Baby's skin diseases
Common Skin Conditions & Rashes in Children: Causes & Treatment
What are skin conditions in children?
Various skin conditions can affect babies, toddlers, children and adolescents throughout their lives. Healthcare providers receive more than 12 million office visits from children each year related to skin concerns. Skin conditions in kids may include hives, warts, acne, birthmarks and all sorts of rashes.
What are the different types of skin rashes in children?
Many different types of rashes can affect your child. Dermatitis, viral infections, bacterial infections, fungal infections and many other conditions may cause rashes.
Dermatitis
Dermatitis is an umbrella term for any condition that causes skin inflammation. These conditions may cause red rashes, itchiness and dry skin on your child and happen at any age. Types of dermatitis include diaper rash, cradle cap, eczema and contact dermatitis.
Diaper rash: Diaper rash is also called diaper dermatitis. It’s the most common skin condition seen in babies. Diaper rash occurs when moisture in your baby’s diaper area causes irritation or growth of fungi or bacteria that normally live in small amounts on the skin. To prevent or treat diaper rash, keep your baby’s diaper area clean and dry by changing diapers frequently. When changing your child's diaper, leave it off for a short while before putting it back on. You can also apply an ointment or cream that contains zinc oxide or petroleum jelly to protect your baby’s skin in the diaper.
Cradle cap: Cradle cap is also called infant seborrheic dermatitis. It’s a skin condition that looks like yellow scaly patches often surrounded by a red rash on your baby’s scalp. Overproduction of the oil-producing sebaceous glands on your baby’s scalp may cause cradle cap. You can treat cradle cap at home with mild baby shampoo and can also lightly rub the scale off if it doesn’t bother your baby.
Eczema: Eczema is also called atopic dermatitis. Eczema makes your child’s skin itchy and then it gets red, irritated and dry. Differences in your child’s skin barrier (compared to normal, healthy skin) and an immune system that tends toward allergies cause eczema. Issues with the barrier make your child’s skin more sensitive and prone to infections and dryness. Controlling your child’s symptoms is the goal of treatment. Often there are seasonal or allergic triggers that you should help your child avoid. Good skin care includes bathing in warm but not overly hot water and moisturizing regularly, especially immediately after baths or water exposure.
Eczema makes your child’s skin itchy and then it gets red, irritated and dry. Differences in your child’s skin barrier (compared to normal, healthy skin) and an immune system that tends toward allergies cause eczema. Issues with the barrier make your child’s skin more sensitive and prone to infections and dryness. Controlling your child’s symptoms is the goal of treatment. Often there are seasonal or allergic triggers that you should help your child avoid. Good skin care includes bathing in warm but not overly hot water and moisturizing regularly, especially immediately after baths or water exposure.
Contact dermatitis: Contact dermatitis can occur when kids have a reaction to an allergen or an irritant. Allergens may include poison ivy or medications. Irritants may include perfumes, soaps, cleaners and paints. Contact dermatitis causes an itchy skin rash that is sometimes also painful. Treatment includes moisturizers, anti-itch creams and topical (or sometimes oral) steroids.
Viral infections
Viral rashes in babies, toddlers and kids are caused by a variety of different viruses. These infections include fifth disease, roseola, chickenpox, measles, rubella, molluscum contagiosum and hand, foot and mouth disease.
Fifth disease: Fifth disease is also called slapped cheek (slap face) disease. It causes a bright red rash on your child’s cheeks. A specific virus, Parvovirus B19, causes fifth disease. Along with the rash, your child may have a fever and other nonspecific symptoms. After a few days, the facial rash will fade. But then pink patches may develop in a lacy pattern on your child’s arms and legs. Treatment includes comfort measures like non-steroidal anti-inflammatory drugs (NSAIDs) anti-itch creams or antihistamines.
Roseola: Roseola is also called sixth disease. Human herpesvirus 6 causes roseola. With roseola, your baby will suddenly develop a high fever that can last up to a week. Once the fever breaks, a slightly raised, spotty pink rash may appear on your baby’s chest or stomach. The rash may spread to your baby’s upper arms and neck, and then it will fade after about 24 hours. Treatment may include acetaminophen for your baby’s fever, but the rash doesn’t itch or cause pain.
Once the fever breaks, a slightly raised, spotty pink rash may appear on your baby’s chest or stomach. The rash may spread to your baby’s upper arms and neck, and then it will fade after about 24 hours. Treatment may include acetaminophen for your baby’s fever, but the rash doesn’t itch or cause pain.
Chickenpox: Varicella zoster virus causes chickenpox. Chickenpox generally causes a rash on your child’s face, chest and back first, but it may travel to their entire body. The rash turns into itchy, fluid-filled blisters, then blisters turn into scabs. Chickenpox usually goes away on its own in one to two weeks. You can treat your child’s symptoms with antihistamines and acetaminophen. They are contagious until all of the blisters are crusted over.
