Breastfeeding dairy intolerance
CMPI - Cow’s Milk Protein Intolerance
Usually when it is recommended that a breastfeeding mother eliminate dairy produce from her diet, it is because of a problem that may be caused by the protein it contains, not because of lactose intolerance. Human milk is full of lactose, and nature has made certain that babies and toddlers can digest it. Large protein molecules from cow’s milk can pass into human milk fairly intact and it is these particles that can bother a sensitive baby. If your baby has Cow’s milk protein intolerance (CMPI) he might have colic-like symptoms, and be wheezy, vomit, have diarrhea (including bloody diarrhea), constipation, a rash, eczema and/or a blocked nose.
If you suspect your baby is sensitive to the cow’s milk protein in your diet you can remove dairy products and see if it makes a difference. It can take up to 21 days for all traces of cow’s milk protein to leave your system so it’s best to wait for two to three weeks to evaluate the results. Some babies will react well if you remove visible dairy products such as milk, yoghurt, cheese, cream and ice-cream; others will not show any improvement unless you remove every trace of cow’s milk protein from your diet so you may need to read the labels of all the food you eat and eliminate hidden sources.
Many babies grow out of their sensitivity, so even if your baby is affected you may be able to add dairy back into your diet as your baby gets older. Some mothers wait until their baby has weaned to reintroduce dairy to their diet.
Some babies will show no improvement and it’s possible other elements of a mother’s diet are causing a problem. See our post on allergies.
If you do eliminate dairy from your diet there are many other sources of calcium, such as broccoli, collard greens, kale, bok choi, pak choi, ground sesame seeds, blackstrap molasses, almonds, brazil nuts, canned sardines or salmon (with soft bones).
Some kinds of calcium supplement are better absorbed and utilized by your body than other types. If you want to take one you can ask your healthcare professional which types of calcium supplement you might take.
If you want to take one you can ask your healthcare professional which types of calcium supplement you might take.
Your body will take what it needs from your nutritional stores to make the perfect milk for your baby. Your body might go short on calcium, but your breastmilk won’t! There is also research showing that while a breastfeeding mother will have reduced bone density while she is breastfeeding, she piles on bone density after her baby weans and is actually at reduced risk for osteoporosis compared to a woman who has never breastfed a baby.
When considering if your baby may be sensitive to something you have eaten it is worth checking if another carer has given him anything at all to eat besides your milk.
Smoking cigarettes and drinking caffeinated or alcoholic beverages can sometimes lead to a fussy baby.
Even if your baby is sensitive to something in your milk, it is still the perfect milk for him. Artificial baby milks are made from cow’s milk. Around half of babies who are sensitive to dairy are also sensitive to soya, and many also react to goat’s and sheep’s milk.
Around half of babies who are sensitive to dairy are also sensitive to soya, and many also react to goat’s and sheep’s milk.
Reflux
Allergies
Alergia a la Proteína de la Leche de Vaca – APLV
Published January 2018.
What should I do if I think my baby is allergic or intolerant to cows' milk?
If you think your baby is having a reaction to cows' milk, see your GP or health visitor to discuss your concerns.
They will be able to assess if your baby's symptoms may be caused by a cows' milk allergy or something else. Make sure you get medical advice before taking cows' milk out of your child's diet as it contains important nutrients.
Cows' milk allergy in babies
Cows' milk allergy (CMA), also called cows' milk protein allergy, is one of the most common childhood food allergies. It is estimated to affect around 7% of babies under 1, though most children grow out of it.
It is estimated to affect around 7% of babies under 1, though most children grow out of it.
CMA typically develops when cows' milk is first introduced into your baby's diet either in formula or when your baby starts eating solids.
More rarely, it can affect babies who are exclusively breastfed because of cows' milk from the mother's diet passing to the baby through breast milk.
There are 2 main types of CMA:
- immediate CMA – where symptoms typically begin within minutes of having cows' milk
- delayed CMA – where symptoms typically begin several hours, or even days, after having cows' milk
Symptoms of cows' milk allergy
Cows' milk allergy can cause a wide range of symptoms, including:
- skin reactions – such as an itchy rash or swelling of the lips, face and around the eyes
- digestive problems – such as stomach ache, vomiting, colic, diarrhoea or constipation
- hay fever-like symptoms – such as a runny or blocked nose
- eczema that does not improve with treatment
Occasionally CMA can cause severe allergic symptoms that come on suddenly, such as swelling in the mouth or throat, wheezing, cough, shortness of breath, and difficult, noisy breathing.
