Where is the placenta during pregnancy
About the placenta – role and complications
About the placenta – role and complications | Pregnancy Birth and Baby beginning of content7-minute read
Listen
What is the placenta?
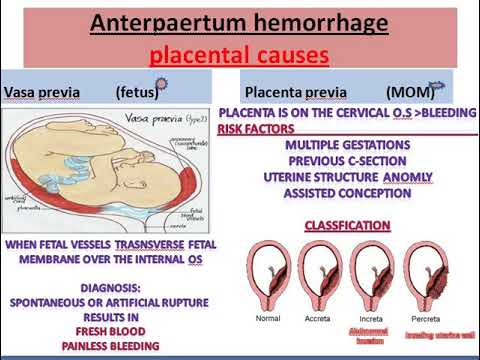
The placenta is a temporary organ that develops during pregnancy. It attaches to the lining of your uterus and delivers oxygen and nutrients to your growing baby through the umbilical cord.
If something goes wrong with the placenta, it can be serious and even life-threatening to both mum and baby.
What is the role of the placenta during pregnancy?
The placenta passes oxygen, nutrients and antibodies from your blood to your baby. It also carries waste products from your baby back to your blood, so your body can get rid of them.
The placenta also produces some hormones like oestrogen and progesterone that are needed during pregnancy.
What is the normal position of the placenta during pregnancy?
The placenta should attach to the wall of the uterus, usually at the top, side, front or back. The exact location will vary from person to person and in each pregnancy.
The placenta can sometimes develop low in the uterus but will generally move higher as your uterus stretches. The position of the placenta will be checked at your 18-week ultrasound.
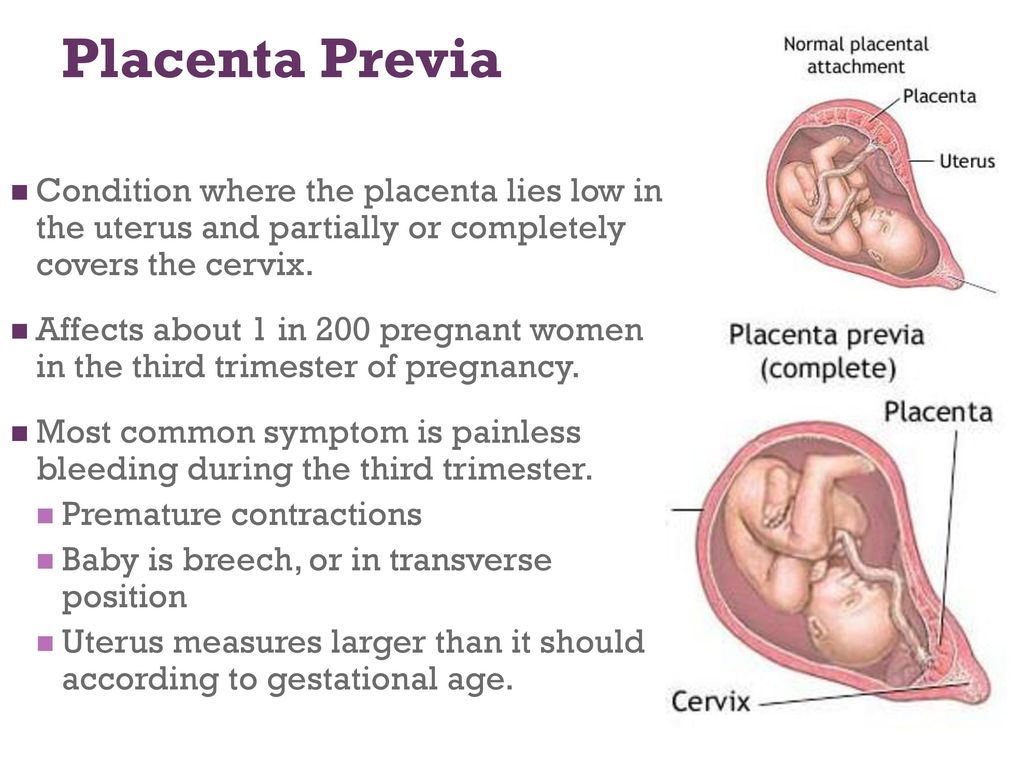
This image shows a normal placental location, with the placenta attached at the top of the uterus.How does the placenta work in twin pregnancies?
Fraternal twins come from separate eggs and each have their own placenta. Identical twins come from the same egg that separates, and they may share a placenta or have their own.
Can medicines cross the placenta?
Alcohol, nicotine, medicines and other drugs can cross the placenta and affect your baby’s health.
What should I do to keep my placenta healthy during pregnancy?
It’s important to visit your healthcare provider regularly during pregnancy. If there are complications, they can be identified during these appointments.
If there are complications, they can be identified during these appointments.
Tell your doctor if you have had problems with the placenta in a previous pregnancy, or if you have had any surgery to your uterus.
If you smoke, drink alcohol or take certain drugs during pregnancy, this increases the likelihood of problems with the placenta.
Always consult your doctor before you take any medicines, including over-the-counter medicines, natural therapies and supplements, while you are pregnant.
Speak with your doctor or midwife if you have any concerns, or if you experience:
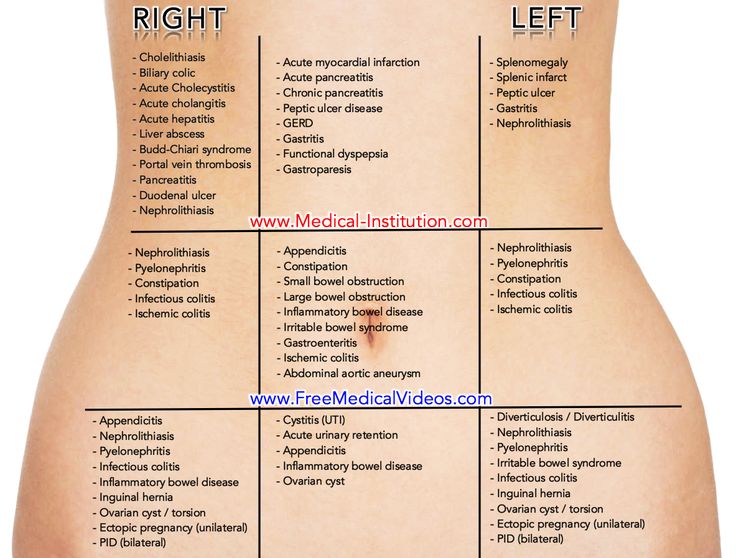
- severe abdominal (stomach) pain or back pain
- vaginal bleeding
- contractions
- any trauma to your abdomen, for example from a fall or car accident
What happens to the placenta after my baby is born?
After your baby is born, you will need to birth your placenta. This is called the third stage of labour.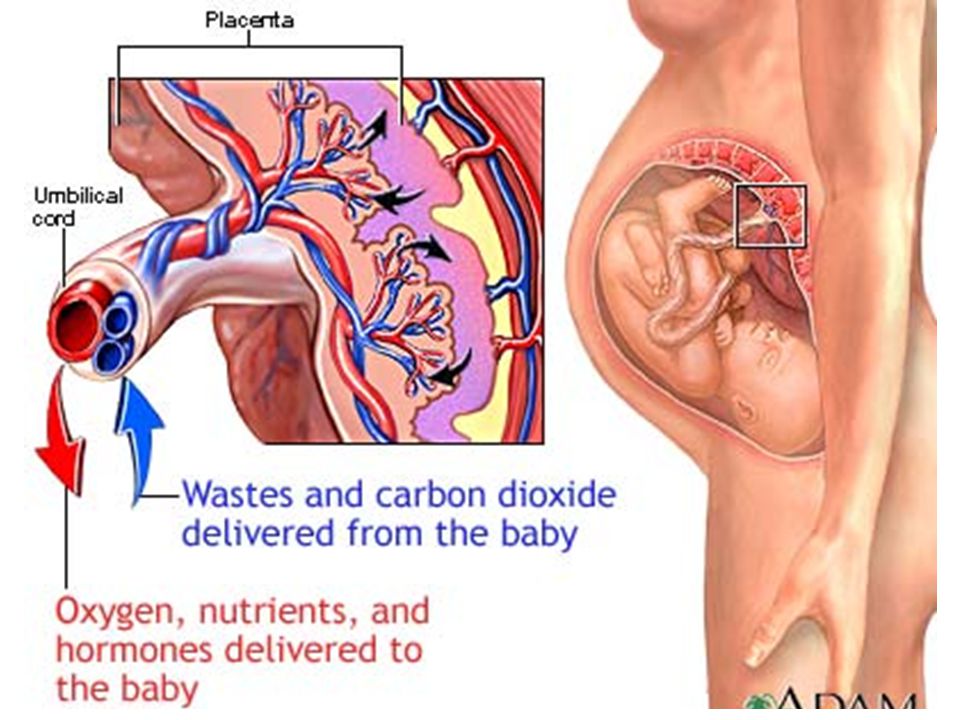 This stage of labour can be managed in different ways.
