Breastfeeding and echinacea
Herbal medicines & breastfeeding | The Royal Women's Hospital
Some complementary and alternative medicines have very good information about their safety and effectiveness while breastfeeding, others have very little because not enough research has been done on them.
Herbal medicines are produced from plants and are based on traditional knowledge. They fall under the umbrella of complementary and alternative medicines (CAM). CAM also include such therapies as acupuncture, dietary supplements, massage, aromatherapy, homeopathy and relaxation therapy.
Herbal and traditional medicines are generally bought from shops such as pharmacies, supermarkets and health food stores. They may have been prescribed by a naturopath, a Chinese doctor or another kind of health provider. While most complementary medicines are used for the relief of symptoms of minor and self-limiting conditions, many are used for maintaining health and wellbeing.
Like conventional medicines, certain herbal and traditional medicines, can transfer into your breast milk. Some herbal and traditional medicines may be harmful to your baby, while others can affect your breast milk production. Unless you or your practitioner are very sure about a product's effect on breastfeeding, it is important that you do not take that product.
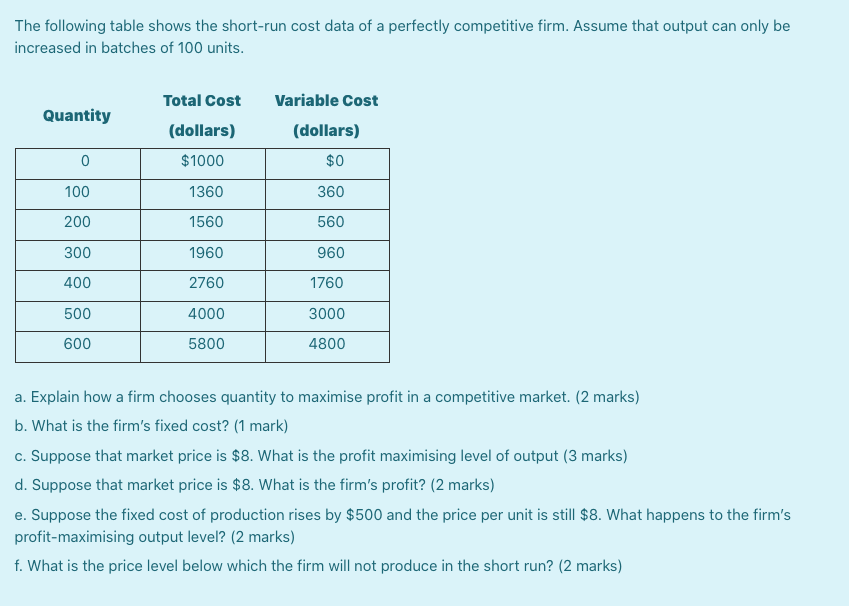
Breast milk is the best nutrient for your baby and has many health benefits for both you and your baby. You should be very careful about what herbal and traditional medicines you use while breastfeeding, especially when your baby is a newborn, or if your baby was born prematurely.
Things to consider
There are concerns around the unregulated use of herbal and traditional medicines in breastfeeding.
-
All herbal and traditional medicines have the potential to pass into breast milk and affect your baby.
-
With most herbal and traditional medicines, there is not enough documented information to determine their safety in breastfeeding.
-
Some herbal and traditional medicines have not been scientifically proven to be effective.

-
Some herbal and traditional medicine products have not been regulated to ensure they are of good quality.
Common herbal and traditional medicines
Aloe vera
Aloe vera gel is used to help heal cracked nipples. Remove aloe gel from the nipple areas before feeding your baby because the bitter taste of the aloe vera gel can affect feeding.
Aloe vera latex is a yellow-coloured liquid that comes from the inner skin of the aloe leaf. It is taken orally in both the dried and liquid form. Avoid taking aloe vera latex as it has a strong laxative effect.
Cranberry
Cranberry may be used to prevent urinary tract infections in breastfeeding mothers. There is no information on the safety and efficacy of the medicine in breastfeeding, but is considered safe to use at the recommended doses.