A severe allergic reaction (anaphylaxis) is a medical emergency. Call 999 for an ambulance immediately if you think your child has anaphylaxis (even if they start to feel better).
Treatment for CMA
If your baby is diagnosed with CMA, you'll be offered advice by your GP or an allergy specialist on how to manage their allergy. You may also be referred to a dietitian.
Treatment involves removing all cows' milk from your child's diet for a period of time.
If your baby is formula-fed, your GP can prescribe special infant formula.
Do not give your child any other type of milk without first getting medical advice.
If your baby is exclusively breastfed, the mother will be advised to avoid all cows' milk products.
Your child should be assessed around every 6 to 18 months to see if they have grown out of their allergy.
Read more about cows' milk allergy in children on National Institute for Health and Care Excellence (NICE).
Could it be lactose intolerance?
Lactose intolerance is another type of reaction to milk, when the body cannot digest lactose, a natural sugar found in milk. However, this is not an allergy.
Lactose intolerance can be temporary – for example, it can come on for a few days or weeks after a tummy bug.
Symptoms of lactose intolerance include:
- diarrhoea
- vomiting
- stomach rumbling and pains
- wind
Treatment for lactose intolerance
Treatment depends on the extent of your child's intolerance. Some children with lactose intolerance may be able to have small amounts of dairy products without having symptoms.
Your child may be referred to a dietitian for specialist advice.
Read more about treatment for lactose intolerance.
Further information:
- Colic
- Food allergies in babies and children
- Reflux in babies
- How can I tell if my baby is seriously ill?
- Your baby's first solid foods
- National Institute for Health and Care Excellence (NICE): food allergy in children
Page last reviewed: 28 November 2022
Next review due: 28 November 2025
dysbacteriosis, lactase deficiency and culture of milk for sterility
MainLibraryHelp for motherNewborn diseases: dysbacteriosis, lactase deficiency ..?
Once I received a task from my management to answer the question of our American colleague, a breastfeeding consultant from the La Lache League: "At parental conferences on the Internet, Russian mothers very often discuss three issues: lactase deficiency, dysbacteriosis and sowing milk for sterility .
What is meant?"
The first two conditions are reminiscent of what they, in LLL, call foremilk imbalance and hindmilk imbalance and dysbiosis. But these conditions are not a terrible pathology, and on the sites they are discussed from this point of view. About sowing milk for sterility - the American asked at all, why is it carried out??
I'll start in order.
Lactase deficiency (or lactose intolerance)
According to specialized literature, carbohydrate metabolism diseases associated with changes in the activity of enzymes that break down sugars, including lactose, are extremely rare in the population. The data for different countries are different. The frequency of such diseases varies from 1 in 20,000 to 1 in 200,000 children. Why do pediatricians talk about lactose intolerance in almost every second child?
How could mankind survive if this disease, which leads, for example, to malnutrition in the absence of treatment and death, occurs in most infants? Mankind has been able to survive to this day because true lactose intolerance, which is genetically determined and associated with the complete absence or serious deficiency of essential enzymes, is very rare. What happens very often? What are modern doctors constantly faced with? With lactose intolerance, formed as a result of improperly organized breastfeeding.
What happens very often? What are modern doctors constantly faced with? With lactose intolerance, formed as a result of improperly organized breastfeeding.
If a mother feeds a child 6-7 times a day, “saves” milk for feeding, expresses after feedings, transfers the child to one or the other breast during feeding, the likelihood of developing lactose intolerance is very high. This is the same lactose intolerance, the cause of which is an imbalance between the "front" and "back" portions of milk. It turns out that the child feeds mainly on the "front" portion of milk, more liquid, containing a large amount of lactose. In the breast between feedings, mainly “front” milk is also collected, “hind” milk, thick, more fatty, is formed mainly during the sucking of the child. If the mother shifts the baby 5-10 minutes after the start of feeding to the other breast, he will suck the front milk out of it. Mom is pumping her hind milk. The baby will not put on weight very well, sometimes just a little. He may have loose stools with greens and foam. Mom will think that she has bad milk, although there is a lot of it.
