C arm radiation exposure and pregnancy
Pregnant operating room staff
Category: Pregnancy and Radiation — Radiation workers/medical technicians
The following question was answered by an expert in the appropriate field:
Q
I work in the operating room and I am exposed to fluoroscopy daily. I am currently five weeks pregnant. Even though I am very cautious and I always wear a lead apron, I am very nervous about the risks to my unborn child. In order for me to do my job correctly, it is essential that I be in the room when the c-arm is being used. Is the lead apron enough? Am I putting my unborn child in danger? What are the risks?
A
The lead apron will protect your unborn child from virtually all of the c-arm radiation exposure so there is no need for extra concern.
Lead aprons are made to attenuate the x-ray beam at least 95 to 98%—meaning that, at most, only 2 to 5% of the x rays could even get through the apron. Most aprons are even better than that.
There are some extra things you can consider doing if they are possible and you are still concerned. If you can put more distance between yourself and where the x rays are entering the patient's body, you can reduce your exposure substantially—even if you can only move another 30 to 60 centimeters (cm) away. Another item is to see if you could get a radiation badge (dosimeter) from your hospital's radiation safety office. If you can, you could wear it under the lead apron for a period of time and then let the radiation safety office determine what the radiation reading is. The regulatory limit for the fetus of an occupationally exposed radiation worker is 5 millisieverts (mSv) during the gestation period (mSv is a unit of effective radiation dose).
We have nearly 2,000 badged staff where I work and do give an extra radiation badge to pregnant workers to wear under their apron. None of the badges worn under the apron at the abdominal level have ever had a radiation reading on them—the lead apron protected the abdomen.
Kelly Classic
Certified Medical Health Physicist
Ask the Experts is posting answers using only SI (the International System of Units) in accordance with international practice. To convert these to traditional units we have prepared a conversion table. You can also view a diagram to help put the radiation information presented in this question and answer in perspective. Explanations of radiation terms can be found here.
To convert these to traditional units we have prepared a conversion table. You can also view a diagram to help put the radiation information presented in this question and answer in perspective. Explanations of radiation terms can be found here.
Answer posted on 8 February 2017. The information posted on this web page is intended as general reference information only. Specific facts and circumstances may affect the applicability of concepts, materials, and information described herein. The information provided is not a substitute for professional advice and should not be relied upon in the absence of such professional advice. To the best of our knowledge, answers are correct at the time they are posted. Be advised that over time, requirements could change, new data could be made available, and Internet links could change, affecting the correctness of the answers. Answers are the professional opinions of the expert responding to each question; they do not necessarily represent the position of the Health Physics Society.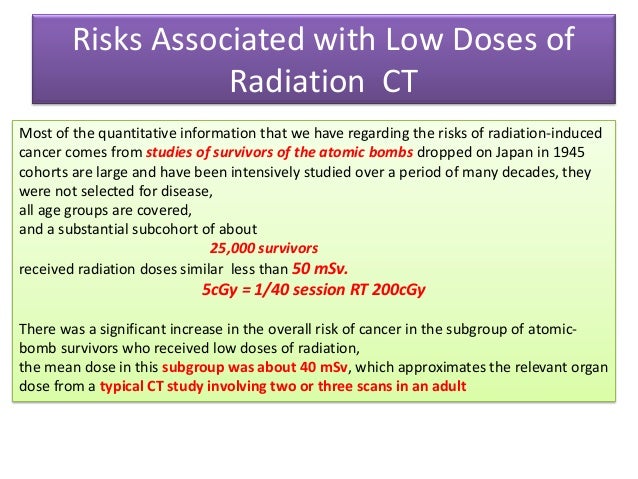
Radiation Exposure In Pregnancy - StatPearls
Ilsup Yoon; Todd L. Slesinger.
Author Information
Last Update: May 8, 2022.
Introduction
Choosing the most appropriate imaging modality for pregnancy patients is a common clinical question encountered daily. The general principle for imaging during pregnancy is similar to imaging for the general population, with the goal of radiation exposure being as low as reasonably achievable (ALARA). What is unique during pregnancy is that fetus radiation exposure is an essential factor in deciding optimal imaging studies. Understanding of consequences of radiation exposure on a fetus, degrees of fetal radiation exposure by each imaging modality, and techniques on reducing fetal radiation exposure is vital in choosing the best diagnostic imaging modality. While it is crucial to minimize fetal radiation exposure as much as possible, it is essential to remember that diagnostic studies should not be avoided for fear of radiation exposure, especially when these studies can dramatically change patient management. This activity will discuss the consequences of radiation exposure on a fetus, degrees of radiation exposure by each modality, and techniques of reducing fetal radiation exposure. Solid understanding of how each imaging modality contributes to fetal radiation dose will significantly help in choosing the most appropriate imaging study that provides the best diagnostic information at the lowest level of radiation exposure.
This activity will discuss the consequences of radiation exposure on a fetus, degrees of radiation exposure by each modality, and techniques of reducing fetal radiation exposure. Solid understanding of how each imaging modality contributes to fetal radiation dose will significantly help in choosing the most appropriate imaging study that provides the best diagnostic information at the lowest level of radiation exposure.
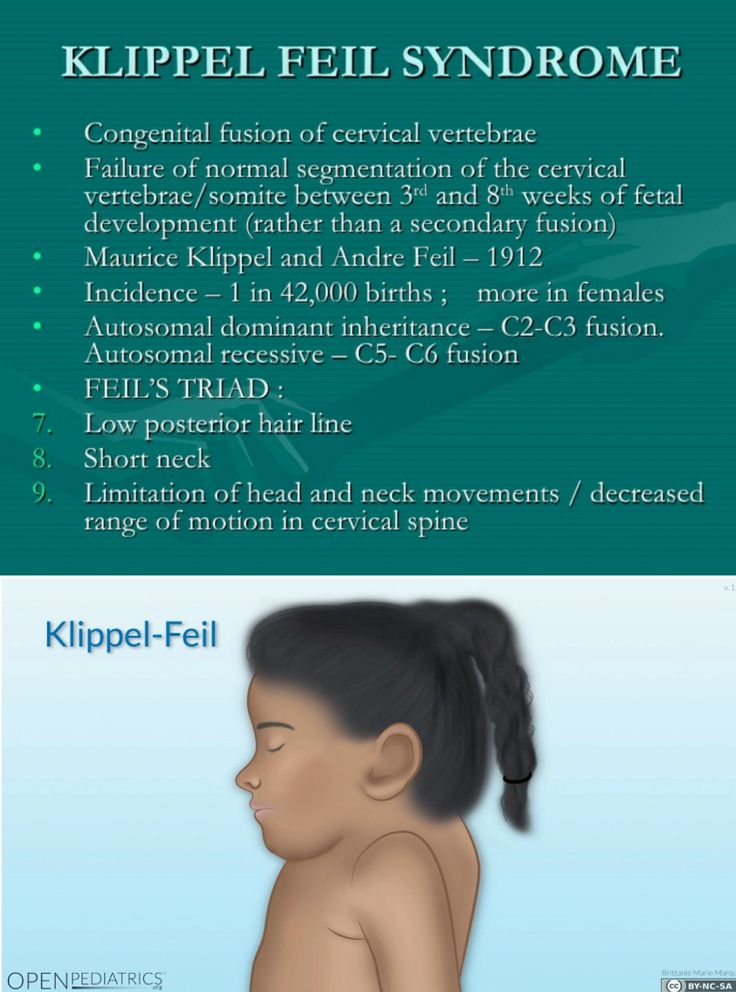
The consequence of radiation exposure in fetuses is mostly based on observations rather than based on scientific research. Ethical issues prohibit researching on the fetus. Therefore, most of the data on the impact of radiation on the fetus derives from observations of patients who suffered Japan’s Hiroshima bombing and the Chernobyl nuclear power plant disaster.[1][2] Based on the observations made from the victims of the high level of radiation exposure, the consequences of radiation exposure can categorize into four broad groups, including pregnancy loss, malformation, developmental delay or retardation, and carcinogenesis. [1] Pregnancy loss most often happens when radiation exposure happens during early gestation (less than two weeks).[2] Malformations of body parts and developmental delays occur during the organogenesis period (2 weeks to 8 weeks) and are dependent on the radiation dose.[2] Below the threshold level of radiation exposure, there is minimal disruption of organogenesis. Above the threshold, the degree of malformation is related to the dose of the radiation. Lastly, carcinogenesis is considered a stochastic effect. In other words, cancer can develop at any level of radiation exposure. However, the probability of developing cancer increases with the increase in the dose of radiation.
[1] Pregnancy loss most often happens when radiation exposure happens during early gestation (less than two weeks).[2] Malformations of body parts and developmental delays occur during the organogenesis period (2 weeks to 8 weeks) and are dependent on the radiation dose.[2] Below the threshold level of radiation exposure, there is minimal disruption of organogenesis. Above the threshold, the degree of malformation is related to the dose of the radiation. Lastly, carcinogenesis is considered a stochastic effect. In other words, cancer can develop at any level of radiation exposure. However, the probability of developing cancer increases with the increase in the dose of radiation.