Echinacea
Echinacea has been commonly used to treat or prevent upper respiratory tract infections. There is no information about the safety and efficacy of echinacea in breastfeeding.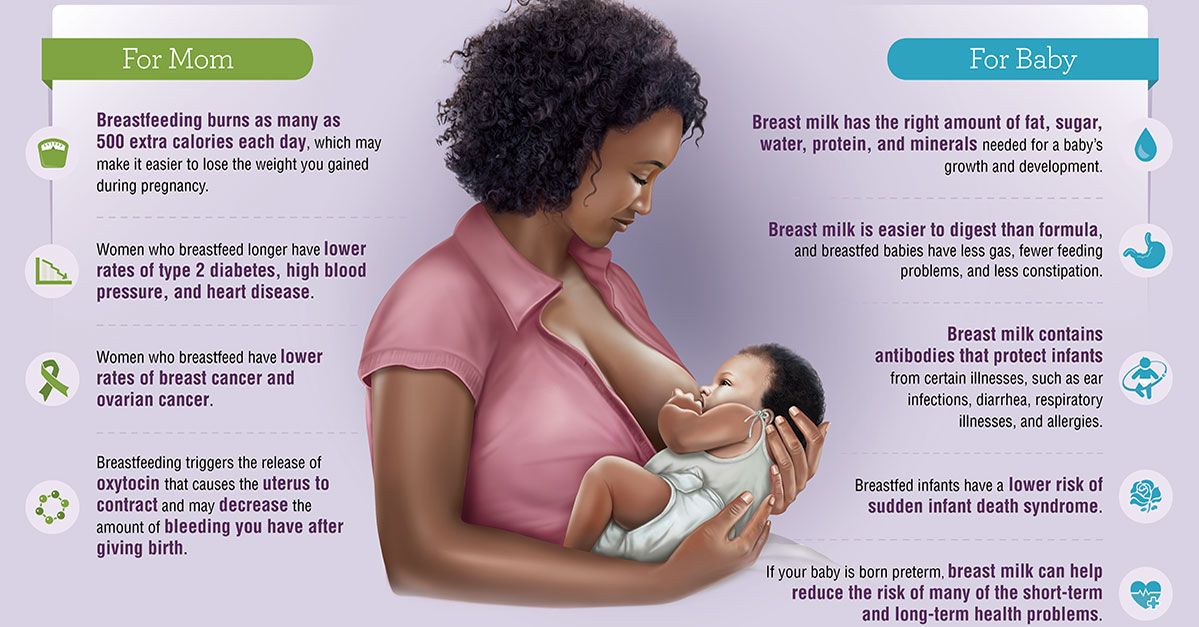 If you take echinacea while breastfeeding, watch for possible side effects in your baby, such as diarrhoea or constipation, poor feeding and skin rashes.
If you take echinacea while breastfeeding, watch for possible side effects in your baby, such as diarrhoea or constipation, poor feeding and skin rashes.
Fenugreek
Traditionally, fenugreek is used to increase milk supply. The transfer of fenugreek into breast milk is unknown and unusual side effects such as allergy, colic, abdominal discomfort and diarrhoea have been reported in babies. Also, there is the potential for fenugreek to interact with other medicines.
Garlic
Garlic appears to be safe in amounts usually used in food preparation. Garlic may change the smell of breast milk and affect your baby’s feeding. There is no information on the safety of garlic supplements in breastfeeding.
Ginger
Ginger appears to be safe in amounts usually used in food preparation. Avoid using large amounts as there is not enough information available about the safety of ginger while breastfeeding.