He may have loose stools with greens and foam. Mom will think that she has bad milk, although there is a lot of it.
The same situation can occur if the mother restricts the child from suckling, for example, strictly for 15-20 minutes. The baby often does not have time to get to the "hind" milk. And besides, he does not sufficiently stimulate the breast to produce milk if he sucks 6-7 times a day for 15-20 minutes. Therefore, in parallel, in the situations described above, a lack of milk will develop. When a child begins to be fed with a lactose-free formula, he will begin to get fat, everyone will breathe a sigh of relief, and the myth that milk can be bad and is generally scarce in modern women will be strengthened in the mind. There is also transient, temporary lactase deficiency. A child on properly organized breastfeeding, with a good weight gain, in general with good health, in the first 2-3 months of life (and sometimes longer) has a frothy stool. If mom tells the doctor about this, an examination will be scheduled, sugars will be found in the analysis.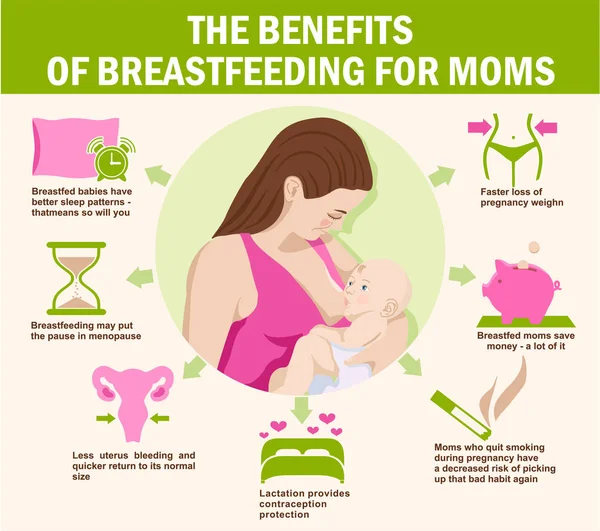 The baby will be switched to a lactose-free formula. However, incomplete absorption of lactose is common for a breastfed baby!!! (66% of children at 6 weeks of age and 60% of children at 3 months of age).
The baby will be switched to a lactose-free formula. However, incomplete absorption of lactose is common for a breastfed baby!!! (66% of children at 6 weeks of age and 60% of children at 3 months of age).
One mother, for example, was told in such a situation: “Your child is in severe pain! Look at his gas formation! And you continue to feed him with your milk! It is poison for him!!!” I am not saying that all doctors act this way. I know pediatricians who, seeing that the child is quite well, do not begin to treat him, relying only on the laboratory results obtained, and do not even prescribe unnecessary examinations! Let's remember that for the past 50 years, doctors have dealt primarily with children who were fed formula. Accordingly, much knowledge and laboratory tests are applicable only to this group of children. The presence of sugar in the stool of a formula-fed baby is a pathology. The presence of sugar in the stool of a breastfed baby is normal!
A significant amount of sugar may be the result of incorrect recommendations for feeding the child (frequent breast changes during feeding, limiting the duration of suckling, pumping after feeding), because. the baby gets plenty of lactose-rich foremilk. Lactose intolerance and a newborn baby - an unheard of combination!!!
the baby gets plenty of lactose-rich foremilk. Lactose intolerance and a newborn baby - an unheard of combination!!!
