What causes a fallopian tube to rupture
Infertility Problems With the Fallopian Tubes and Abnormalities in the Pelvis - Women's Health Issues
By
Robert W. Rebar
, MD, Western Michigan University Homer Stryker M.D. School of Medicine
Medically Reviewed Oct 2022
VIEW PROFESSIONAL VERSION
Topic Resources
If a fallopian tube is blocked or damaged, women may have fertility problems. A blocked or damaged fallopian tube can prevent the sperm from reaching the egg or prevent the egg or fertilized egg (zygote) from moving from the ovary to the uterus to be implanted. Abnormalities in the uterus or pelvis can prevent the egg from attaching to (implanting in) the lining of the uterus and can block the fallopian tubes.
To identify the problem, doctors may take x-rays as a radiopaque contrast agent is injected through the cervix (hysterosalpingography), do ultrasonography after a salt solution is injected inside the uterus (sonohysterography), or view the organs through a viewing tube (laparoscope) inserted through an incision just below the navel.
Treatment depends on the type and location of the abnormality (fallopian tubes or uterus) and the age of the woman, but in vitro fertilization or, in younger women, surgery may be recommended.
(See also Overview of Infertility Overview of Infertility Infertility is usually defined as the inability to achieve a pregnancy after 1 year of regular sexual intercourse without birth control. Frequent intercourse without birth control usually results... read more .)
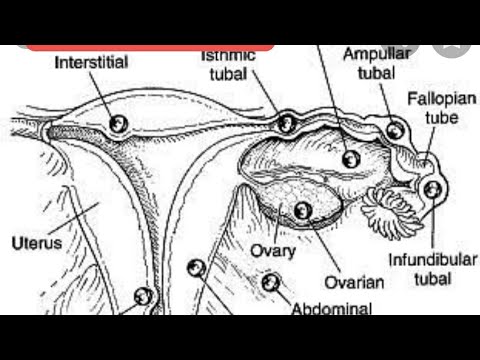
Locating the Female Reproductive Organs
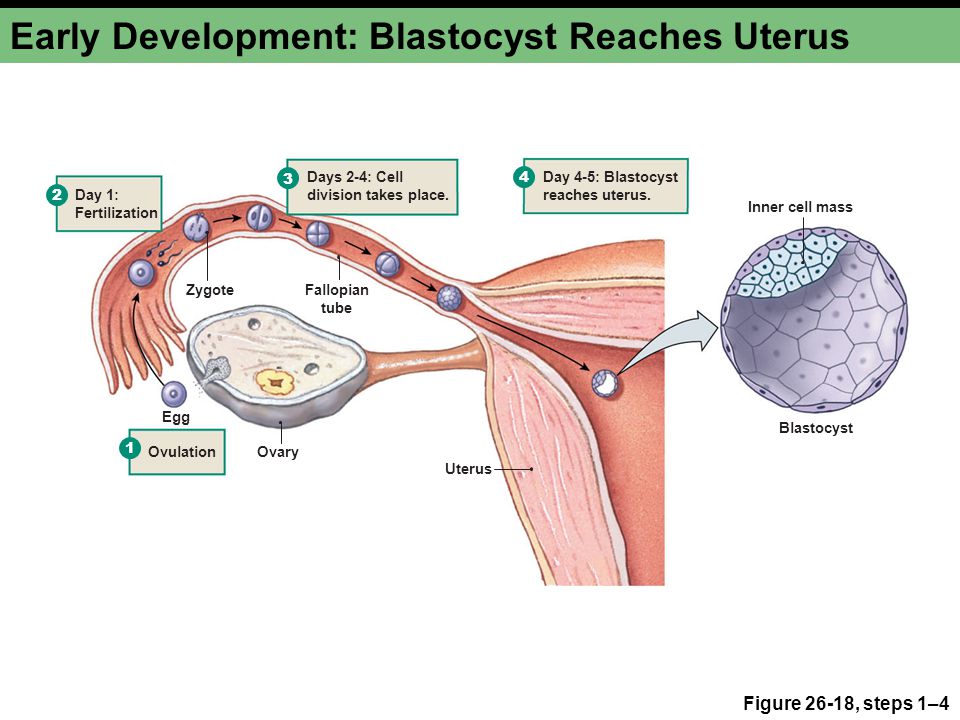
Ovulation and Implantation
Fallopian tube problems result from conditions that block or damage the tube, including the following:
Pelvic infections (such as pelvic inflammatory disease Pelvic Inflammatory Disease (PID) Pelvic inflammatory disease is an infection of the upper female reproductive organs (the cervix, uterus, fallopian tubes, and ovaries).
 Pelvic inflammatory disease is usually transmitted during... read more )
Pelvic inflammatory disease is usually transmitted during... read more )A past pregnancy in the fallopian tubes (ectopic pregnancy Ectopic Pregnancy Ectopic pregnancy is attachment (implantation) of a fertilized egg in an abnormal location, such as the fallopian tubes. In an ectopic pregnancy, the fetus cannot survive. When an ectopic pregnancy... read more )
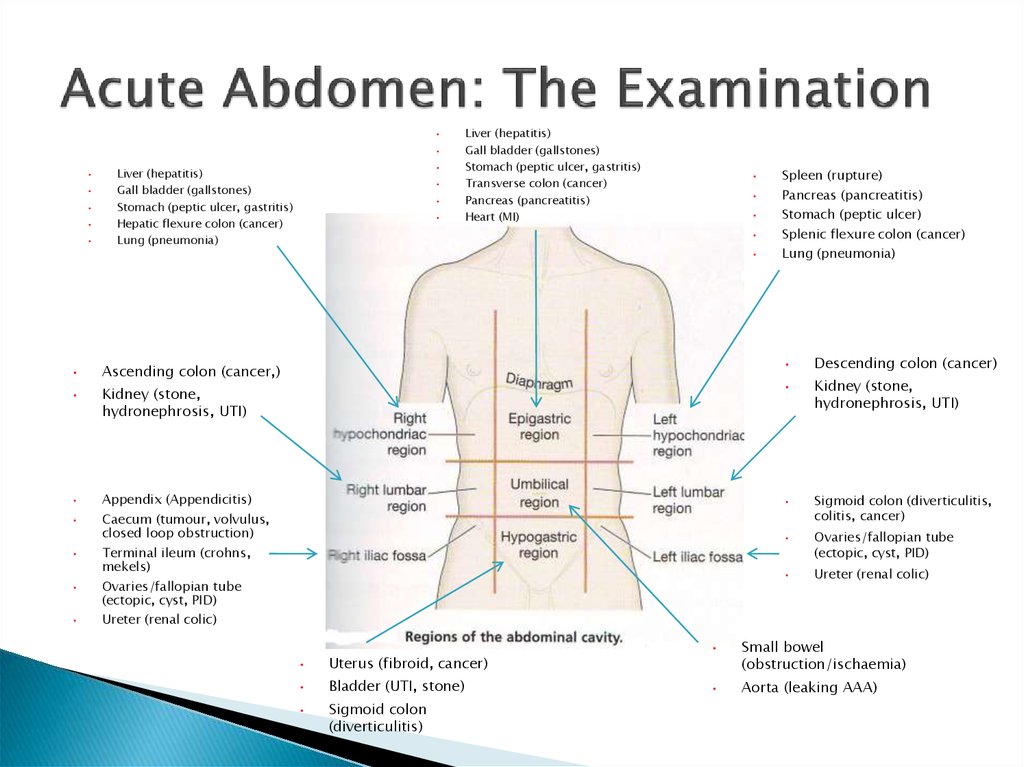
A ruptured appendix Appendicitis Appendicitis is inflammation and infection of the appendix. Often a blockage inside the appendix causes the appendix to become inflamed and infected. Abdominal pain, nausea, and fever are common... read more
Surgery in the pelvis or lower abdomen
Inflammation that damages the uterus and fallopian tubes (such as that caused by tuberculosis Extrapulmonary tuberculosis or inflammatory bowel disease Overview of Inflammatory Bowel Disease (IBD) In inflammatory bowel diseases, the intestine (bowel) becomes inflamed, often causing recurring abdominal pain and diarrhea.
