Milk fever in women
Symptoms (Fever After Breastfeeding), Treatment & Prevention
Written by Danny Bonvissuto
In this Article
- Causes
- Symptoms
- Diagnosis
- Treatment
- Prevention
On a good day, your breasts can feel tender. They're always out on the front lines, taking the brunt of every afternoon jog and pouncing toddler. They don't get infected often, but when they do, it can hurt like no bad bra or PMS pain ever has.
The catchall name for an infection of the breast tissue is mastitis. If you're breastfeeding, it's called lactation or puerperal mastitis. If you're not, it's called periductal mastitis. Mastitis can make you feel like you have the flu, but it can be cured a lot quicker.
Causes
Mastitis is a common condition in women who breastfeed. As many as 1 in 10 breastfeeding women in the U.S. get it. It's caused by a backup of milk in the milk ducts. This happens when your baby isn't sucking or attaching properly, or favors one breast over the other. Mastitis can also happen if you don't feed or pump regularly.
Breastfeeding women aren't the only ones who get mastitis. If you're not breastfeeding, a cracked nipple or nipple piercing can cause the breast infection. Both allow bacteria to get into the milk ducts. This is especially common in women who smoke.
Symptoms
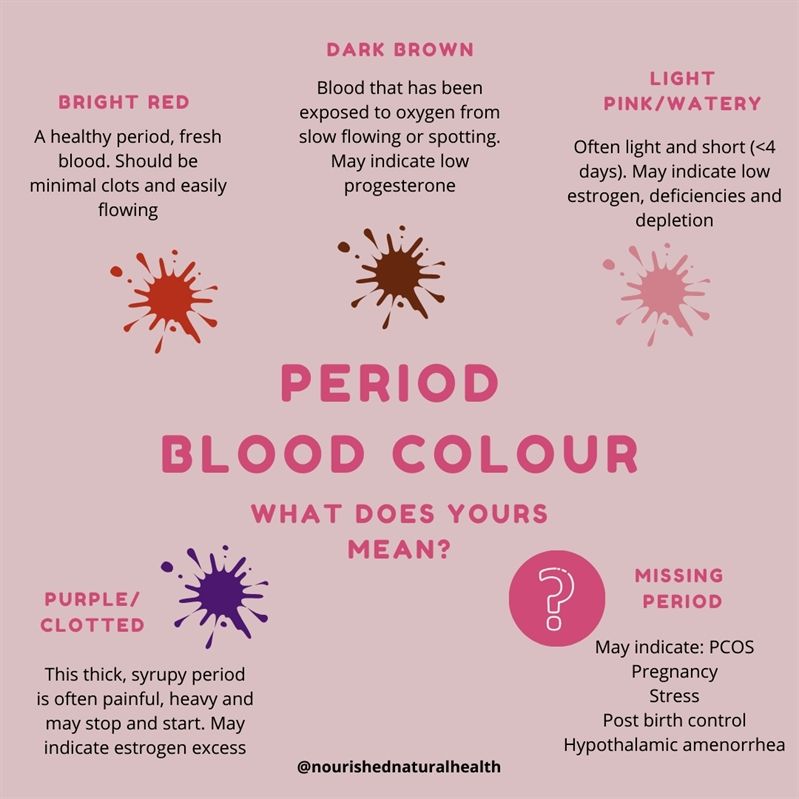
Just like any other infection, the tissue around the infected area becomes inflamed to keep it from spreading to other parts of the body. With mastitis, the infected milk duct causes the breast to swell. Your breast may look red and feel tender or warm.
Many women with mastitis feel like they have the flu, including achiness, chills, and a fever of 101 F or higher.
You may also have discharge from your nipple or feel a hard lump in your breast.
Diagnosis
The symptoms of mastitis can come on very suddenly. You may feel like you're getting the flu before you feel any discomfort in your breast. When you feel that pain or see the telltale redness, call your doctor as soon as possible.
Your doctor can diagnose mastitis based on a physical exam. The fever and chills give it away, as does a red, wedge-shaped area on the breast that points toward the nipple.