This stage of labour can be managed in different ways.
If you had a vaginal birth, you will usually have some mild contractions and need to give a few pushes to help your placenta to come out.
If you have a caesarean section, your doctor will remove the placenta at the same time your baby is born.
Once you birth your placenta your doctor or midwife will check that it looks complete. If there is any concern that your placenta isn’t complete, they may suggest further investigations. If any bits of placenta are retained (stay inside you), they may have to be surgically removed to prevent infection.
Can I take my placenta home with me?
It is your choice what you do with your placenta. You may choose to discard it; in which case your hospital or birthing centre will take care of this.
If you wish to take your placenta home, you can speak to your doctor or midwife to arrange this.
In some cultures, people bury the placenta in a special place.
‘Placentophagy’ is a practice where people cook and eat their placenta. There is no research to support health benefits from this. However, you may choose to do this for cultural, spiritual, or personal reasons.
There is no research to support health benefits from this. However, you may choose to do this for cultural, spiritual, or personal reasons.
Some commercial service providers offer to turn your placenta into capsules for you to swallow. It should be noted that there may be a risk of infection from poor preparation. These practices should be treated with caution.
Can anything go wrong with my placenta?
Problems with your placenta can happen during pregnancy, birth and after birth. These are potentially dangerous for both you and your baby.
If your bleeding is severe and you have significant pain, call triple zero (000) for an ambulance or go to your nearest hospital emergency department.
If you have any vaginal bleeding during pregnancy, it’s important to see your doctor as soon as possible.
Placental abruption is when some or all the placenta comes away from the wall of the uterus before your baby is born.
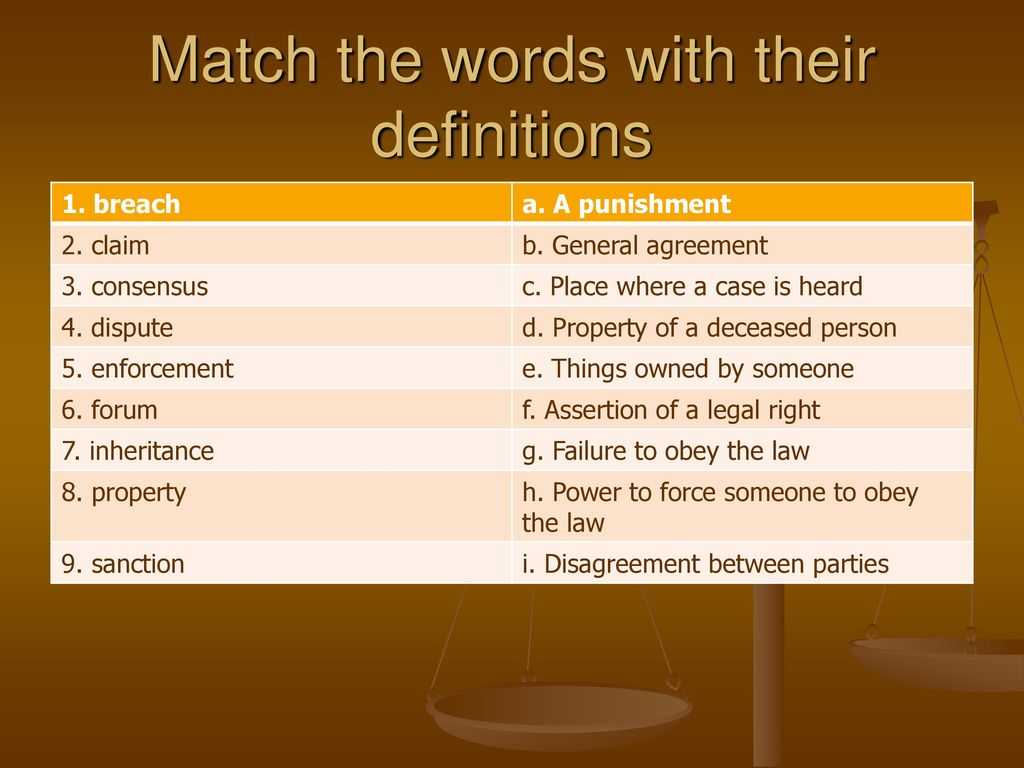
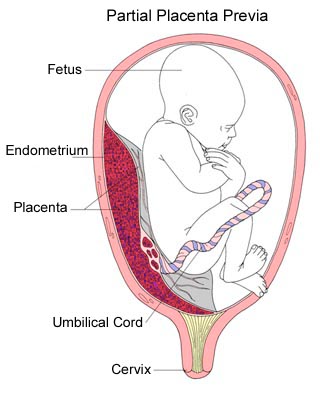
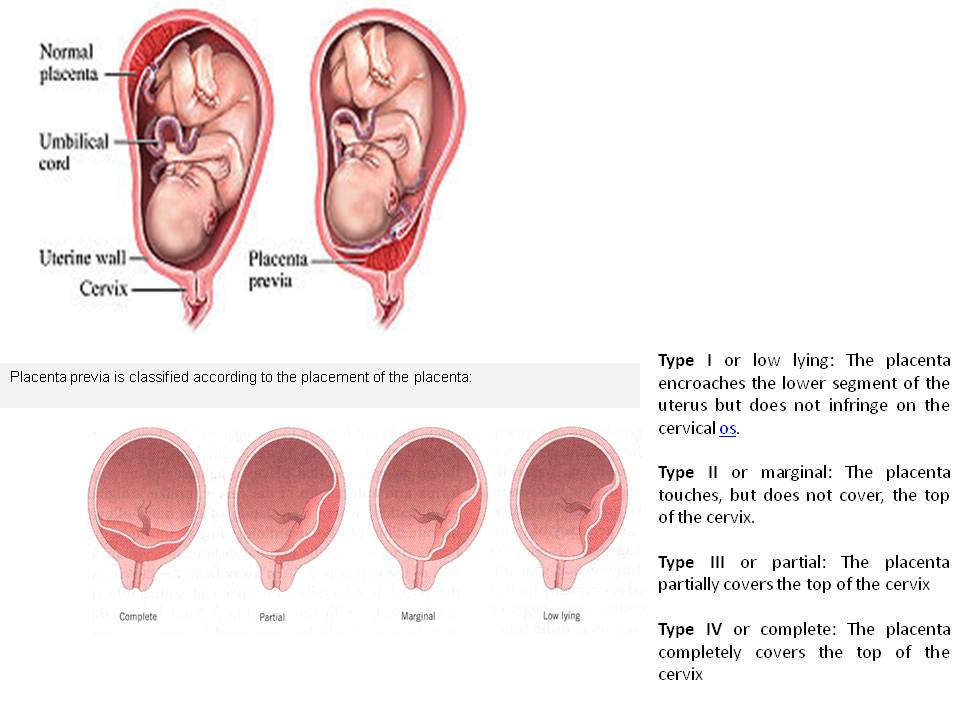
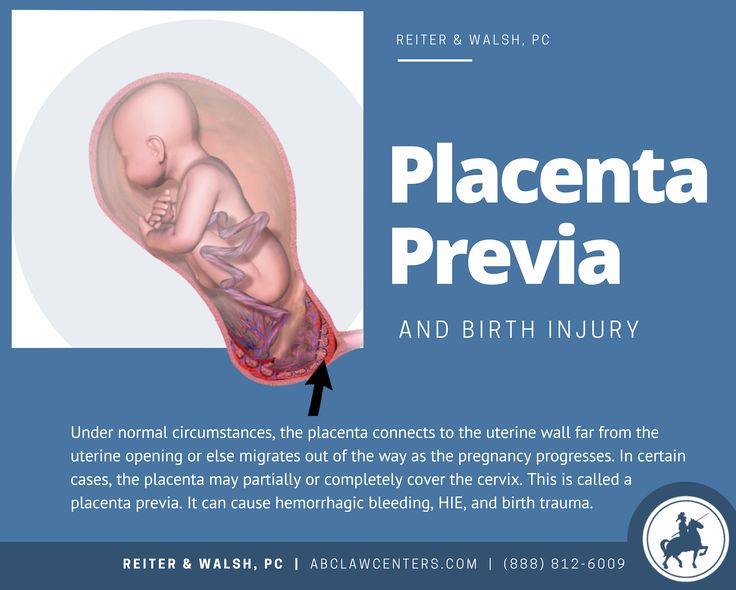
Placenta praevia is when the placenta partially or totally covers the cervix (the narrow opening in the uterus).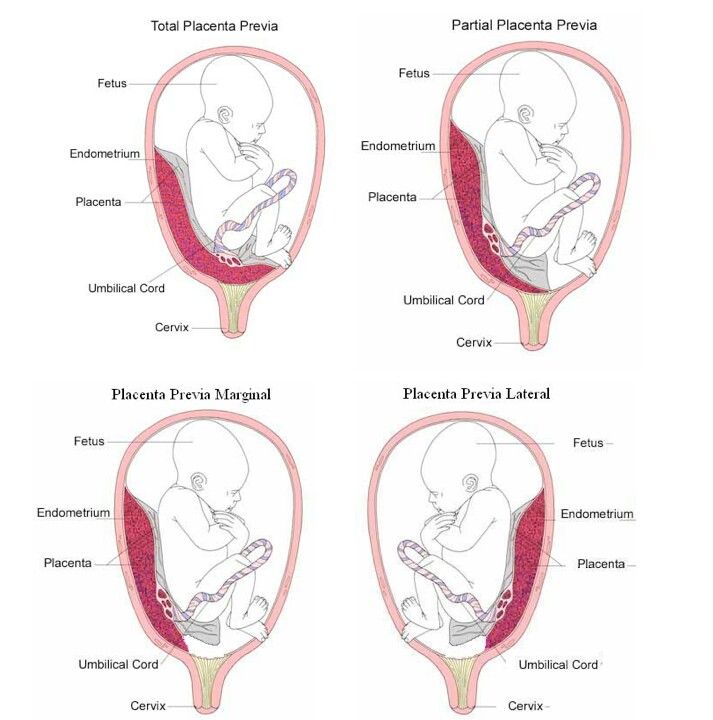
Placental insufficiency is when the placenta doesn’t work properly during pregnancy. It deprives the baby of oxygen and nutrients they need to grow and develop.
