What is a cervix sweep
What you need to know before your membrane sweep
The stretch and sweep, or membrane sweep, done late in pregnancy can help you go into labour sooner. Here’s what you’ll want to know before you get it done.
When you’re so pregnant and uncomfortable you can barely roll over in bed, you may not know what to think when your doctor or midwife suggests an even more uncomfortable procedure to hurry up labour: a stretch and sweep. Is it worth the additional pain and discomfort you might endure? Here’s what you need to know about what happens in the procedure, why it’s done and how you’ll feel both during and after. (The great news: It’s not as bad as you might think.)
How does a stretch and sweep work?Also referred to as a membrane sweep, a membrane stripping or simply a sweep, this technique involves gently lifting the amniotic sac—or fetal membrane—from the cervix and lower part of the uterus. Late in pregnancy, a doctor or midwife inserts a gloved finger through the cervical canal and uses a sweeping motion to separate the membrane from the cervix. This “sweep,” releases prostaglandins, which are chemicals that help soften and open the cervix for delivery. “The hope is to accelerate that onset of labour by the increase of prostaglandins,” explains George Carson, a Regina-based obstetrician.
The “stretch,” which refers to gently widening the inner part of the cervix, is meant to further stimulate labour. Alix Bacon, a registered midwife in Ladner, BC, says while one finger is required for a membrane sweep, a stretch needs two fingers to be able to fit through the cervix in order to “literally stretch those fingers apart.” If your cervix isn’t ready to be widened, this part of the procedure won’t be done, she says.
Why do you get a membrane sweep?A stretch and sweep is not an induction; rather, it’s an equipment-free, drug-free way to coax someone already in late pregnancy into spontaneous labour. The main purpose of a stretch and sweep is to reduce the need for a medical induction after the due date, says Dustin Costescu, an obstetrician in Hamilton, Ont. “Because it causes a natural release of chemicals, it is less risky than medications used for induction such as oxytocin or prostaglandin gels,” he explains. Contescu says some women even request a stretch and sweep to help get labour started, particularly if they have a history of going past their due date. It’s a completely optional procedure—even if your caregiver suggests it.
“Because it causes a natural release of chemicals, it is less risky than medications used for induction such as oxytocin or prostaglandin gels,” he explains. Contescu says some women even request a stretch and sweep to help get labour started, particularly if they have a history of going past their due date. It’s a completely optional procedure—even if your caregiver suggests it.
You may go into active labour within a few hours, a few days, or not at all—it depends on how ready your body is. “One sweep might not do anything, but if you have a sweep at weeks 38, 39 and 40, it’s the cumulative effect of those sweeps,” says Bacon.
Is a stretch and sweep safe?It’s a safe procedure, but Costescu says in very rare cases your water will break inadvertently. “While messy, this is not generally harmful,” he says. As with any time in your pregnancy, if you experience leaking fluid or heavy bleeding afterwards, call your healthcare provider.
When can you get a membrane sweep?It’s only offered at 38 weeks or later, and in order to do a sweep, the cervix must already be partially opened, explains Kim Campbell, a registered midwife in Vancouver. If your body isn’t readying itself for labour, the cervix will be out of reach and firmly closed, so the sweep can’t be done. “If this is the case, the care provider normally just massages the cervix and there is no contact possible with the membranes,” she says. The massage will help stimulate the area and hopefully soften the cervix.
If your body isn’t readying itself for labour, the cervix will be out of reach and firmly closed, so the sweep can’t be done. “If this is the case, the care provider normally just massages the cervix and there is no contact possible with the membranes,” she says. The massage will help stimulate the area and hopefully soften the cervix.
Campbell says some of her patients describe a stretch and sweep as uncomfortable, while others call it painful. “Any pain is short-lived, and when the procedure is done, there is no residual pain,” she offers. The whole procedure, which can be done at the doctor’s office, in a midwife’s clinic or at home, is over in about a minute, and you’ll be fine to drive home afterwards if needed. Later that day, you may have period-like cramps along with some light spotting, which is all normal.