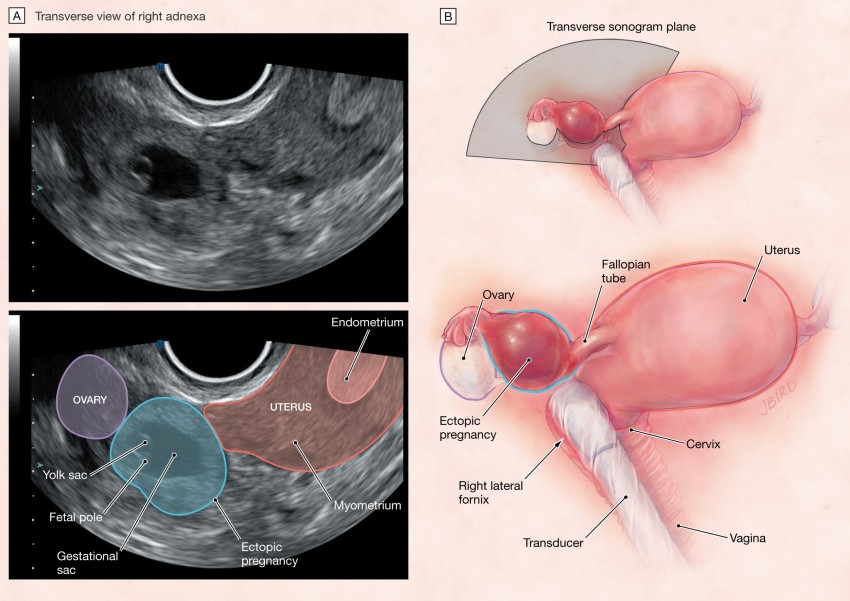
There are two things to rule out: a breast abscess, which happens when mastitis isn't treated quickly, and inflammatory breast cancer, which is rare and shares the symptoms of redness and swelling.
Treatment
Whether or not you're breastfeeding, antibiotics should have you feeling better in a day or two. Take them as directed.
If you are breastfeeding, continue drinking lots of water, wearing loose bras, and resting as much as you can. Your doctor may suggest ibuprofen, or something like it, to take care of the fever and pain.
It's important to keep breastfeeding and move that milk in and out of the ducts. Continue expressing milk if it is too painful to feed from the breast.
Prevention
Tight bras and clothing put pressure on your breasts. Keep things light and loose.
To keep milk from backing up, make sure your baby attaches correctly, and get all the milk out of each breast during every feeding. A lactation consultant can help if you need support.
Symptoms (Fever After Breastfeeding), Treatment & Prevention
Written by Danny Bonvissuto
In this Article
- Causes
- Symptoms
- Diagnosis
- Treatment
- Prevention
On a good day, your breasts can feel tender. They're always out on the front lines, taking the brunt of every afternoon jog and pouncing toddler. They don't get infected often, but when they do, it can hurt like no bad bra or PMS pain ever has.
The catchall name for an infection of the breast tissue is mastitis. If you're breastfeeding, it's called lactation or puerperal mastitis. If you're not, it's called periductal mastitis. Mastitis can make you feel like you have the flu, but it can be cured a lot quicker.
Causes
Mastitis is a common condition in women who breastfeed. As many as 1 in 10 breastfeeding women in the U.S. get it. It's caused by a backup of milk in the milk ducts. This happens when your baby isn't sucking or attaching properly, or favors one breast over the other. Mastitis can also happen if you don't feed or pump regularly.
As many as 1 in 10 breastfeeding women in the U.S. get it. It's caused by a backup of milk in the milk ducts. This happens when your baby isn't sucking or attaching properly, or favors one breast over the other. Mastitis can also happen if you don't feed or pump regularly.
Breastfeeding women aren't the only ones who get mastitis. If you're not breastfeeding, a cracked nipple or nipple piercing can cause the breast infection. Both allow bacteria to get into the milk ducts. This is especially common in women who smoke.
Symptoms
Just like any other infection, the tissue around the infected area becomes inflamed to keep it from spreading to other parts of the body. With mastitis, the infected milk duct causes the breast to swell. Your breast may look red and feel tender or warm.
Many women with mastitis feel like they have the flu, including achiness, chills, and a fever of 101 F or higher.
You may also have discharge from your nipple or feel a hard lump in your breast.
Diagnosis
The symptoms of mastitis can come on very suddenly. You may feel like you're getting the flu before you feel any discomfort in your breast. When you feel that pain or see the telltale redness, call your doctor as soon as possible.