Measles: Morbillivirus causes measles. Measles is very contagious and prevented by the measles vaccine or MMR vaccine. It causes a rash that starts on your child’s face. It’s typically seen behind the ears or around your child’s mouth. Then it moves down over their body. The rash starts as flat red spots, but then smaller raised white spots may appear on top of the red spots. The spots may join together as it moves down your child’s body. Measles has to run its course. It will go away within about two weeks unless complications develop. You can treat your child’s symptoms of fever and achiness with acetaminophen or NSAIDs.
It’s typically seen behind the ears or around your child’s mouth. Then it moves down over their body. The rash starts as flat red spots, but then smaller raised white spots may appear on top of the red spots. The spots may join together as it moves down your child’s body. Measles has to run its course. It will go away within about two weeks unless complications develop. You can treat your child’s symptoms of fever and achiness with acetaminophen or NSAIDs.
Rubella: Rubella is also called German measles and can be prevented by a vaccine. It can look similar but is caused by a different virus than measles. Rubella causes a red or pink rash that starts on your baby’s face and neck. The rash then spreads to other parts of your baby’s body and lasts about three days unless complications develop. Your baby may have a fever, cough or runny nose before the rash appears. Rubella has to run its course. You can treat your child’s symptoms of fever and achiness with acetaminophen or NSAIDs.
Molluscum contagiosum: Molluscum contagiosum virus causes this benign but sometimes unpleasant rash. Molluscum contagiosum has raised bumps on your child’s skin. The bumps are usually flesh-colored, pink or pearly white with indentations in the center. The bumps will show up on your child’s face, chest, stomach, arms and legs. They’re painless but they may not go away for several months or years. Molluscum contagiosum will eventually go away on its own without treatment.
Hand, foot and mouth disease: A virus in the enterovirus family causes hand, foot and mouth disease. The disease causes a red rash to develop around your toddler’s mouth, and on the palms of their hands and soles of their feet. It may also affect other areas. The rash may turn into bumps or blisters on your baby’s skin and in their mouth, and they can be very painful. Hand, foot and mouth disease usually goes away on its own within one to two weeks. You can treat your toddler’s symptoms with acetaminophen or NSAIDs.
You can treat your toddler’s symptoms with acetaminophen or NSAIDs.
Bacterial infections
Types of baby rashes may also include bacterial infections such as scarlet fever and impetigo.
Scarlet fever: A bacteria called group A Streptococcus causes strep throat and scarlet fever. Scarlet fever usually starts with a fever, sore throat and headache, but the key symptom is a raised, red rash on your child’s neck and upper chest. The rash may then spread to other areas of your child’s body. Your child’s face may be red with a pale area left around their mouth. The rash feels rough like sandpaper and may look like your child has a sunburn. Treatment for scarlet fever includes antibiotics.
Impetigo: Group A Streptococcus or Staphylococcus aureus bacteria cause impetigo. It’s most common in kids aged 2 to 5 years old but can happen at any age. Impetigo causes red bumps, blisters or crusty spots to develop. These are most common around your toddler’s mouth and nose and can be anywhere that skin gets repeatedly irritated. Treatment for impetigo usually includes antibiotics that may be oral or put directly onto the skin.
These are most common around your toddler’s mouth and nose and can be anywhere that skin gets repeatedly irritated. Treatment for impetigo usually includes antibiotics that may be oral or put directly onto the skin.
Fungal infections
Common skin rashes seen in babies, toddlers and children can also include fungal infections such as ringworm.
Ringworm: Despite its name, a fungus causes ringworm, not a worm. It causes round or oval patches to develop on your child’s skin. The patches have smooth centers and red, scaly borders and may not look like rings right away. But you’ll notice the rings when they get bigger. The patches may be itchy and painful and may become puffy and inflamed. You can treat your child’s ringworm with antifungal medicines either orally or put directly on the skin.
What is a teething rash?
When your baby’s teeth are starting to come in, they may drool a lot more than usual. Drool can irritate your baby’s skin. This can cause a harmless rash known as a teething rash. The rash causes tiny, red raised bumps on your baby’s face, neck or chest. Teething rashes may come and go as new teeth pop up or when your baby stops drooling as much.
This can cause a harmless rash known as a teething rash. The rash causes tiny, red raised bumps on your baby’s face, neck or chest. Teething rashes may come and go as new teeth pop up or when your baby stops drooling as much.
Teething rashes don’t cause fevers, so if your baby has a fever with a rash, talk with their healthcare provider. You can treat your baby’s teething rash by keeping the area clean and dry. You can also apply emollient cream to the affected area. This may prevent your baby’s drool from irritating their skin.
