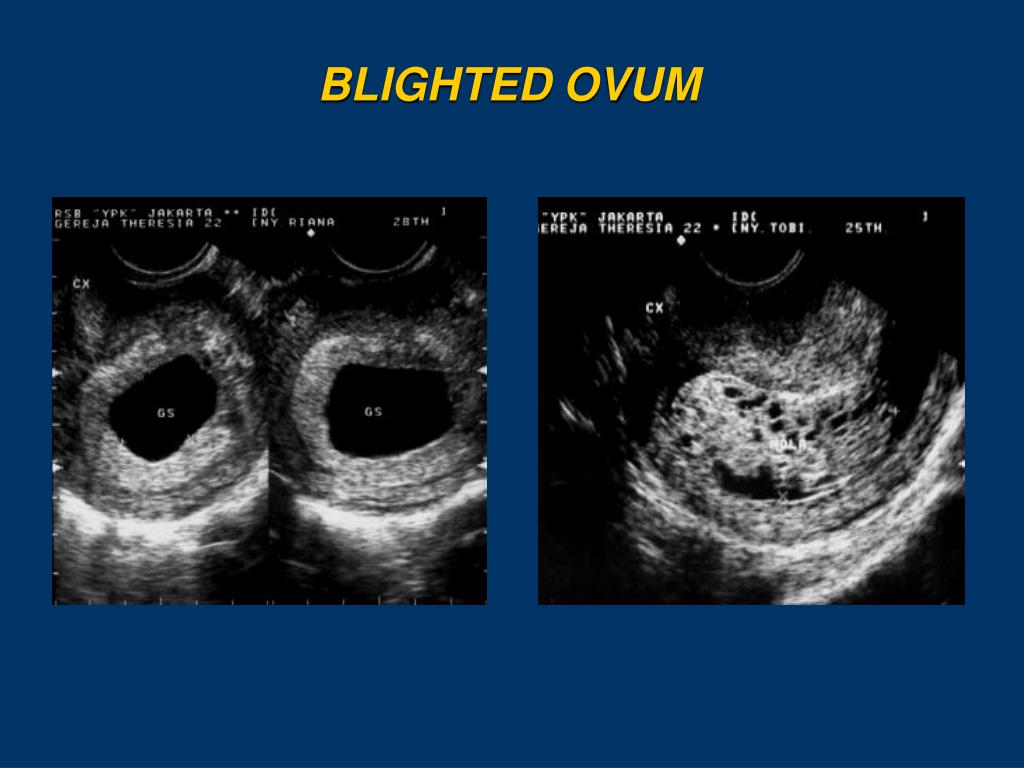
Blighted ovum with twins
What is vanishing twin syndrome?
Vanishing twin syndrome is the name given to a type of miscarriage that usually happens in early pregnancy with twins or triplets, when one embryo miscarries and the pregnancy continues. This means that you may be told that you’re carrying more than one baby, usually twins, at an early scan but only one baby is seen at your later appointment. Vanishing twin is the term given to your baby that doesn’t fully develop. We explain more about vanishing twin syndrome, possible causes and explain more about your pregnancy after it happens.
What is vanishing twin syndrome and how does it happen?
When a fertilised egg develops into an embryo, a protective membrane filled with fluid grows around it. This is called the gestational sac. Sometimes in a twin or multiple pregnancy, usually very early on, one of your embryos doesn't develop at all within one of the sacs (an anembryonic pregnancy, which is also known as a blighted ovum). Or one embryo simply stops growing, and its tissue may be absorbed into your placenta or your other baby.
In most cases, the exact cause of vanishing twin syndrome isn’t known. However, it's thought that most vanishing twins happen because of genetic conditions that exist from conception.
How is vanishing twin syndrome diagnosed?
Because of developments in scans, very early pregnancy loss, including vanishing twin syndrome, is diagnosed more often. Ultrasonography technology is now so advanced that it can tell us all sorts of things that may once have gone unnoticed. For example, a vaginal ultrasound scan can locate two gestational sacs at just five weeks of pregnancy. And embryos with a heartbeat can be seen clearly after about six weeks gestation.
Vanishing twin syndrome usually happens in the first trimester. This means you may be completely unaware that you were ever carrying twins. Or if you have an early scan that showed you were carrying twins, you may only discover that you're carrying one baby at your follow-up ultrasound scan, such as the routine dating scan at 12 weeks.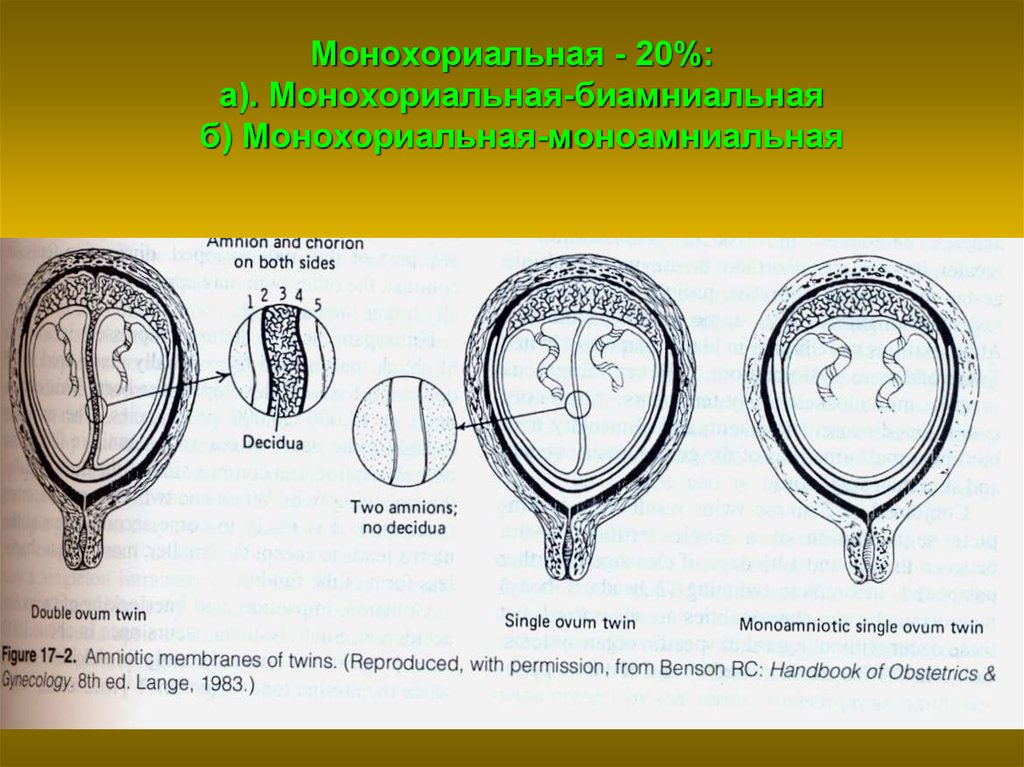
What are the symptoms of vanishing twin syndrome?
