Blighted ovum successful pregnancy
Blighted Ovum Miscarriage - Meaning, Treatment, Causes
A blighted ovum is a miscarriage that occurs very early in pregnancy. The fertilized egg is unable to develop into an embryo after it has attached to the uterine wall. This type of miscarriage usually occurs within the very early stages of pregnancy (weeks 2-6), often before a woman even knows she's pregnant.
Still, losing your baby, even at an early stage of pregnancy, can be devastating for the parents, far more so than people appreciate who have not been through it.
Unfortunately, blighted ovum miscarriages are not rare. It is the leading cause of miscarriages. A blighted ovum is one of the more common forms of miscarriages and is invariably associated with a chromosomal abnormality.
Thankfully, as we discuss below, having an early miscarriage like this does not have any impact on having a healthy pregnancy in the future. This article addresses the causes of blighted ovum, treatment for it, and the long-term outlook for fertility after a miscarriage from an anembryonic pregnancy.
What Is a Blighted Ovum Miscarriage?
A blighted ovum occurs very early in the process of embryonic development. When sperm reaches an egg, the egg becomes fertilized and begins the rapid production of new cells within only a few hours. With a normal pregnancy, the fertilized egg will grow from a clump of cells into an embryo by the 10th day of development.
The embryo will then implant itself into the wall of the uterus. This triggers the release of high levels of pregnancy hormones in the body and causes the placenta to start developing to support the fetus. The fetus will continue to grow over the next few weeks, and around the 6th week of pregnancy, it will finally be visible on an ultrasound.
When blighted ovum occurs, this initial process is not completed. Sometimes the fertilized egg is not able to develop into an embryo but still implants itself into the uterus. In other cases, the transition from fertilized egg to embryo was successful but the embryo stops developing a few days after attaching.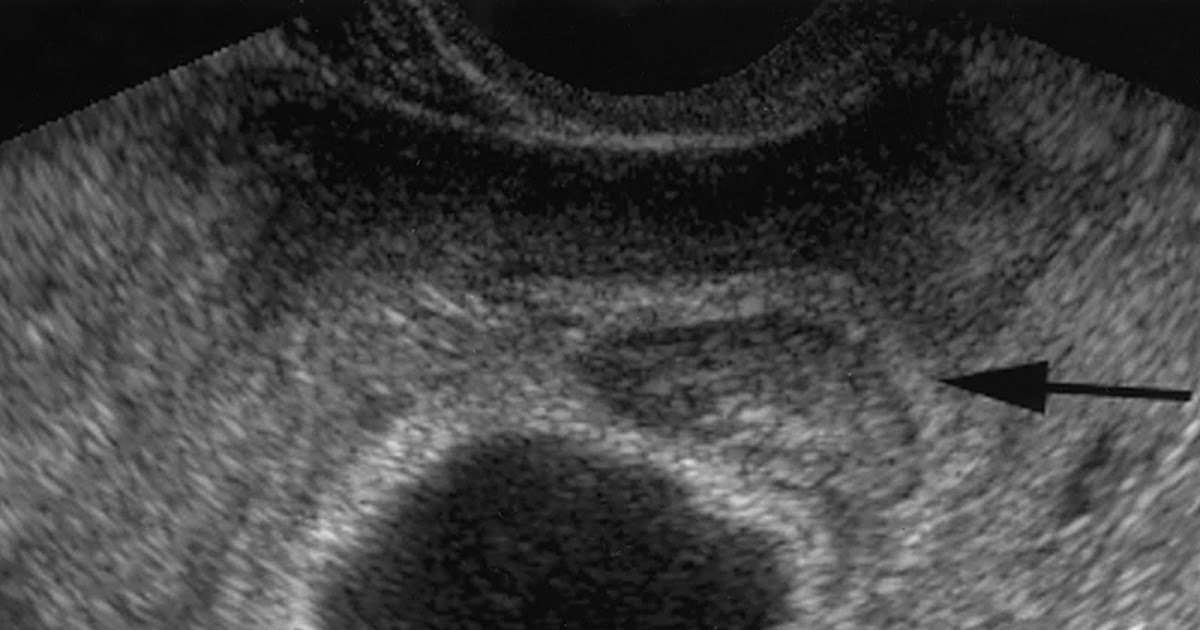
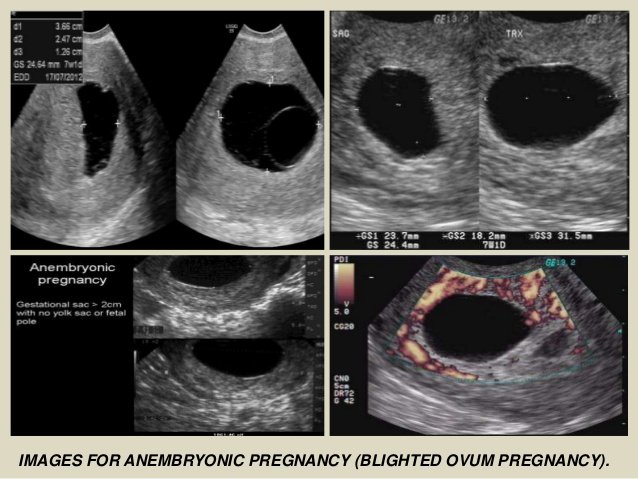
For a doctor to diagnose a blighted ovum, an ultrasound will be performed and the doctor will identify an empty gestational sac with no signs of an embryo. This empty sac can usually be confirmed by the 8th week of pregnancy when the embryo would normally be visible. How long you carry a blighted ovum depends on what stage the blighted ovum miscarries.
