Blister on my nose
8 Nose Blister Causes | How to Treat a Blister on the Nose
Skin abscess
A skin abscess is a large pocket of pus that has formed just beneath the skin. It is caused by bacteria getting under the skin, usually through a small cut or scratch, and beginning to multiply. The body fights the invasion with white blood cells, which kill some of the infected tissue but form pus within the cavity that remains.
Symptoms include a large, red, swollen, painful lump of pus anywhere on the body beneath the skin. There may be fever, chills, and body aches from the infection.
If not treated, there is the risk of an abscess enlarging, spreading, and causing serious illness.
Diagnosis is made through physical examination.
A small abscess may heal on its own, through the body's immune system. But some will need to be drained or lanced in a medical provider's office so that the pus can be cleaned out. Antibiotics are usually prescribed.
Keeping the skin clean, and using only clean clothes and towels, will help to make sure that the abscess does not recur.
Rarity: Common
Top Symptoms: rash with bumps or blisters, red rash, red skin bump larger than 1/2 cm in diameter, pus-filled rash, rash
Symptoms that always occur with skin abscess: rash with bumps or blisters
Urgency: Primary care doctor
Relapsing polychondritis
Relapsing polychondritis is an episodic, inflammatory and destructive disorder involving primarily cartilage of the ear and nose. It can also potentially affect the eyes, tracheobronchial tree, heart valves, kidneys, joints, skin, and blood vessels.
You should visit your primary care physician for mild severity of relapsing polychondritis. Medications such as NSAIDs and steroids are generally prescribed.
Pimple
Pimples are also called comedones, spots, blemishes, or "zits." Medically, they are small skin eruptions filled with oil, dead skin cells, and bacteria.
Pimples often first start appearing at puberty, when hormones increase the production of oil in the skin and sometimes clog the pores.
Most susceptible are teenagers from about ages 13 to 17.
Symptoms include blocked pores that may appear flat and black on the surface, because the oil darkens when exposed to the air; blocked pores that appear white on the surface because they have closed over with dead skin cells; or swollen, yellow-white, pus-filled blisters surrounded by reddened skin.
Outbreaks of pimples on the skin can interfere with quality of life, making the person self-conscious about their appearance and causing pain and discomfort in the skin. A medical provider can help to manage the condition, sometimes through referral to a dermatologist.
Diagnosis is made through physical examination.
Treatment involves improving diet; keeping the skin, hair, washcloths, and towels very clean; and using over-the-counter acne remedies.
Rarity: Common
Top Symptoms: pink or red facial bump, small facial lump, painful facial bump, marble sized facial lump
Symptoms that always occur with pimple: pink or red facial bump
Urgency: Self-treatment
Non-specific nose rash
A rash is an area of irritated or swollen skin. Often, rashes are unidentifiable and some variation of normal. For example, scratching one's arm causes it to turn red (which is caused by mast cells releasing chemicals into the local area), but that's completely normal.
Often, rashes are unidentifiable and some variation of normal. For example, scratching one's arm causes it to turn red (which is caused by mast cells releasing chemicals into the local area), but that's completely normal.
At this time, you do not need treatment for this rash. If it worsens, you may need to consult a physician.
Rarity: Common
Top Symptoms: nose redness
Symptoms that always occur with non-specific nose rash: nose redness
Urgency: Wait and watch
Granulomatosis with polyangiitis
Granulomatosis with polyangiitis, or shortened GPA, was formerly known as Wegener's granulomatosis. It is caused by inflammation of the blood vessels by the body's immune system. The inflammation can happen anywhere, but often affects the sinuses, lungs, and kidneys.