Placenta accreta is when the placenta grows too deeply into the wall of the uterus. This can lead to severe bleeding during or after delivery and can be life-threatening.
Retained placenta is when your placenta does not completely come out after the birth. This might be because it is stopped by your cervix or is still attached to your uterus.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
UNSW Embryology (KA02 Fetus or newborn affected by complications of placenta), Royal Women's Hospital (Placenta problems), RANZCOG (Intrauterine Growth Restriction: Screening, Diagnosis, and Management - Placenta accreta), The Royal Women’s Hospital Victoria Australia (Taking Your Placenta Home For Burial Or Consumption), International Journal of Women’s Health (Retained placenta after vaginal delivery: risk factors and management), NHS UK (What complications can affect the placenta?)Learn more here about the development and quality assurance of healthdirect content.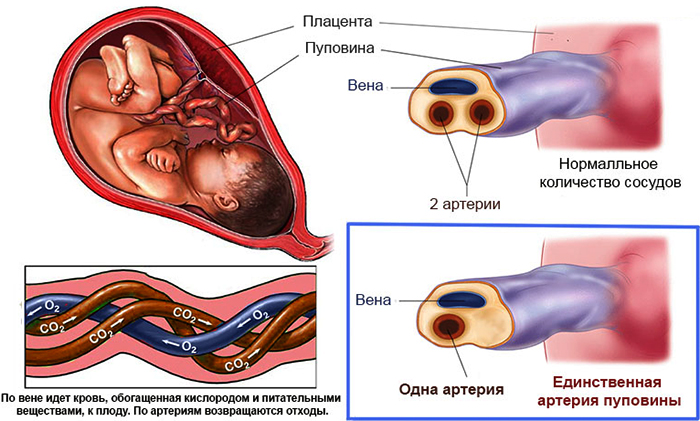
Last reviewed: July 2022
Back To Top
Related pages
- Mum's first 24 hours after birth
- Giving birth - stages of labour
- Placenta complications in pregnancy
Need more information?
Placenta previa - Better Health Channel
Placenta previa means the placenta has implanted at the bottom of the uterus, over the cervix or close by.
Read more on Better Health Channel website
Retained placenta
A retained placenta is when part or all of the placenta is not delivered after the baby is born. It can lead to serious infection or blood loss.
Read more on Pregnancy, Birth & Baby website
Placenta praevia
Placenta praevia is a condition where the placenta lies low and may cover the cervix, blocking the baby's exit during birth.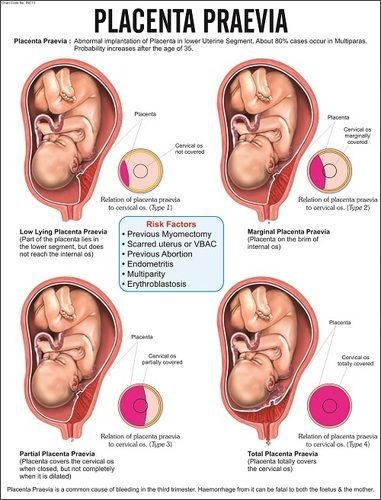
Read more on Pregnancy, Birth & Baby website
Placenta accreta
Placenta accreta is a serious but rare pregnancy complication that causes heavy bleeding. If you have it, you will need special care at the birth.
Read more on Pregnancy, Birth & Baby website
Placental abruption - Better Health Channel
Placental abruption means the placenta has detached from the wall of the uterus, starving the baby of oxygen and nutrients.
Read more on Better Health Channel website
Placental insufficiency
Placental insufficiency occurs when the placenta does not work properly and your baby doesn't get the oxygen and nutrients they need.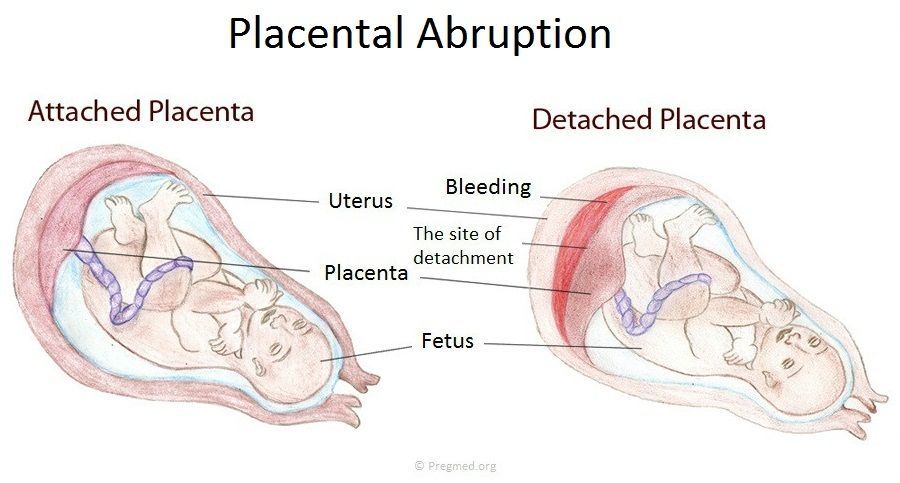
Read more on Pregnancy, Birth & Baby website
It is not just a woman’s issue - Alcohol and Drug Foundation
If a woman drinks during pregnancy the alcohol crosses the placenta to the baby. But what about the effect of alcohol on men?