What Causes Blighted Ovum Miscarriage?
There are several causes of a blighted ovum. The common thread is any anembryonic pregnancy is a genetic error or a genetic mistake.
From research conducted on multiple women who experienced a blighted ovum, there is a consensus that the wide majority of blighted ovum miscarriages are due to abnormal chromosomes[2]. The fertilized egg or embryo might be missing chromosomes or developed too many. This disrupts the normal process of development. In rare cases, genetic mutations can also be a cause for a blighted ovum, specifically for embryos that stopped developing after attaching to the uterus.
A blighted ovum is similar to other miscarriages in the sense that there was some developmental abnormality that ultimately caused the pregnancy to fail. It can create feelings of loss and despair, but it's important to understand that there is no way to prevent it from happening and women should not blame themselves. For early miscarriages, there is often no way to know that something has gone wrong until your doctor identifies it. If you are a woman reading this, you have already heard this but you should hear it again: it is not your fault.
How Common is Blighted Ovum Miscarriage?
Accurate occurrence rates for blighted ovum miscarriages are understandably difficult because many women choose not to share their miscarriage stories. However, miscarriages are actually very common, with around 10-20% of pregnancies ending in miscarriage[4]. In that statistic, early miscarriages are most prevalent with 80% of them occurring within the first 12 weeks. Additionally, many women have one or multiple miscarriages before they have a normal pregnancy.
Additionally, many women have one or multiple miscarriages before they have a normal pregnancy.
The statistics for how common blighted ovum is can be hard to measure due to difficulties diagnosing the condition. Since it occurs so early, women may not even know they were pregnant and do not notice the miscarriage happening. From what is known, experts believe blighted ovum accounts for a third of miscarriages that occur before 8 weeks gestation[3].
Blighted Ovum Symptoms
Even though the embryo is not developing properly or has stopped altogether, a woman may experience early pregnancy symptoms since the body has recognized something attached to the uterus.
Until the embryo has been expelled from the body, hormones are still being produced and pregnancy tests can have positive results. A woman may have morning sickness, bloating, sore breasts, and other common symptoms that show up during the first weeks of pregnancy. However, some signs may indicate a woman has a blighted ovum or is experiencing a miscarriage:
However, some signs may indicate a woman has a blighted ovum or is experiencing a miscarriage:
- Abnormal heavy bleeding
- Severe abdominal cramping
- An ultrasound that shows an amniotic sac is but is missing an embryo
A blighted ovum is confirmed when a sonogram shows no fetal heart tone.
Treatment for Blighted Ovum
After you have been diagnosed with a blighted ovum, there are a few different treatments available depending on how your body reacts to the attached egg or embryo.
For some women, there may be no treatment at all, as the body recognizes that there is no development and naturally passes the embryo by expelling the contents of the uterus. In these cases, the miscarriage will be similar to a heavy period, which can feel completely normal for someone unaware they had a blighted ovum.
If the blighted ovum is diagnosed but the body continues to act pregnant and releases hormones, your doctor may wait a few days to see if the body adjusts and eventually passes the embryo. If the body continues to keep the embryo attached despite no development, medication or surgery can be used to clear the contents of the uterus. Medication like Cytotec can induce a miscarriage which causes temporary heavy bleeding. A brief surgical procedure can be also be given by dilating the cervix and manually emptying the uterus.
If the body continues to keep the embryo attached despite no development, medication or surgery can be used to clear the contents of the uterus. Medication like Cytotec can induce a miscarriage which causes temporary heavy bleeding. A brief surgical procedure can be also be given by dilating the cervix and manually emptying the uterus.
Can A Blighted Ovum Give a False Positive Pregnancy Test?
A blighted ovum may occur before a woman is aware she is pregnant. What often happens in these cases is the placenta will continue to develop after the miscarriage. This is called an anembryonic pregnancy in which the body does not adapt to the miscarriage and continues to prepare for the baby. This will often lead to a false positive pregnancy test.
Can I Get Pregnant Again After a Blighted Ovum?
Miscarriages can be scary and make you feel like something is wrong with your fertility, but in most cases, this is not reality. Miscarriages are a natural part of pregnancies and often have no bearing on how fertile you are. Having one anembryonic pregnancy is usually no cause for concern. Normal pregnancies after a blighted ovum are normal. Statistics show you will likely have a normal and healthy pregnancy in the future, even immediately after a blighted ovum.
Miscarriages are a natural part of pregnancies and often have no bearing on how fertile you are. Having one anembryonic pregnancy is usually no cause for concern. Normal pregnancies after a blighted ovum are normal. Statistics show you will likely have a normal and healthy pregnancy in the future, even immediately after a blighted ovum.
In a study involving women with early miscarriages, around 80% were able to have a successful pregnancy within the next five years[1]. The reason for these success stories is that treatments used for blighted ovum also have no negative effects on future pregnancies, even for surgical procedures.
If you have experienced multiple blighted ova or are struggling with miscarriages, there may be a different underlying problem, such as a hormone imbalance or genetic mutation. Your doctor can run tests to identify possible causes for complications in development.
