Bleeding after a baby
Bleeding after birth: 10 things you need to know | Life as a parent articles & support
It may be one of the few things you haven’t discussed with friends. Here’s an honest, clear account of what you can expect with bleeding after birth.
1. Every woman bleeds after they give birth
You will have vaginal bleeding after you’ve given birth(NHS, 2021). This bleeding is known as lochia. The lochia is a combination of mucous, tissue and blood that your womb sheds as it replaces its lining after you’ve given birth (UHS NHS Foundation Trust, 2020).
2. Bleeding after birth may last for a while
Bleeding often lasts for around for four to six weeks, but could last up to 12 weeks after your baby's born (RCOG, 2016). If you’re worried, you can talk to a health professional.
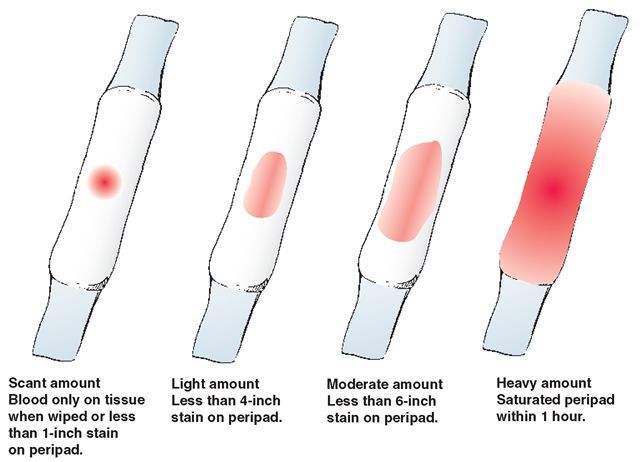
Bleeding will start off heavy and red to browny red. It will become lighter in colour and flow over time (NHS, 2021).
Here’s what you can expect:
- Day 1: Fresh red to brownish-red blood.
Heavy flow that probably soaks one maternity pad every few hours, with one or two clots or several smaller ones.
- Day 2 to 6: Darker brown or pinkish red blood. Moderate flow with 7 cm to 12 cm stains on your maternity pads and smaller blood clots.
- Day 7 to 10: Darker brown or pinkish red blood, becoming lighter. Variable but lighter flow, with less than a 7 cm stain on your pads.
- Days 11 to 14: Darker brown or pinkish red blood, becoming lighter. Lighter flow, you may have some sanitary towels that are hardly stained.
- Week 3 to 4: Paler, possibly a creamy white blood loss. Lighter flow.
- Week 5 to 6: Brown, pinkish red, or creamy yellow stains, possibly for several weeks, and possibly only on some days (UHS NHS Foundation Trust, 2020).
3. Don’t keep quiet about clots
They’re common. Discuss any clots with your midwife as she’ll want to keep track of what’s happening. Save your maternity pads to show your midwife if possible. Passing a lot of large clots can flag up something more serious (NHS, 2021).
Passing a lot of large clots can flag up something more serious (NHS, 2021).
4. If you pass a lot of large blood clots or more than a pint of blood in the first 24 hours, talk to a health professional immediately
Passing lots of large blood clots or more than a pint of blood in the first 24 hours after birth are symptoms of primary postpartum haemorrhage (RCOG, 2016).
Severe postnatal blood loss can make you feel even more exhausted than is normal after giving birth but it can also be life threatening. Getting quick treatment is essential before it becomes a major haemorrhage.
Treatment normally involves helping your uterus to contract through massaging the belly, an injection to contract the uterus, and a catheter into your bladder. The doctors will check to make sure all of the placenta has come out, and may have to do this under general anaesthetic. You will also have a drip in your arm and blood taken for tests.
5. The risk factors for primary postpartum haemorrhage
Before labour, risk factors are:
- Previous postpartum haemorrhages
- A body mass index (BMI) above 35
- A twin or triplet pregnancy
- Low-lying placenta (placenta previa)
- Placenta coming away early (placental abruption)
- Pre-eclampsia or high blood pressure
- Anaemia
- Growths in or around the womb (e.
 g. fibroids)
g. fibroids) - Taking blood-thinning medication
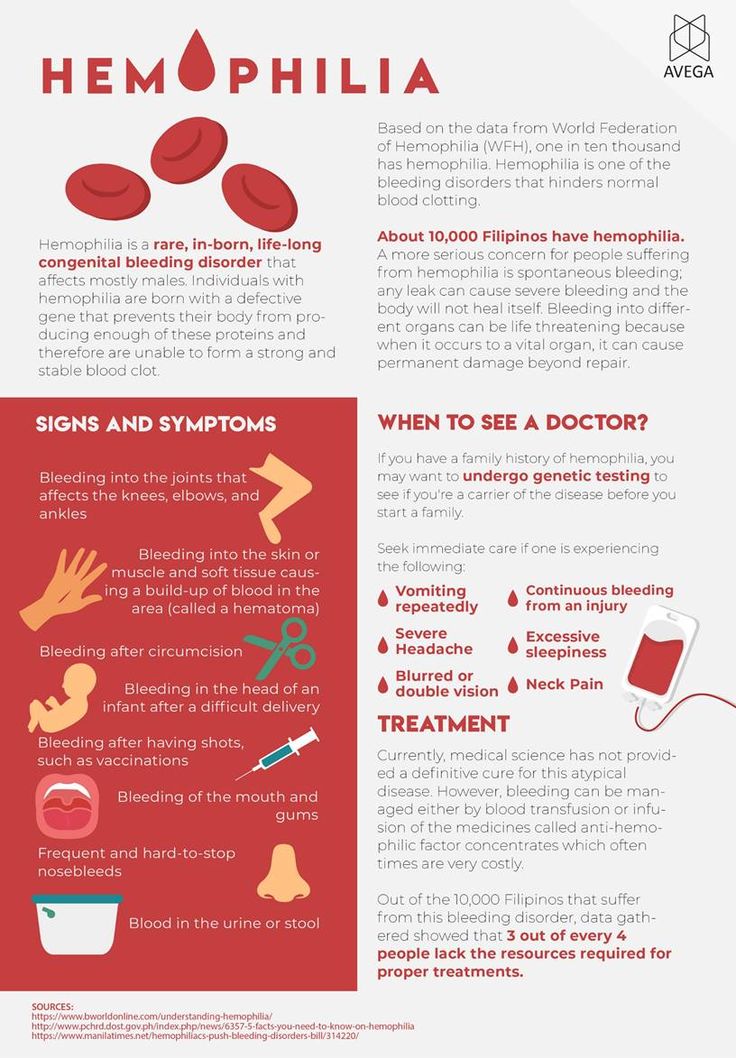
- Blood clotting problems.