You should visit your primary care physician soon to provide an early diagnosis. Treatment of inflammatory diseases commonly involve prescription medications such as a steroid to decrease inflammation, and a cell-damaging medicine to kill abnormal cells.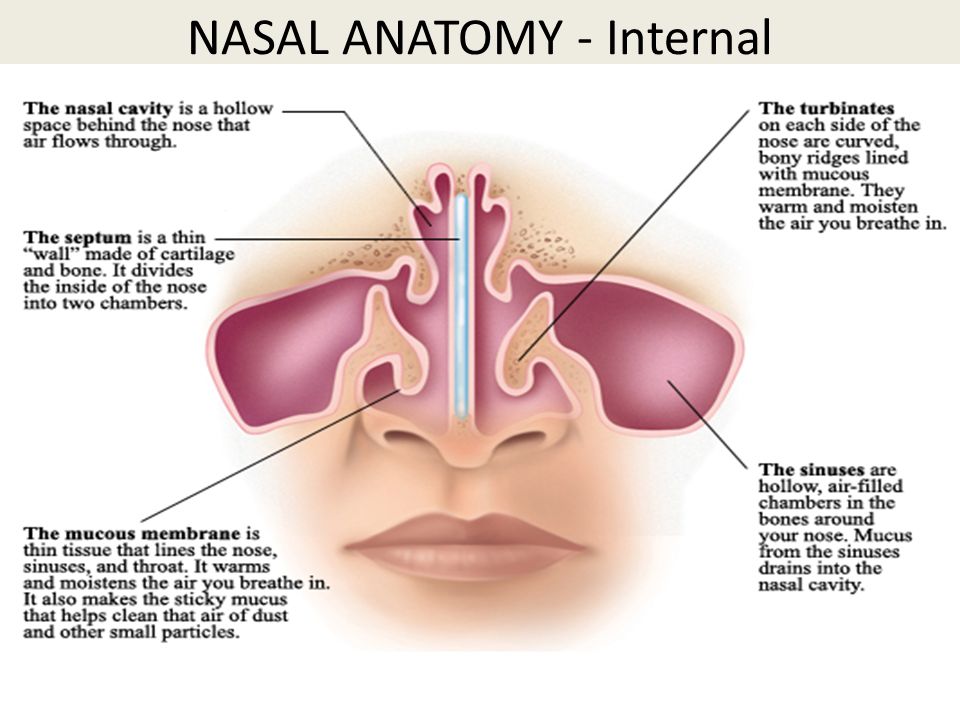
Chronic allergies
New-onset seasonal allergies, also called adult-onset seasonal allergies, are sensitivities to pollen, mold, and other irritants that cause nasal congestion, runny nose, sneezing, itchy eyes, and sore throat.
Seasonal allergies commonly begin in childhood but can start at any age, especially among those with a family history. Moving to a different geographic location may trigger the allergy in someone with a genetic predisposition. Anyone with asthma is more likely to experience adult-onset seasonal allergies.
Sometimes the symptoms are actually from "pregnancy rhinitis" – nasal congestion and sneezing due to the effects of pregnancy hormones on the nasal tissue.
A new-onset allergy is often thought to be a cold, but a cold will clear up without treatment. Allergies persist, never getting better or worse, and can interfere with quality of life.
Diagnosis is made by an allergist, who will use skin tests and blood tests.
There is no cure for seasonal allergies but the symptoms can be managed for greater comfort and relief. Antihistamines, corticosteroid nasal sprays, and immunotherapy or "allergy shots" can be very effective.
Antihistamines, corticosteroid nasal sprays, and immunotherapy or "allergy shots" can be very effective.
Rarity: Common
Top Symptoms: fatigue, irritability, trouble sleeping, runny nose, congestion
Symptoms that never occur with chronic allergies: fever, yellow-green runny nose, chills, muscle aches
Urgency: Self-treatment
Allergic contact dermatitis of the nose
Allergic contact dermatitis means the skin has touched something that provoked an allergic reaction, causing inflammation and irritation.
"Contact" means the allergic reaction came from touching something, not from consuming something. The first exposure to the substance sensitizes the immune system, and then the second exposure actually causes the symptoms.
The most common causes of allergic contact dermatitis are:
- Nickel, a metal often used in belt buckles, the buttons on pants, and jewelry, including piercing jewelry.
- Poison ivy.