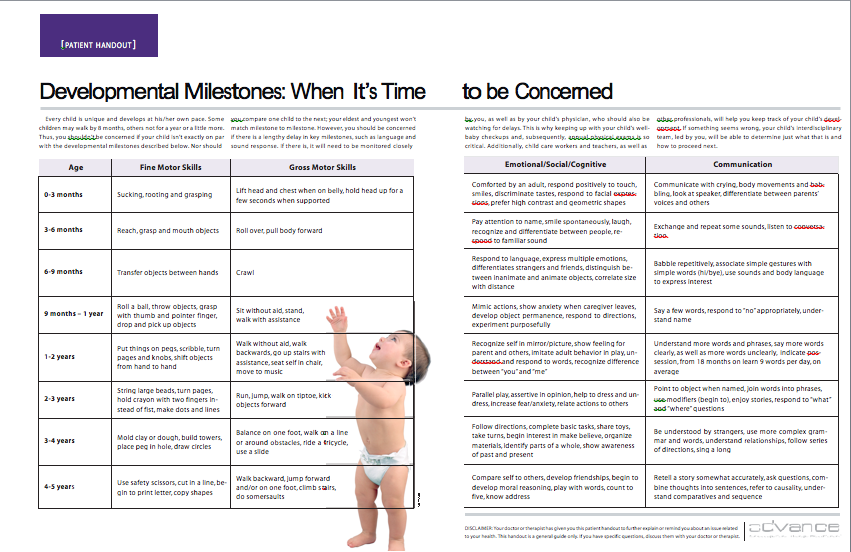
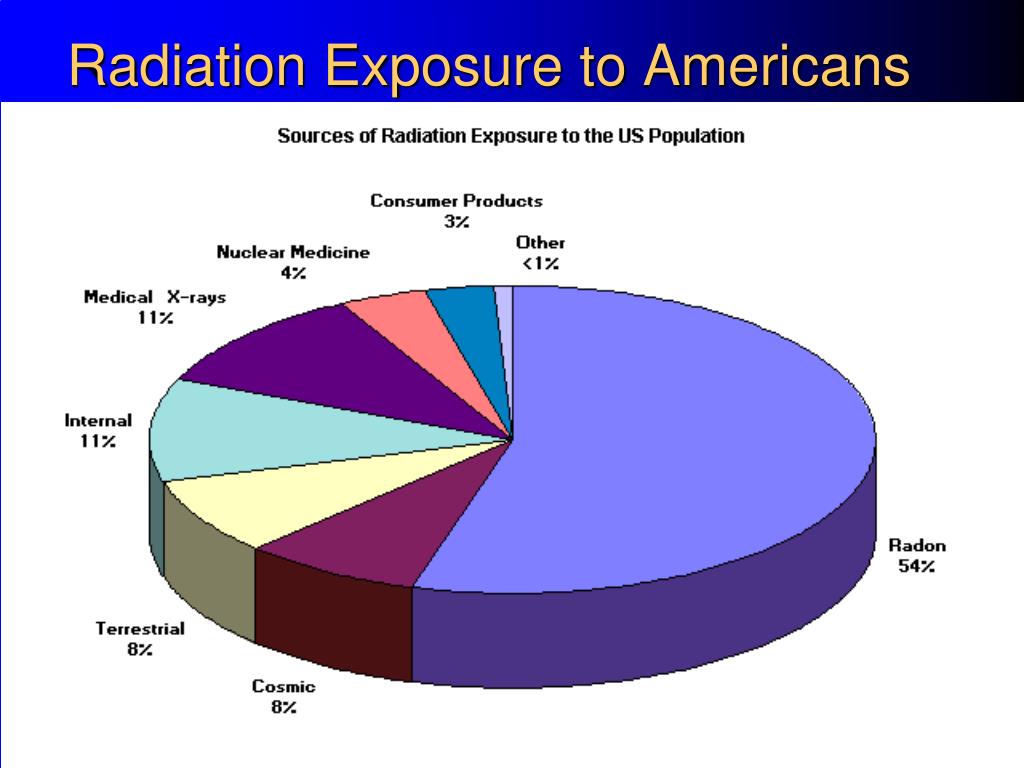
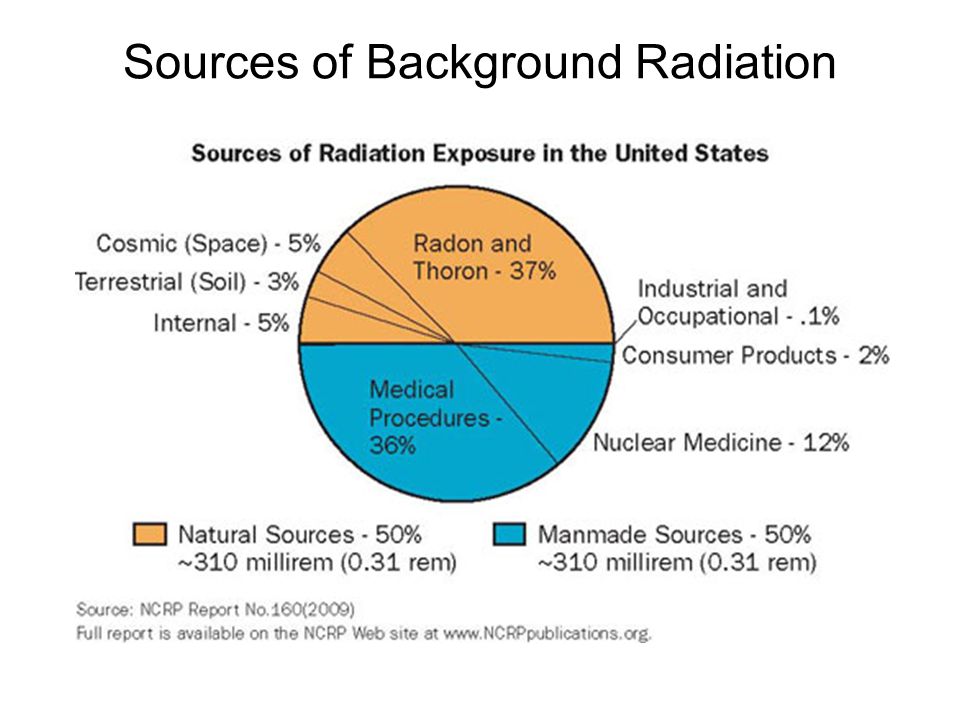
In the United States, the background radiation exposure for the whole body per year is estimated to be 3.1 mSv (310 mrem). United States Nuclear Regulation Commission (USNRC) also recommends total fetus exposure during pregnancy to be less than 5.0 mSv (500 mrem). The fetus radiation dose below 50 mGy is considered safe and not cause any harm.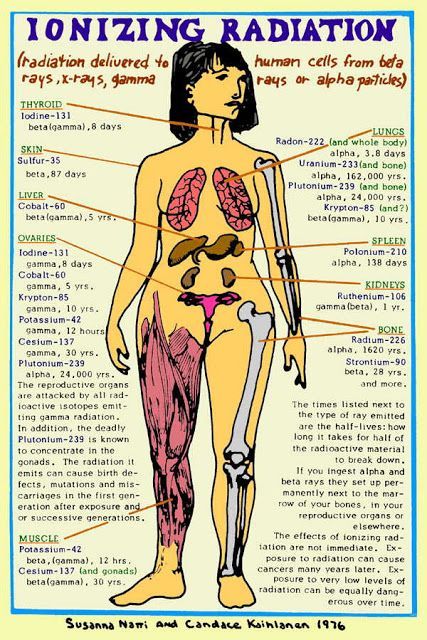 According to the Center for Disease Control (CDC), radiation dose between 50 mGy to 100 mGy is regarded inconclusive in terms of impact on the fetus. Doses above 100 mGy, especially doses above 150 mGy, are viewed as the minimum amount of dosage at which negative fetal consequences will occur, based on observation. The majority of the diagnostic studies performed during the pregnancy are below the threshold level.
According to the Center for Disease Control (CDC), radiation dose between 50 mGy to 100 mGy is regarded inconclusive in terms of impact on the fetus. Doses above 100 mGy, especially doses above 150 mGy, are viewed as the minimum amount of dosage at which negative fetal consequences will occur, based on observation. The majority of the diagnostic studies performed during the pregnancy are below the threshold level.
The effect of radiation exposure during pregnancy also depends on the gestational age of the fetus. The embryo/fetus is most susceptible to radiation during organogenesis (2 to 7 weeks gestational age) and in the first trimester. The fetus is more resistant to the radiation during the second and third trimester. Dose between 0.05 to 0.5 Gy is generally considered safe for the fetus during the second and third trimester while it is considered potentially harmful during the 1st-trimester fetus. Even though the fetus is more resistant to the radiation during the second and third trimester, a high dose of radiation (greater than 0.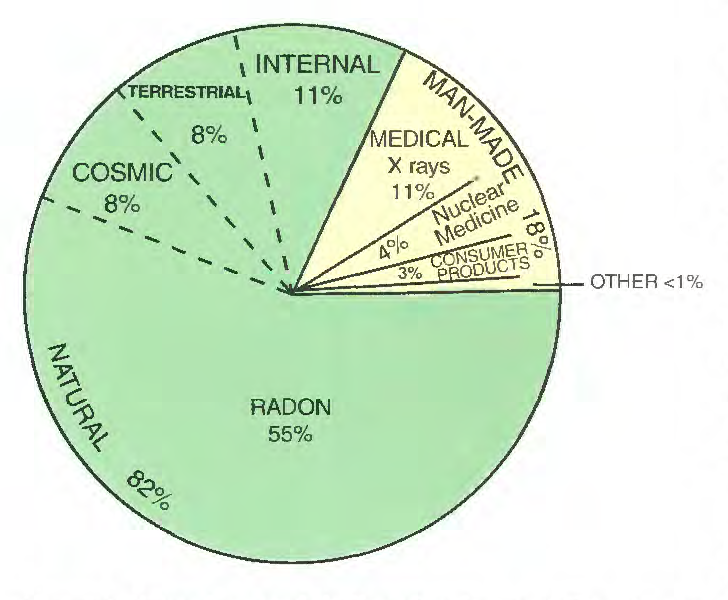 5 Gy or 50 rad) may result in adverse effects including miscarriage, growth reduction, IQ reduction, and severe mental retardation. Therefore, clinicians and radiologists should counsel the pregnant patient regardless of the gestational age.[3]
5 Gy or 50 rad) may result in adverse effects including miscarriage, growth reduction, IQ reduction, and severe mental retardation. Therefore, clinicians and radiologists should counsel the pregnant patient regardless of the gestational age.[3]
Occupational radiation exposure for a pregnant employee should be monitored to make sure the total amount of radiation exposure is under the regulatory limit. According to the National Council of Radiation Protection and Measurement (NCRP), the total dose equivalent to the embryo/fetus should not exceed 500 mRem during the length of the pregnancy. It should not exceed 50mRem in any month during pregnancy.[4]
The practice decision on selecting the most appropriate imaging modality for pregnancy should have their basis in the expert opinions of the treating clinician. Nonetheless, the American College of Radiology does provide recommendations on the appropriateness of imaging modalities in accessing common clinical conditions. Each imaging modality is categories into usually appropriate, may be appropriate, and usually not appropriate. For instance, for a pregnant patient presenting with right lower abdominal pain concerning for appendicitis, ultrasound and MRI are usually appropriate imaging modality. CT abdomen and pelvis with or without contrast is categorized as may be appropriate. Abdominal radiograph, Tc-99m WBC scan, and fluoroscopy contrast enema are considered usually not appropriate. The American College of Radiology appropriateness criteria provides the current practice policies and guidelines in the US regarding imaging in pregnant patients.
For instance, for a pregnant patient presenting with right lower abdominal pain concerning for appendicitis, ultrasound and MRI are usually appropriate imaging modality. CT abdomen and pelvis with or without contrast is categorized as may be appropriate. Abdominal radiograph, Tc-99m WBC scan, and fluoroscopy contrast enema are considered usually not appropriate. The American College of Radiology appropriateness criteria provides the current practice policies and guidelines in the US regarding imaging in pregnant patients.