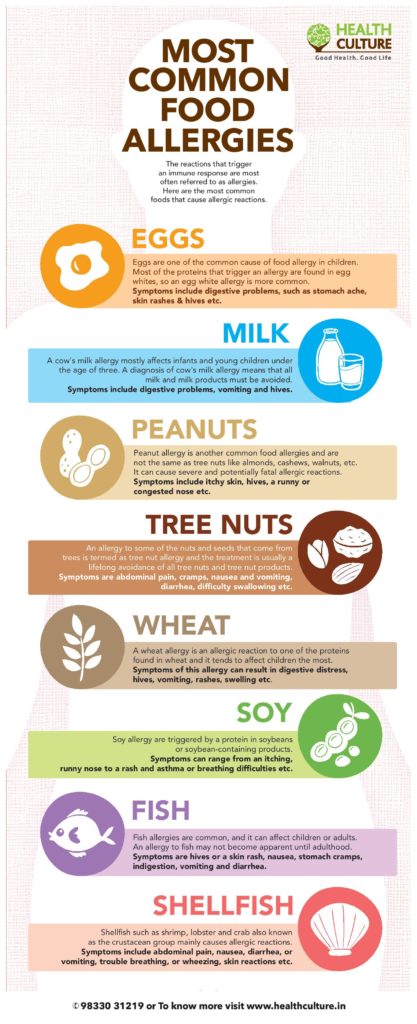
What causes hives in children?
Hives are also called urticaria. Hives are itchy pink, pale or red bumps on your baby’s skin. They may be small slightly raised spots or large welts of different shapes. Sometimes hives are ring-shaped or look like targets. The rings may have normal-looking skin in the center, or they may look pale, purple or blue. Hives can appear anywhere on your child’s body and may flatten out over several hours. But new bumps can keep showing up for days or weeks.
But new bumps can keep showing up for days or weeks.
Viral infections are a common cause of hives. But allergic reactions to foods, medicines and additives, or even cold temperature and stress may also cause hives. But many cases of hives have no known reason. The best treatment for hives is antihistamines.
What causes warts in children?
Warts on kids are a type of skin infection caused by the human papillomavirus (HPV). There are multiple types of HPV that cause infections in different areas of skin. The infection causes hard bumps to form on your child’s skin. Warts most commonly appear on your child’s hands and fingers, but they can also appear on their feet, face, genitals and knees. Warts are common in children of all ages. Warts often go away on their own after your child’s immune system fights off the virus, but they can be painful and unpleasant in appearance.
What is baby acne?
Baby acne causes little white bumps and pink pimples to appear on your baby’s face including their forehead, cheeks, eyelids and chin. An inflammatory reaction to yeast on your baby’s skin may cause baby acne. Sometimes baby acne is seen on your baby’s chest or neck. Baby acne usually goes away on its own within your baby’s first three months of life.
An inflammatory reaction to yeast on your baby’s skin may cause baby acne. Sometimes baby acne is seen on your baby’s chest or neck. Baby acne usually goes away on its own within your baby’s first three months of life.
What are birthmarks in children?
There are two main types of birthmarks — red birthmarks and pigmented birthmarks. Red birthmarks are skin markings caused by a collection of blood vessels. Pigmented birthmarks are areas in which the color of your child’s birthmark is different from their skin color.
Red birthmarks
Strawberry hemangiomas: Strawberry hemangiomas can be found anywhere, but are most commonly found on your baby’s face, scalp, back or chest. They’re made up of small, closely packed blood vessels. Strawberry hemangiomas usually fade or go away as your child ages. Some minor discoloration or wrinkling of your child’s skin may remain at the site of the hemangioma.
Cavernous hemangiomas: Cavernous hemangiomas look sort of like strawberry hemangiomas.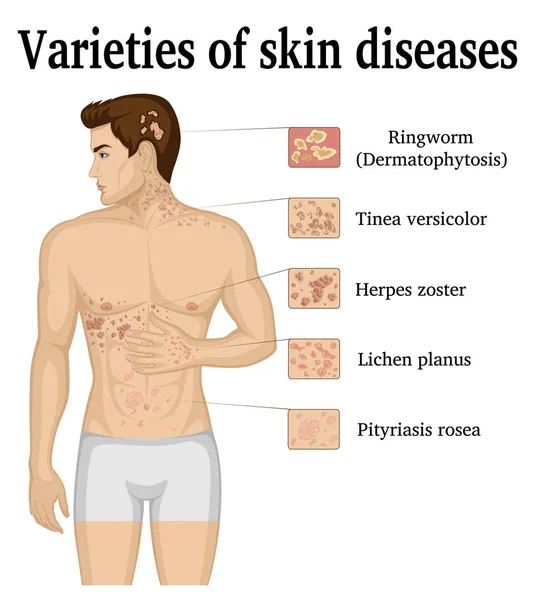 But they’re deeper in your child’s skin and often darker in color. They look like reddish-blue spongy masses of tissue filled with blood. Cavernous hemangiomas usually go away on their own as your child ages.
