Sonograms of down syndrome babies
Ultrasound Markers for Down Syndrome
Back to Search Results
1/5/2021
Add to your favorites list
Author: Meaghan Shanahan, MD
Mentor: James F. Smith, MD, MA
Editor: Peter F. Schnatz, DO
Registered users can also download a PDF or listen to a podcast of this Pearl.
Log in now, or create a free account to access bonus Pearls features.
Download
Down Syndrome (trisomy 21) is the most common chromosomal disorder in live born infants. About 6,000 babies are born with Down Syndrome each year in the United States, or about 1 in every 700 births. There are multiple prenatal genetic screening strategies and diagnostic tests aimed at accurate prenatal identification of Down Syndrome and other aneuploidies.
Ultrasound is a key component of aneuploidy screening. Both major structural abnormalities and minor “soft markers” can be detected by ultrasound in fetuses affected with aneuploidies. Down Syndrome can include cardiovascular, central nervous, craniofacial, musculoskeletal, gastrointestinal, and urinary tract system anomalies. Major structural anomalies include duodenal atresia and cardiac anomalies such as septal defects, tetralogy of Fallot, and atrioventricular canal defects. These anomalies are not always detected by prenatal ultrasound screening.
Nuchal translucency (NT) can be assessed in the first trimester. NT reflects the subcutaneous fluid-filled space between the back of the fetal neck and the overlying skin. There is an association between increased NT measurement and risk of aneuploidies, including Down Syndrome, with the detection rate for Down Syndrome being 64-70%. A nuchal cystic hygroma represents pathologic nuchal edema and is associated with aneuploidy, including Down Syndrome, in about 50% of cases. A hypoplastic or absent nasal bone can be detected in the first trimester in 62-70% of fetuses with Down Syndrome, but is present in only 1% of normal fetuses.
In the second trimester, the most commonly assessed soft markers include echogenic intracardiac foci, pyelectasis, short femur length, choroid plexus cysts, echogenic bowel, thickened nuchal skin fold, and ventriculomegaly. While the likelihood ratios associated with the first four are generally less than 2, the likelihood ratios for echogenic bowel, thickened nuchal fold, and ventriculomegaly are all over 5. The predictive value for echogenic bowel, thickened nuchal fold, and ventriculomegaly, even when isolated, is sufficiently high to prompt further genetic counseling and offering additional aneuploidy screening or diagnostic testing. Findings with lower predictive values such as an isolated choroid plexus cyst, echogenic intracardiac focus, or pyelectasis may prompt aneuploidy screening if not already done. The probability of Down Syndrome is increased when multiple soft markers are present and may prompt diagnostic testing. As an isolated finding, an increased nuchal skin fold confers the highest risk of aneuploidy and is the most powerful second trimester ultrasound marker, with a likelihood ratio of 11-18 and > 99% specificity for Down Syndrome.
Ultrasonography should not be used by itself to diagnose or exclude Down Syndrome. Sensitivity for detecting Down Syndrome is increased when ultrasound findings are interpreted in combination with serum analyte screening tests such as first and second trimester screening and integrated and sequential screening. Cell-free DNA has a detection rate for Down Syndrome of 99%. Diagnostic testing, such as amniocentesis or chorionic villus sampling, should be offered when screening test results are positive.
Further Reading:
American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics; Committee on Genetics; Society for Maternal-Fetal Medicine. Screening for Fetal Chromosomal Abnormalities: ACOG Practice Bulletin, Number 226. Obstet Gynecol. 2020 Oct;136(4):e48-e69. doi: 10.1097/AOG.0000000000004084. PMID: 32804883.
Committee on Practice Bulletins—Obstetrics and the American Institute of Ultrasound in Medicine. Practice Bulletin No. 175: Ultrasound in Pregnancy. Obstet Gynecol. 2016 Dec;128(6):e241-e256.
Practice Bulletin No. 175: Ultrasound in Pregnancy. Obstet Gynecol. 2016 Dec;128(6):e241-e256.
Initial approval: November 2017. Reaffirmed May 2019, Reaffirmed January 2021, Minor Revision July 2022
********** Notice Regarding Use ************
The Society for Academic Specialists in General Obstetrics and Gynecology, Inc. (“SASGOG”) is committed to accuracy and will review and validate all Pearls on an ongoing basis to reflect current practice.
This document is designed to aid practitioners in providing appropriate obstetric and gynecologic care. Recommendations are derived from major society guidelines and high-quality evidence when available, supplemented by the opinion of the author and editorial board when necessary. It should not be construed as dictating an exclusive course of treatment or procedure to be followed.
Variations in practice may be warranted when, in the reasonable judgment of the treating clinician, such course of action is indicated by the condition of the patient, limitations of available resources, or advances in knowledge or technology. SASGOG reviews the articles regularly; however, its publications may not reflect the most recent evidence. While we make every effort to present accurate and reliable information, this publication is provided “as is” without any warranty of accuracy, reliability, or otherwise, either express or implied. SASGOG does not guarantee, warrant, or endorse the products or services of any firm, organization, or person. Neither SASGOG nor its respective officers, directors, members, employees, or agents will be liable for any loss, damage, or claim with respect to any liabilities, including direct, special, indirect, or consequential damages, incurred in connection with this publication or reliance on the information presented.