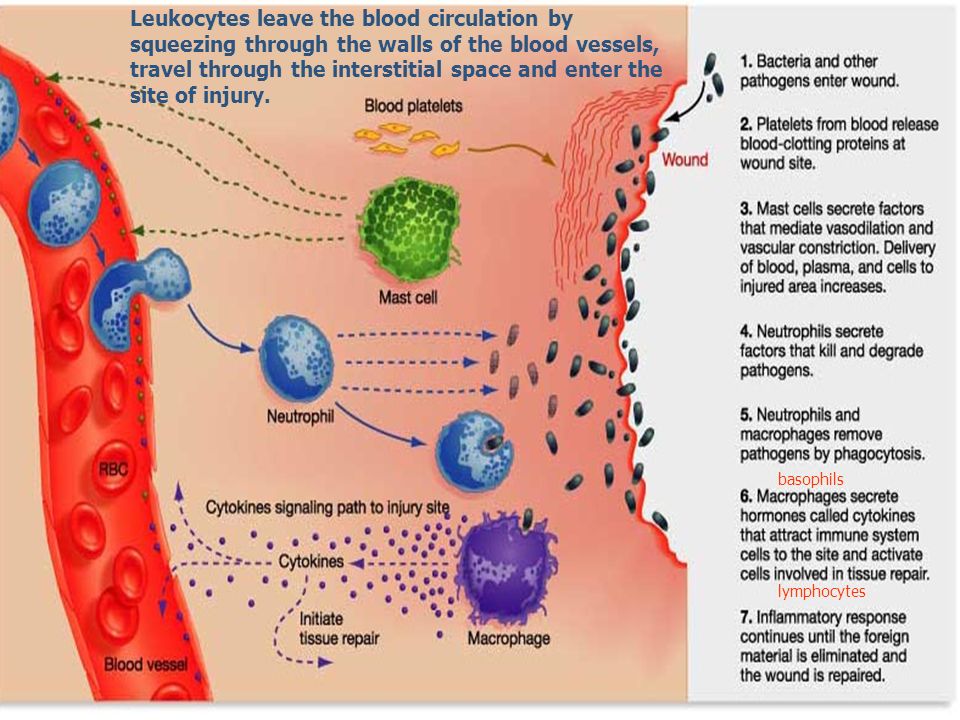
Neonatal dysbacteriosis
This condition is extremely popular. The baby, as you know, is born with a sterile intestine. If, from the moment of birth, nothing enters his mouth except the mother's nipple (which, by the way, is only designed by nature), then quite quickly the child's gastrointestinal tract is sown with normal microflora. Colostrum and breast milk contain factors that promote the growth of normal microflora and suppress the pathogenic one. In the event that breastfeeding was organized incorrectly (and this case, unfortunately, is the most common), if already on the first day after childbirth, before getting to know the maternal microflora, the baby began to receive various liquids through the mouth, colonization of the intestines is far from ideal.
But even in this case, mother's milk will help to cope with problems. The most interesting thing happens when the baby comes home. The normal stool of a breastfed child is liquid, yellow, with white lumps, it can be 7-10 times a day, a little bit, or 1 time in several days, but in large volume. Most often, the chair is 3-5 times a day, in babies in the first months of life. District pediatricians call these normal children's poop diarrhea and send their mother to take a stool test for dysbacteriosis.
The normal stool of a breastfed child is liquid, yellow, with white lumps, it can be 7-10 times a day, a little bit, or 1 time in several days, but in large volume. Most often, the chair is 3-5 times a day, in babies in the first months of life. District pediatricians call these normal children's poop diarrhea and send their mother to take a stool test for dysbacteriosis.
This does not take into account the fact that the baby for the first six months of life has the right to dysbiosis in his intestines and to any stool, especially if he grows and develops well. Then treatment begins, one of the main points of which is the transfer of the child, for example, to fermented milk formula. The pediatricians are not to blame. They are accustomed to the stool of a bottle-fed baby - thicker and more uniform. An even more interesting situation occurs later, when, despite drinking, for example, various biological products, the child continues to inoculate microorganisms that are not suitable for his intestines. In this case, the mother is told that it's all about her milk, and they insist on stopping breastfeeding.
In this case, the mother is told that it's all about her milk, and they insist on stopping breastfeeding.
The following case is indicative in this respect. In a breastfed baby, Candida fungi and hemolyzing Escherichia coli were constantly sown in large quantities. No treatment had any effect on these microorganisms. Mom was told all the time that milk was to blame. Having fed the child up to a year, the mother took him away from the breast. The child began to get sick often, and mushrooms and sticks remained in the same quantities.