 The two primary types of inflammatory bowel disease (IBD) are Crohn... read more )
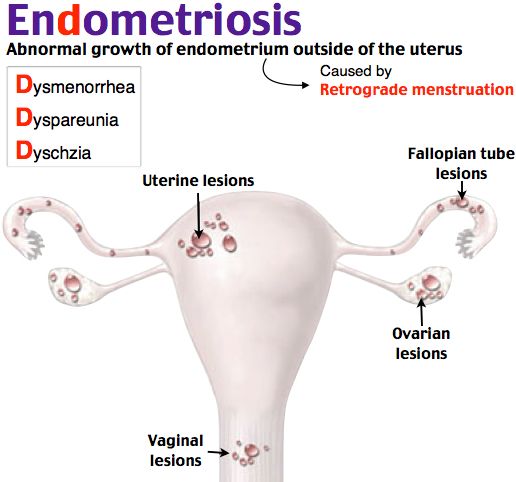
The two primary types of inflammatory bowel disease (IBD) are Crohn... read more )Endometriosis Endometriosis In endometriosis, patches of endometrial tissue—normally occurring only in the lining of the uterus (endometrium)—appear outside the uterus. Why endometrial tissue appears outside the uterus... read more
Bacteria, such as those that can cause pelvic inflammatory disease, can enter the vagina during sexual activity with a partner who has a sexually transmitted infection Overview of Sexually Transmitted Infections (STIs) Sexually transmitted (venereal) diseases are infections that are typically, but not exclusively, passed from person to person through sexual contact. Sexually transmitted infections may be caused... read more , such as gonorrhea. The bacteria can spread from the vagina to infect the cervix. They may then spread upward, to the uterus and sometimes the fallopian tubes. Some bacteria such as chlamydiae Chlamydial and Other Nongonococcal Infections Chlamydial infections include sexually transmitted infections of the urethra, cervix, and rectum that are caused by the bacteria Chlamydia trachomatis.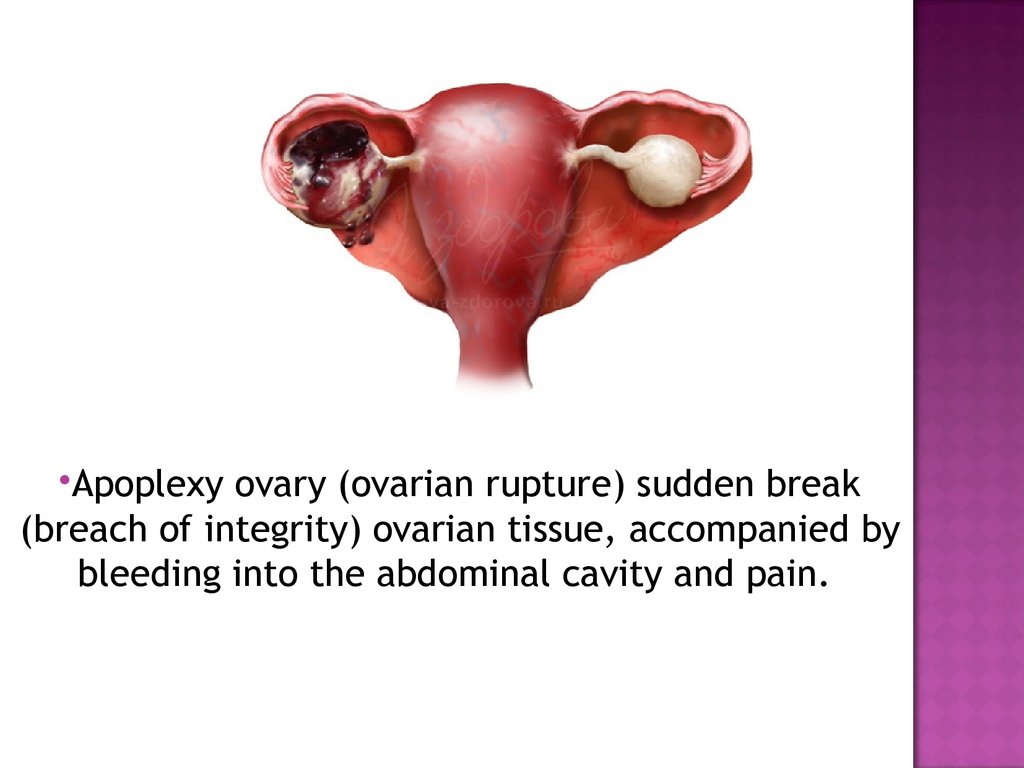 These bacteria can also infect... read more can infect the fallopian tubes without causing any symptoms. These infections may permanently damage the fallopian tubes. Scar tissue may form and block the fallopian tubes.
These bacteria can also infect... read more can infect the fallopian tubes without causing any symptoms. These infections may permanently damage the fallopian tubes. Scar tissue may form and block the fallopian tubes.
Abnormalities in the pelvis can block the tubes or prevent the egg from implanting in the uterus. They include the following:
Birth defects of the uterus and fallopian tubes
Endometriosis Endometriosis In endometriosis, patches of endometrial tissue—normally occurring only in the lining of the uterus (endometrium)—appear outside the uterus. Why endometrial tissue appears outside the uterus... read more
Fibroids Fibroids A fibroid is a noncancerous tumor composed of muscle and fibrous tissue. It is located in the uterus. Fibroids can cause pain, abnormal vaginal bleeding, constipation, repeated miscarriages... read more or polyps Polyps of the Cervix Cervical polyps are common fingerlike growths of tissue that protrude into the passageway through the cervix.
 Polyps are almost always benign (noncancerous). Cervical polyps may be caused by... read more in the uterus
Polyps are almost always benign (noncancerous). Cervical polyps may be caused by... read more in the uterusBands of scar tissue (adhesions) that form between normally unconnected structures in the uterus or pelvis
Adhesions in the uterus are usually caused by infections or an injury during surgery, usually dilation and curettage Dilation and Curettage Sometimes doctors recommend screening tests, which are tests that are done to look for disorders in people who have no symptoms. If women have symptoms related to the reproductive system (gynecologic... read more (D and C). This disorder is called Asherman syndrome.
Sometimes tests for pelvic infection
Hysterosalpingography or sonohysterography
Hysteroscopy to further evaluate abnormalities
Rarely, laparoscopy
If pelvic infection is suspected, tests to check for gonorrhea or chlamydial infection are done.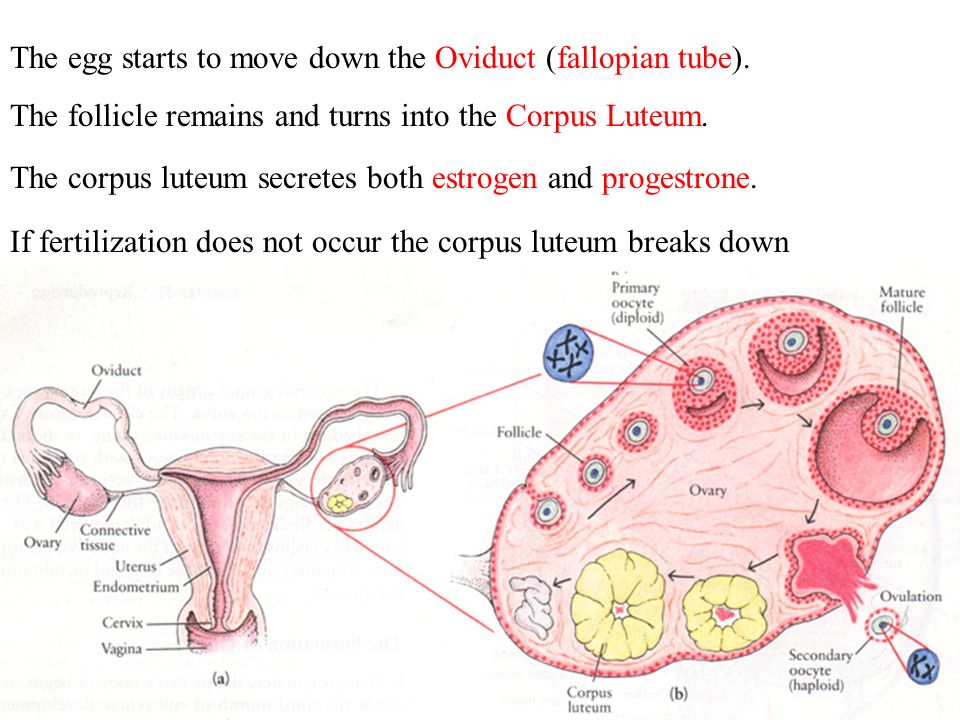 Screening for sexually transmitted infections is a usual part of routine care when women are trying to become pregnant.
Screening for sexually transmitted infections is a usual part of routine care when women are trying to become pregnant.
Procedures are done to determine whether the fallopian tubes are blocked. They include hysterosalpingography, sonohysterography, laparoscopy, and hysteroscopy. During laparoscopy and hysteroscopy, diagnosis and treatment are often done at the same time.
Hysterosalpingography Hysterosalpingography Sometimes doctors recommend screening tests, which are tests that are done to look for disorders in people who have no symptoms. If women have symptoms related to the reproductive system (gynecologic... read more is most commonly used to check for problems with the fallopian tubes.
X-rays are taken as a radiopaque contrast agent is injected through the cervix. The contrast agent outlines the interior of the uterus and fallopian tubes. This procedure is done a few days after a woman’s menstrual period ends and before ovulation occurs. Hysterosalpingography does not require an anesthetic.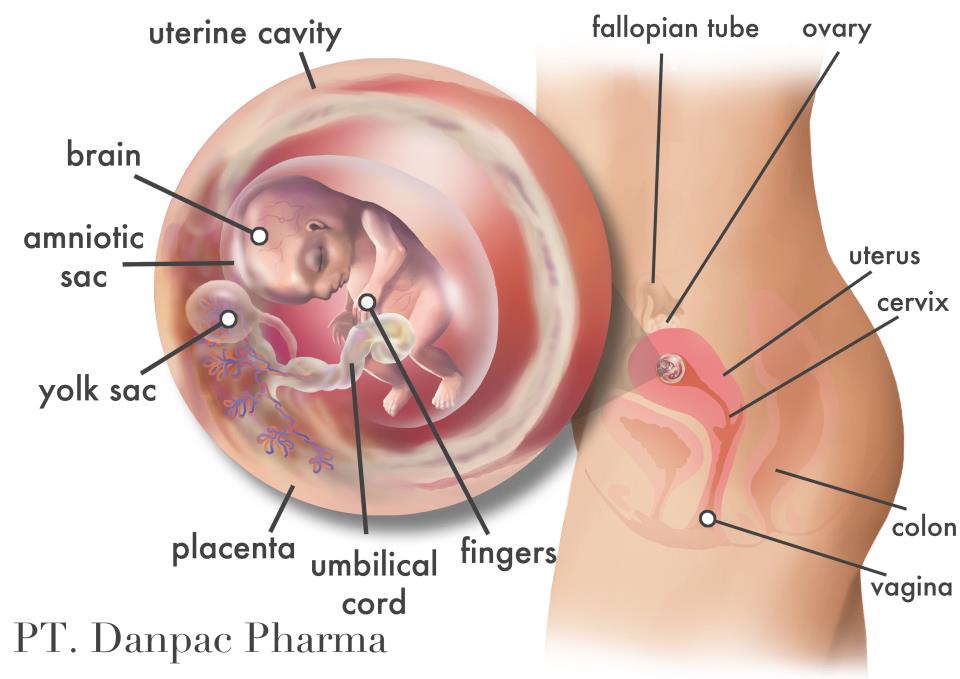
Hysterosalpingography can detect some structural disorders that can block the fallopian tubes. However, in about 15% of cases, hysterosalpingography indicates that the fallopian tubes are blocked when they are not—called a false-positive result.