But they’re deeper in your child’s skin and often darker in color. They look like reddish-blue spongy masses of tissue filled with blood. Cavernous hemangiomas usually go away on their own as your child ages.
Port-wine stains: Port-wine stains are flat, reddish-purple birthmarks. They’re made up of dilated blood capillaries. They’re commonly seen on your child’s face and they vary in size. Port-wine stains are permanent, without treatment. They might thicken or darken over time.
Salmon patches: Salmon patches are also called stork bites or angel’s kisses. Salmon patches are small blood vessels that are visible through your baby’s skin. They are frequently seen on your baby’s forehead, eyelids, upper lips, between their eyebrows and on the back of their neck. Salmon patches fade as your baby grows.
Pigmented birthmarks
Slate gray nevus or congenital dermal melanocytosis (previously called Mongolian spots): These birthmarks are typically bluish and may look like bruises. They’re often found on your baby’s buttocks and/or lower back. Sometimes they appear on your baby’s chest, back or arms. Mongolian spots are seen most often in babies with darker skin.
They’re often found on your baby’s buttocks and/or lower back. Sometimes they appear on your baby’s chest, back or arms. Mongolian spots are seen most often in babies with darker skin.
Pigmented nevi: Pigmented nevi are also called moles. Moles are growths on your baby’s skin that typically are flesh-colored, brown or black. Moles can appear anywhere on your baby’s skin. Your baby may have one mole or several in a group.
Congenital nevi: Congenital nevi are moles that your baby was born with. These moles have a slightly increased risk of becoming skin cancer. Larger congenital nevi have a greater risk than smaller congenital nevi do. Your baby’s healthcare provider should examine all congenital nevi and may refer you to dermatology.
Cafe-au-lait spots: Cafe-au-lait spots are light tan or brownish-colored spots. They’re usually oval-shaped. They commonly appear at birth but might develop in the first few years of your child’s life. Cafe-au-lait spots are usually harmless. But if your child has many cafe-au-lait spots, or if they are large, consult their healthcare provider. It may indicate a serious genetic condition.
Cafe-au-lait spots are usually harmless. But if your child has many cafe-au-lait spots, or if they are large, consult their healthcare provider. It may indicate a serious genetic condition.
A note from Cleveland Clinic
Finding a rash, bump, mark or other skin condition on your child’s body may be scary. But kids get tons of rashes, and most of the time, these rashes and other conditions shouldn’t cause too much worry. If you have any concerns, check in with your child’s healthcare provider. They can usually easily diagnose the skin condition and get your child started on any treatment, if necessary.
Skin Conditions in Newborns | Advice for New Parents
It is not uncommon for babies to get skin rashes. Rashes can look different on different babies’ skin. As a parent, you may not know if the rash is something to worry about. Remember that you can always call your baby’s doctor’s office and ask to speak with a nurse if you are concerned. Some rashes are more commonly seen during the first few months of life.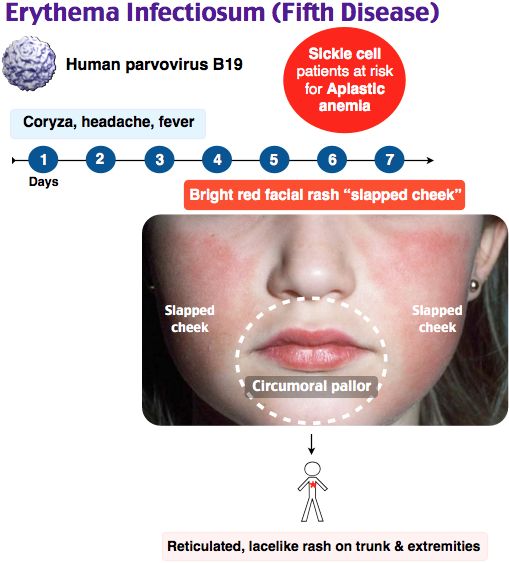
Baby Acne
You may think that only teens and young adults get acne. But your baby may get it too. Baby acne shows up around 2 to 3 weeks of age because of mom’s hormones. The pimples are harmless and won’t leave scars. Just leave them alone and keep the area clean with water only.
Cradle Cap
Cradle cap is very common, and just like its name implies, you typically see it on the scalp. Most of the time, it appears in the first several weeks after birth. It will get better on its own but may be treated if it becomes severe. Remember to call your baby’s doctor’s office and ask to speak with a nurse if you think your baby’s cradle cap is getting worse.
