Baby has tiny red bumps on body
Common childhood rashes | Pregnancy Birth and Baby
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
Key facts
- There are many different types of childhood rashes. Many are not serious.
- If your child has a rash and fever, they should see their doctor.
- If your child has a meningococcal rash, go immediately to the emergency department.
Meningococcal rash
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
You can read more about serious childhood rashes here.
Rashes with no fever or itching
Milia (blocked oil glands)
Up to 1 in every 2 newborn babies develop small white spots called milia on their face, especially on the nose. These are just blocked pores, and they’re not itchy or contagious. They usually clear up without treatment within a few weeks.
Erythema toxicum
Many newborns develop a blotchy red skin reaction called erythema toxicum, which can appear between 2 days and 2 weeks after birth. Flat, red patches or small bumps often first appear on the face and spread to the body and limbs. The rash is harmless, not contagious, and will clear after a few days or a week.
Baby acne
Some babies get pimples on their cheeks and nose in the first three months of life. These pimples normally disappear without any treatment, usually within a few months.
Nappy rash
Nappy rash is inflammation of the skin in the nappy area. It can look red, sore and inflamed. Nappy rash is usually caused by urine (wee) or faeces (poo) irritating the skin.
To avoid nappy rash, keep the nappy area clean and dry with frequent nappy changes and nappy-free time. You can help protect the skin by putting on a barrier cream such as zinc or soft white paraffin at each nappy change.
Persistent nappy rash can be treated with a medicated cream. Don’t use talcum powder or antiseptics to treat nappy rash. If your baby develops a fungal infection, you’ll need to use an antifungal ointment. Ask your doctor or pharmacist for advice.
Erythema multiforme (minor)
Erythema multiforme is a rash triggered by an infection (most commonly herpes simplex virus), medicine or an illness. Your baby might feel unwell or have a mild fever before the rash appears. Red spots develop on the hands, feet, arms and legs and spread symmetrically across both sides of the body. The spots often become raised or blistered and then develop into classic target-like lesions.
Erythema multiforme is not contagious, and usually resolves without treatment in 3 to 6 weeks.
Keratosis pilaris (‘chicken skin’)
Keratosis pilaris is a harmless condition where the skin becomes rough and bumpy, as if permanently covered in goose pimples. These bumps most commonly occur on the upper arms and thighs. You can try several things to help the rash to clear up, including moisturising regularly.
You can try several things to help the rash to clear up, including moisturising regularly.
Rashes that might be itchy
Eczema (Atopic dermatitis)
Eczema is a very common skin condition affecting 1 in 3 Australians. It causes the skin to become itchy, red, dry and cracked, often in the creases at the knees and elbows.
Eczema commonly starts before a baby is 12 months old. Eczema follows a relapsing-remitting course. This means that there are flare-ups of the rash, followed by periods where there is no rash or a minimal rash.
Eczema management includes preventative treatment such as avoiding skin irritants, moisturising regularly and using bath oil. Treatment of flare-ups includes using steroid and anti-inflammatory creams.
Ringworm (tinea)
Ringworm is a common, contagious skin infection that causes a ring-like red rash with a clear centre. It commonly occurs on the scalp, feet and groin, but it can appear almost anywhere on the body.
Ringworm is caused by a fungus, not a worm, and is usually treated with over-the-counter antifungal creams. You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
Prickly heat (heat rash)
Heat rash might appear if your baby gets hot in a humid environment. The rash shows as tiny red bumps or blisters on the skin, which can be very itchy. Cooling your baby down and avoiding humidity is the best way to prevent heat rash, which usually clears within 2 to 3 days without treatment.
Impetigo (school sores)
Impetigo is a highly contagious bacterial infection of the skin. It causes red sores and blisters that form a yellow crust. It is very common in children aged 2 to 6, and it is not usually serious in this age group, but it can be dangerous for newborn babies.
If your child has impetigo, you should see your doctor, who might prescribe an antibiotic cream, ointment or tablet. This should clear the infection within 7 to 10 days. Keep your child home from childcare or school and away from young babies until the sores have dried up, usually a few days after treatment starts.
Hives (urticaria)
Hives is a raised, red, itchy rash. It is common on the chest, stomach and back, as well as the throat and limbs, but it can appear on any part of the body. Hives usually disappears within a few days without any treatment. Antihistamines can be given to relieve itching. If the rash doesn't go away, you should see your doctor.
Hives isn’t usually serious, but it can be a sign of a more serious allergic reaction (anaphylaxis). If your child develops hives after eating, or together with other symptoms such as vomiting, dizziness or trouble breathing, you should seek urgent medical attention.
If your child has symptoms of a serious allergic reaction (anaphylaxis), call triple zero (000) immediately and ask for an ambulance.
Pityriasis rosea
Pityriasis rosea is a mild skin rash that sometimes appears after a sore throat, cold or fever. It begins with a single pink or tan-coloured patch on the chest or back. Red, oval-shaped patches, which may be itchy, then appear on the chest or back and limbs over the next weeks.
The exact cause of pityriasis rosea is unclear, and it is not thought to be contagious. The rash usually clears up within a couple of months without treatment.
If you are pregnant, pityriasis rosea can in rare cases lead to complications. See your doctor if you are pregnant and have contact with a child who has pityriasis rosea.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that is spread by skin-to-skin contact or by sharing swimming pool water, bath water or towels.
Molluscum contagiosum spots look like pimples and grow into round pearly white lumps, usually 2 to 5 millimetres in size. They can be itchy. They usually heal without treatment within 6 months, but sometimes longer.
Rashes with fever
Slapped cheek disease (fifth disease)
Slapped cheek disease is a viral infection that mainly affects pre-school and school-age children. It typically causes a bright red rash on both cheeks that spreads as a ‘lacy’ rash on the body and limbs. Occasionally, it causes a fever.
Occasionally, it causes a fever.
Slapped cheek disease is usually mild and clears up in a few days without treatment. The child is contagious before the rash appears, but not once it has appeared.
If you are pregnant and catch the virus, it may cause a type of anaemia in your unborn baby. It can also cause miscarriage. If you suspect you or your child has slapped cheek disease, you should avoid contact with people who might be pregnant.
Hand, foot and mouth disease
Hand, foot and mouth disease is a mild but highly contagious viral illness. It causes a rash on the palms of the hands and soles of the feet and blisters in the mouth. It is not the same as the foot-and-mouth disease that affects farm animals.
The disease is common in childcare and kindergartens. Your child might feel unwell and have a fever and blisters on the hands and feet and in the mouth and in the nappy area. The illness usually lasts about 7 to 10 days. Children with hand, foot and mouth disease should stay away from childcare or school until all the blisters have dried up.
Hand, foot and mouth disease usually resolves on its own without complications. In rare cases, it can be more serious, especially if you have a weakened immune system or are pregnant. Complications can include infections of the brain and heart muscle and miscarriage.
Roseola infantum
Roseola infantum is a contagious viral infection that can cause cold-like symptoms and a high fever. The high fever may last for a few days. Roseola infantum can also cause some children to have a febrile convulsion (seizure).
Children with roseola infantum develop a rash after the fever has resolved. The rash looks like raised pink spots that start on the chest, stomach and back and spread to the limbs. The child is contagious before the rash appears, but not after. The rash usually lasts 3 to 5 days.
Febrile convulsions can look scary but are generally not harmful.
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
When to seek help
Many babies develop a skin rash in their first days or weeks of life as their sensitive skin adapts to a new environment. Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Whatever their age, you should take your child to the doctor if they have a rash and persistent high temperature, cold or cough symptoms or swollen neck glands.
Treatment of common childhood rashes
If you think your child might be contagious, they should stay at home. Keep them away from school, childcare and other children. You should also keep them away from people who are pregnant, or who might be pregnant, since some childhood infections can cause serious problems in unborn babies.
You can use paracetamol or ibuprofen (in babies aged over 3 months) to reduce fever — read the packet instructions carefully to ensure your child receives the right amount for their age and weight.
Your pharmacist can advise you on treating the symptoms of common rashes. For example, you can use over-the-counter creams to prevent itchiness.
If you are concerned about your child’s rash, call Pregnancy, Birth and Baby on 1800 882 436 to talk to a maternal child health nurse, or call Healthdirect on 1800 022 022 to talk to a registered nurse. Alternatively, contact your doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
17 Most Common Types of Baby Rashes (With Pictures)
Are small red bumps popping up on your baby’s body? There are many possible reasons for baby rashes, so it can be difficult to know what causes them.
Chances are, it’s something completely harmless that will resolve itself within a few days. But it’s still important to keep an eye on any rashes that pop up on your little one.
Our medical team will give you the lowdown on the 17 most common types of baby rashes to help you identify those bumps and set your mind at ease.
Table of Contents
- 1. Baby Acne
- 2. Cradle Cap
- 3. Erythema Toxicum Neonatorum (ETN)
- 4. Atopic Eczema
- 5. Hives
- 6. Diaper Rash
- 7. Milia
- 8. Impetigo
- 9. Fifth Disease
- 10. Hand, Foot, and Mouth Disease
- 11. Measles
- 12. Miliaria
- 13. Scabies
- 14. Ringworm
- 15. Meningitis
- 16. Chickenpox
- 17. Molluscum Contagiosum
- When to Worry About a Rash
- Make a Rash Decision
1. Baby Acne
This rash is nothing to worry about. Most babies have experienced it. It usually shows up within the first couple of weeks of a baby’s life and can last from several days to several months (1).
Causes
Doctors are still not entirely sure why some babies develop acne. But it may be caused by the maternal hormones your baby is exposed to in the womb.
Symptoms
Baby acne is distinguished by tiny red or white pimples on a baby’s cheeks, nose, forehead, and chin. Basically, they look like a tiny teenager going through puberty.
Basically, they look like a tiny teenager going through puberty.
Treatment
The best way to get rid of baby pimples is to keep your baby’s skin clean. Gently wipe the area using soft materials like cotton balls or gentle washcloths.
Moisturizing the skin is essential, so try a mild baby lotion or baby oil. But don’t use too much since this could block the pores and worsen the acne. Most baby acne goes away on its own.