After hysterosalpingography, fertility in young women appears to be slightly improved if the results are normal, possibly because the procedure temporarily widens (dilates) the tubes or clears the tubes of mucus and debris. Doctors may wait to see if young women become pregnant after this procedure before additional tests of fallopian tube function are done.
Sonohysterography Saline Sonography Sometimes doctors recommend screening tests, which are tests that are done to look for disorders in people who have no symptoms. If women have symptoms related to the reproductive system (gynecologic... read more is sometimes used to detect and/or to further evaluate problems with the fallopian tubes and other abnormalities in the pelvis.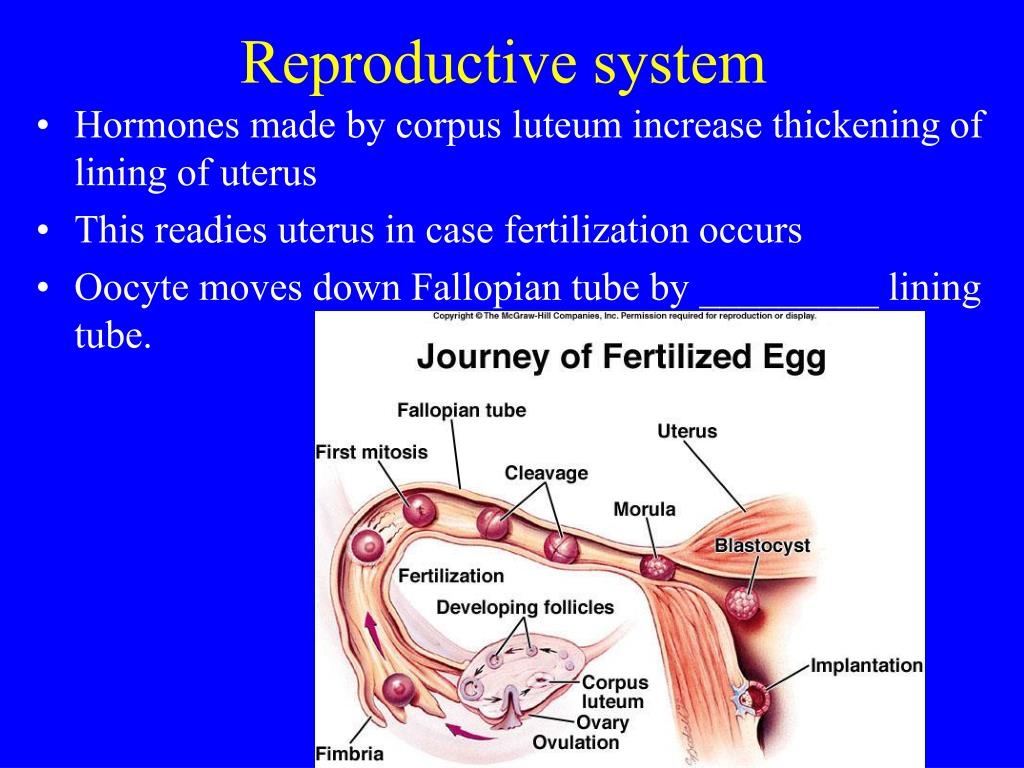
A salt (saline) solution is injected into the interior of the uterus through the cervix during ultrasonography so that the interior is distended and abnormalities can be seen more easily. If the solution flows into the fallopian tubes, the tubes are not blocked.
Sonohysterography is quick and does not require an anesthetic. It is considered safer than hysterosalpingography because it does not require radiation or injection of a contrast agent. However, its accuracy depends on the skill of the practitioner doing the test.
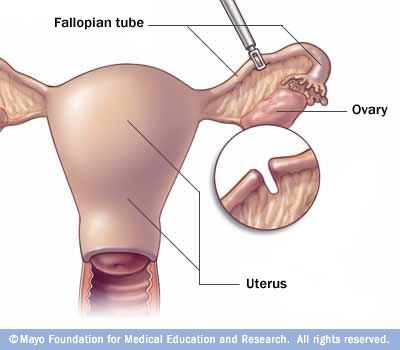
If evidence suggests that the fallopian tubes are blocked or that a woman may have endometriosis, a small viewing tube called a laparoscope Laparoscopy Sometimes doctors recommend screening tests, which are tests that are done to look for disorders in people who have no symptoms. If women have symptoms related to the reproductive system (gynecologic... read more is inserted in the pelvic cavity through a small incision just below the navel.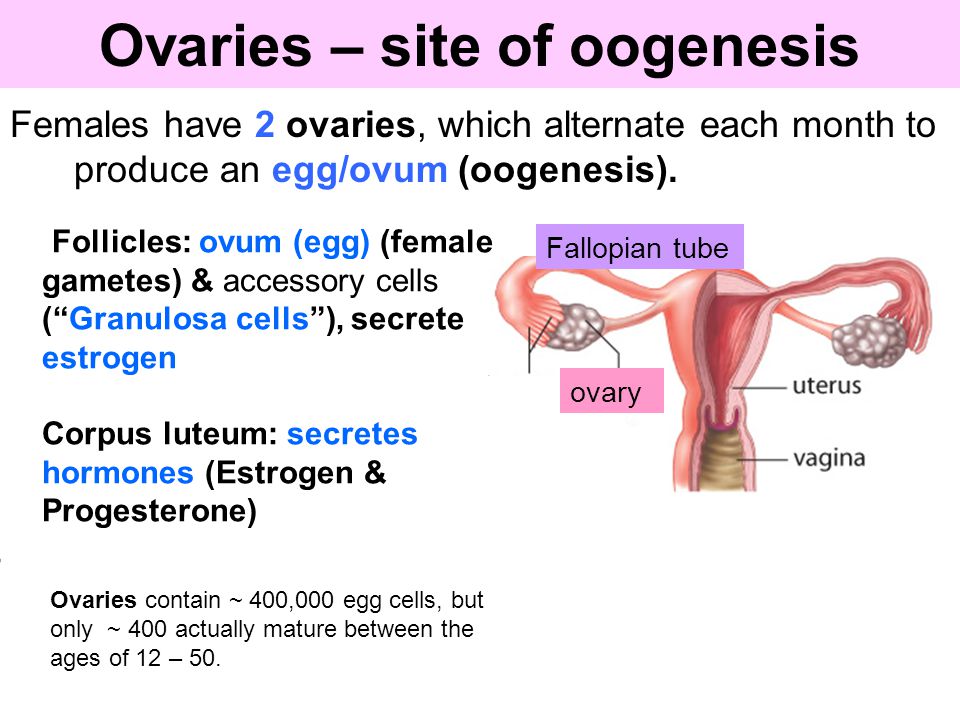 Usually, a general anesthetic is used. Laparoscopy enables doctors to directly view the uterus, fallopian tubes, and ovaries. However, this procedure is rarely done.
Usually, a general anesthetic is used. Laparoscopy enables doctors to directly view the uterus, fallopian tubes, and ovaries. However, this procedure is rarely done.
Instruments inserted through the laparoscope may also be used to dislodge or remove abnormal tissue in the pelvis.
If an abnormality within the uterus is detected, doctors examine the uterus with a viewing tube called a hysteroscope Hysteroscopy Sometimes doctors recommend screening tests, which are tests that are done to look for disorders in people who have no symptoms. If women have symptoms related to the reproductive system (gynecologic... read more , which is inserted through the vagina and cervix into the uterus. If adhesions, a polyp, or a small fibroid is detected, instruments inserted through the hysteroscope may be used to dislodge or remove the abnormal tissue, increasing the chances that the woman will become pregnant.