- Various types of perfumes, including those founds in soaps, fabric softeners, and detergents.
- Of course, there are many more.
Symptoms include red, itching, scaling, flaking skin that may be painful due to the irritation and inflammation.
Diagnosis is made through first avoiding contact with any suspected substance, to see if the dermatitis clears. Patch testing can be done if the results are not certain.
Treatment involves fully avoiding the allergy-provoking substance and using topical steroid cream as prescribed. Cool compresses and calamine lotion can help to ease the discomfort.
Rarity: Common
Top Symptoms: nose itch, nose redness, scabbed area of the nose
Symptoms that always occur with allergic contact dermatitis of the nose: nose redness
Urgency: Self-treatment
Acne rosacea
Rosacea is a long-term disease that affects the skin and sometimes the eyes. It causes redness and breakouts. Acne rosacea is the type of Rosacea that causes pimples. Rosacea is most common in women and people with fair skin. It most often affects middle-aged and older adults.
It causes redness and breakouts. Acne rosacea is the type of Rosacea that causes pimples. Rosacea is most common in women and people with fair skin. It most often affects middle-aged and older adults.
You should visit your primary care physician, who could help with a treatment plan (no diagnostic testing necessary). Treatment can't cure you, but helps the symptoms and includes brimonide gel, laser therapy, and even an antibiotic.
Rarity: Common
Top Symptoms: facial redness, rough skin on the face, pink or red facial bump, nose redness, raised rash
Symptoms that always occur with acne rosacea: facial redness
Urgency: Primary care doctor
Wegener's granulomatosis
Wegener's granulomatosis, more recently re-named granulomatosis with polyangiitis, is a disorder in which a dysregulated immune system causes widespread inflammation of small blood vessels throughout the body. This results in slower or impaired blood flow to your nose, sinuses, throat, lungs, and kidneys.
Symptoms can be widespread and affect various parts of the body such as the eyes and ears or respiratory system, yet usually begin more generally with fever, fatigue, a loss of appetite, and weight loss. With treatment, a full recovery is possible; however, this condition can be fatal.
Treatments include immunosuppressive medications in order to control the disease in the short- and long-term.
Rarity: Ultra rare
Top Symptoms: fatigue, loss of appetite, joint pain, shortness of breath, fever
Urgency: Primary care doctor
How to Treat Sores Inside Nose
Back to Dealing with Cold Sores articles
Pretty much everyone has heard of cold sores. They're fairly common, if frustrating, blisters that appear near or around your mouth. But can cold sores appear elsewhere too like on your nose? Let's explore the answer to find out whether or not you can get cold sores near or on your nose and other conditions that may cause nose irritation.
Can you get nose cold sores?
Yes. Believe it or not, you can get cold sores in areas other than the most common spots near the mouth and lips. You can also get cold sore blisters on or around your nose and chin as well as on the lips and skin around the mouth. These nose cold sores should behave the same way a cold sore near the mouth does.1 Just like mouth cold sores, cold sores under the nose develop over time. These nose cold sore symptoms include:1
- Itching and tingling near your nose a day or two before the cold sore shows up
- Small, painful blisters form under, beside, or on your nose
- The blisters burst on their own after a few days, then crust over
- The blisters scab over, fall off, and heal after a period of about 10 days
Cold sores are caused by certain strains of the herpes simplex virus and can spread from contact with someone infected with the cold sore virus. Once infected, the virus typically lies dormant in nerve cells in the skin on your face. It depends on where the virus travels as to what part of the face the virus lives in and then comes back when you get a cold sore outbreak. Cold sores outbreaks can be triggered by the same things as cold sores near the mouth, such as viral infections, hormonal changes, stress, environmental exposure, injuries, fatigue, and more.2
It depends on where the virus travels as to what part of the face the virus lives in and then comes back when you get a cold sore outbreak. Cold sores outbreaks can be triggered by the same things as cold sores near the mouth, such as viral infections, hormonal changes, stress, environmental exposure, injuries, fatigue, and more.2
What to do if you get a nose cold sore
First, don't panic! A nose cold sore is just like any other, even if located somewhere else. Cold sores aren't generally dangerous and don’t cause permanent damage to the skin. Make sure to avoid picking your scab or popping the cold sore blister, which can increase the risk of secondary infections or scarring.1 When you have a cold sore, make sure to wash your hands after touching your face and do not share any items that may touch your face to prevent spreading the cold sore virus.