SASGOG reviews the articles regularly; however, its publications may not reflect the most recent evidence. While we make every effort to present accurate and reliable information, this publication is provided “as is” without any warranty of accuracy, reliability, or otherwise, either express or implied. SASGOG does not guarantee, warrant, or endorse the products or services of any firm, organization, or person. Neither SASGOG nor its respective officers, directors, members, employees, or agents will be liable for any loss, damage, or claim with respect to any liabilities, including direct, special, indirect, or consequential damages, incurred in connection with this publication or reliance on the information presented.
Copyright 2022 The Society for Academic Specialists in General Obstetrics and Gynecology, Inc. All rights reserved. No re-print, duplication or posting allowed without prior written consent.
Back to Search Results
Ultrasound scan spots Down's syndrome
Ultrasound scan spots Down's syndrome
Download PDF
- Published:
- Kendall Powell
Nature (2002)Cite this article
-
55k Accesses
-
1 Altmetric
-
Metrics details
Nasal bone holds key to safer test for birth defects.
You have full access to this article via your institution.
Download PDF
Download PDF
Women over 35 have a 1-in-300 chance of having a Down's syndrome baby. Credit: © ISUOG
An ultrasound scan could save many mothers the decision over whether to have an amniocentesis and risk losing a baby.
Nearly two-thirds of 15-22-week-old fetuses with Down's syndrome lack a nasal bone, fetal-medicine specialist Kypros Nicolaides, of King's College, London, and his colleagues found1.
For normal fetuses, the figure is 1%. This makes it unlikely that the test would wrongly diagnose Down's syndrome.
The nasal scan is more accurate than previous ultrasound markers, such as the length of leg bones. Some UK and US doctors are already using the nose-bone scan in combination with other tests.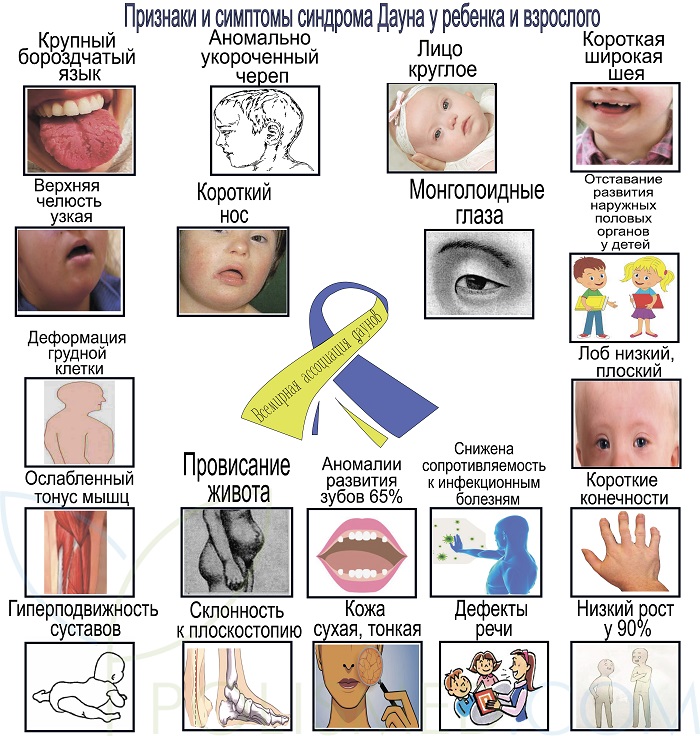
The detection of Down's syndrome requires a sample of fetal cells from the fluid surrounding the fetus. This test, called an amniocentesis, causes miscarriage in about 1% of women who have it.
The nose-bone scan will reduce these tests, says Nicolaides. Women over 35 have a 1-in-300 chance of having a Down's syndrome baby. Each year, in the United States, 375,000 such women are encouraged to have an amniocentesis.
The scan could save many mothers the agonizing decision over whether to have an amniocentesis and risk losing a normal baby. "If the nasal bone is present, then the risk of having a baby with Down's syndrome is automatically reduced to one-third of what it was before the scan," says Nicolaides.
The nasal bone can be a good marker for Down's syndrome, agrees Rosemary Reiss, who practises maternal fetal medicine at Brigham and Women's Hospital in Boston, Massachusetts.
But the proportion of false alarms jumps to 8% for patients of African descent, says Reiss. Differences among ethnic groups will have to be understood for screening to succeed, she says.
Differences among ethnic groups will have to be understood for screening to succeed, she says.
Testing time
The nasal-bone test gives similar results in fetal scans as early as 11-14 weeks2. The 15-22-week point coincides with the traditional check-up for high-risk mothers. "This is a simple scan that women have anyway," says Nicolaides.
The new test will help give patients a better idea of the risk they face, says Richard O'Shaughnessy, director of the fetal treatment programme at Ohio State University. He suggests combining it with blood tests and another ultrasound marker that looks for fluid collecting behind the neck.