Milk thistle
Avoid using milk thistle because there is no information on the safety of this traditional medicine when used by breastfeeding mothers.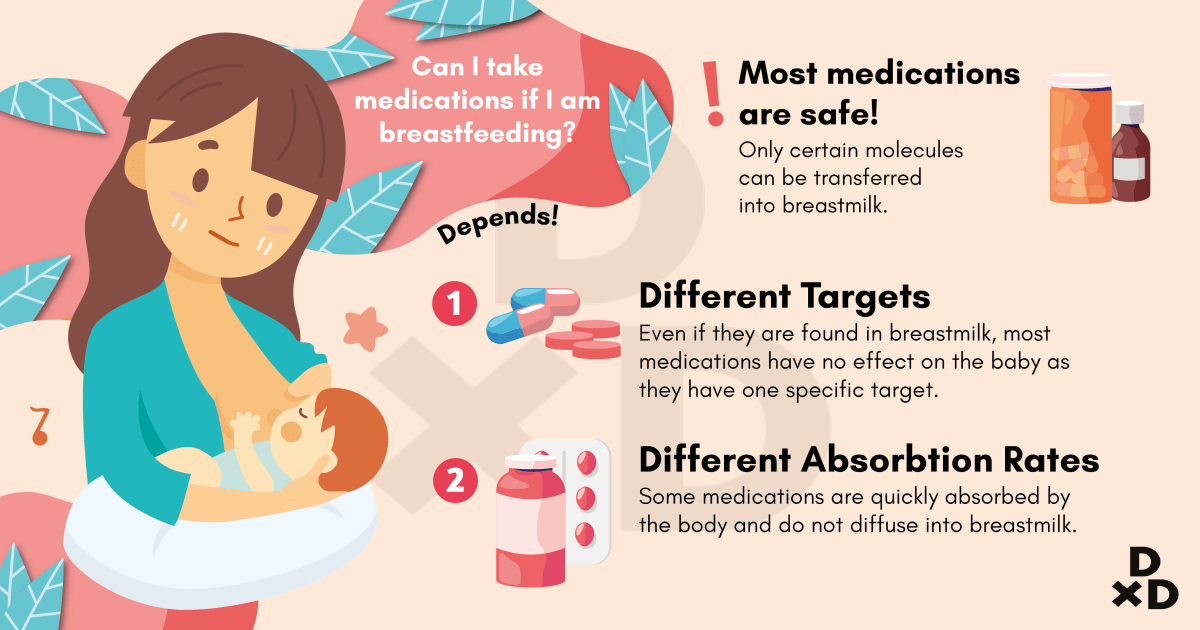
Raspberry leaf
When used as a tea, raspberry leaf is safe to use while breastfeeding. Raspberry leaf supplements should be avoided because there is limited safety information.
St John’s Wort
There is very little information available about the safety and efficacy of St John’s Wort in breastfeeding women. It is recommended that an alternative medicine be considered. See your doctor or pharmacist for advice before starting St John’s Wort.
References
-
McGuire T, Walters J, Dean A, et al. Review of the Quality of Complementary Medicines Information Resources: Summary Report. In: Service NP, ed. Sydney; 2009.
-
The regulation of complementary medicines in Australia – an overview. 2012. (Accessed 29/06/12, 2012, at http://www.tga.gov.au/industry/cm-basics-regulation-overview.htm)
-
Loke Y, ed. Pregnancy and Breastfeeding Medicines Guide. 1st ed. Melbourne: The Royal Women’s Hospital, Pharmacy Department; 2010.

-
Hale TW. Medications and mothers’ milk. 14th ed ed. Texas: Hale Publishing; 2010.
-
Lactmed. In: Lactmed; 2012.
-
Australian Pharmaceutical Formulary and Handbook. 22 ed. Canberra: Pharmaceutical Society of Australia; 2012.
-
Braun L, Cohen M. Herbs and Natural Supplements. 3 ed; 2010.
-
Francois CA, Connor SL, Bolewicz LC, Connor WE. Supplementing lactating women with flaxseed oil does not increase docosahexaenoic acid in their milk. Am J Clin Nutr 2003;77:226–33.
-
Swiss Ultiboost Spirulina. 2012. (Accessed June 2012, at http://www.swisse.com/products/superfoods/ultiboost-spirulina)
The Women’s does not accept any liability to any person for the information or advice (or use of such information or advice) which is provided on the Website or incorporated into it by reference. The Women’s provide this information on the understanding that all persons accessing it take responsibility for assessing its relevance and accuracy. Women are encouraged to discuss their health needs with a health practitioner. If you have concerns about your health, you should seek advice from your health care provider or if you require urgent care you should go to the nearest Emergency Dept.