During labour, risk factors are:
- Caesarean section birth
- Induced labour
- Retained placenta
- Episiotomy
- Forceps or vacuum-assisted vaginal delivery (ventouse) birth
- Your labour lasted longer than 12 hours
- Having a baby that weighs more than 4kg (9lbs)
- Having your first baby when you’re over 40 years old
- Having a raised temperature during labour
- Having a general anaesthetic.
(RCOG, 2016)
6. Think about postpartum bleeding when you pack your hospital bag
Pack maternity pads rather than menstrual pads as they’ll be more absorbant and allow the area between the vagina and anus (perineum) to heal with the least irritation. Describing the number of maternity pads you’re using also gives your midwife a clear picture of how much blood loss you’re experiencing.
7. Lots of things can affect the amount of blood loss
Breastfeeding makes your body release oxytocin. This makes your womb contract so it releases the lochia blood more quickly (but it will be the same amount of blood overall).
This makes your womb contract so it releases the lochia blood more quickly (but it will be the same amount of blood overall).
Any sort of gentle exercise – even a quick vacuum of the lounge – could also make bleeding heavier. This is especially true in the first two weeks.
Bleeding will tend to be heavier in the morning too. This is because blood pools when you lay down sleeping.
8. It’s important to keep an eye on your blood loss in the weeks after giving birth
It’s possible to get secondary postpartum haemorrhage, which is abnormal or heavy bleeding between 24 hours and 12 weeks after giving birth. It’s often associated with an infection, and sometimes with part of the placenta remaining in the womb (RCOG, 2016).
Symptoms include:
- Feeling shaky, feverish, and generally ill.
- Having lochia with an offensive smell.
- Heavier than expected bleeding, or bleeding that becomes heavier rather than lighter over time. (UHS NHS Foundation Trust, 2015; RCOG, 2016)
If you have any of these symptoms, you should speak to your GP or health visitor immediately (RCOG, 2016). Treatment for an infection includes antibiotics, so remind the health professional if you are breastfeeding so they can select the most appropriate antibiotic.
Treatment for an infection includes antibiotics, so remind the health professional if you are breastfeeding so they can select the most appropriate antibiotic.
Severe pain in the womb in the six weeks after birth could be a sign of a serious infection called sepsis, and should be treated with urgency because it can be life-threatening (RCOG, 2012). Other symptoms of sepsis include a high or low temperature, vomiting, diarrhoea, a rash and offensive discharge (RCOG, 2012). If you are experiencing these symptoms, go straight to the emergency department, say that you have recently given birth, and ask if this could be sepsis.
9. It’s important to reduce your risk of infection
Wash your hands thoroughly before and after using the toilet and changing your maternity pad (NICE, 2021).
10. Always speak to your GP or health visitor if anything doesn’t feel right
In the end, trust your judgement. If you have any worries about your bleeding after you give birth, talk to a health professional.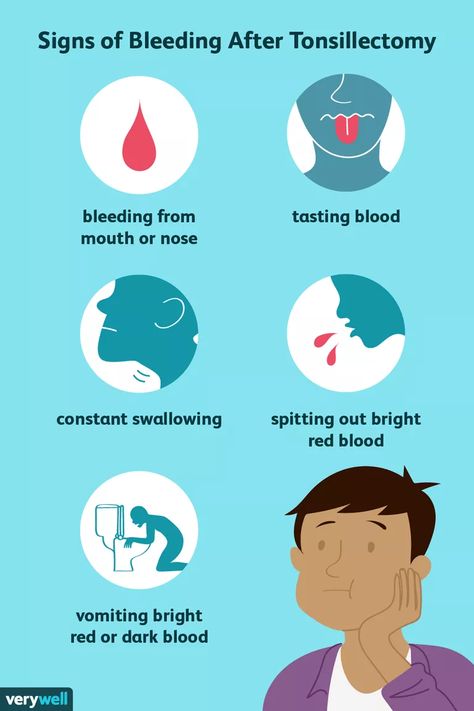 They’re there to help.
They’re there to help.
This page was last reviewed in November 2021
Further information
Our support line offers practical and emotional support with feeding your baby and general enquiries for parents, members and volunteers: 0300 330 0700.
You might find attending one of our Early Days groups helpful as they give you the opportunity to explore different approaches to important parenting issues with a qualified group leader and other new parents in your area.
Make friends with other parents-to-be and new parents in your local area for support and friendship by seeing what NCT activities are happening nearby.
Postpartum hemorrhage | March of Dimes
Postpartum hemorrhage (also called PPH) is a serious but rare condition when a woman has heavy bleeding after giving birth.
If you think you’re having PPH, call your health care provider or 911 immediately.
You may have PPH if you have heavy bleeding from the vagina that doesn’t slow or stop, blurred vision or chills, or if you feel weak or like you’re going to faint.

You’re more likely to have PPH if you’ve had it in the past or if you have certain medical conditions, especially conditions that affect the uterus (womb) or the placenta or conditions that affect how your blood clots.
Postpartum hemorrhage (also called PPH) is when a woman has heavy bleeding after giving birth. It’s a serious but rare condition. It usually happens within 1 day of giving birth, but it can happen up to 12 weeks after having a baby. About 1 to 5 in 100 women who have a baby (1 to 5 percent) have PPH.
It’s normal to lose some blood after giving birth. Women usually lose about half a quart (500 milliliters) during vaginal birth or about 1 quart (1,000 milliliters) after a cesarean birth (also called c-section). A c-section is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus (womb). With PPH, you can lose much more blood, which is what makes it a dangerous condition. PPH can cause a severe drop in blood pressure. If not treated quickly, this can lead to shock and death. Shock is when your body organs don’t get enough blood flow.
