Baby movement in 9th month pregnancy
Belly, Symptoms, Baby’s Development, More
By now, at 9 months pregnant, you’ve been anticipating the birth of your little one for what feels like forever. (Remember when you wondered if your bump could possibly get any bigger? That was adorable.)
You’ve read all the pregnancy books, taken the birthing classes, and likely oohed and awed over tiny baby clothes at your baby shower — virtual option included, of course. And while anticipating your baby’s arrival has been fun, you’re probably ready to get this show on the road.
Here’s what to expect at 9 months pregnant — from how you can tell if labor is starting to when it’s time to head to the hospital. (Finally!)
The main symptom you may notice at this stage in pregnancy is called “Get-this-baby-out-of-me-itis.” Rest assured, it’s completely normal.
You’re probably feeling more than a little uncomfortable as your baby reaches full-term — on average, around 7 pounds 6 ounces for boys and 7 pounds 2 ounces for girls — so your discomfort is for good reason.
Along with that sizeable baby and your body preparing for birth, here’s what may be in store for you this month:
- back pain, thanks to the constant work required to keep you from toppling over frontward
- pelvic pressure, as baby’s head moves lower and grows bigger
- lightening, when the baby drops into the birth canal and you may be able to breathe easier (but you’ll probably feel more discomfort with the baby in a lower position)
- interrupted sleep, as those once-fluttering kicks become quite forceful
- exhaustion, because, well, you’ve been growing a human (or two) for 9 months
- constipation, as the baby grows and interferes with traffic flow
- frequent urination, due to pregnancy hormones and your baby literally tap-dancing on your bladder
- changes in appetite, but it’s different for everyone — you could feel hungrier or experience a decreased appetite, thanks to the cramped abdominal real estate
You may also have:
- Braxton-Hicks contractions
- nesting instincts
- increased vaginal discharge
During your last weeks of pregnancy, your baby goes through a lot of growth, which means that you will, too.
Depending on your body mass index before becoming pregnant, and if you’re pregnant with one baby or twins, you may gain approximately 1 to 2 pounds per week during the third trimester. (This may slow in the final weeks before giving birth.)
While it can be tempting to compare, everyone’s baby bumps look different. Your height and abdominal muscle strength make a big difference in how your body carries your baby.
If you’re taller, you may tend to carry your baby more in front, and if you have more toned abdominal muscles, you may carry higher.
If you have any concerns about your weight gain or the size of your pregnant belly, let your doctor know. They may request an ultrasound if your measurements aren’t what they expect.
Since last month, your baby has most likely packed on 1 to 2 extra pounds and 1 to 2.5 inches.
In addition to rocking an impressive growth spurt, your baby experiences significant development during the ninth month of pregnancy.
For instance, baby’s lungs are maturing to breathe outside of the womb, their reflexes are more coordinated, and they can blink, turn their head, and grasp.
Because babies are still developing every day in the womb, it’s important to avoid induction before 39 weeks unless medically indicated. (You’re considered full-term at 37 weeks, but most doctors recommend avoiding elective C-section or induction until 39 weeks, unless there’s a medical reason.)
As you near the end of your pregnancy, your baby will start to settle lower in the abdomen. Your baby’s position should also change to head down to prepare for delivery. (Most babies turn head down by week 36 of pregnancy.)
If your baby hasn’t flipped yet, your doctor will discuss any next steps with you. They may recommend some methods to help turn your baby — or a C-section may be recommended for babies that insist on staying breech.
It may seem like your baby is moving less during this time due to the tighter space. Your doctor may ask that you keep a kick count to keep track of fetal movements. If you notice any decrease in your baby’s movements, or have any concerns about your baby’s activity, be sure to contact your doctor.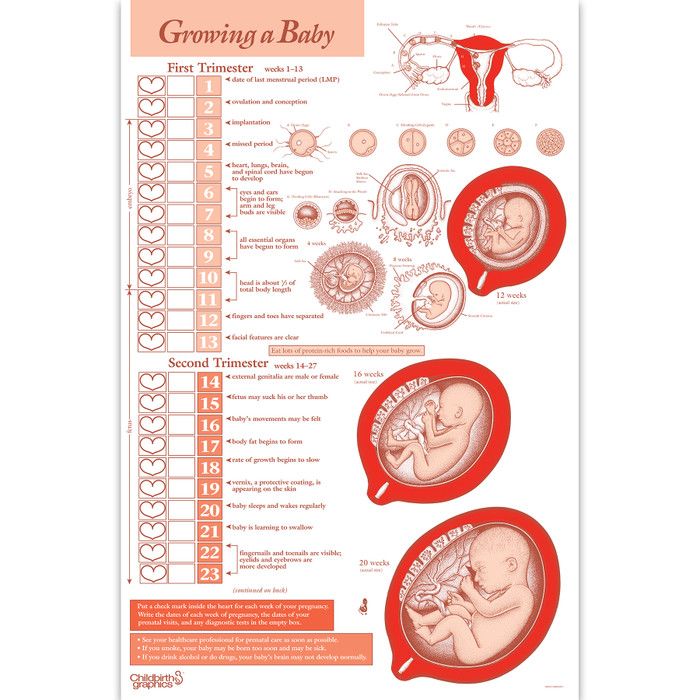
If you’re expecting twins, there’s a good chance that you’ll be meeting them this month. A majority of twins are born before 37 weeks and some even before 34 weeks.