In the end, you’re the only person who can decide if it’s the right procedure for you. But if you’re anxious to go into labour, or worried about being induced, it’s a safe, fairly simple step that could have you meeting your little one very soon.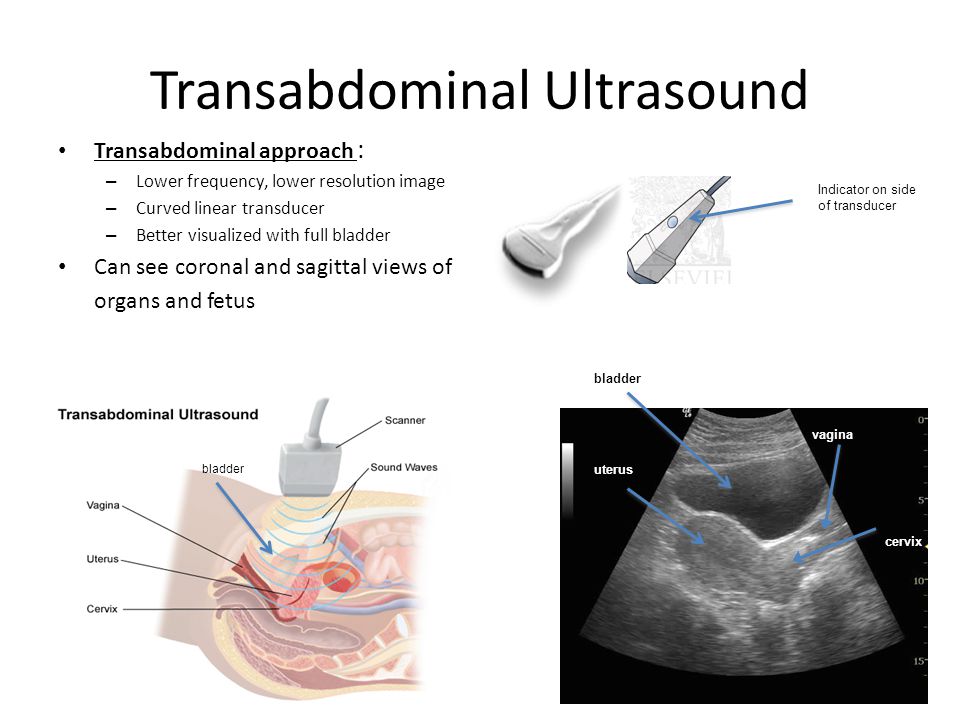
Watch Baby Grow!
Subscribe to Today’s Parent’s baby newsletter and find out what to expect for every stage and milestone, from birth to two years.- Email*
- Baby's due/birth date*
Month223456789101112
Day12345678910111213141516171819202122232425262728293031
Year2024202320222021
- CAPTCHA
- Consent*
Yes, I would like to receive Today's Parent's Baby newsletter. I understand I can unsubscribe at any time.**
FILED UNDER: birth Giving birth health service seo Labour and delivery Pregnancy
Stretch and sweep | Pregnancy Birth and Baby
Stretch and sweep | Pregnancy Birth and Baby beginning of content3-minute read
Listen
What is a stretch and sweep?
A stretch and sweep or membrane sweep is a relatively gentle way of trying to start labour. It is a simple procedure that sometimes initiates labour, reducing the risk of babies being born over the due date (42 weeks of pregnancy).
It is a simple procedure that sometimes initiates labour, reducing the risk of babies being born over the due date (42 weeks of pregnancy).
When is a stretch and sweep offered?
Your midwife or doctor may offer to perform a stretch and sweep when you have reached full term (38 weeks) to try to start labour. Some hospitals and doctors recommend the procedure only if you are 40 to 41 weeks pregnant in an attempt to prevent an overdue delivery, which may place the baby at risk.
What to expect from a stretch and sweep
The procedure is carried out by a midwife or doctor as part of an internal vaginal examination. They put a couple of lubricated, gloved fingers into your vagina and insert their index finger into the opening of the cervix or neck of your womb
They then use a circular movement to try to separate the membranes of the amniotic sac, containing the baby, from your cervix. This action, which releases hormones called prostaglandins, prepares the cervix for birth and may initiate labour.