Read more on Alcohol and Drug Foundation website
Placental abruption
Placental abruption is when some or all of the placenta peels away from the uterus wall before birth. It can deprive the baby of oxygen and nutrients.
Read more on Pregnancy, Birth & Baby website
Pregnancy test - Pathology Tests Explained
Starting approximately two weeks after conception, a hormone called human chorionic gonadatropin (hCG) hormone is produced by the developing placenta and can be detected in urine and in blood
Read more on Pathology Tests Explained website
4 weeks pregnant: Key points
When you are 4 weeks pregnant your body and your new baby are undergoing rapid changes. The placenta forms and begins producing a hormone called human chorionic gonadotrophin (hCG), which is the substance a pregnancy test detects to confirm you are pregnant. The cells which are growing into your new baby establish membranes which connect them to the placenta and prepare themselves for differentiation into different types of cells, which will occur next week when you are 5 weeks pregnant. These developments may cause you to experience unusual emotions and also cause changes in your body such as darkening of the areolas of your nipples.
The placenta forms and begins producing a hormone called human chorionic gonadotrophin (hCG), which is the substance a pregnancy test detects to confirm you are pregnant. The cells which are growing into your new baby establish membranes which connect them to the placenta and prepare themselves for differentiation into different types of cells, which will occur next week when you are 5 weeks pregnant. These developments may cause you to experience unusual emotions and also cause changes in your body such as darkening of the areolas of your nipples.
Read more on Parenthub website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.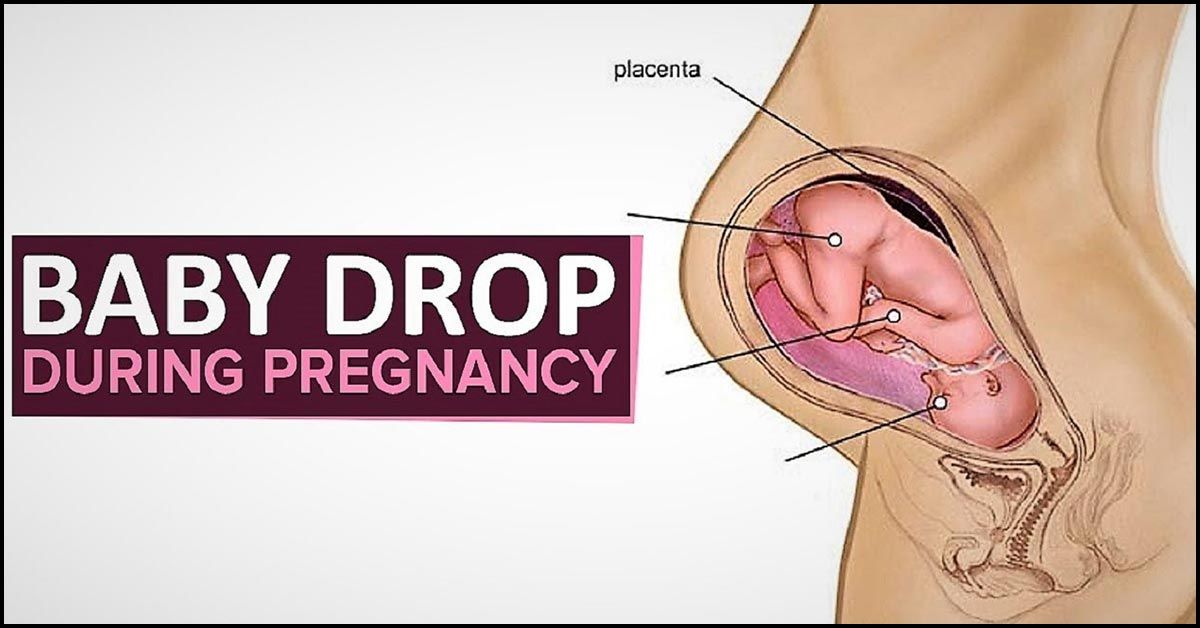
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.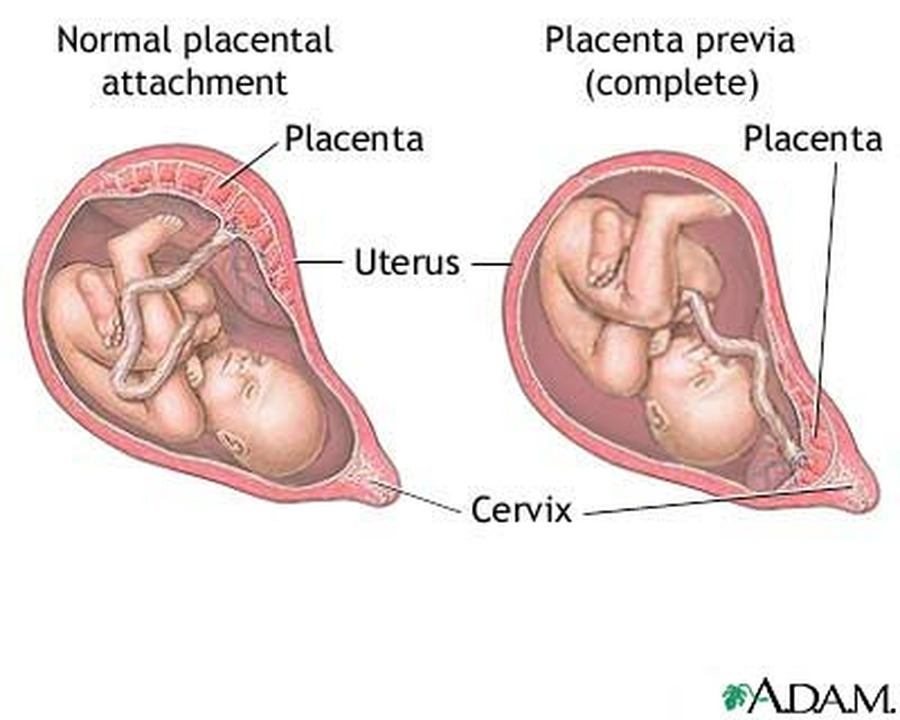
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Low-lying placenta (placenta praevia) | Tommy's
Is a low-lying placenta common?
The position of your placenta will be checked at your mid-trimester ultrasound scan, at around 18-21 weeks of pregnancy. If your placenta is low-lying, you have another scan later in your pregnancy (usually about 32 weeks).
Because the lower part of the womb stretches more as the baby grows, the placenta usually moves into the upper part of the womb by this point.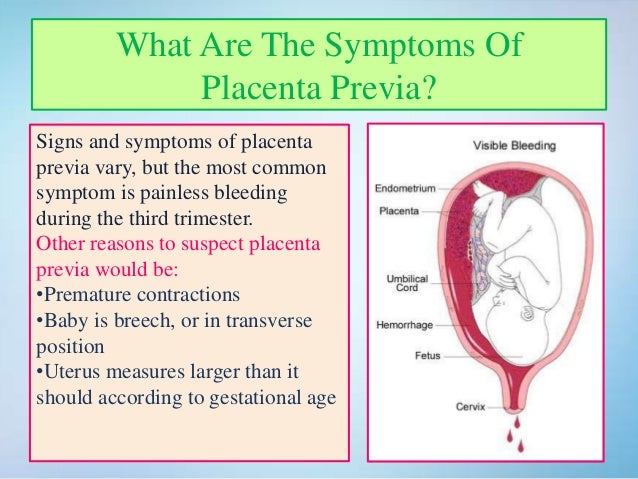 90% of women who have a low-lying placenta at 20 weeks will not go on to have a low-lying placenta later in the pregnancy.