References
Cicero, S. et al. Nasal bone hypoplasia in trisomy 21 at 15-22 weeks' gestation. Ultrasound in Obstetrics and Gynecology, Published online, doi:10.1002/uog.19, (2002).
Cicero, S.
 , Curcio, P., Papageorghiou, K. H., Sonek, J.. & Nicolaides, A.B. Absence of nasal bone in fetuses with trisomy 21 at 11-14 weeks of gestation: an observational study. Lancet , 358, 1665 - 1667, (2001).
, Curcio, P., Papageorghiou, K. H., Sonek, J.. & Nicolaides, A.B. Absence of nasal bone in fetuses with trisomy 21 at 11-14 weeks of gestation: an observational study. Lancet , 358, 1665 - 1667, (2001).Article Google Scholar
Download references
Authors
- Kendall Powell
View author publications
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and Permissions
About this article
Diagnosis of Down's syndrome according to ultrasound, timing of the examination, signs of fetal chromosomal pathology
It is possible to diagnose Down's syndrome already in the early stages of pregnancy according to ultrasound examination (ultrasound) of the fetus . The method is based on the use of high-frequency sound, which is reflected from various surfaces with different intensities. Deciphering the signals allows the doctor to create a two-dimensional image of the internal structure of the area under study. nine0003
Deciphering the signals allows the doctor to create a two-dimensional image of the internal structure of the area under study. nine0003
Is it possible to detect Down syndrome by ultrasound
Down syndrome in the fetus is diagnosed by ultrasound in 60-90% of cases. High accuracy of the examination is achieved by comparing the development of the fetus with the norm. In addition to Down syndrome, ultrasound can detect signs of a number of other genetic malformations. Pathologies in the structure of the heart, incomplete rotation of the intestine, duodenal atresia can also serve as signs of Down syndrome in the fetus, all these malformations are recorded by ultrasound. nine0003
Tests before marriage
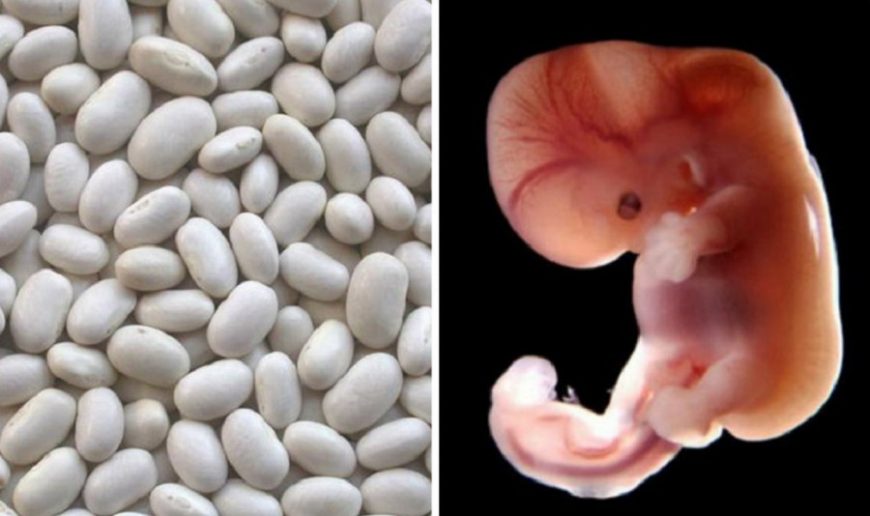
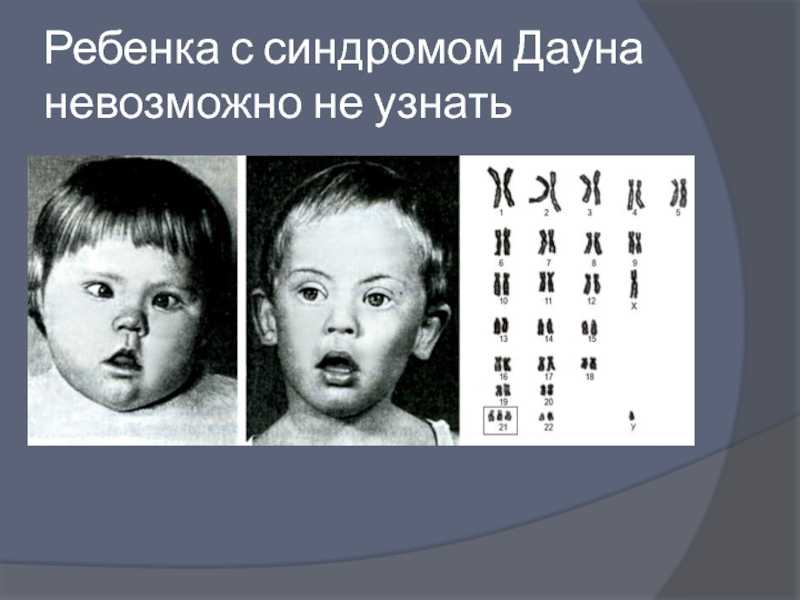
Down syndrome is observed in one case in 700-800 pregnancies and is characterized by the presence of an extra 21st chromosome. The syndrome affects the future life of the child.