You may not have any symptoms at all, particularly if you miscarry your twin in the first trimester.
If do you experience symptoms, you're most likely to notice vaginal bleeding and cramping. As with any pregnancy, if you experience these symptoms, contact your midwife or maternity unit.
How common is vanishing twin syndrome and who is most at risk?
It’s difficult to say how common vanishing twin syndrome is because of how early it can happen. It usually happens before any scans take place. However, we do know that many more twins are conceived than are eventually born. Some studies suggest vanishing twin syndrome happens in nearly a third of all multiple pregnancies while others put it at much less.
Experts don't know for sure if vanishing twin syndrome is hereditary, which means it’s passed down through families. But they do know that your age might increase your risk of vanishing twin syndrome, as it’s more common in pregnancies in women aged over 30.
Vanishing twin syndrome is slightly less common if you become pregnant with twins or more after fertility treatment, such as in vitro fertilisation (IVF) and intracytoplasmic sperm injection (ICSI), compared to natural conception.
How does vanishing twin syndrome affect my surviving baby or babies?
It depends on when you miscarry your twin. If it happens early in the first trimester, you’re likely to have a healthy pregnancy that continues as if you were carrying one baby right from the start and no special treatment is needed.
If you miscarry your twin in the second or third trimester, there are increased risks to your surviving baby, including a higher chance of cerebral palsy. You're likely to be referred for specialist care, including more testing and monitoring for potential problems with the placenta, infections and for signs of premature labour.
Researchers have found that if you conceived through fertility treatment, there may be a slightly higher chance that your surviving baby may be born small or early.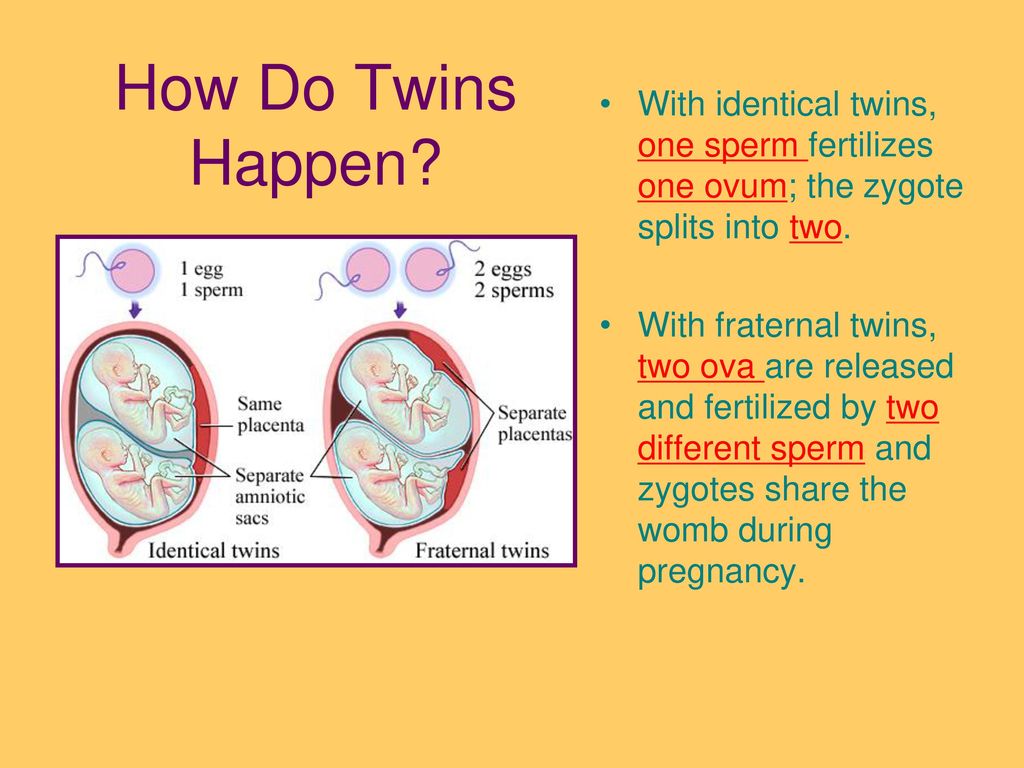 This may mean that they are more likely to need special care.
This may mean that they are more likely to need special care.
Can a vanishing twin affect screening tests for Down's syndrome?
If you're having non-invasive prenatal testing (NIPT) or a combined screening test for Down's syndrome, Edwards’ syndrome and Patau’s syndrome, it may still be accurate for your surviving baby, as long as there's no sign of the vanished twin and some time has passed since the miscarriage.
Although NIPT is very accurate, sometimes it shows a false positive result. If you have a positive result, you may choose to have a diagnostic test such as a chorionic villus sampling (CVS) or amniocentesis for a definite diagnosis.
During the combined screening test, sometimes a second sac with a tiny undeveloped embryo is still visible. This may influence the blood test results, so the screening result would be calculated on the scan alone.
Dealing with difficult feelings after vanishing twin syndrome
The loss of a twin can hit you hard, no matter how early it happens. If you had an early scan that showed multiple babies, you're bound to have spent several weeks before your next scan imagining what it would be like to have them. It’s only natural if you now feel confusion and a sense of sadness and loss. It's particularly confusing because although you've lost a baby, you're still pregnant. Rest assured that your pregnancy is likely to continue as normal.
If you had an early scan that showed multiple babies, you're bound to have spent several weeks before your next scan imagining what it would be like to have them. It’s only natural if you now feel confusion and a sense of sadness and loss. It's particularly confusing because although you've lost a baby, you're still pregnant. Rest assured that your pregnancy is likely to continue as normal.
Dealing with miscarriage looks different for everyone. It’s really important to be kind to yourself. You're likely to go through the complex feelings and emotions as you'd have while coping with a miscarriage of a singleton pregnancy.
Talk through your feelings with someone who has had a similar experience and devote time to looking after yourself and your surviving baby. Try these ideas:
- Self-care for the first trimester
- Self-care for the second trimester
For more information and support, check out our advice on coping with the loss of a twin.