Your baby may need treatment for moderate to severe acne to prevent scarring. Never buy any over-the-counter acne treatment creams intended for teens or adults. These are not safe for newborns. Consult your pediatrician to find the appropriate treatment for the baby acne.
If the acne does not go away on its own, or if it worsens despite treatment, talk to your doctor immediately. Your baby may have a hormonal imbalance issue or other causes of rashes that would warrant a medical exam.
2. Cradle Cap
Cradle cap is easy to recognize and common in newborns. It results in greasy yellow or brown scales at the top of the baby’s head. In some cases, it will move down to the face or neck.
It usually develops within the first two or three months. Cradle cap is not contagious (2).
Causes
Nobody is 100% sure what causes cradle cap. However, it is linked to two common factors:
- Fungus: Some babies react to Malassezia, a fungus naturally found on the skin.
- High sebum levels in the affected area: Sebum is an oily substance consisting of fat, keratin, and cellular debris.
Symptoms
Cradle cap won’t cause fever or discomfort for your baby. However, it can cause large flakes to develop. As the scales fall off, you might notice a few hair strands following.
The skin around the scales can become red, and you might notice a smell in severe cases. I find it similar to the aroma of unwashed hair.
I find it similar to the aroma of unwashed hair.
Treatment
Cradle cap will often clear up on its own within a few weeks, although you can help to get rid of it faster. Treating cradle cap is relatively easy:
- Wash your baby’s hair: Using a mild shampoo, lather your baby’s head, and let the shampoo sit for a minute. Then brush the hair with a soft brush before rinsing.
- Apply baby oil: Baby oil or coconut oil will loosen the scales. Brush your baby’s hair with a soft brush to remove loose flakes.
- Soak overnight: Apply Vaseline, olive oil, coconut oil, or vegetable oil, and let it soak overnight. The following morning, wash your baby’s hair with a mild shampoo and rinse.
- Steroid cream and antifungal shampoo: In more severe cases, your physician may prescribe a low-potency steroid and antifungal cream to alleviate cradle cap.
There are special cradle cap shampoos available. These soften the scales quickly, making them easy to remove. The shampoo also prevents new scales from forming.
These soften the scales quickly, making them easy to remove. The shampoo also prevents new scales from forming.
You should never pick at the scales, although I know it can be very tempting. Removing them from the scalp in this way could result in an infection.
3. Erythema Toxicum Neonatorum (ETN)
ETN is a widespread rash that occurs within the first few days of a newborn’s life. It’s most common in full-term babies.
ETN appears as blotchy red bumps that can sometimes look pale and raised due to fluid buildup. If the fluid looks like pus, this can indicate an infection. But in most cases, it’s only a bodily fluid (3).
Causes
The cause of ETN is unknown but is thought to be related to immune system development.
Symptoms
ETN symptoms include a red rash with bumps that sometimes look white or yellow. It shouldn’t cause any discomfort or fever.
It shouldn’t cause any discomfort or fever.
This rash most commonly appears on the baby’s chest, neck, and face. It can develop anywhere except the palms and soles.
Treatment
There is no treatment necessary. However, if it becomes more severe, you should consult your doctor for advice.
4. Atopic Eczema
Eczema can be extremely uncomfortable as the affected area becomes red, itchy, and even cracked.
It could be a long-term, chronic condition that requires extensive treatment. However, it often clears over time as your little one grows (4).
Causes
Atopic eczema can be passed down by your parents. If you suffer from it or have previously, your newborn might also develop the condition.
If your baby is born with an increased risk, keep them away from specific triggers such as these:
- Soaps and detergents: Don’t use scented detergents or soaps. Make sure all soap residue is rinsed off your baby after a bath.

- Allergens: These could be cold, dry weather or a humid environment. Even dust mites, fur, pollen, mold, heat, sweat, and certain foods can cause an allergy.
- Certain fabrics: Wool and synthetic materials are known to trigger eczema.
Symptoms
The affected area will become red, dry, itchy, cracked, and sore. This could result in bleeding skin and inflammation, and secondary infections may occur.
The areas of skin affected might become darker or lighter after eczema has cleared, although this is only temporary.
Treatment
Keeping the skin hydrated is the best way to avoid a rash. Moisturizers, steroids, or eczema creams can help alleviate this. Consult your pediatrician for creams or ointments to help ease the symptoms.
Covering up the area with bandages might be necessary in some instances. However, damaging the skin could cause more eczema.
You may want to consider putting mittens on your baby. Newborns aren’t coordinated enough to scratch, but they might do some accidental damage. I had some great sleepsuits with integrated foldover mitts and found these worked much better than the loose mittens, which quickly fell off.
Newborns aren’t coordinated enough to scratch, but they might do some accidental damage. I had some great sleepsuits with integrated foldover mitts and found these worked much better than the loose mittens, which quickly fell off.
5. Hives
People of all ages can develop hives. The rash features red raised patches or bright red spots.
Hives can appear anywhere on the body. They’re often extremely itchy and are sometimes accompanied by a stinging or burning sensation (5).
Causes
When hives occur, it is because the body has been in contact with a trigger. This could be allergens, such as certain foods, pollen, latex, medications, or insect bites. Infections can also trigger hives.
The trigger causes the body to release histamines. These carry white blood cells to the affected area, which will repair the damage and eliminate the intruder (the trigger). The histamines cause swelling, redness, and itchiness.
Symptoms
The rash will be made up of swollen, red welts of different sizes. They will be well-defined with a pale center and red surrounding it (similar to mosquito bites but usually bigger).
They will be well-defined with a pale center and red surrounding it (similar to mosquito bites but usually bigger).
Hives can easily spread across the skin in different areas. They can last a few hours, days, or, on rare occasions, weeks.
Treatment
Antihistamines, such as Benadryl, are the best treatment for hives. However, you should never give your baby any medication without consulting a pediatrician first.
If your baby doesn’t seem too bothered by the rash and the size of it isn’t concerning, don’t worry. It should ease and disappear within a day or two.
You can always try different methods to ease the irritation. Wet a washcloth in water, similar to the temperature of a bath, and gently apply it to the affected area.
6. Diaper Rash
A diaper rash is something nearly all parents have to deal with at some point in their child’s life. The rash can be mild, with only a few red spots in one area. More severe rashes will look red and tender (6).
Causes
The leading cause of a diaper rash is prolonged exposure to urine or poop. Here are some other possible causes:
- Disposable diapers: These can sometimes contain chemicals or fragrances which might be causing the reaction.
- Fungal or yeast infection: Bacterias thrive in warm, moist environments, so they often cause rashes in the folds within the diaper area.
- Food: As your baby starts to have solid foods, their stools will change. Acidic foods are known to cause diaper rash in some babies.
- Antibiotics: These will increase the chance of a yeast infection.
Symptoms
The diaper area will be red, a little swollen, and warm to the touch. The rash can spread to the baby’s thighs, stomach, and back.
Some babies will seem troubled by it and uncomfortable during diaper changes. Older children may be holding themselves because it’s painful to pee.
Treatment and Prevention
A diaper rash can be difficult to deal with. But don’t worry, there are many effective ways to treat and prevent it:
But don’t worry, there are many effective ways to treat and prevent it:
- Keep the area dry and clean: Change your baby’s diaper frequently. Gently pat the area dry — never rub!
- Apply ointment or cream: Diaper rash ointments or creams will treat the area and create a barrier on the skin to protect it.
- Loosen the diaper: A good tip is to use a bigger diaper, as this allows for more airflow. You can even leave your baby without the diaper, but make sure to waterproof the surrounding area, particularly if you have a boy!
Cloth diapers are a great option and good for the environment. They need more work since you have to wash them. But they eliminate all the possible chemicals and harsh edges on disposable diapers.
My little one loves cloth diapers as they are softer than disposables. Just remember to wash them in fragrance-free detergent, and never use fabric softeners or dryer sheets.
7.
 Milia
MiliaMilia is common among newborn babies. It looks like tiny white spots that usually form around a baby’s nose (7).
Causes
Milia is entirely harmless. It is the result of the baby’s pores being blocked by dead skin cells.
Symptoms
Small white bumps will appear on a baby’s face and sometimes even on the limbs or the upper body. They can also appear on the roof of the baby’s mouth or on their gums, looking like little teeth coming through. The spots shouldn’t be itchy or painful.
Treatment
The spots will usually clear up on their own within the first four weeks after birth. Never try to squeeze them.
8. Impetigo
Impetigo is a highly contagious infection that causes blisters and sores. Babies and adults can get it, though it’s most common in young children aged 2 to 6 years old. For newborns, it can be dangerous.
The sores and blisters grow quickly and then burst, leaving golden, crusty patches. These may grow and spread to other parts of the body. The patches can also be itchy and painful (8).
These may grow and spread to other parts of the body. The patches can also be itchy and painful (8).
Causes
The rash occurs when bacteria enters the skin — this could be through a cut or a sore. If someone with impetigo comes into contact with your baby, there is a high risk of it being passed on.
Symptoms
Impetigo usually starts as a cluster of red blisters. These will grow, burst, ooze, and then spread. The rash is itchy, which increases the spreading.
The skin in the affected area will be red, and the lymph nodes may also become swollen.
Treatment
Mild cases of impetigo won’t require much treatment. By keeping the area clean, it should clear itself up.
A pediatrician might prescribe antibiotics to help your baby’s body fight off the bacteria. Depending on the child’s age, this could be given orally or as a cream.
Trim your baby’s nails and keep them clean to prevent the bacteria from spreading. Wash the scabs gently, twice a day, using warm water and soap. Dry with a towel that is only used for your baby.
Dry with a towel that is only used for your baby.
9. Fifth Disease
Fifth disease, also known as slapped cheek syndrome or parvovirus B19, takes its unique name from how it looks. Any guesses on what it looks like?
It starts as small red patches on the child’s cheeks. It is most common in preschoolers, but babies can also contract the virus, and pregnant mothers can pass it on to their babies.
It’s highly contagious but not harmful. After recovery, most people develop an immunity to the virus (9).