Sowing milk for sterility
When sowing milk for sterility, various microorganisms are sown in 50-70% of cases, most often staphylococcus aureus and epidermal. Very often, when these organisms are found, the mother is prescribed a course of antibiotic treatment, at which time the child is fed formula for a week, after which he usually refuses to breastfeed. This is the worst option, but the most common one. Either mother and child begin to be treated using biological products, or mother and child drink chlorophyllipt.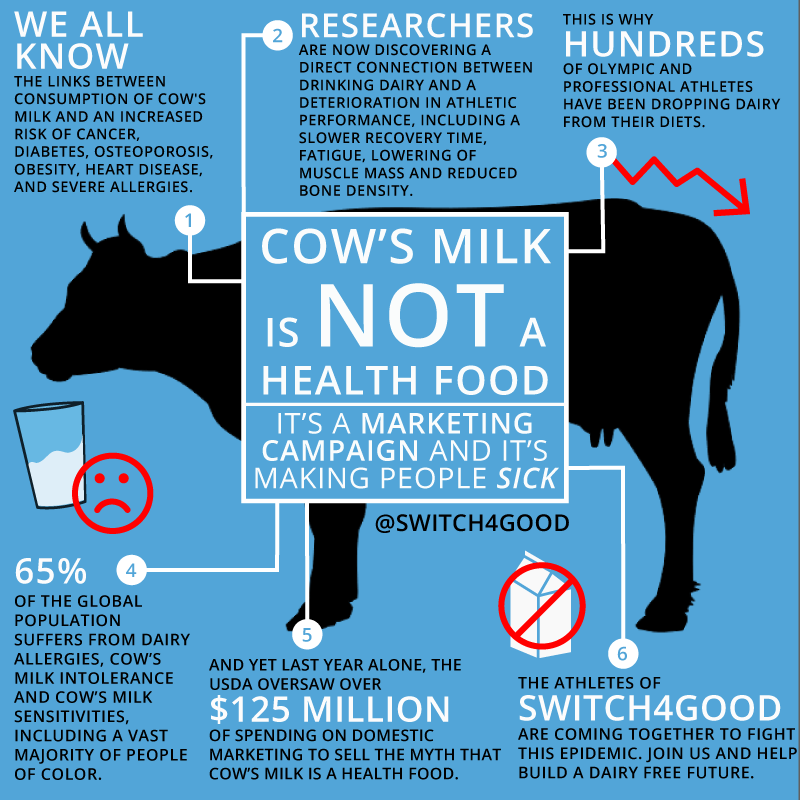 Meanwhile, the presence of staphylococci in milk does not mean anything! Both Staphylococcus aureus and epidermal Staphylococcus aureus live on human skin, and are also found on most of the surrounding objects. For example, staphylococcus has a tropism for cotton fabric. When moving a stack of diapers, the number of staphylococci in the air increases dramatically! Together with mother's milk, the child receives specific antibodies that help him cope with staphylococcus aureus if necessary.
Meanwhile, the presence of staphylococci in milk does not mean anything! Both Staphylococcus aureus and epidermal Staphylococcus aureus live on human skin, and are also found on most of the surrounding objects. For example, staphylococcus has a tropism for cotton fabric. When moving a stack of diapers, the number of staphylococci in the air increases dramatically! Together with mother's milk, the child receives specific antibodies that help him cope with staphylococcus aureus if necessary.
It turns out that mother's milk staphylococcus comes to the child along with protection from it. It is not dangerous for the child! Moreover, the child needs, in the first hours after childbirth, to be populated by his mother's staphylococcus aureus. From this staphylococcus, he will be protected by his mother's antibodies, which he will receive with colostrum and milk, and which he has already received transplacentally! The entire microflora of the mother's body is already "familiar" to the child's immune system, thanks to antibodies penetrating the placenta. It is dangerous for a child to be populated by the microflora of the maternity hospital, including hospital strains of staphylococcus resistant to antibiotics! He is not familiar with these microorganisms and their colonization of his skin and gastrointestinal tract is dangerous for the baby. If a child does not have the opportunity to "populate" with his mother's microflora, he is populated by what is around. As they say, a holy place is never empty. If it is not possible for a “home” strain of Staphyloccocus aureus to settle on an infant, a hospital strain will take its place. But this is not scary for a breastfed child, the mother's body, by producing appropriate antibodies, will help the child. Unless, of course, in the life of a child there will be a place for breastfeeding.