References
This article was written using the following sources:
Anderson-Berry AL. 2016. Vanishing twin syndrome. MedScape. emedicine.medscape.com [Accessed February 2021]
APA. 2017. Vanishing twin syndrome. American Pregnancy Association. americanpregnancy.org [Accessed February 2021]
Balaguer N, Mateu-Brull E, Serra V, Simón C, Milán M. Should vanishing twin pregnancies be systematically excluded from cell-free fetal DNA testing? Prenat Diagn. 2020 Aug 24. doi: 10.1002/pd.5817. pubmed.ncbi.nlm.nih.gov [Accessed March 2021]
Chasen ST, Chervenak FA. 2020. Twin syndrome: prenatal issues. UpToDate. www.uptodate.com [Accessed February 2021]
Chaveeva P, Wright A, Syngelaki A, et al. 2020. First-trimester screening for trisomies in pregnancies with vanishing twin. Ultrasound Obstetric Gynecology 55(3):326-331. doi: 10.1002/uog.21922. pubmed.ncbi.nlm.nih.gov [Accessed February 2021]
Kamath MS, Antonisamy B, Selliah HY, et al. 2018. Perinatal outcomes of singleton live births with and without vanishing twin following transfer of multiple embryos: analysis of 113,784 singleton live births. . Human Reproduction 33(11):2018-2022. academic.oup.com [Accessed February 2021]
2018. Perinatal outcomes of singleton live births with and without vanishing twin following transfer of multiple embryos: analysis of 113,784 singleton live births. . Human Reproduction 33(11):2018-2022. academic.oup.com [Accessed February 2021]
Márton V, Zádori J, Kozinszky Z, Keresztúri A. 2016. Prevalences and pregnancy outcome of vanishing twin pregnancies achieved by in vitro fertilization versus natural conception. Fertil Steril 106(6):1399-1406. pubmed.ncbi.nlm.nih.gov [Accessed February 2021]
Moore KL, Persaud TVN and Torchia MG. 2019. Third week of human development. Chapter 4 in The developing human: clinically oriented embryology. 11th edition. Elsevier
Moore KL, Persaud TVN and Torchia MG. 2019. Fourth to eighth weeks of human development. Chapter 5 in The developing human: clinically oriented embryology. 11th edition. Elsevier
Napolitano R, Papageorghiou AT. 2014. First-trimester detection of fetal anomalies. Chapter 1 in Coady AM, Bower S. Twining's textbook of fetal abnormalities e-book. books.google.co.uk [Accessed February 2021]
Twining's textbook of fetal abnormalities e-book. books.google.co.uk [Accessed February 2021]
NICE. 2019. Twin and triplet pregnancy. National Institute of Health and Care Excellence, Guideline 137. www.nice.org.uk [Accessed February 2021]
Pinborg A, Lidegaard O, Cour Freiesleben N, et al. 2005. Consequences of vanishing twins in IVF/ICSI pregnancies. Human Reproduction 20(10):2821-9. academic.oup.com [Accessed February 2021]
Zhou F, Li Y, Wang H, Liu S, et al. 2020. Perinatal outcomes in vanishing twin pregnancies following assisted reproductive technology (ART) - a systematic review and meta-analysis. J Perinat Med 48(7):639-647. doi: 10.1515/jpm-2020-0088. pubmed.ncbi.nlm.nih.gov [Accessed February 2021]
Zhu J, Wang Z, Chen L, et al. 2020. The late vanishing of a co-twin contributes to adverse perinatal outcomes in the surviving twin. Human Reproduction 35(7):1553-1561. doi: 10.1093/humrep/deaa120. pubmed.ncbi.nlm.nih.gov [Accessed February 2021]
Show references Hide references
Blighted Ovum – Newborn Baby
Blighted ovum is not a common term but it accounts for 45 to 55% of all miscarriages. That’s a huge amount of percentage there.
That’s a huge amount of percentage there.
So, what you should know about this?
Blighted ovum and its causes
[mobile_add addrotate_number="95"]
The term “blighted ovum”, also known as an “anembryonic pregnancy” (nonviable pregnancy) may not be as commonly known, but it is also termed as missed abortion or a silent or missed miscarriage. It occurs when a fertilised egg implants in the uterus but the embryo does not grow.
A blighted ovum may also occur in a twin pregnancy. In this instance, it is called a blighted twin, one of the fertilised eggs fails to develop properly while the second develops normally, completely unaffected by the blighted twin.
What can cause a blighted ovum?
Once the egg is fertilised and implants in the uterus and the placenta and membrane begins to develop. The fetus fails to form or stops developing very early on causing the pregnancy to miscarry, usually between 7 and 12 weeks. A blighted ovum often happens so early in a pregnancy that the woman never knew she was pregnant. It happened because your body would recognise that there are abnormal chromosomes in a fetus and naturally does not try to carry on with the pregnancy because the fetus will not develop into a normal, healthy baby. This occurs because of abnormal cell division, or poor quality sperm or egg.
It happened because your body would recognise that there are abnormal chromosomes in a fetus and naturally does not try to carry on with the pregnancy because the fetus will not develop into a normal, healthy baby. This occurs because of abnormal cell division, or poor quality sperm or egg.
Miscarriage may also be caused by:
- ectopic pregnancy
- molar pregnancy
- bleeding during pregnancy and others.
Signs of blighted ovum
Most of the time, blighted ovum occurs very early in pregnancy – before most women even realise they are pregnant.
- Just like with a normal pregnancy you may even begin to experience the early pregnancy signs and symptoms.
- Sometimes, symptoms of blighted ovum can be mistaken as dysmenorrheal symptoms because of some cramping and minor spotting or bleeding, and then ends with your body flushing out the uterine lining and you have a period which may be heavier than normal.
- In some cases, women simply assume that they are having early pregnancy, as everything appears to be normal.
 It is caused by Human chorionic gonadotrophin (hCG) levels which continue to raise and the placenta continues to grow and support itself.
It is caused by Human chorionic gonadotrophin (hCG) levels which continue to raise and the placenta continues to grow and support itself.
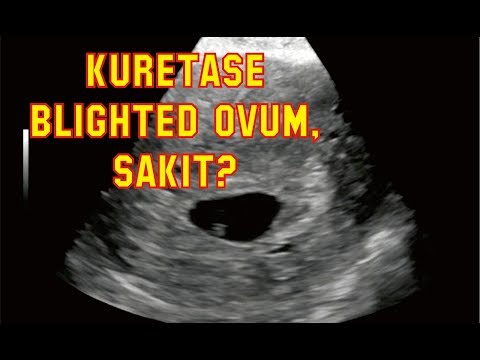
This type of miscarriage is usually diagnosed using ultrasound that can be usually done on the 8th week of pregnancy. It will show a large gestational sac, but no embryo. Many doctors use the term “early pregnancy failure,” instead of “blighted ovum” to describe this common type of miscarriage that accounts for approximately 50 percent of first trimester miscarriages.
Click here to know more about miscarriage.
The Criteria For A Diagnosis Of Blighted Ovum Are:
- Failure to identify an embryo in a gestational sac measuring at least 20 mm via transabdominal ultrasound.
- Failure to identify an embryo in a gestational sac measuring approximately 18mm or more via transvaginal ultrasound.
- Failure to identify a yolk sac in a gestational sac measuring 13mm or more.