Causes
The cause of fifth disease is the same as most other viruses. If your baby is in contact with another person carrying the virus, they are at risk.
Symptoms
Apart from the red cheeks, there are a few other symptoms you might notice:
- Fever before the rash appears.
- Stuffy or runny nose.
- Sore throat.
- Upset stomach.
- Headache.
- Fatigue.
- Anemia (lack of red blood cells).

The rash can be itchy and will start on the face, but it can also appear on the arms, legs, and buttocks.
Treatment
You should treat fifth disease like any other cold. Your child will need rest and lots of fluids. However, you should always see your pediatrician when a rash occurs. Though harmless, it’s best to rule out other diseases. In rare instances when anemia becomes severe, further medical interventions such as blood transfusion may be warranted.
10. Hand, Foot, and Mouth Disease
Hand, foot, and mouth disease (HFMD) is another widespread viral disease most common in those under 5 years of age.
The child will begin to develop sores around and inside the mouth. You might find them on the tongue, back of the mouth, or inside of the cheeks (10).
Causes
HFMD is due to the infection commonly caused by a coxsackie virus and is highly contagious. It will spread through sneezes, coughs, stool, and fluid from sores and blisters.
Like any other viral infection, children often pass it on to each other.
Symptoms
There are a few symptoms you might notice before the rash begins. These include the following:
- Fever.
- Loss of appetite.
- Sore throat.
- Fatigue.
After the fever starts, usually within a few days, the first sores or blisters will appear on the hands, feet, or mouth.
These can be extremely painful. Older children will surely complain, while younger children and babies will seem super irritated (because they can’t complain).
Sometimes, the rash appears on the buttocks as well.
Treatment
Mild cases only need observation. Make sure to check your baby’s temperature often. They should drink and eat plenty to give the body strength. However, more severe cases require doctor visits and hospitalization.
Your baby might be miserable, so comfort them as much as possible. Treat them with cold drinks or ice cream, which can ease the discomfort. Never give salty, spicy, or acidic foods.
Never give salty, spicy, or acidic foods.
11. Measles
Measles is another viral infection similar to fifth disease. It starts as small red bumps with white dots inside the cheeks, followed by a fever.
A rash will quickly appear and spread from the face down the back and torso, making its way to the arms and legs.
The rash will look like red patches at first, but it will soon develop into itchy raised bumps. Measles is most likely to occur in unvaccinated children (11).
Causes
Measles is highly contagious and is caused by a virus called paramyxovirus. When a person carrying the virus sneezes or coughs, the virus will spread. The droplets containing the virus stay active for up to two hours outside the body.
The United States was considered measles-free in the year 2000. But it has been appearing again mainly because some parents choose not to vaccinate their children (12).
Symptoms
As the first few bumps begin appearing, you might also notice these symptoms:
- Red and runny nose.

- Low energy levels.
- Loss of appetite.
- Nausea and vomiting.
- Diarrhea.
- Swollen lymph nodes.
Treatment
It is critical you contact a doctor immediately if you suspect your child has measles.
Once confirmed, it is crucial to keep your child away from others to prevent the disease from spreading.
Some studies have demonstrated that vitamin A and antiviral agent ribavirin can play roles in the recovery process (13).
Ensure your little one is as comfortable as possible and watch closely for signs of a fever. Measles can cause the temperature to rise to 105 degrees Fahrenheit, which is dangerous.
Talk with your doctor if your child hasn’t been vaccinated yet and is exposed to the virus. They can give an immune globulin injection, which may prevent or ease the symptoms.
The MMR vaccine is usually scheduled at the age of 12 to 15 months, with a booster vaccine at 4 to 6 years.
12. Miliaria
Miliaria, also called sweat rash, prickly heat, or heat rash, usually occurs if your baby has been sweating excessively. It normally occurs in hot, humid conditions (14).
It normally occurs in hot, humid conditions (14).
Causes
If you live in a hot environment, your baby might sweat quite a lot. The sweat glands can become blocked, resulting in a rash. This can also happen if your baby is dressed too warmly or if they are in an overly hot room, such as a room with a fireplace that has been burning all day.
Symptoms
The rash looks like tiny red bumps or blisters, as sweat is trapped under the skin. There will be a lack of sweat in the affected area, and your baby will experience a prickly feeling.
Treatment
Miliaria doesn’t require any treatment since it usually goes away on its own once your baby cools down. Moving your baby to a cooler environment helps. If the rash takes a little longer to clear, your pediatrician might recommend a cream or ointment.
13. Scabies
Scabies is an infestation of the skin. People of all ages can become infected. A baby with scabies will develop small, red spots all over the body (15).
Causes
Scabies is caused by tiny parasitic mites which burrow into the skin. (Eww!) It most often makes its way to your baby with the help of friends or other family members.
Symptoms
The rash will feature little bumps that can form a line. There will be extreme itchiness that is worse at night with potential sores and crusty areas. Scabies usually occurs on hands and arms but can develop anywhere on a baby’s skin.
Treatment
It’s necessary to contact your doctor and obtain treatment that will kill the mites. However, it’s not enough to only treat your child; it’s crucial to treat everyone who might also be infected. Some people choose to treat the whole house.
14. Ringworm
Ringworm is a common fungal infection. It causes a unique red rash in the form of a ring. Ringworm can develop anywhere on the body.
In babies, it is most often seen on the scalp, feet, and groin area (16).
Causes
Ringworm is actually caused by fungi — not a worm! It spreads as people come into contact with others who are infected — humans or animals. The fungi may also be present on bedsheets, towels, and even combs.
The fungi may also be present on bedsheets, towels, and even combs.
Symptoms
The rash will have round patches that are red or silver. It may be dry, scaly, itchy, and swollen. You might also notice blister-like lesions or some hair loss if the rash appears on the scalp.
Treatment
An antifungal cream, gel, or spray is an effective method. It’s essential to finish the whole course of treatment to make sure the infection is completely cleared.
15. Meningitis
Meningitis is a severe condition that affects the protective membranes surrounding the spinal cord and brain.
While meningitis can affect anyone, it’s most common in babies and children. The infection should be treated immediately. It could develop into life-threatening blood poisoning, called septicemia, which can lead to permanent brain and nerve damage.
Vaccines are available to protect against some forms of meningitis (17).
Causes
A viral or bacterial infection can cause meningitis. Viral infections are the most common cause, including the following :
Viral infections are the most common cause, including the following :
- Enteroviruses.
- Influenza.
- Herpes simplex viruses.
- Varicella-zoster virus.
- Measles and mumps.
- Haemophilus influenza type b (Hib).
- Group B Streptococcus.
- E. coli.
- Streptococcus pneumoniae.
- Listeria monocytogenes.
- Neisseria meningitis.
Symptoms
A patchy rash with lots of small red spots gathered in one area is the first sign. One way to tell if it’s a meningitis rash is by pressing a glass over it. If the rash doesn’t fade, it could be meningitis.
These are some other symptoms of meningitis:
- Fever of 100.4 degrees Fahrenheit or above.
- Lack of energy or extreme sleepiness.
- Rapid breathing.
- Cold hands and feet.
- Pale skin.
- A stiff neck and body.
- Swelling of the fontanelle (the soft spot on a baby’s head).
- Drowsiness or unresponsiveness.

- Seizures.
- Refusing to feed.
- Not wanting to be picked up.
- Unusual high-pitched cry.
- Shivering.
Treatment
If there are any signs of meningitis, it is vital you get your baby to a hospital immediately. This is a medical emergency.
Antibiotics may be given and fluids to treat dehydration. Some cases require steroid medication to reduce swelling around the brain.
Treatment in the hospital can take anywhere from a few days to several weeks. Your baby might also need some aftercare once home again.
16. Chickenpox
Chickenpox is a rash due to the varicella-zoster virus (VZV) infection. The baby may first show flu-like symptoms before developing a rash, which appears as red, itchy spots over the body.
Babies are especially susceptible to chickenpox infection because they cannot get immunization until the age of one year old. Fortunately, the incidence of chickenpox has declined by 90% since 1995 with the introduction of the varicella vaccine. Since the prevalence of chickenpox decreased drastically in the general population, there are fewer carriers who can pass the disease on to infants, a phenomenon called “herd immunity” (18).
Since the prevalence of chickenpox decreased drastically in the general population, there are fewer carriers who can pass the disease on to infants, a phenomenon called “herd immunity” (18).
Causes
VZV infection occurs through viral transmission similar to that of measles. When a person coughs or sneezes, the air droplets containing the virus can spread to unvaccinated babies, leading to chickenpox. Transmission can also occur through physical contact with those who have a chickenpox rash. Vertical transmission can also occur when an infected pregnant mother transmits the virus directly to the fetus.
Symptoms
Flu-like symptoms can occur in infants infected with chickenpox days before the development of the rash. The flu-like symptoms include:
- Fever.
- Cough.
- Poor feeding.
- Fussiness.
- Fatigue.
- Sleepiness.
The rash starts at the torso and the head, then spreads to limbs over several days. The rash starts as itchy, red bumps, which later become fluid-filled blisters. The blisters burst to become open sores that scab over and heal. This whole process can last from five days to two weeks.
The rash starts as itchy, red bumps, which later become fluid-filled blisters. The blisters burst to become open sores that scab over and heal. This whole process can last from five days to two weeks.
Treatment
You should notify your pediatrician immediately if you suspect your baby has a chickenpox infection, even if the symptoms are mild. You should also let your physician know right away if your baby develops any of the following symptoms:
- High fever.
- Rash on the eyelid or around the eyes.
- Stiff neck.
- Vomiting.
- Severe cough.
- Difficulty breathing.
- Extreme sleepiness or difficulty waking up.
- Rash that has become warm and swollen.
Treatment of chickenpox is usually supportive. However, in more severe cases of chickenpox, or if a baby is born with chickenpox (congenital chickenpox) due to an infected mother, the physician may prescribe an antiviral agent called acyclovir.
To prevent chickenpox from infecting an unvaccinated baby, avoid contact with anyone who is infected with chickenpox.