And although there’s a good chance your twins will be on the smaller side — most twins weigh less than 6 pounds — babies born between 34 and 36 weeks have a near 100 percent chance of survival.
And if your babies do require any care after birth, your medical team will be prepped and ready as they welcome them into the world.
As your due date approaches, you may find yourself slowing down activity-wise, and that’s completely OK. Every pregnant person is different.
Some may stay active right up until their due date, while others may need to kick back and put their feet up more often. Listen to your own body and rest when you need to.
The good news is there’s no reason to slow down your activities unless your doctor has told you otherwise. You can maintain your normal exercise routine — although now isn’t the time to take up anything new, like CrossFit or rock climbing — and modify exercises as needed.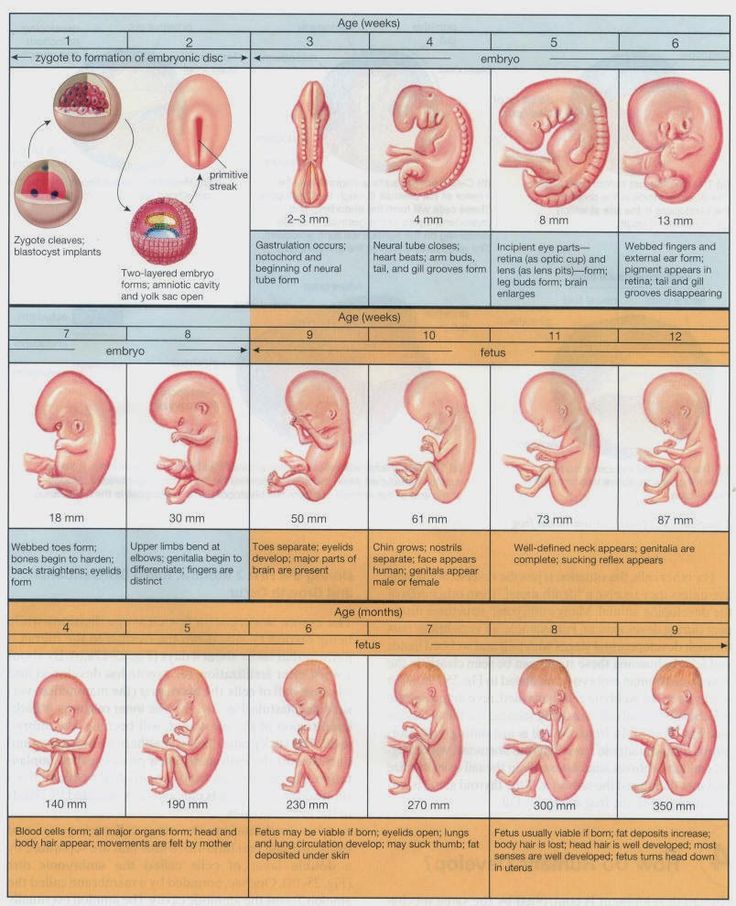
If you’re still feeling frisky, you can still engage in sexual activity unless your doctor has told you otherwise. In fact, sex might help speed up labor if you’re full-term. Sperm in the vagina could help the cervix ripen, and orgasms may help get contractions going.
On the other hand, if you’re at high risk for preterm labor, your doctor may ask you to refrain from sexual activity. Also, keep in mind that if your water does happen to break, you’ll want to avoid any sexual activity after that, as it could pose a risk of infection.
The big day is coming, so make sure you’re ready by checking these pre-baby items off your list:
- Finish up any prep classes you might need. You’ve probably already finished your childbirth classes (and if you haven’t, it’s not too late!), but you could also take an infant CPR class, lactation class, or baby care course.
- Take a hospital or birth center tour. Call your birthing facility to arrange an in-person or virtual tour.
- Pack your labor and delivery bags. You don’t need a ton of stuff for baby — a take-home outfit or two will do — but you’ll want to be sure to bring:
- your insurance card
- your COVID-19 vaccination card, if you have one
- comfy clothes for you
- a pair of cheap slippers or slides, as hospital floors can be pretty gross
- some comfort items, like a favorite blanket or pillow
- phone chargers
- snacks, but keep in mind you may not be able to eat during labor
- copies of your birth plan
- Pick a pediatrician. Many pediatricians offer consults to new parents, so you can determine if they’re a good fit. You’ll visit your baby’s pediatrician a lot in the first year (and for many years after!), so it’s worth spending time finding one you connect with.
- Prep your birth team. There will most likely be restrictions on who can be in the room with you, but if you have a doula or partner, prep them about what to do when you go into labor.

