Vaccine vs shot difference
Immunisation or vaccination - what's the difference?
Immunisation or vaccination - what's the difference? | Pregnancy Birth and Baby beginning of content6-minute read
Listen
What is a vaccine?
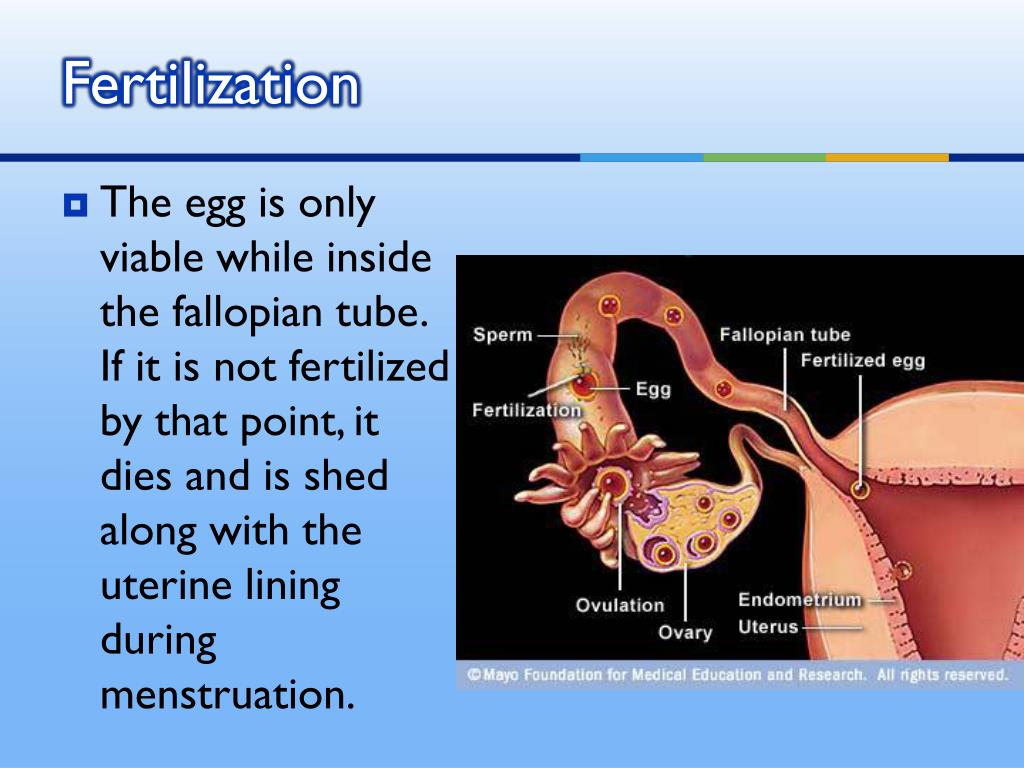
Vaccination prepares the immune system to fight against a future infection. Vaccines often contain tiny amounts of dead or weakened viruses or bacteria, called antigens. The immune system responds to these antigens without you getting sick, effectively training the immune system to fight the disease if exposed to it in the future.
Some vaccines need to be given more than once — known as ‘booster’ vaccinations. Some vaccines, such as the seasonal influenza (flu) vaccine, only work for a short period of time. This is because the virus itself can change over time.
Vaccines are usually given with an injection.
What is in vaccines?
Some vaccines contain a very small dose of a live but weakened form of a virus. Some vaccines contain a very small dose of killed bacteria or small parts of bacteria, and other vaccines contain a small dose of a modified toxin produced by bacteria.
Vaccines may also contain either a small amount of preservative or a small amount of an antibiotic to preserve the vaccine. Some vaccines may also contain a small amount of an aluminium salt, which helps produce a better immune response.
How does immunisation work?
The terms ‘vaccination’ and ‘immunisation’ don’t mean quite the same thing. Vaccination is the term used for getting a vaccine — that is, actually getting the injection or taking an oral vaccine dose. Immunisation refers to the process of both getting the vaccine and becoming immune to the disease following vaccination.
All forms of immunisation work in the same way. When someone is injected with a vaccine, their body produces an immune response in the same way it would following exposure to a disease but without the person getting the disease.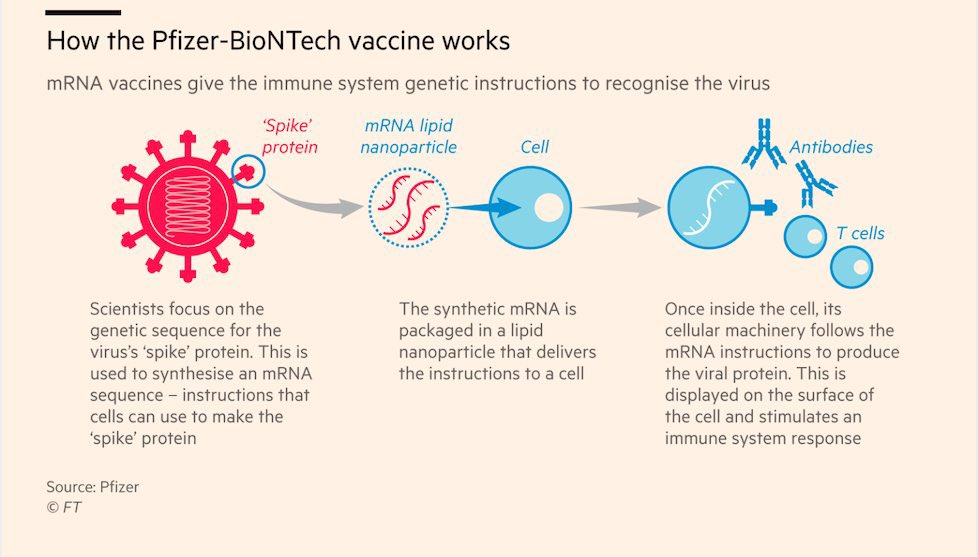 If the person comes in contact with the disease in the future, the body is able to make an immune response fast enough to prevent the person developing the disease or developing a severe case of the disease.
If the person comes in contact with the disease in the future, the body is able to make an immune response fast enough to prevent the person developing the disease or developing a severe case of the disease.
What’s the difference between a booster dose and a primary vaccine course?
A primary vaccine course involves the vaccine doses you need for very good protection against a disease.
A booster dose refers to an extra dose of a vaccine that is given after you’ve completed the primary vaccine course.
It gives your immune system a 'boost' and helps provide a higher level of protection from the disease.
Booster doses are common with diseases such as COVID-19, tetanus and whooping cough (pertussis).
How long do immunisations take to work?
In general, the normal immune response takes approximately 2 weeks to work. This means protection from an infection will not occur immediately after immunisation. Most immunisations need to be given several times to build long-lasting protection.
A child who has been given only 1 or 2 doses of the DTPa vaccine is only partially protected against diphtheria, tetanus and pertussis (whooping cough) and may become sick if exposed to these diseases until they have all the doses they need. However, some of the new vaccines, such as the meningococcal ACWY vaccine, provide long-lasting immunity after only one dose.
How long do immunisations last?
The protective effect of immunisations is not always lifelong. Some, like tetanus vaccine, can last up to 10 years depending on your age, after which time a booster dose may be given. Some immunisations, such as whooping cough vaccine, give protection for about 5 years after a full course. Influenza immunisation is needed every year due to frequent changes to the type of flu virus in the community.
Is everyone protected from disease by immunisation?
Even when all the doses of a vaccine have been given, not everyone is protected against the disease. Measles, mumps, rubella, tetanus, polio, hepatitis B and haemophilus influenzae type b (Hib) vaccines protect more than 95% of children who have completed the course. One dose of meningococcal ACWY vaccine at 12 months protects over 90% of children.
One dose of meningococcal ACWY vaccine at 12 months protects over 90% of children.
Three doses of whooping cough vaccine protect about 85% of children who have been immunised, and will reduce the severity of the disease in the other 15% if they do catch whooping cough. Booster doses are needed because immunity decreases over time.
Some vaccinations, like for COVID-19, won’t necessarily prevent you from catching the disease, but can reduce the risk of serious illness.
How are vaccines approved in Australia?
Before a vaccine becomes available in Australia, it must pass the rigorous approval processes of the Therapeutic Goods Administration (TGA). This includes assessing every ingredient in the vaccine for safety, quality and effectiveness.
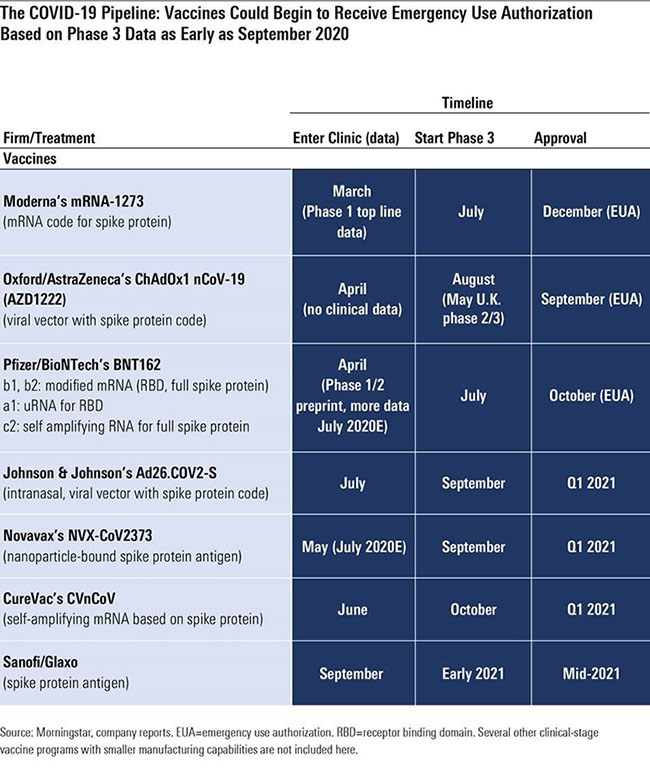
A clinical trial is a scientific study conducted by the makers of a vaccine. Clinical trials of medicines are done in phases.