90% of women who have a low-lying placenta at 20 weeks will not go on to have a low-lying placenta later in the pregnancy.
If you have had a baby by caesarean section before, the placenta is less likely to move upwards.
Only 1 in every 200 women have placenta praevia at the end of their pregnancy.
Am I likely to have placenta praevia?
Placenta praevia is more likely if you:
- smoke cigarettes
- have had fertility treatment to get pregnant, such as in vitro fertilisation (IVF)
- have had 1 or more caesarean sections
- are aged 40 or older
- are having more than 1 baby
- have had surgery on the womb
- are a cocaine user
- are expecting a boy
- have endometriosis.
Is there anything I can do to help the placenta move up?
Unfortunately not. The best thing you can do is concentrate on staying as healthy as you can. You may need extra scans, so make sure you go to all your antenatal appointments and follow your healthcare professional’s advice.
How can placenta praevia affect me and my baby?
There is a risk that you may have vaginal bleeding, particularly towards the end of your pregnancy. Bleeding from placenta praevia may be very heavy and can sometimes put mum and baby at risk.
How is a low-lying placenta diagnosed?
Your midwife or doctor will look at your placenta’s position at your 18 to 21 week ultrasound scan.
If your placenta is low, you'll be offered an extra ultrasound scan later in your pregnancy (usually at about 32 weeks) to check its position again.
In 90% of cases, the placenta is no longer low-lying by this point.
Your midwife or doctor may think you have placenta praevia if:
- you have bleeding during the second or third trimester – this is usually painless and may happen after sex
- if the baby is lying in an unusual position, for example bottom first (breech) or lying across the womb (transverse)
If you have any bleeding during pregnancy, with or without pain, you should always get checked out straight away.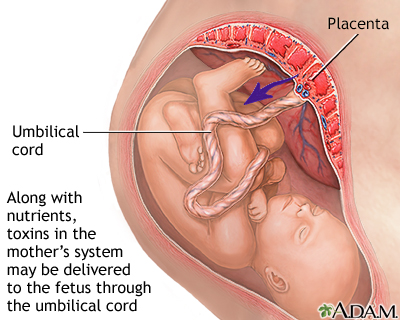 If you’re in your first trimester, contact your doctor, midwife or Early Pregnancy Unit. If you are more than 12 weeks pregnant, go to your local A&E or contact your hospital maternity unit immediately.
If you’re in your first trimester, contact your doctor, midwife or Early Pregnancy Unit. If you are more than 12 weeks pregnant, go to your local A&E or contact your hospital maternity unit immediately.
You may be advised to avoid having sex (including the use of penetrative sex toys) for the rest of your pregnancy.
What treatment will I have?
Extra scans
If your placenta is low-lying at your 20-week scan, you’ll be offered another ultrasound scan at around 32 weeks. This may include a transvaginal ultrasound scan, which is when a probe is gently placed inside the vagina to check exactly where your placenta is lying. Don’t worry, this is safe for you and your baby.
The length of your cervix may also be measured at your 32-week scan to predict whether you may go into labour early and whether you are at increased risk of bleeding.
If the placenta hasn’t moved up, you should be offered another ultrasound scan at 36 weeks. The results of this scan will help you and your doctor plan the safest way for you to give birth.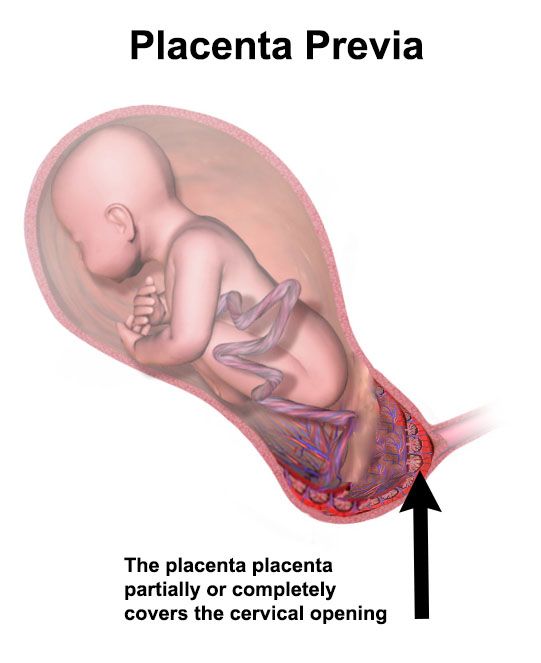
Medication
If you have placental praevia, there is a risk you may give birth prematurely. So you may be offered a course of steroid injections between 34 and 36 weeks of pregnancy to help your baby’s lungs to become more mature.
If you do go into labour early, you may be offered medication to try to stop your contractions. This will give you time to have a course of steroid injections. If you have severe bleeding or progressing labour your baby may need to be delivered.
If you have vaginal bleeding, you may need to be admitted to hospital. This is because there is a small risk that you could bleed suddenly and heavily. If this happens, you may need an emergency caesarean section.
What do I need to do if I have a low-lying placenta?
If you know you have a low-lying placenta, you should contact the hospital immediately if you have:
- vaginal bleeding, including spotting
- contractions
- pain, including any vague, period-like aches.
If you have any bleeding, your doctor may need to do an internal examination to check where it’s coming from. This is safe and they will ask for your permission before they start.
Anaemia
Anaemia is a blood condition that develops when you don’t have enough red blood cells. Red blood cells contain haemoglobin, a protein that carries oxygen around your body and to your baby.
If you have a low-lying placenta, it’s important to try to avoid developing anaemia, which can be common in pregnancy. Eating a healthy, balanced diet will help you either prevent or manage anaemia. Iron supplements may also help, if your healthcare team recommends them.
How will my baby be born?
Your healthcare team will talk to you about what your options are for giving birth.
You may be advised to give birth early if you have any heavy bleeding before your due date.
If the edge of your placenta is very close (less than 20mm) to your cervix (entrance to the womb), the Royal College of Obstetricians and Gynaecologists state that the safest way to give birth is by caesarean section. This will usually be between 36 and 37 weeks. Your doctor will discuss your options with you, but how you give birth is ultimately your decision. But if you have had vaginal bleeding during your pregnancy, you may be advised to have your caesarean earlier than this.
This will usually be between 36 and 37 weeks. Your doctor will discuss your options with you, but how you give birth is ultimately your decision. But if you have had vaginal bleeding during your pregnancy, you may be advised to have your caesarean earlier than this.
If the placenta is further than 20mm from your cervix, you may be able to have a vaginal birth if you want one.
If you are having a caesarean section, a senior obstetrician (a doctor who specialises in pregnancy) will be there. This is because you may have heavy bleeding during the surgery. If this happens, you may need a blood transfusion. This is more likely if you have placenta praevia.
Talk to your doctor before your surgery if, for any reason, you do not want a blood transfusion.
Unfortunately, complications are more common in caesarean sections if you have a low-lying placenta. Your doctor should talk to you about the risks of major bleeding and hysterectomy (removal of the womb) before your caesarean. For most women, the risk of hysterectomy is low and will only occur as a last resort if other measures to control bleeding are not effective.
For most women, the risk of hysterectomy is low and will only occur as a last resort if other measures to control bleeding are not effective.
If you have placenta praevia:
- you are at higher risk of having your baby early (less than 37 weeks).
- your baby will need to be born by caesarean section because the placenta is blocking the birth canal.
Your mental health
Being diagnosed with complications in pregnancy can be hard. And being asked to look out for certain symptoms, such as bleeding, and needing extra appointments and check-ups can cause anxiety and stress. It may also be a lonely experience when those around you don’t understand what it’s like.
Remember that you can tell your midwife or doctor how you feel. They will do their best to reassure you and answer any questions you may have.