- Research photographers. If you’d like any final pregnancy photos, want birth photography, or are hoping to squeeze in a newborn photoshoot, now is a great time to get this scheduled.
- Wash a few of your baby’s outfits. There’s no need to wash everything, but take advantage of your nesting instincts (if you’ve got ’em) to get a few outfits ready. Leave tags on the other outfits in case you need to return them.
- Install the car seat. To bring your baby home, you’ll need an up-to-date infant car seat. Check if it’s installed correctly with a trained technician, and ask for tips if you need help figuring out that weird buckle. (We’ve all been there.)
After you hit 36 weeks, you’ll see your doctor every week until you give birth. Each appointment will include routine checks of your baby’s position, you and your baby’s vitals, and of course, your pee. (You know the drill by now.)
This month, your doctor will also check you for group B strep (GBS). GBS is a type of bacteria that some pregnant people have. It can harm your baby, so if you test positive for it, you’ll need antibiotics when you’re in labor.
GBS is a type of bacteria that some pregnant people have. It can harm your baby, so if you test positive for it, you’ll need antibiotics when you’re in labor.
You should notify your doctor or head to the hospital if you have these symptoms:
- contractions lasting 1 minute long that are 5 minutes apart for at least 1 hour
- a gush of fluids (your water breaks)
- any vaginal bleeding
- severe abdominal pain
- a decrease in fetal movement
- constant, dull back pain before you’re 37 weeks
What to do if you don’t have a doctor
Free birthing or birthing without support isn’t medically recommended.
If you haven’t found an OB-GYN or midwife yet, there’s still time, even at 9 months pregnant! You can also change medical professionals if you decide that yours isn’t the right fit. Ask friends or a local doula for a referral.
If you go into labor without a doctor, head to a local general hospital. If you can’t get to the hospital, call 911 as soon as possible.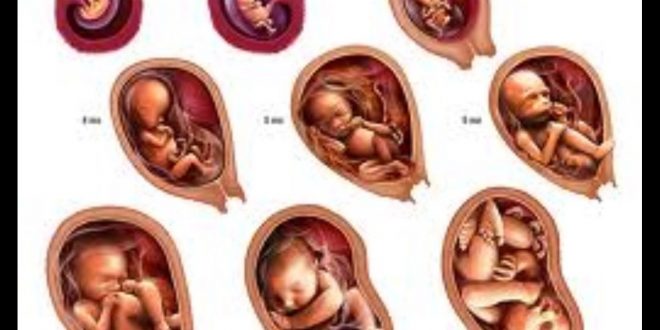
Whether you’re counting down the days until you get to meet your little one or wishing you could freeze time, your baby is officially coming soon. In other words, you won’t be pregnant forever, promise.
Try to use this time to finish up any last-minute prep you need to do, keep a close eye out for any signs of labor, and be sure to sneak in some self-care before the big day. Foot massage, anyone?
Belly, Symptoms, Baby’s Development, More
By now, at 9 months pregnant, you’ve been anticipating the birth of your little one for what feels like forever. (Remember when you wondered if your bump could possibly get any bigger? That was adorable.)
You’ve read all the pregnancy books, taken the birthing classes, and likely oohed and awed over tiny baby clothes at your baby shower — virtual option included, of course. And while anticipating your baby’s arrival has been fun, you’re probably ready to get this show on the road.
Here’s what to expect at 9 months pregnant — from how you can tell if labor is starting to when it’s time to head to the hospital. (Finally!)
(Finally!)
The main symptom you may notice at this stage in pregnancy is called “Get-this-baby-out-of-me-itis.” Rest assured, it’s completely normal.
You’re probably feeling more than a little uncomfortable as your baby reaches full-term — on average, around 7 pounds 6 ounces for boys and 7 pounds 2 ounces for girls — so your discomfort is for good reason.
Along with that sizeable baby and your body preparing for birth, here’s what may be in store for you this month:
- back pain, thanks to the constant work required to keep you from toppling over frontward
- pelvic pressure, as baby’s head moves lower and grows bigger
- lightening, when the baby drops into the birth canal and you may be able to breathe easier (but you’ll probably feel more discomfort with the baby in a lower position)
- interrupted sleep, as those once-fluttering kicks become quite forceful
- exhaustion, because, well, you’ve been growing a human (or two) for 9 months
- constipation, as the baby grows and interferes with traffic flow
- frequent urination, due to pregnancy hormones and your baby literally tap-dancing on your bladder
- changes in appetite, but it’s different for everyone — you could feel hungrier or experience a decreased appetite, thanks to the cramped abdominal real estate
You may also have:
- Braxton-Hicks contractions
- nesting instincts
- increased vaginal discharge
During your last weeks of pregnancy, your baby goes through a lot of growth, which means that you will, too.
Depending on your body mass index before becoming pregnant, and if you’re pregnant with one baby or twins, you may gain approximately 1 to 2 pounds per week during the third trimester. (This may slow in the final weeks before giving birth.)