Diagnosis and misdiagnoses of blighted ovum
Miscarriage – It is needed to expel the gestational sac and accumulated tissue by the end of your first trimester, though it can happen sooner than that.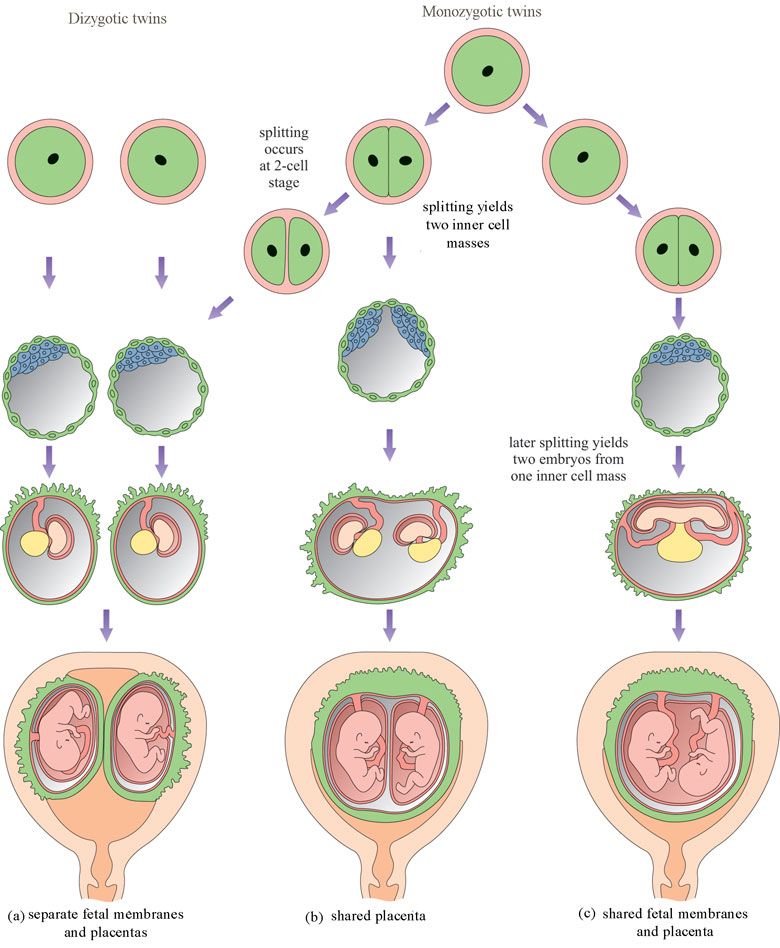 The miscarriage process can take weeks, though, and once you find out you aren’t pregnant; you may be too emotional about it or would make you feel physically uncomfortable to wait for a spontaneous miscarriage.
The miscarriage process can take weeks, though, and once you find out you aren’t pregnant; you may be too emotional about it or would make you feel physically uncomfortable to wait for a spontaneous miscarriage.
You may be able to use medication to speed up the miscarriage process. It can be managed medically, using drugs which facilitate the expulsion of the uterine contents. The drugs are usually administered orally and vaginally. The oral tablet is usually taken first followed by the vaginal tablet 24 to 48 hours later. The miscarriage will conclude shortly after this.
If there are instances like significant bleeding or signs of infection, it is unsafe to wait for a miscarriage. You can also have a dilation and curettage (D&C) or what is referred to as “raspa” in local parlance which can be carried out as a day procedure to remove the tissue. Though, most doctors do not recommend a D&C for an early pregnancy loss as it is believed that a woman’s body is capable of passing tissue on its own and there is no need for an invasive surgical procedure with a risk of complications.
Is misdiagnosis possible?
Majority of diagnosed miscarriages are in fact miscarriages. However, it is believe that there are few pregnant women that are misdiagnosed with a blighted ovum. Online testimonies show that most of them were misdiagnosed of early pregnancy failure when they consulted for a scan earlier that the eight week of their pregnancy.
The beginnings of a developing baby typically become visible on a transvaginal ultrasound around 5 to 6 weeks of pregnancy and on an abdominal ultrasound as late as 6 to 7 weeks of pregnancy. And if the dates of the pregnancy are even a little bit off, a viable pregnancy could theoretically be misdiagnosed as a blighted ovum.
Tips to avoid blighted ovum misdiagnoses
- Wait until you are entering your 11th or 12 weeks for an ultrasound. Except if you show signs of complications such as infection or pain, an earlier ultrasound may be needed.
- Don’t get anxious with the hCG levels – hCG levels are a very poor indicator of a blighted ovum.

- Do Not Read too Much about Pregnancy Symptoms – There are times that you can read in a site that if you lose pregnancy symptoms, this probably is a blighted ovum or miscarriage. Again, this is not necessarily true. As a matter of fact, pregnancy symptoms may persist until you have a true diagnosis. This is a result of the hCG and not the empty gestational sac. The hCG is what triggers symptoms and, as stated, hCG can rise even with empty sacs.
- Time Is The Only True Test of a Blighted Ovum – It is believed by most health care professionals that having a natural miscarriage before ten weeks is preferable. But most misdiagnosed blighted ova are seen by ten weeks.
- Get A Second Opinion – You can always find a new doctor. If you have no complications, you can ask to wait out the diagnosis. If you feel unsure to end your pregnancy or feel your doctor is not doing enough, find a new doctor who is willing to listen to your concerns.
FAQ (Frequently Asked Questions)
Can anything be done to prevent a blighted ovum?
Unfortunately, there is nothing that can be done to prevent a blighted ovum. A blighted ovum is often a one-time occurrence and rarely experienced by a woman again. It is believed that low progesterone may be a factor in early pregnancy loss and progesterone supplements have been shown to lower the miscarriage risk in some women with recurrent miscarriages. The importance of progesterone supplements during early pregnancy shows that it has saved some pregnancies. If you believe that progesterone may be a problem, try to have your progesterone tested as early as possible.
A blighted ovum is often a one-time occurrence and rarely experienced by a woman again. It is believed that low progesterone may be a factor in early pregnancy loss and progesterone supplements have been shown to lower the miscarriage risk in some women with recurrent miscarriages. The importance of progesterone supplements during early pregnancy shows that it has saved some pregnancies. If you believe that progesterone may be a problem, try to have your progesterone tested as early as possible.
When can I be pregnant after a blighted ovum?
Most women might want to wait a couple of months just to give the body a rest, and to feel emotionally ready, before trying again for a baby. But after having a blighted ovum, you’ll probably get your period again in four to six weeks after you miscarry or have the tissue removed. Some doctors say you can start trying to conceive again after this first period, but others recommend that you wait until you’ve been through another menstrual cycle.
It is natural to be very anxious that you may have a miscarriage again. But statistically, most women have a high rate of successful viable pregnancy the next time they conceive. Early scan may be recommended to reassure you.When you get pregnant again, wait until you are more than six weeks pregnant, or better still, more than seven or eight weeks pregnant, if you want to avoid the uncertainty that very early scans may bring. Once a heartbeat has been seen, the pregnancy is said to be viable and the chance of a successful outcome is much better.