If not treated quickly, this can lead to shock and death. Shock is when your body organs don’t get enough blood flow.
When does PPH happen?
After your baby is delivered, the uterus normally contracts to push out the placenta. The contractions then help put pressure on bleeding vessels where the placenta was attached in your uterus. The placenta grows in your uterus and supplies the baby with food and oxygen through the umbilical cord. If the contractions are not strong enough, the vessels bleed more. It can also happen if small pieces of the placenta stay attached.
How do you know if you have PPH?
You may have PPH if you have any of these signs or symptoms. If you do, call your health care provider or 911 right away:
- Heavy bleeding from the vagina that doesn’t slow or stop
- Drop in blood pressure or signs of shock. Signs of low blood pressure and shock include blurry vision; having chills, clammy skin or a really fast heartbeat; feeling confused, dizzy, sleepy or weak; or feeling like you’re going to faint.

- Nausea (feeling sick to your stomach) or throwing up
- Pale skin
- Swelling and pain around the vagina or perineum. The perineum is the area between the vagina and rectum.
Are some women more likely than others to have PPH?
Yes. Things that make you more likely than others to have PPH are called risk factors. Having a risk factor doesn’t mean for sure that you will have PPH, but it may increase your chances. PPH usually happens without warning. But talk to your health care provider about what you can do to help reduce your risk for having PPH.
You’re more likely than other women to have PPH if you’ve had it before. This is called having a history of PPH. Asian and Hispanic women also are more likely than others to have PPH.
Several medical conditions are risk factors for PPH. You may be more likely than other women to have PPH if you have any of these conditions:
Conditions that affect the uterus
- Uterine atony.
 This is the most common cause of PPH. It happens when the muscles in your uterus don’t contract (tighten) well after birth. Uterine contractions after birth help stop bleeding from the place in the uterus where the placenta breaks away. You may have uterine atony if your uterus is stretched or enlarged (also called distended) from giving birth to twins or a large baby (more than 8 pounds, 13 ounces). It also can happen if you’ve already had several children, you’re in labor for a long time or you have too much amniotic fluid. Amniotic fluid is the fluid that surrounds your baby in the womb.
This is the most common cause of PPH. It happens when the muscles in your uterus don’t contract (tighten) well after birth. Uterine contractions after birth help stop bleeding from the place in the uterus where the placenta breaks away. You may have uterine atony if your uterus is stretched or enlarged (also called distended) from giving birth to twins or a large baby (more than 8 pounds, 13 ounces). It also can happen if you’ve already had several children, you’re in labor for a long time or you have too much amniotic fluid. Amniotic fluid is the fluid that surrounds your baby in the womb. - Uterine inversion. This is a rare condition when the uterus turns inside out after birth.
- Uterine rupture. This is when the uterus tears during labor. It happens rarely. It may happen if you have a scar in the uterus from having a c-section in the past or if you’ve had other kinds of surgery on the uterus.
Conditions that affect the placenta
- Placental abruption.
 This is when the placenta separates early from the wall of the uterus before birth. It can separate partially or completely.
This is when the placenta separates early from the wall of the uterus before birth. It can separate partially or completely. - Placenta accreta, placenta increta or placenta percreta. These conditions happen when the placenta grows into the wall of the uterus too deeply and cannot separate.
- Placenta previa. This is when the placenta lies very low in the uterus and covers all or part of the cervix. The cervix is the opening to the uterus that sits at the top of the vagina.
- Retained placenta. This happens if you don’t pass the placenta within 30 to 60 minutes after you give birth. Even if you pass the placenta soon after birth, your provider checks the placenta to make sure it’s not missing any tissue. If tissue is missing and is not removed from the uterus right away, it may cause bleeding.
Conditions during labor and birth
- Having a c-section
- Getting general anesthesia.
 This is medicine that puts you to sleep so you don’t feel pain during surgery. If you have an emergency c-section, you may need general anesthesia.
This is medicine that puts you to sleep so you don’t feel pain during surgery. If you have an emergency c-section, you may need general anesthesia. - Taking medicines to induce labor. Providers often use a medicine called Pitocin to induce labor. Pitocin is the man-made form of oxytocin, a hormone your body makes to start contractions.
- Taking medicines to stop contractions during preterm labor. If you have preterm labor, your provider may give you medicines called tocolytics to slow or stop contractions.
- Tearing (also called lacerations). This may happen if the tissues in your vagina or cervix are cut or torn during birth. The cervix is the opening to the uterus that sits at the top of the vagina. You may have tearing if you give birth to a large baby, your baby is born through the birth canal too quickly or you have an episiotomy that tears. An episiotomy is a cut made at the opening of the vagina to help let the baby out.
 Tearing also can happen if your provider uses tools, like forceps or a vacuum, to help move your baby through the birth canal during birth. Forceps look like big tongs. A vacuum is a soft plastic cup that attaches to your baby’s head. It uses suction to gently pull your baby as you push during birth.
Tearing also can happen if your provider uses tools, like forceps or a vacuum, to help move your baby through the birth canal during birth. Forceps look like big tongs. A vacuum is a soft plastic cup that attaches to your baby’s head. It uses suction to gently pull your baby as you push during birth. - Having quick labor or being in labor a long time. Labor is different for every woman. If you’re giving birth for the first time, labor usually takes about 14 hours. If you’ve given birth before, it usually takes about 6 hours. Augmented labor may also increase risk of PPH. Augmentation of labor means medications or other means are used to make more contractions of the uterus during labor.
Other conditions
- Blood conditions, like von Willebrand disease or disseminated intravascular coagulation (also called DIC). These conditions can increase your risk of forming a hematoma. A hematoma happens when a blood vessel breaks causing a blood clot to form in tissue, an organ or another part of the body.
 After giving birth, some women develop a hematoma in the vaginal area or the vulva (the female genitalia outside of the body). Von Willebrand’s disease is a bleeding disorder that makes it hard for a person to stop bleeding. DIC causes blood clots to form in small blood vessels and can lead to serious bleeding. Certain pregnancy and childbirth complications (like placenta accreta), surgery, sepsis (blood infection) and cancer can cause DIC.