While it can be tempting to compare, everyone’s baby bumps look different. Your height and abdominal muscle strength make a big difference in how your body carries your baby.
If you’re taller, you may tend to carry your baby more in front, and if you have more toned abdominal muscles, you may carry higher.
If you have any concerns about your weight gain or the size of your pregnant belly, let your doctor know. They may request an ultrasound if your measurements aren’t what they expect.
Since last month, your baby has most likely packed on 1 to 2 extra pounds and 1 to 2.5 inches.
In addition to rocking an impressive growth spurt, your baby experiences significant development during the ninth month of pregnancy.
For instance, baby’s lungs are maturing to breathe outside of the womb, their reflexes are more coordinated, and they can blink, turn their head, and grasp.
Because babies are still developing every day in the womb, it’s important to avoid induction before 39 weeks unless medically indicated. (You’re considered full-term at 37 weeks, but most doctors recommend avoiding elective C-section or induction until 39 weeks, unless there’s a medical reason.)
As you near the end of your pregnancy, your baby will start to settle lower in the abdomen. Your baby’s position should also change to head down to prepare for delivery. (Most babies turn head down by week 36 of pregnancy.)
If your baby hasn’t flipped yet, your doctor will discuss any next steps with you. They may recommend some methods to help turn your baby — or a C-section may be recommended for babies that insist on staying breech.
It may seem like your baby is moving less during this time due to the tighter space. Your doctor may ask that you keep a kick count to keep track of fetal movements. If you notice any decrease in your baby’s movements, or have any concerns about your baby’s activity, be sure to contact your doctor.
If you’re expecting twins, there’s a good chance that you’ll be meeting them this month. A majority of twins are born before 37 weeks and some even before 34 weeks.
And although there’s a good chance your twins will be on the smaller side — most twins weigh less than 6 pounds — babies born between 34 and 36 weeks have a near 100 percent chance of survival.
And if your babies do require any care after birth, your medical team will be prepped and ready as they welcome them into the world.
As your due date approaches, you may find yourself slowing down activity-wise, and that’s completely OK. Every pregnant person is different.
Some may stay active right up until their due date, while others may need to kick back and put their feet up more often. Listen to your own body and rest when you need to.
The good news is there’s no reason to slow down your activities unless your doctor has told you otherwise. You can maintain your normal exercise routine — although now isn’t the time to take up anything new, like CrossFit or rock climbing — and modify exercises as needed.
If you’re still feeling frisky, you can still engage in sexual activity unless your doctor has told you otherwise. In fact, sex might help speed up labor if you’re full-term. Sperm in the vagina could help the cervix ripen, and orgasms may help get contractions going.
On the other hand, if you’re at high risk for preterm labor, your doctor may ask you to refrain from sexual activity. Also, keep in mind that if your water does happen to break, you’ll want to avoid any sexual activity after that, as it could pose a risk of infection.
The big day is coming, so make sure you’re ready by checking these pre-baby items off your list:
- Finish up any prep classes you might need. You’ve probably already finished your childbirth classes (and if you haven’t, it’s not too late!), but you could also take an infant CPR class, lactation class, or baby care course.
- Take a hospital or birth center tour. Call your birthing facility to arrange an in-person or virtual tour.
- Pack your labor and delivery bags. You don’t need a ton of stuff for baby — a take-home outfit or two will do — but you’ll want to be sure to bring:
- your insurance card
- your COVID-19 vaccination card, if you have one
- comfy clothes for you
- a pair of cheap slippers or slides, as hospital floors can be pretty gross
- some comfort items, like a favorite blanket or pillow
- phone chargers
- snacks, but keep in mind you may not be able to eat during labor
- copies of your birth plan
- Pick a pediatrician. Many pediatricians offer consults to new parents, so you can determine if they’re a good fit. You’ll visit your baby’s pediatrician a lot in the first year (and for many years after!), so it’s worth spending time finding one you connect with.
- Prep your birth team. There will most likely be restrictions on who can be in the room with you, but if you have a doula or partner, prep them about what to do when you go into labor.
- Research photographers. If you’d like any final pregnancy photos, want birth photography, or are hoping to squeeze in a newborn photoshoot, now is a great time to get this scheduled.
- Wash a few of your baby’s outfits. There’s no need to wash everything, but take advantage of your nesting instincts (if you’ve got ’em) to get a few outfits ready. Leave tags on the other outfits in case you need to return them.
- Install the car seat. To bring your baby home, you’ll need an up-to-date infant car seat. Check if it’s installed correctly with a trained technician, and ask for tips if you need help figuring out that weird buckle. (We’ve all been there.)
After you hit 36 weeks, you’ll see your doctor every week until you give birth. Each appointment will include routine checks of your baby’s position, you and your baby’s vitals, and of course, your pee. (You know the drill by now.)
This month, your doctor will also check you for group B strep (GBS). GBS is a type of bacteria that some pregnant people have. It can harm your baby, so if you test positive for it, you’ll need antibiotics when you’re in labor.