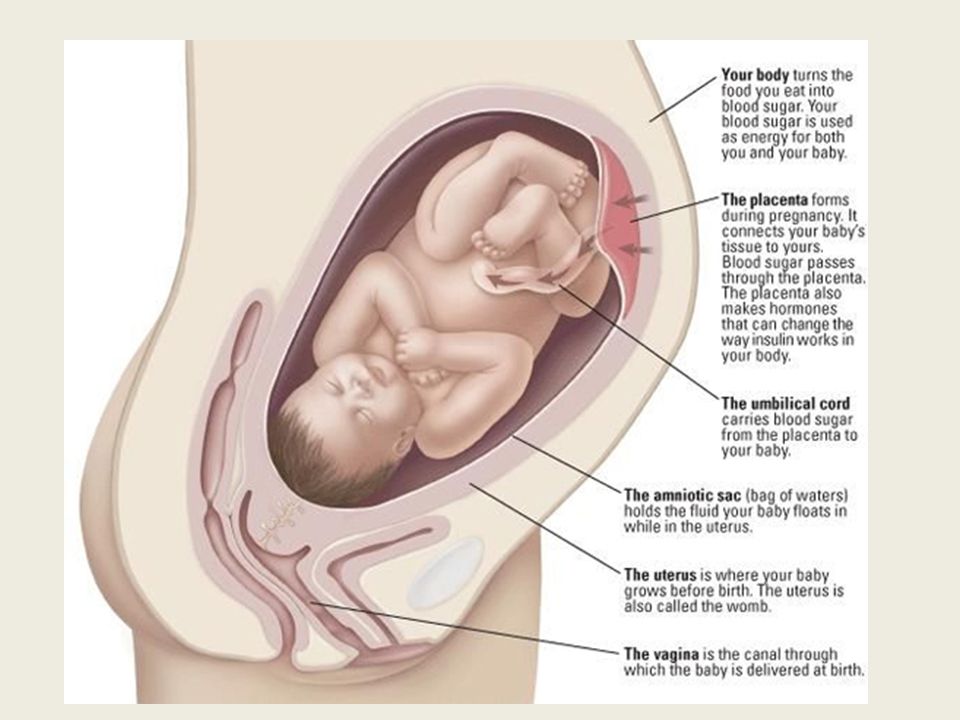
Anatomy
Understanding the anatomic location of the uterus is essential in understanding why a particular type of study contributes to a higher radiation dose. The uterus is located within the female pelvis. Therefore, studies that are further away from the pelvis contribute to less radiation dose than the studies that aim at the pelvis. Additionally, the uterus is located superior and anterior aspect of the pelvis during the pregnancy. X-ray beams that project in a posterior to anterior (PA) direction contribute to less radiation than the beam projected in anterior to posterior (AP) direction because, in PA projection, the X-ray gets attenuated before reaching anteriorly located uterus.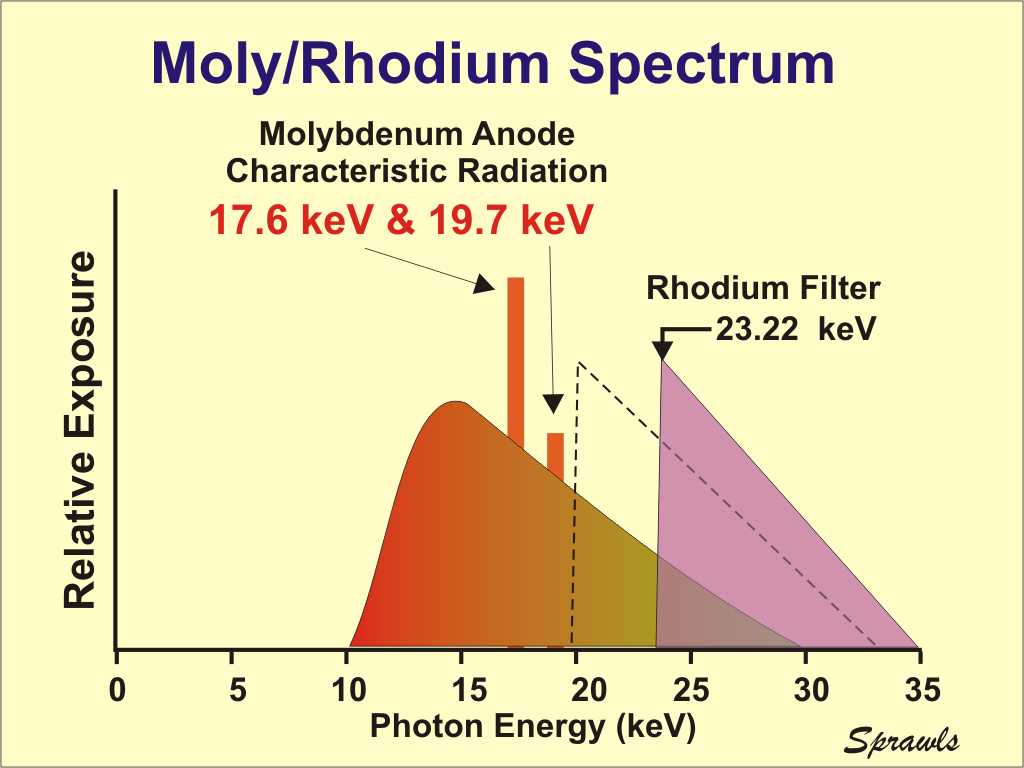
Plain Films
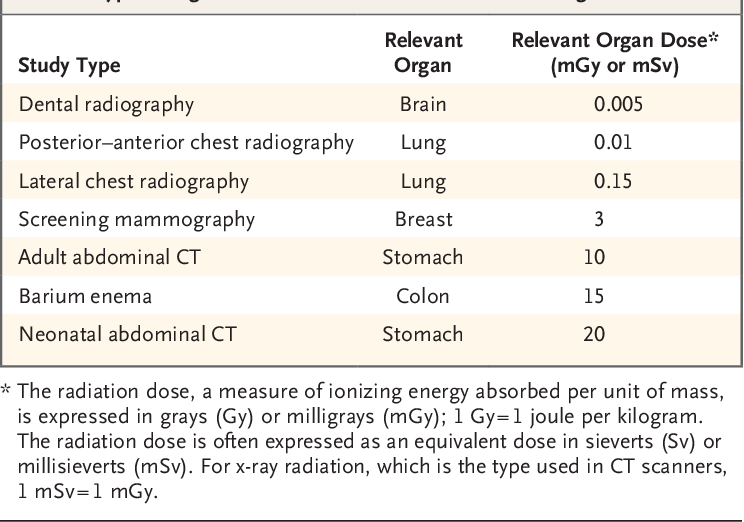
A single plain radiograph does not contribute to a significant radiation dose to the fetus. The estimated radiation dose to the fetus varies and ranges from 0.001 mGy to 10 mGy depending on the type of the study.[5] The highest radiation dose is the lumbar spine radiograph, which has a maximal fetal radiation dose of 10 mGy.[5] Nonetheless, even fetus radiation exposure for the lumbar spine radiograph is significantly lower than the threshold limit of the safe radiation exposure dose of 50 mGy, radiation level that is considered safe and without significant harm.
Regardless of the radiation dose, it is vital to reduce radiation exposure to the fetus as much as possible. Plain films are obtained more frequently than computed tomography (CT), and radiation doses from multiple plains films can easily accumulate. Therefore, it is essential to employee dose reducing techniques as often as possible. When performing plain film examination of non-pelvis structure, pelvic lead apron should always be utilized to reduced unnecessary fetus radiation.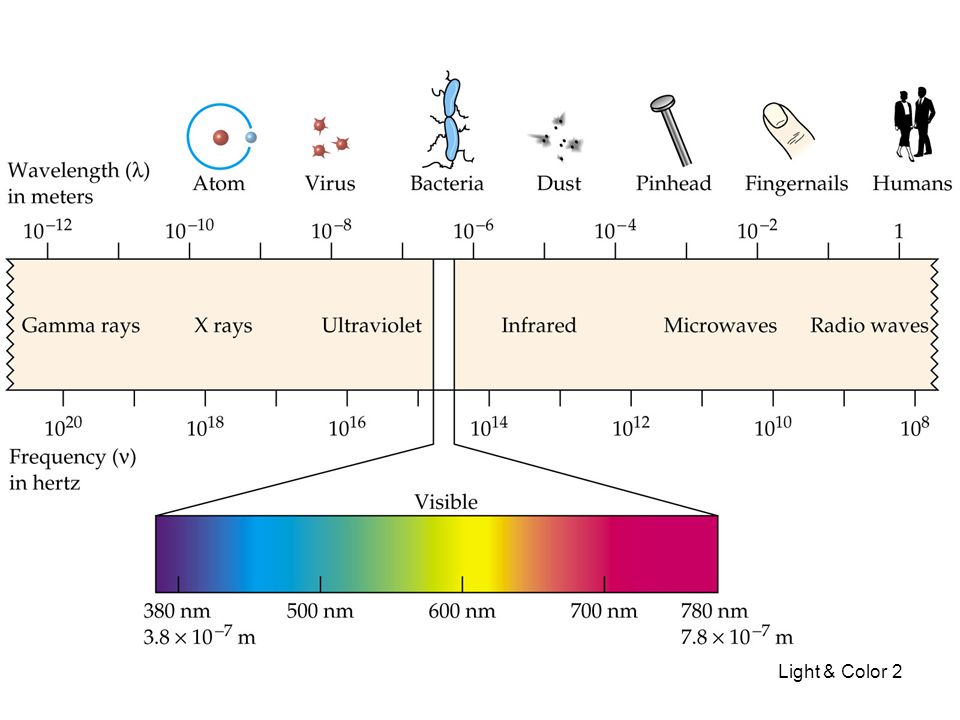 PA projection of the pelvis also contributes to the lower dose than the AP projection. Technologists should optimally position patients before taking a radiograph to reduce the number of repeat examinations from unsatisfactory views. Lastly, clinicians should obtain radiographs only when it is helping clinical management.
PA projection of the pelvis also contributes to the lower dose than the AP projection. Technologists should optimally position patients before taking a radiograph to reduce the number of repeat examinations from unsatisfactory views. Lastly, clinicians should obtain radiographs only when it is helping clinical management.
Computed Tomography
On the other hand, CT contributes to a significant amount of fetal radiation. The amount of fetus radiation exposure again varies by the type of study with CT pelvis contributing the highest amount of fetal radiation of 50 mGy.[5] This dose is right at the limit above which there is a documented negative impact to the fetus.
