Blood clot and miscarriage
Blood Tests for Miscarriage Risk
When they can help—and when they don’t
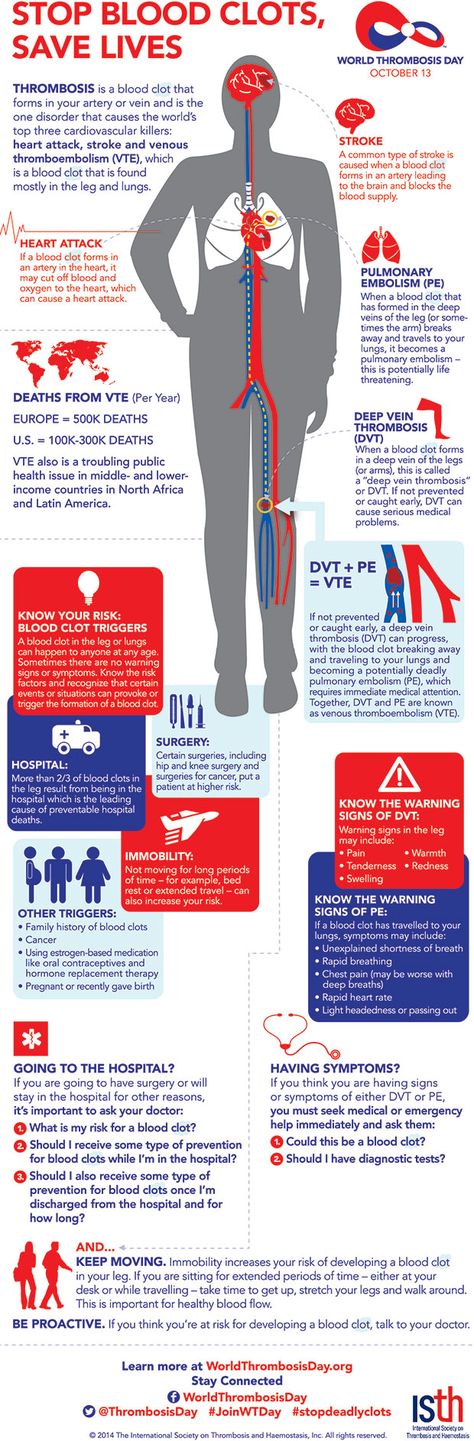
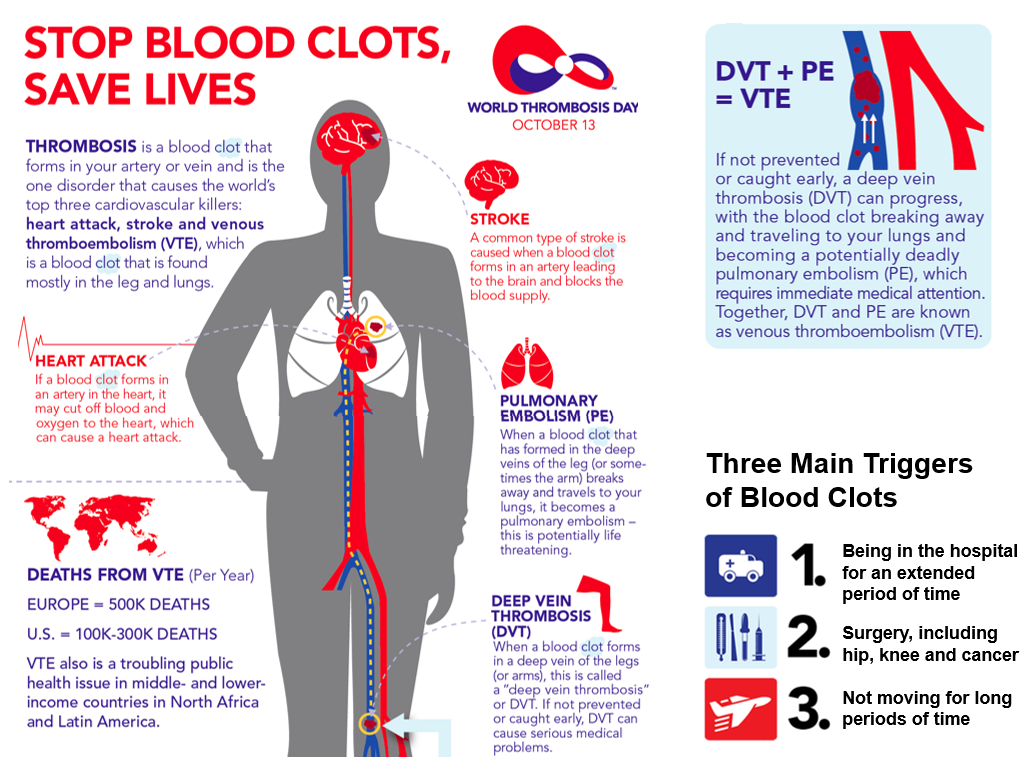
Blood tests to show your risk of miscarriage have become more common. The tests show if you have a condition called “thrombophilia.” This condition can increase blood clots. It may increase the risk of a miscarriage or other problems during pregnancy.
There are many different tests for thrombophilia. Doctors often order the tests for pregnant women who have had problems—such as miscarriage, a sharp rise in blood pressure (pre-eclampsia), or a baby that did not develop normally.
But often, tests are not needed. Even if you have had a pregnancy problem, you may not need any of these tests. Here’s why:
The test results are not always useful.
Usually, the test results do not help you and your doctor make decisions about your care.
For example, some blood tests look for certain genes. The genes can increase the risk of blood clots. But the genes do not increase your risk of miscarriage or other problems in pregnancy. Often, thrombophilia is mild and does not cause any problems. Many women who have it go on to give birth to healthy babies.
The tests can lead to unnecessary treatments and risks.
If the test shows that you have thrombophilia, your doctor may want you to take a drug called heparin during your pregnancy. This drug is injected and helps prevent blood clots.