Is it possible to have a recurrent blighted ovum?
This question will probably be on your mind when you start trying to get pregnant again, having suffered a blighted ovum doesn’t mean that are at a higher risk of miscarrying again. Blighted ovum will have no bearing whatsoever on future pregnancies. The chances of a normal pregnancy, following a blighted ovum, are not diminished in any way.
Coping
Early pregnancy failure (Blighted ovum) is a traumatic experience to a woman when it comes to her life unexpectedly. Others may not understand why a woman grieves a blighted ovum though it may appear that there was never a baby. It is true that the baby did not develop enough to be visible on ultrasound, but a conception did occur and the pregnancy did exist — and it is OK to grieve the loss of the baby.
Others may not understand why a woman grieves a blighted ovum though it may appear that there was never a baby. It is true that the baby did not develop enough to be visible on ultrasound, but a conception did occur and the pregnancy did exist — and it is OK to grieve the loss of the baby.
If diagnosed with a blighted ovum and feels unsure of the diagnosis. Consider postponing any treatment decisions until you check with your regular doctor or ask for a second opinion. If your doctor feels there is any uncertainty about the diagnosis, the doctor will most likely ask the woman to return for a follow up ultrasound in a few days or a week. Waiting can be frustrating and stressful, but it is a good way for doctors to avoid the possibility of misdiagnosis.
Multiple pregnancy
Author: Mikheeva Natalia Grigoryevna, Malyshok magazine
A multiple pregnancy is a pregnancy in which two or more fetuses develop simultaneously in the uterus. Multiple pregnancy occurs in 0. 4 - 1.6% of all pregnancies. Recently, there has been an obvious trend towards an increase in the incidence of such pregnancies due to the active use of assisted reproduction technologies, including in vitro fertilization (IVF). nine0005
4 - 1.6% of all pregnancies. Recently, there has been an obvious trend towards an increase in the incidence of such pregnancies due to the active use of assisted reproduction technologies, including in vitro fertilization (IVF). nine0005
Types of multiple pregnancies
Children born in multiple pregnancies are called TWINS. There are two main types of twins: monozygotic (identical, homologous, identical, similar) and dizygotic (fraternal, heterologous, different). African countries have the highest twin birth rate, Europe and the USA have an average rate, and Asian countries have a low rate.
Dizygotic (fraternal) twins are more common (in 66-75% of all twins). The birth rate of dizygotic twins varies from 4 to 50 per 1000 births. Dizygotic twins occur when two separate eggs are fertilized. The maturation of two or more eggs can occur both in one ovary and in two. The predisposition to develop dizygotic twins may be maternally inherited. Dizygotic twins can be either same-sex or opposite-sex, they look like each other like ordinary brothers and sisters.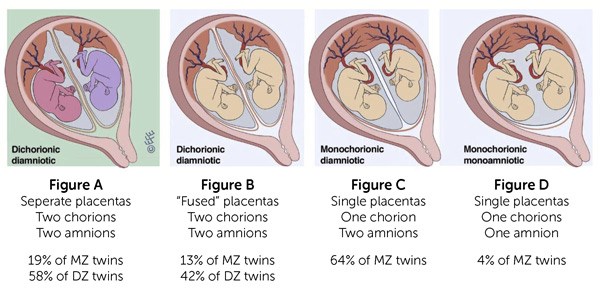 With fraternal twins, two placentas are always formed, which can be very close, even touching, but they can always be separated. Two fruit spaces (i.e., fetal bladders or two “houses”) are separated from each other by a septum consisting of two chorionic and two amniotic membranes. Such twins are called dizygotic dichorionic diamniotic twins. nine0005
With fraternal twins, two placentas are always formed, which can be very close, even touching, but they can always be separated. Two fruit spaces (i.e., fetal bladders or two “houses”) are separated from each other by a septum consisting of two chorionic and two amniotic membranes. Such twins are called dizygotic dichorionic diamniotic twins. nine0005
Monozygotic (identical) twins are formed as a result of the separation of one fetal egg at various stages of its development. The frequency of birth of monozygotic twins is 3-5 per 1000 births. The division of a fertilized egg into two equal parts can occur as a result of a delay in implantation (immersion of the embryo in the uterine mucosa) and oxygen deficiency, as well as due to a violation of the acidity and ionic composition of the medium, exposure to toxic and other factors. The emergence of monozygotic twins is also associated with the fertilization of an egg that had two or more nuclei. If the separation of the fetal egg occurs in the first 3 days after fertilization, then monozygotic twins have two placentas and two amniotic cavities, and are called monozygotic diamniotic dichoriones (Fig. A). If the division of the ovum occurs between 4 - 8 days after fertilization, then two embryos will form, each in a separate amniotic sac. Two amniotic sacs will be surrounded by a common chorionic membrane with one placenta for two. Such twins are called monozygotic diamniotic monochorionic twins (Fig. B). If division occurs by 9- 10th day after fertilization, then two embryos are formed with a common amniotic sac and placenta. Such twins are called monozygotic monoamniotic monochorionic (Fig. B) If the egg is separated at a later date on the 13th - 15th day after conception, the separation will be incomplete, which will lead to the appearance of conjoined (undivided, Siamese) twins. This type is quite rare, approximately 1 observation in 1500 multiple pregnancies or 1: 50,000 - 100,000 newborns. Monozygotic twins are always the same sex, have the same blood type, have the same eye color, hair, skin texture of the fingers, and are very similar to each other. nine0005
A). If the division of the ovum occurs between 4 - 8 days after fertilization, then two embryos will form, each in a separate amniotic sac. Two amniotic sacs will be surrounded by a common chorionic membrane with one placenta for two. Such twins are called monozygotic diamniotic monochorionic twins (Fig. B). If division occurs by 9- 10th day after fertilization, then two embryos are formed with a common amniotic sac and placenta. Such twins are called monozygotic monoamniotic monochorionic (Fig. B) If the egg is separated at a later date on the 13th - 15th day after conception, the separation will be incomplete, which will lead to the appearance of conjoined (undivided, Siamese) twins. This type is quite rare, approximately 1 observation in 1500 multiple pregnancies or 1: 50,000 - 100,000 newborns. Monozygotic twins are always the same sex, have the same blood type, have the same eye color, hair, skin texture of the fingers, and are very similar to each other. nine0005
Twin births occur once in 87 births, triplets - once in 87 2 (6400) twins, quadruples - once in 87 3 (51200) triplets, etc. (according to the Gallin formula). The origin of triplets, quadruplets, and more twins varies. So, triplets can be formed from three separate eggs, from two or one egg. They can be monozygotic and heterozygous. Quadruples can also be identical and fraternal.
(according to the Gallin formula). The origin of triplets, quadruplets, and more twins varies. So, triplets can be formed from three separate eggs, from two or one egg. They can be monozygotic and heterozygous. Quadruples can also be identical and fraternal.