It is dangerous for a child to be populated by the microflora of the maternity hospital, including hospital strains of staphylococcus resistant to antibiotics! He is not familiar with these microorganisms and their colonization of his skin and gastrointestinal tract is dangerous for the baby. If a child does not have the opportunity to "populate" with his mother's microflora, he is populated by what is around. As they say, a holy place is never empty. If it is not possible for a “home” strain of Staphyloccocus aureus to settle on an infant, a hospital strain will take its place. But this is not scary for a breastfed child, the mother's body, by producing appropriate antibodies, will help the child. Unless, of course, in the life of a child there will be a place for breastfeeding.
The presence of staphylococcus in milk does not affect its quality in any way. Staphylococcal enterocolitis, which is often used to scare mothers, convincing them to stop feeding their “poisonous” milk, is an extremely rare condition that occurs with diseases of the immune system, and which is facilitated by artificial feeding! It must be assumed because even if the baby, for some internal reasons, has weakened immunity, he will still receive significant support with mother's milk.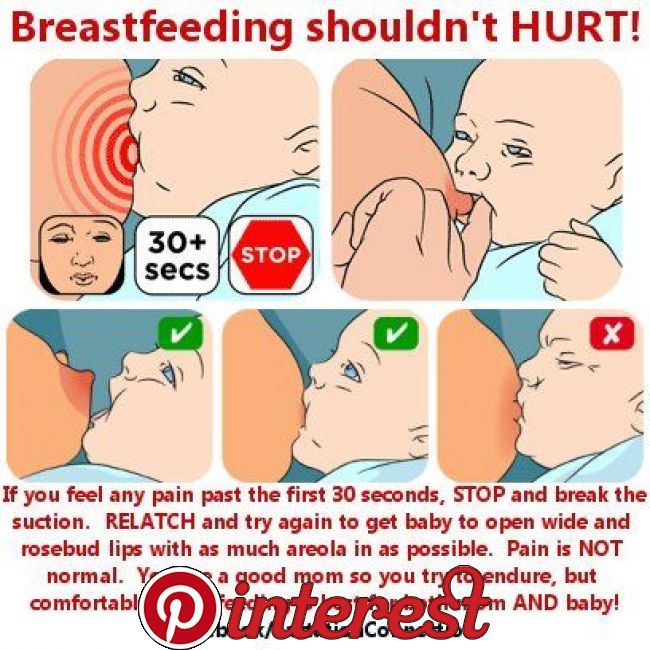 When transferred to artificial feeding, he loses this support.
When transferred to artificial feeding, he loses this support.
Appeal to pediatricians
Dear colleagues! If the somatically healthy breastfed child you are observing is not gaining weight well, has green, unstable stools, skin problems, before transferring him to artificial feeding, prescribing an examination and treatment, try to find out if breastfeeding of this child is properly organized. baby? Breastfeeding is a very simple process, if not elementary. But! Only if the breastfeeding mother follows a few simple rules and actions.
These rules and practices related to the culture of motherhood have been widely known and used for thousands of years. And now almost lost. Without knowledge of these rules, full breastfeeding cannot take place.
If a mother feeds her baby 6-7 times a day, uses a pacifier, gives her baby tea or water to drink, expresses herself, does not feed her at night, she performs actions for which neither the child nor she herself is designed by nature. It is impossible to establish a natural process by acting unnaturally! If a child has improper attachment to the breast, and no one notices this, this is very sad, because. nature did not expect that a woman starting to feed would not accumulate experience of observing other nursing women throughout her life and would not have an experienced mother nearby who could correct her.
It is impossible to establish a natural process by acting unnaturally! If a child has improper attachment to the breast, and no one notices this, this is very sad, because. nature did not expect that a woman starting to feed would not accumulate experience of observing other nursing women throughout her life and would not have an experienced mother nearby who could correct her.
