Average temperature for infants
Fever (0-12 Months)
Is this your child's symptom?
- An abnormal high body temperature
- Fever is the only symptom. Your child has a true fever if:
- Rectal (bottom), Ear or Forehead temperature: 100.4° F (38.0° C) or higher
- Under the arm (armpit) temperature: 99° F (37.2° C) or higher
- Caution: Ear temperatures are not accurate before 6 months of age
- Caution: Forehead temperatures must be digital. Forehead strips are not accurate.
Causes of Fever
- Overview. Almost all fevers are caused by a new infection. Viruses cause 10 times more infections than bacteria. The number of germs that cause an infection are in the hundreds. Only a few common ones will be listed.
- Viral Infections. Colds, flu and other viral infections are the most common cause. Fever may be the only symptom for the first 24 hours. The start of viral symptoms (runny nose, cough, loose stools) is often delayed.
Roseola is the most extreme example. Fever may be the only symptom for 3 to 5 days. Then a rash appears.
- Bacterial Infections. A bladder infection is the most common cause of silent fever in girls.
- Vaccine Fever. Fever with most vaccines begins within 12 hours. It lasts 2 to 3 days. This is normal and harmless. It means the vaccine is working.
- Newborn Fever (Serious). Fever that occurs during the first 3 months of life can be serious. All of these babies need to be seen as soon as possible. The fever may be due to sepsis (a bloodstream infection). Bacterial infections in this age group can get worse quickly. They need rapid treatment.
- Meningitis (Very Serious). A bacterial infection of the membrane that covers the spinal cord and brain. The main symptoms are a stiff neck, headache and confusion. Younger children are lethargic or so irritable that they can't be consoled. If not treated early, can suffer brain damage.
- Overheated. The fever is usually low grade. Can occur during heat waves or from being overdressed. The temp becomes normal in a few hours after moving to a cooler place. Fever goes away quickly with rest and drinking extra fluids.
- Not Due to Teething. Research shows that "getting teeth" does not cause fevers.
Fever and Crying
- Fever on its own shouldn't cause much crying.
- Frequent crying in a child with fever is caused by pain until proven otherwise.
- Hidden causes can be ear infections, kidney infections, sore throats and meningitis.
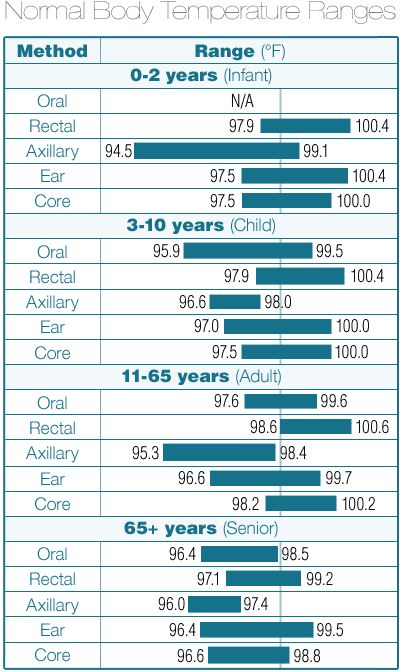
Normal Temperature Range
- Rectal. A reading of 98.6° F (37° C) is just the average rectal temp. A normal low can be 96.8° F (36° C) in the morning. It can change to a high of 100.3° F (37.9° C) late in the day. This is a normal range.
When to Call for Fever (0-12 Months)
Call 911 Now
- Not moving
- Can't wake up
- Severe trouble breathing (struggling for each breath; can barely speak or cry)
- Purple or blood-colored spots or dots on skin
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Trouble breathing, but not severe
- Great trouble swallowing fluids or spit
- Fever in baby less than 12 weeks old.
 Caution: Do NOT give your baby any fever medicine before being seen.
Caution: Do NOT give your baby any fever medicine before being seen. - Fever over 104° F (40° C)
- Shaking chills (shivering) lasting more than 30 minutes
- Nonstop crying or cries when touched or moved
- Won't move an arm or leg normally
- Dehydration suspected. No urine in over 8 hours, dark urine, very dry mouth and no tears.
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Age 3-6 months old with fever
- Age 6-12 months old with fever that lasts more than 24 hours. There are no other symptoms (such as cough or diarrhea).
- Fever lasts more than 3 days
- Fever returns after gone for more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Fever with no other symptoms and your child acts mildly ill
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Fever
- What You Should Know About Fever:
- Having a fever means your child has a new infection.