You can also call our pregnancy line on 0800 014 7800 (Monday to Friday, 9am to 5pm), or email us at [email protected]
If you are struggling to cope, there is professional support available.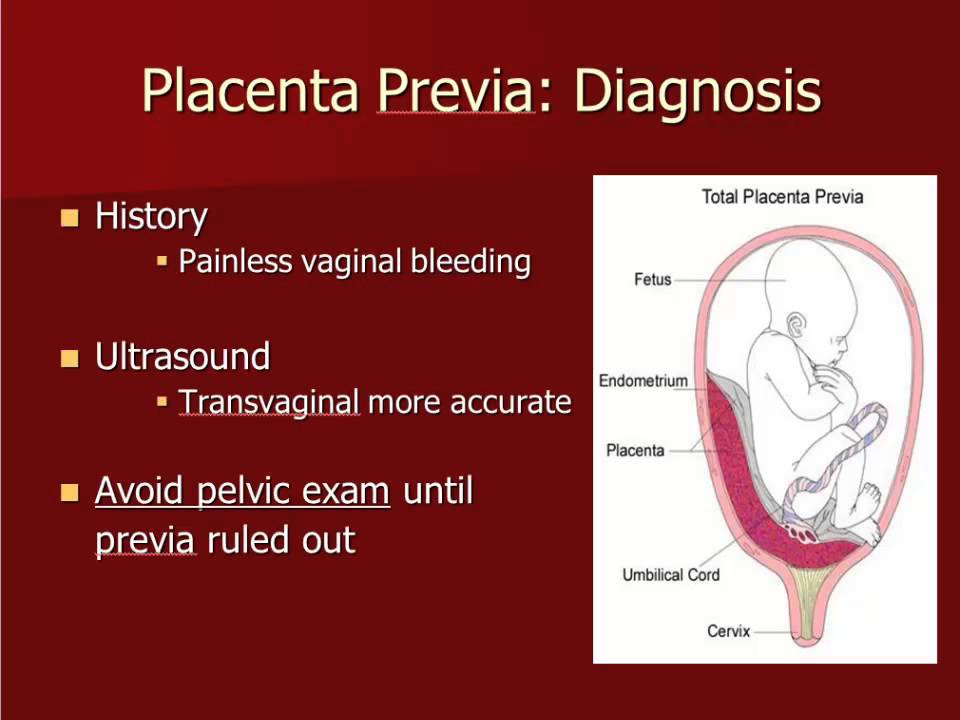 Don’t suffer in silence. Tell your midwife or GP how you feel. They will help you access the support you need.
Don’t suffer in silence. Tell your midwife or GP how you feel. They will help you access the support you need.
Find out more about looking after our mental health in pregnancy.
What is the placenta
It connects two organisms - the mother and the fetus, providing it with the necessary nutrients.
Where is the placenta located and what does it look like?
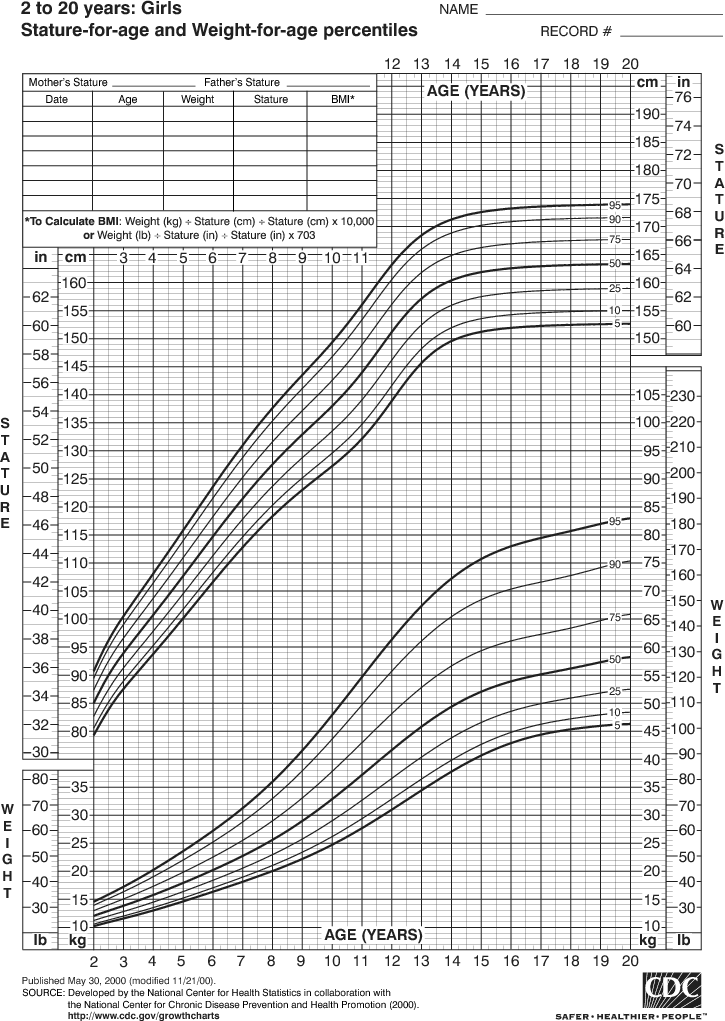
In a normal pregnancy, the placenta is located in the body of the uterus along its posterior (more often) or anterior wall. It is fully formed by the 15-16th week of pregnancy, after the 20th week, active exchange begins through the placental vessels. From the 22nd to the 36th week of pregnancy, an increase in the mass of the placenta occurs, and by the 36th week it reaches full functional maturity.
Figure 1. Schematic representation of the location of the placenta in the uterus of a pregnant woman. Photo: Wikipedia (Public Domain) In appearance, the placenta looks like a round flat disk.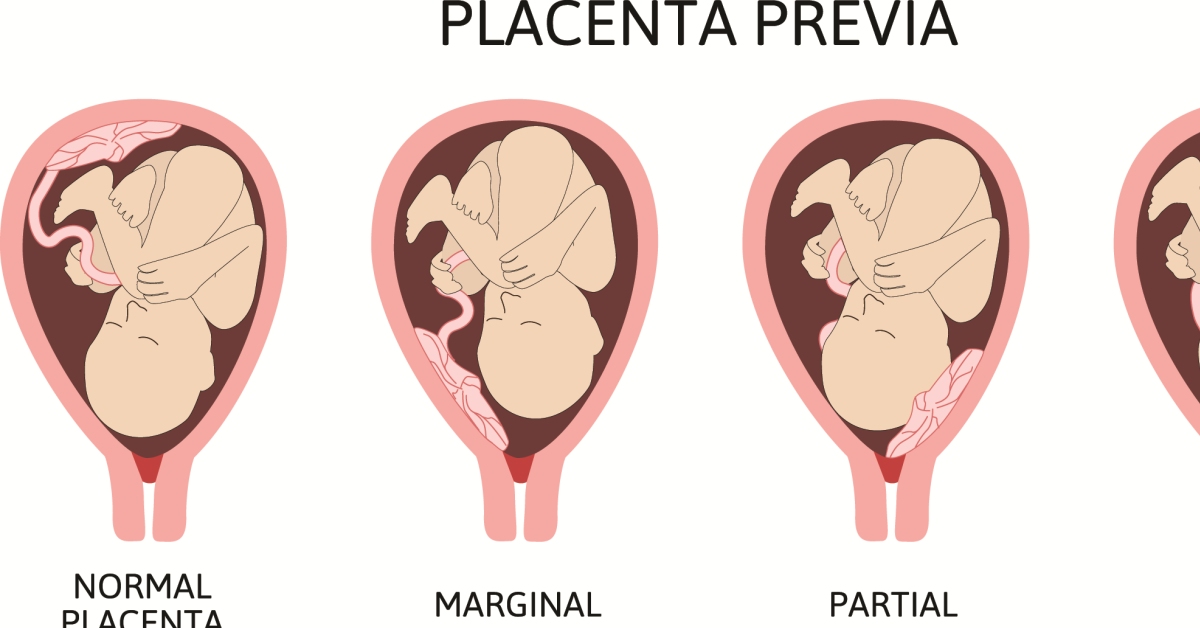 By the time of delivery, the weight of the placenta is 500-600 g, the diameter is 15-18 cm and the thickness is 2-3 cm.
By the time of delivery, the weight of the placenta is 500-600 g, the diameter is 15-18 cm and the thickness is 2-3 cm.