Antibiotics, if a pelvic infection is diagnosed
Laparoscopy and/or hysteroscopy to dislodge or remove any abnormal tissue
In vitro fertilization or, in younger women, sometimes surgery
If pelvic infection is diagnosed, it is treated with antibiotics.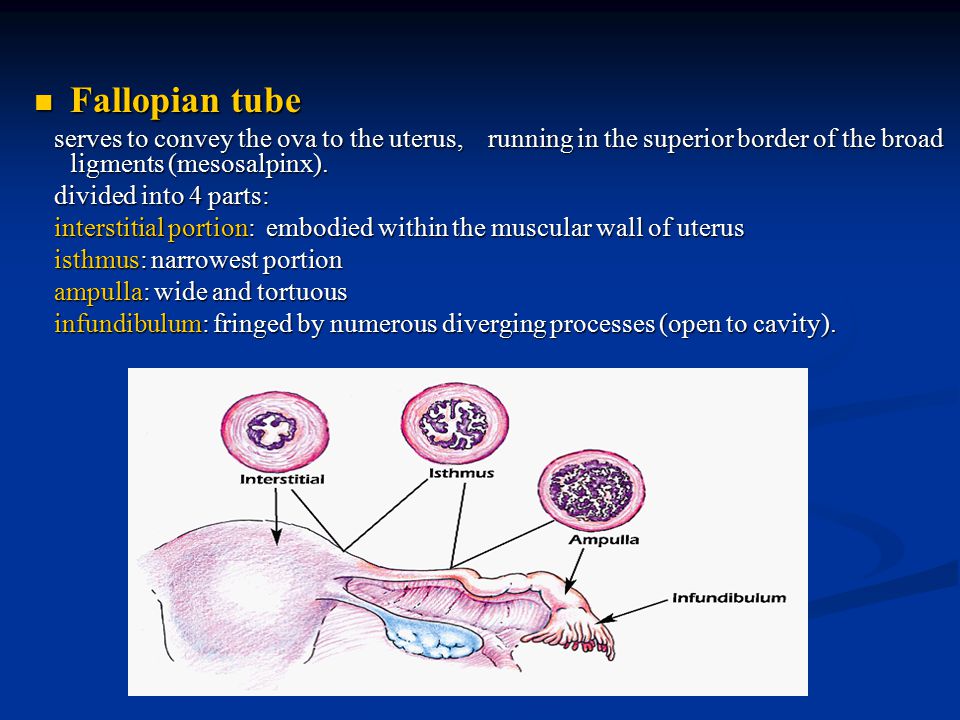
Treatment of fallopian tube or pelvic problems depends on the cause. Abnormal tissue is sometimes dislodged or removed during diagnosis (during hysteroscopy or laparoscopy). The pregnancy rate after one of these procedures is
Surgery can be done to repair a fallopian tube damaged by an ectopic pregnancy or an infection, especially in younger women if the problem was not severe. However, after such surgery, the chances of a normal pregnancy are small. The chances of an ectopic pregnancy are higher than usual both before and after such surgery. Consequently, in vitro fertilization In vitro (test tube) fertilization (IVF) Assisted reproductive technologies involve working with sperm and eggs or embryos in a laboratory (in vitro) with the goal of producing a pregnancy. (See also Overview of Infertility.) If treatment... read more is often recommended instead.
Assisted reproductive technologies Assisted Reproductive Technologies Assisted reproductive technologies involve working with sperm and eggs or embryos in a laboratory (in vitro) with the goal of producing a pregnancy.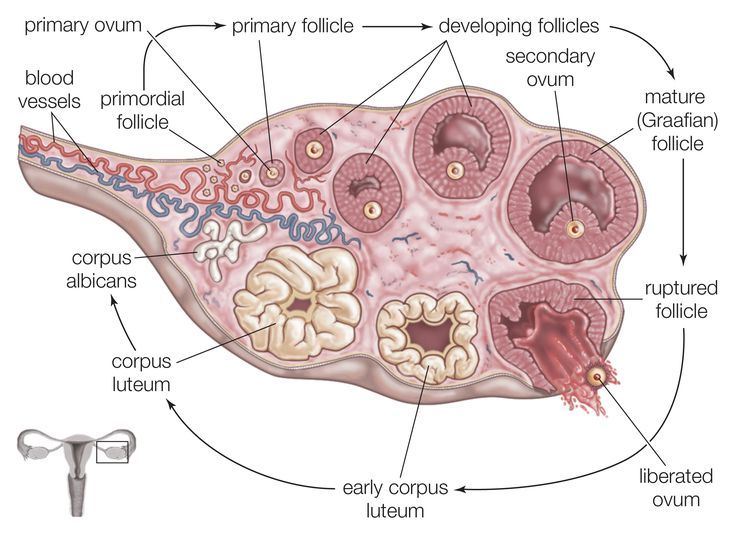 (See also Overview of Infertility.) If treatment... read more are often a necessity or an alternative, particularly in women under age 30.
(See also Overview of Infertility.) If treatment... read more are often a necessity or an alternative, particularly in women under age 30.
VIEW PROFESSIONAL VERSION
Copyright © 2022 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Test your knowledge
Take a Quiz!Ectopic (Extrauterine) Pregnancy
Series Ectopic Pregnancy
Written by Shishira Sreenivas
What Is Ectopic Pregnancy?
Usually, a fertilized egg attaches itself to the lining in your uterus. But with an ectopic pregnancy (also called extrauterine pregnancy), the fertilized egg grows outside your uterus.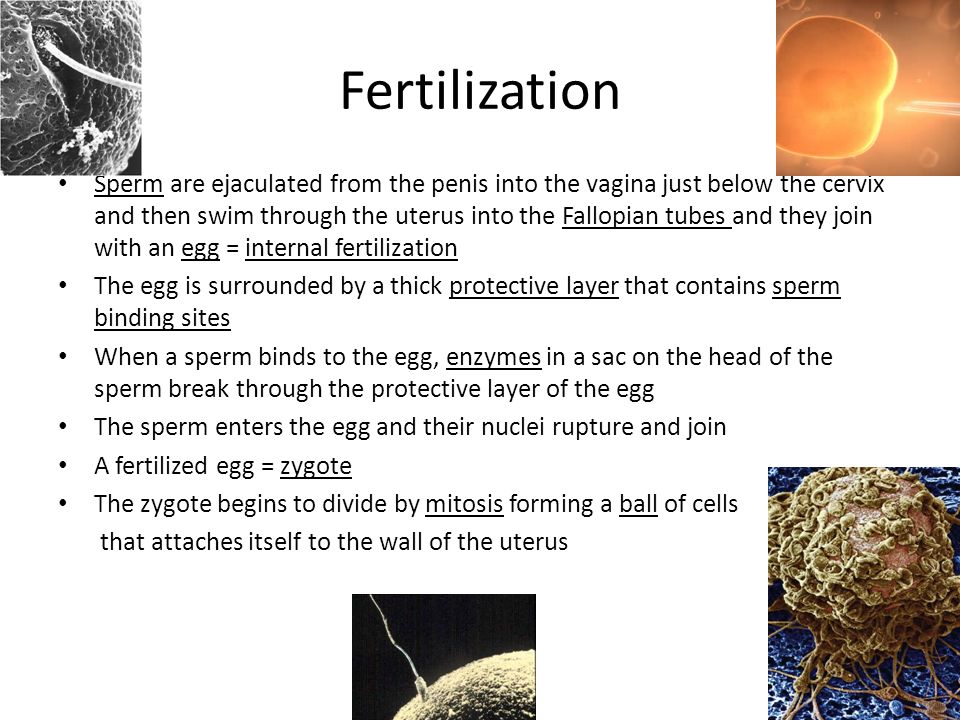 This can include other areas like a fallopian tube, the ovaries, in your belly, or the lower part of your cervix, which is above the vagina. In more than 90% of cases, the egg attaches itself in a fallopian tube. This is called a tubal pregnancy.
This can include other areas like a fallopian tube, the ovaries, in your belly, or the lower part of your cervix, which is above the vagina. In more than 90% of cases, the egg attaches itself in a fallopian tube. This is called a tubal pregnancy.
Rates are hard to determine, but one study suggests that about 1 in 50 pregnancies in the U.S. are ectopic. As the fertilized egg grows, it can burst (rupture) and can cause life-threatening bleeding. If this happens, you will need medical care right away. If you don’t treat it, it can be deadly. In fact, ectopic pregnancies are the leading cause of pregnancy-related deaths in the first trimester.
It’s important to note that the fertilized egg in an ectopic pregnancy is not “viable.” That means it’s impossible for the egg to survive and grow into a baby that can survive in or outside your body. It will always result in a pregnancy loss. That’s because the egg can’t get the blood supply and support it needs to grow outside of the uterus.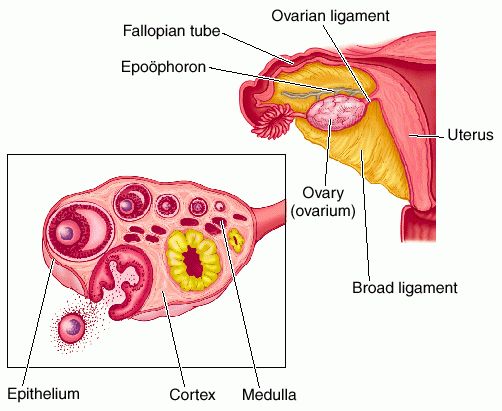
Ectopic Pregnancy Signs and Symptoms
Most of the time, an ectopic pregnancy happens within the first few weeks of pregnancy. You might not even know that you're pregnant and may not notice any problems.