- It's most likely caused by a virus.
- You may not know the cause of the fever until other symptoms develop. This may take 24 hours.
- For infants more than 3 months old, most fevers are good for sick children. They help the body fight infection.

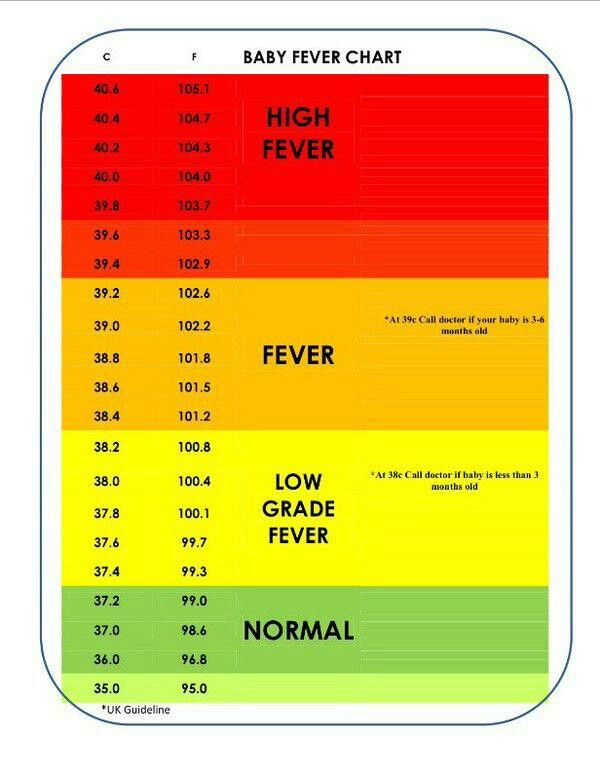
- Use the ranges below to help put your child's level of fever into perspective:
- 100° - 102° F (37.8° - 39° C) Low grade fever: helpful, good range. Don't treat.
- 102° - 104° F (39 - 40° C) Average fever: helpful. Treat if causes discomfort.
- Over 104° F (40° C) High fever: causes discomfort, but harmless. Always treat.
- Over 106° F (41.1° C) Very high fever: important to bring it down. Rare to go this high.
- Over 108° F (42.3° C) Dangerous fever: fever itself can be harmful.
- Treatment for All Fevers - Extra Fluids:
- Fluids alone can lower the fever. Reason: being well hydrated helps the body give off heat through the skin.
- For shivering (or the chills), give your child a blanket. Make them comfortable.
- Offer your child extra water or other fluids by mouth. Cold fluids are better. Until 6 months old, only give extra formula or breastmilk.
- For all children, dress in 1 layer of light weight clothing, unless shivering.
 Reason: also helps heat loss from the skin.
Reason: also helps heat loss from the skin. - For shivering (or the chills), give your child a blanket. Make them comfortable.
- Caution: if a baby under 1 year has a fever, never overdress or bundle up. Reason: Babies can get over-heated more easily than older children.
- Fever Medicine:
- Caution: Do not give a baby under 3 months any fever medicine. Most of these babies will need to be seen.
- For fevers 100°-102° F (37.8° - 39°C), fever meds are not needed. Reason: fevers in this range help the body fight the infection. Fevers turn on the body's imune system. Fevers don't cause any discomfort. Fever meds are mainly needed for fevers higher than 102° F (39° C).
- Give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil) if over 6 months old.
- Goal of treatment: keep the fever at a helpful level. Most often, the fever meds lower the fever by 2° to 3° F (1 - 1.
 5° C). They do not bring it down to normal. It takes 1 or 2 hours to see the effect.
5° C). They do not bring it down to normal. It takes 1 or 2 hours to see the effect. - Do not use aspirin. Reason: Risk of Reye syndrome, a rare but serious brain disease.
- Do not use both acetaminophen and ibuprofen together. Reason: Not needed and a risk of giving too much.
- Pain: fever does not cause pain. If your child also has pain, it's from the infection. It may be a sore throat or muscle pain. Treat the pain, if it's more than mild.
- Return to Child Care:
- Your child can return to child care after the fever is gone. Your child should feel well enough to join in normal activities.
- What to Expect:
- Most fevers with viral illnesses range between 101° and 104° F (38.4° and 40° C).
- They may last for 2 or 3 days.
- They are not harmful.