After giving birth, some women develop a hematoma in the vaginal area or the vulva (the female genitalia outside of the body). Von Willebrand’s disease is a bleeding disorder that makes it hard for a person to stop bleeding. DIC causes blood clots to form in small blood vessels and can lead to serious bleeding. Certain pregnancy and childbirth complications (like placenta accreta), surgery, sepsis (blood infection) and cancer can cause DIC. - Infection, like chorioamnionitis. This is an infection of the placenta and amniotic fluid.
- Intrahepatic cholestasis of pregnancy (also called ICP). This is the most common liver condition that happens during pregnancy.
- Obesity. Being obese means you have an excess amount of body fat. If you’re obese, your body mass index (also called BMI) is 30 or higher. BMI is a measure of body fat based on your height and weight. To find out your BMI, go to www.cdc.gov/bmi.

- Preeclampsia or gestational hypertension. These are types of high blood pressure that only pregnant women can get. Preeclampsia is a condition that can happen after the 20th week of pregnancy or right after pregnancy. It’s when a pregnant woman has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working properly. Signs of preeclampsia include having protein in the urine, changes in vision and severe headache. Gestational hypertension is high blood pressure that starts after 20 weeks of pregnancy and goes away after you give birth. Some women with gestational hypertension have preeclampsia later in pregnancy.
How is PPH tested for and treated?
Your provider may use these tests to see if you have PPH or try to find the cause for PPH:
- Blood tests called clotting factors tests or factor assays
- Hematocrit. This is a blood test that checks the percent of your blood (called whole blood) that’s made up of red blood cells.
 Bleeding can cause a low hematocrit.
Bleeding can cause a low hematocrit. - Blood loss measurement. To see how much blood you’ve lost, your provider may weigh or count the number of pads and sponges used to soak up the blood.
- Pelvic exam. Your provider checks your vagina, uterus and cervix.
- Physical exam. Your provider checks your pulse and blood pressure.
- Ultrasound. Your provider can use ultrasound to check for problems with the placenta or uterus. Ultrasound is a test that uses sound waves and a computer screen to make a picture of your baby inside the womb or your pelvic organs.
Treatment depends on what’s causing your bleeding. It may include:
- Getting fluids, medicine (like Pitocin) or having a blood transfusion (having new blood put into your body). You get these treatments through a needle into your vein (also called intravenous or IV), or you may get some directly in the uterus.
- Having surgery, like a hysterectomy or a laparotomy. A hysterectomy is when your provider removes your uterus. You usually only need a hysterectomy if other treatments don’t work. A laparotomy is when your provider opens your belly to check for the source of bleeding and stops the bleeding.
- Massaging the uterus by hand. Your provider can massage the uterus to help it contract, lessen bleeding and help the body pass blood clots. Your provider may also give you medications like oxytocin to make the uterus contract and lessen bleeding.
- Getting oxygen by wearing an oxygen mask
- Removing any remaining pieces of the placenta from the uterus, packing the uterus with gauze, a special balloon or sponges, or using medical tools or stitches to help stop bleeding from blood vessels.
- Embolization of the blood vessels that supply the uterus. In this procedure, a provider uses special tests to find the bleeding blood vessel and injects material into the vessel to stop the bleeding.
 It’s used in special cases and may prevent you from needing a hysterectomy.
It’s used in special cases and may prevent you from needing a hysterectomy. - Taking extra iron supplements along with a prenatal vitamin may also help. Your provider may recommend this depending on how much blood was lost.
See also: Maternal death
Last reviewed March 2020
Complications after childbirth - causes and consequences
- Increased discharge
- Retention of part of the placenta in the uterine cavity
- Changes in the blood coagulation system
- Disorder of uterine muscle contraction
- Inflammatory process in the vagina or uterus
- Vaginal candidiasis (thrush)
- Postpartum endometritis
- Laktostasis and mastitis
- Postpartum pyelonephritis
- Venous thrombosis
- Discomfort in the area of postoperative sutures
- Urinary incontinence, feces, uterine prolapse
- Hemorrhoids
After giving birth, a woman often thinks that all worries and anxieties are behind her.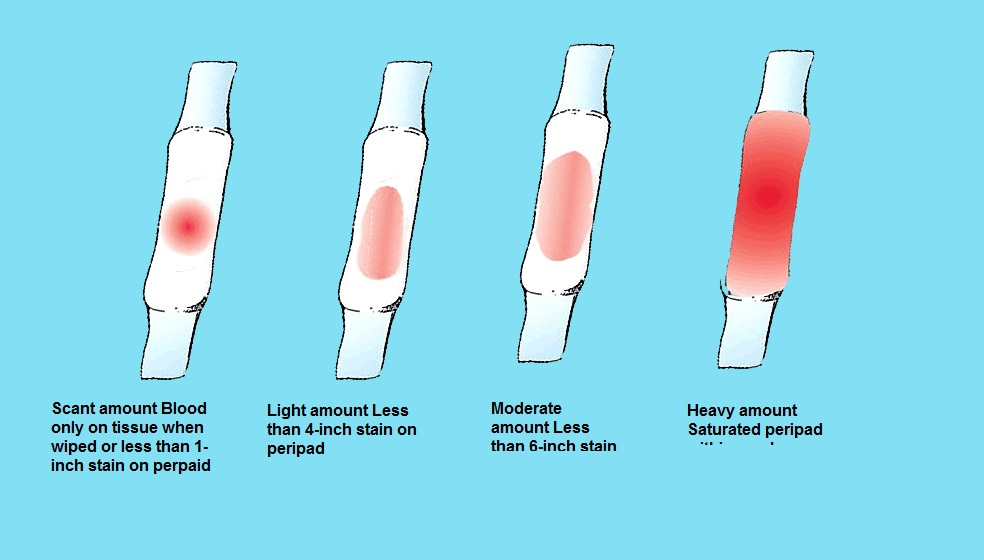 But, alas, sometimes the first, happiest days or weeks of the life together of mother and baby can be overshadowed by various complications. In what cases are postpartum changes normal, and when should you see a doctor? nine0031