But it is not clear that this drug lowers the risk of miscarriage or other problems. Also, the injections can cause side effects, such as heavy bleeding and allergic reactions.
The tests can be a waste of money.
The blood tests can cost $1,000 or more. Some health plans don’t pay for them. And you may also waste a lot of money on unneeded treatments. Heparin, for example, can cost hundreds of dollars, too.
Most people don’t need the tests.
You do not need to get tested just because you’ve had a miscarriage or pregnancy complication in the past. There are more effective ways to reduce your risks.
There are more effective ways to reduce your risks.
Consider a thrombophilia test if:
- You have had a blood clot in a vein deep in the body (a deep vein thrombosis).
- You have had a clot that traveled to a lung for no known reason (a pulmonary embolism).
- You have had three or more miscarriages. In this case, you should consider being tested for a form of thrombophilia called “antiphospholipid syndrome.” This syndrome increases the risks of miscarriage, poor growth of the fetus, and pre-eclampsia. This syndrome can be treated with aspirin and heparin. In this case, the test and treatment have more benefits than risks.
This report is for you to use when talking with your health-care provider. It is not a substitute for medical advice and treatment. Use of this report is at your own risk. © 2018 Consumer Reports. Developed in cooperation with the Society for Maternal-Fetal Medicine.
01/2015
Thrombophilias & Recurrent Miscarriage: University Reproductive Associates (URA): Reproductive Endocrinologists
Thrombophilias & Recurrent Miscarriage: University Reproductive Associates (URA): Reproductive EndocrinologistsThrombophilias are a group of clotting disorders that predispose individuals to inappropriate blood clot formation.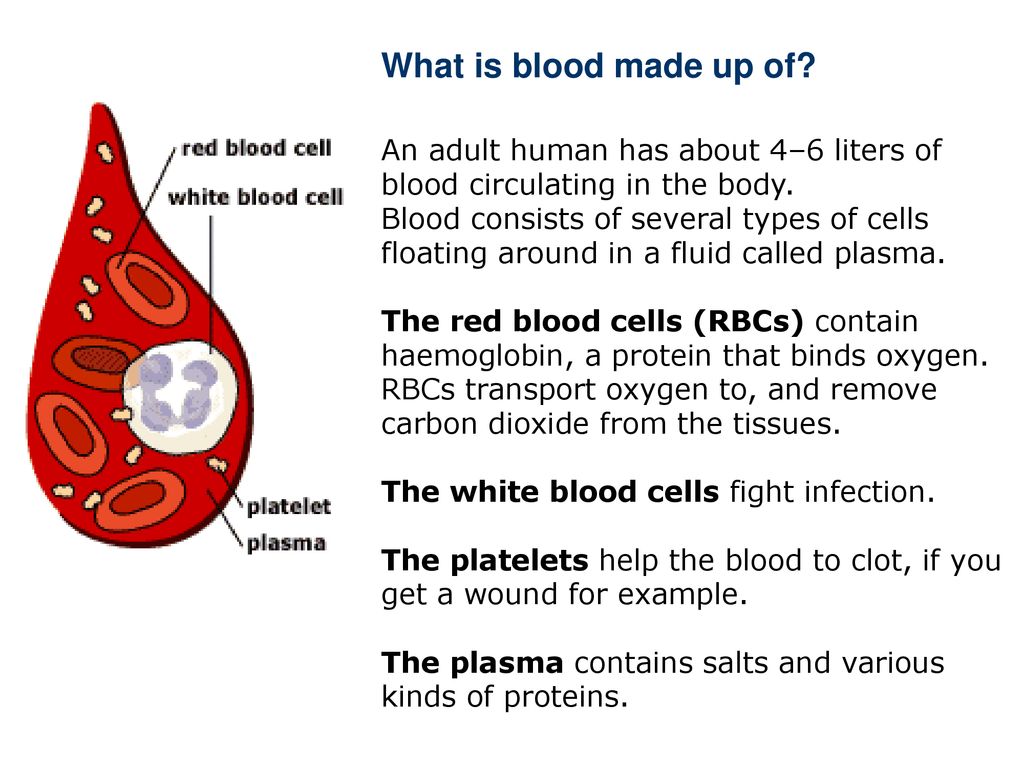 These disorders can lead to health problems and recurrent miscarriage.
These disorders can lead to health problems and recurrent miscarriage.