How Long Can You Carry a Blighted Ovum?
When deciding how long to carry a blighted ovum, you are trying to balance the ease and low risk of a natural miscarriage (Dilation and Curettage or D&C surgery, for example, has some risks) versus the risk of infection if you do not have a natural miscarriage. Some suggest you can wait between 9 to 11 weeks with an anembryonic pregnancy.
Some suggest you can wait between 9 to 11 weeks with an anembryonic pregnancy.
But you want to discuss with your doctor who will be able to best gauge the optimal path for you.
How Long Until I Can Try to Get Pregnant After a Blighted Ovum?
Doctors often suggest women wait three months before attempting to conceive after a blighted ovum while others say less. You should talk to your doctor.
Do the COVID-19 Vaccines Cause a Blighted Ovum?
Three studies have been published that showed women are not at higher risk for a miscarriage after taking a COVID-19 vaccine.
Sources and Additional Reading
Chaudhry, K., et al. (2021). Anembryonic Pregnancy. StatPearls [Internet]. StatPearls Publishing.
This article provided an overview of a blighted ovum. It detailed its risk factors, clinical presentation, treatment and management options, differential diagnosis, and prognosis. The researchers also reported on patient education and the enhancement of healthcare team outcomes.
The researchers also reported on patient education and the enhancement of healthcare team outcomes.
Sanni, R. R., et al. (2020). Blighted Ovum: A Case Report. Women’s Health Open Journal.
This case study looked at a late 20-something woman who suffered a blighted ovum. The researchers recommended healthcare providers should know how to properly manage and treat a blighted ovum.
Andriani, F., & Mardhiyah, I. (2019, March 22). Blighted ovum detection using convolutional neural network. AIP Conference Proceedings, 2084(1), 020012.
This article looked at the use of the convolutional neural network method to timely detect a blighted ovum. The researchers reported that the algorithm implementation’s accuracy was less than 60 percent. However, they also reported that this was because of the lack of data and the difficulties of distinguishing between blighted ovum and non-blighted ovum data.
Aroke, D., et al. (2018). Blighted ovum and tubal pregnancy: a rare form of heterotopic pregnancy: case report. BMC Research Notes, 11(1), 1-4.
BMC Research Notes, 11(1), 1-4.
This case study looked at a 25-year-old woman who suffered both a blighted ovum and an ectopic pregnancy. She underwent surgery. Her pregnancy was ultimately uneventful. The researchers concluded that blighted ova and ectopic pregnancies could occur at the same time. They recommended timely diagnoses and prompt management that could yield a favorable prognosis.
Horner-Johnson, W., et al. (2017). Live birth, miscarriage, and abortion among US women with and without disabilities. Disability and health journal, 10(3), 382-386.
This study looked at the live birth, miscarriage, and abortion rates among American women with and without disabilities. The researchers found that women with disabilities were less likely to have live births compared to women without. However, they reported that these differences were insignificant when controlling for covariates. They also found that women with complex limitations were more likely to suffer miscarriages. The researchers concluded that disability status did not have a significant impact on pregnancy outcomes.
The researchers concluded that disability status did not have a significant impact on pregnancy outcomes.
Smith, L.F., et al. (2009). Incidence of pregnancy after expectant, medical, or surgical management of spontaneous first trimester miscarriage: long term follow-up of miscarriage treatment (MIST) randomised controlled trial. BMJ, 339.
This study looked at whether three early miscarriage management methods impacted future pregnancy rates. The researchers found that the live birth rates across all three groups were similar. They concluded that miscarriage management methods did not impact subsequent pregnancy rates.
Lathi, R. B., et al. (2007). Cytogenetic testing of anembryonic pregnancies compared to embryonic missed abortions. Journal of Assisted Reproduction and Genetics, 24(11), 521-524.
This study compared the abnormality rate detected by cytogenetic testing in first semester miscarriages involving a fetal pole or a blighted ovum. The researchers found that 65 percent of all miscarriages showed abnormalities. They also found that the rates were 58 percent in miscarriages involving a blighted ovum and 68 percent in miscarriages involving a fetal pole. The researchers concluded that cytogenetic testing would help determine abnormalities during pregnancy.
They also found that the rates were 58 percent in miscarriages involving a blighted ovum and 68 percent in miscarriages involving a fetal pole. The researchers concluded that cytogenetic testing would help determine abnormalities during pregnancy.
Regan, L., & Rai, R. (2000). Epidemiology and the medical causes of miscarriage. Baillieres Best Practice & Research Clinical Obstetrics & Gynaecology, 14(5), 839-854.
This study summarized a miscarriage’s epidemiology and medical causes. It also discussed the genetic abnormalities that contribute to a miscarriage.
Blighted ovum | Pregnancy Birth and Baby
Blighted ovum | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Key facts
- A blighted ovum is a type of miscarriage that can happen early in a pregnancy.

- A blighted ovum is when a sac and placenta grow, but a baby does not.
- A miscarriage can be extremely upsetting, and you may need support and time to grieve.
- Having a blighted ovum in one pregnancy does not change your chance of having a successful pregnancy in the future.
What is a blighted ovum?