Because CT contributes to much higher fetal radiation, it is essential always to be considerate of other options when contemplating utilizing CT on pregnancy patients. Other imaging modalities, including MRI, plain radiograph, ultrasound, and nuclear medicine studies, should be considered first before performing CT.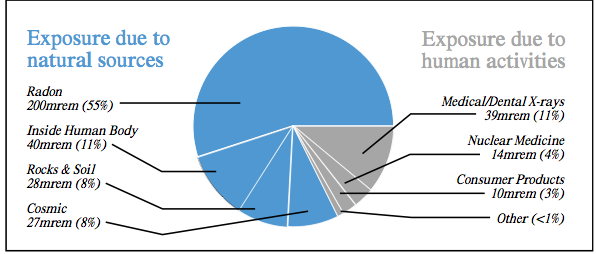 Common clinical presentations like appendicitis first require evaluation with MRI instead of CT.[6] Right upper quadrant ultrasound should be utilized if there is a clinical concern for cholecystitis.[7] Renal ultrasound should merit consideration before CT for nephrolithiasis and collecting system obstruction. If CT is the first indicate study of choice as in traumatic pregnancy patients to evaluate for intra-abdominal trauma, it is crucial to optimize CT setting to minimize the dose. Using wide pitch and narrow collimation can reduce the radiation dose. Besides, CT protocols should be optimized to minimize unnecessary radiation exposure. Clinicians should only perform additional delayed imaging when there is a clinical indication. Unnecessary multiphasic protocols should get simplified into a single-phase protocol.
Common clinical presentations like appendicitis first require evaluation with MRI instead of CT.[6] Right upper quadrant ultrasound should be utilized if there is a clinical concern for cholecystitis.[7] Renal ultrasound should merit consideration before CT for nephrolithiasis and collecting system obstruction. If CT is the first indicate study of choice as in traumatic pregnancy patients to evaluate for intra-abdominal trauma, it is crucial to optimize CT setting to minimize the dose. Using wide pitch and narrow collimation can reduce the radiation dose. Besides, CT protocols should be optimized to minimize unnecessary radiation exposure. Clinicians should only perform additional delayed imaging when there is a clinical indication. Unnecessary multiphasic protocols should get simplified into a single-phase protocol.
When obtaining CT images of body parts outside of the abdomen and pelvis, the scattered radiation exposure to the fetus is minimal. Therefore, a shield does not significantly reduce the radiation exposure on the fetus during the CT scan. A lead shield may be an unnecessary precaution. However, it does minimally reduce the dose from scatter radiation and may provide patients a sense of reassurance and protection. The use of a lead shield is up to the discretion of the institution and provider.[8]
A lead shield may be an unnecessary precaution. However, it does minimally reduce the dose from scatter radiation and may provide patients a sense of reassurance and protection. The use of a lead shield is up to the discretion of the institution and provider.[8]
Magnetic Resonance
MRI uses a magnetic field to generate diagnostic images and does not contribute to ionizing radiation.
Ultrasonography
Ultrasound uses sound waves to generate diagnostic images and does not contribute to ionizing radiation.
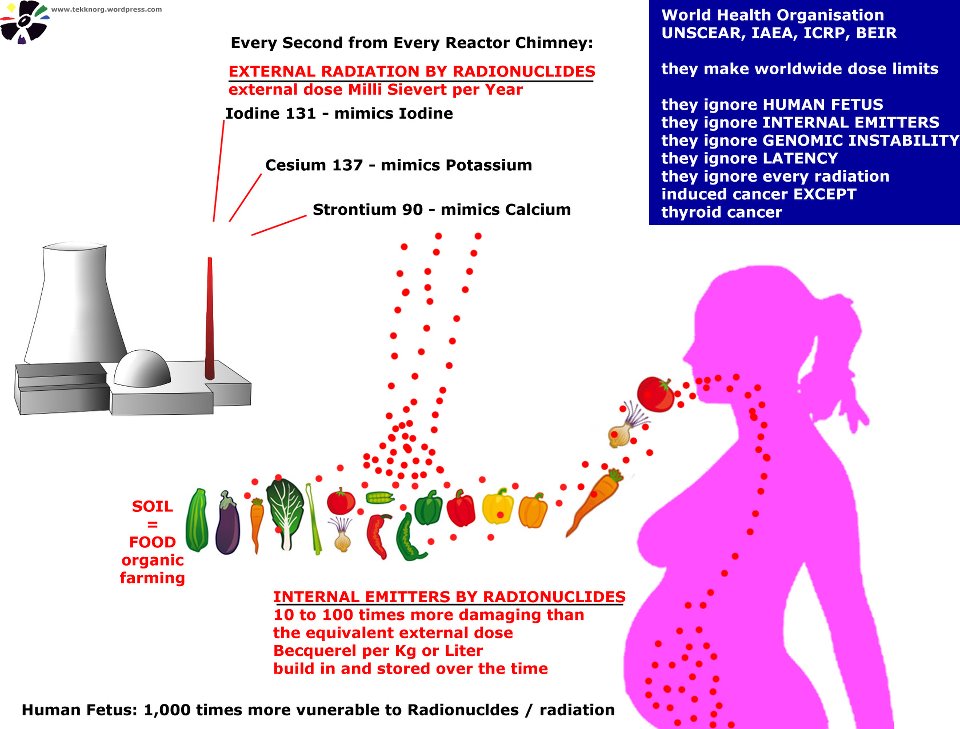
Nuclear Medicine
In nuclear medicine, radiopharmaceuticals are injected into patients. These radiopharmaceuticals are distributed throughout the body and emit radiation at the target location. Radiation energies from these radiotracers then convert into diagnostic images. The overall radiation exposure to the fetus depends on how much radiotracer gets delivered to or near the fetus. Fetal radiation exposure in nuclear medicine depends on multiple variables, including maternal excretion and uptake of the radiopharmaceutical, fetal distribution of the radiopharmaceutical, placental permeability of the radiopharmaceutical, tissue affinity of the radiopharmaceutical, the half-life of the radiotracer, the dose of the radiotracer, and type of radiation emitted from the radiotracer.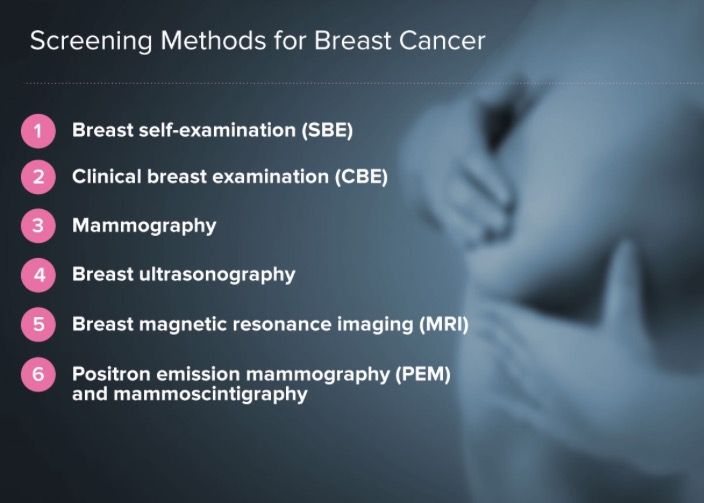 Generally, for nuclear medicine studies utilizing a radiopharmaceutical that gets excreted through the kidneys, patients are encouraged to hydrate and urinate to maximize the urinary excretion of radiopharmaceuticals.
Generally, for nuclear medicine studies utilizing a radiopharmaceutical that gets excreted through the kidneys, patients are encouraged to hydrate and urinate to maximize the urinary excretion of radiopharmaceuticals.
Specific clinical scenarios worth mentioning for nuclear medicine study is pregnancy patient with concern for pulmonary embolism. The first imaging modality should be an ultrasound of lower extremity to look for deep venous thrombosis. If there is still clinical suspicion for pulmonary embolism, CT pulmonary angiogram (CTPA) is preferable to the ventilation-perfusion (VQ) scan. The fetal dose of VQ is much higher than CTPA, even though the maternal dose is much lower. Due to the lower fetal dose, CTPA is the preferred test of choice.[9]
The thyroid iodine scan is not an option during pregnancy. Iodine 121 and 131 are taken up by fetus thyroid and therefore contraindicated.[10]
Angiography
Fetal radiation exposure from angiography and fluoroscopy should only be for emergent clinical settings.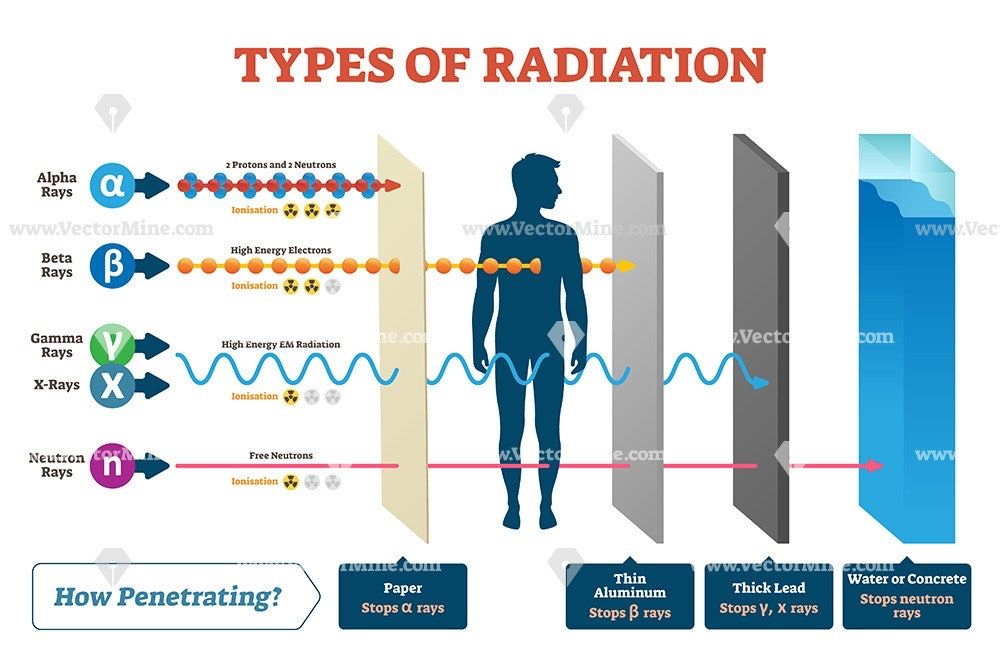 A physician performing fluoroscopy should utilize essential dose reducing techniques including pulse fluoroscopy instead of continuous fluoroscopy, last image hold rather than full exposure, and colimitation to appropriate field of view. Magnification increases the radiation dose and should be used only if necessary.
A physician performing fluoroscopy should utilize essential dose reducing techniques including pulse fluoroscopy instead of continuous fluoroscopy, last image hold rather than full exposure, and colimitation to appropriate field of view. Magnification increases the radiation dose and should be used only if necessary.
Patient Positioning
Appropriate patient positioning is vital in producing a diagnostic quality of images and prevent repeat examination that increases fetal radiation. Technologists should optimally position patients before imaging to obtain appropriate views for the exam. Obtaining diagnostic imaging at the first attempt eliminates the need for a repeat examination and significantly reduces unnecessary radiation exposure to the fetus.