Your doctor can diagnose mastitis based on a physical exam. The fever and chills give it away, as does a red, wedge-shaped area on the breast that points toward the nipple.
There are two things to rule out: a breast abscess, which happens when mastitis isn't treated quickly, and inflammatory breast cancer, which is rare and shares the symptoms of redness and swelling.
Treatment
Whether or not you're breastfeeding, antibiotics should have you feeling better in a day or two. Take them as directed.
If you are breastfeeding, continue drinking lots of water, wearing loose bras, and resting as much as you can. Your doctor may suggest ibuprofen, or something like it, to take care of the fever and pain.
It's important to keep breastfeeding and move that milk in and out of the ducts. Continue expressing milk if it is too painful to feed from the breast.
Continue expressing milk if it is too painful to feed from the breast.
Prevention
Tight bras and clothing put pressure on your breasts. Keep things light and loose.
To keep milk from backing up, make sure your baby attaches correctly, and get all the milk out of each breast during every feeding. A lactation consultant can help if you need support.
Lactostasis in nursing: symptoms, treatment, signs
Obstetrician-gynecologist, reproductologist, member of the Russian Association of Human Reproduction
Perevoznikova
Ekaterina Mikhailovna
Experience 13 years
Obstetrician-gynecologist
Make an appointment
Laktostasis - a delay in the separation of milk in women during lactation. The cause of this phenomenon in most cases is a blockage or spasm of the milky passages. Other factors can provoke milk retention in the ducts of the mammary glands: wearing tight underwear, injuries, abrupt cessation of breastfeeding. nine0003
nine0003
Causes of pathology
The development of lactostasis occurs against the background of a decrease in the patency of the excretory duct of the mammary gland with excessive milk production. The milky passages are prone to spasms, which cause their obturation. Anatomical features of the structure of the mammary glands of patients have a significant impact on the likelihood of developing lactostasis:
- flat teat;
- sagging breasts;
- narrowed milk ducts. nine0022
Often, pathology develops due to an abrupt cessation of lactation or difficulty feeding. Cracks may form on the nipples. Similarly, the likelihood of developing lactostasis in a nursing girl is affected by:
- incorrect attachment of the infant to the breast;
- insufficient sucking activity of the child;
- tight underwear;
- falling asleep on the stomach;
- chest hypothermia; nine0022
- stressful situations.

Some women experience blockage of the milky passages due to excessive physical exertion after the birth of a child.
Symptoms of pathology
Symptoms of lactostasis in a nursing mother are diverse. The primary sign of pathology is the compaction of the area of \u200b\u200bthe mammary gland. Patients complain of fullness and a feeling of heaviness in the chest. The impossibility of outflow of milk over a long period of time leads to an increase in local temperature and a change in the pigmentation of the skin. In the absence of medical assistance, the girl's condition worsens. Body temperature with advanced lactostasis rises to 38-39degrees.
The pain syndrome is not always accompanied by the formation of a subcutaneous seal. Attempting to feed a baby can lead to a short-term relief of symptoms. The focus of stagnation remains mobile, the affected area can change location and increase.
Diagnostic measures
Diagnosis of lactostasis is not difficult. An obstetrician or gynecologist examines the patient and palpation determines the localization of the seal in the chest. The girl is encouraged to track changes in body temperature. If there are signs of an inflammatory process, the patient is prescribed tests. Their data allows doctors to develop a strategy for drug treatment that will not affect the quality of the milk received by the child. nine0003
An obstetrician or gynecologist examines the patient and palpation determines the localization of the seal in the chest. The girl is encouraged to track changes in body temperature. If there are signs of an inflammatory process, the patient is prescribed tests. Their data allows doctors to develop a strategy for drug treatment that will not affect the quality of the milk received by the child. nine0003
Treatment
The main task of all therapeutic manipulations is to create conditions for emptying the mammary glands. Moderate warming and light breast massage contribute to the normalization of the state of the milky passages. Girls should follow the regime and devote the necessary amount of time to rest. Relatives of patients should maintain a conflict-free home environment. Nursing mothers are advised not to sleep on their back or stomach, but on their side.
