancy
Relevance
Down syndrome (also known as Down syndrome or Trisomy 21) is an incurable genetic disorder that causes significant physical and mental health problems and disability. However, there is great variation in how Trisomy Down affects people. Some individuals have severe suffering, while others have little problems and are able to lead relatively normal lives. There is no way to predict how badly each child may be affected.
However, there is great variation in how Trisomy Down affects people. Some individuals have severe suffering, while others have little problems and are able to lead relatively normal lives. There is no way to predict how badly each child may be affected.
Parents-to-be are given the option of taking a Down test during pregnancy to help them make decisions. If a pregnant woman is carrying a child with Down syndrome, then a decision must be made whether to terminate or continue the pregnancy. This information offers parents the opportunity to plan for life with a Down child.
The most accurate tests to detect Down include testing of amniotic fluid (fluid around the fetus, amniocentesis required) or placental tissue (chorionic villus biopsy (CVS)) for abnormal chromosomes associated with Down. Both tests require the insertion of a needle into the mother's abdomen and increase the risk of miscarriage. Thus, the tests are not suitable to be given to all pregnant women. Instead, screening uses tests that measure markers in the mother's blood, urine, or baby's ultrasound. These screening tests are not perfect, they can miss cases of Down and also give a "high risk" result to some women whose children do not have Down. Thus, pregnancies identified as Down's "high risk" pregnancies using these screening tests require further testing by amniocentesis or CVS to confirm a Down's diagnosis.
These screening tests are not perfect, they can miss cases of Down and also give a "high risk" result to some women whose children do not have Down. Thus, pregnancies identified as Down's "high risk" pregnancies using these screening tests require further testing by amniocentesis or CVS to confirm a Down's diagnosis.
What we did
The aim of this review was to find out which of the screening tests done during the first 24 weeks of pregnancy are most accurate in predicting the risk of Down pregnancy. We studied 7 different urinary markers that can be used alone, in ratios, or in combination taken up to 24 weeks of gestation. This cumulatively creates 24 screening tests for Down. We found 19 studies involving 18,013 pregnant women, of which 527 were pregnancies with Down syndrome.
What we found
Evidence does not support the use of urine tests to screen for Down syndrome during the first 24 weeks of pregnancy. The amount of evidence is limited.