Eczema
(pronounced: ek-suh-muh)
Eczema can begin in the first few weeks of life, or may not begin until your baby is older. Eczema is dry skin that gets red and irritated, mostly seen on the scalp, face, trunk, elbows, knees or the diaper area. Apply Vaseline or an unscented moisturizing lotion to keep skin from becoming too dry. If the skin continues to look red and irritated, contact your baby’s doctor’s office and ask to speak with a nurse.
If the skin continues to look red and irritated, contact your baby’s doctor’s office and ask to speak with a nurse.
Erythema Toxicum
(pronounced: er-uh-thee-muh tox-i-cum)
Half of all newborns develop this rash, usually within two to three days after birth. The rash begins red and raised and can appear on the face, arms or legs. This is a normal baby rash. It is not warm to touch and does not cause any problems. There is nothing that needs to be done about it. It will go away within a few days.
Heat Rash
You may see this rash, sometimes called "prickly heat rash," if your baby gets too warm. You may notice it on your baby’s neck, armpits and diaper area. It may itch and make your baby uncomfortable. You can help by keeping your baby in a comfortable temperature. Most of the time, prickly heat will go away on its own in a couple of days.
Jaundice
(pronounced: jawn-dis)
Jaundice is commonly seen within a few days of birth. It appears as a yellowing of the skin, lips and eyes. Many babies go home from the hospital with a little bit of jaundice. But if your baby looks more yellow in the eyes or skin, is not eating well, not making as many wet diapers, or is hard to wake up, it is important to call your baby’s doctor’s office right away and ask to speak with a nurse.
Many babies go home from the hospital with a little bit of jaundice. But if your baby looks more yellow in the eyes or skin, is not eating well, not making as many wet diapers, or is hard to wake up, it is important to call your baby’s doctor’s office right away and ask to speak with a nurse.
Mongolian Spots
These gray-blue patches usually appear within the first year of life. They might look like a big bruise, but they do not hurt. They may show up on your baby’s back, bottom or legs. These spots are caused by simple differences in skin color and are perfectly harmless. They range from the size of a pinhead to 6 inches across.
Newborn Dry Skin
Dry skin is common. Your baby was surrounded by fluid in your womb for several months. It takes a while for your baby to get used to its new surroundings. There is no need to do anything. Your baby’s dry skin will get better on its own.
White Bumps Called Milia
(pronounced: mil-ee-uh)
Milia are small white bumps that are common on newborn skin. Milia are generally seen on the forehead, cheeks, nose and chin. Leave them alone. They will go away on their own.
Milia are generally seen on the forehead, cheeks, nose and chin. Leave them alone. They will go away on their own.
For Information
For more information, contact your child’s doctor’s office.
Reviewed by Nick DeBlasio, MD
Skin diseases in children | 1DMC
A child should not be taken lightly as a small adult. The child is not just small, it is characterized by anatomical, physiological, immunological and many other age-related features of childhood. These age features are also present in the skin.
The skin is the largest human organ. And also the most vulnerable. Often it is she who takes the first blow, and even more often she becomes a signaling system that says that something is going wrong in the body.
Skin diseases have different causes and course, but they have one thing in common - they often irritate patients more than any other diseases. Some skin conditions are mildly annoying, others cause pain.
Not every symptom is dangerous. But sometimes we ignore those symptoms that require urgent medical attention. Someone is embarrassed by the problem, someone is afraid of doctors, someone prefers to apply plantain.
Children's dermatologists of the First Children's Medical Center will tell in this article about the most common skin diseases in children, why they appear and how to deal with them.
The most common skin diseases in children
Herpes simplex. One of the most common viral skin diseases. Antibodies to this virus are found in 90% of people. The main symptom of herpes are fluid-filled blisters that appear in the mucosal area - more often the lips or nose. Lack of treatment can provoke a decrease in immunity and, as a result, an increased risk of acquiring new diseases.
Pyoderma are infectious skin diseases caused by pathogenic bacteria (staphylococci, streptococci, Proteus vulgaris, pneumococci, Pseudomonas aeruginosa, etc. ). Manifested by rashes of pustules and flaccid blisters (pustules and conflicts). The disease often proceeds acutely, sometimes chronically relapsing and rarely chronically.
). Manifested by rashes of pustules and flaccid blisters (pustules and conflicts). The disease often proceeds acutely, sometimes chronically relapsing and rarely chronically.
You can become infected through contact with infected people, animals and contaminated objects.
The main risk factors for the development of pyoderma are microtrauma, burns, softening of the skin during prolonged contact with water, general and local overheating or hypothermia, prolonged friction and pressure on the skin with tools and clothing.
Chronic purulent inflammation occurs when the body's reaction to pyococci changes. Patients with diabetes mellitus, blood diseases, immunodeficiencies, gastrointestinal diseases such as ulcerative colitis and Crohn's disease are susceptible to it.