- Call Your Doctor If:
- Your child looks or acts very sick
- Any serious symptoms occur such as trouble breathing
- Fever goes above 104° F (40° C)
- Any fever occurs if less than 12 weeks old
- Fever without other symptoms lasts more than 24 hours
- Fever lasts more than 3 days (72 hours)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 10/31/2022
Last Revised: 09/18/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
Fever in Infants & Children - Infant Fever Reducer
What is fever in infants and children?
A fever is a sign that your body is sick or has an infection. A fever helps kill infections, bacteria and viruses that are causing the fever. Your child has a fever if his or her body temperature his higher than normal. A normal temperature is 98.6°F when checking by mouth. Some doctors ask you to check your baby or young child’s temperature rectally (in their bottom). Normal for that method is 99.6°F.
Symptoms of fever in infants and children
- Constant vomiting or diarrhea
- Dry mouth
- Earache or pulling at ears
- Fever comes and goes over several days
- High-pitched crying
- Fussiness
- No appetite
- Pale appearance
- Seizures
- Severe headache
- Skin rash
- Sore or swollen joints
- Sore throat
- Stiff neck
- Stomach pain
- Swelling of the soft spot on an infant’s head
- Unresponsiveness or limpness
- Wheezing or problems breathing
- Whimpering
What causes fever in infants and children?
Most fevers are caused by infections (bacteria or virus). Other reasons for a fever include:
Other reasons for a fever include:
- Certain medicines. This would include antibiotics, anti-seizure and blood pressure medicines.
- A heat-related illness.
- Cancers
- Autoimmune disorders (when your body mistakenly attacks healthy tissue).
- Some childhood vaccinations
How is fever in infants and children diagnosed?
Many doctors diagnose a fever as an oral temperature above 99.5°F. They diagnose fever as a rectal temperature above 100.4°F. But fever standards also depend on age, so what may be a fever in one person may not rate as a fever in someone else.
To take your child’s temperature rectally, use a digital thermometer. Place your child on his or her stomach across your lap. Apply petroleum jelly (brand name: Vaseline) to the tip of the thermometer. Insert it half an inch into your child’s bottom. Stop if you feel any resistance. Hold the thermometer still and do not let go. When the thermometer beeps, remove it and check the digital reading. Taking temperatures rectally is the preferred method for children.
Taking temperatures rectally is the preferred method for children.
To take your child’s temperature orally, use a digital thermometer. Place the end of the thermometer under his or her tongue. Go towards the back of the mouth. Have your child close his or her lips around the thermometer. Tell your child not to bite down or talk. When the thermometer beeps, remove it and check the digital reading.
Never use a mercury thermometer. Mercury is poison.
Other temperature-taking tips include:
- Label your rectal thermometer so that it isn’t accidentally used in your child’s mouth.
- Start by cleaning the thermometer in warm, soapy water. Rinse well with cool water.
- For oral temperatures, wait 20 minutes after your child eats or drinks hot or cold foods and drinks before taking his or her temperature.
- Don’t bundle your baby or child up too tightly before taking his or her temperature.
- Don’t take your child’s temperature right after he or she has had a bath.
- Never leave your child alone when using a thermometer.
- When you are finished, clean the thermometer again with rubbing alcohol or with cool, soapy water.
Can fever in infants and children be prevented or avoided?
Fevers caused by illness or infection can be avoided by avoiding the things that cause illness and infection. Fevers caused by vaccinations can be avoided by giving your child acetaminophen. This is an over-the-counter medicine (brand name: Tylenol). This should be given just before or right after the vaccination.
Fever in infants and children treatment
Acetaminophen can be given to reduce a fever. Ibuprofen (brand names Children’s Advil, Children’s Motrin) is another medicine that can be used to lower a fever in children older than 6 months of age. Ask your doctor for the correct dosage. This will vary by your child’s age and weight. Don’t give your child medicine if he or she is between 3 months and 3 years of age and has a temperature of 102°F or lower. If your child is achy and fussy, and his or her temperature is above 102°F (38.8°C), you may want to give him or her acetaminophen.
If your child is achy and fussy, and his or her temperature is above 102°F (38.8°C), you may want to give him or her acetaminophen.
Tips for giving medicine:
- Don’t give more than 5 doses in 1 day.
- Don’t give a baby younger than 2 months of age any medicine unless your doctor tells you to.
- Read package directions carefully.