Clinical Significance
The plain film, CT, nuclear medicine studies, and fluoroscopy uses ionizing radiation to obtain diagnostic images. A high level of radiation has adverse effects on the fetus; therefore, referring clinicians should consider alternative imaging modalities for pregnancy patients.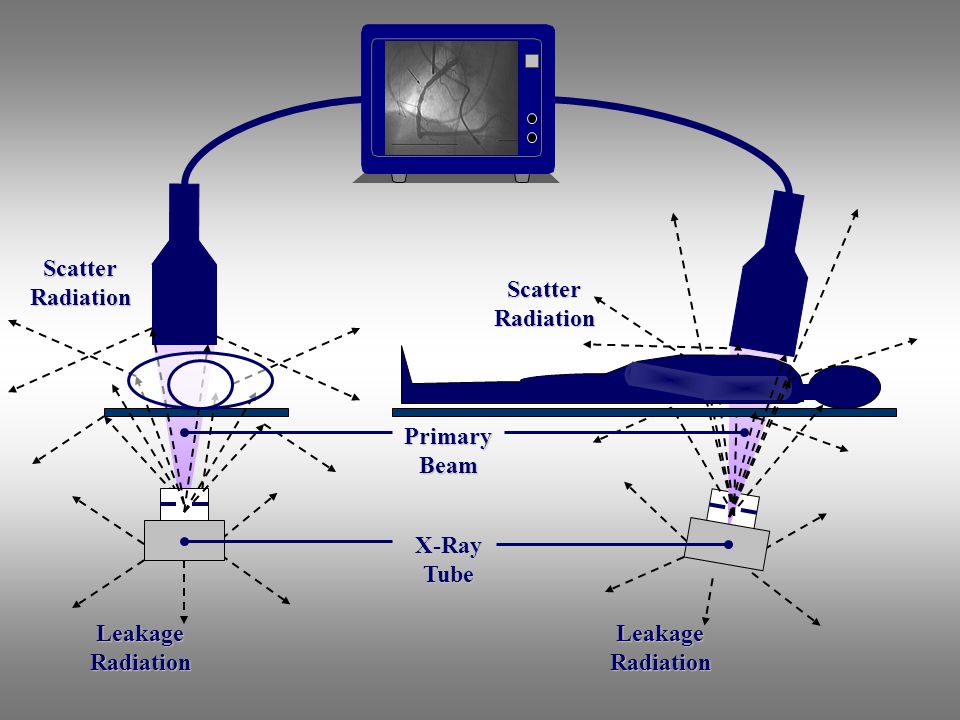 If diagnostic studies that expose radiation to the fetus are clinically required, it should be performed without delay but must take place in a way that minimizes radiation exposure to the fetus. Solid understanding of how each imaging modality contributes to fetal radiation exposure, techniques to reducing radiation exposure in the fetus, and adverse consequences of high radiation exposure is critical in providing the most appropriate imaging studies for pregnant patients.
If diagnostic studies that expose radiation to the fetus are clinically required, it should be performed without delay but must take place in a way that minimizes radiation exposure to the fetus. Solid understanding of how each imaging modality contributes to fetal radiation exposure, techniques to reducing radiation exposure in the fetus, and adverse consequences of high radiation exposure is critical in providing the most appropriate imaging studies for pregnant patients.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Brent RL. Saving lives and changing family histories: appropriate counseling of pregnant women and men and women of reproductive age, concerning the risk of diagnostic radiation exposures during and before pregnancy. Am J Obstet Gynecol. 2009 Jan;200(1):4-24. [PubMed: 19121655]
- 2.
De Santis M, Cesari E, Nobili E, Straface G, Cavaliere AF, Caruso A.
 Radiation effects on development. Birth Defects Res C Embryo Today. 2007 Sep;81(3):177-82. [PubMed: 17963274]
Radiation effects on development. Birth Defects Res C Embryo Today. 2007 Sep;81(3):177-82. [PubMed: 17963274]- 3.
Williams PM, Fletcher S. Health effects of prenatal radiation exposure. Am Fam Physician. 2010 Sep 01;82(5):488-93. [PubMed: 20822083]
- 4.
McCollough CH, Schueler BA, Atwell TD, Braun NN, Regner DM, Brown DL, LeRoy AJ. Radiation exposure and pregnancy: when should we be concerned? Radiographics. 2007 Jul-Aug;27(4):909-17; discussion 917-8. [PubMed: 17620458]
- 5.
Tremblay E, Thérasse E, Thomassin-Naggara I, Trop I. Quality initiatives: guidelines for use of medical imaging during pregnancy and lactation. Radiographics. 2012 May-Jun;32(3):897-911. [PubMed: 22403117]
- 6.
Vu L, Ambrose D, Vos P, Tiwari P, Rosengarten M, Wiseman S. Evaluation of MRI for the diagnosis of appendicitis during pregnancy when ultrasound is inconclusive. J Surg Res. 2009 Sep;156(1):145-9. [PubMed: 19560166]
- 7.
Wallace GW, Davis MA, Semelka RC, Fielding JR. Imaging the pregnant patient with abdominal pain. Abdom Imaging. 2012 Oct;37(5):849-60. [PubMed: 22160283]
- 8.
Uzoigwe CE, Middleton RG. Occupational radiation exposure and pregnancy in orthopaedics. J Bone Joint Surg Br. 2012 Jan;94(1):23-7. [PubMed: 22219242]
- 9.
Pahade JK, Litmanovich D, Pedrosa I, Romero J, Bankier AA, Boiselle PM. Quality initiatives: imaging pregnant patients with suspected pulmonary embolism: what the radiologist needs to know. Radiographics. 2009 May-Jun;29(3):639-54. [PubMed: 19270072]
- 10.
Jain C. ACOG Committee Opinion No. 723: Guidelines for Diagnostic Imaging During Pregnancy and Lactation. Obstet Gynecol. 2019 Jan;133(1):186. [PubMed: 30575654]
Is X-ray examination dangerous during pregnancy - MEDSI
01/15/2018
Is X-ray examination dangerous during pregnancy
X-ray examinations are carried out to determine the presence of any pathologies, neoplasms or diseases. For this, a directed beam of electromagnetic waves of a given length and frequency is used. It passes through human organs, the tissues of which reflect and absorb it in different ways.
For this, a directed beam of electromagnetic waves of a given length and frequency is used. It passes through human organs, the tissues of which reflect and absorb it in different ways.
Due to this difference, various anomalies can be seen. The result is sent to the screen or recorded on a special film.
During a preventive examination, this examination is carried out in a special room. In case of injury to the patient, it can be used immediately in the emergency department, operating room or intensive care unit.
Influence of irradiation on the fetus
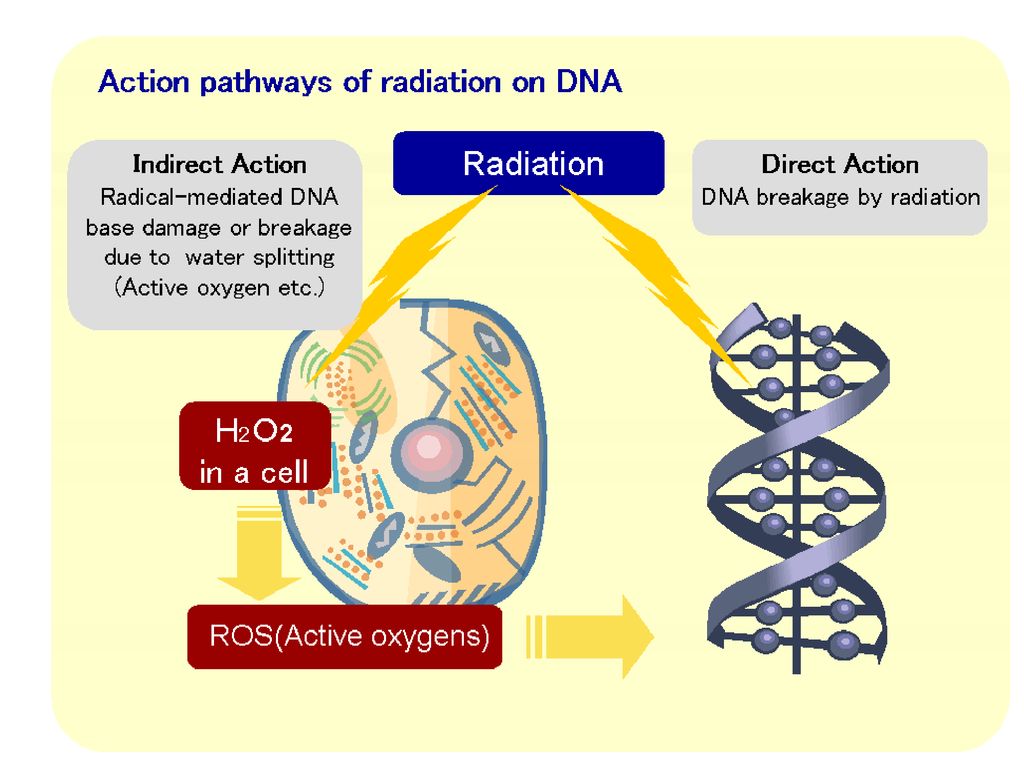
X-rays in general are not always beneficial for the body, as it destroys those of its cells that are in a state of constant division. This leads to the destruction or mutation of DNA chains.
There are not many such newly formed cells in the body of an adult. But in the fetus in the early stages of development, they are the basis. Therefore, such an examination is quite dangerous for him. The most likely occurrence of complications when using x-rays during pregnancy in its first trimester (initial 12 weeks).
What problems can X-rays cause in early pregnancy?
Due to the gradual development of the fetus, in each week of its existence, the formation of future systems of the child's body takes place. Therefore, the mother's body receiving a large amount of X-rays at these stages can have various serious consequences:
- The first two weeks. Possible death of the embryo, miscarriage, ectopic pregnancy.
- Weeks three and four. Pathologies at an early stage of fetal development, miscarriage.
- Fifth-sixth weeks. Disturbances in the development of a number of organs and systems: thyroid, thymus and gonads; immune, nervous, circulatory, endocrine systems.
- Seventh week. Damage to the liver, intestines. Metabolic disease.
- Eighth. Pathologies of the development of joints and limbs, the oral cavity.
- Ninth week. Damage to the respiratory and reproductive systems.
- Tenth and eleventh weeks.
 Problems associated with the development of teeth. Heart disease.
Problems associated with the development of teeth. Heart disease. - Twelfth week. Pathology of the thyroid gland, disorders of the immune system.
After this period, the effect of radiation on the fetus decreases, but it is still not recommended to do such a study until the end of pregnancy, except in cases of emergency.