The TGA carefully assesses the results of clinical trials, as well as the way in which the trials were run.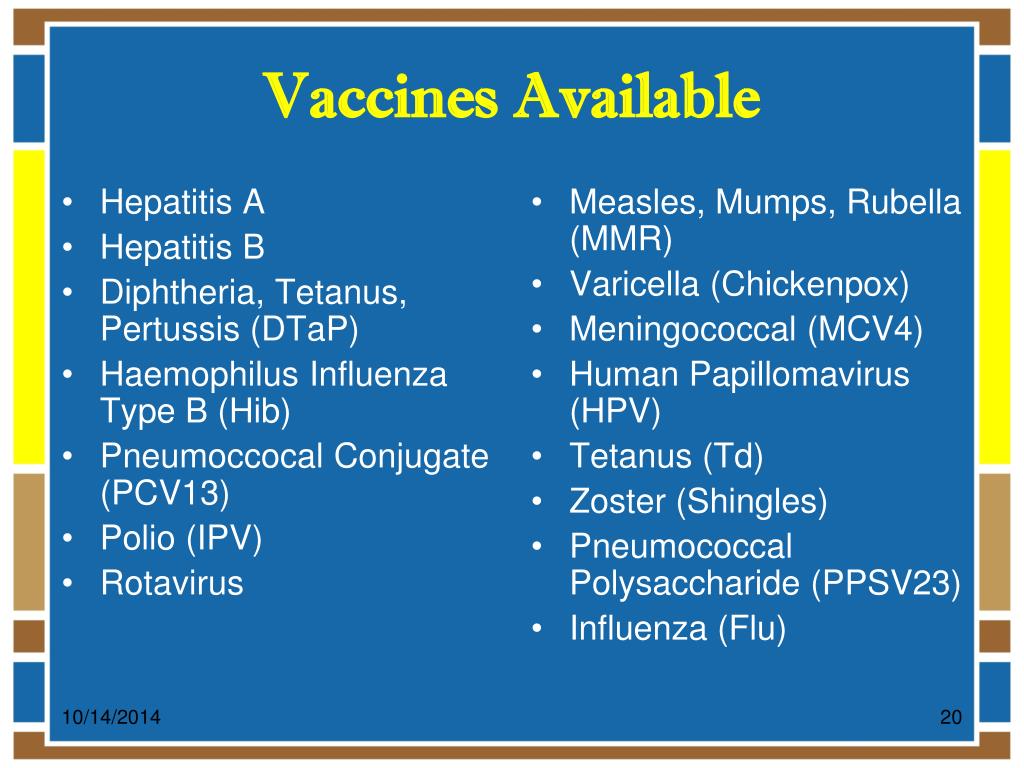 The TGA also checks that the trials involved enough human participants that represented the people for whom the vaccine is intended.
The TGA also checks that the trials involved enough human participants that represented the people for whom the vaccine is intended.
The TGA ensures that vaccine manufacturers meet manufacturing quality standards. TGA laboratories assess the quality of every batch of a vaccine before it can be supplied in Australia.
Sometimes a ‘provisional approval pathway’ is needed for the temporary registration of promising new medicines and vaccines — where the need for early access outweighs any risks.
Resources and support
In Australia, vaccines are funded by the National Immunisation Program and protect millions of Australians from vaccine-preventable diseases.
If you have any questions, you can speak to your doctor or call healthdirect on 1800 022 222 (known as NURSE-ON-CALL in Victoria).
Sources:
Department of Health (The Australian Immunisation Handbook), Raising Children Network (Immunisation in childhood), Raising Children Network (Immunisation FAQs), Department of Health (National Immunisation Program Schedule), Australian Government Department of Health (COVID-19 vaccines), NSW Health (Booster vaccination - frequently asked questions), Therapeutic Goods Administration (COVID-19 vaccine approval process)Learn more here about the development and quality assurance of healthdirect content.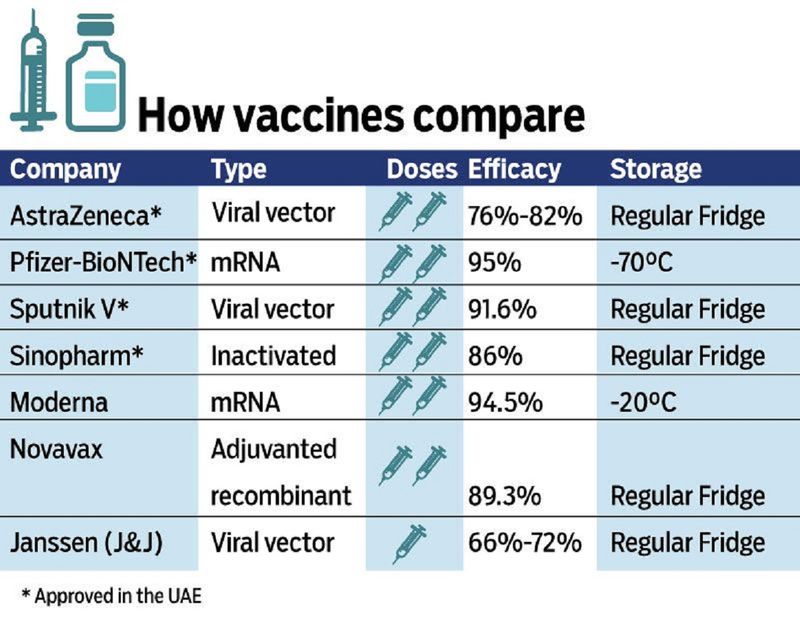
Last reviewed: May 2021
Back To Top
Related pages
- Immunisation and vaccinations for your child
- Vaccinations and pregnancy
Need more information?
Immunisation | Tasmanian Department of Health
Learn about information about immunisation, vaccines and diseases preventable by immunisation in Tasmania.
Read more on Tasmanian Department of Health and Human Services website
Immunisation and vaccinations for your child
Immunisation is a simple, safe and effective way of protecting children against certain diseases. Discover more about childhood vaccinations.
Read more on Pregnancy, Birth & Baby website
Immunisation | SA Health
Information for consumers on vaccines, immunisation programs and immunisation records for you and your children
Read more on SA Health website
Immunisation records | NCIRS
Your immunisation history statement has all your vaccines that have been recorded on the Australian Immunisation Register (AIR)
Read more on National Centre for Immunisation Research and Surveillance (NCIRS) website
What is immunisation? | Australian Government Department of Health and Aged Care
On this page Immunisation or vaccination — what's the difference? Australia's National Immunisation Program Immunisation is a safe and effective way of protecting you and your child against serious diseases.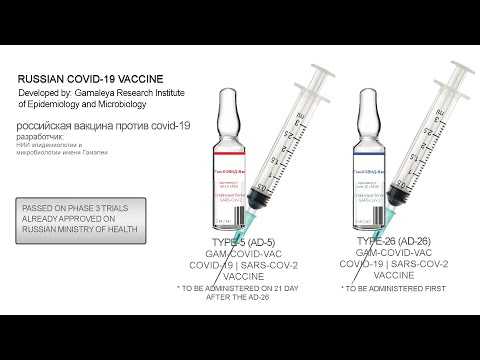
Read more on Department of Health and Aged Care website
Where can I get immunised? | Australian Government Department of Health and Aged Care
You can get vaccinations from a range of vaccination providers, including your local GP and school-based immunisation programs.
Read more on Department of Health and Aged Care website
Immunisation schedules | NCIRS
The Australian National Immunisation Program (NIP) is funded by the Australian government and implemented by state and territory departments of health
Read more on National Centre for Immunisation Research and Surveillance (NCIRS) website
Kids - Immunisation Coalition
Find out how to protect your kids from infectious diseases.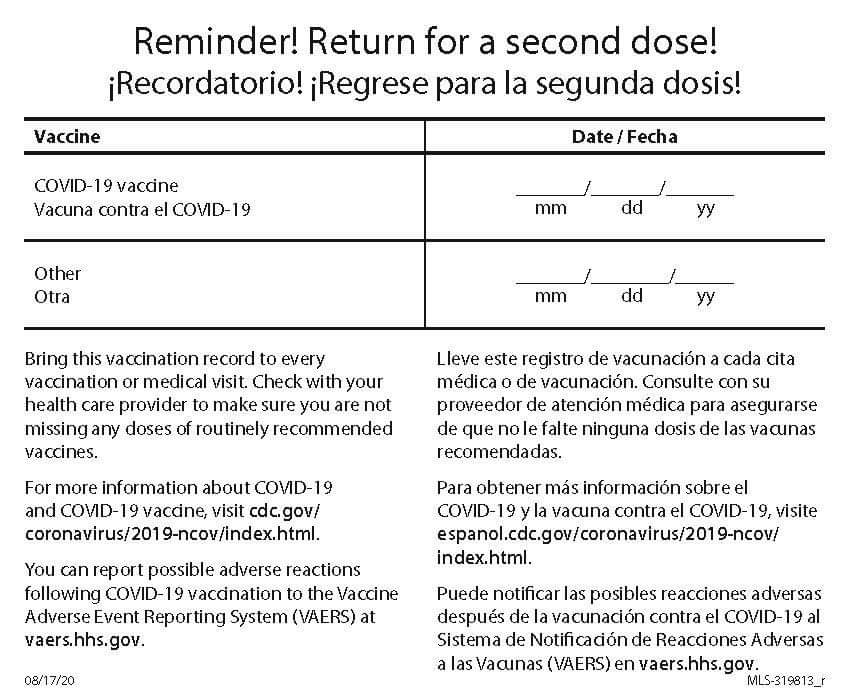 Keep up to date with the Childhood National Immunisation Program schedule.