- For liquid medicines, use a special measuring device to get the right dose. You can get one at your drug store. An ordinary kitchen teaspoon may not hold the right amount of medicine.
If your baby is younger than 3 months old and has a rectal temperature of 100.4°F or higher, call the doctor or go to the emergency room. A fever can be a sign of a serious infection in young babies.
Never give your child aspirin for any reason. Aspirin can cause Reye’s syndrome. Reye’s syndrome is a serious childhood illness that can lead to death. Do not give aspirin to children younger than 18 years of age.
Giving your child acetaminophen and a warm bath may lower his or her fever. Give the acetaminophen before the bath. A bath without medicine will cause your child to shiver. This will raise his or her body temperature. Never use rubbing alcohol or cold water for baths.
Give the acetaminophen before the bath. A bath without medicine will cause your child to shiver. This will raise his or her body temperature. Never use rubbing alcohol or cold water for baths.
Living with fever in infants and children
It’s important to make your child comfortable when he or she has a fever. Things that can help include:
- Give your child fluids to prevent dehydration (not enough fluid in the body). It will help the body cool itself. Water, clear soups, popsicles and flavored gelatin are good choices.
- Don’t force your child to eat if he or she doesn’t feel like it.
- Make sure your child gets plenty of rest.
- Keep the room temperature at about 70°F to 74°F.
- Dress your child in light cotton pajamas. Overdressing can trap body heat and cause your child’s temperature to rise.
- If your child has chills, give him or her an extra blanket. Remove it when the chills stop.
Questions to ask your doctor
- Can I tell if my child has a fever by touching his forehead?
- How many days should a fever last before I should get concerned?
- Why does my child’s fever come and go?
- Can a high fever make my child confused?
Resources
U. S. National Library of Medicine, Fever
S. National Library of Medicine, Fever
Copyright © American Academy of Family Physicians
This information provides a general overview and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject.
Normal values of body temperature in children, measurement of the child's body temperature
It is believed that a healthy child should have a body temperature of 36.6 °C. And its increase over 37 degrees is regarded as a sign of illness. But it is not so.
Body temperature depends on age and measurement area. It can increase after physical exertion, emotional arousal and feeding.
Devices and time for measuring body temperature
To determine the temperature, the following types of thermometers are used:
-
digital;
-
mercury;
-
infrared.
The optimal time for thermometry is 7-9 am and 17-19 pm. As prescribed by the doctor, the determination of the temperature during the day in children can be performed 3-4 times.
As prescribed by the doctor, the determination of the temperature during the day in children can be performed 3-4 times.
What temperature is considered normal for a child?
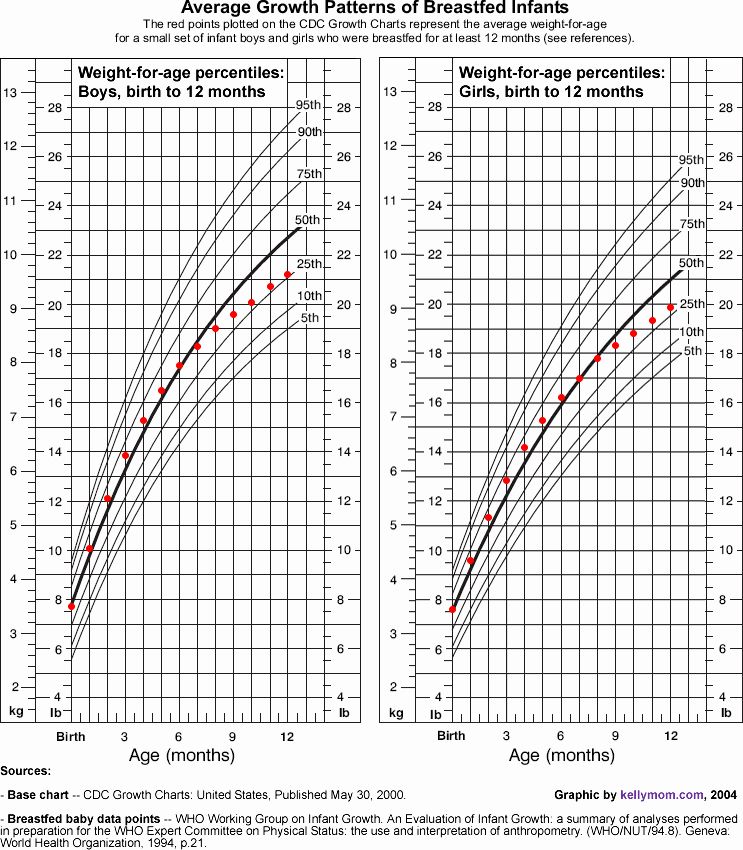
Immediately after the birth of a newborn, the temperature of his body decreases by 1-2 ° C, then within 24 hours it rises to 36-37 ° C. In the first 3 months of a baby's life, its indicators are unstable and depend on external factors: air temperature in the room, sleep, food intake. Normally, these fluctuations do not exceed 0.6 °C per day. For children of the first year of life, a temperature of 37.7 is the norm.