Features of the course of multiple pregnancy
In case of multiple pregnancies, the woman's body is subject to increased requirements. All organs and systems function with great tension. In connection with the displacement of the diaphragm by the enlarged uterus, the activity of the heart becomes difficult, shortness of breath, fatigue occur. Enlargement of the uterus, especially towards the end of pregnancy, leads to compression of the internal organs, which is manifested by impaired bowel function, frequent urination, and heartburn. Almost 4-5 times more often there is the development of preeclampsia, which is characterized by an earlier onset, a protracted and more severe clinical course, often combined with acute pyelonephritis of pregnant women. Due to the increased need and consumption of iron, iron deficiency anemia often develops in pregnant women. Significantly more often than with a singleton pregnancy, complications such as bleeding during pregnancy and childbirth, anomalies in labor, and a low location of the placenta are observed. Often, with multiple pregnancies, abnormal positions of the fetus occur. One of the most common complications in multiple pregnancy is its premature termination. Preterm birth is observed in 25-50% of cases of such pregnancies. nine0005
Due to the increased need and consumption of iron, iron deficiency anemia often develops in pregnant women. Significantly more often than with a singleton pregnancy, complications such as bleeding during pregnancy and childbirth, anomalies in labor, and a low location of the placenta are observed. Often, with multiple pregnancies, abnormal positions of the fetus occur. One of the most common complications in multiple pregnancy is its premature termination. Preterm birth is observed in 25-50% of cases of such pregnancies. nine0005
The development of term twins is normal in most cases. However, their body weight is usually less (by 10% or more) than in singleton pregnancies. With twins, the weight of children at birth less than 2500 g is observed in 40-60%. The low weight of twins is most often due to insufficiency of the uteroplacental system, which is not able to adequately provide several fetuses with nutrients, trace elements and oxygen. The consequence of this is a delay in the development of the fetus, which is a common occurrence in multiple pregnancies. The mass of twins, respectively, decreases in proportion to their number (triplets, quadruplets, etc.). nine0005
The mass of twins, respectively, decreases in proportion to their number (triplets, quadruplets, etc.). nine0005
With monochorionic twins in the placenta, anastomoses are often formed between the vascular systems of the fetus, which can lead to a serious complication - the syndrome of feto-fetal transfusion. In this case, there is a redistribution of blood from one fetus to another, the so-called "stealing". The severity of feto-fetal transfusion (mild, moderate, severe) depends on the degree of redistribution of blood through the anastomoses, which vary in size, number and direction.
Diagnosis in multiple pregnancy
The most reliable method for diagnosing multiple pregnancies is ultrasound, which allows not only early diagnosis of multiple pregnancies, but also to determine the position and presentation of fetuses, localization, structure and number of placentas, the number of amniotic cavities, the volume of amniotic fluid, congenital malformations and antenatal fetal death, the state of the fetus from a functional point of view, the nature of the uteroplacental and fetal-placental blood flow. nine0005
nine0005
In multiple pregnancies, due to the higher risk of complications, ultrasound monitoring is performed more frequently than in singleton pregnancies. With dizygotic twins, about once every 3-4 weeks, with monozygotic twins - once every 2 weeks.
In addition, examinations and control of clinical tests are carried out with great care, and CTG is regularly recorded from 28 weeks of pregnancy.
Birth management
Indications for caesarean section associated with multiple pregnancies are triplets (quadruple), the transverse position of both or one of the fetuses, breech presentation of both fetuses or the first of them, and not associated with multiple pregnancy - fetal hypoxia, anomalies labor activity, prolapse of the umbilical cord, extragenital pathology of the mother, severe gestosis, placenta previa and abruption, etc.
-
ECO
In the department of assisted reproductive technologies of the Maternity Hospital No. 2
2
, IVF is performed at the expense of the Republican budget for couples
who have received a positive decision from the Minsk city or regional commissions to provide one free IVF attempt.
No drug supply problem. There is no waiting list. nine0005 -
Farewoman
-
Individual care for patients
-
Ultrasound diagnostics
- Pregnant women often complain of fatigue and shortness of breath, which increases towards the end of pregnancy. The cause of shortness of breath is a difficulty in the activity of the heart due to a significant displacement of the diaphragm by the bottom of the uterus, the size of which is larger in multiple pregnancy than in singleton. nine0054
- Often there is a dilation of the veins of the lower extremities. By the end of pregnancy, there is often an increase in the urge to urinate due to the pressure of a large fetus on the bladder.
- Pregnant women often complain of heartburn and constipation.
- In multiple pregnancies, toxicosis occurs more often than in singleton pregnancies: vomiting, salivation, edema, nephropathy, eclampsia.
- With twins, polyhydramnios of one of the fetuses is often found, which leads to a sharp increase and overstretching of the uterus, shortness of breath, tachycardia and other disorders.
 Polyhydramnios is more common in one of the identical twins. In some cases, the polyhydramnios of one twin is accompanied by an oligohydramnios of the other fetus. nine0054
Polyhydramnios is more common in one of the identical twins. In some cases, the polyhydramnios of one twin is accompanied by an oligohydramnios of the other fetus. nine0054 - Premature termination of multiple pregnancies often occurs.
- With twins, preterm birth is observed in at least 25% of women.
- Triplets are more likely to miscarry than twins. The greater the number of gestated fetuses, the more often preterm births are observed.
- Development of term twins is normal in most cases. However, their body weight is usually less than that of single fetuses. Often there is a difference in body weight of twins by 200-300 g, and sometimes more. nine0054
- Uneven development of twins is associated with unequal intake of nutrients from a single placental circulation.
- Often there is a difference not only in weight, but also in the length of the body of the twins. In connection with this, the theory of supergenesis (superfoetatio) was put forward.
 Proponents of this hypothesis believe that fertilization of eggs of different ovulation periods is possible, i.e., the onset of a new pregnancy in the presence of an already existing, previously occurring, pregnancy. nine0054
Proponents of this hypothesis believe that fertilization of eggs of different ovulation periods is possible, i.e., the onset of a new pregnancy in the presence of an already existing, previously occurring, pregnancy. nine0054 - Due to the uneven delivery of nutrients and oxygen, a significant developmental disorder and even death of one of the twins can occur. This is more commonly seen in identical twins. The dead fetus is squeezed by the second, well-growing fetus, the amniotic fluid is absorbed, the placenta undergoes regression. The compressed mummified fetus ("paper fetus") is released from the uterus along with the placenta after the birth of a live twin. Polyhydramnios of one fetus, which occurs during multiple pregnancies, often also prevents the other twin from developing correctly. With pronounced polyhydramnios, certain anomalies in the development of the fetus, which grows with an excess of amniotic fluid, are often observed. Rarely, fused twins are born (fusion can be in the head, chest, abdomen, pelvis) and twins with other malformations.
 nine0054
nine0054 - The position of the fetuses in the uterine cavity in most cases (about 90%) is normal. In the longitudinal position, different presentation options are observed: both fetuses are presented with the head, both with the pelvic end, one with the head, and the other with the pelvic end. With longitudinal presentation, one fetus may be behind the other, which makes diagnosis difficult. Less commonly observed is the longitudinal position of one fetus and the transverse position of the other. The most rare is the transverse position of both twins. nine0054
- The position of the twins in the uterus, both fetuses are presented with the head, one fetus is presented with the head, the second - with the pelvic end, both fetuses are in the transverse position
- In case of multiple pregnancies, women are taken into special account and carefully monitored. When the earliest signs of complications appear, the pregnant woman is sent to the pregnancy pathology department of the maternity hospital.