Functions of the placenta
Photo: zffoto / freepik.com- First, gas exchange occurs through the placenta: oxygen penetrates from the mother's blood to the fetus, and carbon dioxide is transported in the opposite direction.
- Secondly, the fetus receives through the placenta the nutrients necessary for its growth and development. It must be remembered that many substances (alcohol, nicotine, drugs, many drugs, viruses) easily penetrate through it and can have a damaging effect on the fetus. In addition, with its help, the fetus gets rid of the products of its vital activity.
- Thirdly, the placenta provides immunological protection for the fetus, delaying the cells of the mother's immune system, which, having penetrated to the fetus and recognized a foreign object in it, could trigger its rejection reactions. At the same time, the placenta passes maternal antibodies that protect the fetus from infections.

- Fourthly, the placenta plays the role of an endocrine gland and synthesizes hormones (human chorionic gonadotropin (hCG), placental lactogen, prolactin, etc.) necessary to maintain pregnancy, growth and development of the fetus.
Normally, the placenta together with the membranes (afterbirth) is born 10-15 minutes after the birth of the fetus. She is carefully examined and sent for a morphological study. First, it is very important to make sure that the whole placenta was born (that is, there are no damages on its surface and there is no reason to believe that pieces of the placenta remained in the uterine cavity). Secondly, according to the state of the placenta, one can judge the course of pregnancy (whether there was an abruption, infectious processes, etc.).
What do doctors want to know about the placenta?
During pregnancy, it is important to look for signs of placental dysfunction - placental insufficiency. To do this, during an ultrasound study, the structure of the placenta, its location in the uterine cavity, thickness, and the correspondence of the size of the fetus to the gestational age are studied. In addition, the blood flow in the placental vessels is studied.
In addition, the blood flow in the placental vessels is studied.
Degree of maturity
Photo: wavebreakmedia-micro / freepik.comThis parameter, as doctors say, is "ultrasonic", that is, it depends on the density of the structures of the placenta determined by ultrasound.
There are four degrees of placental maturity:
- Normally, zero degree of placental maturity should be determined before 30 weeks of pregnancy.
- The first degree is considered valid from 27 to 34 weeks.
- Second - from 34 to 39.
- Starting from 37 weeks, the third degree of placental maturity can be determined.
At the end of pregnancy, the so-called physiological aging of the placenta occurs, accompanied by a decrease in the area of its exchange surface, the appearance of areas of salt deposition.
Place of attachment
Photo: kuprevich / freepik.com Determined by ultrasound. As mentioned above, during a normal pregnancy, the placenta is located in the body of the uterus.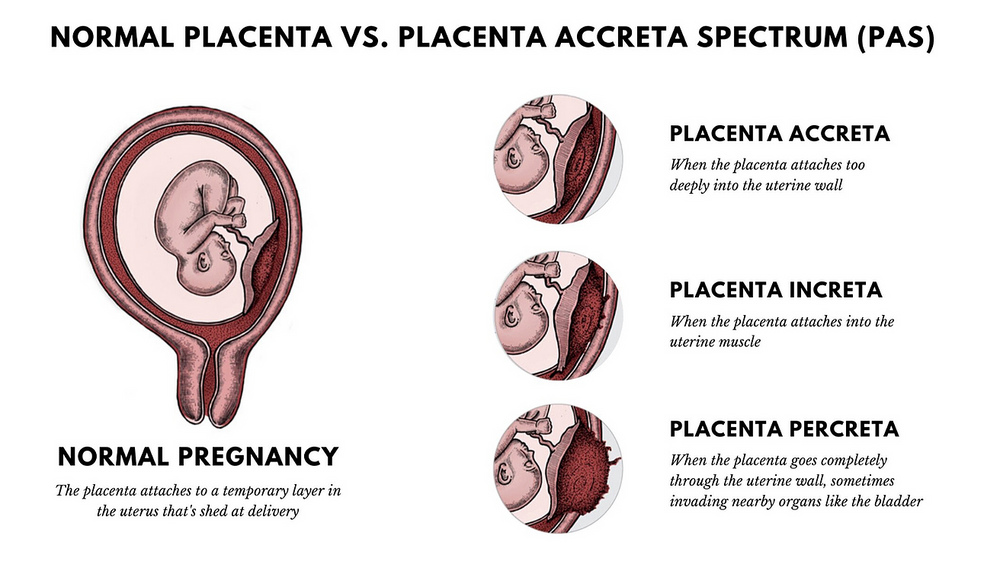 Sometimes, during an ultrasound examination in the first half of pregnancy, it is found that the placenta is located in the lower parts of the uterus, reaching or even overlapping the area of the internal os of the cervix. In the future, as pregnancy progresses, the placenta most often shifts from the lower sections of the uterus to the top. However, if after 32 weeks the placenta still overlaps the area of the internal os, this condition is called *placenta previa**, which is a serious complication of pregnancy.
Sometimes, during an ultrasound examination in the first half of pregnancy, it is found that the placenta is located in the lower parts of the uterus, reaching or even overlapping the area of the internal os of the cervix. In the future, as pregnancy progresses, the placenta most often shifts from the lower sections of the uterus to the top. However, if after 32 weeks the placenta still overlaps the area of the internal os, this condition is called *placenta previa**, which is a serious complication of pregnancy.
Placenta previa can lead to bleeding, which can occur during the second or third trimester of pregnancy or during childbirth.
Ultrasound with placenta previa. Turk J Obstet Gynecol / ResearchGate (Creative Commons Attribution 2.5 Generic license)Thickness
Also determined by ultrasound - placentometry: after establishing the site of attachment of the placenta, the area where it has the largest size is found, which is determined. The thickness of the placenta, as already mentioned, continuously increases until 36-37 weeks of pregnancy (by this time it ranges from 20 to 40 mm). Then its growth stops, and in the future the thickness of the placenta either decreases or remains at the same level.
Then its growth stops, and in the future the thickness of the placenta either decreases or remains at the same level.
Deviation from the norm of at least one of these indicators may indicate trouble during pregnancy.
References
- Tiwari D., Das CR., Sultana R., Kashyap N., Islam M., Bose PD., Saikia AK., Bose S. Increased homocysteine mediated oxidative stress as key determinant of hepatitis E virus ( HEV) infected pregnancy complication and outcome: A study from Northeast India. // Infect Genet Evol - 2021 - Vol - NNULL - p.104882; PMID:33905889
- Salmanian B., Belfort M.A., Shamshirsaz A.A. The risk of placenta accreta spectrum in women with in vitro fertilization in different populations. // Am J Obstet Gynecol - 2021 - Vol - NNULL - p.; PMID:33905744
- Olmos-Ortiz A., Olivares-Huerta A., García-Quiroz J., Zariñán T., Chavira R., Zaga-Clavellina V., Avila E., Halhali A., Durand M., Larrea F., Díaz L. Placentas associated with female neonates from pregnancies complicated by urinary-tract infections have higher cAMP content and cytokines expression than males.
 // Am J Reprod Immunol - 2021 - Vol - NNULL - p.e13434; PMID:33905581
// Am J Reprod Immunol - 2021 - Vol - NNULL - p.e13434; PMID:33905581 - Tandl V., Hoch D., Bandres-Meriz J., Nikodijevic S., Desoye G., Majali-Martinez A. Different regulation of IRE1α and eIF2α pathways by oxygen and insulin in ACH-3P trophoblast model. // Reproduction - 2021 - Vol - NNULL - p.; PMID:33904834
- Ji S., Gumina D., McPeak K., Moldovan R., Post MD., Su EJ. Human placental villous stromal extracellular matrix regulates fetoplacental angiogenesis in severe fetal growth restriction. // Clin Sci (Lond) - 2021 - Vol - NNULL - p.; PMID:33904582
- Shmeleva EV., Colucci F. Maternal natural killer cells at the intersection between reproduction and mucosal immunity. // Mucosal Immunol - 2021 - Vol - NNULL - p.; PMID:33903735
- Moreno-Sepulveda J., Espinós JJ., Checa MA. Lower risk of adverse perinatal outcomes in natural versus artificial frozen-thawed embryo transfer cycles: a systematic review and meta-analysis. // Reprod Biomed Online - 2021 - Vol - NNULL - p.