You should notify your doctor or head to the hospital if you have these symptoms:
- contractions lasting 1 minute long that are 5 minutes apart for at least 1 hour
- a gush of fluids (your water breaks)
- any vaginal bleeding
- severe abdominal pain
- a decrease in fetal movement
- constant, dull back pain before you’re 37 weeks
What to do if you don’t have a doctor
Free birthing or birthing without support isn’t medically recommended.
If you haven’t found an OB-GYN or midwife yet, there’s still time, even at 9 months pregnant! You can also change medical professionals if you decide that yours isn’t the right fit. Ask friends or a local doula for a referral.
If you go into labor without a doctor, head to a local general hospital. If you can’t get to the hospital, call 911 as soon as possible.
Whether you’re counting down the days until you get to meet your little one or wishing you could freeze time, your baby is officially coming soon. In other words, you won’t be pregnant forever, promise.
Try to use this time to finish up any last-minute prep you need to do, keep a close eye out for any signs of labor, and be sure to sneak in some self-care before the big day. Foot massage, anyone?
Fetal movement - how and when does it occur
- At what time does fetal movement begin
- Fetal movement rate
- Methods for assessing the "sufficiency" of fetal movements
- Changes in fetal activity
- Determination of the condition of the fetus
“Dear patients, we are glad to welcome you to the website of the Fetal Medicine Center – a medical center of expert level in the field of modern prenatal medicine.
We see our mission in making the expectation of a child and its birth a happy, calm and most comfortable period for every woman. By providing professional medical support, we help couples plan pregnancy, control its harmonious course, conduct expert-level prenatal diagnostics, providing comprehensive care for the health of the expectant mother and baby.”
Roza Saidovna Bataeva
Head of the Fetal Medicine Center in Moscow
From the very beginning of pregnancy, every expectant mother begins to listen carefully to the sensations inside her growing belly. Can't wait to feel your baby move. When does the fetus begin to move? At what time can a pregnant woman begin to listen carefully to herself, waiting for the first movements of her child? Should I be worried if they are not felt or the baby suddenly calmed down? And can movements carry any other information, besides communicating with mom?
At what time does the fetal movement begin
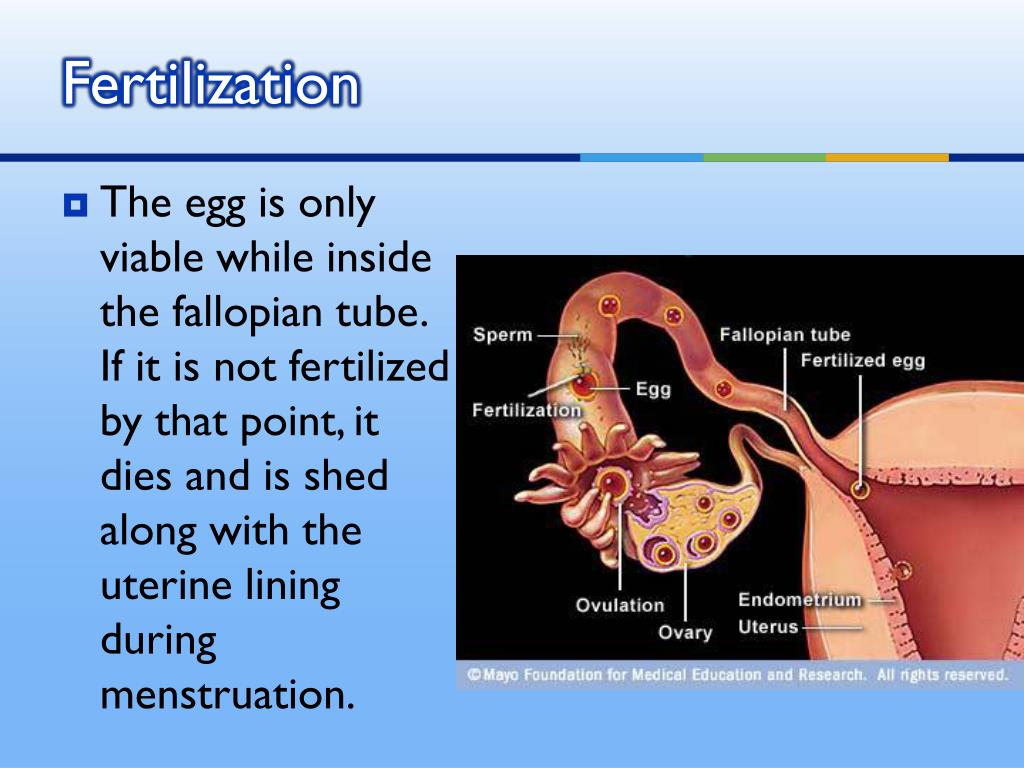
The first movements of the future baby begin early - already at 7-8 weeks of pregnancy . It was at this time that the first muscles and the rudiments of the nervous system of the fetus are formed. Naturally, at this time, the movements of the embryo are still very primitive - these are muscle contractions in response to nerve impulses.