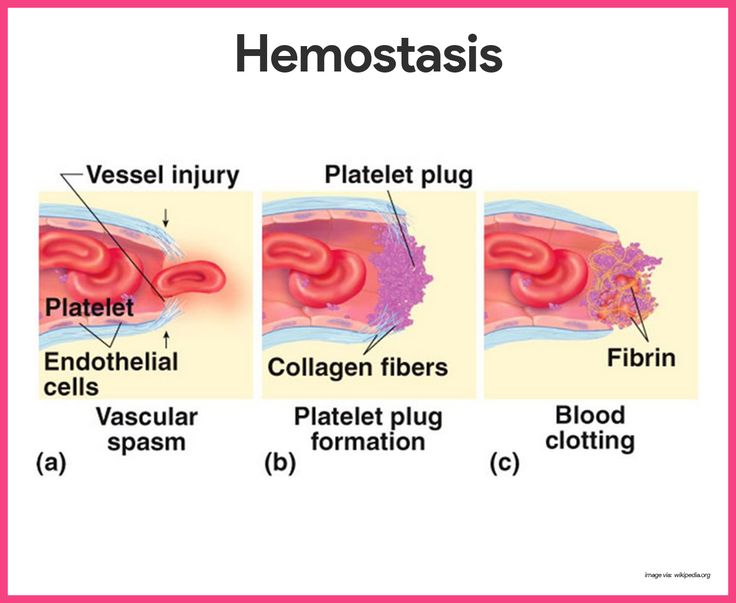
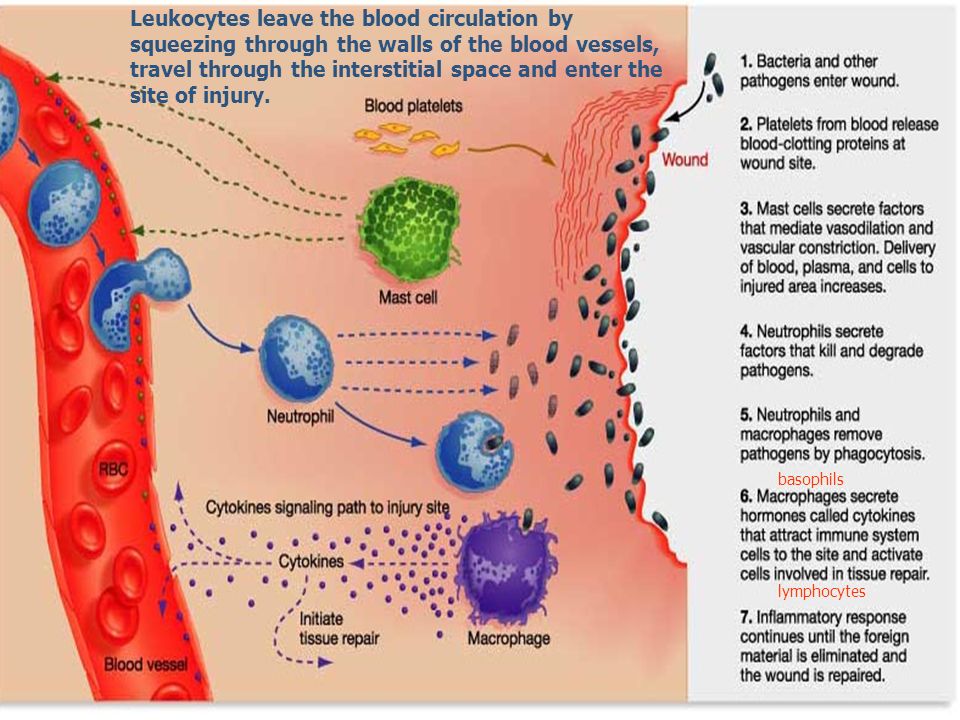
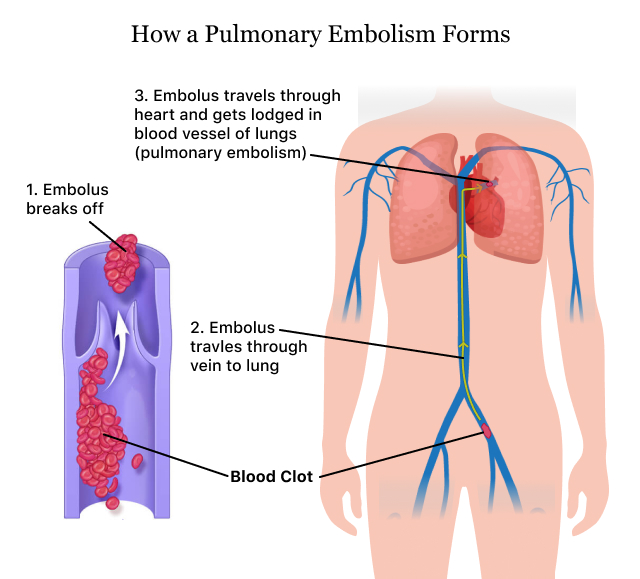
Thrombophilias increase the risk of developing thromboembolism, or blood clots. These clots block the blood vessels throughout the body. If the clots travel to the brain, they can lead to stroke. Those that move to the lung results in a pulmonary embolism.
In women who are pregnant, thrombophilias can cause pregnancy complications or loss including:
- First-trimester miscarriage
- Stillbirth
- Placental abruption (a condition where the placenta pulls away from the uterine wall)
- Preeclampsia
- Fetal growth problems
These conditions occur when blood clots develop obstructing blood vessels in the placenta and interfering with blood flow to the fetus.
During normal pregnancy, even women without thrombophilia are more likely to develop a venous thrombosis (blood clot in the leg) because of the changes that take place in the blood clotting system that help to prevent severe blood loss during childbirth.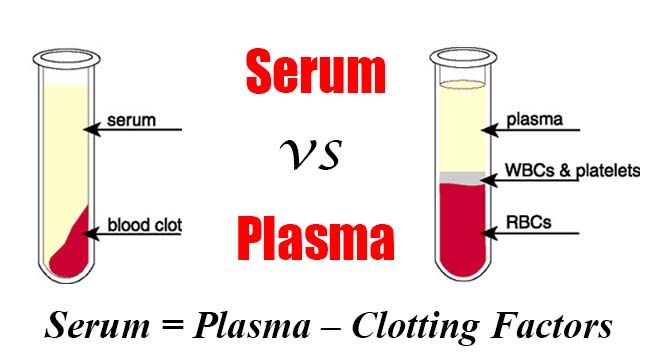
TYPES OF THROMBOPHILIAS
Thrombophilias can be acquired or inherited. Acquired thrombophilias may be associated with certain medical conditions that cause hypercoagulability of the blood, such as sickle cell anemia, cancer, inflammation or diabetes.
Antiphospholipid syndrome (APS) is an autoimmune system disorder linked to excessive clotting of the blood. In those who suffer from autoimmune disorders, the body cannot distinguish between normal tissues and harmful bacteria, viruses, toxics and other foreign substances. It responds by attacking its own healthy tissue. Women who test positive for antiphospholipid antibodies (APLA) have been shown to be at risk for developing blood clots in both the veins and arteries.