A blighted ovum is a type of miscarriage that can happen early in a pregnancy. It is also called an 'anembryonic pregnancy' as there is no embryo (developing baby). In this type of miscarriage, a sac and placenta grow, but there is no baby. Because a blighted ovum still makes pregnancy hormones, it may still show up as a positive pregnancy test.
A blighted ovum will eventually cause a miscarriage, usually at 7 to 12 weeks of pregnancy. Your body realises that the pregnancy is not developing properly and starts to shed blood and tissue from the uterus. You may notice pain in your lower abdomen, or bleeding from your vagina.
How common is miscarriage?
Miscarriage is very common, and up to 1 in 5 people who know that they are pregnant will miscarry before 20 weeks of gestation. The actual rate of miscarriage is even higher, as a very early miscarriage may happen before you even realise that you’re pregnant.
What causes a blighted ovum?
When the egg is fertilised, cells that make the pregnancy sac and placenta start multiplying. But occasionally, the cells that are supposed to develop into a baby don’t multiply.
The cause isn’t known. It isn’t caused by anything you have done.
How and when is blighted ovum diagnosed?
Sometimes, it is picked up during a routine ultrasound. This can be particularly difficult if you’ve gone for an ultrasound expecting good news.
At other times, there may have been bleeding at the start of the pregnancy and an ultrasound is used to investigate the cause.
How is blighted ovum treated?
Your doctor will discuss the options with you. You might choose to allow a natural miscarriage to happen. Once this starts, it can take days or weeks for the bleeding to finish. If the bleeding is getting heavier, if you are in pain or you feel unwell, see your doctor.
You might choose to allow a natural miscarriage to happen. Once this starts, it can take days or weeks for the bleeding to finish. If the bleeding is getting heavier, if you are in pain or you feel unwell, see your doctor.
You could also have a termination by taking medicines or by having a type of surgery known as D & C.
Does it affect my chances of having a baby?
No. Having a blighted ovum in one pregnancy does not alter your chance of having a successful pregnancy in the future.
If you have had one miscarriage, your next pregnancy is likely to be normal. If you have had 3 miscarriages in a row, you should see your doctor to rule out any problems.
Where can I go for support and information?
Speak with your doctor if you are concerned that you may have a blighted ovum.
A miscarriage can be extremely upsetting. If you’ve experienced a miscarriage you may need support and time to grieve. There is no right way to feel after a miscarriage. Different people react to a miscarriage with different emotions, including anger, guilt or relief.
Different people react to a miscarriage with different emotions, including anger, guilt or relief.
Pregnancy, Birth and Baby helpline can offer emotional support and trusted advice to anyone who is dealing with pregnancy loss. Call Pregnancy, Birth and Baby on 1800 882 436 anytime of the day or night.
Sources:
Raising Children (Miscarriage : what it is and how to cope), Pink Elephants Network (What is miscarriage?), Red Nose (Reasons for miscarriage)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2022
Back To Top
Related pages
- Fathers and miscarriage
- Emotional support after miscarriage
- Miscarriage
- Pregnancy loss
Need more information?
Reasons for Miscarriage | Red Nose Australia
Read more on Red Nose website
Experiencing a pregnancy loss
Losing a baby at any stage of pregnancy can be devastating. Remember, pregnancy loss is more common than you probably think – and it’s not your fault. This article aims to help you deal with the many emotions you will be feeling.
Remember, pregnancy loss is more common than you probably think – and it’s not your fault. This article aims to help you deal with the many emotions you will be feeling.
Read more on Pregnancy, Birth & Baby website
Miscarriage
A miscarriage is the loss of a baby, usually during the first three months or first trimester of pregnancy.
Read more on Pregnancy, Birth & Baby website
Pregnancy: miscarriage & stillbirth | Raising Children Network
Have you experienced a miscarriage or stillbirth? Find articles and videos about coping with the grief of losing a pregnancy or having a stillbirth.
Read more on raisingchildren.net.au website
Miscarriage: a guide for men | Raising Children Network
This Dads Guide to Pregnancy covers miscarriage, the grief men might experience after miscarriage, and how to support partners after pregnancy loss.