Without proper latching, there will not be sufficient stimulation of the breast to produce the required quantities of milk, even with frequent feedings, and a baby with improper latching will find it difficult to extract “hind”, fatty, thick milk from the breast! In such a situation, it is necessary to teach mother and child how to properly attach to the breast, establish frequent feedings at the request of the child, exclude the use of other oral objects and supplementation, establish full-fledged night feedings, and eliminate pumping, if any. Look at the baby again after 2-4 weeks. AT 9In 9% of cases, neither artificial nutrition, nor examination, nor treatment will be needed for the child.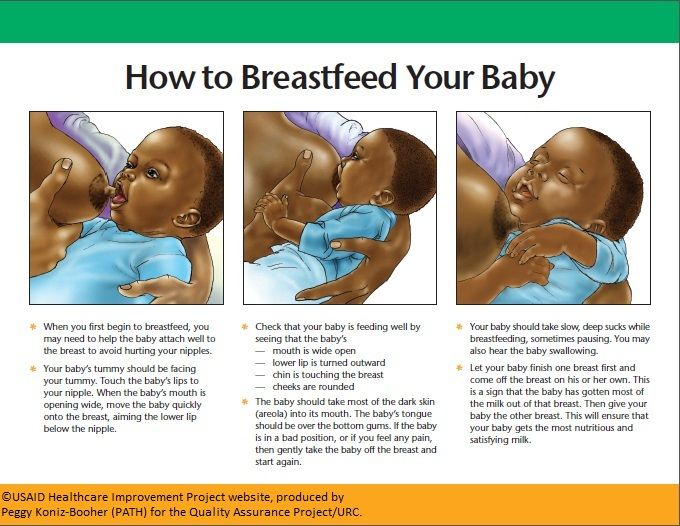
Author: Lilia Kazakova, pediatrician,
Head of Breastfeeding and Child Care Counseling Services
Breastfeeding and Lactose Intolerance
Infant formula companies like to use this label to their advantage, such as in ads for Similac Sensitive®: For Restless Behavior and gas formation caused by lactose intolerance. Many children sometimes act up and suffer from colic. But if it seems to you that whims and bloating have become more frequent, this may be a sign that the baby needs a different milk formula. You can trust Similac Sensitive to start effective development of your children's digestive systems."
In fact, you can't trust the advice of infant formula companies about breastfeeding, as it's in their best interest to have a mother replace her breast milk with artificial formula. Would you go to a tobacco company for advice on how to quit smoking? Probably not.
Many newborn babies spit up and suffer from colic because their digestive system is still immature, it has just begun the transition from intrauterine nutrition (where it received nutrients through the placenta) to self-digestion of milk.
Starting with a small amount of colostrum, it is easier for a newborn's digestive system to accept more breast milk later on. After the milk has “come”, the next step in the nursing mother is transitional milk (a mixture of colostrum and milk), and a little later mature milk, about 7-10 days after the birth of the baby.
Although breast milk is much easier to digest than formula milk, occasional regurgitation, restless behavior and gas are to be expected in all newborns, whether breastfed or formula fed. Many mothers worry about their babies having frequent watery stools, but this is normal for exclusively breastfed babies.
In addition to an immature digestive system, regurgitation and gas, and even burping, can also be caused by supplements such as fluoride or iron, or gastrointestinal illnesses (eg, stomach flu).
Mothers of babies with gas go to the doctor with questions about how to avoid bloating or spitting up, and in most cases doctors are unable to give an answer. Doctors simply hate these kinds of questions, because for most of them they cannot give an exact answer: what caused it and how to treat it. Unhappy baby - unhappy parents, especially if they see that they can do nothing to improve his well-being.
Doctors simply hate these kinds of questions, because for most of them they cannot give an exact answer: what caused it and how to treat it. Unhappy baby - unhappy parents, especially if they see that they can do nothing to improve his well-being.
Over time, most children's digestive system matures and they outgrow the symptoms - some sooner, some later, but most by 3-4 months. Of course, when your child is ill or in pain, even a couple of minutes seem like an eternity.
What you need to know about breastfeeding and lactose intolerance:
Lactose is a sugar found in all dairy products, including breast milk and formula.
Lactose intolerance is caused by a lack of the enzyme lactase, which breaks down lactose (milk sugar) for easier digestion in the intestines.