INHERITED THROMBOPHILIAS
Those with genetic or hereditary thrombophilias have a predisposition to blood clotting and are at a greater risk of developing blood clots in veins throughout the body. These conditions also increase the risk of miscarriage or other pregnancy complications such as miscarriage, poor fetal growth, and fetal loss.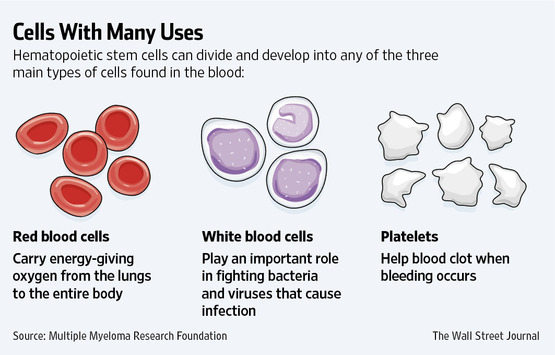
INHERITED THROMBOPHILIAS INCLUDE THE FOLLOWING:
- Factor V Leiden Mutation – the most common of the inherited thrombophilias those with this condition have a resistance to the action of activated protein C
- Prothrombin G20210A Mutation – this mutation of this particular gene leads to increased levels of plasma prothrombin, increasing the risk of venous thromboembolism
- Antithrombin deficiency – this rare condition blocks clotting factors impacting coagulation and increasing the chance of developing blood clots
- Protein S/Protein C deficiency – rare inherited thrombophilias caused by too little-activated protein C or protein S
LINK BETWEEN THROMBOPHILIA & RECURRENT MISCARRIAGE
There is evidence to support a link between APLAs and recurrent fetal loss less than ten weeks.
Women with congenital or acquired antithrombin deficiency are at extremely high risk for developing clots during pregnancy or after delivery.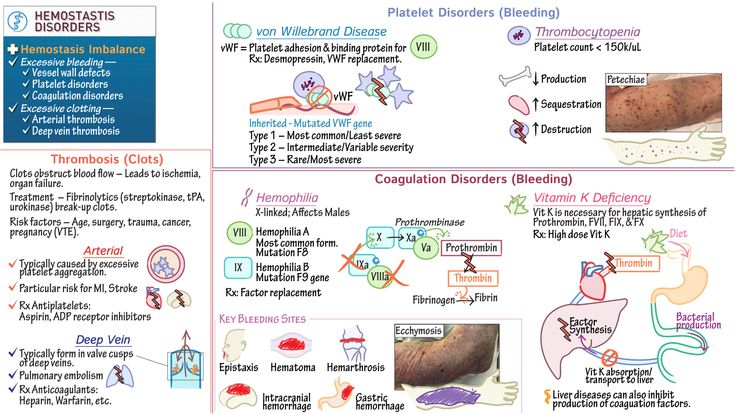 Without treatment, the risk of pregnancy loss is also slightly increased and is usually due to blood clots that develop in the placenta, depriving the fetus of blood and oxygen.
Without treatment, the risk of pregnancy loss is also slightly increased and is usually due to blood clots that develop in the placenta, depriving the fetus of blood and oxygen.
MANAGING THROMBOPHILIA IN PREGNANCY
Heparin (a medication that helps to prevent the formation of blood clots) injections may be recommended for pregnant women diagnosed with antithrombin deficiency due to the increased risk of miscarriage.
A low-dose aspirin regimen may also be prescribed during pregnancy and for a few weeks after delivery.
A carefully prescribed treatment regimen can reduce the risk of miscarriage and other pregnancy complications.
Contact your local URA clinic in Hasbrouck Heights, Hoboken, and Wayne, NJ for more information. Your friendly URA team will be happy to provide more details on thrombophilias and discuss treatment options.
Becoming Two Dads: Understanding Your Fertility Treatment Options
Family planning with two fathers requires a bit of help.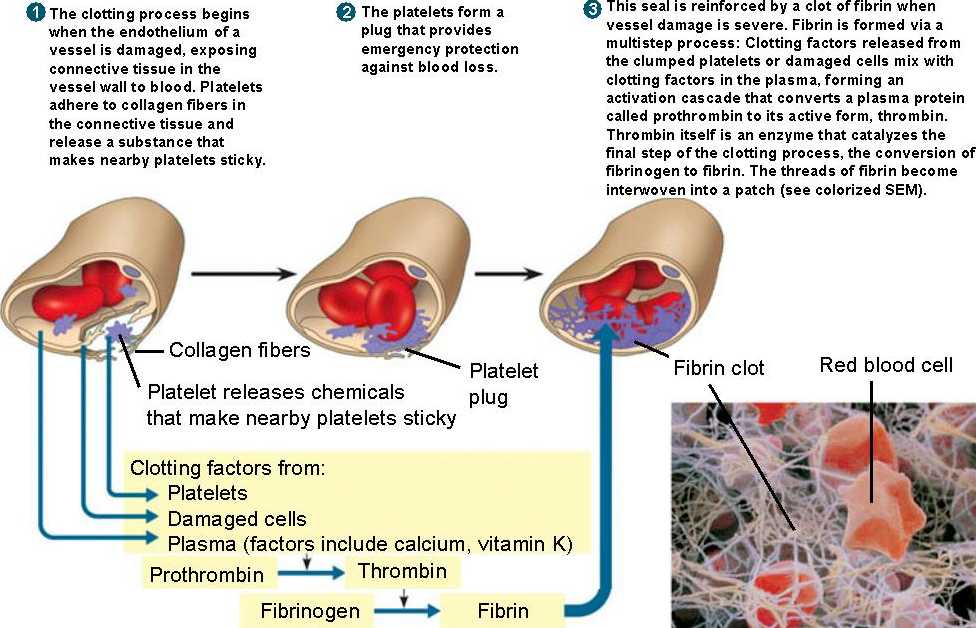 With a team of understanding and compassionate specialists in your corner, you can begin building your family right away. Read on to learn more.
With a team of understanding and compassionate specialists in your corner, you can begin building your family right away. Read on to learn more.
10 Steps to IVF
Infertility issues, same sex partnerships, and genetic concerns can all lead an individual or couple to seek IVF. This common process has 10 steps and a high success rate. Read on to learn more.
2 Ways to Induce Ovulation
When infertility issues arise, your brain may immediately rush to solutions, such as surrogacy or adoption. There are other solutions — ovulation induction could be all you need to get pregnant. Read on to learn more.