Read more on raisingchildren.net.au website
The Pink Elephants Support Network - Supporting Your Physical Wellbeing After Miscarriage
Physical Wellbeing can be an important factor when trying to conceive
Read more on Pink Elephants Support Network website
The Pink Elephants Support Network - Supporting Your Emotional Wellbeing After Miscarriage
It can be challenging to maintain a positive outlook after early pregnancy loss
Read more on Pink Elephants Support Network website
The Pink Elephants Support Network - Holistic Options for Miscarriage Management
Some women may find holistic options can help them feel nurtured and empowered on their journey to future pregnancy
Read more on Pink Elephants Support Network website
The Pink Elephants Support Network - Causes of Miscarriage - Pink Elephants
There are a number of possible reasons that a miscarriage may occur, and often it’s not until extensive testing is done that you may find out why
Read more on Pink Elephants Support Network website
The Pink Elephants Support Network - Pregnancy After Loss - Pink Elephants
Pregnancy after loss is a time that can be fraught with many conflicting emotions
Read more on Pink Elephants Support Network website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.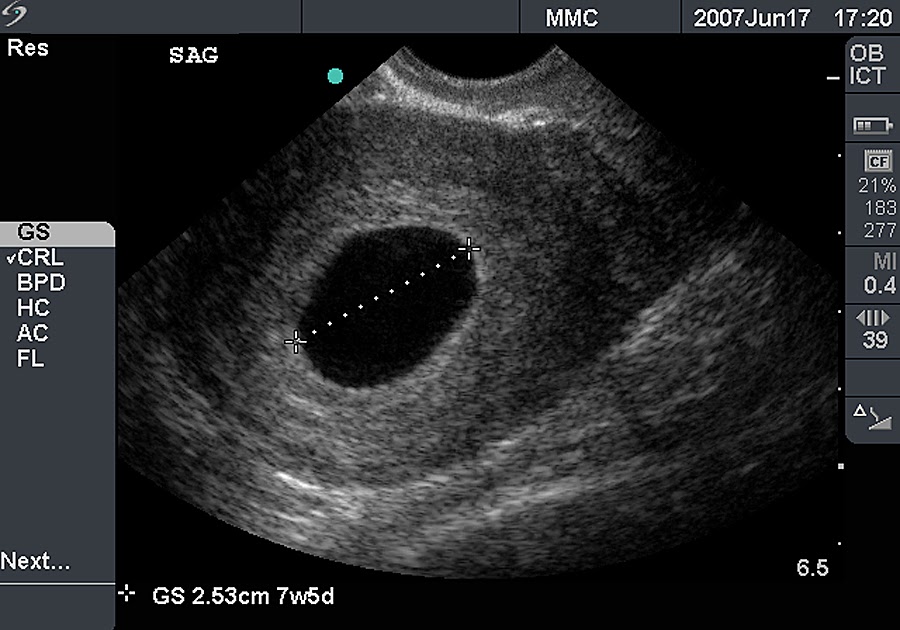
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Female infertility - articles from the specialists of the clinic "Mother and Child"
Astakhova Elena Stanislavovna
Otorhinolaryngologist (ENT)
MD GROUP Clinical Hospital
Every month, hormonal changes occur in a woman's body. Thanks to them, eggs mature in the structure of the ovaries (in the follicles). In the middle of the menstrual cycle, ovulation occurs, that is, the follicle ruptures and the egg is released. It enters the fallopian tube, where it is fertilized by spermatozoa. Then the fertilized egg begins to divide and move along the fallopian tube to the uterus, which accepts it and ensures the further course of the pregnancy.
With hormonal disorders, ovulation does not occur. The egg does not mature, which means that pregnancy is impossible. If the fallopian tubes are impassable, then the fertilization process also cannot occur. Violation of ovulation and obstruction of the fallopian tubes are the reasons why a woman cannot become pregnant.
Factors affecting the possibility of conception are also inflammatory and non-inflammatory diseases of the female genital area, the presence of concomitant extragenital pathology.
In the presence of intrauterine pathology, the difficulty in the onset of pregnancy is associated with the impossibility of attaching the embryo to form a fetal egg and / or further development of the fetus.
Ovarian endometriosis is an unfavorable factor in infertility that has a negative impact on folliculogenesis, egg quality, and the formation of the corpus luteum, thereby reducing the effectiveness of treatment, including the use of in vitro fertilization. The duration of the presence of endometriosis also has a significant impact on the outcome of treatment, determining the need to start planning pregnancy as soon as possible, avoiding a significant increase in the experience of infertility.
The duration of the presence of endometriosis also has a significant impact on the outcome of treatment, determining the need to start planning pregnancy as soon as possible, avoiding a significant increase in the experience of infertility.
Pathology of the cervix can also be the cause of non-pregnancy. Timely and high-quality treatment of cervical diseases made it possible to obtain pregnancy in vivo in 15% of patients with this pathology and who received treatment at our Centers at the stage of preparation for ART programs. Thus, these women avoided the need for in vitro fertilization.
The causes of female infertility or non-carrying of pregnancy in some cases are violations of individual genes, structure or number of chromosomes. In these cases, conducting a preliminary genetic examination allows you to establish the nature of genetic disorders and choose tactics to overcome reproductive problems.
Increasingly, women seek to have children after 30 years, which is explained by the desire to sufficiently establish their social positions.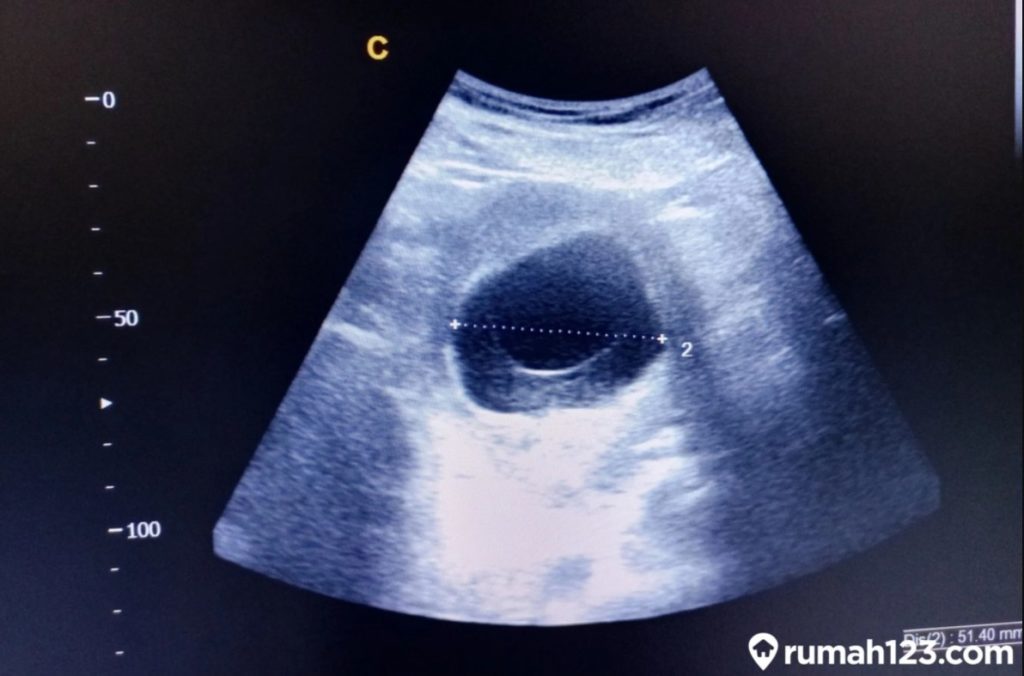 However, with age, the cumulative effect of numerous risk factors for infertility increases both due to an increase in the duration of their exposure, and due to the addition of more and more new causes that negatively affect the onset of pregnancy. In addition, the reproductive potential of a woman has significant age restrictions, creating additional difficulties in the treatment of infertility, especially in women over 37 years of age.