Your midwife or doctor will:
- check the estimated date of delivery
- ask you to empty your bladder and lie down
- detect your baby’s position by feeling your abdomen
- do an internal examination to find if your cervix is closed or open
- massage around the neck of your womb if it is soft but closed — this 'stretch' can stimulate your body to release prostaglandins, which encourage the cervix to open
- insert an index finger into the neck of the womb, if it is open, and use circular motions to loosen or 'sweep' the amniotic sac membranes from the top of the cervix — this triggers the release of hormones and may start labour
If you find the procedure too uncomfortable, ask your midwife or doctor to stop.
Afterwards you might experience:
- discomfort
- mild or occasionally strong pain
- slight bleeding
- cramps or irregular contractions
Take paracetamol and have a warm bath if you are in pain. If your membranes rupture, the pain is bad or you have fresh, red bleeding, contact your midwife, doctor or maternity unit.
If your membranes rupture, the pain is bad or you have fresh, red bleeding, contact your midwife, doctor or maternity unit.
The process can be repeated if labour does not start over the next couple of days.
What are the benefits and risks of a stretch and sweep?
Stretch and sweep procedures at 41 weeks of pregnancy greatly reduce the percentage of women who deliver their babies beyond term. They may be offered as an alternative to inducing birth through medication or by rupturing the membranes.
The procedure is safe in a normal pregnancy. There is a slight chance the membranes may break during the procedure.
Ask your doctor or midwife about the benefits and risks before agreeing to a stretch and sweep procedure.
Sources:
BabyCenter (What is a membrane sweep?), Queensland Health (Queensland Clinical Guidelines, Induction of labour), The Royal Hospital for Women (Sweeping membranes to encourage spontaneous labour), Cochrane (Membrane sweeping for induction of labour), NSW Health (Pregnancy beyond 41 weeks)Learn more here about the development and quality assurance of healthdirect content.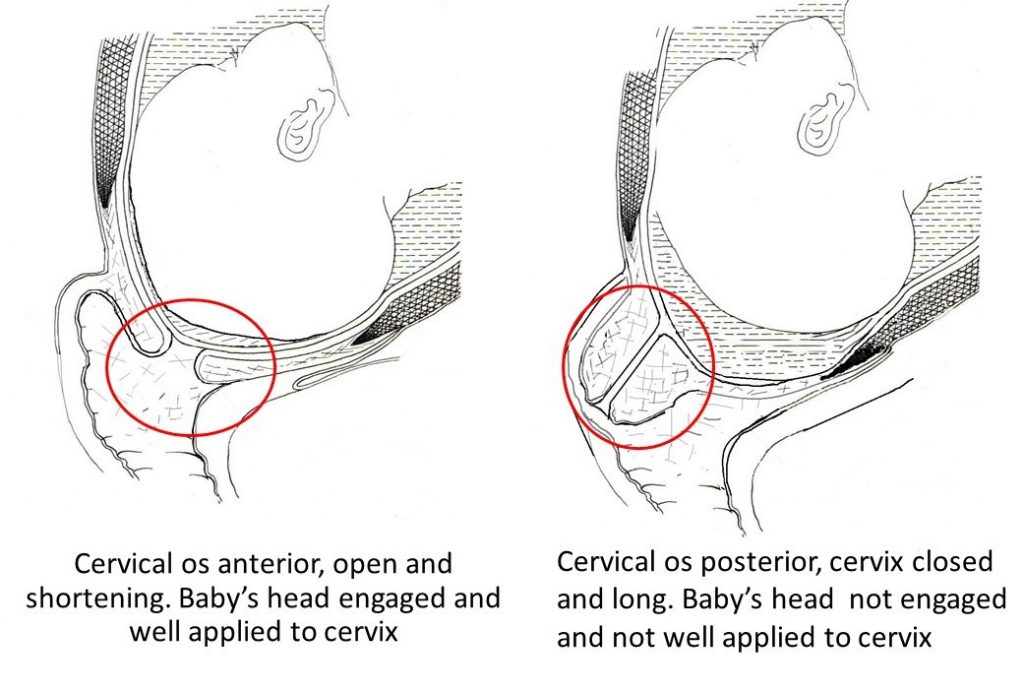
Last reviewed: January 2021
Back To Top
Related pages
- Having the baby
Need more information?