You can use soothing creams or ice to treat the symptoms of the cold sores, but you can't outright cure nose cold sores.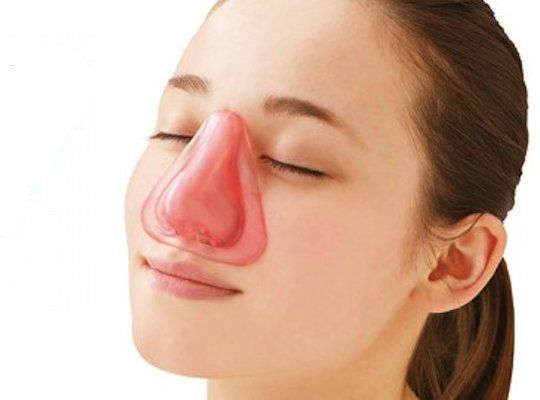 You can also use treatments like Abreva Cream to help heal your cold sore quicker when used at the first signs of an emerging cold sore.
You can also use treatments like Abreva Cream to help heal your cold sore quicker when used at the first signs of an emerging cold sore.
Other reasons for scabs or irritation near your nose
While irritation and blisters near your nose may be a cold sore, it's not the only condition that can cause irritation around your nose. Talk to your doctor and look into other irritation-causing conditions before deciding it's truly cold sores. Some causes of irritation near your nose include:3
Nose Injuries: The most obvious reason for irritation or scabs around your nose are nose injuries. If you run into something or fall on your face and injure your nose, it’s likely you'll have some degree of pain, swelling, and scabbing of injuries.
Inflammation: Nose inflammation can sometimes cause scabbing if you repeatedly rub your nose and cause an abrasion. Inflammation can be caused by allergies, sinusitis, or other chronic inflammatory conditions.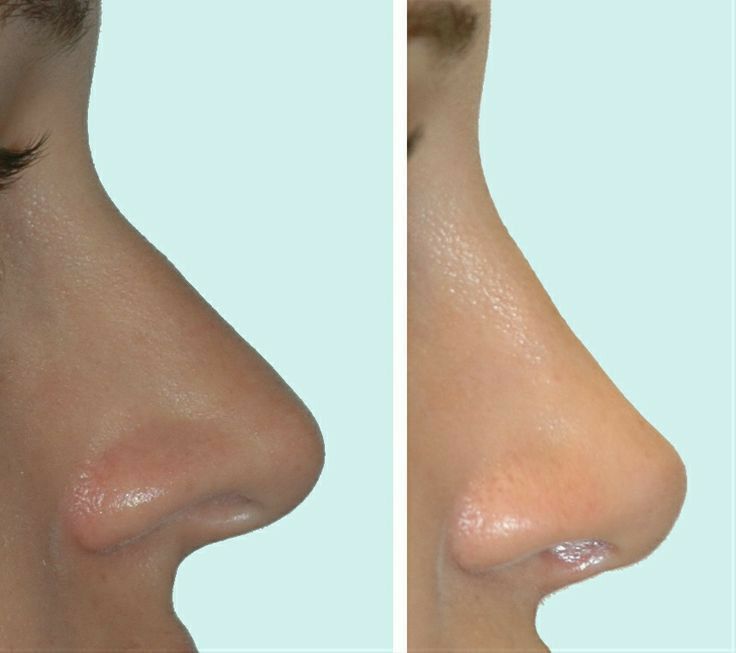
Dryness and Temperature Changes: Either very hot or cold environments as well as very dry air can damage your nasal lining, which may cause scabs or cause irritation.