However, with age, the cumulative effect of numerous risk factors for infertility increases both due to an increase in the duration of their exposure, and due to the addition of more and more new causes that negatively affect the onset of pregnancy. In addition, the reproductive potential of a woman has significant age restrictions, creating additional difficulties in the treatment of infertility, especially in women over 37 years of age.
Types of infertility
Infertility I - primary infertility. It is installed in a woman who has not had a single pregnancy.
Infertility II - secondary infertility. A condition in which a woman has had pregnancies in the past (regardless of their outcome), but at the present time, conception does not occur without protection for a year.
Absolute is infertility, in which the possibility of becoming pregnant is excluded, for example, in the absence of internal genital organs or their surgical removal.
Relative infertility - when a woman and a man are able to have children each separately outside of marriage, but with a long life together their marriage is fruitless.
In addition, female infertility is divided into congenital (malformations, hereditary disorders) and acquired (due to adverse effects of various external and internal causative factors on the reproductive system after birth).
Make an appointment
to the doctor - Astakhova Elena Stanislavovna
MD GROUP Clinical Hospital
Otorhinolaryngology
By clicking on the submit button, I consent to the processing of personal data
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
Clinical Hospital MD GROUPClinical Hospital Lapino-1 "Mother and Child"Clinic "Mother and Child" Khodynskoye PoleClinic "Mother and Child" KuntsevoClinic "Mother and Child" SavelovskayaClinic "Mother and Child" South-WestClinic "Mother and Child" Lefortovo
All directionsEco DepartmentEco services
01.
IVF department
02.
Eco services
Nothing found
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of the tests by calling
1-4 weeks of pregnancy
From a tiny fetus to a small person, a child's body develops in just 9 months. What changes are happening to the expectant mother and what changes are observed inside her during this difficult and joyful period of life?
Each new life begins with the union of the egg and sperm. Conception is the process by which a sperm enters an egg and fertilizes it.
It should be noted that the embryonic and obstetric terms are different. The thing is that among specialists it is customary to consider the period from the first day of the last menstruation, that is, the obstetric period includes the period of preparation for pregnancy. So it turns out that the embryo has just appeared, and the gestation period is already two weeks. It is the obstetric period that is indicated in all the documents of a woman and is the only reporting period for specialists.
So it turns out that the embryo has just appeared, and the gestation period is already two weeks. It is the obstetric period that is indicated in all the documents of a woman and is the only reporting period for specialists.
Until the moment of the meeting, the spermatozoon and the ovum lived for a certain time, being in the stage of development and maturation. The development of the future fetus significantly depends on the quality of these processes.
First week
Growth and maturation of the egg starts from the first day of the cycle. A mature egg contains 23 chromosomes as the genetic material for the future embryo, and also contains all the nutrients necessary to start its development. It contains reserves of carbohydrates, proteins and fats, designed to support the embryo during the first days after its occurrence.
A certain number of eggs are laid in each ovary of a girl before she is born. During the childbearing period, they only grow and develop, the process of their formation does not occur. By the time a girl is born, the number of cells from which eggs can develop in the future reaches a million, but this number decreases significantly over the course of life. So, by the time of puberty, there are several hundred thousand of them, and by maturity - about 500.
By the time a girl is born, the number of cells from which eggs can develop in the future reaches a million, but this number decreases significantly over the course of life. So, by the time of puberty, there are several hundred thousand of them, and by maturity - about 500.
The ovary each month gives the opportunity to develop most often one egg, the maturation of which occurs inside a vesicle with a liquid called a follicle. From the first day of the cycle, the uterine mucosa begins to prepare for a possible pregnancy. For implantation, i.e., the introduction of the resulting embryo into the wall of the uterus, an optimal environment is created. To do this, due to the influence of hormones, the endometrium thickens, it becomes covered with a network of vessels and accumulates the nutrients necessary for the future embryo.