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.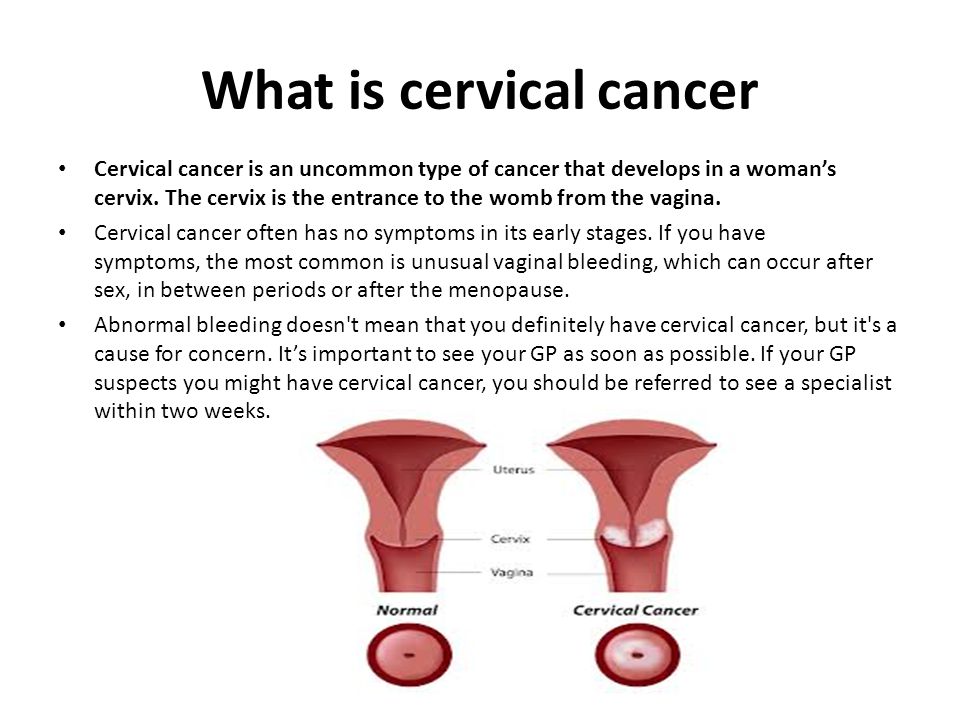
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.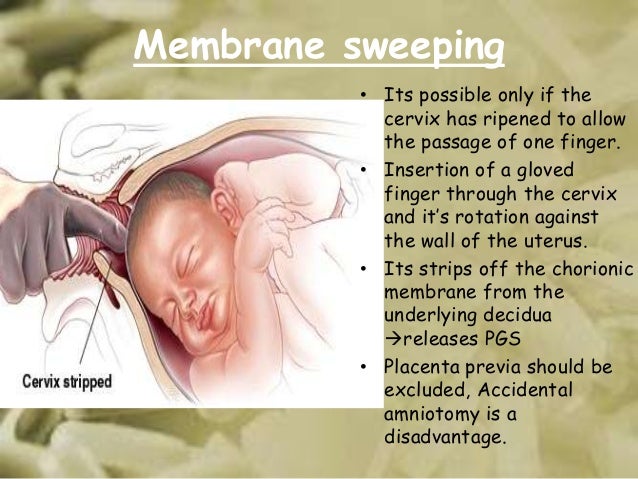
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
🎖▷ Why you don't have to worry about weight gain with Lamictal
psychology
4,569 2 minutes read
If you're worried that taking Lamictal (lamotrigine) may cause weight gain, there's good news. It probably won't affect your weight much. If anything, you're more likely to lose weight due to Lamictal than gain weight, but either way, the changes are likely to be pretty small.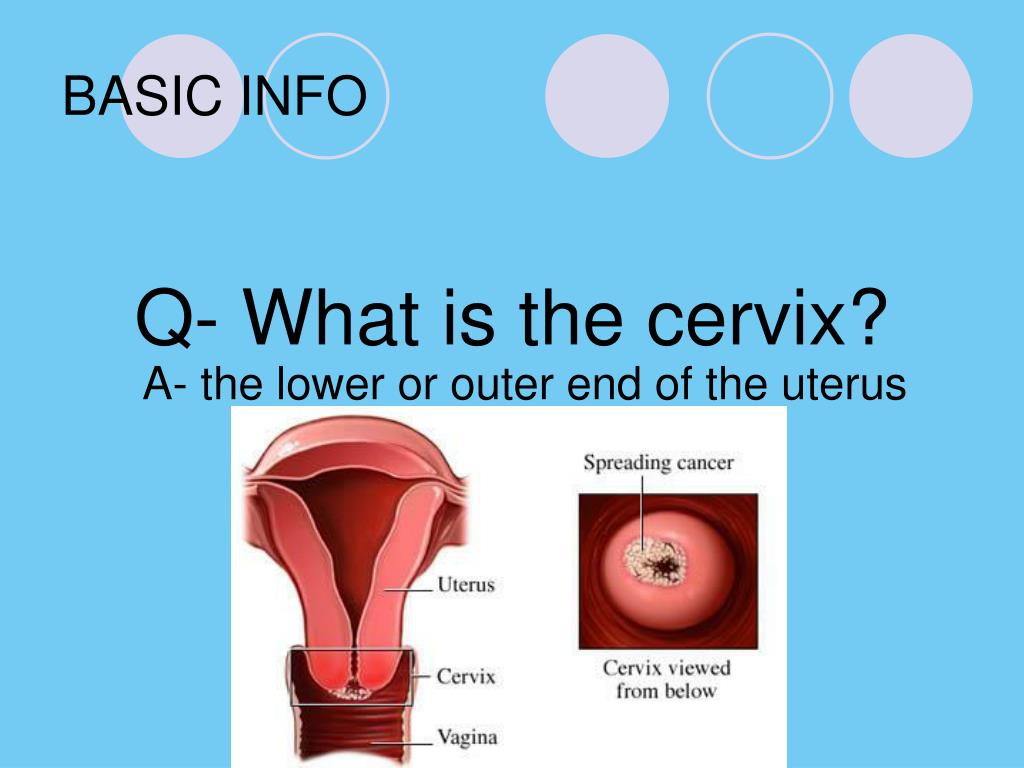
The effect of Lamictal on weight has been little studied and various clinical trials have found minimal effect. In fact, some researchers even considered the drug as a possible remedy for obesity and as a remedy for overeating. This information should be reassuring for people with bipolar disorder, as many of the medications used to treat this condition can cause weight gain.
Lamictal findings and weight gain or loss
Lamictal is an anticonvulsant that can be used to treat seizures such as epilepsy. It is also used as a mood stabilizer for bipolar disorder.
In the first clinical trials with the drug, 5 percent of adults with epilepsy lost weight while taking Lamictal, while 1 to 5 percent of patients with bipolar I disorder gained weight while taking the drug. The researchers do not disclose how much weight patients have gained or lost.