Expressing milk is an effective way to prevent lactostasis at the first sign of milk retention. The procedure may be painful, but it should be systematically repeated until the symptoms of the pathology disappear completely. A side effect of pumping is a burning sensation in the chest after the opening of the milky passage. nine0003
A side effect of pumping is a burning sensation in the chest after the opening of the milky passage. nine0003
Prolonged lactostasis is a reason to see a doctor. A visit to the clinic is required for persistent pain, fever, hyperemia. Patients may experience breast inflammation. In this case, any warming procedures are contraindicated, as they will accelerate the progression of the infection.
Self-treatment of lactostasis is not recommended for mothers who are breastfeeding for the first time. Erroneous actions can lead to a complicated course of lactostasis and a complete loss of milk. nine0003
Complication
The most severe complication of lactostasis is mastitis - inflammation of the breast tissue. Patients face increasing pain syndrome. Later, fever and fever in the affected area join it. The skin of the mammary glands is covered with red stripes. Milk contains impurities of blood and purulent discharge.
The occurrence of mastitis is promoted by hypothermia (lactation in a cool room or in a draft) or overheating (hot shower, sauna) of the patient. Running lactostasis, complicated by mastitis, often causes the formation of a breast abscess. nine0003
Running lactostasis, complicated by mastitis, often causes the formation of a breast abscess. nine0003
Preventive measures
Prevention of lactostasis involves the observance of several recommendations by the nursing mother. The infant should be fed regularly (but no more than once every two hours), and milk residues should be carefully expressed using a manual or automatic breast pump.
Avoid wearing tight underwear. Limiting physical activity and stress during lactation significantly reduces the likelihood of lactostasis. An important role is given to the diet - it must include fresh vegetables and fruits. nine0003
When symptoms of lactostasis appear, you should not refuse to feed the baby. With a long delay in the outflow of milk, you should consult a doctor. Self-administration of any drugs is not recommended. It should be borne in mind that the affected mammary gland after recovery may produce less milk. Over time, the secretory function will be restored in full.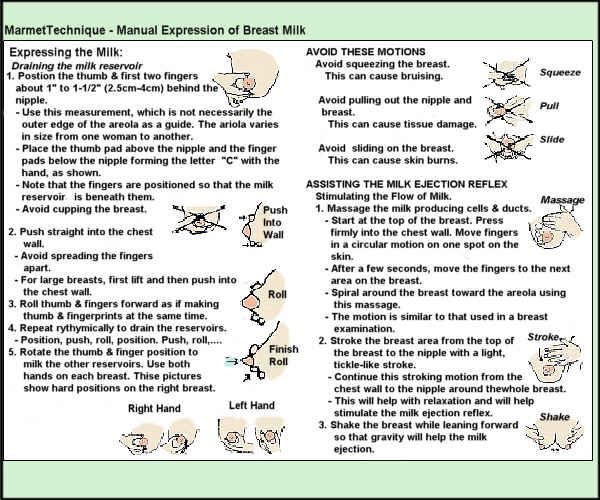
FAQ
Why should you not stop breastfeeding with lactostasis? nine0003
Refusal of lactation can provoke the development of complications, the most severe of which remains mastitis. Inflammatory processes in the mammary glands cause the formation of abscesses. Their treatment is a long and painful process that will not allow the patient to continue breastfeeding the baby.