The possibility of having a child with Down syndrome increases with the age of the parents.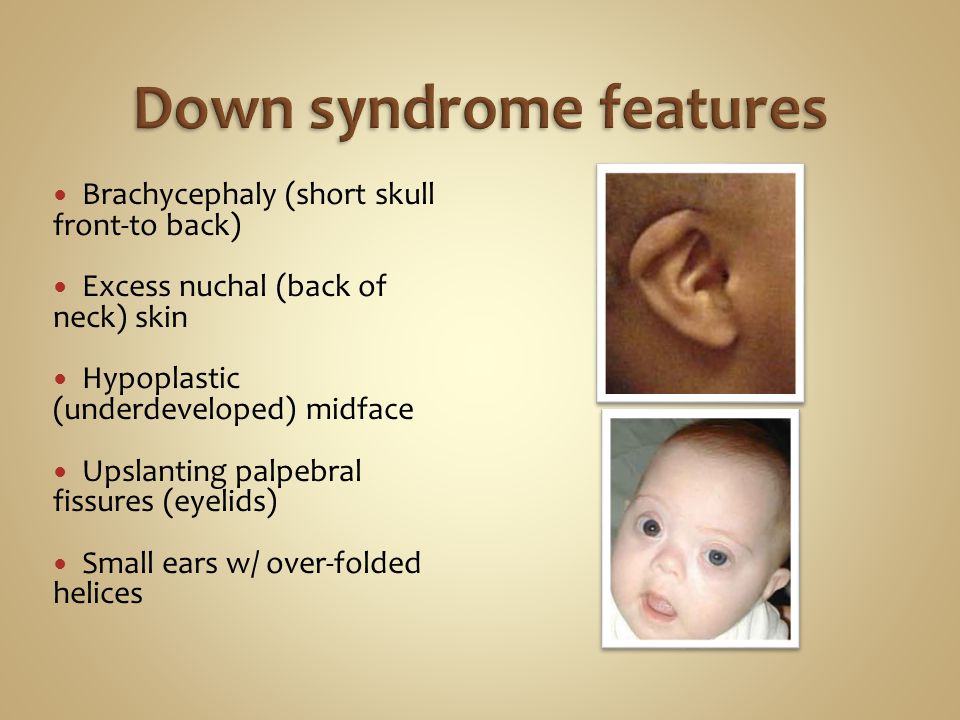 In addition, the risk of a chromosomal abnormality increases significantly if one of the parents already has Down syndrome. In some cases, the pathology is mosaic in nature and may be invisible even to very close people. nine0003
In addition, the risk of a chromosomal abnormality increases significantly if one of the parents already has Down syndrome. In some cases, the pathology is mosaic in nature and may be invisible even to very close people. nine0003
Down's syndrome is reliably diagnosed in the perinatal period using ultrasound and a number of other methods.
How does Down syndrome manifest itself after birth?
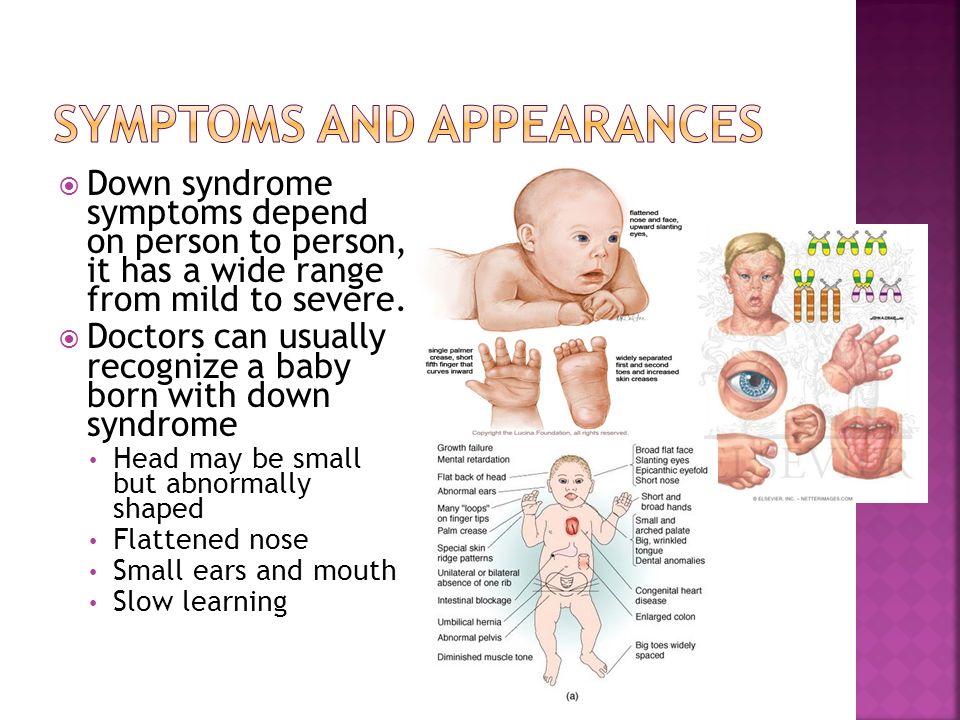
Children with Down syndrome have a number of external differences. Their faces are flatter, with a slightly pronounced bridge of the nose and an epicanthal fold at the inner corners of the eyes. The skull of the child is shortened, with a flat occiput.