Keep up to date with the Childhood National Immunisation Program schedule.
Read more on Immunisation Coalition website
Keeping your child’s vaccinations up to date during COVID-19
The COVID-19 pandemic has led to a decrease in children getting their routine childhood vaccinations.
Read more on Pregnancy, Birth & Baby website
Vaccination matters
Ensure your decisions about immunisation are based on fact. When doing your personal reading, make sure your source of information is based on scientific fact.
Read more on Queensland Health website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.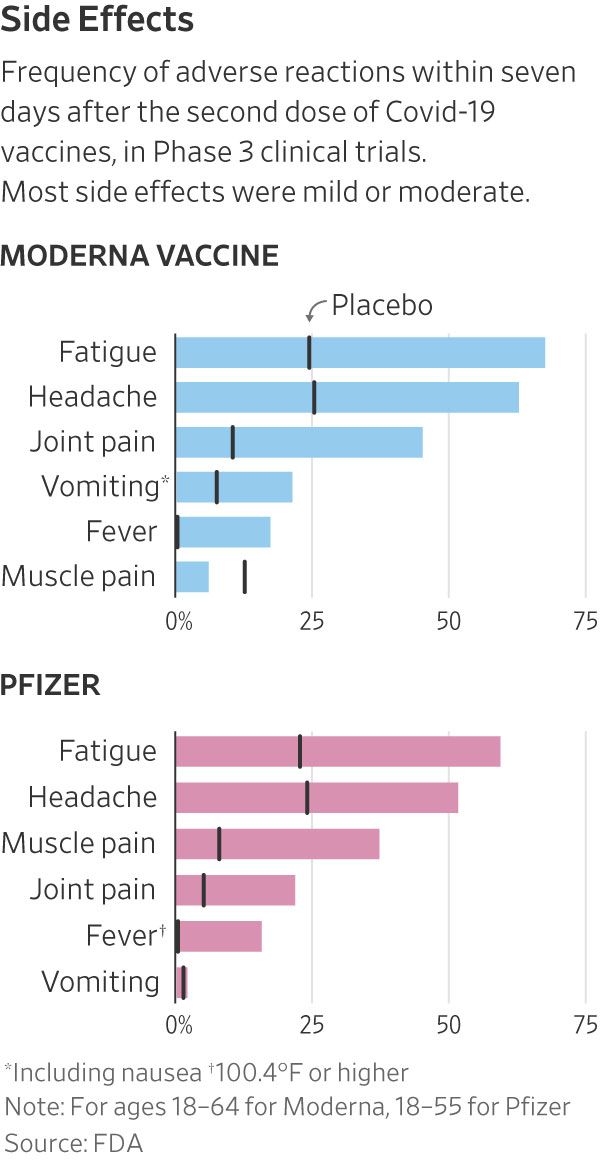
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Difference Between Immunization & Vaccination
Immunization means to make someone immune to something. Vaccination, by contrast, according to Dorland’s Medical Dictionary, just means to inject “a suspension of attenuated or killed microorganisms…administered for prevention…or treatment of infectious disease.”
Most people do not realize that when you receive a shot or a vaccine it does not mean you are immunized. Many people believe that once you are vaccinated you are completely protected. That belief is wrong.
The use of the word “immunization” instead of “vaccination” is everywhere.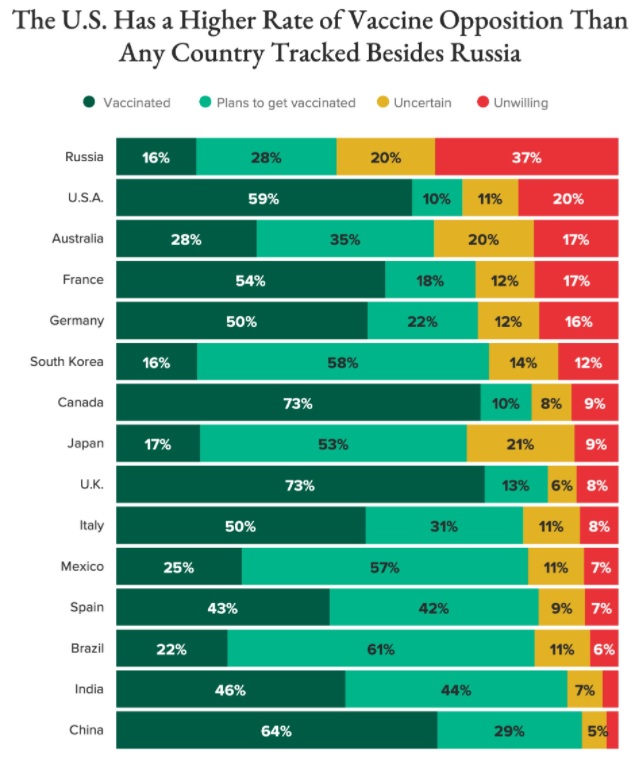 Most importantly, news outlets tell the public that immunization is the same as vaccination. However, there is a large difference between the two.
Most importantly, news outlets tell the public that immunization is the same as vaccination. However, there is a large difference between the two.
Vaccines contain a dead or live weakened germ that can cause a particular disease, like tetanus, or parts of a germ. When we are given a vaccine shot, our body immediately produces antibodies against the germ.
It is at this point that most believe the body’s defense mechanism kicks in and immunity will occur in the event that the said antigen gains entry again into the body but, this is not the case with all vaccines.
Vaccination Doesn’t Guarantee Immunity
Vaccination does not guarantee immunity. Natural immunity happens only after one recovers from the actual disease. During the disease, the microorganism usually has to pass through many of the body’s natural immune defense systems—in the nose, throat, lungs, digestive tract and lymph tissue—before it reaches the bloodstream.
As it does, the microorganism triggers many biological events that are essential in building true natural immunity. When a child gets a new disease, he may feel sick for several days, but, in the vast majority of cases, he will recover.
When a child gets a new disease, he may feel sick for several days, but, in the vast majority of cases, he will recover.
According to the Center for Disease and Prevention Control, CDC, not all that receive a vaccination will have immunity.
Defending what they believe is a misconception that the majority of people who get disease have been vaccinated, they state, “In fact it is true that in an outbreak those who have been vaccinated often outnumber those who have not – even with vaccines such as measles, which we know to be about 98% effective when used as recommended.”
“This is explained by two factors. No vaccine is 100% effective. Most routine childhood vaccines are effective for 85% to 95% of recipients.”
Everyone’s Immune System Reacts Differently
For reasons related to the individual, some will not develop immunity.
The second fact is that in a country such as the United States the people who have been vaccinated vastly outnumber those who have not.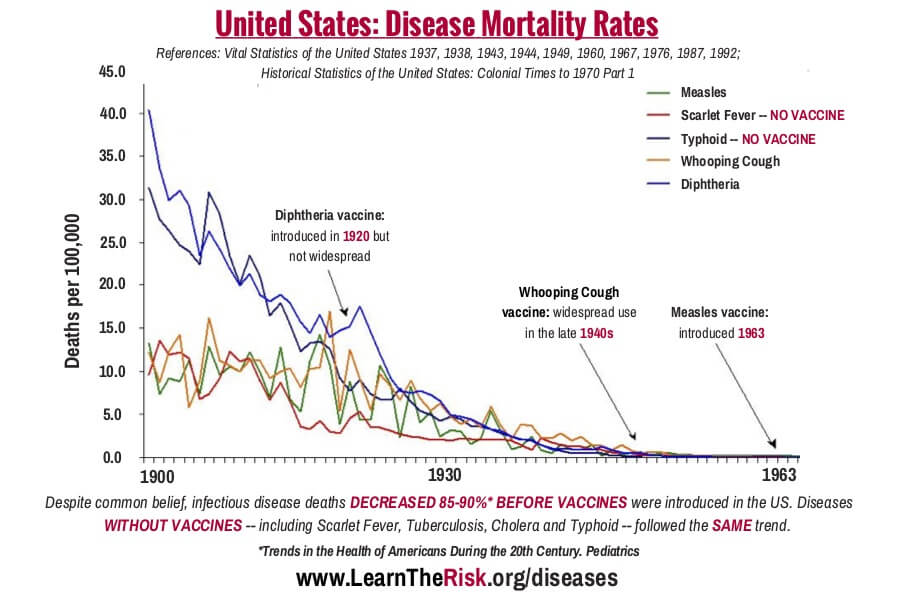 Here’s a hypothetical example of how these two factors work together.
Here’s a hypothetical example of how these two factors work together.
The National Network of Immunization Information provides, “Although vaccines have very high effectiveness rates, they are not completely effective for 100% of the people who receive them. For example, a full series of measles vaccine will protect 99 of 100 children from measles and polio vaccine will protect 99 of 100 children from polio. This means when there is a disease outbreak, the very small number of people for whom the vaccine did not work may still be able to catch the disease. Because almost all of our children are immunized and only few are not, it can be the case that during an epidemic the majority of cases occur among children who were immunized. However, the fact remains that those who have not received the vaccine are much more likely to catch the disease.”
Types of Vaccines
There are several different approaches that are used when vaccines are made. Each approach has its own way that it keeps the virus from sickening the recipient of the vaccine. When a company is developing a vaccine, they will have to choose which one of these methods works best to make the vaccine the most effective.
When a company is developing a vaccine, they will have to choose which one of these methods works best to make the vaccine the most effective.