Women are encouraged to discuss their health needs with a health practitioner. If you have concerns about your health, you should seek advice from your health care provider or if you require urgent care you should go to the nearest Emergency Dept.
Echinacea - Drugs and Lactation Database (LactMed)
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
Drugs and Lactation Database (LactMed) [Internet].
Show details
- Contents
Search term
Last Revision: October 18, 2021.
Estimated reading time: 2 minutes
CASRN: 84696-11-7; 90028-20-9; 97281-15-7
Drug Levels and Effects
Summary of Use during Lactation
Echinacea species (Echinacea angustifolia, Echinacea purpurea, Echinacea pallida) contain high molecular weight polysaccharides (e. g., heteroxylan, arabinogalactan) and lower molecular weight compounds (e.g., alkylamides, caffeoyl conjugates such as cichoric acid and echinacosides), but no single chemical is known to be responsible for Echinacea's biological activity. Some products have been standardized based on echinacoside, and others on cichoric acid. Echinacea has no specific uses during breastfeeding, but is commonly used orally to treat or prevent upper respiratory infections. Excretion of some of the purportedly active alkamides was found in breastmilk in one mother. No data exist on the safety and efficacy of Echinacea in nursing mothers or infants. In general, Echinacea is well tolerated with gastrointestinal upset, diarrhea and constipation, skin rash and rarely allergic reactions reported. It may also alter the metabolism of some dugs metabolized by the P450 enzyme system. Some sources indicate that Echinacea is safe in recommended doses,[1] while others recommend avoiding it during breastfeeding because of the lack of published safety data.
g., heteroxylan, arabinogalactan) and lower molecular weight compounds (e.g., alkylamides, caffeoyl conjugates such as cichoric acid and echinacosides), but no single chemical is known to be responsible for Echinacea's biological activity. Some products have been standardized based on echinacoside, and others on cichoric acid. Echinacea has no specific uses during breastfeeding, but is commonly used orally to treat or prevent upper respiratory infections. Excretion of some of the purportedly active alkamides was found in breastmilk in one mother. No data exist on the safety and efficacy of Echinacea in nursing mothers or infants. In general, Echinacea is well tolerated with gastrointestinal upset, diarrhea and constipation, skin rash and rarely allergic reactions reported. It may also alter the metabolism of some dugs metabolized by the P450 enzyme system. Some sources indicate that Echinacea is safe in recommended doses,[1] while others recommend avoiding it during breastfeeding because of the lack of published safety data. Echinacea has also been used topically to treat skin infections. A topical combination with Calendula (Calendit-E) was more effective than breastmilk in treating sore and cracked nipples in one study.[2-4]
Echinacea has also been used topically to treat skin infections. A topical combination with Calendula (Calendit-E) was more effective than breastmilk in treating sore and cracked nipples in one study.[2-4]
Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to prove the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does not certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information about dietary supplements is available elsewhere on the LactMed Web site.
Drug Levels
Maternal Levels. One woman was given 4 Echinacea Premium tablets (each containing the equivalent of 675 mg of Echinacea purpurea root and 600 mg of Echinacea angustifolia root made from the dried ethanolic extracts). The total dose of N-isobutyldodeca-2E,4E,8Z,10E/Z-tetraenamide alkamides was 13.1 mg. The alkamides were present in breastmilk between 1 and 4 hours after ingestion in concentrations similar to those reported in the blood with the same dose of the product.[5] Further details were not present in the abstract.
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
Relevant published information was not found as of the revision date.
Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date.
References
- 1.
Perri D, Dugoua JJ, Mills E, et al. Safety and efficacy of echinacea (Echinacea augustafolia, E.
 purpurea and E. pallida) during pregnancy and lactation. Can J Clin Pharmacol. 2006;13:e262–7. [PubMed: 17085774]
purpurea and E. pallida) during pregnancy and lactation. Can J Clin Pharmacol. 2006;13:e262–7. [PubMed: 17085774]- 2.