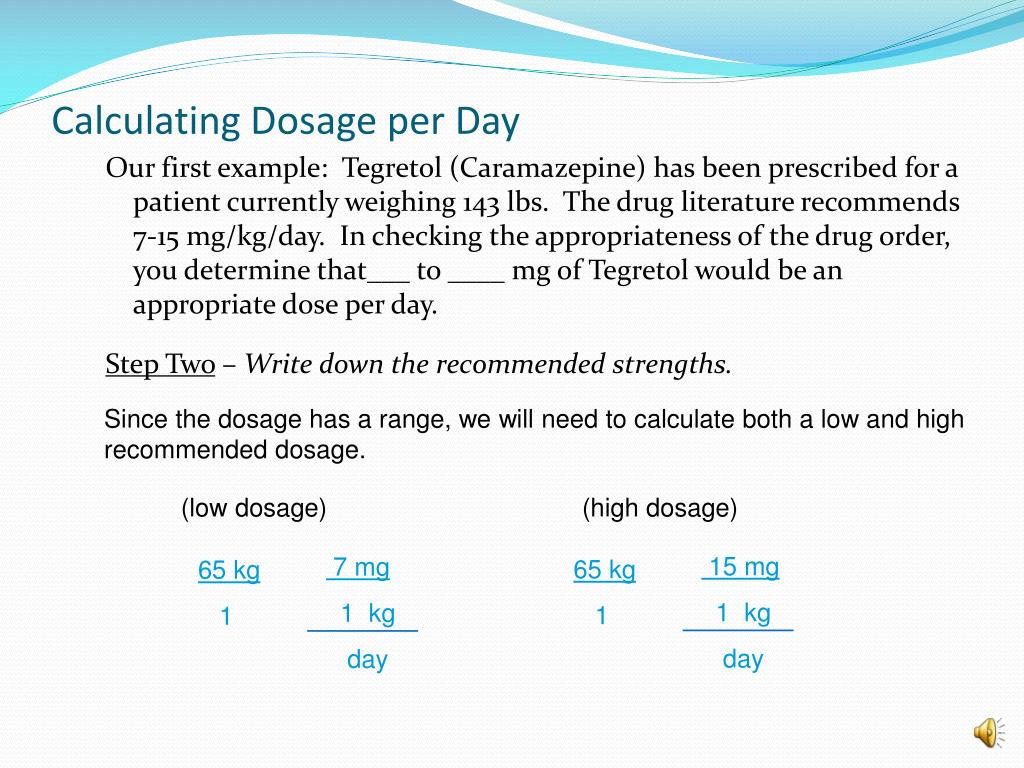
What drugs are allowed for girls in the treatment of lactostasis?
Treatment of uncomplicated lactostasis does not involve the use of drug therapy. Girls need to express milk with a breast pump. An important role in the expansion of the lactiferous passages is assigned to the manual effect on the mammary gland. Massaging the affected area helps to normalize the outflow of milk. Taking anti-inflammatory drugs is justified in the development of mastitis. Antibiotics help eliminate the possibility of developing an abscess, the treatment of which will require surgical intervention. nineOl000 One of the most common problems breastfeeding moms face is blocked milk ducts, also known as milk stasis or lactostasis. What sensations arise with a clogged milk duct? A sensitive seal appears in the chest, and slight pain and discomfort may occur. nine0105
nineOl000 One of the most common problems breastfeeding moms face is blocked milk ducts, also known as milk stasis or lactostasis. What sensations arise with a clogged milk duct? A sensitive seal appears in the chest, and slight pain and discomfort may occur. nine0105
We'll cover the most common questions about this problem and provide you with all the important information about blocked ducts, from symptoms of blocked ducts in the breast to treatments and tips to prevent the condition.
If you need more information, ask someone else.
Signs of blocked milk duct
What is blocked milk duct and how is it different from other breast conditions like mastitis? Blockage of the milk duct, also known as milk stasis or lactostasis, is a condition in which a milk clot forms in the breast, preventing milk from flowing out of the duct. A painful lump forms in the chest, and there may be a feeling of discomfort around it. nine0105
Common symptoms of blockage of the breast duct are:
- pain in a certain area of the breast;
- painful lump in the mammary gland the size of a pea or more;
- slight increase in temperature in the area of blockage;
- sometimes a small white bubble forms on the nipple.
In a nutshell, duct blockage is the formation of a localized lump in the chest that causes discomfort, in the absence of any other signs of illness or fever. If there is a fever or flu-like symptoms and if the chest feels hot to the touch, it may be mastitis. nine0105
More information on symptoms and treatment for mastitis can be found here.
Causes of blockage of the breast duct
Blockage of the milk duct can occur for several reasons:
- incomplete flow of milk from the breast during feeding;
- incorrect attachment of the child, due to which he cannot fully suckle the breast;
- engorgement;
- excess milk production; nine0022
- abrupt cessation of breastfeeding;
- putting pressure on the mammary gland: for example, wearing tight clothing that compresses the chest.
Blockage of the milk duct is usually the result of incomplete emptying of the breast or excessive pressure on the breast for a long period of time.
How to remove blockage of the milk duct?