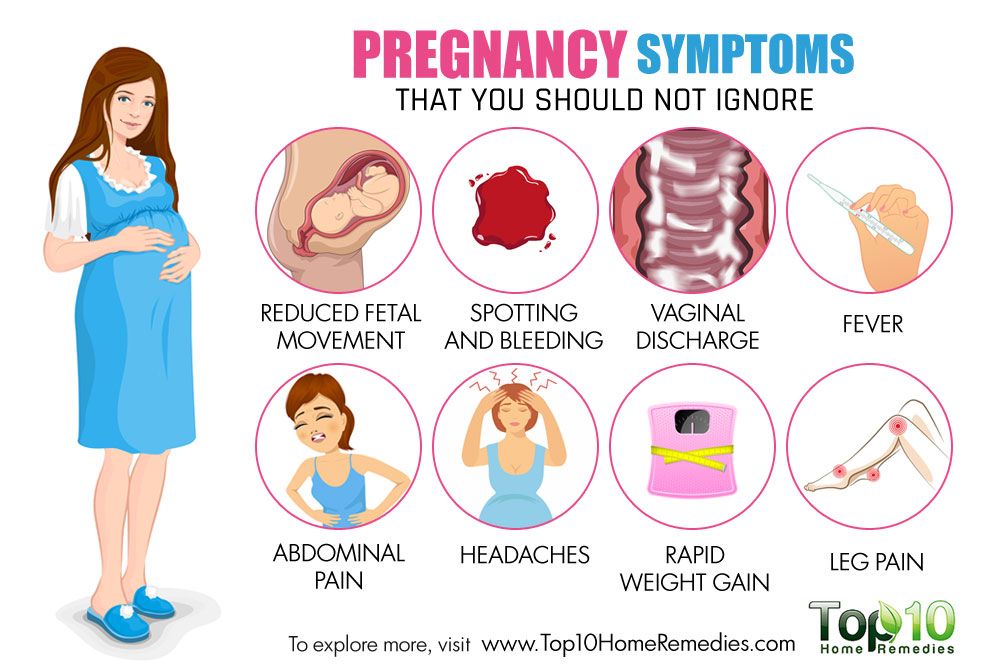
Early signs of an ectopic pregnancy include:
- Light vaginal bleeding and pelvic pain
- Upset stomach and vomiting
- Sharp abdominal cramps
- Pain on one side of your body
- Dizziness or weakness
- Pain in your shoulder, neck, or rectum
An ectopic pregnancy can cause your fallopian tube to burst or rupture. Emergency symptoms include major pain, with or without severe bleeding. Call your doctor right away if you have heavy vaginal bleeding with lightheadedness, fainting, or shoulder pain, or if you have severe belly pain, especially on one side.
You might need to call 911 or head to the nearest hospital to have it treated right away.
Ectopic Pregnancy Causes and Risk Factors
You may never know why you have an ectopic pregnancy.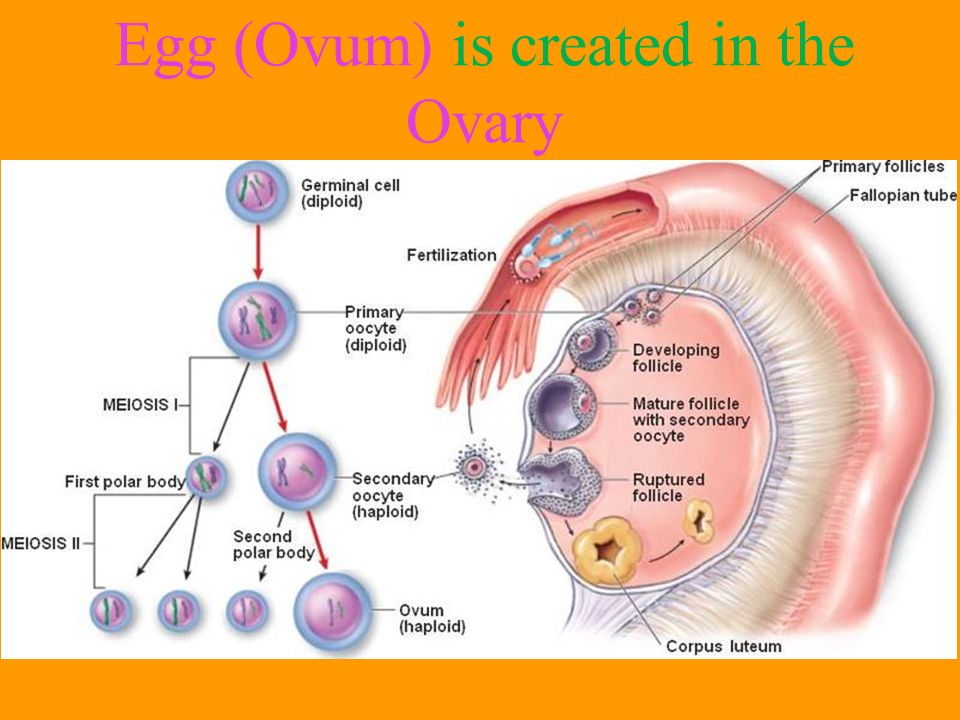 One cause could be a damaged fallopian tube. It could keep the fertilized egg from getting into your uterus.
One cause could be a damaged fallopian tube. It could keep the fertilized egg from getting into your uterus.
You’re more likely to have an ectopic pregnancy if you:
- Have pelvic inflammatory disease (PID)
- Smoke cigarettes
- Are older than 35
- Have a sexually transmitted infection
- Have scarring from pelvic surgery
- Had a previous ectopic pregnancy
- Tried to have tubal ligation (tubes tied) or tubal ligation reversal
- Use fertility drugs
- Had fertility treatments such as in vitro fertilization (IVF)
It could also happen if you become pregnant while you have an intrauterine device (IUD) for birth control.
Ectopic Pregnancy Complications
During an ectopic pregnancy, the fertilized egg is wrapped in a structure that can grow for several weeks outside your uterus. But the structure usually bursts between 6 and 16 weeks. This can cause severe bleeding. If the bleeding isn’t stopped, your body might start to shut down due to the blood loss (hemorrhagic shock), and the odds of dying from it increases.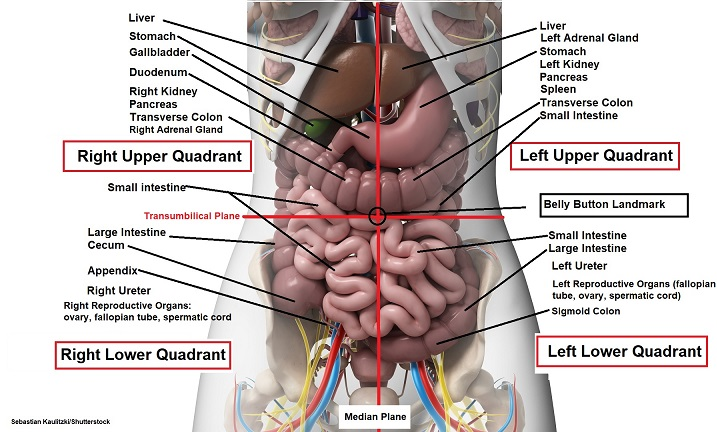 If it’s treated before it bursts, it rarely results in death.
If it’s treated before it bursts, it rarely results in death.
If the structure does burst, it may damage the fallopian tube it was attached to. Your doctor might remove the fallopian tube during the surgery. But you have two fallopian tubes. If your other fallopian tube is healthy, you should still be able to get pregnant. But if your other fallopian tube is damaged or not there, you may have fertility issues. In this case, talk to your doctor about other ways to get pregnant, like IVF (in vitro fertilization).
Ectopic Pregnancy Diagnosis
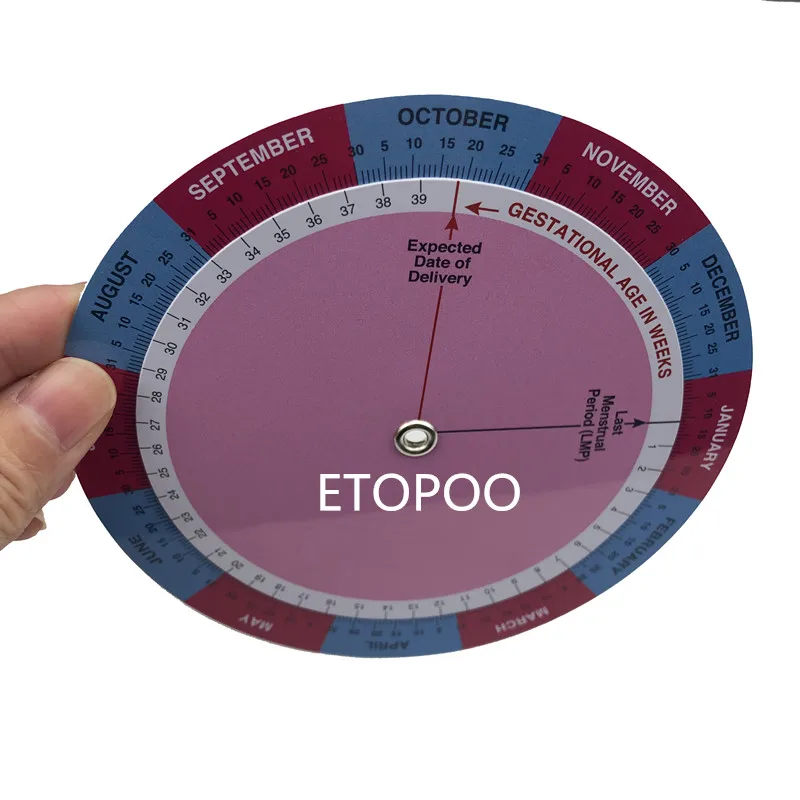
Your doctor will probably do tests that include a pregnancy test and a pelvic exam. They might give you an ultrasound to look at your uterus and fallopian tubes.
Ectopic Pregnancy Treatment
Because a fertilized egg can’t survive outside a uterus, your doctor will need to take it out, so you don’t have serious health problems. They’ll use one of two methods: medication or surgery.