Niazi A, Rahimi VB, Soheili-Far S, et al. A systematic review on prevention and treatment of nipple pain and fissure: Are they curable? J Pharmacopuncture. 2018;21:139–50. [PMC free article: PMC6168189] [PubMed: 30283701]
- 3.
As'adi N, Kariman N. Herbal prevention and treatment of nipple trauma and/or pain in Iranian studies: A systematic review. J Herbmed Pharmacol. 2018;7:168–75. [CrossRef]
- 4.
Pezeshki B, Pouredalati M, Zolala S, et al. Comparison of the effect of aloe vera extract, breast milk, calendit-E, curcumin, lanolin, olive oil, and purslane on healing of breast fissure in lactating mothers: A systematic review. Int J Pediatr-Mashhad. 2020;8:10853–63. [CrossRef]
- 5.
Matthias A, Merika H, Addison RS, et al. Bioavailability of echinacea alkamides in human breast milk.
 Planta Med 2008;74:921. Abstract. doi:10.1055/s-002-12952. [CrossRef]
Planta Med 2008;74:921. Abstract. doi:10.1055/s-002-12952. [CrossRef]
Substance Identification
Substance Name
Echinacea
Scientific Name
Echinacea angustifolia; Echinacea purpurea; Echinacea pallida
CAS Registry Number
84696-11-7; 90028-20-9; 97281-15-7
Drug Class
Breast Feeding
Lactation
Complementary Therapies
Phytotherapy
Plants, Medicinal
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
Copyright Notice
Bookshelf ID: NBK501810PMID: 30000869
Contents
- PubReader
- Print View
- Cite this Page
- PDF version of this page (107K)
- Disable Glossary Links
In this Page
- Drug Levels and Effects
- Substance Identification
Bulk Download
LactMed Support Resources
- User and Medical Advice Disclaimer
- LactMed App
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
Related information
Similar articles in PubMed
- Review Calendula[Drugs and Lactation Database (.
 ..]
..] - Review Goldenseal[Drugs and Lactation Database (...]
- Review Feverfew[Drugs and Lactation Database (...]
- Review Marshmallow[Drugs and Lactation Database (...]
- Review Cranberry[Drugs and Lactation Database (...]
See reviews...See all...
Recent Activity
ClearTurn OffTurn On
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
See more...
Echinacea and breastfeeding. Can Echinacea be taken while breastfeeding?
Echinacea and breastfeeding. Can Echinacea be taken while breastfeeding? | E-lactationCan Echinacea be taken while breastfeeding? What are the alternatives to Echinacea?
July 1, 2015 (Low risk)
A herb that is widely used even during pregnancy and breastfeeding. Due to the lack of toxicity with an appropriate dose and moderate consumption, it should be compatible with breastfeeding. nine0003
nine0003
Roots and aerial tops are used. It contains polysaccharides, essential oil, flavonoids, pyrrolizidine alkaloids and others.
Unproven effects: immune stimulant, wound healing, anti-inflammatory.
Indications are: colds, bronchitis, skin lesions. Edges and air vertices are used.
It contains polysaccharides, essential oil, flavonoids, pyrrolizidine alkaloids ...
Unproven effects: immune stimulant, wound healing, anti-inflammatory. nine0003
Indications according to Commission E of the German Ministry of Health: colds, bronchitis, skin lesions.
Unlike the European Scientific Collaboration for Phytotherapy (ESPC), the European Medicines Agency does not recommend use under 12 years of age (allergy risk). Avoid use for more than 8 weeks (risk of leukopenia)
Alternatives
We do not have alternatives to echinacea .
Very low risk
Breastfeeding compatible. Low risk for the baby.
Low risk
Moderately safe. Read the comment carefully.
Read the comment carefully.
High risk
Dangerous. Use a less risky alternative. Read the comment.