After birth, children with Down syndrome are somewhat behind in physical and mental development. Over time, the mental retardation, in comparison with other children, will be more and more noticeable. nine0003
In addition, people with Down syndrome are more likely to suffer from congenital heart defects (occur in almost 40% of cases).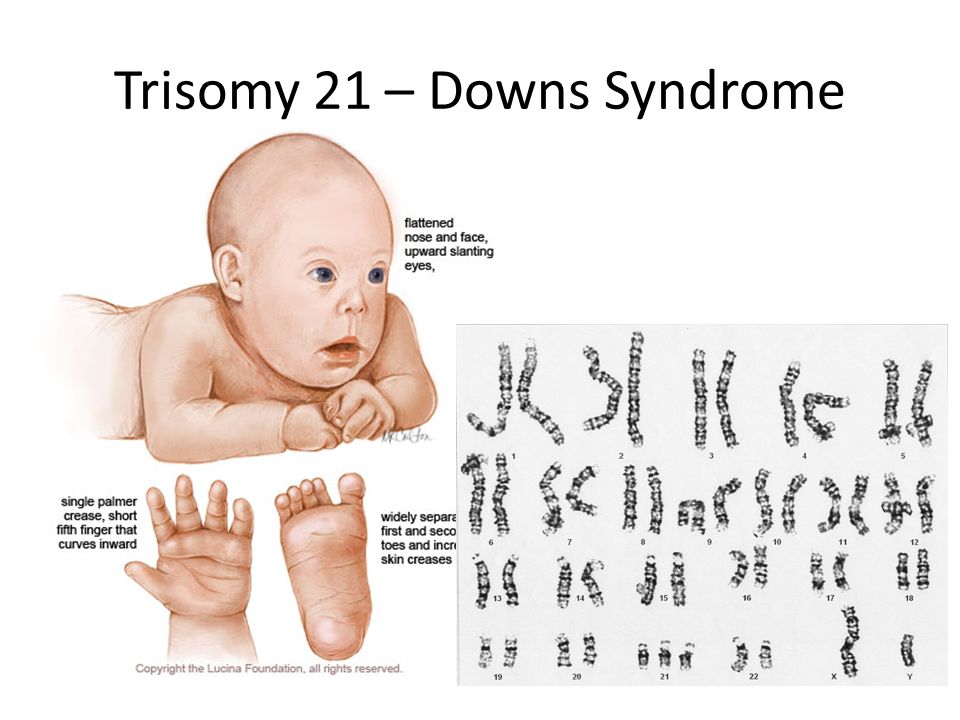 The presence of an extra chromosome significantly increases the risk of developing some other diseases: cataracts, Alzheimer's, myeloid leukemia, and often there are disorders in the digestive system. Weakened immunity makes people with the syndrome more vulnerable to viruses and colds.
The presence of an extra chromosome significantly increases the risk of developing some other diseases: cataracts, Alzheimer's, myeloid leukemia, and often there are disorders in the digestive system. Weakened immunity makes people with the syndrome more vulnerable to viruses and colds.
Methods for diagnosing chromosomal abnormalities
Chromosomal abnormalities can be diagnosed by non-invasive and invasive methods. The first allow you to establish a number of pathologies characteristic of chromosomal abnormalities. Invasive methods are used to make an accurate diagnosis. nine0003
ultrasound
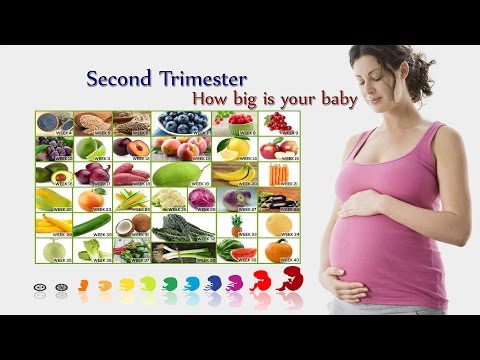
Establishing the risk of Down syndrome in a fetus by ultrasound is called ultrasound screening. Often the method is used in combination with a biochemical analysis of the mother's blood. The accuracy of diagnosing Down syndrome on ultrasound in the second trimester of pregnancy can reach 91%. The examination is carried out at 11-13 and 16-18 weeks of pregnancy.
Invasive techniques
Invasive prenatal diagnosis can lead to a number of complications. The risk to the fetus and mother is small. However, the procedure is prescribed only if necessary, if Down's syndrome in the fetus is confirmed by ultrasound data and maternal blood tests. nine0003
Biochemical screening
The main task of screening is to identify risk groups in terms of having a child with serious illnesses, including those with chromosomal disorders. Biochemical screening is recommended for all women in the first and second trimesters of pregnancy.