Medication. If your fallopian tube hasn’t ruptured and your pregnancy isn’t far along, your doctor can give you a shot of methotrexate (Trexall).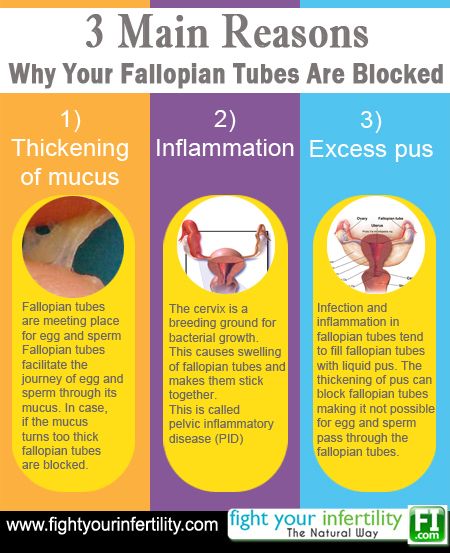 You only need one dose of the injection. It stops the fertilized egg from growing. Your body will absorb the egg in about 4-6 weeks. With this treatment, there’s no need to remove the fallopian tube.
You only need one dose of the injection. It stops the fertilized egg from growing. Your body will absorb the egg in about 4-6 weeks. With this treatment, there’s no need to remove the fallopian tube.
Before you can take methotrexate, your doctor will need to run a few blood tests to measure your hCG levels (human chorionic gonadotropin). It’s the hormone your body produces when it detects a pregnancy. You won’t be able to take methotrexate if you’re breastfeeding or have certain health problems.
Once you get the shot, the doctor will check your hCG levels during follow-up appointments. If your levels don’t drop after the first dose, you might need a second dose of the same medication. You’ll need to follow up until your blood no longer has hCG.
It’s important to note that taking methotrexate is not the same as having a medical abortion, as you could get if you had a “viable” pregnancy in which the fertilized egg attaches inside the uterus. For a medical abortion, you need a combination of two prescription drugs: mifepristone and misoprostol.
The methotrexate that you take during an ectopic pregnancy before the egg bursts is medically necessary. It can lower your risk of dying or other serious complications.
Surgery. In other cases, you’ll need surgery. The most common is laparoscopy. Your doctor will make very small cuts in your lower belly and insert a thin, flexible tube called a laparoscope to remove the ectopic pregnancy. If your fallopian tube is damaged, they may have to remove it as well. If you’re bleeding a lot or your doctor suspects that your fallopian tube is ruptured, you might need emergency surgery with a larger cut. This is called a laparotomy.
Surgery side effects can include:
- Pain
- Fatigue
- Bleeding
- Infection
Whether you take methotrexate or have surgery, you may feel tired for a few weeks and have some discomfort in your belly. You may continue to have pregnancy-like symptoms for a bit. It might take a few period cycles before you feel back to normal.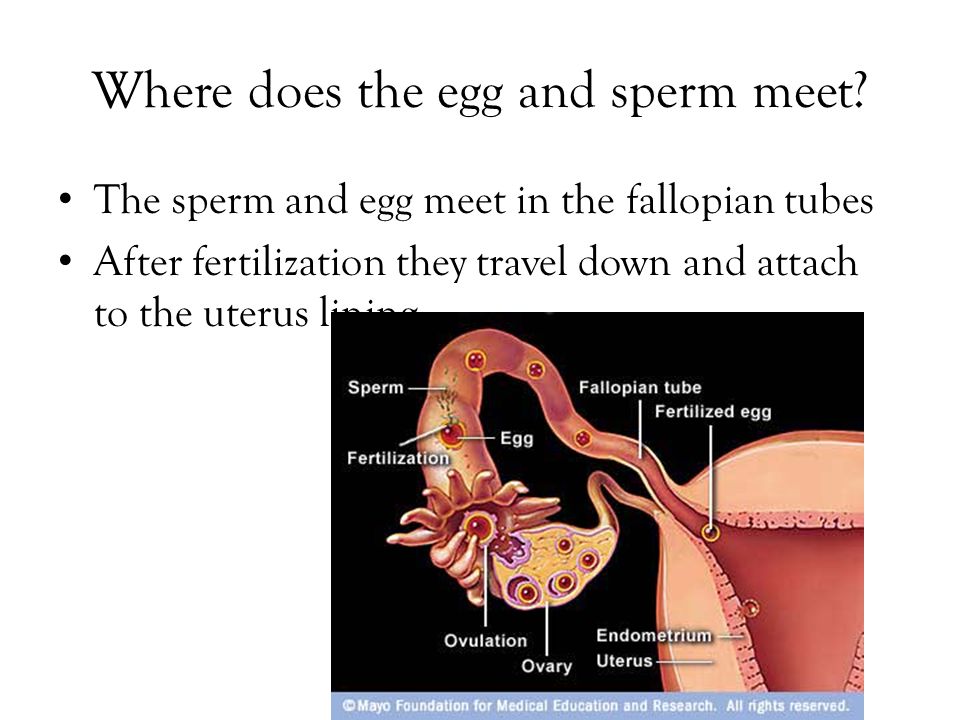
After an Ectopic Pregnancy
It might be hard for you to have a typical pregnancy afterward. Consider talking to a fertility specialist, especially if you had a fallopian tube removed.
And talk to your doctor about how long to wait before trying again. Some experts suggest giving yourself at least 3 months so your body has time to heal.
An ectopic pregnancy raises your risk of having another one. If you think you’re having another pregnancy, be mindful of the changes in your body. Check with your doctor, and they can confirm it and take the necessary steps.
An ectopic pregnancy can take a toll on your mental health, too. Don’t hesitate to reach out to mental health experts like a licensed counselor or therapist.
There’s no way to prevent an ectopic pregnancy. But you can lower your odds with certain lifestyle choices.
You can:
- Use a condom when you have sex. This can lower your risk for PID and other sexually transmitted infections (STIs)
- Quit smoking.
- Avoid using a vaginal douche. Studies show that using a douche can increase the risk of ectopic pregnancy.
Next In Ectopic Pregnancy Series:
SymptomsRemoval of the fallopian tube in the multidisciplinary clinic Miracle Doctor in Moscow
Removal of the fallopian tube is performed surgically. In some cases, one pipe is removed, sometimes both. This operation is called salpingectomy or tubectomy. It is carried out as planned or on an emergency basis in the presence of vital indications.
The fallopian tubes serve as a connecting element between the uterus, peritoneal cavity and ovaries. Their main function is to transport the egg after fertilization to the uterus. There is a fixation of the fetal egg and further development of the embryo.
Reasons for pipe removal
Serious violations, sometimes even life-threatening women, can serve as indications for the removal of the fallopian tube. If the affected organ is not removed, the embryo inside the uterus will die due to exposure to pathogenic microflora present in the appendages.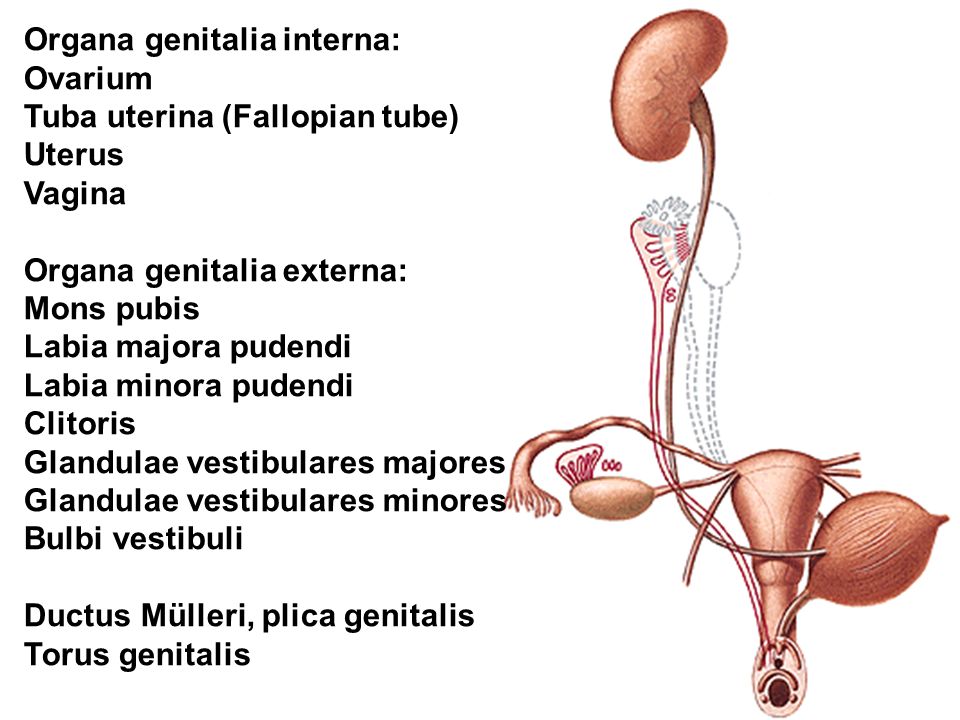 Removal is assigned:
Removal is assigned:
- in ectopic pregnancy, if the appendage is torn due to the growth of the embryo or the attachment of the fetal egg to the same tube occurs repeatedly;
- in case of growth of adhesions in the small pelvis on the tube;
- if the previous operation was unsuccessful with a bleeding complication;
- for accumulation of pus;
- in case of organ deformation due to salpingitis or adnexitis.
resection of the appendages is performed if their functionality cannot be restored. Often, such a procedure is performed before in vitro fertilization, since inflammatory exudate can enter the uterine cavity, preventing the fixation of the fetal egg. A toxic effect on the embryo is not excluded.