Meanwhile, a 2006 study comparing the effects on weight of Lamictal, lithium, and placebo found that some Lamictal-treated patients gained weight, some lost weight, and most remained about the same weight.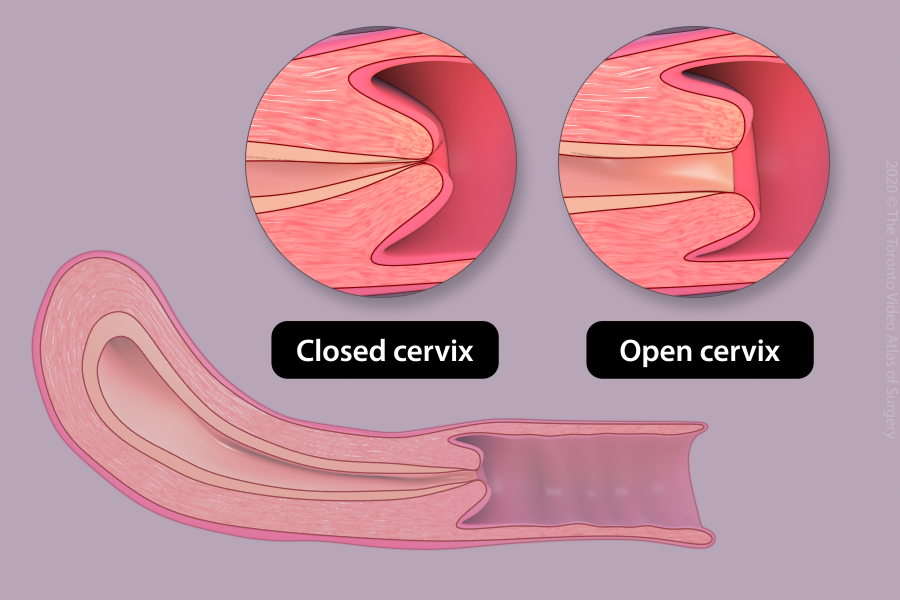 Weight changes are usually not many pounds anyway. Obese patients taking Lamictal lost an average of four pounds, while the weight of non-obese patients remained virtually unchanged.
Weight changes are usually not many pounds anyway. Obese patients taking Lamictal lost an average of four pounds, while the weight of non-obese patients remained virtually unchanged.
Relationship between weight gain and other bipolar drugs
Weight gain from medications used to treat bipolar disorder is unfortunately quite common. Some mood stabilizers commonly used for bipolar disorder, especially lithium and Depakote (valproate), carry a high risk of weight gain.
In addition, the atypical antipsychotics Clozaril (clozapine) and Zyprexa (olanzapine) tend to cause significant weight gain in people who take them. Finally, some antidepressants, notably Paxil (paroxetine) and Remeron (mirtazapine), have been associated with weight gain.
Therefore, if you are already overweight, you and your psychiatrist may want to consider additional weight gain when determining your bipolar medication regimen. Based on this, Lamictal may be a good choice.
Lamictal as a possible treatment for obesity
Lamictal has also been studied as a possible treatment for obesity in people without epilepsy or bipolar disorder.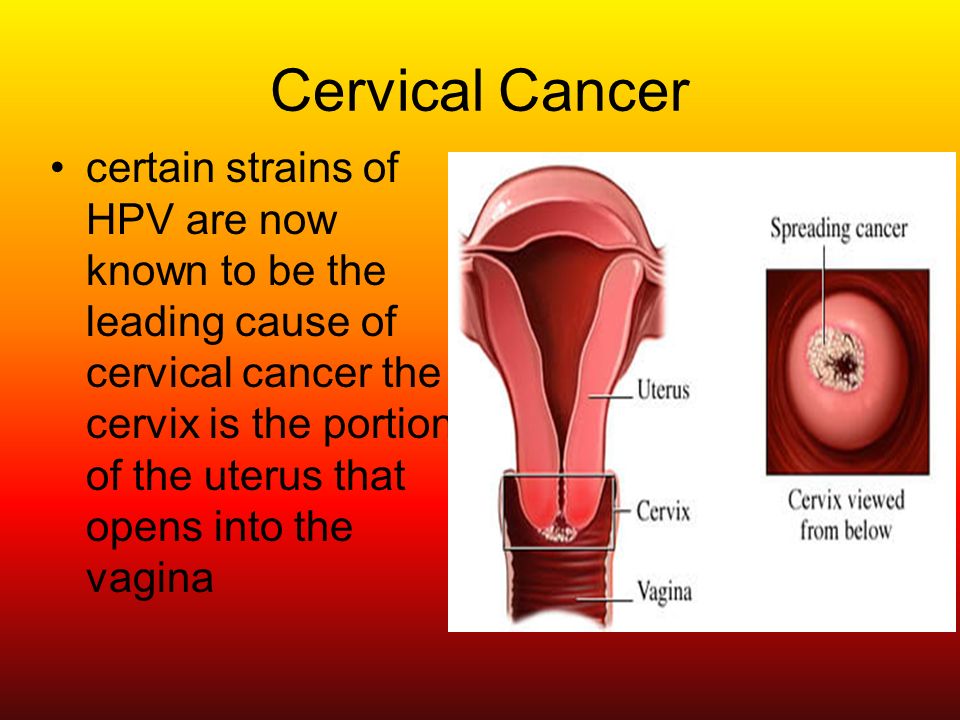
In a small clinical study of 40 people conducted in 2006, researchers randomly assigned participants to receive either lamiktal or placebo for up to 26 weeks. Each participant in the study had a body mass index (BMI) between 30 and 40, placing them in the obese group to the level of severe obesity. Those who took Lamictal lost an average of just over 10 pounds. Those who took the placebo lost about 7 pounds in the meantime, so while those who took Lamictal lost more weight, they didn't lose all that much more.