But, alas, sometimes the first, happiest days or weeks of the life together of mother and baby can be overshadowed by various complications. In what cases are postpartum changes normal, and when should you see a doctor? nine0031
Labor ends after the third stage of labor, that is, after the birth of the placenta. Following this, the uterus immediately significantly decreases in size, becomes spherical, its cavity is filled with blood clots; the bottom of the uterus at this moment is located approximately in the middle between the womb and the navel. The early postpartum period lasts for 2 hours and during this time the woman is in the maternity ward. Then comes the late postpartum period. This period lasts 6-8 weeks. During this time, there is a reverse development (involution) of all organs and systems that have undergone changes due to pregnancy and childbirth. The exception is the mammary glands, whose function reaches its peak precisely in the postpartum period. The most pronounced involutional changes occur in the genital organs, especially in the uterus. The rate of involutional changes is most pronounced in the first 8-12 days. The uterus and cervix are significantly reduced in size. After the birth of the placenta, a large wound surface remains in the uterus, which takes about 4-6 weeks to heal. During this period, the placental site in the uterus bleeds, spotting - lochia - in the first days is bloody in nature, gradually their color changes from red to reddish-brown, brownish, by the 4th week the discharge almost stops and soon disappear completely. In women who have undergone a cesarean section, everything happens more slowly, because, due to the presence of a suture on the uterus, it contracts worse. Their total amount of spotting during the postpartum period is 500-1500 ml. nine0031
The rate of involutional changes is most pronounced in the first 8-12 days. The uterus and cervix are significantly reduced in size. After the birth of the placenta, a large wound surface remains in the uterus, which takes about 4-6 weeks to heal. During this period, the placental site in the uterus bleeds, spotting - lochia - in the first days is bloody in nature, gradually their color changes from red to reddish-brown, brownish, by the 4th week the discharge almost stops and soon disappear completely. In women who have undergone a cesarean section, everything happens more slowly, because, due to the presence of a suture on the uterus, it contracts worse. Their total amount of spotting during the postpartum period is 500-1500 ml. nine0031
What complications can occur after childbirth
You should consult a gynecologist in the following cases:
Increased amount of discharge
discharge does not stop for a long time, large blood clots appeared. When bleeding occurs, you need to contact an obstetrician-gynecologist, preferably at the maternity hospital where the birth took place. If the bleeding is very heavy (several pads are required within an hour), you do not need to go to the hospital yourself, you need to call an ambulance. nine0031
If the bleeding is very heavy (several pads are required within an hour), you do not need to go to the hospital yourself, you need to call an ambulance. nine0031
Retention of part of the placenta in the uterine cavity
The most common cause of late postpartum hemorrhage (that is, those that occur later than 2 hours after birth) is the retention of a part of the placenta in the uterine cavity. The diagnosis in this case is confirmed by ultrasound. To remove the remnants of the placenta, the walls of the uterus are scraped under general intravenous anesthesia with mandatory subsequent antibiotic therapy to prevent infectious complications. nine0031
Changes in the blood coagulation system
In rare cases, the causes of bleeding may be changes in the blood coagulation system of a hereditary or acquired nature, blood diseases. In these cases, complex drug therapy is required.
Violation of contraction of the muscles of the uterus
Development of bleeding associated with impaired contraction of the muscles of the uterus is possible.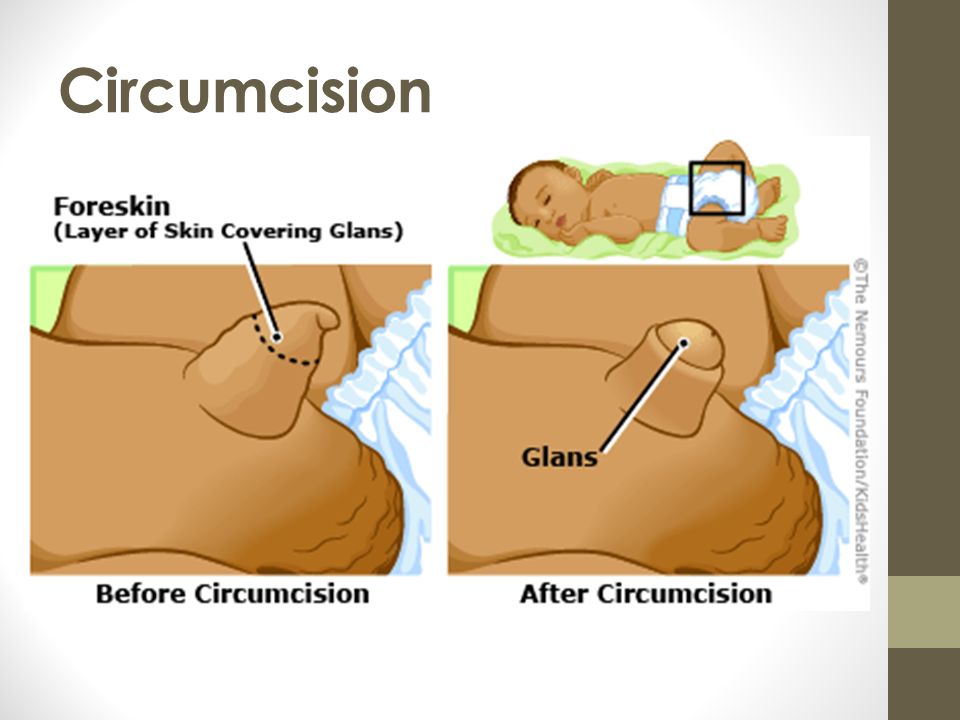 This is the so-called hypotonic bleeding. In the subsequent period, the hypotonic state of the uterus can be caused by its overstretching due to polyhydramnios, multiple pregnancies, large fetuses, and underdevelopment of the uterus. A decrease in the contractility of the uterus is also caused by changes in its very wall (fibroids, the consequences of inflammatory processes, frequent abortions). These bleeding most often occur in the first hours after childbirth and require active treatment with medications, and in severe cases, surgery. nine0053 A sharp, unexpected cessation of spotting should also alert the woman and requires urgent medical attention. In this case, the outflow of blood from the uterus may be disturbed, that is, lochia accumulate in the cavity and the so-called lochiometer develops. Blood clots are a good breeding ground for bacteria, so if the lochiometer is not treated in time, bacteria enter the uterine cavity and endometritis develops - inflammation of the uterine mucosa.