Does Endometriosis Resolve on Its Own?
Endometriosis is an under-researched and chronic condition that affects millions of women. Getting a diagnosis can be difficult, and obtaining treatment can feel even harder.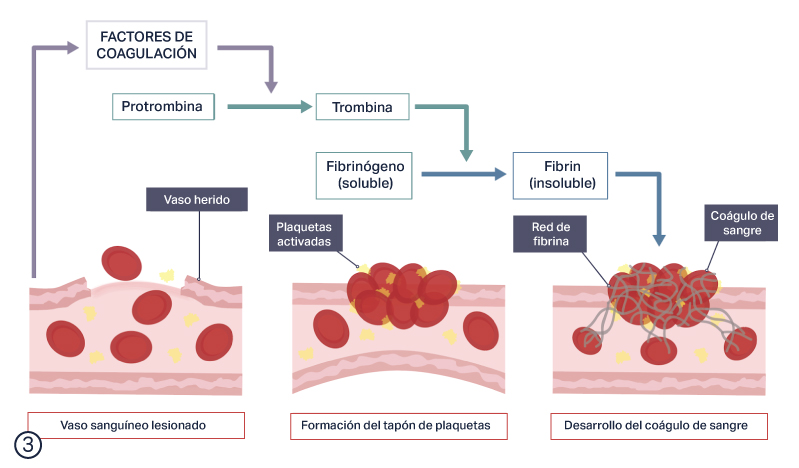 Read on to learn if endometriosis can resolve on its own.
Read on to learn if endometriosis can resolve on its own.
What's Making Me Gain Weight?
When diet and exercise can’t seem to stop weight gain, it’s time to look deeper for a more insidious cause. For women, that can mean the reproductive system. Read on to learn more.
How to Manage the Skin Symptoms of PCOS
Is PCOS affecting your skin? Many women find that the visible side effects of PCOS are apparent on their faces and bodies. Fortunately, there are solutions that can help. Read on to learn more.
What is a spontaneous miscarriage and how does it happen? It's unpleasant and painful. But why is this happening and how to avoid such situations in the future? Find out more about this later.
What is it?
Early miscarriage is the death of an embryo or fetus in the womb before the 22nd week of pregnancy. It is usually caused by genetic breakdowns, pathologies, injuries or stress. Such a nuisance is quite common and approximately 15-20% of all successful conceptions can end in miscarriage.
It is usually caused by genetic breakdowns, pathologies, injuries or stress. Such a nuisance is quite common and approximately 15-20% of all successful conceptions can end in miscarriage.
What are the signs of a miscarriage?
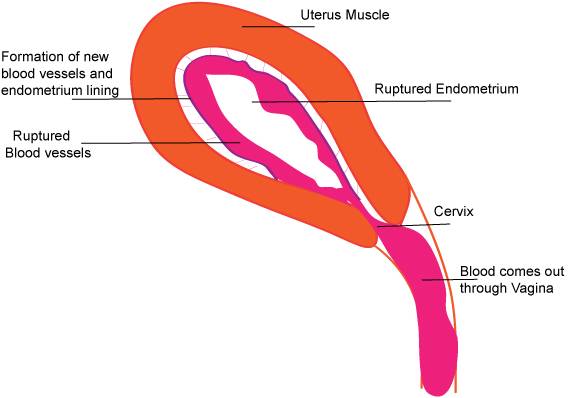
To understand what's going on, you need to understand what a miscarriage looks like. The most common symptom is profuse bleeding with clots. Sometimes they can be mild at first, and then quite large. You should monitor your condition and if at least a slight bleeding has begun, you should immediately consult a doctor.
Sometimes a miscarriage can start suddenly. But it happens that before this there may be small pulling pains in the lower abdomen, lower back, smearing brown discharge.
Women may not immediately realize that they have had a miscarriage. Especially if the delay is only a few days, and the test was not done, then you might think that your period just started.
But usually a woman who already knows about her pregnancy remembers how a spontaneous miscarriage occurs forever.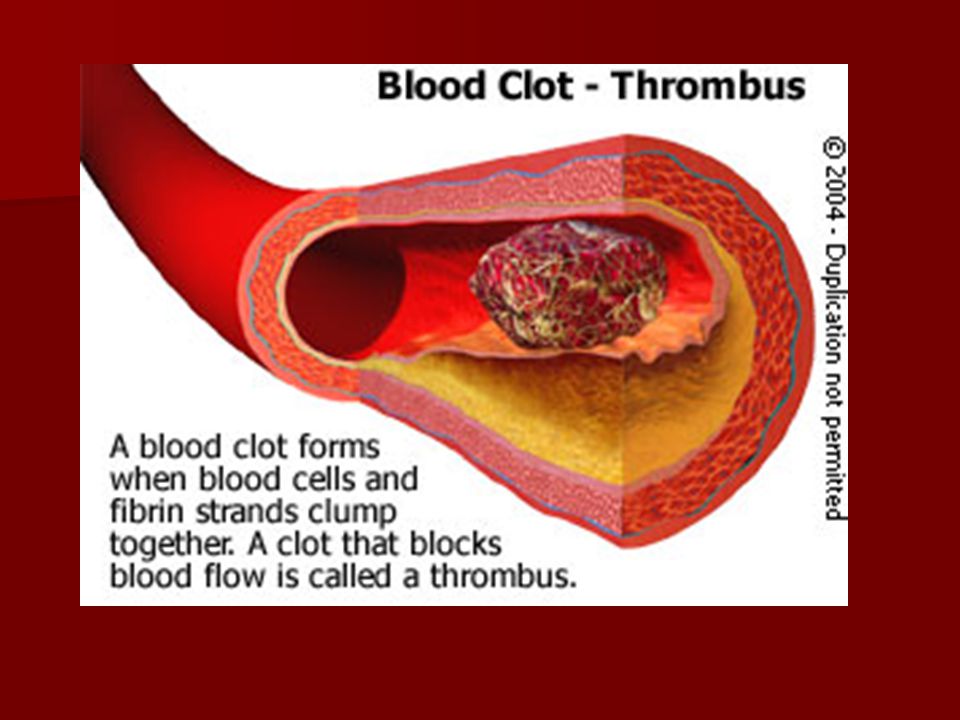 In most cases, this is profuse bleeding with blood clots, mucus and severe pain in the abdomen. If you do not immediately take action, you may experience chills, fever, the skin will become pale. The patient may even lose consciousness. If a woman does not immediately see a doctor or call an ambulance, she may even die from blood loss, as sometimes such bleeding is incredibly serious.