X-rays in early pregnancy
Doctors try not to prescribe X-rays to pregnant women, because even a minimal risk of harm from radiation always remains. It is especially great in the first twelve weeks.
The most dangerous tests for the fetus are:
- Abdominal X-ray
- X-ray of the pelvis and spine
- Mammography
- Fluorography
- Computed tomography
- Isotope scanning
Less dangerous X-rays are:
- Chest (lungs, heart)
- Brain
- Limbs
Are there any non-hazardous examinations?
The safest types of X-ray examination are:
- X-ray of teeth
- X-ray of the nose
In these cases, the exposure occurs locally, so the radiation dose is minimal.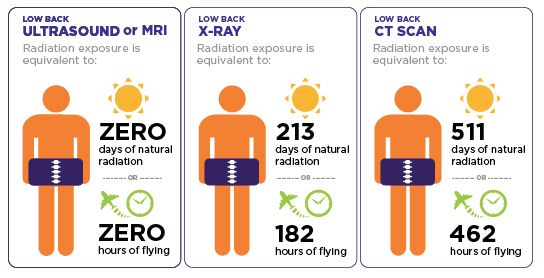
The amount of radiation that a fetus can receive in two months is regulated by the Sanitary Rules and Regulations and should not exceed 1 millisievert (mSv).
There are other types of examinations that can be used instead of X-ray during pregnancy:
- MRI
- Visiography
- Ultrasound
Nevertheless, doctors try not to prescribe MRI in the first trimester of pregnancy, since statistical studies are not enough to clarify its safety during this period.
What if X-rays are indispensable?
X-rays for pregnant women may be necessary in a situation where the disease or injury threatens the life and health of the mother and child, and it is impossible to use other diagnostic methods. And the harm from not using x-rays outweighs the potential harm from its use.
- If it is necessary to examine an area that does not touch the pelvis, abdomen or spine, they must be shielded with lead aprons and pads.
- If an X-ray is to be taken directly through the fetus in early pregnancy, the doctor may suggest that it be interrupted to avoid mutations and miscarriage.
- A woman may refuse to have an abortion, but in this case she must understand the risks she is taking and the pathologies that may appear in the fetus.
In all these cases, after passing the examination, it is recommended to go for an ultrasound scan to monitor the condition of the fetus and the appearance of certain pathologies.
If it is possible to postpone the use of x-rays until the last trimester or postpartum, then this should be done.
At the earliest possible time, a woman may not be aware of the pregnancy. Therefore, before x-rays, it is recommended to undergo an additional examination.
Benefits of X-ray analysis at MEDSI:
- 30 x-ray examinations
- The latest equipment with the ability to control the intensity of radiation
- Urgent examination in case of injury or other medical indications
- Technologies suitable for both adults and children
- Radiologists of high qualification categories, candidates of medical sciences
- Appointment for research and consultation by phone 8 (495) 7-800-500
- More than 20 diagnostic centers
Do not delay treatment, see a doctor right now:
- Pregnancy tests
- Planning and management of pregnancy
- Obstetrician-gynecologist appointment
X-ray - BUZOO City polyclinic No.
 9
9 Working hours of the X-ray room
X-rays are taken from 8-00 to 11-00;
Fluoroscopy 8:30 am to 1:00 pm and 3:00 pm to 6:00 pm;
The work schedule of the Fluorography Room is from Mon to Fri, the first shift is from 8-30 to 13-00, the second shift is from 15-00 to 18-00.
Day off Sat, Sun.
X-ray examination: types of examinations, radiation doses, safety and risks of X-ray examination.
X-ray examinations are among the most common in modern medicine. X-rays are used to obtain simple x-rays of bones and internal organs, fluorography, computed tomography, angiography, etc. . Conducting most modern methods of X-ray examination involves irradiating the subject with negligible doses of radiation, which are completely safe for human health.
X-ray examination methods are used much less often in the case of pregnant women and children, however, even in these categories of patients, if necessary, an X-ray examination can be performed without significant risk to the development of pregnancy or the health of the child.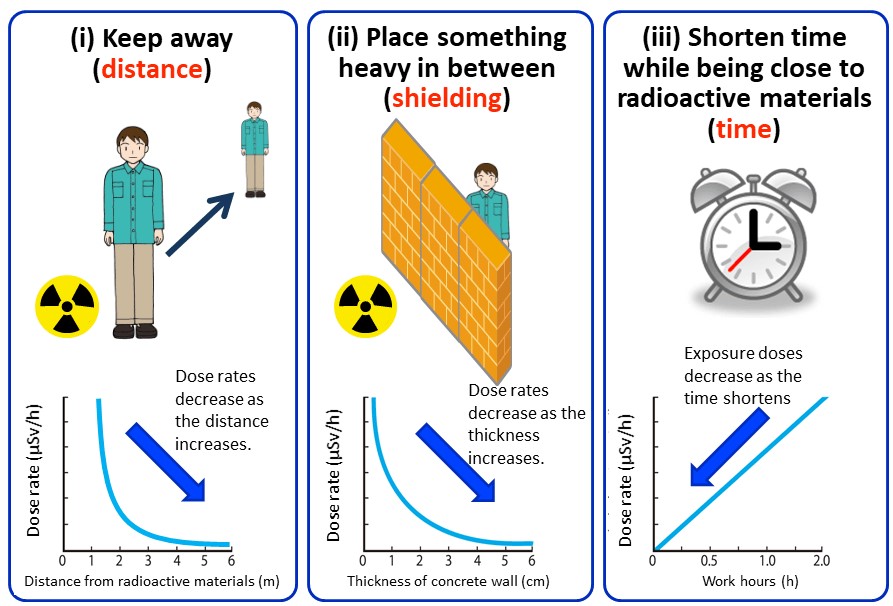
What are X-ray waves and what effect do they have on the human body?
X-rays are a form of electromagnetic radiation, other forms of which are light or radio waves. A characteristic feature of X-ray radiation is a very short wavelength, which allows this type of electromagnetic wave to carry a lot of energy and gives it a high penetrating power. Unlike light, X-rays are able to penetrate through the human body (“shine through it”), which allows the radiologist to obtain images of the internal structures of the human body.
In fact, X-rays are “very strong light” that is not visible to the human eye, but can “see through” even dense objects such as metal plates.
Medical X-ray examinations (X-ray examinations) in many cases provide important information about the state of health of the examined person and help the doctor to make an accurate diagnosis in the case of a number of complex diseases.
X-ray examination allows you to get images of the dense structures of the human body on photographic film (radiography) or on the screen (fluoroscopy).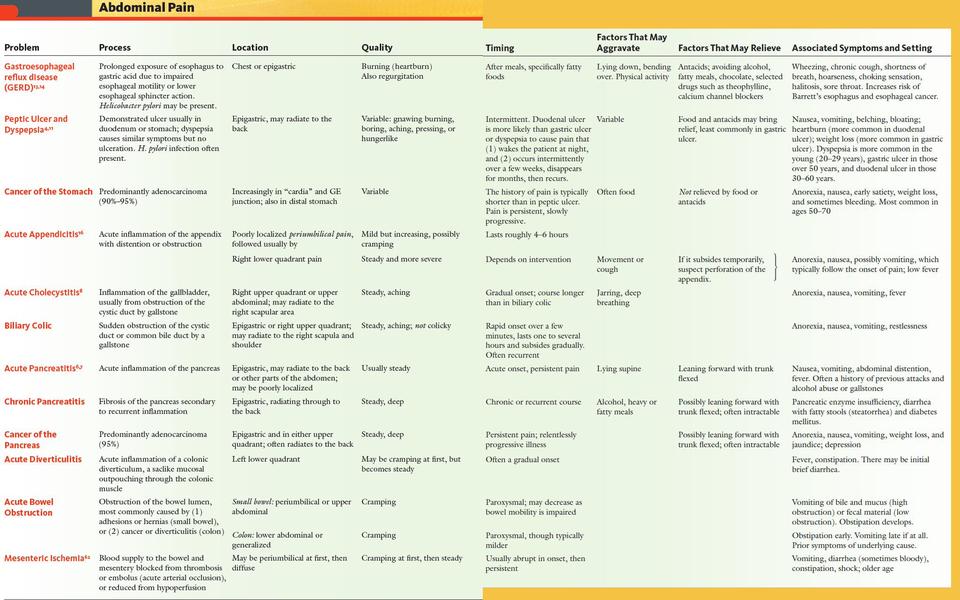
The high penetrating power and energy of X-rays make them quite dangerous for the human body. X-ray radiation is one of the most common types of radiation. During the passage through the human body, X-rays interact with its molecules and ionize them. Simply put, X-rays are able to "break" the complex molecules and atoms of the human body into charged particles and active molecules. As in the case of other types of radiation, only X-rays of a certain intensity are considered dangerous, which affects the human body for a sufficiently long period of time. The vast majority of medical examinations that use X-rays use low-energy X-rays and irradiate the human body for very short periods of time, and therefore, even when they are repeated many times, they are considered practically harmless to humans.
The doses of x-rays that are used in a conventional x-ray of the chest or bones of the extremities cannot cause any immediate side effects and only very slightly (no more than 0.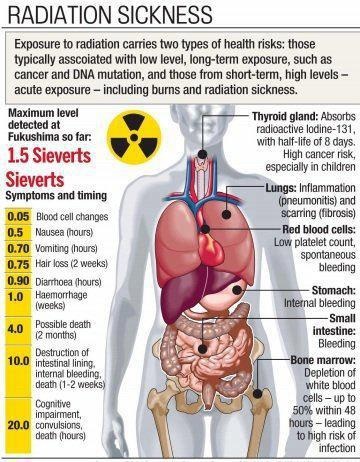 001%) increase the risk of developing cancer in the future.
001%) increase the risk of developing cancer in the future.
Measurement of radiation dose during X-ray examinations
As mentioned above, the effect of X-rays on the human body depends on their intensity and exposure time. The product of the radiation intensity and its duration represents the radiation dose.
The unit of total human body dose is milliSievert (mSv). Also, other units of measurement are used to measure the dose of x-rays, including rad, rem, roentgen, and grey.
Different tissues and organs of the human body have different sensitivity to radiation, and therefore, the risk of radiation exposure of different parts of the body during an x-ray examination varies significantly.