Another study in 2009 looked at Lamictal as a remedy for overeating. This study involved 51 people with the condition that 26 of them received Lamictal, and 25 - placebo.
Those who took Lamictal lost more weight than those who took placebo (about 2.5 pounds vs. about one third of a pound) and did have significant improvements in blood sugar and cholesterol lab test results. However, Lamictal did not appear to affect other aspects of the eating disorder when compared to placebo.
Tags
Lamictal You don't need to worry about why increases
Back to top button
Strippen Russisch - Voorlichting Vertaald
In the Netherlands, you can wait up to 42 weeks of pregnancy to find out if you spontaneously deliver. Pregnancy beyond 42 weeks can be hazardous to your baby's health. If you haven't had a spontaneous delivery at 42 weeks, your midwife will refer you to a gynecologist in the hospital. At the hospital, labor is induced with an IV to induce contractions. If you don't want to give birth in a hospital and don't want to induce contractions with medication, a midwife can help you have a spontaneous birth up to 42 weeks. The midwife may begin to "tear" your membranes from 41 weeks pregnant to increase the chances that you will give birth.
1. Induce labor with a reamer
When removing the membranes, the midwife separates the membranes that surround the placenta from the cervix.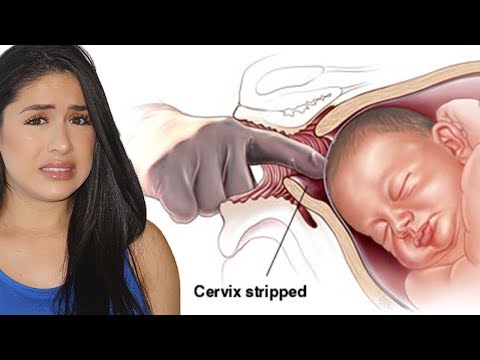 This releases hormones that soften the cervix and usually induce labor.
This releases hormones that soften the cervix and usually induce labor.
2. Membrane reamer - yes or no?
Membrane reaming is mainly done if you do not want to give birth in the hospital and if you have not yet had a baby at 41 weeks. You are allowed to wait no more than 7 days until you can give birth at home and have to go to the hospital. The midwife may also decide to rupture the membranes if you feel very tired and can no longer support the pregnancy (you are ready for delivery).
3. What is a membrane reamer
First, the midwife will perform an external examination and listen to the baby's heartbeat. She will then do an internal examination during which she inserts 1 finger into your vagina and checks to see if you are dilated. If the midwife can insert a finger into the cervix, the procedure can be performed. The midwife then makes three circles around the baby's head, causing the membranes to move away from the uterine wall.
4.
 How often
How often Membrane reaming does not always lead to labor induction. If the sweep is effective, contractions should begin within 20 hours. Note: These are regular abdominal cramps that occur every 3-5 minutes and last at least 1 minute. If you have irregular spasms that also go away, it is most likely Braxton-Hicks contractions, but not yet a sign of labor onset. If you do not have contractions within 20 hours, the midwife may re-examine. We always do this one day apart so your body can recover too.
5. Does it hurt?
Reaming can be painful, but it doesn't have to be. Rotation and loosening of the membranes can cause pain. There may also be pain in the abdomen.
6. Blood loss
There may be some blood loss after the scan, this is normal. It is best to put a gasket after reaming. Pay attention: is your pad full of blood or is it dripping down your legs? Then call the midwife immediately, even at night!
The phone number of the midwife: .