Viral warts. A common viral skin disease caused by the entry of papillomavirus into human skin cells. Often the virus is transmitted by household means (when shaking hands, using carrier items). Convex nodules - warts are formed at the site of the introduction of the virus.
Convex nodules - warts are formed at the site of the introduction of the virus.
Molluscum contagiosum is a viral skin disease that manifests itself as pink hemispherical nodules with an indentation in the center. It got such an interesting name because of the similarity of nodules with a strong increase to a snail or a pearl. The disease has nothing to do with eating seafood or swimming in the sea.
The disease is caused by the molluscum contagiosum virus. In children, rashes usually appear on the trunk, limbs, head and neck. Infection occurs mainly by contact - by contact with the skin of an infected person or an infected object when visiting a swimming pool or sports sections.
Patients with atopic dermatitis are at risk of contracting molluscum contagiosum. Due to itching, multiple skin lesions (scratches and cracks) occur, through which the virus can spread from one part of the body to another. This leads to a relapsing course of the disease.
Microsporia ("ringworm"). It is an infectious skin disease caused by a fungus. At the beginning of its development, ringworm appears on the skin as a red, rough spot, and after a while it turns into an itchy red ring with swollen, rough edges.
This disease is transmitted through physical contact with a sick person or animal with hair (cats, dogs, hamsters, guinea pigs, rabbits).
There are also allergic and autoimmune skin diseases - they are not transmitted to other people
Atopic dermatitis - the inability of the skin to resist allergens, external irritants and pathogenic microorganisms. As a rule, a tendency to atopic dermatitis is in children whose close relatives suffer from the same disease.
The main symptom of atopic dermatitis is itching of varying intensity and rashes on the face, scalp, elbows and knees, the outer surface of the legs, forearms, trunk, buttocks, skin folds, dryness.
Due to the decrease in the protective function of the skin, patients with atopic dermatitis often develop secondary infections, bacterial: streptococcal, staphylococcal; viral: herpes simplex virus, human papillomavirus, which can lead to various complications.
Psoriasis is a systemic chronic skin disease. The development of psoriasis is promoted by hereditary predisposition, disorders of the nervous, endocrine, immune systems, psycho-emotional stress, chronic infections, and taking certain drugs. Psoriasis is a frequent companion of other diseases, such as: diabetes mellitus, diseases of the cardiovascular system, metabolic syndrome.
Psoriasis, like many other chronic skin diseases, is difficult to diagnose. The main signs of psoriasis are yellowish, pink-red rashes, gradually merging and forming scaly plaques of various shapes and sizes. Plaques can be found anywhere: the scalp, elbows, knees, lower back, palms and soles. Patients with psoriasis complain of itching of varying intensity.
Advanced cases of psoriasis can lead to pathological changes in the musculoskeletal system, often cases of nail psoriasis.
Allergic contact dermatitis is an inflammatory skin disease caused by a reaction to an allergen.
Identify several types of contact dermatitis:
- Acute contact dermatitis - occurs after a single contact with a substance that causes skin irritation
- Allergic contact dermatitis is an immune response of the skin to allergic substances.
Acute and allergic contact dermatitis are very similar in their manifestations: itching, burning, skin soreness, redness, swelling, rashes. In acute contact dermatitis, such manifestations are local in nature (exactly at the point of contact with the irritating substance). In allergic contact dermatitis, all of the above symptoms extend beyond exposure to the allergen and can appear anywhere on the skin.
- Chronic contact dermatitis - develops after repeated and prolonged contact with substances that have weak irritating properties, such as: cleaning solutions, acids and alkalis, powders. Chronic contact dermatitis is expressed by foci of soft redness, cracks, weeping, crusts, spots. Even after the elimination of the allergen, without proper treatment, the process can continue for years.

Seborrheic dermatitis is not just dandruff. Seborrheic dermatitis is a chronic skin disease in the form of peeling and rashes with frequent relapses.
The cause of seborrheic dermatitis may be the presence of the yeast fungus Malassezia spp., intense production of sebum of a modified composition caused by emotional stress, stressful situations, immune, neuroendocrine and hormonal disorders, as well as taking certain medications.
An early sign of seborrheic dermatitis is scalp dandruff. Later, itching, redness, peeling, plaques and crusts appear.
Seborrheic rashes can also appear on the face (in the area of the cheekbones, wings of the nose, forehead, eyebrows), auricles, upper body (in the area of the chest and shoulder blades), in large folds.