The average body temperature for a child is 37°C. Usually in the morning - 36.3 ° C, and in the evening it can rise to 37.6 ° C.
In what areas can the temperature of children be taken?
Underarm
The temperature measurement time under the arm is 5-10 minutes and depends on the type of device.
In the rectum
It is used in children under 5 years of age and in debilitated patients. For this method, it is desirable to use medical electronic thermometers with a soft tip. It will take 1-1.5 minutes to determine the rectal temperature.
For this method, it is desirable to use medical electronic thermometers with a soft tip. It will take 1-1.5 minutes to determine the rectal temperature.
Oral
The procedure is performed both under the tongue and behind the cheek. Contraindications to the use of this method are: children under 4-5 years of age, increased excitability and impaired nasal breathing. The duration of temperature measurement by the oral method is from 10 seconds to 3 minutes.
In the ear
The temperature in the ear is measured with an infrared sensor. The tip of the thermometer is inserted into the ear canal and the result appears on the display.
On forehead
Forehead temperature can be measured with a contact and non-contact thermometer. It will take 3 to 5 seconds to get the result. If the baby is sleeping or excited, then it is more convenient to use a non-contact method for measuring temperature.
Crotch
Mainly used in infants. The measurement time in the inguinal fold is 5 minutes. The method is inconvenient because the baby is not easy to keep in one position during this time.
The measurement time in the inguinal fold is 5 minutes. The method is inconvenient because the baby is not easy to keep in one position during this time.
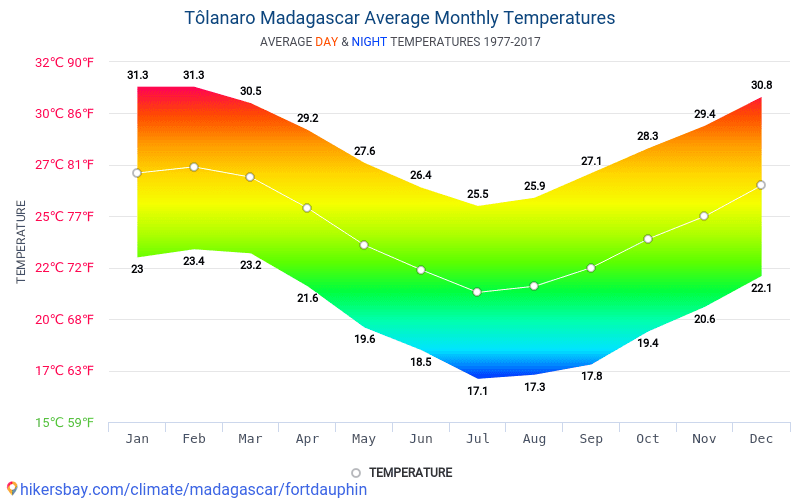
Ranges of normal temperature in children depending on age and area of measurement are presented in the following table:
| 0-2 years | 3-10 years | 11-18 years old | |
|---|---|---|---|
| In the armpit | 34.7 - 37.2 | 35.8 - 36.6 | 35.1 - 36.8 |
| On the forehead | 36.7 - 37.5 | 36.7 - 37.5 | 36.5 - 37.4 |
| in the ear | 36.3 - 37.7 | 36.3 - 37.7 | 36.7 - 37.8 |
Fever in children - NCCH
36.6˚ is the average normal body temperature for an adult. In children, the average body temperature is 0. 3-0.4˚ C higher than in adults. In addition, the temperature in children is characterized by significant lability and its average fluctuations in newborns can be about 0.4 ° C, and in older children up to 1 ° C. Factors such as food intake, hunger, movement, restlessness, alternation of sleep and wakefulness. It must be remembered that there are daily fluctuations in temperature, in the evening it is usually slightly higher. In young children with insufficient maturity of thermoregulation processes, environmental factors have a significant impact, it is important to remember that children are very easy to both overcool and overheat, so the air temperature in the room, the quantity and quality of clothes on the child, etc. are important. If the child seemed hot to you, and you decided to measure the temperature, you must wait 15-20 minutes after sleep or physical activity, uncover the child. The temperature should not be measured in the hands of the mother, but in a calmly sitting or lying child.