Diagnostics in the first trimester of pregnancy
In the first trimester of pregnancy, Down syndrome can be diagnosed by ultrasound, due to the presence of a number of pathologies. These include an increased thickness of the nuchal space in the fetus, reduced, compared with the norm, the size of the cerebellum and frontal lobe, impaired bone formation, heart defects, absence of the nasal bone, etc.
It is important to remember that no single marker will be considered sufficient for a reliable diagnosis of Down syndrome - there is not enough ultrasound data for this. Therefore, having received the results of the examination, you do not need to be upset ahead of time - you need to consult a specialist.
What to do if the diagnosis is confirmed?
Examination can show pathology in the fetus. It is up to the parents to decide what to do next. If they are ready for responsibility, then, even if Down syndrome is confirmed by ultrasound and invasive research methods, parents can leave the child. Despite the peculiarities of development, he can live a long and happy life. In cases where there are too many pathologies, doctors may recommend terminating the pregnancy. However, even in this case, the decision will be made by the parents. nine0003
Sign up for a consultation or diagnostic today!
You can make an appointment by phone: +7 (812) 901-03-03
Or leave a request
full name
Phone number
By clicking the "Make an appointment" button, I accept the terms of the Personal Data Processing and Security Policy and consent to the processing of my personal data. nine0003
nine0003
Our medical centers
Making an appointment
Patient's last name *
Incorrect first name
nine0002 Name *Middle name
nine0002 Contact phone *E-mail *
nine0002 By clicking the "Make an appointment" button, I accept the terms of the Personal Data Processing and Security Policy and consent to the processing of my personal data.
Registration and payment for repeated online appointment
Patient's last name *
Incorrect first name
nine0002 Name *Middle name *
nine0002 Contact phone *E-mail *
nine0002 By clicking the "Submit request" button, I accept the terms of the Personal Data Processing and Security Policy and consent to the processing of my personal data.
About cookies on this website
We use cookies, IP addresses and device data for analytics to make your visit to the site convenient and personalized. You can disable cookies in your browser settings. By continuing to use our site, you consent to the processing of the listed data and accept the terms of the Privacy Policy. nine0003
Ultrasound diagnostics of Down syndrome and other chromosomal abnormalities
- Ultrasound of the fetus is the main method for diagnosing the likelihood of Down syndrome
- Basic ultrasound markers of Down syndrome
- Signs of Down syndrome with ultrasound in the second trimester of pregnancy
- How else can you determine the risk of having a baby with Down syndrome
Down's syndrome is a relatively common congenital pathology caused by the presence of an extra chromosome in 21 pairs. Down syndrome is also called trisomy on 21 pairs of chromosomes. Of all the chromosomal abnormalities, this pathology is the most well-known for a wide range of people.
Of all the chromosomal abnormalities, this pathology is the most well-known for a wide range of people.
Down's syndrome is associated with many significant malformations. Such as, for example, congenital heart defects, duodenal atresia (a condition where part of the small intestine does not develop), an increased risk of developing acute leukemia (leukemia). About 50% of children with this condition are born with heart defects, the most common of which is a ventricular septal defect. Another disease that is often observed in such children is Hirschsprung's disease - an aganglionic area of the large intestine, leading to the development of intestinal obstruction. nine0003