Very high risk
Very dangerous. High risk of stopping breastfeeding.
Synonyms
- Black Sampson
- Brauneria angustifolia
- Coneflower
- Amer MR, Cipriano GC, Venci JV, Gandhi MA. Safety of Popular Herbal Supplements in Lactating Women. J Hum Lact. 2015 Abstract
- Kennedy DA, Lupattelli A, Koren G, Nordeng H. Herbal medicine use in pregnancy: results of a multinational study. BMC Complement Altern Med. 2013 Abstract Full text (link to source) Full text (link to our server)
- The Royal Women’s Hospital Victoria Australia. nine0070 Herbal and Traditional Medicines in Breasfeeding. Fact sheet. 2013 Full text (link to source) Full text (link to our server)
- Sachs HC; committee on drugs.
.jpg) The transfer of drugs and therapeutics into human breast milk: an update on selected topics. Pediatrics. 2013 Abstract Full text (link to source) Full text (link to our server)
The transfer of drugs and therapeutics into human breast milk: an update on selected topics. Pediatrics. 2013 Abstract Full text (link to source) Full text (link to our server) - Amir LH, Pirotta MV, Raval M. Breastfeeding--evidence based guidelines for the use of medicines. Aust Fam Physician. 2011 Abstract Full text (source link) Full text (link to our server)
- Cuzzolin L, Francini-Pesenti F, Verlato G, Joppi M, Baldelli P, Benoni G. Use of herbal products among 392 Italian pregnant women: focus on pregnancy outcome. Pharmacoepidemiol Drug Saf. 2010 Abstract
- Shah SA, Sander S, White CM, Rinaldi M, Coleman CI. nine0070 Evaluation of echinacea for the prevention and treatment of the common cold: a meta-analysis. Lancet Infect Dis. 2007 Abstract
- Perri D, Dugoua JJ, Mills E, Koren G.
 Safety and efficacy of echinacea (Echinacea angustafolia, e. purpurea and e. pallida) during pregnancy and lactation. Can J Clin Pharmacol. 2006 Abstract
Safety and efficacy of echinacea (Echinacea angustafolia, e. purpurea and e. pallida) during pregnancy and lactation. Can J Clin Pharmacol. 2006 Abstract - Zaffani S, Cuzzolin L, Benoni G. Herbal products: behaviors and beliefs among Italian women. nine0071 Pharmacoepidemiol Drug Saf. 2006 Abstract
- Huntley AL, Thompson Coon J, Ernst E. The safety of herbal medicinal products derived from Echinacea species: a systematic review. Drug Safe. 2005 Abstract
- Nordeng H, Havnen GC. Use of herbal drugs in pregnancy: a survey among 400 Norwegian women. Pharmacoepidemiol Drug Saf. 2004 Abstract
- Tesch BJ. Herbs commonly used by women: an evidence-based review. Am J Obstet Gynecol. 2003 Abstract
- Einarson A, Lawrimore T, Brand P, Gallo M, Rotatone C, Koren G.
 Attitudes and practices of physicians and naturopaths towards herbal products, including use during pregnancy and lactation. Can J Clin Pharmacol. 2000 Abstract
Attitudes and practices of physicians and naturopaths towards herbal products, including use during pregnancy and lactation. Can J Clin Pharmacol. 2000 Abstract - Gallo M, Sarkar M, Au W, Pietrzak K, Comas B, Smith M, Jaeger TV, Einarson A, Koren G. Pregnancy outcome following gestational exposure to echinacea: a prospective controlled study. Arch Intern Med. 2000 Abstract
- WHO. World Health Organization. Geneva. WHO monographs on selected medicinal plants. Volume I. WHO monographs 1999 Full text (link to source) Full text (link to our server)
- U
- Ф
- x
- C h
- Sh
- s E
- U
- I
- I
- I
- I
- I
- I
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
Book a consultation Book a consultation
- Data and statistics »
- Newsletter
- The facts are clear
- Publications nine0047 b
- e
- i
- i
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages nine0048
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Highlights "
- About WHO »
- General director
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center / nine0047 Questions and answers /
- Questions and answers /
- Breastfeeding COVID-19 Frequently Asked Questions
May 7, 2020 | Questions and answers
Can COVID-19 be transmitted through breastfeeding?