3-0.4˚ C higher than in adults. In addition, the temperature in children is characterized by significant lability and its average fluctuations in newborns can be about 0.4 ° C, and in older children up to 1 ° C. Factors such as food intake, hunger, movement, restlessness, alternation of sleep and wakefulness. It must be remembered that there are daily fluctuations in temperature, in the evening it is usually slightly higher. In young children with insufficient maturity of thermoregulation processes, environmental factors have a significant impact, it is important to remember that children are very easy to both overcool and overheat, so the air temperature in the room, the quantity and quality of clothes on the child, etc. are important. If the child seemed hot to you, and you decided to measure the temperature, you must wait 15-20 minutes after sleep or physical activity, uncover the child. The temperature should not be measured in the hands of the mother, but in a calmly sitting or lying child.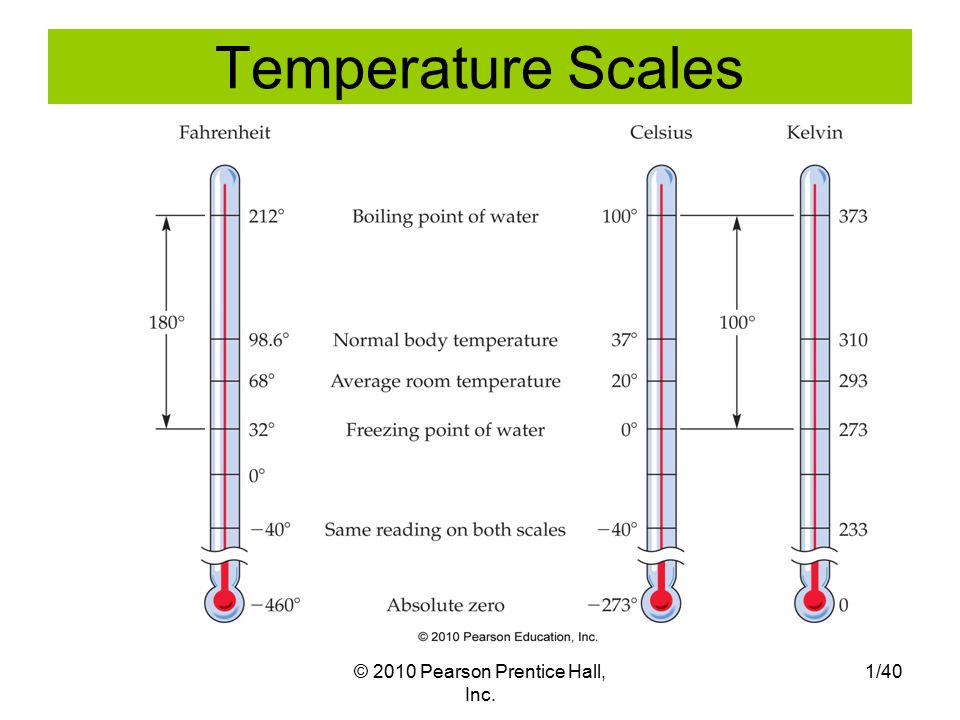 When measuring the temperature in the armpit, you just need to hold the child's hand with a thermometer with your hand or use an ear infrared thermometer.
When measuring the temperature in the armpit, you just need to hold the child's hand with a thermometer with your hand or use an ear infrared thermometer.
Fever is an increase in body temperature ≥38˚ C, in most cases it is not dangerous, it is a normal physiological reaction of the body to infectious and non-infectious diseases. In young children, febrile illnesses are common and are usually caused by viral infections.
In the body, the role of the thermoregulation center is performed by the hypothalamus, its mechanism of action is based on achieving a balance between heat production and heat loss.
Febrile convulsions are genetically determined, develop in 3-4% of children, as a rule, are not accompanied by epileptic activity of the brain, do not affect the further development of the child and do not recur after 6 years. In almost 50% of cases, febrile convulsions are single, however, if they are present in the history of the child, antipyretics are recommended for him at lower fever numbers.