Types of surgery
Fallopian tubes are removed in two ways: laparoscopy and laparotomy. In the first case, minimal incisions are sufficient, the procedure is more gentle, does not injure organs and tissues.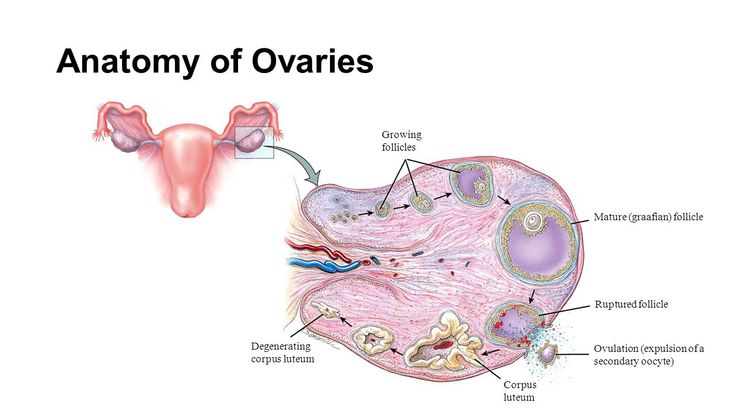 The period of recovery and rehabilitation after it is short.
The period of recovery and rehabilitation after it is short.
Laparotomy is prescribed for rupture of the tube against the background of an ectopic pregnancy. Such a process usually accompanies bleeding, hemorrhagic shock or other complications may develop. Often, only emergency surgery can save the patient's life. The operation is performed under general anesthesia in a certain sequence:
- incision above the womb or below the umbilical region;
- pumping out blood that has entered the peritoneum;
- removal of the uterus and fallopian tubes;
- identifying the source of bleeding and stopping it with clamps;
- clipping of the appendage;
- sanitation of the cavity, suturing.
Laparoscopy has several contraindications. These include peritonitis, heart attack, stroke, high degrees of obesity. Do not remove the fallopian tube in diabetes mellitus from the decompensation stage, cancerous lesions of the uterus or appendages. In all these cases, the choice is made in favor of laparotomy.
In all these cases, the choice is made in favor of laparotomy.
After laparotomy
Sometimes partial removal of the organ is possible. It is done in the presence of adhesions in a small area, benign neoplasms in one of the corners of the uterus, ectopic pregnancy at the very initial stage. If only part of the appendage was removed, it is possible to restore it. Plastic surgery is performed when the doctor considers a future pregnancy possible in a natural way. Completely removed pipes are not restored.
During the rehabilitation period, the patient is recommended antibiotic therapy to prevent the inflammatory process. Prevention of the formation of adhesions is the introduction of barrier gels into the abdominal cavity at the final stage of the operation. They provide the separation of organs for a while, and then resolve themselves.
What is tubal and peritoneal infertility and how is it treated?
Tubal-peritoneal infertility is the inability to conceive a child due to impaired patency of the fallopian tubes, when the egg formed in the ovary cannot enter the uterine cavity, where it should meet with the sperm. This type of infertility is very common, mainly due to inflammatory diseases that develop in the fallopian tubes and adjacent organs. The risk group includes women with a history of abortion or surgery on the pelvic organs.
This type of infertility is very common, mainly due to inflammatory diseases that develop in the fallopian tubes and adjacent organs. The risk group includes women with a history of abortion or surgery on the pelvic organs.
Tubal-peritoneal female infertility is not diagnosed by "ordinary" ultrasound: more sophisticated methods are needed to detect it. It is more difficult to treat this condition, the longer it exists. If the patency of the fallopian tubes cannot be restored, it is possible to conceive a child only with the help of IVF or other assisted reproductive technologies.
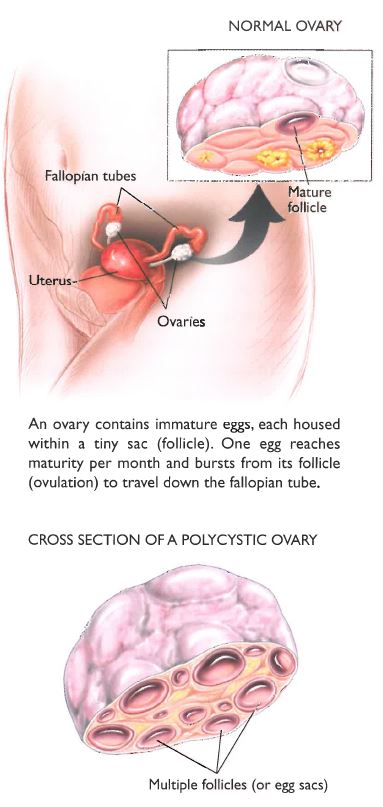
Several times a year (in young women every month) an egg matures in the ovaries. Having become completely ready for fertilization, she breaks her shell and comes out, ending up on the peritoneum (this is a thin film-shell lining the cavity of the abdomen and pelvis from the inside). The fallopian tubes end in a funnel-shaped extension, on which "villi", fimbriae, grow. These fimbriae perform special movements that are supposed to "suck" the egg into the opening of the fallopian tube.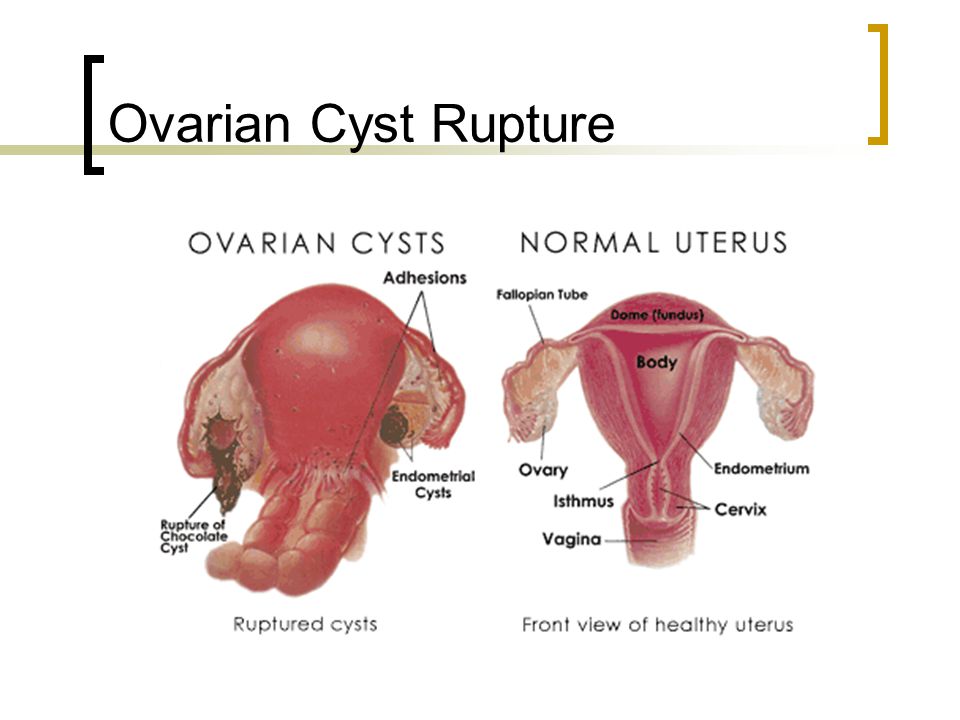
Next, the tube must contract (similar to the way the intestines do to pass food) so that the egg reaches the place where the fallopian tube enters the uterus. It is in this place that the female cell must meet the “carrier” of male information, and if there is no chemical or immunological conflict between them (when one cell considers the other an “enemy”), fertilization will occur.
If one of the mechanisms is broken, getting pregnant becomes problematic:
- tubal infertility - a condition when violations have touched the canal of the fallopian tube;
- of a peritoneal (that is, peritoneal) nature occurs when connective tissue grows between the ovary and the entrance to the tube, which prevents the egg from entering the tube cavity.
Classifications of pathology
Tubal-peritoneal infertility causes a lack of conception in 35-60% of married couples who have regular sexual life without the use of contraceptives.
Functional tubal infertility
There is no disruption in the structure of the fallopian tube, it is quite passable, but its ability to contract is impaired. This can happen in one of three types:
- hypertonicity: "tense" pipe is reduced very quickly;
- discoordination, when different parts of the "tube" are reduced in their own rhythm;
- hypotonicity: the organ is "flaccid", it contracts weakly.