Male reproductive cells are formed in the gonads - in the testicles or testes. The maturation of spermatozoa occurs in the epididymis, into which they move after formation. The liquid structure of semen is formed due to the secretion of the seminal vesicles and the prostate gland. A liquid medium is necessary for storing mature spermatozoa and creating favorable conditions for their life.
The liquid structure of semen is formed due to the secretion of the seminal vesicles and the prostate gland. A liquid medium is necessary for storing mature spermatozoa and creating favorable conditions for their life.
The number of spermatozoa is quite large: tens of millions in one milliliter. Despite such a significant number, only one of them will be able to fertilize the egg. In spermatozoa, there is exclusively genetic material - 23 chromosomes, which are necessary for the appearance of the embryo.
Spermatozoa are characterized by high motility. Once in the female genital tract, they begin their movement towards the egg. Only half an hour or an hour passes from the moment of ejaculation, when sperm enter the uterine cavity. It takes one and a half to two hours for spermatozoa to penetrate into the widest part, which is called the ampulla. Most spermatozoa die on the way to the egg, meeting the folds of the endometrium, getting into the vaginal environment, cervical mucus.
Second week
In the middle of the cycle, the egg fully matures and leaves the ovary. It enters the abdominal cavity. This process is called ovulation. With a regular cycle of 30 days, ovulation occurs on the fifteenth. The egg is unable to move on its own. When she leaves the follicle, the fimbriae of the fallopian tube ensure her penetration inside. The fallopian tubes are characterized by longitudinal folding, they are filled with mucus. The muscular movements of the tubes have a wave-like character, which, with a significant number of cilia, creates optimal conditions for transporting the egg.
Through the tubes, the egg enters their widest part, which is called the ampulla. This is where fertilization takes place. If there is no meeting with the sperm, the egg dies, and the female body receives the appropriate signal to start a new cycle. There is a rejection of the mucous membrane, which was created by the uterus. The manifestation of such rejection is bloody discharge, which is called menstruation.
The waiting period for fertilization by the egg is short. On average, it takes no more than a day. Fertilization is likely on the day of ovulation and maximum on the next. Sperm have a longer lifespan, averaging three to five days, in some cases seven. Accordingly, if a spermatozoon enters the female genital tract before ovulation, there is a possibility that it will be able to wait for the appearance of an egg.
When the egg is in a state of waiting for fertilization, certain substances are released that are designed to detect it. If spermatozoa find an egg, they begin to secrete special enzymes that can loosen its shell. As soon as one of the spermatozoa penetrates the egg, the others can no longer do this due to the restoration of the density of its shell. Thus, one egg can only be fertilized by one sperm.
After fertilization, the chromosome sets of the parents merge - 23 chromosomes from each. As a result, one cell is formed from two different cells, which is called a zygote.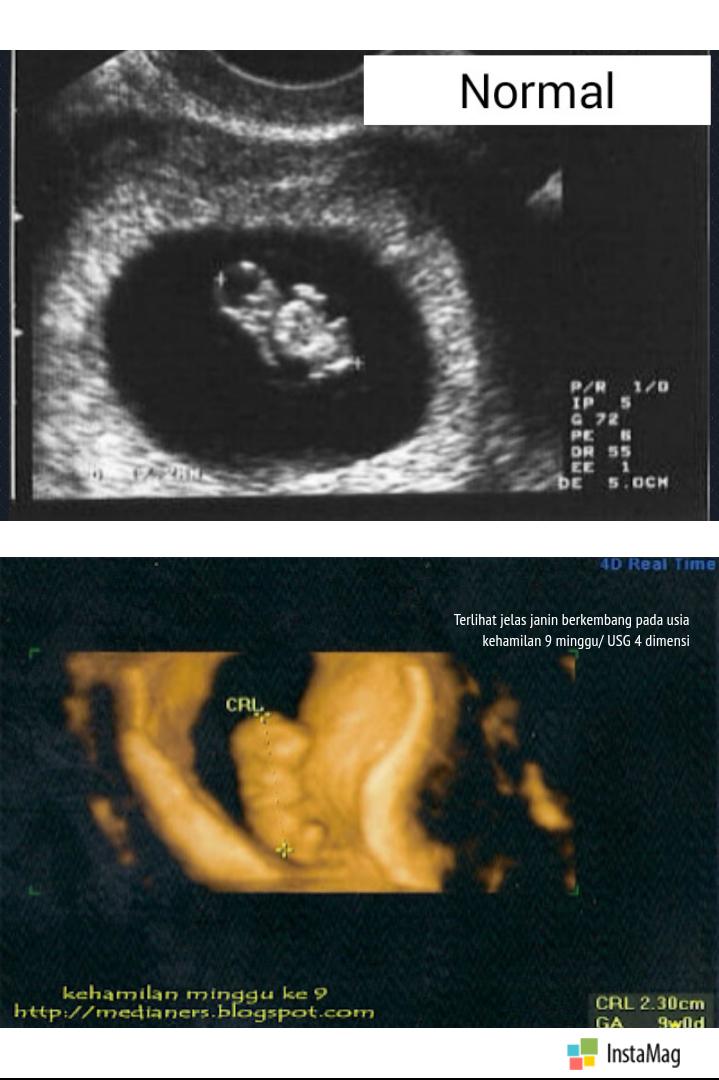 The sex of the unborn child depends on which of the chromosomes, X or Y, was in the sperm. Eggs contain only X chromosomes. When XX is combined, girls are born. If the spermatozoon contains a Y chromosome, that is, with a combination of XY, boys are born. As soon as a zygote is formed in the body, a mechanism is launched in it aimed at maintaining pregnancy. There are changes in the hormonal background, biochemical reactions, immune mechanisms, and the receipt of nerve signals. The female body creates all the necessary conditions for the safe development of the fetus.