This is the so-called hypotonic bleeding. In the subsequent period, the hypotonic state of the uterus can be caused by its overstretching due to polyhydramnios, multiple pregnancies, large fetuses, and underdevelopment of the uterus. A decrease in the contractility of the uterus is also caused by changes in its very wall (fibroids, the consequences of inflammatory processes, frequent abortions). These bleeding most often occur in the first hours after childbirth and require active treatment with medications, and in severe cases, surgery. nine0053 A sharp, unexpected cessation of spotting should also alert the woman and requires urgent medical attention. In this case, the outflow of blood from the uterus may be disturbed, that is, lochia accumulate in the cavity and the so-called lochiometer develops. Blood clots are a good breeding ground for bacteria, so if the lochiometer is not treated in time, bacteria enter the uterine cavity and endometritis develops - inflammation of the uterine mucosa.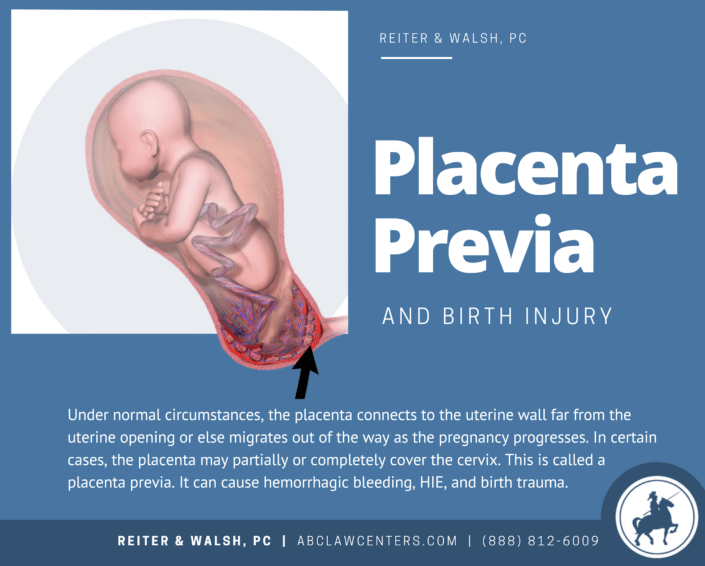 After a caesarean section, a lochiometer occurs more often than after a vaginal birth. Treatment consists in prescribing drugs that reduce the uterus, while using antispasmodics to relax the cervix and restore the outflow of lochia. In some cases, it is necessary to resort to vacuum aspiration of the contents of the uterus under general intravenous anesthesia and mandatory follow-up antibiotic therapy. nine0031
After a caesarean section, a lochiometer occurs more often than after a vaginal birth. Treatment consists in prescribing drugs that reduce the uterus, while using antispasmodics to relax the cervix and restore the outflow of lochia. In some cases, it is necessary to resort to vacuum aspiration of the contents of the uterus under general intravenous anesthesia and mandatory follow-up antibiotic therapy. nine0031
Learn more about the services:
- Ultrasound of the pelvic organs
Inflammatory process in the vagina or uterus
The discharge has acquired an unpleasant odor. This may indicate the development of an inflammatory process in the vagina or in the uterus. In the postpartum period, there was a significant increase in the composition of most groups of bacteria, including bacteroids, Escherichia coli, streptococci, staphylococci. Potentially, all of these species can be the cause of postpartum infectious diseases. A common problem for women after childbirth is the development of bacterial vaginosis. Bacterial vaginosis is a pathology of the vaginal ecosystem caused by the increased growth of predominantly anaerobic bacteria (that is, those that grow in an oxygen-free environment) that actively proliferate in the postpartum period in the woman's vagina and can be pathogens in postpartum endometritis or suppuration of the sutures of the vagina and cervix. Diagnosis of bacterial vaginosis is based on measuring the acidity of the vagina and detecting in a smear on the flora specific for this disease "key cells" (these are cells of the vaginal mucosa covered with anaerobic bacteria). Treatment of bacterial vaginosis in the postpartum period is carried out with local preparations. nine0031
A common problem for women after childbirth is the development of bacterial vaginosis. Bacterial vaginosis is a pathology of the vaginal ecosystem caused by the increased growth of predominantly anaerobic bacteria (that is, those that grow in an oxygen-free environment) that actively proliferate in the postpartum period in the woman's vagina and can be pathogens in postpartum endometritis or suppuration of the sutures of the vagina and cervix. Diagnosis of bacterial vaginosis is based on measuring the acidity of the vagina and detecting in a smear on the flora specific for this disease "key cells" (these are cells of the vaginal mucosa covered with anaerobic bacteria). Treatment of bacterial vaginosis in the postpartum period is carried out with local preparations. nine0031
Vaginal candidiasis (thrush)
The appearance of curdled discharge, itching, burning in the genital area, redness indicates the development of vaginal candidiasis (thrush). The risk of this complication increases with antibiotics. Diagnosis is based on the detection of a large number of yeast-like fungi in a smear on the flora. For treatment, local preparations are used in the form of vaginal suppositories or tablets.
Diagnosis is based on the detection of a large number of yeast-like fungi in a smear on the flora. For treatment, local preparations are used in the form of vaginal suppositories or tablets.
Postpartum endometritis
Purulent discharge, lower abdominal pain, fever. These symptoms may indicate the development of a serious complication - postpartum endometritis (inflammation of the inner lining of the uterus). Most often, endometritis occurs in patients after cesarean section, manual examination of the postpartum uterus, manual separation of the placenta and removal of the placenta (if independent separation of the placenta is difficult due to a violation of the contractile function of the uterus), with a long anhydrous interval (more than 12 hours from the moment of amniotic fluid outflow to the birth of a baby), in women admitted to childbirth with inflammatory diseases of the genital tract (for example, against the background of sexually transmitted infections), in patients with a large number of abortions in the past. The classic form of endometritis occurs on days 1-5. Body temperature rises to 38-39degrees, heart rate increases to 80-100 beats per minute. They note depression of the general condition, chills, dryness and hyperemia of the skin, soreness of the body of the uterus, purulent discharge with a smell. The erased form appears on the 5-7th day, develops sluggishly. The temperature does not exceed 38 degrees, there is no chill. Endometritis after caesarean section always proceeds in a severe form.