Urticaria. In case of urticaria on the skin of the face, shoulders, buttocks, thighs, blisters and swelling, red spots appear, sometimes accompanied by a burning sensation and itching.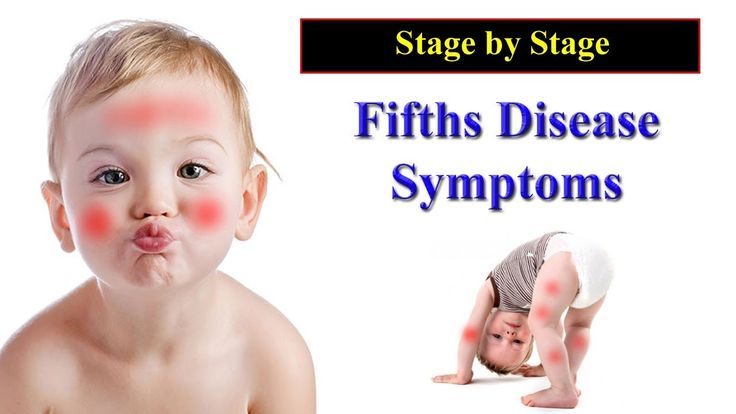
Urticaria may be caused by:
- eating foods rich in preservatives and dyes, flavor enhancers, citrus fruits, eggs, chocolate, nuts;
- taking certain medications (antibiotics, painkillers).
- infectious diseases
Acne. Acne, or acne, is an inflammatory skin disease resulting from blockage of the sebaceous glands. More than 80% of the world's population is prone to acne, most of them are teenagers.
There are several main factors influencing the development of acne: follicular hyperkeratosis, sebaceous hypertrophy, microbial colonization and inflammation.
The triggering factor is a genetically determined increase in the amount of androgens in the body and / or increased sensitivity of sebaceous gland cell receptors to testosterone derivatives. As a result of excessive production of sebum, hyperkeratosis occurs, which contributes to the formation of plugs at the mouth of the follicles. This leads to the accumulation of keratin masses, excess sebum and various bacteria in the lower part of the follicle. Then, successively, the expansion of the upper part of the hair follicle and the formation of a microcomedo occur. Microcomedone containing keratin, sebum and bacteria continues to expand, the wall of the follicle breaks, and the inflammatory process begins. Increased secretion of sebum leads to the growth of microorganisms (Propionibacterium acnes, Staphylococcus epidermidis, fungi of the genus Pityrosporum).
Then, successively, the expansion of the upper part of the hair follicle and the formation of a microcomedo occur. Microcomedone containing keratin, sebum and bacteria continues to expand, the wall of the follicle breaks, and the inflammatory process begins. Increased secretion of sebum leads to the growth of microorganisms (Propionibacterium acnes, Staphylococcus epidermidis, fungi of the genus Pityrosporum).
Decrease in the number of lactobacilli in the gastrointestinal tract, leading to an increase in blood lipids, is often cited as the cause of acne.
In addition, it has been noticed that people who eat a lot of foods rich in fats and fast carbohydrates suffer from acne more often.
Treatment of skin diseases in children
Everything is interconnected in our body and unfortunately there is no one universal remedy for the treatment of skin diseases. Therefore, the task of a dermatologist is to analyze the characteristics of the manifestations of the disease, identify the triggering mechanism of the disease (causes): the external environment (temperature changes, contact with an irritating substance), nutrition, lifestyle, stress, chronic diseases and hidden pathologies (diseases of the gastrointestinal tract, endocrine pathology, etc. ) and only after that treatment is prescribed, which consists of a complex and individually selected complex of various drugs, regular monitoring and evaluation of the effectiveness of therapy with possible subsequent correction.
) and only after that treatment is prescribed, which consists of a complex and individually selected complex of various drugs, regular monitoring and evaluation of the effectiveness of therapy with possible subsequent correction.
Therefore, if you experience any skin rash, you should contact a pediatric dermatologist as soon as possible. This will significantly reduce the duration of treatment, reduce the likelihood of infecting others.
At the First Children's Medical Center, you can get a consultation from a pediatric dermatologist in Saratov: our doctors aim not only to rid your child of the external symptoms of the disease, but also to find and eliminate the cause that caused it. At the First DMC, you can undergo all the necessary diagnostic procedures, as well as get advice from related specialists.
You can make an appointment with a pediatric dermatologist in Saratov at the First DMC from 8.00 to 20.00 by calling (8452) 244-000. Reception is by appointment.
What are the specific skin diseases in children of the first year of life?
In children of the first year of life there are features of the structure of the skin. Anatomical, functional feature their skin contributes to the very rapid appearance of scuffs, irritations and the spread of infection. Therefore, they often have skin diseases. Except specific skin diseases inherent only in children of the first year of life, they may have exactly the same dermatological diseases as older ones children and adults.
- Newborn pimples
Skin diseases may arise from the first month of life and manifest themselves in the form of various rashes. At first, they appear mainly on the face in the form of dots and are called milia. Cause in the fact that against the background of maternal hormones in children, a blockage of sebaceous and sweat glands. By the month, pimples spread all over the face. They are also called “pimples of newborns”, and people say - “the child is blooming”.