The sex of the unborn child depends on which of the chromosomes, X or Y, was in the sperm. Eggs contain only X chromosomes. When XX is combined, girls are born. If the spermatozoon contains a Y chromosome, that is, with a combination of XY, boys are born. As soon as a zygote is formed in the body, a mechanism is launched in it aimed at maintaining pregnancy. There are changes in the hormonal background, biochemical reactions, immune mechanisms, and the receipt of nerve signals. The female body creates all the necessary conditions for the safe development of the fetus.
Third week
As soon as a day has passed after the formation of the embryo, he will need to make his first journey. The movements of the cilia and the contraction of the muscles of the tube direct it into the uterine cavity. During this process, inside the egg, fragmentation into identical cells occurs.
After four days, the appearance of the egg changes: it loses its round shape and becomes vine-shaped. This stage is called morula, embryogenesis begins - an important stage in the development of the embryo, during which the formation of the rudiments of organs and tissues occurs. Cleavage of cells continues for several days, on the fifth day their complexes are formed, which have different functions. The central cluster forms directly the embryo, the outer one, called the trophoblast, is designed to melt the endometrium - the inner layer of the uterus.
This stage is called morula, embryogenesis begins - an important stage in the development of the embryo, during which the formation of the rudiments of organs and tissues occurs. Cleavage of cells continues for several days, on the fifth day their complexes are formed, which have different functions. The central cluster forms directly the embryo, the outer one, called the trophoblast, is designed to melt the endometrium - the inner layer of the uterus.
It takes 5-7 days for the embryo to reach the uterus. When implantation occurs in its mucous membrane, the number of cells reaches one hundred. The term implantation refers to the process of implantation of the embryo into the endometrial layer.
After fertilization on the seventh or eighth day, implantation takes place. The first critical period of pregnancy is this stage, since the embryo will have to demonstrate its viability for the first time.
During implantation, the outer cells of the embryo actively divide, and the process itself takes about forty hours. The number of cells outside the embryo increases dramatically, they stretch, they penetrate into the uterine mucosa, and the thinnest blood vessels are formed inside, which are necessary for the supply of nutrients to the embryo. Time will pass, and these vessels will be transformed first into the chorion, and subsequently into the placenta, which will be able to supply the fetus with everything necessary until the baby is born.
The number of cells outside the embryo increases dramatically, they stretch, they penetrate into the uterine mucosa, and the thinnest blood vessels are formed inside, which are necessary for the supply of nutrients to the embryo. Time will pass, and these vessels will be transformed first into the chorion, and subsequently into the placenta, which will be able to supply the fetus with everything necessary until the baby is born.
The embryo at this stage of life is called a blastocyst. It contacts with the endometrium, melts the cells of the endometrium with its activity, creates a path for itself to the deeper layers. The blood vessels of the embryo intertwine with the mother's body, which allows it to immediately begin to extract useful and necessary substances for development. This is vital, because by this time the stock that the mature egg carried in itself is exhausted.
Next, the production of the trophoblast cells, i.e., the outer cells of human chorionic gonadotropin, the hCG hormone, begins. The distribution of this hormone throughout the body notifies it of the onset of pregnancy, which causes the launch of active hormonal changes and the beginning of corresponding changes in the body.
The distribution of this hormone throughout the body notifies it of the onset of pregnancy, which causes the launch of active hormonal changes and the beginning of corresponding changes in the body.
After fertilization and before the start of hCG, it usually takes eight or nine days. Therefore, already from the tenth day after fertilization, it becomes possible to determine this hormone in the mother's blood. Such an analysis is the most reliable confirmation of the onset of pregnancy. The tests that are offered today to determine pregnancy are based on the detection of this hormone in the urine of a woman. After the first day of delayed menstruation with its regular cycle, it is already possible to determine pregnancy using a test on your own.
What happens to a woman in the third week of pregnancy
If a woman is planning a pregnancy, 21-24 days, subject to a regular cycle, should be important for her. This is a period of possible implantation, when you should pay special attention to your own lifestyle. During this period, thermal effects and excessive physical exertion are undesirable, and the influence of various kinds of radiation should also be prevented.
During this period, thermal effects and excessive physical exertion are undesirable, and the influence of various kinds of radiation should also be prevented.
The woman does not feel anything at this stage, because implantation has no external signs. If you adjust your lifestyle in accordance with the simple rules listed above, you will be able to create optimal conditions for successful implantation.
Fourth week
At the fourth obstetric week or the second week of the fetus's life, its body consists of two layers. Endoblast - cells of the inner layer - will become the beginning of the digestive and respiratory systems, ectoblast - cells of the outer layer - will start the development of the nervous system and skin.
The size of the embryo at this stage is 1.5 mm. The flat arrangement of the cells determined the name of the embryo of this age - the disc.
The fourth week is characterized by intensive development of extra-embryonic organs. Such organs should surround the embryo and create the most favorable conditions for its development.