The term effective dose is used in relation to the risk of exposure to the whole body of a person. For example, during an x-ray examination of the head area, other parts of the body are practically not directly exposed to x-rays. However, in order to assess the risk presented to the health of the patient, it is not the dose of direct exposure to the examined area that is calculated, but the dose of total exposure to the body is determined - that is, the effective dose of exposure.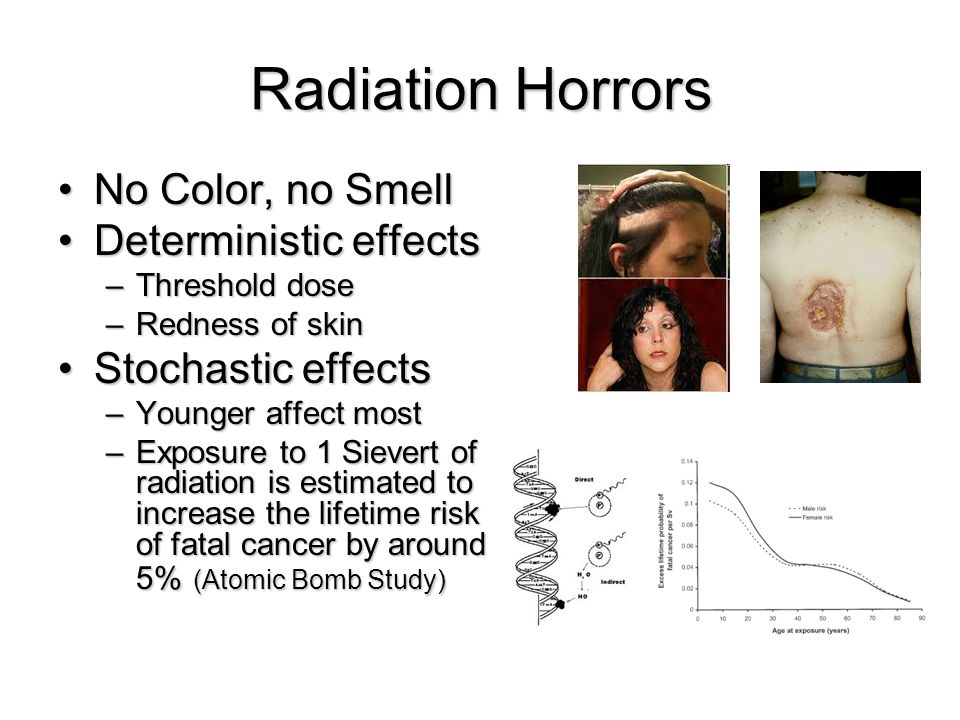 The determination of the effective dose is carried out taking into account the relative sensitivity of different tissues exposed to radiation. Also, the effective dose makes it possible to compare the risk of X-ray studies with more common sources of exposure, such as, for example, background radiation, cosmic rays, etc.
The determination of the effective dose is carried out taking into account the relative sensitivity of different tissues exposed to radiation. Also, the effective dose makes it possible to compare the risk of X-ray studies with more common sources of exposure, such as, for example, background radiation, cosmic rays, etc.
Radiation dose calculation and risk assessment of radiological exposure
Below is a comparison of the effective dose of radiation received during the most commonly used diagnostic procedures using x-rays with the natural radiation that we are exposed to under normal conditions throughout our lives. It should be noted that the doses indicated in the table are indicative and may vary depending on the devices used and methods of examination.
| Procedure | Effective radiation dose | Comparable to natural exposure received during the specified period of time |
| Chest X-ray | 0. | 10 days |
| Chest X-ray | 0.3 mSv | 30 days |
| Computed tomography of the abdomen and pelvis | 10 mSv | 3 years |
| Whole body computed tomography | 10 mSv | 3 years |
| Intravenous pyelography | 3 mSv | 1 year |
| Radiography - upper stomach and small intestine | 8 mSv | 3 years |
| X-ray of the colon | 6 mSv | 2 years |
| X-ray of the spine | 1. | 6 months |
| Radiography of the bones of the arms or legs | 0.001 mSv | Less than 1 day |
| Computed tomography - head | 2 mSv | 8 months |
| Computed tomography of the spine | 6 mSv | 2 years |
| Myelography | 4 mSv | 16 months |
| Computed tomography of the chest | 7 mSv | 2 years |
| Voiding cystourethrography | 5-10 years: 1. Infant: 0.8 mSv | 6 months 3 months |
| Computed tomography of the skull and paranasal sinuses | 0.6 mSv | 2 months |
| Bone densitometry (bone density determination) | 0.001 mSv | Less than 1 day |
| Galactography | 0.7 mSv | 3 months |
| Hysterosalpingography | 1 mSv | 4 months |
| Mammography | 0.7 mSv | 3 months |
*1 rem = 10 mSv
Based on the latest data on the risk of radiation exposure to human health, a quantitative risk assessment is carried out only in case of receiving a radiation dose above 5 rem (50 mSv) within one year (for adults in children) , or in the case of receiving a dose of radiation above 10 rem throughout life, in addition to natural exposure.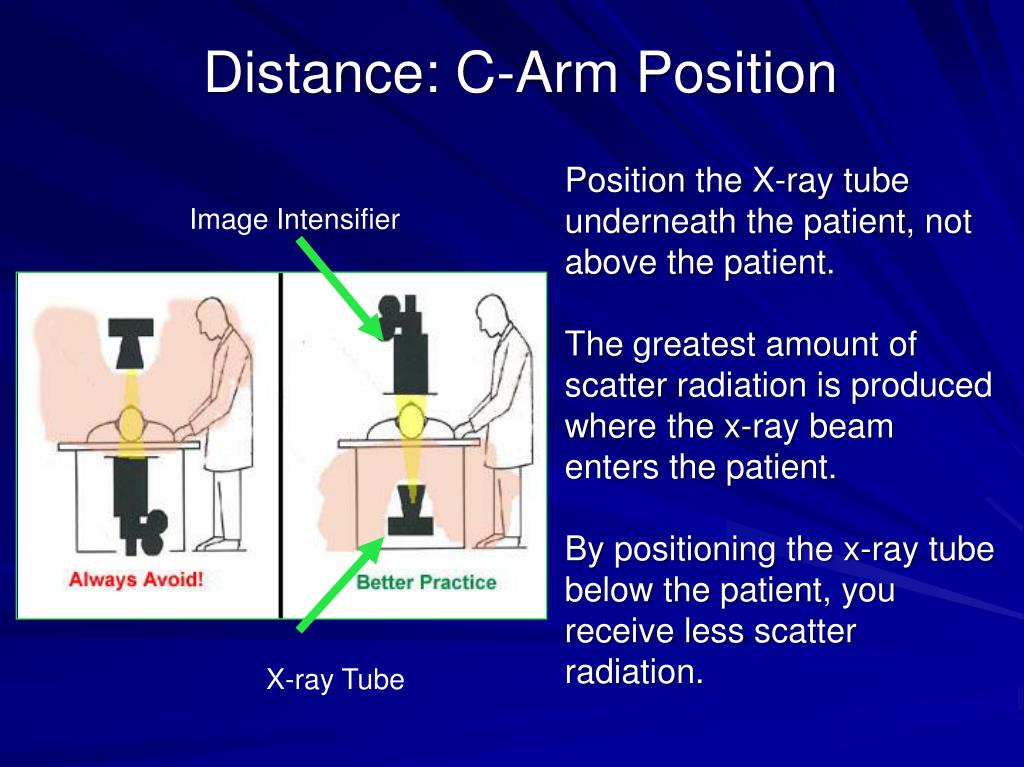
There is clear medical evidence regarding the risks associated with high doses of radiation. In the event that the total exposure dose is below 10 rem (including natural exposure and exposure in the workplace), the risk of harm to health is either too low to be accurately assessed, or does not exist at all.
As a result of epidemiological studies among people exposed to relatively high doses of radiation (for example, people who survived the atomic bomb explosion in Japan in 1945) there were no side effects on the health of people who received low doses of radiation (less than 10 rem) for many years.
Natural exposure
X-ray examinations are far from the only source of radiation for humans. People are constantly exposed to radioactive radiation (including in the form of X-rays) from various sources, such as radioactive metals in the soil and cosmic radiation.
According to modern estimates, the exposure from one chest x-ray is approximately equal to the amount of radiation received in normal living conditions in 10 days.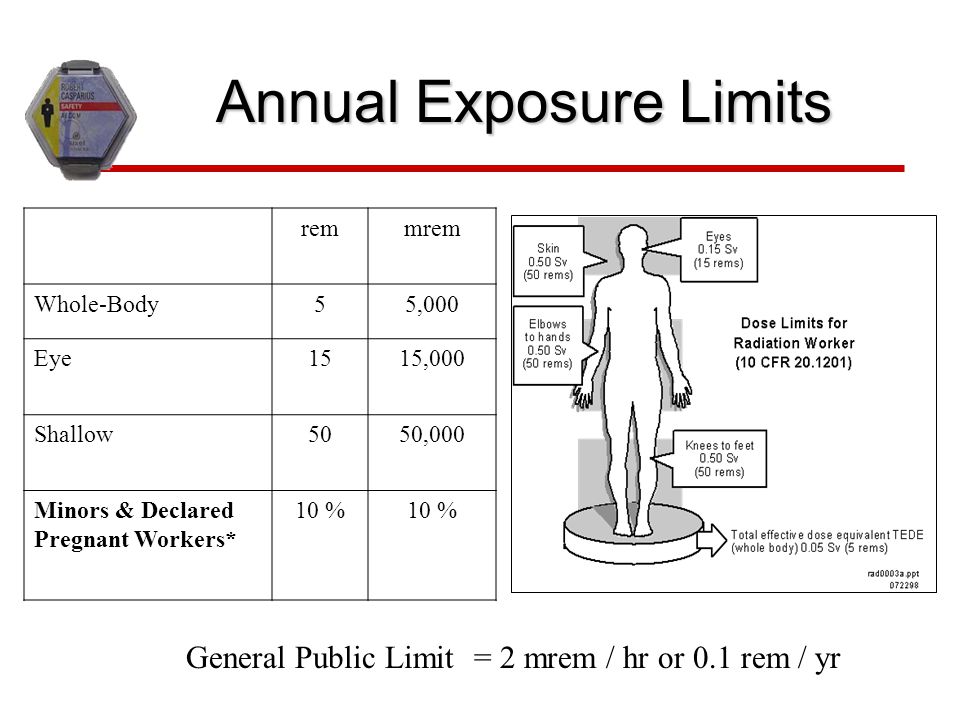
X-Ray Safety Level
As with many other medical procedures, X-rays are safe when used carefully and rationally. Radiologists are trained to use the minimum dose of radiation necessary to obtain the desired result. The amount of radiation used in most medical examinations is very small, and the benefit of the examination almost always far outweighs the risk to the body.
X-rays affect the human body only at the moment the device switch is turned on. The duration of "transmission" of X-rays in the case of conventional radiography does not exceed a few milliseconds.
Collective exposure to x-rays throughout life
The decision to perform an x-ray examination must be medically justified and can only be made after comparing the likely benefits of the study and the potential risk associated with exposure.