To prevent a breast infection, it is important to find a way to clear the blocked milk duct as soon as possible. nine0003
Here's what to do if your milk duct is blocked:
- Continue to breastfeed your baby. If the milk duct is blocked, you should continue to feed the baby and try to do it so that the baby sucks out all the milk. You can also try breastfeeding a baby with a blocked duct every two hours. This will help keep the milk flowing and possibly clear blockages. Continuous stimulation of the flow of milk is the key to eliminating blockage of the duct.
These bra pads help prevent milk stains on clothes while breastfeeding. Their porous top layer and excellent absorbency will help keep clothes dry and comfortable.
- Massage and express between feeds. Before each feeding, it is recommended that the mother massage the breast with stroking movements from the periphery of the breast to the nipple.
 This stimulates the flow of milk even before the start of feeding. After breastfeeding, a mother can express any milk left in a breast with a blocked duct to ensure that the ducts are completely emptied. Stimulating the flow of milk can help prevent blockages in the milk ducts, but there are times when a mother cannot be with her baby during breastfeeding. To stimulate the flow of milk in such situations, it is very important to express milk manually. nine0105
This stimulates the flow of milk even before the start of feeding. After breastfeeding, a mother can express any milk left in a breast with a blocked duct to ensure that the ducts are completely emptied. Stimulating the flow of milk can help prevent blockages in the milk ducts, but there are times when a mother cannot be with her baby during breastfeeding. To stimulate the flow of milk in such situations, it is very important to express milk manually. nine0105
Check out these manual breast pumps for expressing milk anywhere, anytime.
- Attach the baby correctly to the breast. Attaching the baby to the breast in such a way that his chin is directed towards the blocked duct can help solve the problem. Such attachment to the breast will help the baby, when sucking, empty exactly the area of \u200b\u200bthe mammary gland where there is a blockage. You can try to apply the baby in different ways, so that it is more convenient for him to extract all the milk from different parts of the breast.
 nine0022
nine0022 - Apply warm and cold compresses. As compresses, you can use a towel, as well as thermal pads 2 in 1. It is recommended to apply a warm thermal pad to the area of the clogged duct several times a day, while doing a light massage. Breast discomfort after feedings can be alleviated somewhat by using cooled thermal pads.
- Wear comfortable, loose-fitting clothing. One of the causes of blockage of the milk ducts is excessive pressure on the mammary glands for an extended period of time.
 This pressure can be exerted by tight clothing or bras, so it is important to wear loose clothing to clear a blocked duct. Sometimes mothers also notice clogged pores on their breasts - loose clothing and a bra will also help to cope with this problem. nine0022
This pressure can be exerted by tight clothing or bras, so it is important to wear loose clothing to clear a blocked duct. Sometimes mothers also notice clogged pores on their breasts - loose clothing and a bra will also help to cope with this problem. nine0022 - Tight clothing encourages more intense perspiration and prevents sweat from evaporating, thus clogging pores. Moms should wear loose-fitting clothing to clear clogged pores and clear blocked milk ducts.
If following these tips fails to open the milk duct, it is recommended that you contact your doctor or lactation consultant to prevent infection.
How to prevent clogged milk ducts? nine0115
Every mother would like to avoid the problem of blocked milk ducts altogether. No one will give a 100% guarantee against blockage of the milk ducts, but you can try to prevent it by using a few useful tips.
- After each feeding, check that there is no feeling of fullness and discomfort in the chest.
 If it is, then it is necessary to additionally express milk, until a feeling of comfort.
If it is, then it is necessary to additionally express milk, until a feeling of comfort. - Feed your baby regularly for as long and as often as he wants
- Express milk between feedings if you experience discomfort and fullness in your breasts.
- Place the baby on the breast so that there is no undue pressure on the breast.
- Wear loose, comfortable clothing and bralettes.
When should I seek professional help?
When a blockage of the milk duct occurs, the mother should not panic. Despite the discomfort and pain, this condition is quite normal and usually goes away if treated immediately. nine0105
If you want to know how to clear a blocked milk duct, or if you are feeling a blocked milk duct, you should seek help from your doctor.
Find out more about other common breastfeeding problems and how to deal with them.
Articles & tips from Philips Avent
Links
The New Breastfeeding Guide for Mothers 3rd Edition (2017)
Baby+ app
Download the app and track your child's development and growth with trackers, and keep those special moments forever.