Infections: It depends on the infection, but some can cause irritation to your nose and scabbing. The skin inside and around your nose is delicate and at risk of irritation.
When to talk to your doctor
Overall, if you're not sure as to what the cause of any blisters, irritation, or pain around or in your nose is, reach out to your doctor. They'll be able to examine and diagnose your condition confidently. In most cases, cold sores don't cause serious complications but you may be at a higher risk you have pre-existing conditions or a weakened immune system. 2 If your cold sore doesn't go away in the normal time span, continues to spread, or gets worse, it's best to talk to your doctor to get help.
Now that you know a little more about nose cold sores, learn more about what cold sores are, how to keep yourself healthy, and how to deal with cold sores more effectively.
SOURCES
1. Cold Sores. Better Health and Human Services. https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/cold-sores/ Accessed 1/29/2020. Referenced text is highlighted in source PDF.
2. Cold Sore. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/cold-sore/symptoms-causes/syc-20371017/ Accessed 1/29/2020. Referenced text is highlighted in source PDF.
3. What are the dangers of nose scabs? ENT Ear Nose & Throat Clinic. https://www.harleystreetent.com/blog/what-are-the-dangers-of-nose-scabs/ Accessed 1/29/2020. Referenced text is highlighted in source PDF.
Treatment of a furuncle in the nose - ENT clinic №1
Article rating
3.70 (Votes: 10)
Contents
- Reasons for the development of the disease
- Stages of development
- Symptoms of a boil in the nose
- Possible complications of the boil of the nose
- Treatment of a furuncle of the nose
Furuncle is an acute inflammation of the hair follicle (bulb) along with the sebaceous gland, adjacent areas of the skin and subcutaneous fat. The initial sections of the nose, called the vestibule of the nose, have a large number of hair follicles, and therefore it is there that boils most often develop. Less often they are found in the area of the tip of the nose, wings and slope of the nose, nasolabial fold.
The initial sections of the nose, called the vestibule of the nose, have a large number of hair follicles, and therefore it is there that boils most often develop. Less often they are found in the area of the tip of the nose, wings and slope of the nose, nasolabial fold.
Causes of disease
Leading role in the development of the disease has a local decrease in the protective properties of the mucous membrane and skin of the nose. The appearance of a furuncle of the nose is promoted by general hypothermia, beriberi, chronic overwork, the presence of diabetes, HIV infection, oncology and other diseases that reduce the local and general immunity of the body.
Stages of development
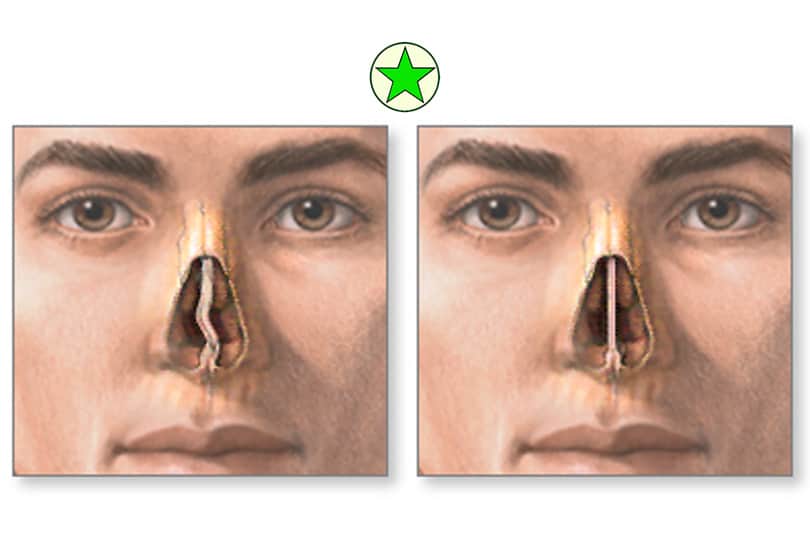
The first stage in the development of the disease is a traumatic injury to the skin and nasal mucosa (such as abrasion, scratch or cut), through which the infection enters deep into the tissue. Pathogenic staphylococci and streptococci usually act as the causative agent of the disease. The infectious agent then spreads along the hair root into the follicle. This process is accompanied by local inflammation and the formation of a painful infiltrate. This stage of the boil is called the stage of infiltration. After this, necrosis develops and a necrotic rod is formed. The surrounding tissues undergo melting and transform into purulent masses, after which they begin to accumulate under the layer of the epidermis surrounding the mouth of the follicle, due to which a subcutaneous abscess develops. This stage of the boil is called the abscess stage.