17. Molluscum Contagiosum
Molluscum contagiosum is another viral infection that causes rashes in babies. The rashes consist of small pink bumps with indented centers. Molluscum contagiosum can occur anywhere on a baby’s body, but it is most commonly found on the head, neck, torso, and armpits.
Causes
The rash is caused by an infection with the molluscum contagiosum virus (MCV). Babies can get molluscum contagiosum rashes in a couple of ways, such as direct skin-to-skin contact with someone who has molluscum contagiosum or contact with objects, such as toys or towels, that have MCV on them.
Most of the time, the only symptom of MCV infection is the rash. The rash appears like pink, skin-colored dome-shaped bumps with central indentations. They can appear anywhere on the body except the palms of the hands, the soles of the feet, and very rarely on the oral mucosa. The bumps can occur in isolations or in groups.
Treatment
Treatment is optional, especially in immunocompetent infants and children, since MCV rashes usually go away on their own within 18 months. Some doctors may use a variety of methods such as freezing the bumps (cryotherapy), removal via sharp instruments (curettage), or application of wart removing chemicals or creams. However, many doctors prefer not to use these methods because they can cause burns and skin scarring.
Some doctors may use a variety of methods such as freezing the bumps (cryotherapy), removal via sharp instruments (curettage), or application of wart removing chemicals or creams. However, many doctors prefer not to use these methods because they can cause burns and skin scarring.
Since molluscum contagiosum can spread from one part of the body to another through contact, it is wise to cover up the areas of rash with small, watertight bandages. Caretakers should also wash their hands often to prevent the spread of the MCV.
When to Worry About a Rash
Babies have sensitive skin, so even the most minor thing can cause a reaction.
Most rashes are harmless and will improve or disappear within a few days. Always contact your pediatrician if a rash looks suspicious or is accompanied by a fever.
Rashes can sometimes be caused by an allergic reaction. With this comes the risk of anaphylactic shock.
These are some of the symptoms of a severe allergic reaction:
- Difficulty breathing.

- Hard for baby to feed or swallow.
- Baby is lethargic.
- Vomiting.
- Increased heart rate.
- Any swelling in the face, around the mouth or throat (19).
Make a Rash Decision
Always take good care of your baby’s precious skin. Don’t bathe your child too frequently using soap. Instead, choose a gentle cleaning product that is unperfumed and moisturizing. End the bath with a lotion or oil massage — this is when you can get a good look at your child’s skin and spot anything out of the ordinary.
Most rashes that appear in newborns are harmless. ETN, baby acne, and heat rash are the most common.
Knowing what to look for should help to ease your mind or let you know when to take action. If you’re ever unsure of a rash and what could be causing it, don’t hesitate to contact your child’s pediatrician.
Feedback: Was This Article Helpful?
Thank You For Your Feedback!
Thank You For Your Feedback!
What Did You Like?
What Went Wrong?
Skin rash in a child causes and diagnostic rules
From the condition of the skin, you can determine whether the function of the body is impaired. The rash varies in small red, intermittent, patchy, colorless, watery, vacant, itchy, knots and nodules. Children's rashes are much more common than adults. Basically, this is due to the influence of external factors (sunlight, temperature, humidity, harmful substances, chemicals, etc.) on the skin. The skin is also affected by the body's process and disease.
The rash varies in small red, intermittent, patchy, colorless, watery, vacant, itchy, knots and nodules. Children's rashes are much more common than adults. Basically, this is due to the influence of external factors (sunlight, temperature, humidity, harmful substances, chemicals, etc.) on the skin. The skin is also affected by the body's process and disease.
If you have a baby rash, you should consult a pediatric dermatologist. The First Children's Medical Center provides competent pediatric dermatologist services in Saratov. Here you can not only get your doctor's advice, but also take all the necessary tests and hear the opinions of related experts. By contacting a doctor in a timely manner, you can find the cause of the rash, remove it and eliminate the risk of recurrence and complications.
Causes of rashes
The reason for this is physiological, which is accompanied by a natural reaction to the body's process. In addition, the background may have a pathological cause.
- Disability and parasites.
- Chemicals, harmful substances
- Metabolism; toxic substances, toxic substances, chemicals, toxic substances, toxic substances, etc.
- Specific vitamins: toxic substances, chemicals, toxic substances, toxic substances and other substances.
- Antibacterial agent; poison; poison; poison; poison;
- Gastrointestinal and renal functional disorders.
- External factors, internal factors
So we can conclude that baby rashes don't come out without a reason.
From a parent's point of view, every breakthrough looks almost the same. However, it can distinguish the first primary rash, and not the primary rash or near the primary rash can be distinguished over time.
Types of rashes
Various childhood diseases appear as a combination of primary and secondary symptoms. The primary rash is different. It is important for parents to respond quickly and confirm the formation formed in the child's body.
- The bumpy details of these rashes are all deep in the dermis, in other words, the rash is not a surface. There is no cavity, it looks a bit like tuberculosis, and the color of the skin may change to red or purple.
- Blister (blister). Therefore, people name most of the things that can be done on the skin. However, the blisters are actually pink rounded shapes and there are no cavities or contents. True blisters are short, last for a few minutes to a few hours, and then disappear without a trace. For example, there is a burning.
- Water blister rash. This rash is also called nodularity because the appearance is similar to nodules with different skin colors and undertones. Papules are superficial and deep, and papules may disappear without a trace.
- Water blister rash. This rash looks like a blister on the skin. In some cases, a colorless or bloody serum may be hidden. COSS integrate alone or merge to form many rooms. Open blisters are the same size as the bottom of the blisters and leave skin on skin.

- Pompholygous (with two sexes). This type of rash also appears in the form of a whistle, but it is characterized by a more impressive size, 5 mm or more in diameter, compared to a small whistle. Such blisters may contain mucus or serum content as small whirlpools.
- Tonu pustules are eruptions of abscesses. From superficial to deep skin. The opening of superficial pustules passes without a trace. Opened medium-deep pustules (boils, carbuncles) can cause severe scarring and scarring.
- Rash on the body. This type of rash does not appear on the surface of the skin, but is characterized by a change in the shade of some parts of the body. Such rashes are vascular or petrifying.
- Roseola is the name given to a rash that occurs in many infectious conditions. All elements of a pink or moderately reduced rash. The structure of roseola resembles spots. When stretched or pressed on the skin, the rash turns pale and disappears for a while.
- hemorrhagic rash.
 This type of rash appears as red blood that forms at the sites of ruptured blood vessels. Stretching the skin does not stop the bleeding.
This type of rash appears as red blood that forms at the sites of ruptured blood vessels. Stretching the skin does not stop the bleeding.
The appearance of the secondary rash is also different. Represents a bench, with the transformation of elements of the primary rash (usually blisters or pustules) into crusts after opening. Growth is often seen as secondary symptoms such as fissures, erosions, abrasions of epithelial cells, abrasions, scars and ulcers.
Where a skin rash can appear
A small, red rash is a type of rash that is more common in children of all ages, especially in early childhood, kindergarten, and high school.
On the hairline, face, armpits, shoulders, abdomen, back, buttocks, groin and groin, small, non-dominant rashes can be seen. Such rashes are caused by allergies (food, drug, cosmetic). It can also be the result of overheating or non-compliance with sanitary rules. This leads to chafing and knocking. In one-year-olds, the rash may cover the head as the skin regulates body temperature.
The skin on the face may be covered with red rashes in some viral diseases. A child may develop a rash on his face if he does not receive suspicious new foods or medicines and does not change his lifestyle. In this case, it is necessary to take a temperature measurement and contact a pediatrician.
Red rashes of various sizes and types may appear on the hands and feet of children due to viral or bacterial infections, red fever, measles or leukemia.
Colorless rashes become more visible over time and are much more difficult to detect. Often these types of rashes indicate the early stages of allergy development. An almost invisible rash that is colorless or very pale may cover the body and be rough to the touch. It resembles a gooseberry, runs over the skin during chills and chills. Eruptions occur close to each other and can be huge.
A watery rash is a clear sign of infections, allergies, insect bites, and sunburn.
These areas may develop blisters filled with fluid.
- On the face (orbital triangle, lips, nose).
- For ribs, limbs, genitals, groin, inner waist, etc.
- near the anus.
In this case, the development of an infection originating from blisters or herpes is suspected. In much the same way, allergic reactions to the use of skin care products, in contact with chemicals and toxins, have caused local reactions resembling chemical burns.
Due to prolonged exposure to the sun, foamy rashes on the skin can turn red, causing the skin to turn red and slightly swollen.
When blisters appear on the skin of the hands and feet, "dyshidrosis" is possible, which is a blockage of the sweat glands. Blisters on the palms and heels are caused by the development of a fungal disease.
Purulent rash
Purulent rash is characteristic of bacterial infections. Such diseases most often develop under the influence of Staphylococcus aureus. It may also be due to the impact on the body of epidermal staphylococcus aureus, streptococcus and other microorganisms.
Such rashes can appear microscopically on the skin, wounds, wounds, which facilitates the penetration of internal microorganisms. Also, if the rash initially itches and itches and the baby begins to comb it, it becomes infected with bacteria and pustules appear.
Pustules on the knees and elbows in childhood can occur as a result of frequent falls and frequent skin injuries. The formation of a deep abscess is called a pyometra.
What parents need to do
To assess this condition, the parent should examine the child's skin and remove clothing. It is necessary to determine the nature of the rash (vesicles, opacities, papules, etc.) and the area. It is necessary to remember and analyze the state before the rash appears.
You will then have your temperature taken, your neck and tonsils examined, and other signs checked. You need to decide whether to call a doctor at home or visit a medical facility yourself.
What not to do when a rash appears
- Compression of pustules.

- Comb the rash.
- Self processing -.
- opening blister
- Since the application on fair skin complicates the diagnostic measures.
Do not forget that there are infectious diseases with rashes. In this regard, you should refrain from visiting the clinic with your child, as you can infect someone else in the hope that your turn will come. In such cases, it is recommended to call a doctor at home.
Diagnosis of the disease
Before treating a rash, it is important to find out the real cause of the rash. The choice of treatment depends on what caused the rash.