 ; PMID:33903031
; PMID:33903031 - Owen M.D., Cassidy A.L., Weeks AD. Why are women still dying from obstetric hemorrhage? A narrative review of perspectives from high and low resource settings. // Int J Obstet Anesth - 2021 - Vol - NNULL - p.102982; PMID:33903002
- Liu CN., Yu FB., Xu YZ., Li JS., Guan ZH., Sun MN., Liu CA., He F., Chen DJ. Prevalence and risk factors of severe postpartum hemorrhage: a retrospective cohort study. // BMC Pregnancy Childbirth - 2021 - Vol21 - N1 - p.332; PMID:33902475
- Munoz JL., Kimura AM., Xenakis E., Jenkins DH., Braverman MA., Ramsey PS., Ireland KE. Whole blood transfusion reduces overall component transfusion in cases of placenta accreta spectrum: a pilot program. // J Matern Fetal Neonatal Med - 2021 - Vol - NNULL - p.1-6; PMID:33
4
Low placenta
Home / Gynecologist / Low placenta
Placenta is a temporary organ that is formed in the body of a pregnant woman in order to maintain a connection between her body and the fetus.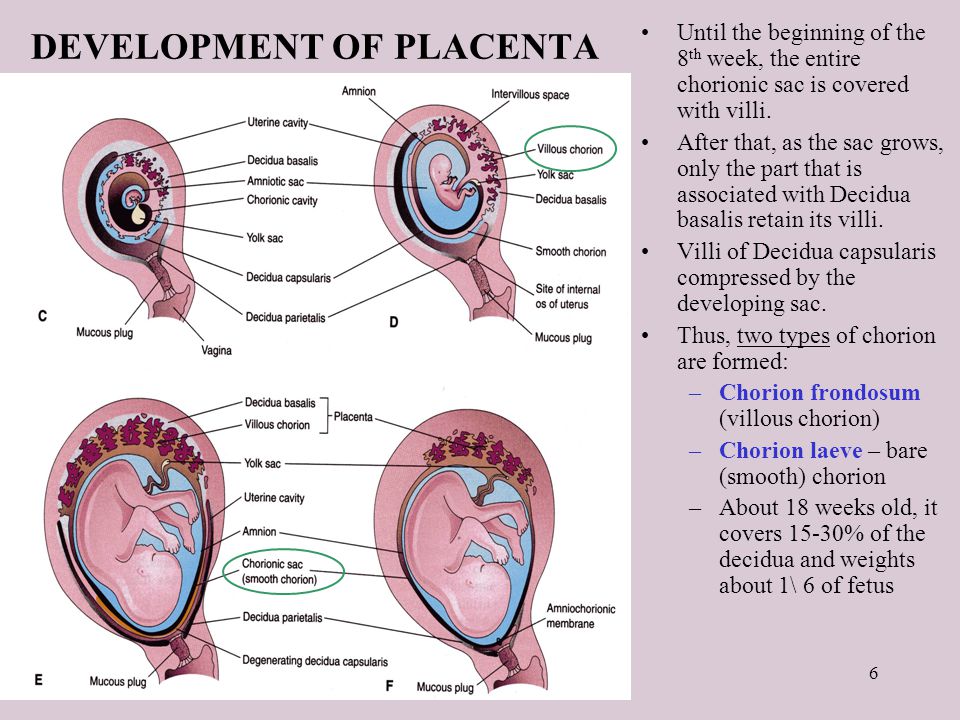 She filters the blood , which the unborn baby feeds on, cleansing it of toxins and other harmful substances.
She filters the blood , which the unborn baby feeds on, cleansing it of toxins and other harmful substances.
This pathology can be very dangerous in some cases, while in others it goes away without any treatment and does not bring problems.
Types of location of the placenta
Usually the placenta is attached to the posterior wall of the uterus closer to its bottom . It is worth noting that the uterus is an inverted vessel, and its bottom is located on top. This is the best option for the location of the placenta. However, this does not always work out. In some cases, the placenta is attached to the anterior wall. Which is also not a pathology.
The low position of the placenta during pregnancy is much more dangerous. If the placenta is located low, it is subjected to stronger pressure from the fetus, and even with any external influence, the risk is damage to the placenta or its detachment increases. In addition, in the later stages, an actively moving baby can also damage the placenta, or squeeze the umbilical cord.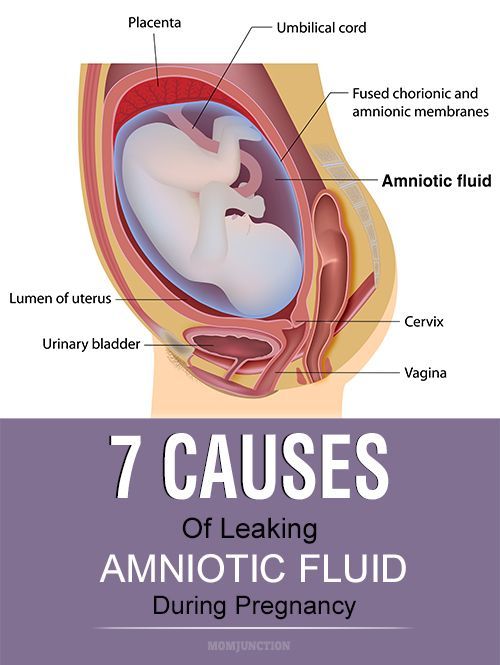
A placenta is said to be low when there is less than 6 cm between its lower edge and the os of the uterus. The anterior wall has a greater tendency to stretch, and migration is also characteristic of it, however, the direction of migration is opposite: usually the placenta moves in the opposite direction, down to the cervix.
An even more complex and dangerous pathology of the location of the placenta is its partial or complete presentation . Previa is a condition when the placenta partially or completely obscures the cervix of the uterus.
Causes of low placenta
Many causes of low placenta are due to internal factors - diseases during pregnancy and the condition of the female genital organs . They can be:
- damage to the mucous membrane of the uterus;
- inflammatory processes;
- infections;
- previous abortions;
- miscarriages in the past;
- cesarean section;
- various gynecological operations;
- pathology of the structure, development, functioning of the uterus;
- multiple pregnancy;
- unhealthy lifestyle: active smoking, excessive alcohol consumption;
- previous diseases of the uterus: endometritis, fibroids;
- parity - many births in the past;
- the woman's age is over 35 years.
Curettage of the uterus in the past is the main cause of this pathology. Damage to the mucosa prevents the fetal egg from gaining a foothold in the upper segment of this organ, and it remains below, at the neck.
Symptoms of low placenta
The danger of this pathology is that it practically does not manifest itself. Usually, signs that not everything is in order with the placenta are the result of already running and irreversible processes - for example, its detachment. It can be:
- drawing pains, feeling of heaviness in the abdomen;
- spotting with a low location of the placenta is an alarm signal that it is necessary to call an ambulance;
- freezing of the fetus in the womb for a long time, or, conversely, its too violent activity - this is caused by hypoxia;
- on ultrasound with such a pathology in 50% of cases is the wrong presentation of the fetus;
- in 30% of cases, women suffer from severe toxicosis.
A pregnant woman herself cannot suspect that she has a low placenta. This can only be seen on planned ultrasounds, which must be passed by everyone. After an ultrasound examination, they can not only clarify or refute the diagnosis, but also determine the type of pathology.
Treatment and prevention of low placentation
Management of pregnancy with low placentation is always very careful. A woman will have to undergo ultrasound many times, limit physical activity and stop sexual activity. For a long time, increased uterine tone can provoke detachment of an improperly located placenta, from there bleeding, and possible death of the fetus as a result of acute hypoxia, if placental abruption is large. Bleeding can even provoke a gynecological examination of the cervix, therefore, for no particular reason, doctors try not to conduct examinations on the chair.
Listen to the doctors and hope for the best. Many women give birth on their own or by caesarean section of healthy babies with low placenta previa.