 Given the frequent occurrence of preterm birth, it is recommended that a pregnant woman with twins be sent to the maternity hospital 2 to 3 weeks before delivery, even in the absence of complications. nine0054
Given the frequent occurrence of preterm birth, it is recommended that a pregnant woman with twins be sent to the maternity hospital 2 to 3 weeks before delivery, even in the absence of complications. nine0054 - The enlargement of the uterus in multiple pregnancies occurs faster than in pregnancy with one fetus, so the size of the uterus does not correspond to the gestational age. The bottom of the uterus is usually high, especially at the end of pregnancy, the circumference of the abdomen during this period reaches 100-110 cm or more.
- The following signs are unstable and not sufficiently reliable: a) deepening of the uterine fundus (saddle uterus), the formation of which is associated with protrusion of the corners of the uterus with large parts of the fetus; b) the presence of a longitudinal depression on the anterior wall of the uterus, which is formed as a result of the fruits that are in a longitudinal position adjacent to each other; c) the presence of a horizontal groove on the anterior wall of the uterus with the transverse position of the fetus. nine0054
- The small size of the presenting head with a significant volume of the pregnant uterus and the high standing of its bottom also make it possible to suspect a multiple pregnancy. The presence of this sign is explained by the fact that the study determines the head of one and the pelvic end (in the bottom of the uterus) of another fetus, which lies slightly higher.
- Feeling the movement of the fetus in different places and probing parts of the fetus in different parts of the abdomen (both on the right and on the left) also indicate multiple pregnancies.
 nine0054
nine0054
Curious facts are
0
, how many are the Geminis? up to 80 million pairs of twins.
The number of twins born in relation to the total number of newborns in different countries and on different continents is different, but in general the trend is such that it continues to grow. Compared with the 60s, the percentage of twins has increased from 1.18 to 2.78, that is, almost 2.5 times. nine0005
The largest number of children
The largest number of children born to one mother, according to official data, is 69. According to reports made in 1782, between 1725 and 1765. The wife of a Russian peasant Fyodor Vasiliev gave birth 27 times, giving birth to twins 16 times, triplets 7 times and 4 twins 4 times. Of these, only 2 children died in infancy.
The wife of a Russian peasant Fyodor Vasiliev gave birth 27 times, giving birth to twins 16 times, triplets 7 times and 4 twins 4 times. Of these, only 2 children died in infancy.
The most prolific mother of our contemporaries is considered to be Leontina Albina (or Alvina) of San Antonio, Chile, who at 1943-81 years gave birth to 55 children. As a result of the first 5 pregnancies, she gave birth to triplets, and exclusively male.
Most birthed
The record 38 births are said to be Elizabeth Greenhillies Abbots-Langley, c. Hertfordshire, UK. She had 39 children - 32 daughters and 7 sons.
The largest number of multiple births in one family
Maddalena Pomegranate from Italy (b. 1839) had triplets born 15 times. nine0071 There is also information about the birth on May 29, 1971 in Philadelphia, Pennsylvania, USA, and in May 1977 in Bagarhat, Bangladesh, 11 twins. In both cases, no child survived.
Most fertile pregnancies
Dr. Gennaro Montanino, Rome, Italy, claimed to have removed, in July 1971, the embryos of 10 girls and 5 boys from the uterus of a 35-year-old woman who was 4 months pregnant. This unique case of 15-fertility was the result of infertility pills. nine0071 9 children - the largest number in one pregnancy - were born on June 13, 1971 by Geraldine Broadrick in Sydney, Australia. 5 boys and 4 girls were born: 2 boys were stillborn, and none of the rest survived more than 6 days.
Gennaro Montanino, Rome, Italy, claimed to have removed, in July 1971, the embryos of 10 girls and 5 boys from the uterus of a 35-year-old woman who was 4 months pregnant. This unique case of 15-fertility was the result of infertility pills. nine0071 9 children - the largest number in one pregnancy - were born on June 13, 1971 by Geraldine Broadrick in Sydney, Australia. 5 boys and 4 girls were born: 2 boys were stillborn, and none of the rest survived more than 6 days.
The birth of 10 twins (2 boys and 8 girls) is known from reports from Spain (1924), China (1936) and Brazil (April 1946).
The father with many children
The largest father in the history of Russia is Yakov Kirillov, a peasant from the village of Vvedensky, who in 1755 was presented to the court in connection with this (he was then 60 years old). The first wife of a peasant gave birth to 57 children: 4 times four, 7 times three, 9once twice and 2 times once. The second wife gave birth to 15 children. Thus, Yakov Kirillov had 72 children from two wives.
Thus, Yakov Kirillov had 72 children from two wives.
Longest Birth Intervals for Multiple Pregnancies
Peggy Lynn of Huntington Pennsylvania, USA, gave birth to a girl, Hanna, on November 11, 1995, and the second of the twins, Erika, only 84 days later (February 2, 1996).
Siamese twins
United twins became known as "Siamese" after Chang and Eng Bunkers were born fused in the area of the sternum on May 11, 1811 in the Maeklong region of Siam (Thailand). They married Sarah and Adelaide Yates of pc. North Carolina, USA, and had 10 and 12 children, respectively. They died in 1874, and with a difference of 3 hours. nine0005
The science of twins - gemellology.
"Secret language"
Twins often talk to each other in a language that others do not understand. This phenomenon is called cryptophasia.