This is a diagnosis.
- are removed from the skin.
- Accumulation of fluid contained in vesicles and pustules.
- Get blood, stool and urine tests.
If necessary, you can visit a specialist nearby, such as a pediatrician, allergist, infectious disease specialist or gastroenterologist.
The treatment of rashes does not consist only of local treatment. To fix the problem, complex treatment is usually required. The main goal is to change the baby's habitat, revise the menu, take medicine.
To fix the problem, complex treatment is usually required. The main goal is to change the baby's habitat, revise the menu, take medicine.
Pediatric Dermatology Treatment
If a rash develops on a child's skin, it is important not to treat it alone, as treatment may worsen symptoms. If you have modulated your child's skin, you need to ask your child's dermatologist for help.
The pediatrician at the pediatric medical center will be diagnosed with the latest research methods. As a result of the test, if it is found that the skin disease is a symptom of other diseases, dermatologists consult, treat and treat them with the help of relevant specialists (digestive, allergic department, endocrinology, gynecology, surgery, etc.). request.
Reservations for pediatric dermatologists in Saratov are accepted from 8.00 to 20.00 at the first DMC by calling (8452) 244-000. Reception will be made in advance.
Food allergy is called a pathological reaction of the body to food ingredients. In this article, pediatrician Olga Nikolaevna Trekteteva explains in detail the symptoms of an allergy to a newborn and treatment.
In this article, pediatrician Olga Nikolaevna Trekteteva explains in detail the symptoms of an allergy to a newborn and treatment.
Children's food allergies are said to be around 10%. This is quite a large percentage, and the increase was recently increased. It is not unusual for a mother who complains of her child's food allergy symptoms to see pediatrics. In order to effectively treat children's food allergies, doctors must not only prescribe medications, but also explain the rules of child care and explain the subtle differences in food therapy.
The genetic background is important in the onset of an allergy. Therefore, if moms and dads have an allergic reaction, children can also cause higher food intolerances.
Types of food allergies in infants
Food allergies are roughly divided into two types: a reaction that occurs immediately after ingestion and an accumulated allergy. To cause an allergic reaction, allergens must be repeated into the body. Allergies are divided into types of skin symptoms, food, breath, etc. , depending on the most damaged organ system.
, depending on the most damaged organ system.
Food allergy symptoms in infants
1. Food allergy symptoms are varied. The most common symptoms are a rash. Immediately after the allergen invades the body, hives can occur, which is an acute allergic reaction. A bright red swelling appears on the baby's skin with different sizes and shapes. Clear bubbles may appear in the center of the spot. The size varies from a few millimeters to several centimeters. This rash usually occurs within 1-3 days. But showing the child to the teacher is still worth it. Sometimes kids need to be prescribed medication so they get more immediate help in major rashes and places of failure. It is necessary to remember which product caused such a reaction and no longer gives.
2. Other types of rash are not as severe. Therefore, it may not be possible to clearly define the relationship between exterior and product. Such a battle is usually not bright, small. It tends to be a wave current. The rash usually becomes bright in the evening and becomes thinner in the morning.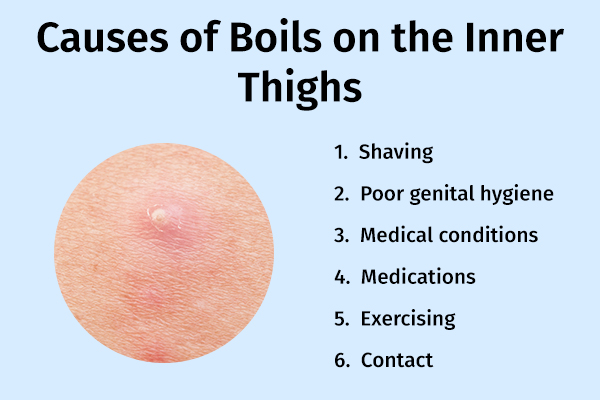 The skin is dry, peeled, and sometimes cracked. It can often be done on the cheek, buttocks, outer waist, and arms. This type of rash requires special medical expert precautions and special treatments.
The skin is dry, peeled, and sometimes cracked. It can often be done on the cheek, buttocks, outer waist, and arms. This type of rash requires special medical expert precautions and special treatments.
The most common symptoms are digestive symptoms. Swelling of the oral mucosa, swelling of the esophagus, single or frequent vomiting. In many cases, these symptoms strongly appear immediately after the use of allergens. In addition, children may suffer from abdominal pain. Sometimes you become sullen, get up or twist your legs. Food allergies can appear when the stool becomes loose. Both diarrhea and constipation can occur. Significant signs of a food allergy include large amounts of backflow, slight weight gain, anorexia, and weakness. Gastrointestinal symptoms may not be accompanied by a rash.
4 Respiratory symptoms may appear in infancy, although the incidence is low. When food enters the mucous membrane, swelling of the upper respiratory tract can occur. It is an acute, life-threatening disease. You need to consult a doctor immediately. If you are exposed to allergens for a long time, you may develop allergic rhinitis or asthma. In many cases, this reaction does not occur after swallowing food, but after inhaling particles. The most common cause of respiratory allergies is inhaling the smoke that comes out when you cook or fry fish.
You need to consult a doctor immediately. If you are exposed to allergens for a long time, you may develop allergic rhinitis or asthma. In many cases, this reaction does not occur after swallowing food, but after inhaling particles. The most common cause of respiratory allergies is inhaling the smoke that comes out when you cook or fry fish.
In addition, there is also a serious acute allergic reaction such as Quinkehremen and anaphylactic shock. Such a reaction occurs immediately after contact with allergens and develops very quickly. This is extremely rare and requires urgent medical attention.
Causes of food allergies in newborns
It is very rare for a newborn baby to cause food allergies. Babies receive only breast milk. This is food made by nature for a child, and there will be nothing else. Therefore, the peak food allergy for breast milk is considered to be around 4-5 months after birth, which begins to produce additional foods that are added to breast milk, such as vegetables, fruits, grains, meats, and dairy products. In the case of a child raised in milk, the situation is slightly different. Powdered milk itself can cause food intensity. Therefore, when choosing a mixture, it is better to consult an expert.
In the case of a child raised in milk, the situation is slightly different. Powdered milk itself can cause food intensity. Therefore, when choosing a mixture, it is better to consult an expert.
What is the most common allergen in infants?
1. 1st place is intensity for milk proteins. Most modern baby milk is based on milk proteins. For this reason, the child causes allergies in the mixture. Also, if the mother's diet is rich in dairy products, babies who are breastfeeding may also react to milk. It is not a specific milk component or powdered milk. Milk ingredients contain many proteins such as albumin, globulin and casein. Some of them can cause allergic reactions, while others do not. Casein makes up about 80% of all milk protein. The ingredients contained in milk are the same as goat's milk. This explains that the baby has a crossover reaction to milk and goat milk. Therefore, if the milk is intolerable, it is not recommended to replace it with a recipe using goat milk or goat milk for baby food. Certain proteins are destroyed by heat treatment. This is because the reactivity of boiled milk (ability to react) is low. There is a protein similar to that of beef and calf. In intolerance to this kind of protein, children will cross milk and meat products.
Certain proteins are destroyed by heat treatment. This is because the reactivity of boiled milk (ability to react) is low. There is a protein similar to that of beef and calf. In intolerance to this kind of protein, children will cross milk and meat products.
2. The next most common cause of a child's allergy is eggs. In the composition of eggs, allergens also act as albumin, a protein. Therefore, it is recommended to include eggs from egg yolk and small amounts when including eggs in a meal. Please carefully observe the child's reaction to this product. In the first feeding of eggs, it is important to carefully observe the reaction with the protein. Please note that the pasta and bakery contain eggs.
3. Gluten is well known as a cause of food intolerance. It is a protein found in some grains. It is recommended to start adding foods that are gluten-free to avoid side effects. Soba, corn, rice, etc. High gluten foods like Maneuvera, Christos and Automeal should be introduced almost a year in advance. During the first year of reaction to gluten, there is not much intolerance to milk proteins and egg whites.
During the first year of reaction to gluten, there is not much intolerance to milk proteins and egg whites.
4. In addition, colorful vegetables and fruits can cause food reactions. Carrots, beets, pumpkin, peach, etc. A good idea is to take green vegetables and white vegetables like zucchini, cabbage, broccoli, etc. And it's better to start with a blue apple or pear for your child's fruit. Exotic fruits such as mango and kiwi should not be rushed.
Be aware that any product can cause an allergic reaction. If you are giving your baby for the first time, your mother should remember the risk of intolerance. In particular, don't be impatient to introduce inferior products. In the morning, give you some unfamiliar foods so that you can reduce the reaction during the day.
How to recognize a food allergy and not confuse it with other diseases?
In most cases, the diagnosis of food allergy requires a doctor's consultation and a detailed examination of the mother. Mom sometimes reveals that he is allergic to food or introduces a specific product for the doctor. It can be difficult to make such a diagnosis at the same time. After that, a doctor can be scheduled for the test. Start, all the calculations of blood cells. If necessary, a specific allergy test will be performed, such as an immunoglobulin test and for subsequent ages. These tests have been selected as the most useful in recent clinical guidelines. Also, depending on the symptoms your child is concerned about, you may need to consult an allergy, dermatology, gastrointestinal department, etc. In addition, additional tests from the gastrointestinal tract.
Mom sometimes reveals that he is allergic to food or introduces a specific product for the doctor. It can be difficult to make such a diagnosis at the same time. After that, a doctor can be scheduled for the test. Start, all the calculations of blood cells. If necessary, a specific allergy test will be performed, such as an immunoglobulin test and for subsequent ages. These tests have been selected as the most useful in recent clinical guidelines. Also, depending on the symptoms your child is concerned about, you may need to consult an allergy, dermatology, gastrointestinal department, etc. In addition, additional tests from the gastrointestinal tract.