Organic tubal infertility
In this case, the patency of the fallopian tubes is disturbed from the outside (adhesions, a tumor from another organ), from the inside - during an inflammatory process, when the edema blocks the lumen of the canal or fluid accumulates in the tube (hydrosalpinx). This type of infertility can occur if during some operation the fallopian tube was partially or completely removed, or a scar developed in it due to surgical intervention.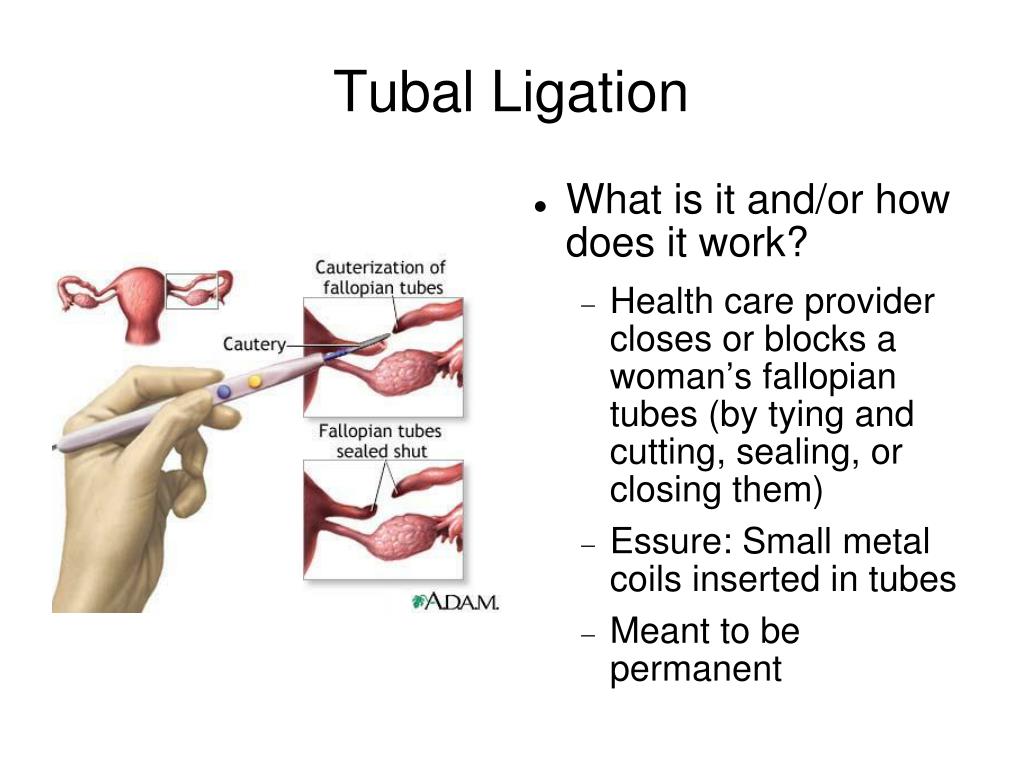
Peritoneal infertility
Always develops due to the presence of adhesions in the small pelvis, which is a response to microbial or aseptic (occurring in sterile conditions) inflammation. It is not subdivided in any way.
Another classification involves the division of infertility into:
- Relative: pregnancy may develop.
- Absolute: conception in a natural way is impossible (for example, with complete obstruction of the appendages from 2 sides at once).
Why tubo-peritoneal infertility occurs
The main causes of tubal infertility are:
- Microbial inflammation , usually starting in the vagina, where the infection is most often transmitted through sexual contact. These are processes caused by ureaplasmas, chlamydia, herpes simplex virus, mycoplasmas, gonococci, trichomonadia and others.
- Operations on the reproductive organs : removal of an apoplectated (“bursted”) ovary, damaged as a result of tubal pregnancy, fibroids, cysts of any size, including dermoid or endometrioid.
 Causes of tubal infertility can also be found in operations on the kidneys or intestines.
Causes of tubal infertility can also be found in operations on the kidneys or intestines. - Postpartum traumatic or inflammatory complications .
Violation of the motor activity of the tubes is due to a change in the level of hormones and those substances that control tubal peristalsis. The main causes of discoordination of the movements of the appendages are chronic stress, increased levels of male hormones, disruption of the adrenal glands, swelling as a result of their independent or postoperative inflammation.
Peritoneal infertility factor is caused by the development of inflammatory diseases of the uterus or appendages, operations performed on them, as well as endometriosis, especially its form when the uterine mucosa begins to develop on the peritoneum.
Infertility itself does not show any special symptoms, except for the impossibility of getting pregnant with frequent unprotected intercourse .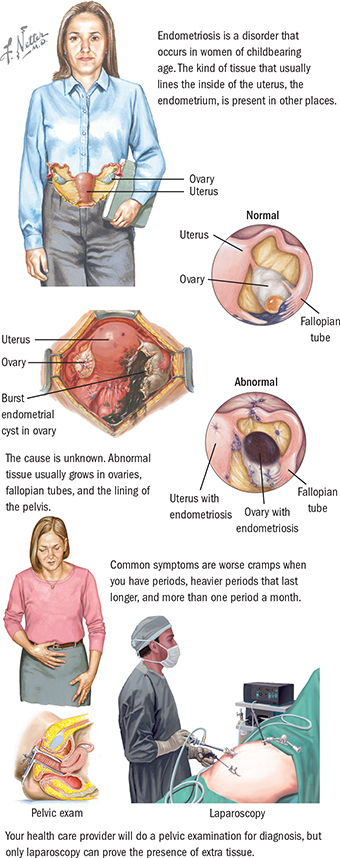
Diagnostics
It is possible to confirm the presence and establish the causes of peritoneal infertility using instrumental laboratory tests:
- Hysterosalpingography: x-ray with filling of the uterus and fallopian tubes with contrast.
- Hydrosalpingoscopy: Ultrasound with filling of the appendages with water, which is a contrast to the ultrasound.
- Kymographic pertubation - the study of the motor activity of the appendages after the introduction of air or carbon dioxide into them.
- Phalloscopy - examination of the cavity of the appendages using fiber optics.
- For the diagnostic purpose of functional tubal infertility, it is necessary to find out the levels of hormones LH, FSH, prolactin, testosterone.
- Laparoscopy is a method in which a tube with a camera at the end is inserted into the abdominal cavity. This is a method by which not only diagnostics is carried out, but also the dissection of adhesions or the removal of endometrioid foci, which cause tubal-peritoneal problems with conception.
Treatment
Treatment of tubal infertility of a functional nature is carried out with medication: anti-inflammatory drugs, antispasmodics, adaptogens. Very good efficiency is given by psychotherapeutic methods, gynecological massage, hydrotherapy, ultrasound, balneotherapy.
If the problem of unsuccessful conception caused damage to the tube, and it consisted in acute or exacerbated at the moment bacterial inflammation of the appendages, antibacterial drugs are prescribed with subsequent restorative treatment (physiotherapy, mud therapy, hirudotherapy).
When the cause is chronic inflammation, therapy is carried out using not only antibiotics, but also drugs that increase immunity. Physiotherapy methods are also involved, aimed at resolving edema and fluid accumulation.
Therapy of endometriosis is carried out by a course of hormonal drugs, after which laparoscopic removal of foci of abnormally located endometrium is usually performed.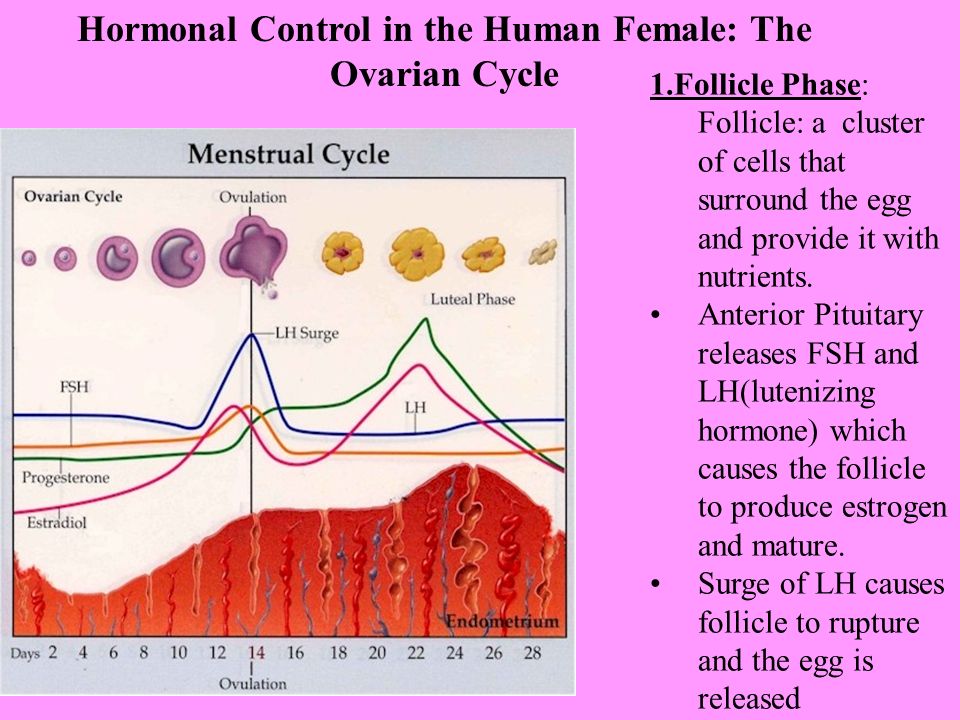
Treatment of peritoneal infertility is carried out promptly: 2 incisions are made on the anterior abdominal wall, through 1, sterile air is first injected into the abdominal cavity, then an apparatus with a camera is inserted there. The second incision serves to insert microinstruments into it, which will dissect the adhesions and cauterize them.
If the fallopian tubes are blocked due to any of the causes, surgical treatment is also needed. The method is selected depending on the situation. So, can be held:
- salpingolysis - dissection of adhesions;
- fimbrioplasty - restoration of only the entrance to the fallopian tube;
- salpingostomy - creation of a new hole in the overgrown section;
- salpingo-salpingoanastomosis - removal of a part of the tube with their subsequent reconnection after restoring the patency of the resected area;
- adnexal implantation in the uterus if there is no patency in the tubal interstitial region.

After any of the operations, you will need course of several courses of anti-inflammatory, absorbable, anti-adhesion therapy . If pregnancy does not occur after the operation for six months or a year, it makes sense to start preparing for IVF, since the more time passes, the less likely it is. Preparation for IVF - preconception preparation is a preliminary stage before reproductive technologies.
Treatment with folk remedies for this pathology is ineffective.
In our clinic you can get all types of physiotherapy used for the treatment of tubal infertility, mud and ozokerite therapy, hirudotherapy and other methods of rehabilitation therapy.
The many years of positive experience of the work of the LENAR IEC testifies to the high expediency of using therapeutic physical factors in the complex of therapeutic measures when planning pregnancy, preparing for the IVF program, in the treatment of gynecological diseases in order to improve the reproductive health of women, the onset of pregnancy and its successful completion.