In most cases, this is profuse bleeding with blood clots, mucus and severe pain in the abdomen. If you do not immediately take action, you may experience chills, fever, the skin will become pale. The patient may even lose consciousness. If a woman does not immediately see a doctor or call an ambulance, she may even die from blood loss, as sometimes such bleeding is incredibly serious.
Spontaneous miscarriage can also have symptoms such as nausea, vomiting, frequent urination, dizziness, weakness,
What can cause an early miscarriage?
Why does it happen that a miscarriage occurs? Here you can name many reasons, but in each case, studies are carried out, the patient takes tests.
The causes of spontaneous abortion may be as follows in the first trimester:
- Increased contractile activity of the uterus, which literally "pushes" the fetus.
- Genetic abnormalities in the fetus. Sometimes this happens once in one woman, as a result of genetic "breakdowns".
 And it happens that the whole thing is in the genes of the future father and mother, and therefore it is necessary to look for problems together with a geneticist.
And it happens that the whole thing is in the genes of the future father and mother, and therefore it is necessary to look for problems together with a geneticist. - Deficiency of the hormone progesterone. This is the so-called "pregnancy hormone". If it is not enough, then it is appointed additionally.
- Immunological disorders that prevent normal development of the embryo.
- Intoxication.
- In the second trimester, the causes of miscarriage may be slightly different:
- Uterine fibroids.
- Adhesions in the pelvic organs.
- Polyps in the uterus that do not allow the embryo to develop normally.
- Endometriosis, which causes connective tissue to grow outside the uterus.
- Pathology of the cervix, namely an open cervix, which does not allow carrying a child and giving birth to it at term.
- Infections that can cross the placenta and cause fetal death.
- Some chronic diseases of the mother.
But besides this, there may be many other specific reasons that are individual for each woman. For example, hard physical work, activities in hazardous enterprises, severe stress and anxiety can also cause spontaneous abortion. The threat of spontaneous miscarriage occurs in many women, but not everyone can have an abortion. Much depends on the state of health, immunity, even emotional state.
For example, hard physical work, activities in hazardous enterprises, severe stress and anxiety can also cause spontaneous abortion. The threat of spontaneous miscarriage occurs in many women, but not everyone can have an abortion. Much depends on the state of health, immunity, even emotional state.
What types of miscarriage can there be?
There are several types of spontaneous abortions:
- Early (up to 12 weeks)
- Late (13-22 weeks).
Some other types can also be distinguished:
- Threatened miscarriage. It is manifested by slight pains in the abdomen, spotting spotting, the muscles of the uterus are quite active. But at the same time, the cervix is closed.
- Incipient miscarriage. There is detachment of the fetal egg, bloody discharge. The cervix is closed, but the internal os is open.
- Abortion in progress. The fertilized egg comes out of the uterus, it is in the cervical canal. Severe pain and bleeding begin.
- Incomplete abortion. Part of the egg may come out of the uterus, and part may still be in it. In this case, there is severe bleeding, abdominal pain, shock may develop
- Complete abortion. With it, the fetal egg completely leaves the uterus. This is a "mini childbirth", while there is a slight bleeding, abdominal pain.
- Missed abortion. With it, the fetal egg remains in the uterus. In this case, the fetus is already dead. Such an egg can remain inside a woman for some time, her condition worsens, signs of pregnancy disappear.
Also, such miscarriages can be divided into several types:
- Interrupted biochemical pregnancy. It happens for 1-3 weeks. But a woman usually perceives it as the beginning of menstruation.
- Spontaneous miscarriage (up to 22 weeks).
- Preterm birth (after 22 weeks).
What cannot cause a miscarriage
Spontaneous abortion can happen to every woman. But there are certain risk factors that by themselves cannot cause a miscarriage, but can be provocateurs:
- Smoking.
- Alcohol abuse.
- Some disease (diabetes mellitus, high blood pressure).
- Age over 35.
Diagnosing a miscarriage
In order to accurately understand that a spontaneous abortion has occurred, it is necessary to correctly diagnose it. To do this, you should:
- Analyze the patient's complaints. Usually this is bleeding, pain and cramps in the abdomen, poor general health, pallor of the skin, fever.
- Perform a gynecological examination. Carry out palpation of the uterus, examination of the cervix, external pharynx.
- Perform colpocytological examination.
- Tests for certain hormones.
- Ultrasound of the pelvic organs is performed.
If such miscarriages occur frequently, the cause must be investigated. To do this, conduct a variety of studies, consultations with geneticists, endocrinologists and other specialists.
How to treat?