Here are the types of vaccines that are used:
Weakening Vaccines (Live Attenuated)
Some viruses reproduce thousands of times within the body. The bacteria invades the body and then it multiplies exponentially. This type of vaccine involves the introduction of the live virus into the body. While you may think that injecting a virus into the body will have harmful effects, the opposite holds true with these types of vaccines. The theory behind these vaccines is that they are intended to “educate” the body to defend itself from the virus. Once that occurs, the viruses will have difficulty reproducing within the body. Here, much of the work is done before the virus is injected into the body. The virus is grown outside of its normal environment. When that happens, it becomes a weakened form of itself. By the time that it is introduced to the body, it is unable to reproduce itself.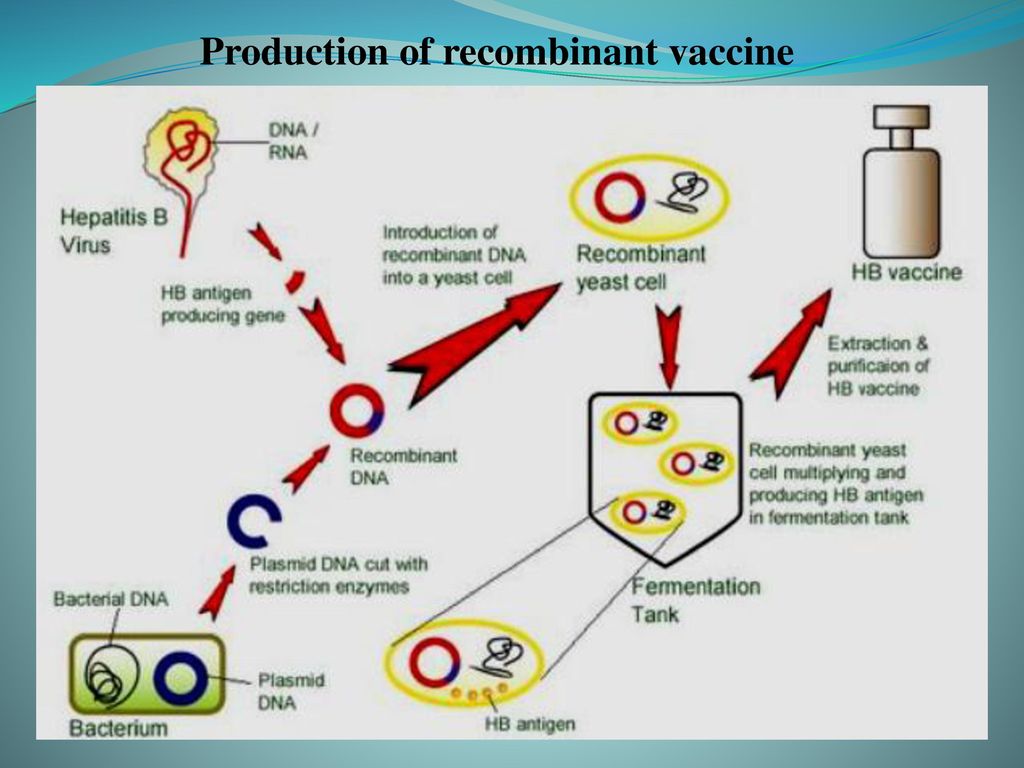
The advantages of live attenuated vaccines include:
- They are relatively easy to create for the viruses that they protect against
- They do not need to be taken more than once or twice
- They help strengthen the immune system since they are very close to the actual virus
However, there are some disadvantages to this type of virus. They include:
- Since they are weakened viruses, they can always re-strengthen and cause the sickness
- They must be well-stored and refrigerated which makes them difficult to ship to certain places
- Attenuated vaccines do not work well with bacterial viruses
Attenuated vaccines are used to immunize against the following diseases:
- Measles, mumps, and rubella
- Chickenpox
- Smallpox
- Yellow Fever
Inactivation Vaccines
Instead of introducing a weakened form of the virus into the body, this type of vaccine aims to completely stop the virus from reproducing.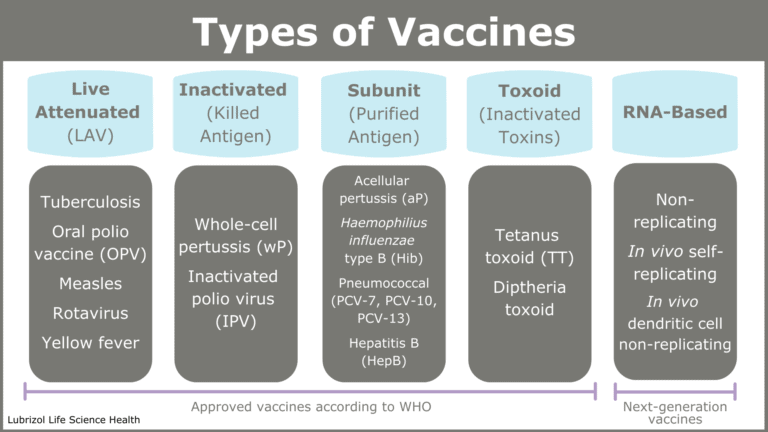 Usually, this type of vaccine will rely on a chemical or a pathogen to achieve that result. The body will continue to recognize the virus so it will keep producing the cells that will protect against the virus. The pathogen will still continue to exist, but it will not be able to replicate within the body.
Usually, this type of vaccine will rely on a chemical or a pathogen to achieve that result. The body will continue to recognize the virus so it will keep producing the cells that will protect against the virus. The pathogen will still continue to exist, but it will not be able to replicate within the body.
The advantages of inactivation vaccines include:
- No form of the disease will be produced by the body whatsoever. This includes even a milder form.
- This is not a type of vaccine that cannot be given to those with weakened immune systems
However, unlike live attenuated vaccines, one or two injections will generally not be enough to provide lifetime protection against these diseases. In addition to the initial vaccination, several long-term booster shots will be necessary to continue to provide immunity against the diseases.
Types of diseases that are protected against by this type of vaccine include:
- Polio
- Rabies
- Hepatitis A
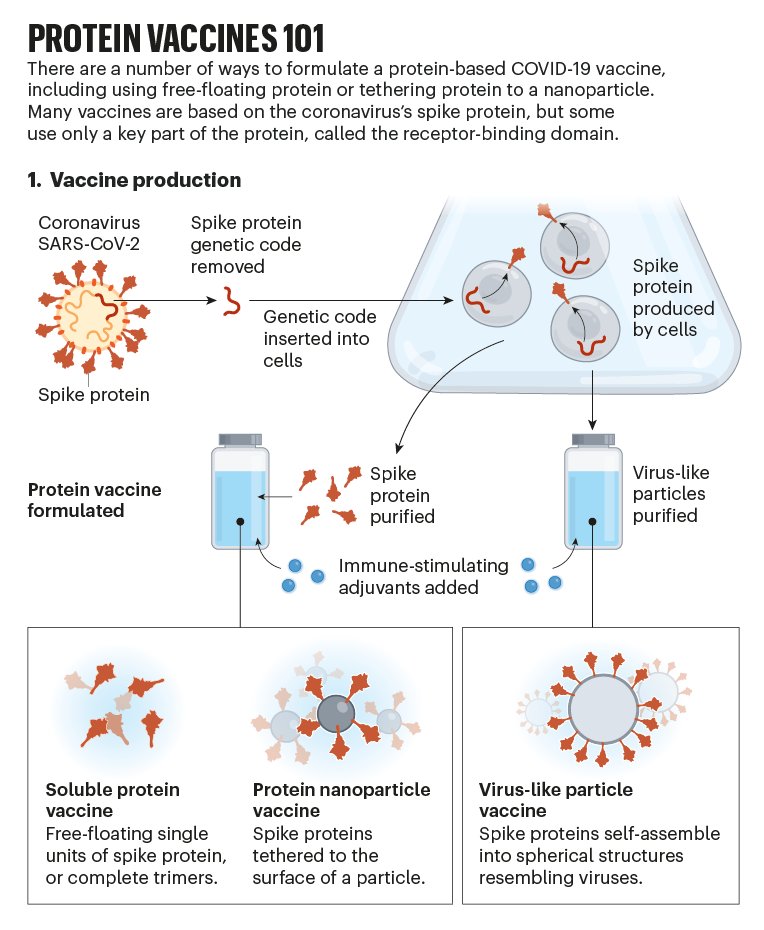
Subunit and Conjugate Vaccines
Subunit vaccines use only a part of the virus in order to create the immunization. They take out only the essential part of the antigen in order to produce the vaccine and leave everything else. This will usually mean that a protein is used that resides on the surface of the virus. This type of vaccine is suitable for an instance where the body needs to protect against one specific part of the virus in order to protect against the entire disease. One of the advantages to this type of vaccine is that the body can give a targeted and focused response to the part of the germ that has been selected.
They take out only the essential part of the antigen in order to produce the vaccine and leave everything else. This will usually mean that a protein is used that resides on the surface of the virus. This type of vaccine is suitable for an instance where the body needs to protect against one specific part of the virus in order to protect against the entire disease. One of the advantages to this type of vaccine is that the body can give a targeted and focused response to the part of the germ that has been selected.
Conjugate vaccines use two different components instead of one. They use parts of the coats of bacteria. These parts are then linked to a protein. The combination of the coats of bacteria and the protein becomes the vaccine. It is the combination of the piece of bacteria and the carrier protein that gives the vaccine its effectiveness.
Some of the positive attributes of these types of vaccines include:
- Those with weakened immune system and other health problems can receive the vaccine without fear of getting the disease
- The immune response is strong and targeted
Those who receive this type of vaccine will likely require booster shots in order to receive continuous protection from the disease. In other words, recipients will not be able to have just one vaccination.
In other words, recipients will not be able to have just one vaccination.
Some of the diseases that this type of vaccine protects against include:
- Shingles
- HPV
- Hepatitis B
- Meningococcal disease
- Whooping cough
- Pneumococcal disease
Toxoid Vaccines
Toxoid vaccines use the harmful thing that is produced by the disease called the toxin, inactivating it with a chemical and reintroducing it into the body. The inactivated toxin becomes the vaccine. As opposed to vaccinating against the entire germ, these vaccinate against the part of the germ that causes the disease. These types of vaccines are considered to be bacterial in nature because they contain the actual bacteria. In other words, when the inactivated toxins are introduced, they stimulate the production of antibodies to the toxin. However, they will not cause the disease itself to take root.