The infectious agent then spreads along the hair root into the follicle. This process is accompanied by local inflammation and the formation of a painful infiltrate. This stage of the boil is called the stage of infiltration. After this, necrosis develops and a necrotic rod is formed. The surrounding tissues undergo melting and transform into purulent masses, after which they begin to accumulate under the layer of the epidermis surrounding the mouth of the follicle, due to which a subcutaneous abscess develops. This stage of the boil is called the abscess stage.
Symptoms of a boil in the nose
- Pain at the site of the boil
- Redness and swelling of surrounding tissues
- Rise in body temperature up to 38C and above
- General weakness and malaise
Possible complications of a nasal furuncle
The furuncle of the nose is not at all such a harmless disease as boils of other localizations.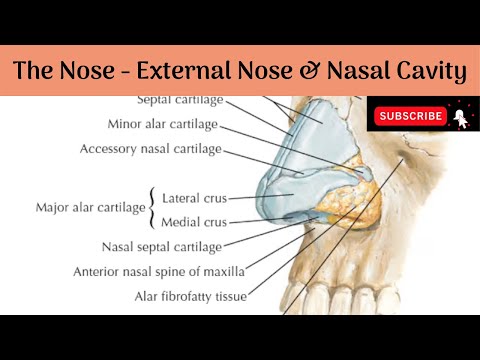 The fact is that it is located in the nasolabial triangle (otherwise it is called the "triangle of death"). Its peculiarity and danger as a focus of inflammation lies in the extremely developed blood supply: there are many vessels of the venous and arterial network. In addition, these veins do not have valves inherent in the veins of other areas, and therefore the formed blood clots, bacteria and their toxins can spread through the venous pathways into the orbit and venous sinuses of the brain. This can cause phlegmon of the nasolabial, buccal region and orbit, thrombophlebitis of the cavernous sinus and other formidable complications - meningitis, encephalitis, brain abscess. Rarely observed generalization of infection - sepsis. Of the local complications, sinusitis, frontal sinusitis and abscesses of the nasal septum are most common.
The fact is that it is located in the nasolabial triangle (otherwise it is called the "triangle of death"). Its peculiarity and danger as a focus of inflammation lies in the extremely developed blood supply: there are many vessels of the venous and arterial network. In addition, these veins do not have valves inherent in the veins of other areas, and therefore the formed blood clots, bacteria and their toxins can spread through the venous pathways into the orbit and venous sinuses of the brain. This can cause phlegmon of the nasolabial, buccal region and orbit, thrombophlebitis of the cavernous sinus and other formidable complications - meningitis, encephalitis, brain abscess. Rarely observed generalization of infection - sepsis. Of the local complications, sinusitis, frontal sinusitis and abscesses of the nasal septum are most common.
Treatment of nasal furuncle
First of all, it is strictly forbidden to try to treat the furuncle of the nose on your own, and even more so to squeeze it out. Due to the high risk of complications in this disease, at the first symptoms it is necessary to contact an otorhinolaryngologist.
Due to the high risk of complications in this disease, at the first symptoms it is necessary to contact an otorhinolaryngologist.
With a small localization of the boil, being in the stage of infiltration and unexpressed symptoms, outpatient treatment is possible. With timely treatment of the patient, the therapeutic program consists of conservative measures: local and general antibacterial therapy, treatment of the boil with antiseptic ointments and solutions, anti-inflammatory and detoxification therapy, etc.