There is currently no evidence of transmission of active COVID-19 (a virus that can cause infection) through breast milk or breastfeeding. There is no reason to refuse or stop breastfeeding. nine0003
There is no reason to refuse or stop breastfeeding. nine0003
Should women living in COVID-19 affected areas breastfeed?
Yes. In all socioeconomic settings, breastfeeding increases survival rates and has long-term health and developmental benefits for newborns and infants. Breastfeeding also has a positive effect on the health of the mother.
Is it still recommended to practice skin-to-skin contact between mother and baby after childbirth and breastfeeding, even if the mother is suspected of having COVID-19?or a confirmed coronavirus infection?
Yes. Prolonged skin-to-skin contact immediately after birth, including kangaroo nursing, normalizes the newborn's body temperature and is associated with better neonatal survival. Placing the newborn in close proximity to the mother also promotes early breastfeeding, which also reduces neonatal mortality.
The many benefits of skin-to-skin contact and breastfeeding far outweigh the potential risk of COVID-19 transmissionand development of the disease.
Can women with suspected or confirmed COVID-19 breastfeed?
Yes. Women with suspected COVID-19 or confirmed coronavirus infection can breastfeed if they choose to. In this case, they are advised to:
- frequently wash their hands with soap and water or use alcohol-based hand rub, especially before touching a child;
- wear a medical mask before any contact with the child, including during breastfeeding; nine0048
- Cover your face with a disposable tissue when sneezing or coughing. The used tissue should be thrown away immediately and the hands washed again;
- regularly clean and disinfect surfaces touched by the baby's mother.
It is important to change medical masks as soon as they become damp and discard them immediately. Do not touch the front of the mask and reuse the mask.
If a mother has suspected or confirmed COVID-19 but does not have a medical mask, can she breastfeed? nine0003
Yes. Breastfeeding has undeniably reduced mortality in newborns and infants and has many positive and long-term effects on the health and development of the child's brain.
It is recommended that mothers with symptoms of COVID-19 wear a medical mask, but even if this is not possible, breastfeeding should be continued. In this case, the mother should follow other infection prevention practices, such as washing hands, disinfecting surfaces, and covering her mouth and nose when sneezing or coughing with a disposable handkerchief. nine0003
The efficacy or safety of non-medical masks (eg, homemade masks made from cloth or other materials) has not yet been studied. At the moment, it is not possible to make recommendations for or against the use of these masks.
I have suspected or confirmed COVID-19 and feel too sick to breastfeed. What should I do?
If you are too unwell to breastfeed because of COVID-19 or other complications, you should be helped to find a way to provide your baby with breast milk that is safe, convenient, and acceptable to you. To do this, you can:
- express milk;
- use donor breast milk.
If expressing milk or using donor milk is not possible, consideration may be given to using a wet nurse (another breastfeeding woman) or formula feeding to the baby, if the formula can be prepared correctly, hygienically and affordably.
I was ill with suspected COVID-19or confirmed coronavirus infection and could not breastfeed. When can I resume breastfeeding?
You can resume breastfeeding as soon as you feel well enough. There is no specific length of time during which a mother with suspected COVID-19 or confirmed coronavirus infection should refrain from breastfeeding. There is currently no data on the impact of breastfeeding on the clinical course of COVID-19at mother. Your healthcare provider or lactation consultant should be able to help you resume breastfeeding.
I have suspected COVID-19 or confirmed coronavirus infection. Wouldn't it be safer to feed my baby artificial milk?
No. Feeding newborns and infants with artificial milk is always associated with some risk, regardless of other conditions. The risk associated with formula feeding increases if there are adverse conditions at home or where the mother and child live, such as limited access to health care if the child is sick, limited access to clean drinking water, or no secure supply of infant formula.