Treatment and prevention of allergies
According to the latest recommendations, breastfeeding is the mainstay of childhood food allergies. Babies who have grown up with only breast milk for a few months are unlikely to develop food allergies. At the same time, healthy breastfeeding does not require special foods. Meals should be perfect and varied, including protein, fat and carbohydrates. It also contains trace elements and vitamins. In addition, it is recommended that the mother of a child at risk of food intolerance not restrict the diet. It is necessary to completely eliminate foods that have reacted from their mother, and make a food diary.
It also contains trace elements and vitamins. In addition, it is recommended that the mother of a child at risk of food intolerance not restrict the diet. It is necessary to completely eliminate foods that have reacted from their mother, and make a food diary.
If artificial nutrition is needed for children with a predisposition to allergies, special hypoallergenic mixtures are chosen. The mixture should be selected by a specialist for the treatment of existing conditions. According to the latest clinical guidelines, in case of intolerance to cow's milk proteins, fully hydrolyzed proteins or mixtures with an amino acid composition are chosen. In this case, it is not advisable to prescribe hypoallergenic mixtures or mixtures based on goat milk protein. Soy-based milk powder itself can cause allergic reactions.
Proper introduction of complementary foods is also an important step in the prevention and treatment of food allergies. Introduce complementary foods early - not earlier than 4 months and not later than 6 months. Choose hypoallergenic foods first, such as Chinese cabbage, green leafy vegetables, and gluten-free cereals. On one day, the babies were given only a small amount of one complementary food and a possible reaction was observed. In the beginning, limit the introduction of new foods to once a week. Mothers of babies who are predisposed to allergies or already suffering from allergies are advised to keep a food diary. In it, the mother writes down all the foods that she gives the child during the day, and possible reactions to them.
Choose hypoallergenic foods first, such as Chinese cabbage, green leafy vegetables, and gluten-free cereals. On one day, the babies were given only a small amount of one complementary food and a possible reaction was observed. In the beginning, limit the introduction of new foods to once a week. Mothers of babies who are predisposed to allergies or already suffering from allergies are advised to keep a food diary. In it, the mother writes down all the foods that she gives the child during the day, and possible reactions to them.
If necessary, the doctor may prescribe medication for your child. They can be considered for both oral administration and dermal treatment. Children with chronic allergic rashes are shown special skin care. Also, after washing, it is necessary to use a special care product - conditioner. It is better to consult a doctor about which conditioner to choose. If you have gastrointestinal or respiratory symptoms, you may need special treatment from your doctor.
Eruptions often appear on the body in children. This may indicate a problem such as an allergy or skin disease. However, in most cases, rashes on the children's body do not pose a threat and go away on their own.
However, if you develop a rash or fever, feel unwell, behave abnormally, or are worried about skin changes, be sure to contact your pediatrician to rule out a serious illness or infection. treatment if necessary.
This article contains information about what causes the rash, but do not take it as a self-diagnosis. This is just an overview of the most common causes of rashes in children. Your pediatrician will be able to tell you more about your child's health. We will talk about the causes of rashes in infants separately.
Chickenpox (chickenpox)
Chickenpox is a common viral illness affecting most children. Chickenpox causes an itchy red patchy rash on the body that turns into blisters of fluid. The blisters then dry out, form a crust, and eventually flake off. Some children have few spots, while others have a rash all over their body.
Some children have few spots, while others have a rash all over their body.
Eczema
Eczema is a condition in which the skin becomes red, itchy, dry and cracked. The most common is atopic dermatitis, which is more common in children but occasionally occurs in adults.
Atopic dermatitis usually causes a rash on the feet (knees), hands (elbows), neck and face (eyelids, ears and cheeks). This is a clear illness, but if the child subsequently becomes infected with the herpes simplex virus, the dermatitis may worsen, and small blisters (called irritable fever) may appear along with the high fever.
Impetigo
Impetigo is a highly contagious disease caused by bacteria. It is characterized by the formation of pustules and blisters on the skin. There are two types of impetigo.
- Bullous contagious impetigo - large painless blisters filled with fluid.
- Impetigo is highly contagious and causes pustules that break open quickly, forming yellow-brown crusts.

If you think your child has impetigo, talk to your pediatrician. You will be given antibiotic cream and should be cured within 7-10 days.
Ringworm
Ringworm is a common, highly contagious infection that causes round, red rash patches on the skin. The plaques can appear anywhere on the body, but are most common on the scalp, legs, and groin.
Consult a dermatologist for an accurate diagnosis. Lichen interstitialis is treated with antifungal agents that are applied to the skin in the form of creams, ointments, shampoos, or given as tablets. Quarantine is provided for the period of illness, children cannot attend school and kindergarten.
Prickly heat
Sweaty babies may experience this option, for example, when worn in extremely hot or humid conditions. In older children, it develops when hygiene rules are not followed or when wearing uncomfortable synthetic clothing. Small red rashes and blisters appear on the skin, but they usually heal quickly without special treatment. To do this, bathe them regularly and wear them according to the weather.
To do this, bathe them regularly and wear them according to the weather.
Exudative erythema multiforme
Pustular erythema - skin reaction caused by:
- bacterial infection
- Herpes simplex virus
Round red spots appear on the arms and legs, which gradually increase and spread throughout the body. Favorite places of rashes Hands, less often feet, to a lesser extent the face, neck, shins, soles of the feet. Sometimes elements of the rash are observed in the oral cavity. The center of the spot gradually turns pale, forming elements that can merge with each other. In addition to blemishes, it can also cause blisters on the skin.
In subtle erythema multiforme, the pediatric focus is often disturbing, the rash is accompanied by fever. Recovery takes 2 to 6 weeks. Rarely, excretory erythema multiforme may develop in response to drugs such as antibiotics or antispasmodics. This is more dangerous, the disease can be life-threatening. Call your pediatrician if you develop a rash and feel unwell.
Call your pediatrician if you develop a rash and feel unwell.
Keratosis follicularis (“goosebumps”)
Thylakotase is a common, asymptomatic condition in which the skin on the forearms becomes rough and itchy when cold. You can also get goosebumps on your lower back and cheeks.
It usually starts in childhood and worsens during adolescence. After that, the condition subsides and may even disappear completely with age. There is no specific treatment for follicular keratosis, but it usually does not matter much.
Hand-foot-mouth syndrome (viral pemphigus)
Hand-foot-mouth syndrome and viral pemphigus are common benign diseases caused by Coxsackie enteroviruses. Accompanied by rashes and small blisters on the palms and feet of children. Mouth ulcers and general malaise may also occur. Itching is usually not noticeable.
The child's immune system fights the virus on its own and symptoms usually disappear within 7-10 days. However, FMD is a highly contagious disease.
Molluscum contagiosum
Molluscum contagiosum is a skin disease caused by a virus that causes small hard blisters to form on the skin.
Molluscum contagiosum most commonly develops in children between 1 and 5 years of age who infect each other. As a rule, there is no pain, but sometimes itching may occur. Without treatment, it usually resolves within 18 months. In some cases, skin formations can be removed, but in this case, you should consult a dermatologist.
Molluscum contagiosum is highly contagious, but most adults develop immunity to the virus and are less likely to become infected through contact with it.
Pityriasis rosea
Rosacea dandruff is a relatively common skin condition. Rounded pink spots appear on the skin, the central part of which gradually turns pale and begins to peel off. The rash is sometimes accompanied by mild itching. After a few weeks, the spots spread all over the body.
Older children and young people between the ages of 10 and 35 are most commonly affected. Dandruff rosacea usually resolves without treatment within 2 to 12 weeks. Its cause is unknown.
Dandruff rosacea usually resolves without treatment within 2 to 12 weeks. Its cause is unknown.
Scabies
Scabies is a contagious skin disease caused by tiny, itchy mites that burrow on the skin. This causes a rash with intense itching. Children become infected with scabies through close contact, such as when playing with sick adults or children.
Ticks prefer thin skin between fingers, skin folds, curved limbs and groin. In young children, the legs, arms, buttocks, face, and scalp are usually affected. It leaves small red bumps or silvery lines on the skin, usually on the palms and soles. Infants often develop blisters on their feet. If you suspect you have scabies, call your doctor for treatment (lotion or cream).
Urticaria (urticaria)
Urticaria is a disease characterized by red, itchy, burning rashes on the skin. This is caused by the release of histamine into the skin. Causes redness, swelling and itching.
Urticaria can be caused by a variety of factors, including allergens (eg food and latex), irritants (eg nettles), medications, and natural factors such as sunlight and heat. However, in most cases the cause cannot be determined. This is a common skin reaction in children. The rash usually resolves quickly with antihistamines.
However, in most cases the cause cannot be determined. This is a common skin reaction in children. The rash usually resolves quickly with antihistamines.
Erythema infectiosum ("fifth disease")
Erythema injectio ("fifth disease") is a viral disease that is common in children that has a red rash on the cheek. In principle, children between the ages of 6 and 10 are eligible. In most cases, the health condition does not appear much and it will subside after a few days, so this is usually not required. This can take 4 to 5 weeks. If you have a rash or fever, contact your doctor.
Psoriasis (psoriasis)
Psoria is a disease in which red spots appear on the skin, covered with a silver scale. Psoriasis can cause beauty defects, and if the course is long, nails and joints can be invaded. This is a chronic condition, but there are treatments to help relieve symptoms, improve the appearance of the rash, and avoid complications.
Cellulitis or phlegmon
Bizitis and sputum is an inflammation of the skin and subcutaneous tissues caused by bacteria. The affected area becomes red, tender, swollen and hot. Changes in the skin are accompanied by high fever, pain and severe exhaustion. If these symptoms appear, contact your pediatrician immediately.
The affected area becomes red, tender, swollen and hot. Changes in the skin are accompanied by high fever, pain and severe exhaustion. If these symptoms appear, contact your pediatrician immediately.
Measles
Motor sickness is a severe infectious disease caused by a virus. Measles can be contracted if you are not vaccinated or have not previously been vaccinated, but if you are one to four years old, you will have measles disease.
Hagan is characterized by a small, reddish brown rash that basically appears behind the ears and then spreads to the head, neck, legs and torso. Children are likely to have flu-like symptoms and a high fever. If you notice the above signs, contact your pediatrician at home.