These vaccines can be given to people who have immune systems that are weakened or compromised.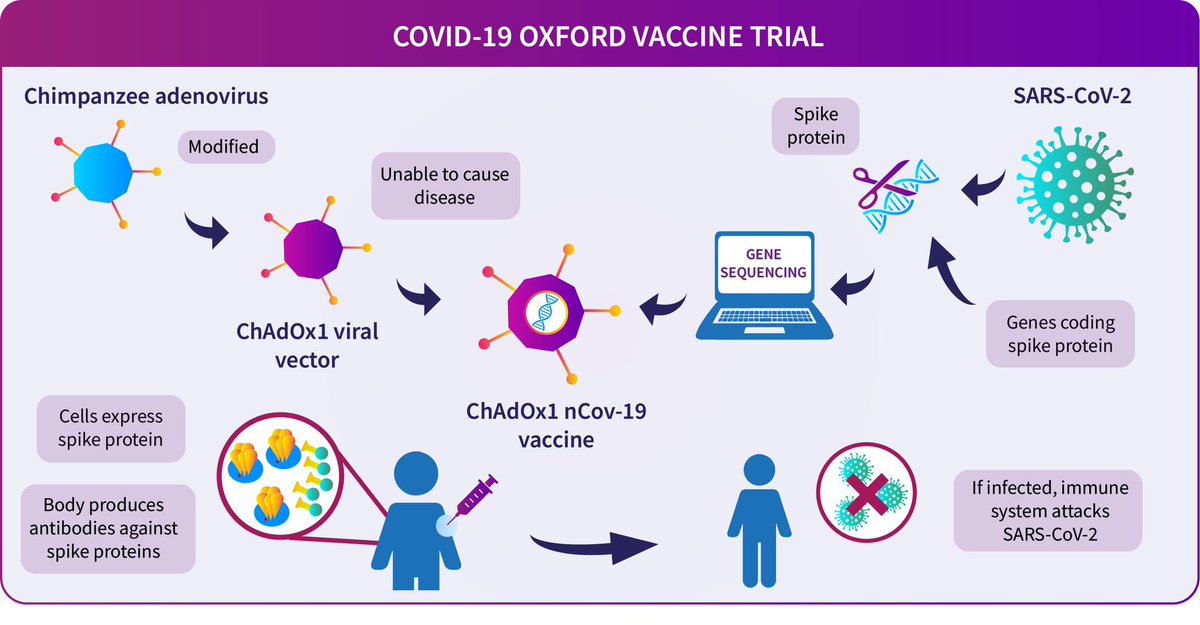 However, the amount of antibodies that is produced by the body declines over time with these types of vaccines. Thus, periodic booster shots are necessary to maintain the proper level of protection.
However, the amount of antibodies that is produced by the body declines over time with these types of vaccines. Thus, periodic booster shots are necessary to maintain the proper level of protection.
Some of the diseases treated by this type of vaccine include:
- Tetanus Diphtheria
How Are Vaccines Administered?
There are several different ways that vaccines are administered. Most vaccines are administered through the form of an injection. However, advances in the medical field have diversified the means of delivery of new types of vaccines. Here are some means of administering vaccines through means other than an injection.
- Nasal Spray – flu injections are given to patients through their nose as a mist.
- Inhalant – There is a type of measles vaccine that is inhalable through the mouth.
- Orally – Certain vaccines can given in tablet form.
- Microneedle – Certain flu vaccines can shoot the substance into the body without the use of needles.
What Are the Types of Immunization?
There are two different types of immunization. Each one has different features to it. The two types are active and passive immunizations. Below is some information on each of the two kinds of immunity.
Active Immunization
The term “active immunization” characterizes how the body responds to receiving a vaccine. The vaccine stimulates the production of antibodies. Then, the antibodies will actively fight off the virus or the bacteria. The vaccine recipient will usually need a strong immune system in order to achieve the desired result. Active immunization cannot occur until the recipient has been exposed to the particular pathogen that is contained in the vaccine. The immunity is triggered by the exposure to the pathogen. Vaccines are considered to be a form of active immunization.
Passive Immunization
Passive immunity comes from the transfer of antibodies of an immune person to the body of a person who is not immune.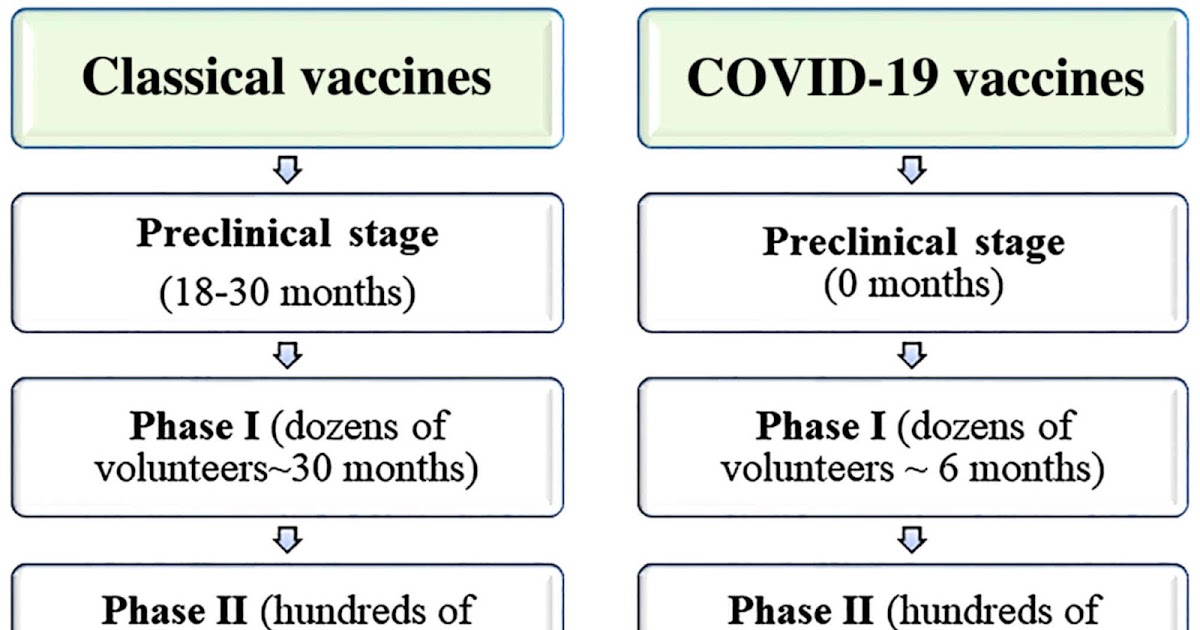 This can happen naturally, such as when a mother passes immunity to a disease to the child through the fetus. It can also occur through a transfer in a substance such as immune globulin, which is given when protection from a certain disease is necessary. This protection occurs immediately, as opposed to active immunization, which takes time for the body to develop the necessary antibodies.
This can happen naturally, such as when a mother passes immunity to a disease to the child through the fetus. It can also occur through a transfer in a substance such as immune globulin, which is given when protection from a certain disease is necessary. This protection occurs immediately, as opposed to active immunization, which takes time for the body to develop the necessary antibodies.
What Are the Differences Between Active and Passive Immunity?
- Active immunity takes some time to develop, usually as a response to receiving the vaccine. Passive immunity comes immediately upon transfer.
- Passive immunity is not permanent and may last for a certain limited period of time. Active immunity is longer-lasting and is either permanent or lasts a long time until a subsequent booster shot is needed.
- In passive immunity, the antibodies comes from outside the body. In active immunity, the antibodies come from within the body in response to the introduction of another substance.
- Passive immunity is usually artificially induced.
Immunization and Vaccine Side Effects
There are three different possible reactions, or lack thereof, that people can experience when they have received immunizations and vaccinations. They are as follows:
- No Side Effects – The majority of people who receive immunizations and vaccinations do not experience any side effects. Sometimes, there is soreness or redness at the site of injection, but nothing further. If there are minor side effects, it is often a sign that the vaccination is working insofar as the body is beginning to build up the resistance necessary to immunize against the disease.
- Common Side Effects – While these side effects may be painful or temporarily debilitating, they are not much about which to be overly concerned. Among other things, these side effects consist of pain and itching at the injection site, dizziness, fever, nausea and a mild rash.
 Most often, these side effects pass after a period of time.
Most often, these side effects pass after a period of time. - Serious Side Effects – In some instances, patients can have severe side effects based on how their bodies react to the vaccination. This could mean seizures, brain damage and in a worst-case scenario, death.
The most important thing is to know what to do when you or someone in your family begins to experience side effects from a vaccination. Here are several important considerations that span both legal and medical issues.
- See a Medical Provider Immediately – If you believe that the side effects are anything more than common, it is essential to be seen by a healthcare provider immediately. From the obvious standpoint, adverse reactions to vaccination can endanger health both in the short and long terms. From a legal perspective, it is essential to document the complications that have been caused by an immunization.
- Report the Side Effect – There is a Vaccine Adverse Event Reporting System that allows people to report any complications.
 Tracking any side effects is essential in order to both know about them and prevent widespread complications if possible.
Tracking any side effects is essential in order to both know about them and prevent widespread complications if possible. - Contact an Attorney – There is a National Vaccine Injury Compensation Program that exists for those who have suffered injury from receiving vaccines. This is a special court that has been set up which has its own rules and procedures. A claim must be filed in order to be eligible for compensation. An attorney who specializes in vaccine injuries will know the most effective way to file a claim for compensation.