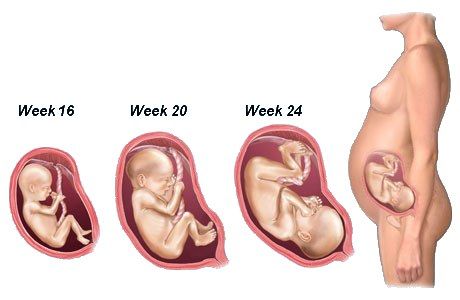
Approximately from 10 weeks of pregnancy the fetus begins to move more actively in the uterus, and, encountering an obstacle on its way (walls of the uterus), change the trajectory of movements. However, the baby is still very small and the impacts on the uterine wall are very weak, the expectant mother cannot yet feel them. At 11-12 weeks of intrauterine life, a little man already knows how to clench his fists, grimace, frown, by 16 weeks of pregnancy he begins to react to loud, sharp sounds with increased motor activity, at 17 weeks the first facial expressions appear, and at 18 weeks he covers his face with his hands and plays with the umbilical cord, compresses and unclenches the fingers of the hands.
Gradually, with increasing gestational age, movements become more coordinated and more like conscious. When the baby grows up, the pregnant woman begins to feel his movements.
When does the fetal movement begin during the first and subsequent pregnancies
It is generally accepted that during the first pregnancy, the expectant mother feels the first fetal movements at 20 weeks of pregnancy, with repeated pregnancies - at 18 weeks. This is not entirely true. A mother who is expecting her first child, indeed, most often begins to feel the movements of the fetus a little later than a multiparous woman. This is due to the fact that "experienced" mothers know how the movements of the crumbs are felt at first and what they should feel. Some primigravidas perceive the first movements of the fetus as an increase in intestinal peristalsis, “gaziki”. Many women describe the first movements of the fetus as a feeling of fluid transfusion in the abdomen, "fluttering butterflies" or "swimming fish."
The first movements are usually rare and irregular. The time of the first sensations of fetal movements naturally depends on the individual sensitivity of the woman. Some future mothers feel the first movements as early as 15-16 weeks, and someone only after 20. Slender women, as a rule, begin to feel movements earlier than full ones. Women who lead an active lifestyle, work hard, usually feel the movements of the fetus later.
By 20 weeks, due to the formation of the spinal cord and brain, as well as the accumulation of a certain amount of muscle mass in the fetus, movements become more regular and noticeable .
From 24 weeks of pregnancy, the movements of the fetus are already reminiscent of the movements of a newborn - the expectant mother feels how the fetus changes position, moves its arms and legs. The motor activity of the fetus increases gradually and its peak falls on the period from the 24th to the 32nd week of pregnancy. At this time, the activity of the baby's movements becomes one of the indicators of its normal development. After 24 weeks, the child begins to "communicate" with the mother with the help of movements, respond to the sounds of voice, music, and the emotional state of the mother. With an increase in the gestational age of more than 32 weeks, the motor activity of the fetus gradually decreases due to the fact that the baby is growing up and he simply does not have enough space for active movements. This becomes especially noticeable at the time of childbirth. By the end of the third trimester of pregnancy, the number of fetal movements may decrease somewhat, but their intensity and strength remain the same or increase.
Fetal movement rate
The baby in the mother's belly moves almost constantly. At the 20th week of pregnancy, the fetus makes about 200 movements per day, and between the 28th and 32nd weeks, the number of movements reaches 600 per day. Naturally, a pregnant woman does not feel all the movements of the fetus, but only a small part of them. So, after 28 weeks, the frequency of fetal movement, according to the sensations of a woman, is usually 4 to 8 times per hour, with the exception of periods of fetal sleep (3-4 hours in a row).
In the third trimester, a pregnant woman may notice that her baby has regular sleep and wake cycles. Children are usually most active from 19:00 to 4:00 in the morning, and the period of "rest" occurs more often from 4 to 9:00 in the morning. Of course, the movements of the fetus depend on the mood of the mother, if the mother is worried or happy, the baby can move more actively, or vice versa, calm down. The fact is that when a mother rejoices, her body significantly increases the amount of hormones of joy - endorphins, which regulate the work of the heart and blood vessels, including the vessels of the placenta. During stress or pronounced negative emotions, biologically active substances are also produced - stress hormones, they also affect the work of the heart and blood vessels. It is thanks to this biological interaction between the organisms of mother and baby that the fetus feels the state of the mother. When the expectant mother is resting, the baby usually becomes more active, if the pregnant woman is active, busy with some kind of work, the child most often calms down. The movements also change depending on the satiety of the expectant mother.
Usually the baby begins to move actively after the mother eats, especially something sweet. At the same time, the level of glucose in the blood increases sharply, which causes the fetus to be more active.
Fetal movements are the language in which the unborn child speaks to the mother. Naturally, a pregnant woman should listen to the movements, because in some cases, changes in the movements of the fetus may indicate a violation of its intrauterine state and a not entirely successful pregnancy.