Scarlet fever
- And it is also a contagious infectious disease in children. The pathogen is a bacterium. A two-year-old child was the most affected. In the scarlet aroma, there is a bright pink rash that is characteristic of the body, and when you touch it, it looks like paper. In many cases, it starts with a sore throat, headache, and fever, and a rash develops after 12-48 hours. If you think your baby is red, contact your family doctor immediately.
In many cases, it starts with a sore throat, headache, and fever, and a rash develops after 12-48 hours. If you think your baby is red, contact your family doctor immediately.
Meningitis
A child's rash may be caused by "meningitis t-mamigitis", a disease that leads to death. The rash resembles roots or appears in red spots. It usually disappears after 2-3 hours. And due to serious causes and dangerous complications, the skin can be bruised. A sign that can be considered for meningitis in children.
- Children are repressed, react to others weak, limited and acute.
- The child is frustrated and hates to be hugged.
- I hate hugs, hate hugs, hate hugs, hate hugs, hate hugs, hate hugs.
- Vomiting and refusal to eat
- Blue and white and spots.
- Anorexia
- The expression is complex.
- We have severe drowsiness.
- It's warm.
- Red rash that does not go away even when pressed against hard objects (eg glass).

Trust your intuition. If you think you have had meningitis, contact your pediatrician at home immediately, and if your condition is serious, call an ambulance (03 from the landline, 911 or 112 from your mobile phone).
Rash in a child: which doctor should I contact?
When you go to your child's body, you can use this service to find a good doctor.
Follow the link to find a clinic where you can call a pediatrician at home.
You might also be interested in reading
Napoprovku.ru was responsible for the localization and translation, and the NHS selection provided the original content for free. Retrieved from www.nhs.uk. Choice The NHS has not endorsed the local content or translation of the website's original content and is not responsible.
Copyright notice
All published materials are reviewed by physicians. However, no matter how reliable the articles are, it is not possible to consider all the characteristics of an individual's disease. Therefore, the information posted on this website is not an alternative to consulting a doctor, but additional. These articles have been created for the purpose of providing information and having advice.
Therefore, the information posted on this website is not an alternative to consulting a doctor, but additional. These articles have been created for the purpose of providing information and having advice.
Baby skin rash often sues during a pediatric consultation. Usually parents consider the cause of the rash to be children's eating habits. There are so many allergic rashes for children, but I will analyze them for what other reasons and how to treat them.
Physiological rashes
These are the types of rashes that appear on newborns. There seem to be various reasons. No special treatment is required and it disappears naturally. These are the following.
- Birotome a - Necessary white spots for the nose and forehead of newborns. Usually it naturally cuts to the first birth age. Special processing is not required.
- Seborrheic dermatitis or milky white crust - development in the year after birth. In tender reddish skin and normal skin, white and yellowish dark skin appears. It can be easily separated from the skin without giving any discomfort. There is no need for treatment. You may want to use shampoos and bubble baths dedicated to the treatment of seborrheic dermatitis sold in pharmacies.
It can be easily separated from the skin without giving any discomfort. There is no need for treatment. You may want to use shampoos and bubble baths dedicated to the treatment of seborrheic dermatitis sold in pharmacies.
- Dess (acne) for babies. It occurs in a newborn within one year of birth. I sometimes stay for a long time. The reason is that the change is due to hormones. The rash is similar to adult acne. Redness and thickening appear on the skin. Then a head appears with a white and yellowish content. For treatment, use a preservative if needed and a retinoid for severe changes.
- Post-erythema of newborns, approximately 2-5 days after birth and completely disappears after 2-3 weeks. This is redness of the skin filled with white or yellow content or shrine. It can appear anywhere on your body. The cause of the occurrence has not been fully elucidated. There is no need for treatment. He disappears without permission.
-Mongolian spots a-pigmented spots with green, blue and gray, usually found on the back and buttocks of a newborn. Appears from birth. Pass independently at the age of 3 years. The kids are not in trouble. There is no need for treatment.
Appears from birth. Pass independently at the age of 3 years. The kids are not in trouble. There is no need for treatment.
- Marble-like skin pigmentation - may increase or decrease over time with a delicate network of blood vessels on the surface of a child's skin. The reason is that the child's autonomic nervous system is immature. Pass without permission. There is no need for treatment.
Allergic rashes
One of the causes of dry skin in children is allergies. Pathogens are divided into food and contact. Respiratory allergens rarely cause a rash. Exposure to allergens causes skin redness, swelling, itching, and sometimes clear blisters. If there is a strong reaction, the bubbles will be large. Damage to the epithelium of the bladder exposes the wound surface and heals under the crust. Acute allergic rashes usually disappear quickly after contact with the allergen is stopped. Rash from prolonged exposure to an allergen is usually less intense. treated worse. Makes it difficult to identify allergens. Severe cases require medical attention and more intensive treatment.
Makes it difficult to identify allergens. Severe cases require medical attention and more intensive treatment.
Atopic dermatitis
This is a skin disease that is accompanied by a violation of its barrier function and the development of inflammation. Atopic dermatitis first appears around 3 months of age. It flows like a wave through a period of improvement. In most cases, it is completely cured within 7 years. Approximately 10% of the changes remain for life. This is dry skin with slight redness, peeling, itching, sometimes small blisters with transparent contents appear. In severe cases, the redness may disappear, and the surface of the skin may crack, with a yellow or clear liquid leaking from it. Topical corticosteroids, pimeclalimus, and toclalimus in ointment or gel form are used to relieve flare-ups. Continue to use emollients to maintain remission and improve skin barrier properties. Antihistamines may be recommended to relieve itching.
Miliaria in infants
Predominantly localized in skin folds. It is characterized by redness of the skin and the appearance of small white dots. The reason is a decrease in the secretion of sweat glands and the inflammation that accompanies it. Contact dermatitis and diaper dermatitis is redness and inflammation of the skin caused by prolonged contact with the urine, feces and saliva of children. Both symptoms usually go away on their own with proper hygiene. Dry creams and powders containing zinc may help. Antifungals and antibiotics are used in severe cases with an infected rash.
It is characterized by redness of the skin and the appearance of small white dots. The reason is a decrease in the secretion of sweat glands and the inflammation that accompanies it. Contact dermatitis and diaper dermatitis is redness and inflammation of the skin caused by prolonged contact with the urine, feces and saliva of children. Both symptoms usually go away on their own with proper hygiene. Dry creams and powders containing zinc may help. Antifungals and antibiotics are used in severe cases with an infected rash.
Rashes associated with skin infections
Chickenpox is an acute, widespread infection that mainly affects children of preschool and primary school age. Symptoms of poisoning appear, sometimes accompanied by an increase in body temperature and the appearance of a characteristic rash. The chickenpox rash begins with red patches on the scalp. Then gradually lower your torso and limbs. It can also appear on the mucous membranes of the mouth and genitals. Soap bubbles with transparent contents appear instead of spots.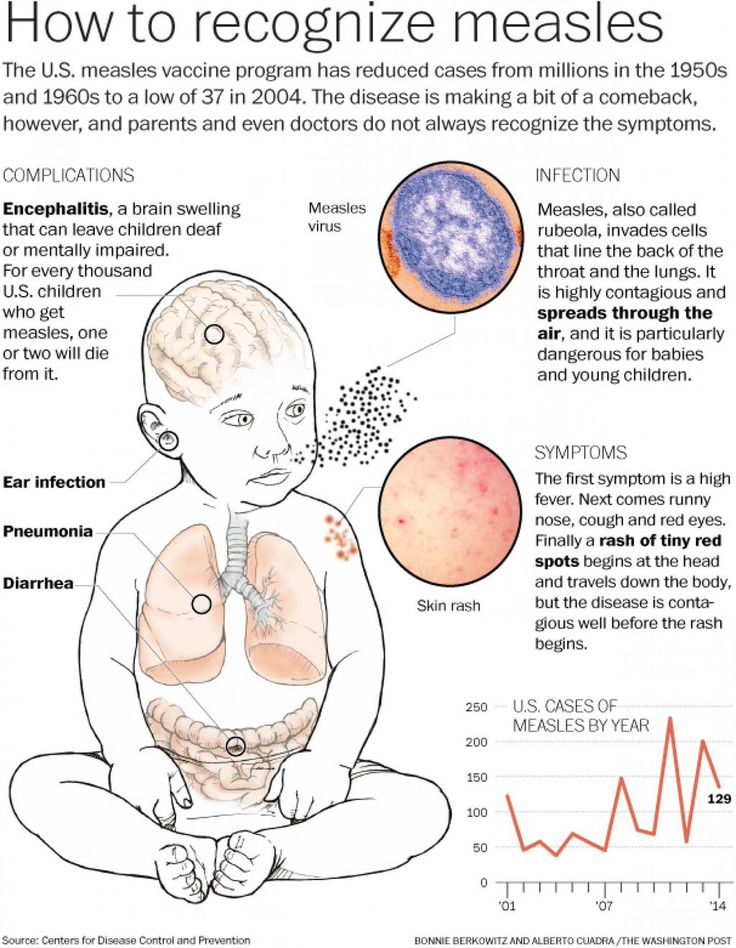 Blisters appear, accompanied by itching of varying intensity. After that, the air bubbles dry up and become covered with a yellow crust, which eventually disappears. One large element can leave a permanent scar on the skin. Treatment is symptomatic. At high temperatures, use an antipyretic. Topically apply an antiseptic to the skin and mucous membranes to prevent infection of the elements. Antihistamines are indicated for severe itching. It will heal on its own in about 10 days. There are vaccines to prevent chickenpox.
Blisters appear, accompanied by itching of varying intensity. After that, the air bubbles dry up and become covered with a yellow crust, which eventually disappears. One large element can leave a permanent scar on the skin. Treatment is symptomatic. At high temperatures, use an antipyretic. Topically apply an antiseptic to the skin and mucous membranes to prevent infection of the elements. Antihistamines are indicated for severe itching. It will heal on its own in about 10 days. There are vaccines to prevent chickenpox.