Common Side Effects
- Pain, redness, tenderness or swelling at injection site
- Fatigue
- Headache
- Itching at injection site
- Nausea
- Dizziness or fainting (most common in adolescents)
- Fever
- Mild rash
Serious Side Effects
- Severe Allergic Reaction (Anaphylaxis)
- Seizures
- Brain Damage
- Blood Disorders
- Bowel Obstruction
- Nerve Damage
- Death
People Ask:
Vaccine Injury Reporting
When one has sustained an injury as a result of being administered a vaccine, there is a different mechanism whereby one would receive compensation. Vaccines have both their own means of the reporting the injury as well as for filing a claim. This is not the same process that one would follow when they are injured by a medical device or medication.
Vaccines have both their own means of the reporting the injury as well as for filing a claim. This is not the same process that one would follow when they are injured by a medical device or medication.
Why Are Vaccines Different Than Other Medical Claims?
Congress passed the National Childhood Vaccine Injury Act in 1986 as a means of encouraging vaccine makers to produce their products while, at the same time, protecting patients from harm. The intent behind the statute was to keep manufacturers from having to face litigation from the products that they sold. On the other side, Congress also wanted to encourage people to be vaccinated by ensuring that they could be compensated for any injuries that they suffered.
How Are Vaccine Injuries Reported?
While the FDA has its own adverse event reporting database, the Centers for Disease Control, in tandem with the FDA, has its own Vaccine Adverse Event Reporting System for vaccine injuries. VAERS exists to serve as a repository for information about vaccine related injuries that can be reported to the database by anyone.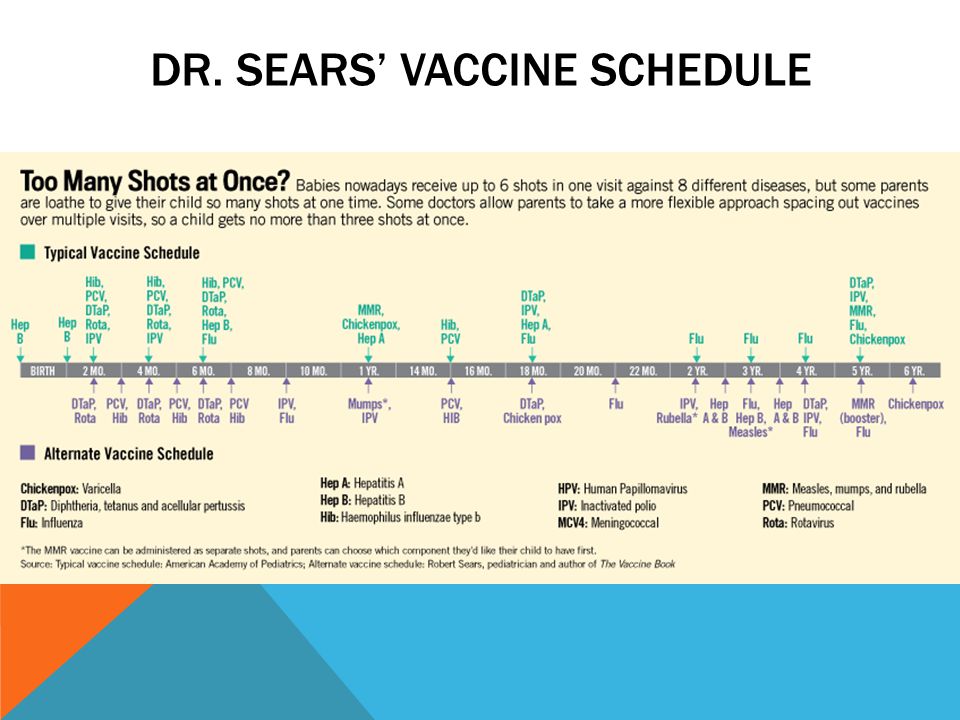 There are several steps that one should take in order to report a vaccine injury to VAERS.
There are several steps that one should take in order to report a vaccine injury to VAERS.
- Contact healthcare provider – The first person to inform of an injury is the physician
- Report the injury – Patients can submit an online report to VAERS
- Update VAERS – If there are medical records pertaining to treatment, they should be uploaded into VAERS.
VAERS is helpful to track various metrics that relate to vaccines. Among the uses of VAERS are:
- It helps to detect any trends in injuries
- Allows people to track the safety of new vaccines
- Gives transparency to adverse events for new vaccinations
- Can identify any patient risk factors for certain vaccine injuries
The National Vaccine Injury Compensation Program
The VICP is the fund that allows those who have suffered vaccine-related injuries to receive compensation for their injuries. The main difference between vaccines and drugs is that, with regard to the VICP, the manufacturers are not paying out the settlement.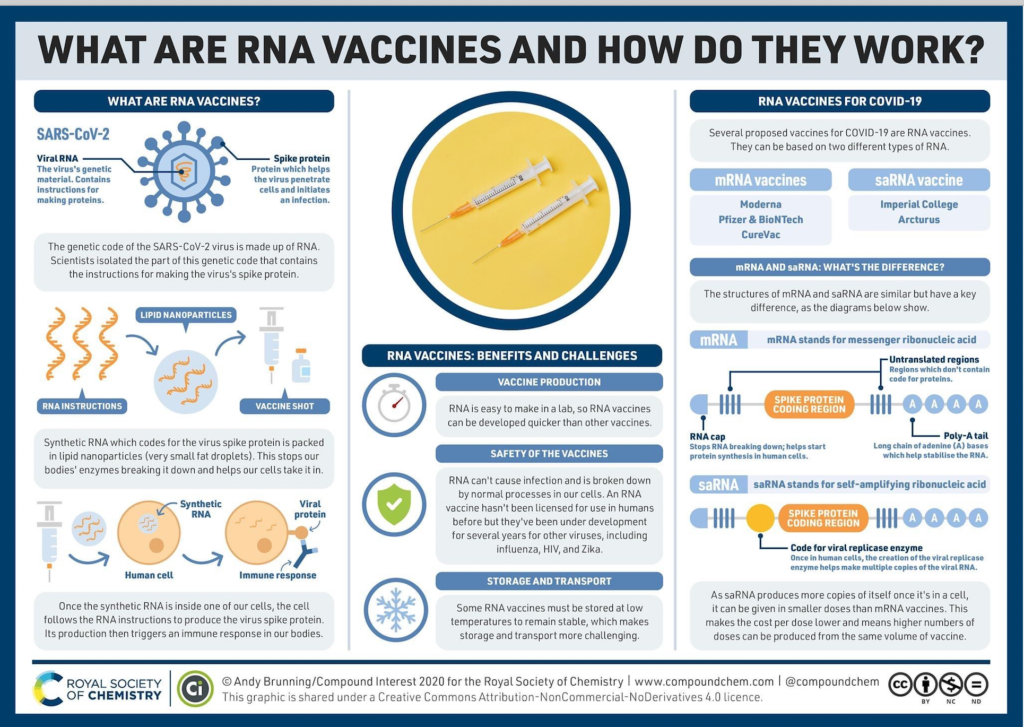 That is because the VICP is intended to shield them from liability in order to encourage them to enter and stay in what is a critical field. The VICP was initially established because there was a scare related to a certain vaccine in the early 1980s that resulted in a threat to the vaccine supply when vaccine makers lost several large lawsuits.
That is because the VICP is intended to shield them from liability in order to encourage them to enter and stay in what is a critical field. The VICP was initially established because there was a scare related to a certain vaccine in the early 1980s that resulted in a threat to the vaccine supply when vaccine makers lost several large lawsuits.
The VICP is funded by a fee that is assessed by the federal government on the sale of every single childhood vaccination. The fees are then placed in the fund which is used to pay out claims as they are filed. This means that patients end up funding the settlements through the vaccines that are purchased.
There is a special mechanism for the VICP that must be followed in order to receive compensation. The process is started by filing a petition with the United States Court of Federal Claims (COFC), which has exclusive jurisdiction over vaccination cases. COFC has Special Masters whose job it is to decide these claims. Before the Special Master issues a decision, the Department of Health and Human Services will make their own recommendation. Then, the Department of Justice develops a report that includes a medical recommendation and legal analysis. After that, the Special Master may hold a hearing and decide the issue of compensation. The petitioner has the right to appeal the Special Master’s decision.
Then, the Department of Justice develops a report that includes a medical recommendation and legal analysis. After that, the Special Master may hold a hearing and decide the issue of compensation. The petitioner has the right to appeal the Special Master’s decision.
It is best to hire an attorney to help with drafting the petition since the case will likely be decided initially on the basis of the petition and any hearing that the Special Master may hold. Given the scientific complexity of vaccines and their injuries, an attorney may best be able to present a case.
Immunizations and vaccines: what is the difference
We work without days off and holidays
COVID 19 antibody tests
Let's get some terminology out of the way. At the household level, many do not feel the difference between serum, vaccine and vaccination, vaccination and immunization - we will try to explain to you the main terms used in vaccine prevention.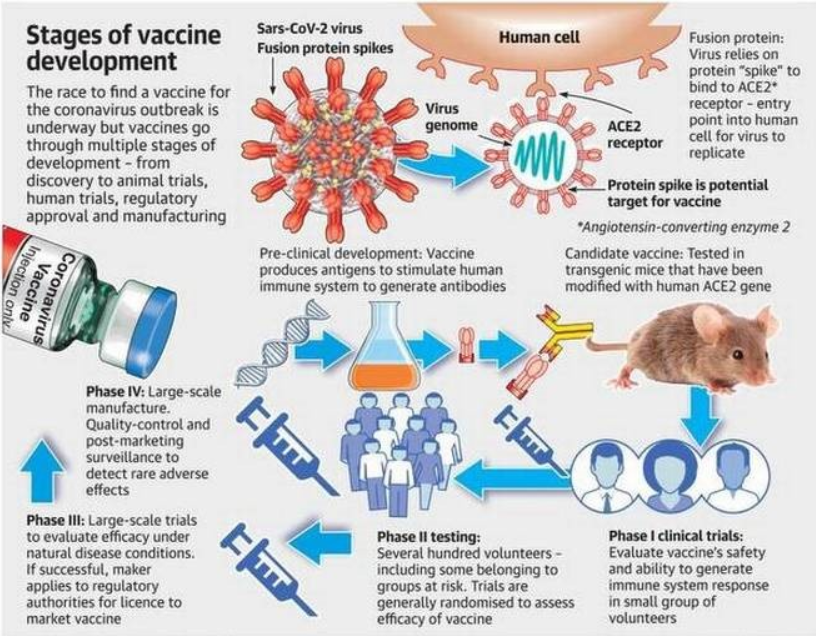 This article does not claim to be fundamental - it is only a quick reference.