Screening tests during pregnancy are used to assess the risk of having a baby with Down syndrome. These tests are painless and non-invasive (do not cause damage to the tissues of the pregnant woman and fetus), but do not accurately judge the presence or absence of congenital pathology. Nevertheless, their widespread use makes it possible to suspect risks and recommend invasive procedures. Invasive diagnostic methods include interventions performed under ultrasound guidance - amniocentesis, chordocentesis and chorionic villus sampling. nine0003
Invasive diagnostic methods include interventions performed under ultrasound guidance - amniocentesis, chordocentesis and chorionic villus sampling. nine0003
Fetal ultrasound is the main way to diagnose the likelihood of Down syndrome
Fetal ultrasound to detect developmental abnormalities is called ultrasound screening. Most often, ultrasound screening is combined with biochemical blood tests of a pregnant woman, and such a study is called combined screening. Depending on the choice of criteria, the probability of detecting Down syndrome in the second trimester is 60-91%. The use of color Doppler technology for ultrasound screening makes it possible to detect defects in the fetal heart and increases the accuracy of diagnosis. nine0003
Major ultrasound markers of Down syndrome
Ultrasound markers are the ultrasound measurements most likely to be associated with a high chance of having Down syndrome in the fetus. None of these markers is specific, that is, inherent only in this pathology.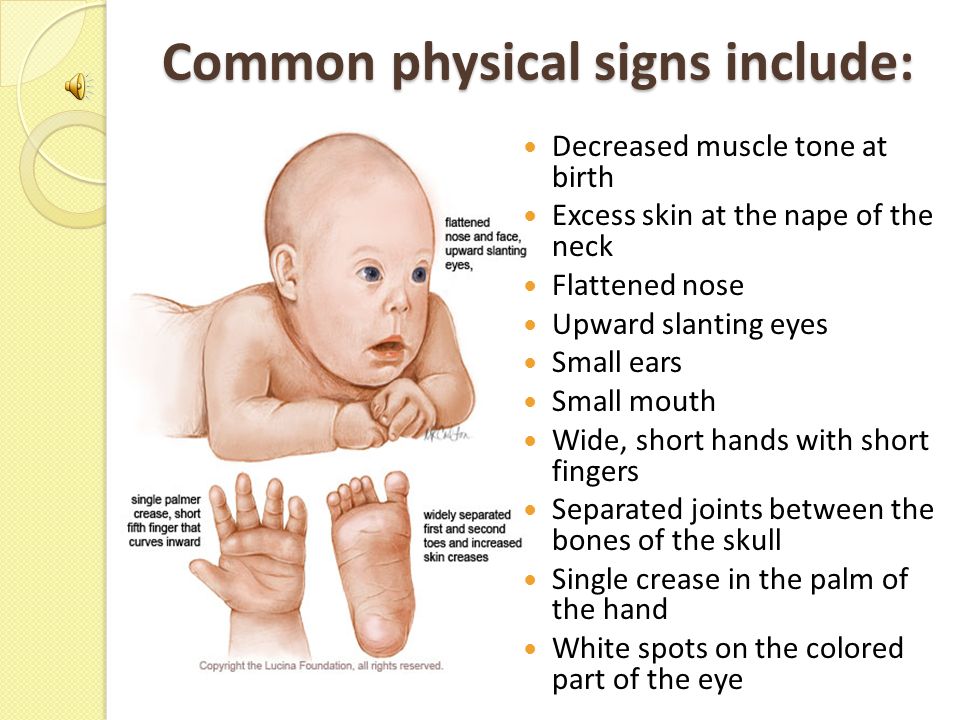 The following indicators are taken into account: the thickness of the collar space (75% of sensitivity), the absence of the nasal bone (58%), heart defects, short femurs and humeri, hyperechoic intestines, choroid plexus cysts, echogenic foci in the heart, signs of duodenal atresia . Of course, none of these markers is an absolute sign of a chromosomal abnormality. nine0003
The following indicators are taken into account: the thickness of the collar space (75% of sensitivity), the absence of the nasal bone (58%), heart defects, short femurs and humeri, hyperechoic intestines, choroid plexus cysts, echogenic foci in the heart, signs of duodenal atresia . Of course, none of these markers is an absolute sign of a chromosomal abnormality. nine0003
Measuring the thickness of the nuchal space
The nuchal space (cervical fold) is the area between the folds of fetal tissues, which is transparent on ultrasound, located below the occiput in the area of neck formation. In children with chromosomal abnormalities, such as Down's syndrome or trisomy 18, fluid accumulates in this place. The measurement of this space is carried out from 11 to 14 weeks during the ultrasound of pregnancy in the first trimester. Measurements obtained at this time are the most significant for predicting the individual risk of developing fetal chromosomal abnormalities. The thickness of the collar space more than 3 mm is taken as an indicator of an increased likelihood of genetic defects in the fetus.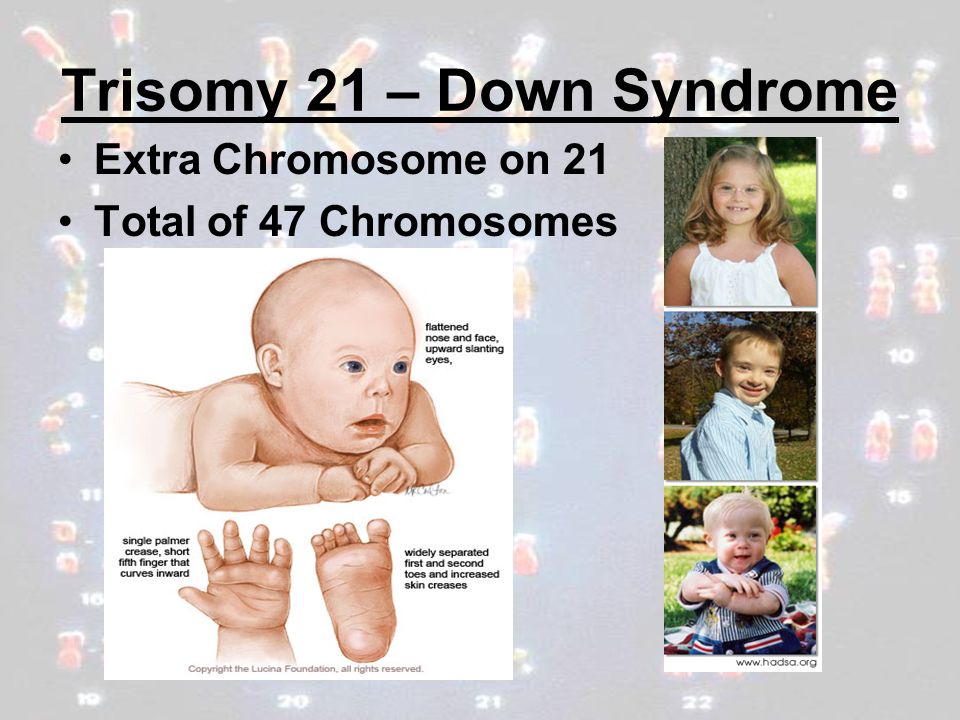 The increase in the collar space does not mean that the fetus necessarily has Down syndrome, but if we take into account the gestational age of the fetus on which measurements were taken, the age of the mother and biochemical screening indicators, the probability of a correct diagnosis becomes higher than 80%. Although nuchal thickness screening is one of the most important tests for detecting chromosomal abnormalities, there are biases. The error arises due to violations of the measurement technique. This applies not only to measurements of the collar space, but also to the nasal bone. There are errors due to the human factor. The correct measurement technique and the experience of the ultrasound specialist are very important. nine0003