The child often touches his face and unclogs clogged pores. They get an infection from the skin, pimples form. They have nothing to do with allergies. At this age, the child develops rarely. In addition, allergic rashes never choose localization - not occur only on the face, or only on the neck, or on the upper chest. Allergic manifestations occur throughout the skin, and this is their main difference.
- Seborrheic crusts
A characteristic disease for children of the first year of life are seborrheic crusts. This is the secretion of the sebaceous glands near the hair follicles on the eyebrows and scalp. They show up at 2 months and go in 6-7 months. Seborrheic crusts require only processing: softening, moisturizing, a little combing - and not with a comb, but with your hands - after washing when the child's skin is steamed. These states do not represent any danger.
- Diaper dermatitis
In a child of the first year of life special skin. It often forms a variety of scuffs, especially when the skin rubs against clothes, or legs rub against each other. These abrasions should be immediately treated to prevent infection.
It often forms a variety of scuffs, especially when the skin rubs against clothes, or legs rub against each other. These abrasions should be immediately treated to prevent infection.
Most common rashes, abrasions, irritations and infections occur in the perineum. In another way, it is called "diaper dermatitis": what occurs under diaper when misused. This disease occurs in children from the first days of life. The child is in pain, the parents are worried. Need a consultation here pediatrician. Parents should discuss with him questions of choice and use diapers and treatment of various stages of diaper dermatitis.
Diaper dermatitis is one of the the most common reasons for visiting a pediatrician worldwide. But it is easily cured requires complex procedures. It is only necessary to create a barrier against further infections, maintain optimal humidity, apply products that have neutral pH, reduce the pain component. The pediatrician leading the child should teach parents how to care for the skin in the diaper area, methods of treatment diaper dermatitis. For treatment to be effective, it is necessary skin examination - it is required to assess the stage of diaper dermatitis, the degree skin lesions and the possible presence of an infectious agent.
For treatment to be effective, it is necessary skin examination - it is required to assess the stage of diaper dermatitis, the degree skin lesions and the possible presence of an infectious agent.
- Atopic dermatitis
Atopy is a type of allergy, not associated with a particular allergen. Roughly speaking, this is an allergy to any impact. Most often it is manifested by severe hyperemia. (redness), swelling, itching and rashes. Atopic dermatitis appears in very early age, literally from the first months of life. This dermatitis often occurs with intolerance to cow's milk protein. First of all, this concerns children who receive artificial feeding or little breast milk, but with This consume a lot of foods containing cow's milk protein. Unlike pimples of a newborn, rashes of atopic dermatitis appear all over body in the form of burn surfaces, especially in the popliteal and ankle areas, in the cervical folds and in the perineum.
Manifestations of this disease occur in children who are prone to atopic process. Usually these are large children with a so-called lymphatic constitution, who quickly put on weight.
Usually these are large children with a so-called lymphatic constitution, who quickly put on weight.
Atopic dermatitis can be of two types: food and contact. The first has to do with nutrition. In that In this case, the pediatrician must evaluate what the mother eats and work out a diet for her. diet moms shouldn't be stingy! In this case, her metabolic processes are disturbed, and the milk also becomes scarce. Ideally, you should try to identify a food allergen. The mother's diet should be handled by a qualified pediatrician, sometimes together with an allergist.
Atopy can also be caused by exposure to an external stimulus during contact interaction. This atopy occurs on washing powders or on some atmospheric manifestations. For example, it is known that in some children atopy can be a reaction to cold, water, changes in weather conditions - that is, literally on any irritant.
Treatment of atopic dermatitis in children of the first year of life is carried out by a pediatrician, and only in the absence of effect, they turn to a dermatologist and an allergist. Atopic manifestations can be long and go into neurodermatitis, eczema and other conditions. Therefore, the treatment of older children is most often carried out jointly. pediatricians and dermatologists.
Atopic manifestations can be long and go into neurodermatitis, eczema and other conditions. Therefore, the treatment of older children is most often carried out jointly. pediatricians and dermatologists.
- Child supervision the first year of life in the Ilyinsky hospital
A pediatrician is the first line of defense for a family. Pediatricians Ilinskaya hospitals monitor the development of the child, carry out the correction of functional disorders and treatment of diseases. We advise parents on basic issues of concern to the family - feeding, assessment of physical and psychomotor development, vaccination, give advice within the framework of the program "Care for development".
At the Ilyinsky hospital, we adhere to internationally recognized position: the child needs additional consultations only if a pediatrician identifies a problem, or if he has doubts about any question. The timing of the examination of the child by narrow profile doctors is determined an objective need for the child, and not just conditional periods of his life.