If the nasal furuncle at the time of examination is in an abscessing form, local and general inflammatory signs are pronounced, there is a risk of complications, then it is necessary to carry out surgical treatment of the nasal furuncle (opening the boil), and only in a hospital under round-the-clock medical supervision.
Our specialists
All specialists
Nasal boil - symptoms, diagnosis and causes
Article rating
5. 00 (Voted: 4)
00 (Voted: 4)
Contents
- Prevalence
- Causes of the development of a furuncle of the nose
- Symptoms of a boil in the nose
- Complications of the boil of the nose
- Diagnosis of the boil of the nose
Furuncle of the nose is a purulent inflammation of the hair follicle and the sebaceous gland of the outer or inner surface of the wing of the nose, the tip of the nose, the skin part of the nasal septum. If several hair follicles and sebaceous glands become inflamed with extensive necrosis of the skin and subcutaneous tissue. That is called a carbuncle.
Prevalence
Most often this pathology affects people aged 15 to 45 years. Men are 1.5 - 1.7 times more likely to get sick than women.
Causes of nasal furuncle development
Most often, furunculosis is caused by staphylococci, less often by streptococci. These representatives of bacteria belong to the normal microflora of the skin and mucous membranes. And only in the presence of concomitant factors does infection occur:
These representatives of bacteria belong to the normal microflora of the skin and mucous membranes. And only in the presence of concomitant factors does infection occur:
- Decreased immunity. General hypothermia, chronic overwork, beriberi, diabetes mellitus, the presence of HIV infection, oncological diseases, completed courses of chemotherapy, and taking systemic corticosteroids can contribute to the appearance of a nasal furuncle.
- Concomitant purulent pathologies. Inflammation of the paranasal sinuses, palatine tonsils, the presence of carious teeth. Pustular diseases of the skin (pyoderma) or vestibule of the nose (sycosis, folliculitis).
- Traumatic injuries. Cuts, scratches, abrasions, any other violations of the integrity of tissues are the entrance gate for infection. This also includes rhinoplasty, implant placement.
- Violation of sanitary and hygienic standards. This is a rare conduct of hygienic procedures in everyday life, which leads to greasy skin and persistence of pathogenic microorganisms.
 In production, this is the inhalation of polluted air, constant contact with fuel-lubricated materials.
In production, this is the inhalation of polluted air, constant contact with fuel-lubricated materials.
Symptoms of nasal furuncle
The development of the disease occurs in two stages - infiltration and abscess formation. The first stage lasts 24-48 hours and is accompanied by the formation of a small cone-shaped seal, a feeling of fullness, redness, swelling, and pain. The pain syndrome is aggravated by chewing, talking, smiling. There is an intoxication syndrome: weakness, malaise, headache, fever up to 39.0 *.
On the 3rd-7th day from the onset of the disease, the second stage begins - abscess formation. Softening occurs in the central part of the formation. At the top, a yellow-white tire is formed - the core of the boil, which quickly breaks through, purulent contents are released. At the same time, pain sensations disappear, body temperature normalizes, the furuncle cavity is emptied, filled with granulation tissues and heals. Leaving behind a whitish scar.
Complications of the furuncle of the nose
Since the development of complications is due to contact and hematogenous spread of infection, if you do not contact an ENT doctor in time, complications such as:
- phlegmon of the orbit, tombophlebitis of the cavernous sinus brain
- sepsis
- sinusitis, frontal sinusitis
- abscess of the nasal septum
Diagnostics of the nasal furuncle
For diagnosis, you need to contact an otorhinolaryngologist (ENT doctor), who, after examining you, interviewing you, taking the necessary laboratory tests, will make a diagnosis and determine the stage. Depending on your specific case, he will select the necessary, high-quality treatment, which is as follows:
- Antibacterial therapy. Initially, broad-spectrum antibiotics are used - aminopenicillins, macrolides, cephalosporins, fluoroquinolones. After receiving the results of a microbiological study, drugs are prescribed, to which the sown microflora is most sensitive.