If, after 20 weeks of pregnancy, the expectant mother does not feel the movement of the fetus, it may be worthwhile to see a doctor and make sure that everything is in order with the baby.
Methods for assessing the "sufficiency" of fetal movements
Counting the number of movements
The easiest way to assess fetal movements is to count the number of movements of the pregnant woman herself. Self-assessment methods are very easy to use, do not require additional equipment, the presence of a doctor and are easily reproducible by any woman. Their disadvantages are that each woman has different thresholds of susceptibility.
Count to ten
The most common method for assessing fetal movements is called count to ten . It can be carried out after 28 weeks of pregnancy, when the fetus is mature enough for active movements. Its essence lies in the fact that the expectant mother counts the movements of the fetus for a 12-hour time interval, for example, from 9 am to 9 pm. The time when a pregnant woman catches the tenth movement is recorded on a tablet. If the fetus makes less than 10 movements in 12 hours, this is a reason to consult a doctor for an additional examination.
Sadowski Method
In the evening after dinneruntil 11 p.m.), the woman lies on her left side and counts the movements of the fetus. At the same time, everything is considered, even the smallest movements. If 10 or more movements are noted within an hour, this indicates that the baby is moving quite actively and feels good. If the fetus moved less than 10 times in an hour, then the movements are counted for the next hour. Evening time for this assessment method was not chosen by chance. It is in the evening hours, especially after dinner and the associated increase in glucose, that the greatest activity of the fetus is noted. If the number of fetal movements during this test is less than 10 per two hours, this should be considered as a sign of a violation of his condition and additional studies should be carried out.
For an obstetrician-gynecologist, fetal movements are also an important diagnostic criterion for some deviations in the course of pregnancy from the norm. Too active, violent, painful fetal movement or weak, rare movements may indicate its unfavorable condition.
Changes in fetal activity
Changes in fetal activity may be associated with external influences. For example, if a pregnant woman lies on her back for a long time, then the enlarged uterus compresses a large vessel - the inferior vena cava, the blood flow to the fetus is disrupted, which immediately causes its violent reaction - active movements. The same changes in the activity of the baby can occur in any other uncomfortable position of the mother - if she leans forward, squeezing her stomach, sits with her legs crossed, the child forces her mother to change her position with her activity. A similar situation occurs if the baby himself squeezes or presses the loops of the umbilical cord, limiting the flow of blood through it. He begins to move more actively, changes his position and relieves pressure on the umbilical cord. However, in some cases, an increase or vice versa, a subsidence of fetal movements can be a sign of a serious pathology.
After 28 weeks of pregnancy, if your baby does not let you know for 3-4 hours, he may just be sleeping. In this case, the expectant mother needs to eat something sweet and lie down on her left side for half an hour. If these simple manipulations do not lead to a result, it is worth repeating them again after 2-3 hours. If this time the baby does not make itself felt, this is an occasion to consult a doctor. Rare and weak movements can also indicate a fetal problem, most often a lack of oxygen for the baby, that is, fetal hypoxia.
Determining the condition of the fetus
To determine the condition of the fetus, the doctor conducts a series of examinations:
Auscultation (listening)
The simplest is auscultation (listening) using a special wooden tube (obstetric stethoscope) or a special device that captures the fetal heartbeat, doctor listens to the baby's heartbeat. Normally, it is about 120-160 beats per minute. A decrease in heart rate less than 120 or an increase of more than 160 indicates intrauterine suffering of the child.
Ultrasound and dopplerometry
During ultrasound, the doctor visually assesses the size of the fetus, the correspondence of the development of the fetus to the gestational age, because with oxygen starvation, the growth rate of the fetus slows down and its size lags behind the norm for each period of pregnancy. Also important is the structure of the placenta, the presence of signs of aging in it, as a result of which the function of transferring blood, oxygen and nutrients to the fetus usually worsens. During ultrasound, the amount and type of amniotic fluid is assessed, which can also change with intrauterine fetal suffering. Dopplerometry of the vessels of the placenta and umbilical cord is a method for studying blood flow velocities in these vessels. With a decrease in the speed of blood flow in any vessel, one can speak of fetal malnutrition of varying severity.
Learn more about services:
- Pregnancy Ultrasound
- First Trimester Ultrasound
Cardiotocography (CTG)
CTG is performed at a gestational age of 33 weeks or more, since only in this period of intrauterine development of the baby is a full-fledged regulation of the activity of the cardiovascular system of the fetus by the centers of the spinal cord and brain. Recording of fetal heartbeats is carried out for at least 40 minutes, and if necessary, the study can be extended up to one and a half hours. The device registers and records the baby's heart rate. For example, with a decrease in the concentration of oxygen in the blood of the fetus, the supply of oxygen to the cells of the nervous system decreases, which in turn affects the heart rate, especially during the period of wakefulness of the child. The obstetrician-gynecologist evaluates the heartbeat recording curve, episodes of slowing down and a sharp increase in the fetal heart rate, and based on these data, makes a conclusion about how comfortable the baby feels in the mother's stomach.