This article does not claim to be fundamental - it is only a quick reference.
As a primary source of terms, we used queries that are most often typed in search engines on the topic of vaccination: in the search, people usually write in ordinary, conversational language. Here we will try to avoid complex medical terminology, because the article is written for people who are far from medicine.
Vaccination is perhaps the main method of preventing many serious infectious diseases. The essence of the method is the artificial reproduction of the immune response of the human body, so that in the future the antibodies produced themselves fight the infection (it is also called active immunity).
Immunoprophylaxis is a broader concept than vaccination: it can be "specific" and "non-specific". The first means measures against a specific infection - this, in fact, is vaccination. The second implies a much wider range of ways to increase the immunity of the body as a whole, and not just creating a barrier for specific diseases: hardening, quality nutrition, proper rest and work, minimizing stress - in short, everything that helps the body stay healthy.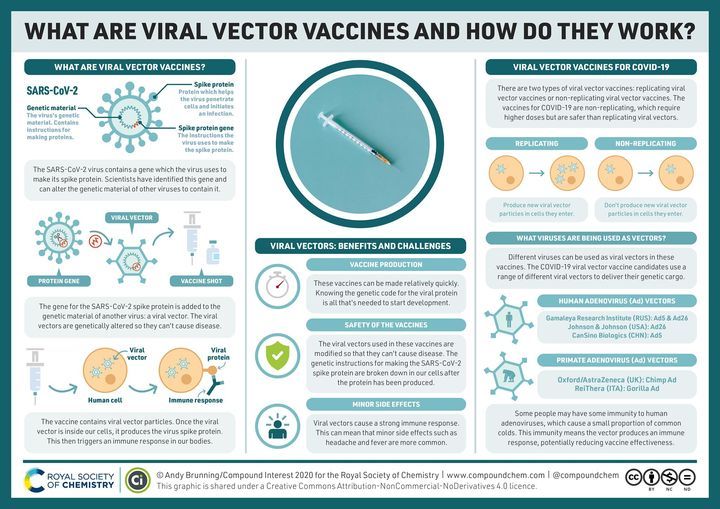 In addition, immunoprophylaxis allows the creation of passive immunity by introducing ready-made antibodies in sera.
In addition, immunoprophylaxis allows the creation of passive immunity by introducing ready-made antibodies in sera.
Vaccination is essentially the same as vaccination, the difference is purely semantic: the word "vaccination" is shorter and easier to pronounce, although the second term is more correct from the point of view of medical science.
Immunization is the same as immunization.
A vaccine is a medical product that is given to a person to develop active immunity to one or more specific diseases. Please note: we are talking about the "drug", and not about the procedure for using it. Sometimes vaccination is understood as the procedure for administering a vaccine, but we will use the word "vaccination" for this.
Serum and vaccine solve the same tasks - they contribute to the development of acquired immunity organisms. But there is also a fundamental difference between them: the vaccine contains weakened or dead agents of infection, and the serum contains ready-made antibodies against a specific disease.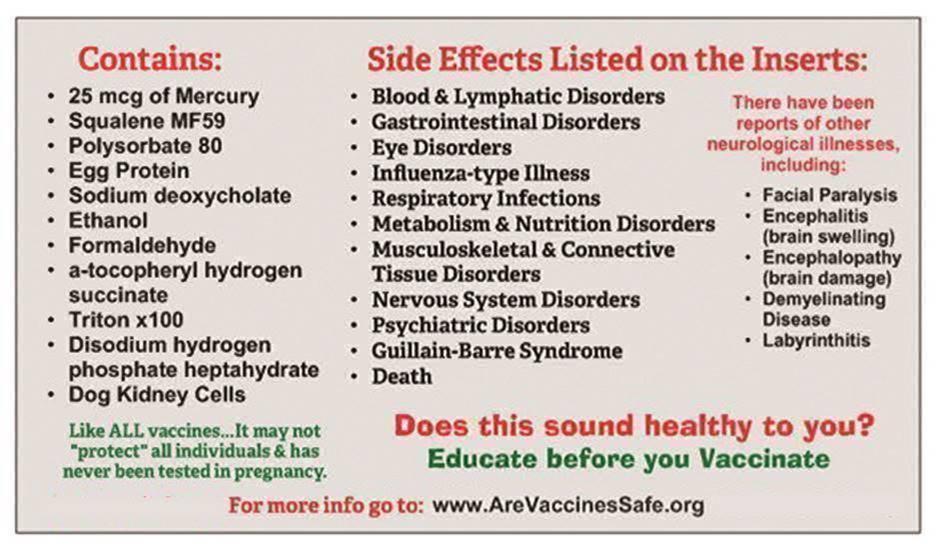 Serum is usually used to fight an already begun disease, that is, it is, in fact, a medicine, not a prophylactic.
Serum is usually used to fight an already begun disease, that is, it is, in fact, a medicine, not a prophylactic.
Inoculation is the procedure for administering a preparation with antigenic material, ie a vaccine or serum. Once again: "vaccine" and "serum" are drugs, "vaccination" is the process of introducing them into the human body. We will adhere to such a division of concepts, but deviations are sometimes possible.
Revaccination is a way to support post-vaccination immunity through repeated vaccinations. Many vaccinations are valid for a limited period, after which the acquired immunity weakens. It is assumed that the primary vaccination has already been carried out, and, based on this, a revaccination schedule is drawn up.
Revaccination is the same as revaccination.
Re-vaccination - the procedure for introducing vaccinations during re-vaccination, that is, during revaccination.
Mandatory vaccination - a list of vaccinations that the state considers necessary: their set and timing are regulated by the National Immunization Schedule. Strictly speaking, there are no mandatory vaccinations in Russia, even children without them are admitted to kindergartens, but only if their parents have officially confirmed their refusal to be vaccinated.
Strictly speaking, there are no mandatory vaccinations in Russia, even children without them are admitted to kindergartens, but only if their parents have officially confirmed their refusal to be vaccinated.
Immunization schedule - a list and schedule of vaccinations. Usually associated with the concept of mandatory vaccinations and the National Immunization Schedule, but can be used wherever it is required to describe the set and timing of vaccinations, for example, during revaccination.
The vaccination schedule is the same as the vaccination schedule.
Vaccination schedule - the same as the vaccination schedule.
Vaccination 2020 is a combination often found in search queries: people want to know which vaccinations are mandatory for the current year, and what changes have been made to the vaccination calendar.
Inoculation is the same as "inoculation". This is usually written in search queries by those who do not know the difference between a vaccine and an inoculation.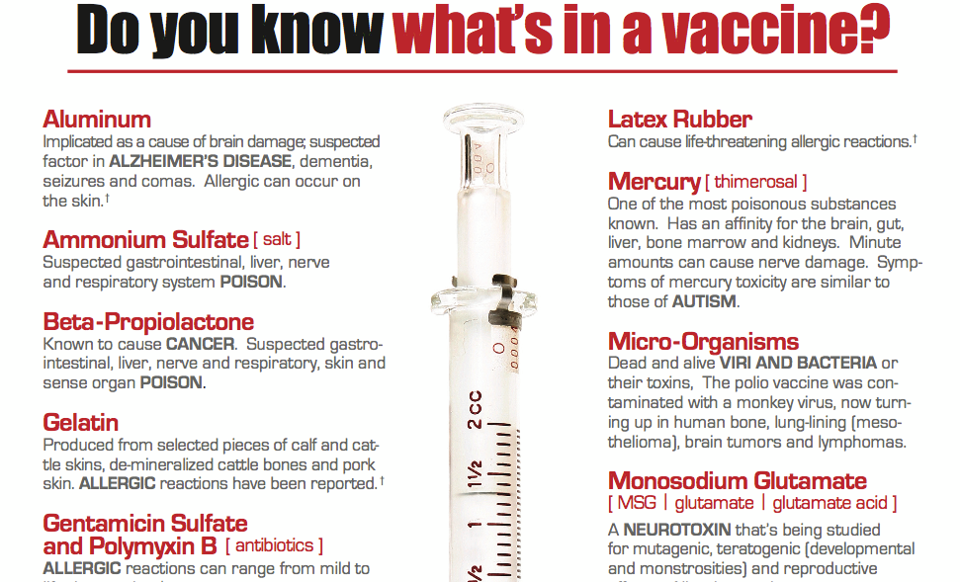
To be vaccinated or vaccinated - "to vaccinate" is a more medical term, an example of professional slang. In everyday life, the word "do" or "do" is usually used. In most cases, we will use the everyday option, but in some more "medical" articles, professional terms are not excluded.
Vaccination schedule - commonly used as a synonym for vaccination schedule.
Deciphering vaccinations - unlike analyzes, where deciphering is understood as the interpretation of their results, in vaccination it is deciphering the abbreviations of vaccines, for example, DTP.
Vaccination room - a place (room) where preventive and diagnostic vaccinations are given. Not to be confused with a treatment room, where other procedures, such as IVs, may be performed.
Live vaccines are one of the types of vaccines that contain weakened or killed infectious agents in the preparation. The classification of vaccines divides them into live, chemical, synthetic, inactivated (there is no single classification), but "live vaccines" are the most famous of them.