The classic form of endometritis occurs on days 1-5. Body temperature rises to 38-39degrees, heart rate increases to 80-100 beats per minute. They note depression of the general condition, chills, dryness and hyperemia of the skin, soreness of the body of the uterus, purulent discharge with a smell. The erased form appears on the 5-7th day, develops sluggishly. The temperature does not exceed 38 degrees, there is no chill. Endometritis after caesarean section always proceeds in a severe form.
An ultrasound examination of the uterus and a complete blood count, which reveal signs of inflammation, help the doctor make a diagnosis. Treatment of endometritis should be started as early as possible. It is carried out in a hospital. Assign bed rest, with acute endometritis cold on the lower abdomen. Postpartum endomeritis is necessarily treated with antibiotics, along with them, agents that reduce the uterus are used. Currently, in many clinics and maternity hospitals, the uterine cavity is washed with cooled solutions of antiseptics. In severe cases, an intravenous infusion of saline solutions is required to improve blood circulation, relieve symptoms of intoxication. nine0031
In severe cases, an intravenous infusion of saline solutions is required to improve blood circulation, relieve symptoms of intoxication. nine0031
In case of untimely treatment, there is a very high risk of spreading the inflammatory process to the entire uterus, small pelvis, the development of sepsis (the appearance of infectious agents in the blood), up to the death of the patient.
Laktostasis and mastitis
In the postpartum period, there may be pain in the mammary glands, a feeling of fullness, an increase in body temperature. When these symptoms appear, you should definitely consult a doctor - an obstetrician-gynecologist in a antenatal clinic or a surgeon. nine0031
Possible causes of pain in the mammary glands and the accompanying fever are lactostasis and mastitis.
Laktostasis (stagnation of milk in the gland), due to blockage of the excretory ducts. Most often, this condition develops when the baby is not properly attached to the chest, violation of the feeding regimen.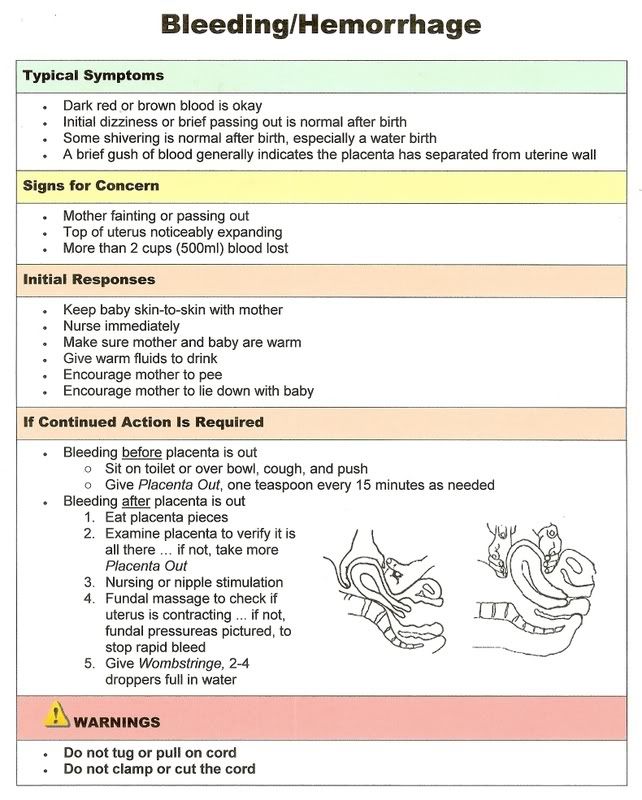 Laktostasis often affects primiparous women. With the stagnation of milk, the mammary gland increases in volume, its dense enlarged lobules are determined. Body temperature can rise to 38-40 degrees. There is no redness of the skin and swelling of the gland tissue, which usually appear with inflammation. After decanting the mammary gland with lactostasis, the pain disappears, painless lobules with clear contours are small in size, and the body temperature decreases. If lactostasis is not eliminated within 3-4 days, mastitis (inflammation of the mammary gland) occurs, since when milk stagnates, the number of microbial cells in the milk ducts increases dramatically, milk is a good breeding ground for various bacteria, which contributes to the rapid progression of inflammation. With the development of mastitis, the body temperature constantly remains high, accompanied by chills. Symptoms of intoxication appear (general weakness, fatigue, headache). The patient is disturbed first by a feeling of heaviness, and then by pain in the mammary gland, which is accompanied by stagnation of milk.
Laktostasis often affects primiparous women. With the stagnation of milk, the mammary gland increases in volume, its dense enlarged lobules are determined. Body temperature can rise to 38-40 degrees. There is no redness of the skin and swelling of the gland tissue, which usually appear with inflammation. After decanting the mammary gland with lactostasis, the pain disappears, painless lobules with clear contours are small in size, and the body temperature decreases. If lactostasis is not eliminated within 3-4 days, mastitis (inflammation of the mammary gland) occurs, since when milk stagnates, the number of microbial cells in the milk ducts increases dramatically, milk is a good breeding ground for various bacteria, which contributes to the rapid progression of inflammation. With the development of mastitis, the body temperature constantly remains high, accompanied by chills. Symptoms of intoxication appear (general weakness, fatigue, headache). The patient is disturbed first by a feeling of heaviness, and then by pain in the mammary gland, which is accompanied by stagnation of milk. The mammary gland increases in volume, areas of redness are noted on the skin. Pumping milk is painful and does not bring relief, after pumping, dense painful areas remain, and a high body temperature persists. In severe cases, pus impurities can be determined in milk. nine0031
The mammary gland increases in volume, areas of redness are noted on the skin. Pumping milk is painful and does not bring relief, after pumping, dense painful areas remain, and a high body temperature persists. In severe cases, pus impurities can be determined in milk. nine0031
To eliminate lactostasis, pumping, local anti-inflammatory ointments, and physiotherapy are used. Mastitis is treated with antibiotics. In some cases, lactation suppression and surgical treatment are required.