In the case of low-dose medical examinations, the decision to take an X-ray examination is usually a fairly simple task. In the case of studies using higher doses of radiation, such as computed tomography, and in the case of procedures involving contrast materials such as barium or iodine, the radiologist may take into account whether the patient has been previously exposed to x-rays, and if so, then in what quantity.
If you have had frequent x-rays and frequently change location or doctor, record your entire history of medical examinations.
X-ray examinations during pregnancy and lactation
Limitation of the use of X-ray examinations during pregnancy is associated with the potential risk of adverse effects of additional radiation on the development of the fetus.
Although the vast majority of medical procedures that use x-rays do not expose the developing child to critical radiation exposure and significant risk, in some cases there may be a small chance of adverse effects of x-ray radiation on the fetus. The risk of having an X-ray examination depends on factors such as the length of pregnancy and the type of procedure performed.
When x-rays of the head, arms, legs or chest using special protective aprons for pregnant women, as a rule, the child is not directly exposed to x-rays and, therefore, the examination procedure is practically safe for him.
Only in rare cases, during pregnancy, it becomes necessary to perform an x-ray examination of the abdomen or pelvis, but even in this situation, the doctor may prescribe a special type of examination or, if possible, limit the number of examinations and the area of radiation.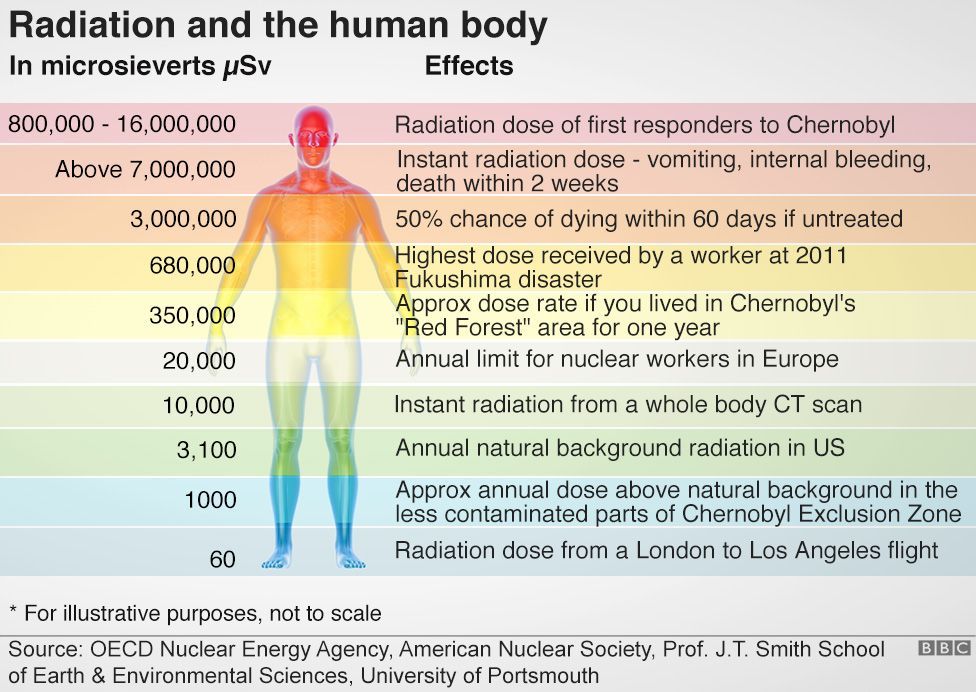
Routine abdominal x-rays are not considered to pose a significant risk to a child's development. Procedures such as CT scans of the abdomen or pelvis expose the child to more radiation, but they also rarely result in developmental abnormalities.
Due to the fact that the vast majority of X-ray examinations in pregnant women are carried out for health reasons (for example, the need to exclude tuberculosis or pneumonia), the risk of these studies for the mother and unborn child is always incomparably lower than the possible harm that the examination can bring to them.
All procedures using x-rays (plain x-ray, fluorography, computed tomography) are safe for breastfeeding mothers. X-rays do not affect the composition of breast milk. If x-ray examinations are necessary for a nursing mother, there is no need to interrupt breastfeeding or express milk.
In the case of breastfeeding mothers, only X-ray examinations that involve the introduction of radioactive substances (eg radioactive iodine) into the body pose a certain danger.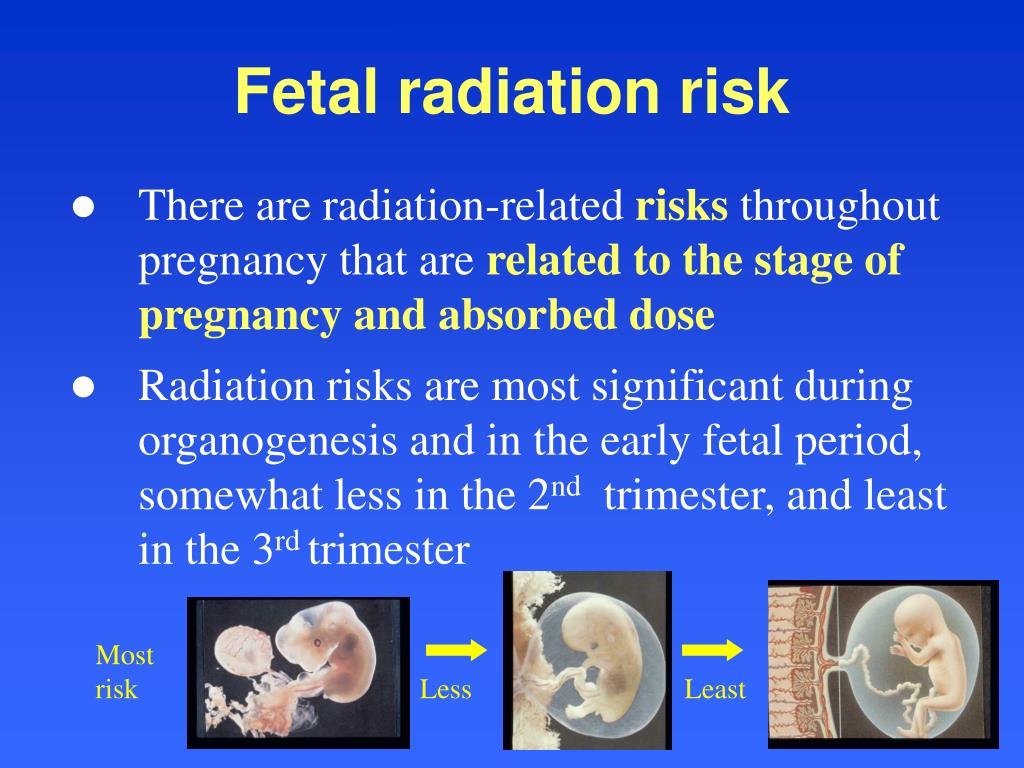 Breastfeeding mothers should inform their doctors about lactation before such examinations, as some drugs used during the examination may pass into the milk. To avoid exposure of the baby to radioactive substances, doctors will likely advise the mother to interrupt feeding for a short time, depending on the type and amount of radioactive substance (radionuclide) used.
Breastfeeding mothers should inform their doctors about lactation before such examinations, as some drugs used during the examination may pass into the milk. To avoid exposure of the baby to radioactive substances, doctors will likely advise the mother to interrupt feeding for a short time, depending on the type and amount of radioactive substance (radionuclide) used.
X-ray examinations of children
Although children are much more sensitive to the effects of radiation than adults, most types of X-ray examinations (even multiple sessions if necessary), but at a total dose below 50 mSv per year, do not pose a serious danger to child's health.
As in the case of pregnant women, X-ray examination in childhood is carried out for health reasons and its risk is almost always much lower than the possible risk of the disease for which the examination is carried out.
How to remove radiation from the body?
In nature, there are a large number of sources of radiation, the carriers of which are various physical phenomena or chemicals.
 1 mSv
1 mSv 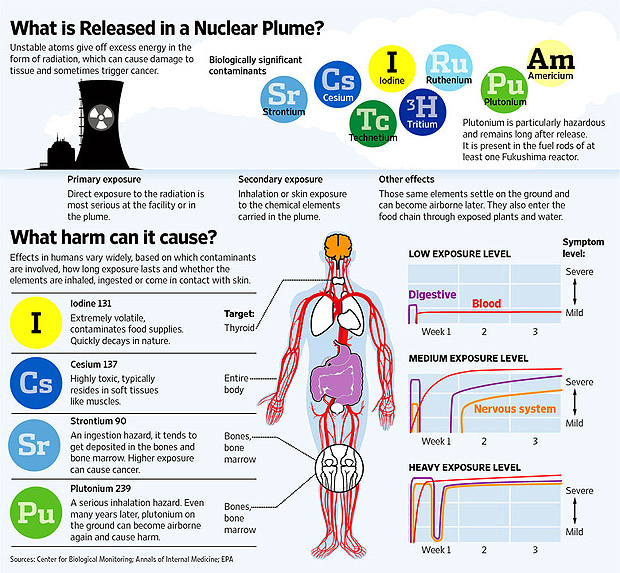 5 mSv
5 mSv 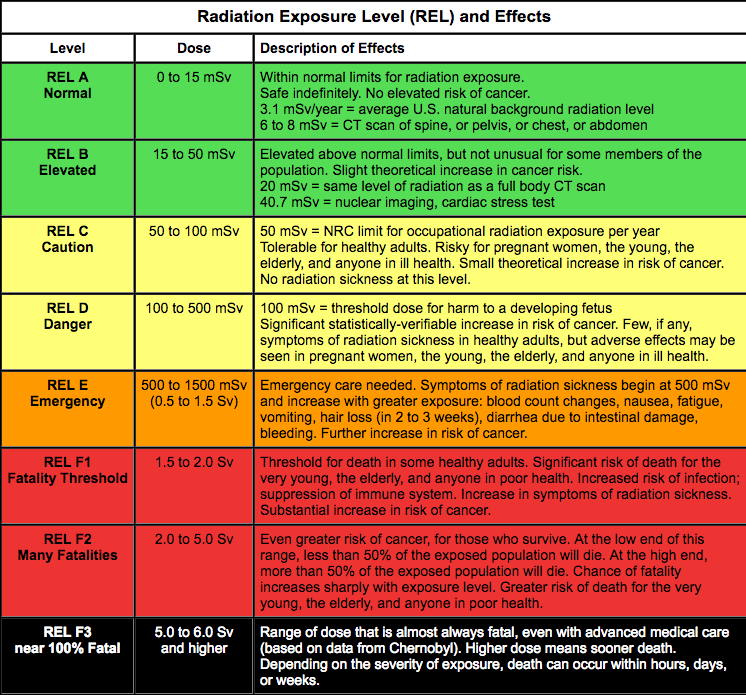 6 mSv
6 mSv