Left-handed twins
18-22% of left-handed twins (for non-twins this percentage is 10).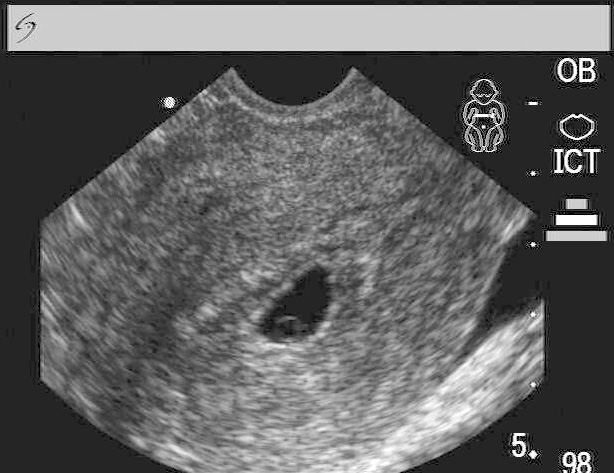
articles from specialists of the clinic "Mother and Child"
Arifullina Claudia Viktorovna nine0005
Gastroenterologist
Clinical Hospital "AVICENNA" GC "Mother and Child"
There is data on the frequency of twins in case of anomalies in the development of the uterus, characterized by its bifurcation (bicornuate uterus, having a septum in the cavity, etc.). The cause of polyembryony may be the separation of blastomeres (in the early stages of crushing), resulting from hypoxia, cooling, acidity and ionic composition of the medium, exposure to toxic and other factors. Multiple pregnancy can occur: as a result of the fertilization of two or more simultaneously mature eggs, as well as the development of two or more embryos from one fertilized egg. nine0005
Twins formed from two (three, etc.) eggs are called dizygotic (polyzygotic), those arising from one are called identical. The origin of fraternal twins (polyzygotic twins): the simultaneous maturation (and ovulation) of two or more follicles in one ovary is possible.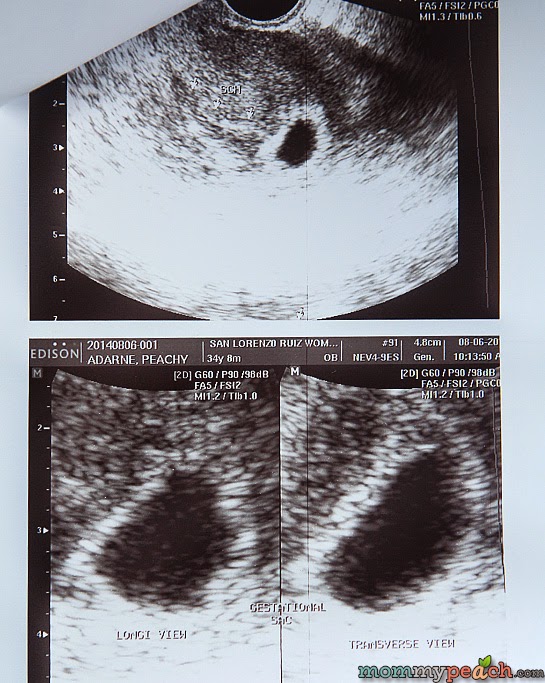 There may be maturation of two or more follicles and ovulation in both ovaries.
There may be maturation of two or more follicles and ovulation in both ovaries.
A third way of the origin of fraternal (multi-ovular) twins is possible - the fertilization of two or more eggs that have matured in one follicle. The origin of identical twins: most often, the occurrence of identical twins is associated with the fertilization of an egg that has two or more nuclei. a single embryonic germ in the stage of crushing is divided into two parts; from each part an embryo (fruit) is formed. Twin twin. Fertilized eggs develop on their own. After penetration into the mucous membrane, each embryo develops its own aqueous and fleecy membranes; in the future, each twin forms its own placenta with an independent network of vessels, each fetal egg, except for the chorion and amnion, has an independent capsular membrane (decidua capsularis). In some cases, anastomoses are formed between the vessels of independent placentas. Twins can be same-sex (both boys or both girls) or different-sex (boy and girl). Their blood type can be the same or different. Identical twin. Identical twins have a common capsular and fleecy membrane and a common placenta; the vessels (both arterial and venous) of both twins in the placenta communicate with the help of numerous anastomoses. The water membrane of each twin is separate, the septum between the fetal sacs consists of two water membranes (biamniotic twins). nine0005
Their blood type can be the same or different. Identical twin. Identical twins have a common capsular and fleecy membrane and a common placenta; the vessels (both arterial and venous) of both twins in the placenta communicate with the help of numerous anastomoses. The water membrane of each twin is separate, the septum between the fetal sacs consists of two water membranes (biamniotic twins). nine0005
Identical twins always belong to the same sex (both boys or both girls), look alike, have the same blood group.
In fraternal twins, the membranes in the septum are arranged as follows: amnion - chorion, chorion - amnion; with monozygotic amnion-amnion.
Important signs for the diagnosis are: blood type (and other blood factors), eye color, hair color, skin texture of the fingertips, shape and location of teeth. In identical twins, these signs are completely the same. Fraternal twins share the same similarities as normal siblings. nine0071
MULTIPLE PREGNANCY
With multiple pregnancy, increased demands are made on the woman's body: the cardiovascular system, lungs, liver, nights and other organs function with great stress.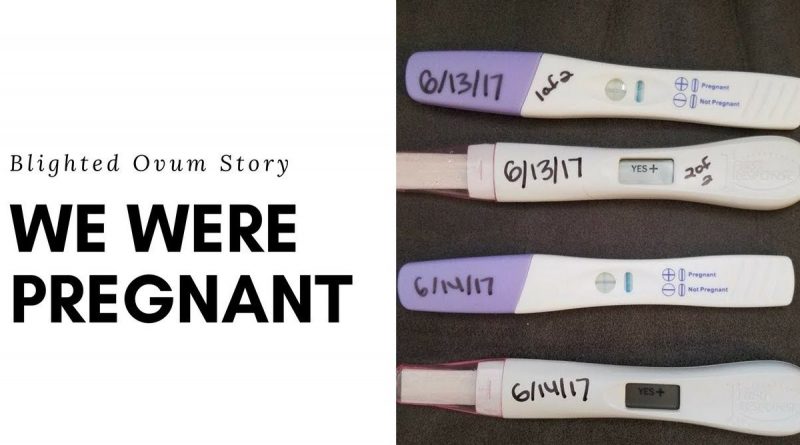 In this regard, multiple pregnancies are more difficult than single pregnancies.
In this regard, multiple pregnancies are more difficult than single pregnancies.
RECOGNITION OF MULTIPLE PREGNANCY
Diagnosis of multiple pregnancy often presents significant difficulties, especially in its first half. In the second half, towards the end of pregnancy, the recognition of twins (triplets) is facilitated. However, diagnostic errors occur during the study at the end of pregnancy and even during childbirth.
When recognizing a multiple pregnancy, the following signs are taken into account: nine0071
Make an appointment
to the doctor - Arifullina Claudia Viktorovna
Clinical Hospital "AVICENNA" GC "Mother and Child"
GastroenterologyPediatric Gastroenterology
By clicking on the submit button, I consent to the processing of personal data
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
nine0002 Clinical Hospital "AVICENNA" Group of Companies "Mother and Child"Novosibirsk Center for Reproductive MedicineAll directionsGynecological proceduresSpecialist consultations (adults)Specialist consultations (children)Laboratory of molecular geneticsGeneral clinical studiesProcedure roomTherapeutic studiesUltrasound examinations for adults
nine0002.Gynecological procedures
02.