If during additional methods for assessing the condition of the fetus, initial disturbances in the supply of oxygen to the baby are detected, drug treatment is carried out aimed at increasing the access of blood and oxygen through the placenta and mandatory control examinations against the background of ongoing therapy. If the changes are profound and the baby experiences a pronounced deficiency of oxygen and nutrients, his condition suffers, an emergency delivery of such a patient is performed.
Fetal movements are not only an indicator of his condition, it is a way of communication between the baby and parents. The movements of the crumbs in the mother's tummy are unforgettable sensations that a woman can experience only in this short, but such a happy period of her life.
Center for Fetal Medicine in Moscow:
The main activities of our center are the early detection of congenital malformations in the fetus, prenatal screening for the detection of chromosomal abnormalities in the fetus, as well as pregnancy complications such as preeclampsia, fetal growth retardation and threatened abortion.
Our center is organized in such a way that the whole range of services is concentrated in one place, where a woman receives the results of various types of examinations, including ultrasound, biochemical, and specialist consultation within 1-1. 5 hours. In the presence of a high risk for chromosomal diseases in the fetus, invasive diagnostics and genetics consultation are carried out here in the center.
Fetal echocardiography is given special attention in our center, since congenital heart defects in the fetus are increasingly common today, but, unfortunately, are often missed during ultrasound during pregnancy.
In view of the ever-increasing number of multiple pregnancies, which requires more time and a special approach, the observation of women with multiple pregnancies has been allocated to us in a separate clinic for multiple pregnancies.
All examinations in the center are carried out according to the international standards FMF (Fetal Medicine Foundation) and ISUOG (International Society for Ultrasound in Obstetrics and Gynecology). In complex clinical cases, we can consult with specialists from King's College Hospital, King's College Hospital (London, UK).
The team is a special pride of the center. Our doctors are not only one of the leading specialists, professors, doctors and candidates of medical sciences, doctors of the highest categories, they are also a team of like-minded people and real enthusiasts in their field. All ultrasound diagnostic doctors in our center have international FMF certificates. Having extensive experience in prenatal diagnostics, we share our knowledge with our colleagues by conducting training courses.
The Center is equipped with the most modern diagnostic equipment: these are the latest generation ultrasound machines, GE Voluson E8 Expert, with a complete set of modern technologies, including three-dimensional ones, this is a biochemical analyzer, Delfia Xpress, these are workplaces with professional computer programs.
Fetal movements during pregnancy
Fetal movements are expected by pregnant women and obstetrician-gynecologists. This is a very important sign that allows you to judge that the pregnancy is going well, and the child is developing successfully. Also, the baby communicates with the mother with the help of movements and can tell her about any inconvenience, so you need to listen to the movements of the fetus.
When fetal movements appear
- The first fetal movements appear at the seventh or eighth week of pregnancy. However, the small fetus does not come into contact with the walls of the uterus, so the mother does not feel its movements.
- Closer to the seventeenth week, the fetus begins to react to loud sound and light, from the eighteenth it begins to consciously move.
- A woman begins to feel movements during her first pregnancy from the twentieth week. In subsequent pregnancies, these sensations occur two to three weeks earlier. Also, a woman will feel the first movement of the fetus earlier if she is slim and leads an active lifestyle.
- From the twenty-eighth week, especially active movements are observed. The child "communicates" with the mother, reacts to her emotions.
This continues until the thirty-second week, when the baby grows so much that it can no longer actively move in the uterus.
Fetal movement - as normal
Except for three to four hours a day when the baby sleeps, he is in constant motion. In the twentieth week, the fetus makes two hundred perturbations a day, from the twenty-eighth to the thirty-second, their number increases to six hundred. Then, the activity decreases again.
Fetal activity may vary depending on the following factors:
- Time of day . Usually the fetus moves more actively in the evening and at night.
- Mother's emotions . If a pregnant woman is under stress, then the child is frightened, may freeze and stop moving, or, conversely, react to adrenaline with active movements.
- Physical activity . During physical activity, the child is usually more calm than at rest. If the mother is in an uncomfortable position for a long time, the fetus may react with strong painful shocks.
- Pregnant diet . If the mother feels hungry, the child begins to move more actively. Also pushing and touching become stronger after eating. Especially if mom eats sweets.
- Environment a. The fetus reacts to loud sounds, sudden switching on of light. He may freeze in fear, or vice versa, begin to move more actively.
Why and how to count fetal movements
Changes in the motor activity of the fetus may be a sign of pregnancy pathology. Too strong, painful, or vice versa, weakened movements signal that the child does not have enough oxygen. This condition is called fetal hypoxia. In addition, sensations change when the amount of amniotic fluid changes. Therefore, it is important to count fetal movements, especially during the first pregnancy.
There are three methods for counting fetal movements:
- Pearson method . Movements are considered from nine in the morning to nine in the evening, during which physical activity is limited.