- As an infectious disease that appears when fever, catalysis and rash appear on the 3rd - 4th day. Rash of measles appears in the mouth. And this extends to the face and to the body. The component of the rash is large and brown. There is no specific treatment for this rash. There is vaccination.
-Reval a is an infectious disease that appears with fever, catalog symptoms, conjunctivitis and rash. Rufella rash is small, bright, spreads over the entire skin. This disease has no silver bullet. Rubla has a vaccine.
This disease has no silver bullet. Rubla has a vaccine.
- Pidera (sudden rash) ... This is a viral disease that develops mainly in children after 10 months. Up to two years of age. Appears with severe poisoning and acute onset with high fever. On the 3rd day, body temperature appears, and several elements of red rash appear. It starts from your head and gradually descends throughout your body. I don't care about the baby's rash. It heals naturally in 2-3 days. This disease does not require treatment.
- Per n-development from preschoolers. A characteristic change appears on the red border between the lips, mucous membranes and the oral cavity. Children feel itching and tingling. Redness appears on the skin, then swells, and a multifunctional graft is formed. When the disease subsides, crusts (cabs) form instead of bubbles, and they disappear without a trace. Herpes treatment includes an antiviral form in the form of a gel, ointment and tablets.
- Infectious flame of the angle of wheat is a viral skin lesion. This is expressed by the appearance of gradually increasing itching on unaffected skin. And a characteristic dent appears in the center. This disease is contagious, not dangerous, lasts a long time, and there is no specific treatment.
This is expressed by the appearance of gradually increasing itching on unaffected skin. And a characteristic dent appears in the center. This disease is contagious, not dangerous, lasts a long time, and there is no specific treatment.
-Scarlac a is an infectious disease caused by bacteria. Appears in intense drunkenness, fever, inflammation of the tonsils and characteristic changes in the skin. The scarlet t-fever rash is patchy and not bright. It occurs in folds such as the groin, elbows, and armpits. And it spreads throughout the body. After recovery, go through without any x-traces. Some time after the disease, the skin may remain on the finger of the extremities. Scary fever is treated with oral antibiotics.
-Marming bacterial infection: a serious bacterial infection that also occurs due to fever, catalytic symptoms and damage to the central nervous system. The rash of meningitis infections has a characteristic appearance. These are the isolated bleeding factors that will add up to the big "subcutaneous bleeding". If such a rash appears on your child's skin, you need to consult a doctor immediately. Treatment with a systemic antibiotic. Mennititis bacterial infections have vaccines.
If such a rash appears on your child's skin, you need to consult a doctor immediately. Treatment with a systemic antibiotic. Mennititis bacterial infections have vaccines.
- Wakig a is a rash caused by bacteria. A brightly painful redness appears around the face, usually around the mouth, and then it will be covered with dirty yellow crusts. External antibiotics are used for treatment. In case of severe diseases, internal medicine is prescribed.
Counseling tells you about the problem you have, the doctor explains the situation, reads the test, answers your questions and makes the necessary suggestion.
There are various reasons for a baby's skin rash. Only typical ones are explained here. It is necessary to consult a pediatrician to understand the symptoms and understand how to help the child. Additional tests may be required.
Rashes on the child's body
Many parents have noticed suspicious rashes on the body of their children. This symptom indicates the presence of any disease of the body or simply its painful condition. In any case, a rash on a child's body can be very dangerous. Therefore, if you notice a rash on the skin, you should immediately make an appointment with the child's pediatrician.
In any case, a rash on a child's body can be very dangerous. Therefore, if you notice a rash on the skin, you should immediately make an appointment with the child's pediatrician.
Rash help
Make an appointment
Online appointment
Phones:
+7 (812) 30-888-03
+7 (812) 242-53-50
Clinic address: St. Petersburg, Vyborgsky district, st. Asafiev, 9, building 2, lit. A (metro station Ozerki, metro station Prosveshcheniya)
Causes of rashes
A rash in children can appear for various reasons. The most “safe” case is when rashes appear due to poor hygiene. In addition, the cause of the rash is allergies, blood diseases, cardiovascular diseases, as well as infections and microbes. In the case of an infection, a rash is not the only symptom: fever, runny nose, sore throat, severe cough, chills, etc. are added to it. Often infections are accompanied by indigestion and vomiting. The rash in such cases does not occur immediately, but appears after a few days.
Rash most often occurs as a symptom of diseases that are commonly referred to as "children's". We are talking about chicken pox, rubella, measles, scarlet fever and some other infections that people get sick, mainly in childhood. Moreover, depending on the disease, the nature of the rash changes, so that doctors can diagnose only one type of rash. The most dangerous rash, which refers to the symptoms of meningitis.
Diseases causing rashes on the skin of children
Let's analyze the types of rash in a child in more detail depending on the disease.
- Chicken pox. Perhaps the most famous disease that is accompanied by a rash. With chickenpox, reddish spots appear on the entire surface of the body, which grow and become bubbles filled with a clear liquid. The growth of the bubbles is accompanied by itching, but over time they dry out and fall off, sometimes leaving characteristic “pockmarks”. Chicken pox often causes fever, and doctors recommend treating blisters of the rash with brilliant green.

- Measles. Initially, a rash in the form of large red spots appears on the face, but literally within 2-3 days it spreads “from top to bottom” along the body to the very legs. In addition, the child begins to have a sore throat, runny nose and cough, and the temperature rises. The largest spots merge into large inflamed areas.
- Meningococcal infection. The most dangerous infection, as it causes meningitis. It is very important to recognize the disease in time, as it develops very quickly. The rash is expressed in the form of large spots resembling bruises. If you see a doctor as soon as possible, the chances of a cure are very high.
- Rubella. The rash is accompanied by fever and inflammation of the lymph nodes. A rash on the body of a child in the form of small red spots appears mainly on the buttocks and in the places where the limbs are bent. After a few days, the rash disappears without leaving any consequences.
- Scarlet fever.
 With scarlet fever, a rash in the form of small pimples appears on the second day all over the body, but their highest concentration is noted in the groin, in the places of the folds of the arms and legs and in the lower abdomen. After a few days, the rash disappears, and the skin in these places begins to peel off strongly. Also during the peak of the disease, swelling, rash and redness of the entire skin are noted.
With scarlet fever, a rash in the form of small pimples appears on the second day all over the body, but their highest concentration is noted in the groin, in the places of the folds of the arms and legs and in the lower abdomen. After a few days, the rash disappears, and the skin in these places begins to peel off strongly. Also during the peak of the disease, swelling, rash and redness of the entire skin are noted. - Enteroviral infection. Redness and rash appear on the third day after infection and last for about two to three days. Their other symptoms, doctors note vomiting, diarrhea, fever and general weakness of the body.
- Parasites. In this case, the rash is not caused by infections, but by scabies mites or other parasites that live on the human body. The scabies mite "drills" holes in the skin, leaving entrances and exits in the form of dots. The most “attractive” parts of the body for a tick are places with thin skin: groin, wrists, areas between fingers, etc.
 Since the tick can be transmitted from one person to another, urgent treatment is necessary after the detection of this pathology.
Since the tick can be transmitted from one person to another, urgent treatment is necessary after the detection of this pathology. - Cardiovascular diseases. As a rule, these diseases are not typical for children, although they occur in them. Vascular disease can be recognized by small hemorrhages under the skin. Larger areas form bruises.
Other causes of rashes
Sometimes, even if all the rules of hygiene are observed and there are no diseases, a rash on the body of a child appears with enviable regularity. In this case, it is most likely an allergic reaction of the body to various substances. If this is true, then allergies can be recognized by other symptoms that will inevitably appear along with the rash: a runny nose, cough, tears, and itching. Also, a rash on the body of a child may appear from burns by plants or insect bites. Even a simple mosquito bite often causes a severe rash in children, which is accompanied by itching.
And, of course, very often a rash appears due to poor hygiene. Unlike adults, children's skin is much thinner and more delicate, so even a short-term lack of care for it can lead to a rash. Children, especially the smallest, should be washed and washed regularly. But wearing a lot of clothes on him or leaving him in wet diapers is not worth it - this can lead to diaper rash, irritation, and a rash.
Unlike adults, children's skin is much thinner and more delicate, so even a short-term lack of care for it can lead to a rash. Children, especially the smallest, should be washed and washed regularly. But wearing a lot of clothes on him or leaving him in wet diapers is not worth it - this can lead to diaper rash, irritation, and a rash.
Rash Help
If you find a rash on your child's body, you should see a doctor as soon as possible. You can make an appointment at our Poem Health clinic. In addition, you can call a doctor at home if the child is in a serious condition. Moreover, sometimes a doctor's house call is mandatory, since many diseases with symptoms in the form of a rash are easily transmitted to such children. You need to be especially careful with rubella, as it seriously affects the health of pregnant women. And if you suspect meningitis, you need to call not just a doctor, but an ambulance team.
Do not try to get rid of the rash on your own before seeing a doctor. Firstly, it will make it difficult for a doctor to determine the diagnosis. Secondly, it can lead to even more rashes in the child. It is best to wait for the examination of the doctor and listen to his recommendations for further treatment of the rash. Bacterial rashes are treated with antibiotics, scabies - with special means against ticks, allergies - with appropriate drugs with isolation from the source of allergies, etc. More complex treatment is needed for cardiovascular diseases, but, in the end, a rash on the body of a child is always treated successfully.
Firstly, it will make it difficult for a doctor to determine the diagnosis. Secondly, it can lead to even more rashes in the child. It is best to wait for the examination of the doctor and listen to his recommendations for further treatment of the rash. Bacterial rashes are treated with antibiotics, scabies - with special means against ticks, allergies - with appropriate drugs with isolation from the source of allergies, etc. More complex treatment is needed for cardiovascular diseases, but, in the end, a rash on the body of a child is always treated successfully.
Prevention of rashes
To avoid rashes on the body, measures must be taken to prevent them. First of all, we are talking about the basic rules of personal hygiene. At the earliest age, parents should take care of this, later they should teach this to their child as early as possible. Compliance with hygiene helps to get rid of not only rashes, sweating and dirt, but also prevents many infectious diseases.