The increase in the collar space does not mean that the fetus necessarily has Down syndrome, but if we take into account the gestational age of the fetus on which measurements were taken, the age of the mother and biochemical screening indicators, the probability of a correct diagnosis becomes higher than 80%. Although nuchal thickness screening is one of the most important tests for detecting chromosomal abnormalities, there are biases. The error arises due to violations of the measurement technique. This applies not only to measurements of the collar space, but also to the nasal bone. There are errors due to the human factor. The correct measurement technique and the experience of the ultrasound specialist are very important. nine0003
Measurements of the pelvis and structures of the fetal brain
In fetuses with trisomy 21, ultrasound may show cerebellar hypoplasia (reduction in size) and a decrease in the frontal lobe. These facts are used to assess the likelihood of Down syndrome. The combination of a shortened transverse size of the cerebellum and a decrease in the fronto-thalamic distance is of greater importance for the diagnosis of this chromosomal anomaly than measuring each distance of intracerebral structures separately. nine0003
The combination of a shortened transverse size of the cerebellum and a decrease in the fronto-thalamic distance is of greater importance for the diagnosis of this chromosomal anomaly than measuring each distance of intracerebral structures separately. nine0003
In a fetus with Down's syndrome during ultrasound, the length of the iliac bones is clearly reduced and the angle between these bones is increased. This can be measured most clearly at the level of the middle of the sacrum in cross section.
Signs of Down's syndrome during ultrasound in the second trimester of pregnancy
When performing ultrasound of the fetus in the second trimester of pregnancy, such abnormalities can be detected as a violation of the formation of bones of the skeleton, expansion of the collar space by more than 5 mm, the presence of heart defects, expansion of the renal pelvis (pyeloectasia ), echogenicity of the intestine, cysts of the choroid plexus of the brain. Moreover, only heart defects, disorders of skeletal formation and expansion of the collar space are independent risk factors.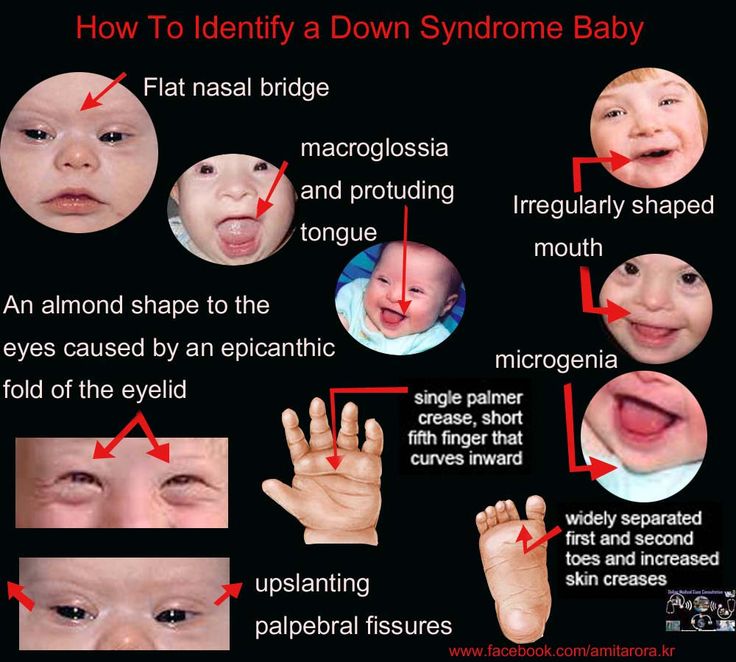 nine0003
nine0003
The use of only one of the measurements in assessing the probability of the presence of chromosomal abnormalities of the fetus, for example, determining the thickness of the collar space or measuring the iliac angle, is less accurate than taking into account the totality of measurements.
Another way to determine the risk of having a baby with Down syndrome
In addition to ultrasound signs, biochemical screening in the first and second trimester is used to determine the degree of risk. In this case, the blood of a pregnant woman is examined. The best results are obtained by combining ultrasonic and biochemical signs. If the combination of factors is threatening, a decision may be made to conduct invasive methods for diagnosing Down syndrome and other chromosomal abnormalities. Invasive techniques consist in obtaining particles of the skin or blood of the fetus, followed by genetic analysis. These methods are 100% reliable. At the same time, even complete well-being during screening in the first and second trimester using ultrasound and biochemical markers cannot guarantee the absence of chromosomal abnormalities in the fetus.