Postpartum pyelonephritis
Fever, pain in the back or side, painful urination. These symptoms may indicate the development of postpartum pyelonephritis, that is, inflammation of the kidneys. Critical periods for the development of postpartum pyelonephritis, doctors consider 4-6 and 12-14 days of the postpartum period. The development of the disease is associated with infection in the urinary tract from the genital tract. Most often, the disease develops in puerperas, in the urine of which a small amount of bacteria was found during pregnancy.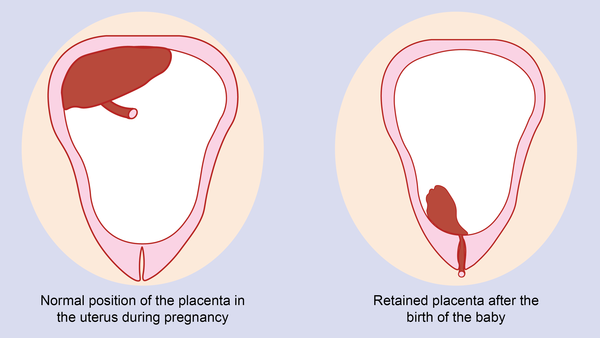 An ultrasound examination of the kidneys and bladder and a urine test help the doctor make the diagnosis. nine0031
An ultrasound examination of the kidneys and bladder and a urine test help the doctor make the diagnosis. nine0031
Treatment of pyelonephritis is mandatory with antibiotics.
Venous thrombosis
Pain in the legs, swelling, redness on the legs along the vein, increased pain when walking - these are symptoms of a serious pathology - venous thrombosis (formation of blood clots in the veins) and require an urgent visit to a surgeon or phlebologist. The most dangerous periods for the occurrence of thrombosis are considered 5-6 days after childbirth or cesarean section, less often thrombosis occurs 2-3 weeks after childbirth. The causes of thrombosis are changes in the blood coagulation system that occur during pregnancy and after childbirth. Physiologically, in the postpartum period, the activation of the coagulation system occurs. As the body tries to stop bleeding. At the same time, the tone of the vessels of the small pelvis and lower extremities is reduced, the veins have not yet had time to adapt to work in new conditions. These conditions trigger the mechanisms of thrombus formation. An important role in the development of postpartum venous thrombosis is also played by the hormonal background, which changes dramatically after the end of pregnancy. nine0031
These conditions trigger the mechanisms of thrombus formation. An important role in the development of postpartum venous thrombosis is also played by the hormonal background, which changes dramatically after the end of pregnancy. nine0031
The risk of developing venous thrombosis is especially high in women with various pathologies of the blood coagulation system, which are detected even before pregnancy or during childbearing. There is a high probability of thromboembolic complications and in the presence of diseases of the cardiovascular system, overweight. The risk of thrombosis also increases in women in the age group after 40 years, in the presence of varicose veins of the lower extremities. The risk of thrombus formation is increased in women who have undergone a caesarean section. An ultrasound examination of the veins, with Dopplerography, that is, an assessment of blood flow in the vessels, helps the doctor in making a diagnosis. For the treatment of venous thrombosis, medications are used, wearing compression stockings. nine0031
nine0031
A severe complication of venous thrombosis is the detachment of part of the thrombus and its movement along the vascular bed. In this case, blood clots, entering the vessels of the lung or brain, cause strokes (impaired cerebral circulation) or pulmonary embolism (blockage of the pulmonary arteries by a thrombus). This serious complication appears as a sharp cough, shortness of breath, pain in the chest, hemoptysis may begin - the appearance of blood streaks in the sputum when coughing. In severe cases, the work of the heart is disrupted and death can occur. nine0031
Unpleasant sensations in the area of postoperative sutures
Discomfort in the area of postoperative sutures after caesarean section or in the area of sutures on the perineum. Normally, after suturing vaginal tears, there may be slight pain for 1-2 days, but they quickly pass. Pain in the postoperative wound after cesarean section may be disturbing for 2 weeks, gradually decreasing. Feeling of heaviness, fullness, pain in the area of the postoperative wound may indicate the accumulation of hematoma (blood) in the area of the sutures.:max_bytes(150000):strip_icc()/hemorrhage-in-miscarriage-meaning-2371523-FINAL-f2ab04cab1cc491e964a45e682f93da5.png) This usually happens in the first three days after childbirth and requires surgical treatment - removal of accumulated blood. Pain, burning, bleeding of the sutures, the appearance of discharge with an unpleasant odor, swelling in the area of the sutures, an increase in body temperature indicates the attachment of an infection and suppuration of the sutures. In these cases, you should also consult a doctor to treat the wound and decide on a further method of treatment. nine0031
This usually happens in the first three days after childbirth and requires surgical treatment - removal of accumulated blood. Pain, burning, bleeding of the sutures, the appearance of discharge with an unpleasant odor, swelling in the area of the sutures, an increase in body temperature indicates the attachment of an infection and suppuration of the sutures. In these cases, you should also consult a doctor to treat the wound and decide on a further method of treatment. nine0031
Urinary incontinence, feces, uterine prolapse
Violation of the physiological functions of the pelvic organs of varying degrees (bladder, rectum), which may appear as in the postpartum period - urinary incontinence, feces, uterine prolapse. The problem of genital prolapse occurs when the pelvic floor muscles have lost the ability to contract so much that individual organs or parts of them do not fall into the projection of the supporting apparatus. The most common cause of pelvic organ prolapse is trauma to the pelvic floor muscles during childbirth. nine0031
nine0031
Hemorrhoids
Quite often, after childbirth, women are worried about the appearance of hemorrhoids - varicose veins of the rectum. The predisposing factor in this case is a significant increase in intra-abdominal pressure during pregnancy and during childbirth. In the case of hemorrhoids, formations appear in the anus, which can be painless, but most often - painful, bleeding and itchy. The appearance of intense pain in the anus, bloody discharge from the rectum are a reason to consult a doctor - a proctologist. Most often, uncomplicated forms of hemorrhoids are treated with local medications - creams and suppositories, in case of complications (nodule pinching, bleeding), surgical treatment is required. nine0031
In any case, if you experience any symptoms that cause concern, it is advisable to consult a doctor, because any complication is best prevented or treated at the very initial stage.
Sitemap
|
|