What is the difference between Russian COVID-19 vaccines
Russia is experiencing another wave of the coronavirus epidemic. The authorities and doctors unanimously say: only vaccination can stop this misfortune. Russia has created four drugs for the prevention of COVID-19, both using modern technologies and classic, time-tested ones. How they work and how they differ - Parlamentskaya Gazeta figured it out.
Pandemic Horrors
As of June 18, more than 17 thousand new infections were detected in the country, which was the maximum since the beginning of February, follows from the data of the operational headquarters. Most of the cases in Moscow - 9056 cases, this is an absolute record for the capital. Moscow Mayor Sergei Sobyanin announced on Channel One that herd immunity in the capital had dropped to 25 percent.
The fact that the lockdown in Russia threatens to repeat itself on an even larger scale is largely to blame for the inertia of Russians who are in no hurry to get vaccinated against the coronavirus. “For the formation of herd immunity, 50-70 percent of the population must be vaccinated. In the meantime, about 13-14 percent of us have been vaccinated, ”senator Vladimir Krugly, Honored Doctor of Russia, told Parliamentary Newspaper.
“For the formation of herd immunity, 50-70 percent of the population must be vaccinated. In the meantime, about 13-14 percent of us have been vaccinated, ”senator Vladimir Krugly, Honored Doctor of Russia, told Parliamentary Newspaper.
According to him, many people refuse vaccinations because of fears and fears that are not really justified. The main fear actively supported by anti-vaccine movements is that vaccines are little studied and may in the future affect important body functions, for example, cause infertility or disorders in the nervous system.
Such "horror stories" are not substantiated by anything, says Vladimir Krugly. He drew attention to the fact that all Russian vaccines were created using already known technologies: vector and whole-virion preparations have long been used in medicine to prevent other diseases. “If there were any dangerous consequences, everyone would have known about it for a long time,” he stressed.
“Therefore, one must cast aside all doubts and fears and get vaccinated. This is the only way we can stop the epidemic,” summed up Vladimir Krugly. Moreover, he added, there are four vaccines in Russia - they are free, absolutely available, and have proven their effectiveness and safety.
This is the only way we can stop the epidemic,” summed up Vladimir Krugly. Moreover, he added, there are four vaccines in Russia - they are free, absolutely available, and have proven their effectiveness and safety.
Parlamentskaya Gazeta explains how Russian vaccines work, how effective they are, and what contraindications and side effects they have.
Sputnik V (Gam-COVID-Wak)
Developer: Scientific Center. N.F. Gamaleya
Operating principle. Vector vaccine - developed on the platform of the human adenovirus vector. Adenovirus has long been known and studied; in its normal state, it causes respiratory diseases. A vector is an adenovirus devoid of a reproduction gene, that is, it does not pose any threat to the body. The vector is used as a "courier" - a gene is inserted into it that encodes the S-protein of the coronavirus. This element is also safe for humans, but thanks to it, the immune system learns to recognize a dangerous infection and defend itself against it, that is, to produce antibodies.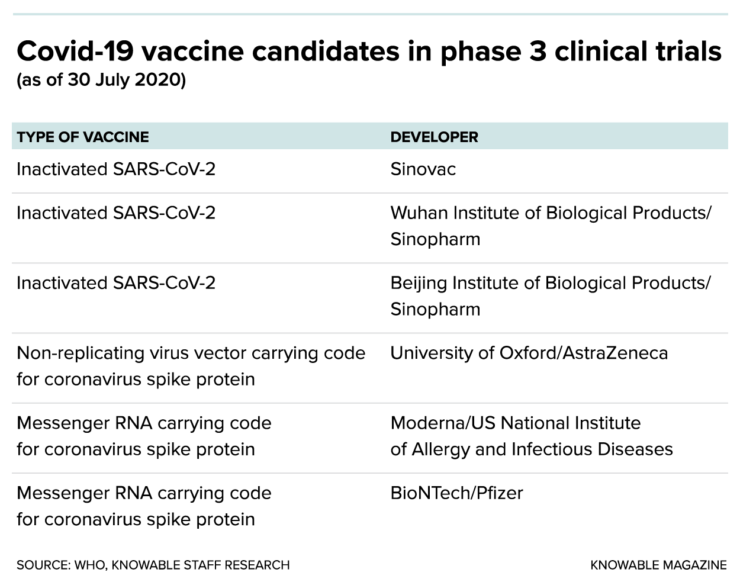
Adenovirus vectors have been used in medicine for over 50 years. Based on them, vaccines against influenza, the Ebola virus and other diseases were previously created.
Sputnik V is a two-component vaccine, each component contains vectors of different types of adenovirus. The first dose promotes the development of immunity. The second, which is administered after 21 days, boosts the immune response, providing long-term resistance to the coronavirus infection.
Recommended for people aged 18 to 60.
The vaccine is 91.6% effective. Vaccine developers expect that immunity will be formed for two years, but so far there is no exact data on this issue. The results of the vaccine studies have undergone a comparative international evaluation, the data are published in The Lancet.
Contraindications: hypersensitivity to vaccine components, severe allergic reactions in the past, acute illnesses, exacerbation of chronic diseases, pregnancy and lactation.
Side effects: chills, general weakness, fever, muscle and joint pain, malaise, flu-like condition, pain and swelling at the injection site; less often - nausea, indigestion, loss of appetite, swollen lymph nodes. The risk of serious side effects is one of the lowest at 0.27 percent. Allergic reactions and anaphylactic shock after the introduction of the vaccine were not detected.
Sputnik Light
Developer: Scientific Center. N.F. Gamalei
How it works. Single component vector vaccine. In composition, this is the first component of the Sputnik V drug, so the principle of its action is similar. But this does not make it an alternative to the first vaccine, the Ministry of Health noted. The "light" version is needed in order to ensure herd immunity in the shortest possible time at the peak moments of the pandemic. In addition, the Ministry of Health believes that Sputnik Light will be useful for revaccination and for vaccinating those who had coronavirus more than six months ago and their antibody titer has already decreased. The department also believes that this version of the vaccine is suitable for immunizing young people.
The department also believes that this version of the vaccine is suitable for immunizing young people.
This vaccine will be put into circulation in a week and a half, Minister of Health Mikhail Murashko announced on June 17.
Recommended for people aged 18 to 60.
The vaccine is 79.5 percent effective. The developers claim that it is effective against all new strains of coronavirus. The duration of protection is not yet known.
Contraindications: hypersensitivity to vaccine components, severe allergic reactions in the past, acute illnesses, exacerbation of chronic diseases, pregnancy and lactation.
Side effects: chills, flu-like condition, fever, general malaise, headache, muscle and joint pain, soreness and swelling at the injection site; sometimes - nausea, loss of appetite, swollen lymph nodes. Serious side effects after the administration of the drug were not registered.
EpiVacCoron
Developer: Scientific Center "Vector"
Operating principle.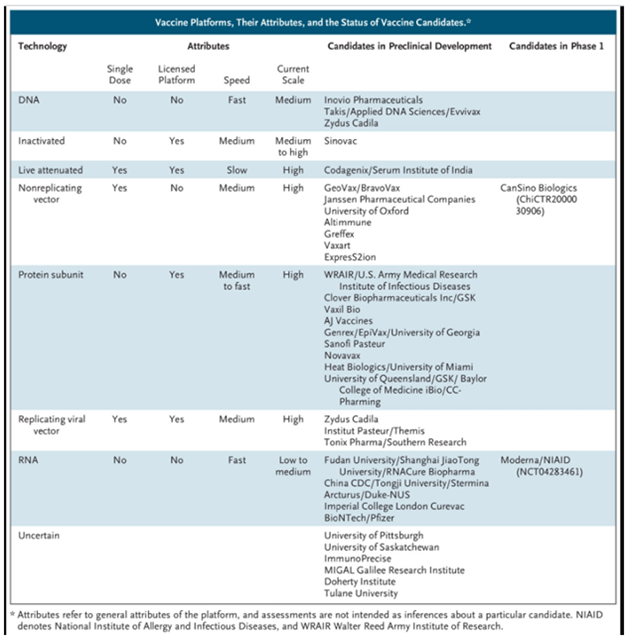 Vaccine based on peptide antigens. Peptides are artificially synthesized short fragments of viral proteins. They contribute to the production of antibodies against the proteins that are most important for the life cycle of the virus, while not burdening the body with the production of antibodies that play a lesser role in the fight against the disease. The vaccine is administered twice with an interval of two to three weeks.
Vaccine based on peptide antigens. Peptides are artificially synthesized short fragments of viral proteins. They contribute to the production of antibodies against the proteins that are most important for the life cycle of the virus, while not burdening the body with the production of antibodies that play a lesser role in the fight against the disease. The vaccine is administered twice with an interval of two to three weeks.
Recommended for people over the age of 18. The drug has passed successful clinical trials and is approved for vaccination of patients over 60 years of age.
The immunological efficacy of the vaccine, according to the results of the first two phases of clinical trials, was 100 percent. The duration of the vaccine's action is not yet known.
Contraindications: hypersensitivity to vaccine components, severe forms of allergic diseases, acute diseases, exacerbation of chronic diseases, pregnancy and lactation, primary immunodeficiency, oncology.
Side effects: transient fever, pain at the injection site. The vaccine is characterized by areactogenicity, that is, the absence of side effects that cause fever and allergic reactions.
KoviVac
Developer: Scientific Center named after. M.P. Chumakova
Operating principle. Whole virion vaccine, that is, it contains the whole virus, not its fragment. But it is deactivated - it is not capable of causing an infection, but it allows you to trigger an immune response and produce antibodies. The developers believe that the vaccine will be effective against all strains of coronavirus, but this requires research.
The drug is administered twice with an interval of 14 days. At the same time, older people may need a third dose, as they have a reduced immune response, said earlier the director of the Center. M.P. Chumakova Aidar Ishmukhametov. According to him, exact recommendations will be made after the completion of the third phase of clinical trials.