How to treat spontaneous miscarriage depends on the type of miscarriage.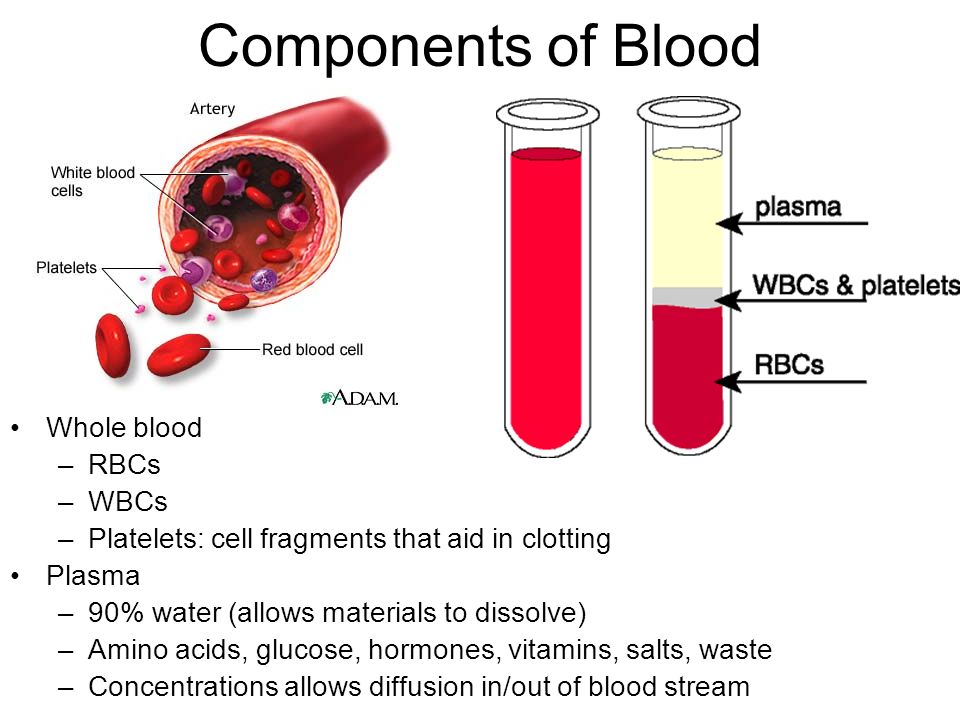 If it is threatening and has begun, then the following should be done:
If it is threatening and has begun, then the following should be done:
- The woman should be in the hospital.
- A diet that contains all the necessary minerals and trace elements.
- The patient must remain in bed.
- Sedative drugs and drugs that relax the muscles of the uterus should be given.
- If an abortion is "in progress", then all measures must be taken to stop the bleeding.
- If the abortion is complete and incomplete, then everything “unnecessary” that is in the uterus should be removed. For this, scraping can be used.
- If there is a failed abortion, then sometimes expectant tactics are used, when they are waiting for everything to “come out of the uterus by itself”. And sometimes they do scraping.
- Also, sometimes with a missed pregnancy, expectant management can be used, especially for nulliparous women. Then after about 4-6 weeks a spontaneous miscarriage can occur. Sometimes drug treatment is used, in which special pills are used to help complete the pregnancy.
 And sometimes they do surgical curettage.
And sometimes they do surgical curettage.
In any case, abortion should not be left to chance, it is necessary to consult a doctor who will choose the treatment tactics.
What are the consequences?
Spontaneous miscarriage in early pregnancy usually carries certain risks. The consequences of spontaneous miscarriage can be different:
- Severe bleeding, pain.
- Infertility.
- But the most difficult and life-threatening miscarriages are those that a woman causes herself, at home. If they are not treated and the consequences are not eliminated, then they can end in the death of a woman.
Usually, if the patient was provided with quality medical care, then there are practically no complications. After about 10 days, the bleeding stops, and after 4 weeks, the woman begins her regular menstruation.
Is there any prevention?
Pregnancy after spontaneous miscarriage can occur and be quite successful.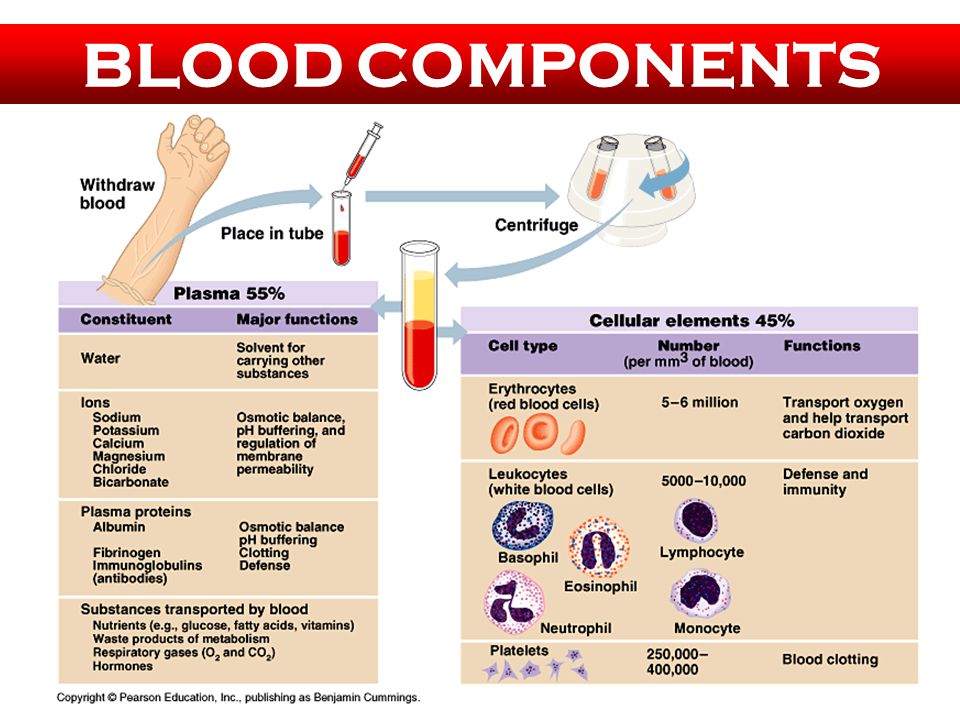 But first you need to establish the cause of the abortion. If these are genetic problems, endocrine pathologies, troubles with the blood or uterus, then special treatment is necessary. But there are general recommendations that will help reduce the risk of miscarriages:
But first you need to establish the cause of the abortion. If these are genetic problems, endocrine pathologies, troubles with the blood or uterus, then special treatment is necessary. But there are general recommendations that will help reduce the risk of miscarriages:
- After an abortion, a woman needs to have a good rest, gain strength, drink a course of vitamins, possibly oral contraceptives, prescribed by a doctor. The next pregnancy is best planned in about 6 months.