All babies are already born with lactose in their intestines. As they grow and are weaned, the amount of the lactase enzyme decreases. This is why sometimes lactose intolerance can show up before the age of 3-4 years, because around this age weaning is natural.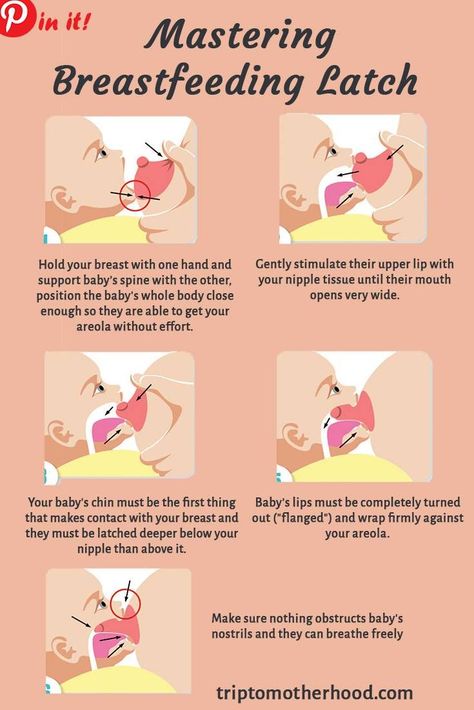
"Primary lactose intolerance" is the inability to digest the lactose found in all dairy products, including both breast milk and formula. This deviation is very rare and is congenital. It is estimated that only 1 in 85,000 children is born with galactosemia. Children with this genetic disorder can become overweight, dehydrated, and unhealthy from the start. They need to be fed a dairy-free formula in order to develop normally.
There is another, much more common type of lactose intolerance called Secondary Lactose Intolerance. Gastrointestinal diseases such as stomach flu (more common among formula fed babies) can cause diarrhea that irritates the stomach lining. This inflammation can cause a temporary decrease in lactase production.
This type of temporary lactose intolerance continues until the child's stomach lining recovers.
No matter what a breastfeeding mother eats or drinks, her breast milk will contain the same amount of lactose.
Most exclusively breastfed infants regulate their milk intake and do not overfeed, but they may become lactose overloaded due to excess milk in the mother.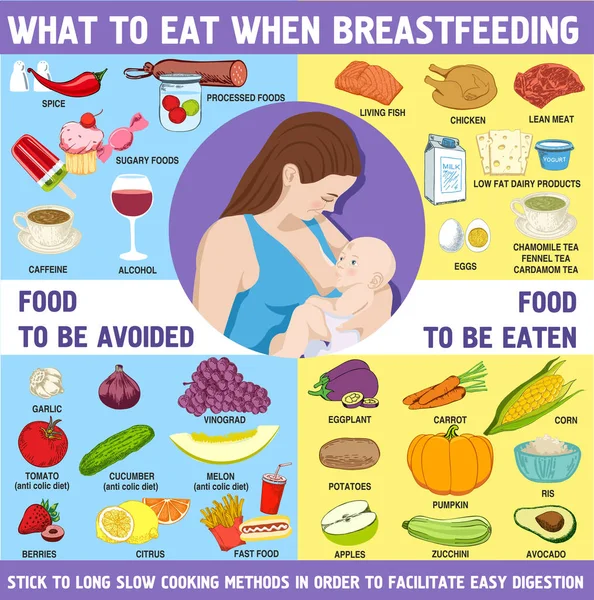 The problem is not the lactose in milk itself - the fact is that the baby eats more milk (and therefore more lactose) than his digestive system can process. This can lead to an imbalance of "front" and "hind" milk.
The problem is not the lactose in milk itself - the fact is that the baby eats more milk (and therefore more lactose) than his digestive system can process. This can lead to an imbalance of "front" and "hind" milk.
Lactose intolerance is a term widely used to encourage breastfeeding mothers to switch to formula, but in reality, very few are lactose intolerant.
When you are told that your baby is "lactose intolerant", think twice before switching to formula. Formula milk companies are very quick to play on the mother's fears by convincing them that their products are healthier for the baby. Remember, it's in their best interest to discourage breastfeeding and promote their products.
I recently saw a very expensive can of formula in a grocery store. The label said "breast milk based".
This already says something.
The buyer needs to be careful, especially when it leads to a decision that will deprive your child of many of the scientifically proven benefits of breastfeeding.