- Maintain a healthy lifestyle.
- Do not smoke or drink alcohol.
- Exercise regularly.
- Take vitamins and balanced meals.
- Visit your gynecologist regularly.
- Have fewer stressful situations, give up heavy physical exertion.
- Minimize work with harmful substances, poisons.
- Normalize the weight if it is too small or too large.
- Consultations of a psychologist and a psychotherapist are available.
Spontaneous abortion is an unpleasant phenomenon that can happen to every woman. But it is necessary to carry out the treatment correctly and consult a doctor in time. In addition, preventive measures should be taken.
But it is necessary to carry out the treatment correctly and consult a doctor in time. In addition, preventive measures should be taken.
Spontaneous abortion (miscarriage)
If the pregnancy is terminated naturally before the fetus reaches gestational age, this is called a spontaneous abortion or miscarriage. More than half of miscarriages occur no later than 12 weeks of gestation due to fetal abnormalities. The rest falls on the period up to 20 weeks and is associated with pathologies of pregnancy. If the pregnancy is terminated in the second half, it is called preterm labor.
Spontaneous abortion, otherwise known as miscarriage, is one of the most common complications during pregnancy, accounting for 10-20% of diagnosed pregnancies, and is the rejection of a fetus weighing no more than 500 grams. and less than 22 weeks. Unfortunately, with such indicators, the fetus is not viable. Usually 80% of the total number of spontaneous abortions occurs before the 12th week of pregnancy.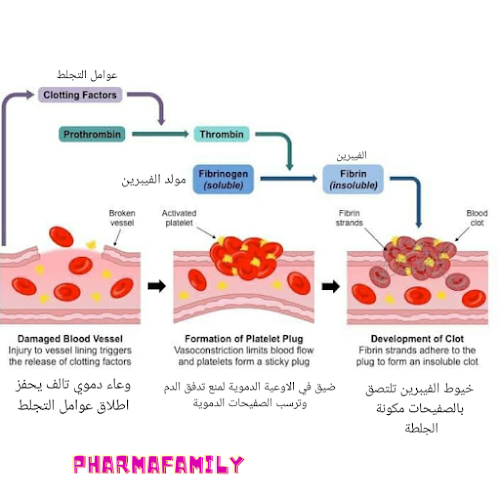
Types of spontaneous abortion
1. Threat of miscarriage - characterized by mild uterine cramps, pulling pain in the lower abdomen and sometimes mild bloody discharge from the vagina.
2. A miscarriage that has begun - is characterized by more severe pain and profuse bleeding. At the same time, the tone of the uterus is slightly increased, and the internal os is closed.
3. Inevitable miscarriage - accompanied by dilatation of the cervix - a fetal egg can be distinguished - with profuse bleeding and severe cramps in the lower abdomen.
4. Incomplete miscarriage - part of the fetus comes out. The bleeding is so profuse that it can lead to the death of a woman.
5. Completed miscarriage - the fetal egg and the fetus itself are completely out. After that, the bleeding and spasms stop.
The etiology of miscarriage is due to many factors. Among them:
- genetic disorders;
- previous induced abortions;
- too little time has passed since the previous pregnancy;
- inflammatory infections in the mother, endocrine disorders;
- blood conflict between mother and fetus;
- taking hormonal contraceptives and certain medications;
- smoking during pregnancy and drinking alcohol;
- unknown causes.
To prevent miscarriage, it is necessary to give up bad habits, not to have abortions and to be regularly examined by a doctor.
Spontaneous abortion begins with the appearance of cramping, drawing pains, similar to pain during menstruation. Then bleeding from the uterus begins. At first, the discharge is slight or moderate, and then, after detachment of the fetal egg, abundant discharge with bloody clots begins. The appearance of these symptoms requires urgent hospitalization.
After examining a woman in a hospital, having determined the degree of detachment of the embryo, one of the following diagnoses will be made:
- the threat of pregnancy - detachment is only outlined or is completely insignificant. In this case, the pregnancy can be saved;
- a miscarriage that has begun - detachment is already quite decent with a pronounced pain syndrome. And in this case, the fetus can be saved;
- abortion in progress - detachment with displacement progresses, labor-like contractions begin.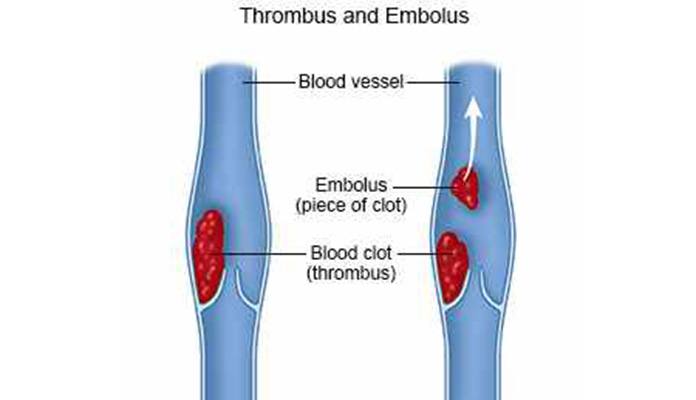 Pregnancy cannot be saved, cleaning is required;
Pregnancy cannot be saved, cleaning is required;
- incomplete miscarriage - independent exit of a part of the fetus and membranes, curettage is necessary for the final curettage of the uterus;
- late abortion - premature delivery of an unviable baby.
After a spontaneous abortion, it is recommended to take a short break in planning and take preventive measures to avoid recurrence.
In case of repeated miscarriage, a thorough comprehensive examination is necessary to determine the causes of miscarriage and eliminate them.
A miscarriage is a severe psychological trauma, especially during the first pregnancy. But do not give up, with a competent approach to planning and bearing, the next pregnancy will certainly end with the appearance of a long-awaited baby.
Causes of spontaneous abortion
1. Doctors call various chromosomal pathologies one of the main reasons: monosomy, autosomal trisomies, polyploidy. They account for 82-88% of spontaneous miscarriages.