Of course, one can understand the excitement of parents and grandparents when a child has a fever, but they need to remember that by lowering the temperature, especially low values, they calm themselves more than help the child. So, in most viral infections, only during an increase in temperature, antibodies to the virus and various active substances are produced that are responsible for the immune response and immunological memory. Therefore, an artificial decrease in temperature can lengthen the period of the disease. If a child has started antibiotic therapy for a bacterial infection, it is important to evaluate the effectiveness of the antibiotic, which can be seen primarily by self-reduction of body temperature. Against the background of antipyretics, this is quite difficult to do, and the sooner the child receives the correct treatment, the lower the risk of possible complications. Taking into account all of the above, international recommendations have been developed for the appointment of antipyretics. They are indicated in initially healthy children under the age of 3 months with an increase in body temperature above 38 °C. For children older than 3 months, antipyretics are prescribed at a temperature above 39-39.5˚С. For children at risk (with congenital heart defects, diseases of the central nervous system, etc.), as well as with previously identified febrile convulsions, the temperature is reduced to a lower temperature - 37.5-38 ° C. If the child feels unwell with a fever, refuses to eat and drink, parents can begin to lower the temperature to a lower temperature. No guideline for the management of children with fever recommends the use of antipyretics solely to reduce fever.
They are indicated in initially healthy children under the age of 3 months with an increase in body temperature above 38 °C. For children older than 3 months, antipyretics are prescribed at a temperature above 39-39.5˚С. For children at risk (with congenital heart defects, diseases of the central nervous system, etc.), as well as with previously identified febrile convulsions, the temperature is reduced to a lower temperature - 37.5-38 ° C. If the child feels unwell with a fever, refuses to eat and drink, parents can begin to lower the temperature to a lower temperature. No guideline for the management of children with fever recommends the use of antipyretics solely to reduce fever.
Temperature reduction is carried out by physical cooling methods and, if necessary, medication. If the child does not have chills, marbling of the skin, the room should be ventilated, the child is open. With cold hands and feet, they must be rubbed to redness or given a no-shpu in order to expand the peripheral vessels for an adequate heat transfer process. The drugs of choice among antipyretics for children are paracetamol and ibuprofen with many convenient dosage forms for the child. A single dose is calculated on body weight and is 10-15 mg / kg (every 6 hours, if necessary) for paracetamol and 5-10 mg / kg (every 6 hours, if necessary) for ibuprofen. If the dose of antipyretics is insufficient, the effect of them may not be. In the presence of vomiting, the form in candles is convenient. A decrease in temperature, as a rule, can be expected 30-60 minutes after taking the drug (somewhat longer with rectal use) and the effect lasts up to 3-8 hours. If the temperature is very high, physical cooling methods can be used until the antipyretic begins to take effect or until the time of the next dose of the drug. Vinegar and vodka, when rubbed, can have both a local irritant effect and a toxic effect when absorbed through the skin. Therefore, the simplest and safest way is to wipe the child with ordinary water at 25-30˚ C. It is necessary to wipe the neck, back of the head, inguinal and axillary folds, forehead, and then other surfaces.
The drugs of choice among antipyretics for children are paracetamol and ibuprofen with many convenient dosage forms for the child. A single dose is calculated on body weight and is 10-15 mg / kg (every 6 hours, if necessary) for paracetamol and 5-10 mg / kg (every 6 hours, if necessary) for ibuprofen. If the dose of antipyretics is insufficient, the effect of them may not be. In the presence of vomiting, the form in candles is convenient. A decrease in temperature, as a rule, can be expected 30-60 minutes after taking the drug (somewhat longer with rectal use) and the effect lasts up to 3-8 hours. If the temperature is very high, physical cooling methods can be used until the antipyretic begins to take effect or until the time of the next dose of the drug. Vinegar and vodka, when rubbed, can have both a local irritant effect and a toxic effect when absorbed through the skin. Therefore, the simplest and safest way is to wipe the child with ordinary water at 25-30˚ C. It is necessary to wipe the neck, back of the head, inguinal and axillary folds, forehead, and then other surfaces.
It is not recommended to alternate paracetamol and ibuprofen, as well as to give their combined preparations, this combination is no more effective than monotherapy, but is fraught with serious side effects and can lead to acute renal failure. Also, nimesulide, acetylsalicylic acid preparations are not used in children with an antipyretic purpose, and metamizole (analgin) can only be administered intramuscularly in order to quickly reduce the temperature. All of these drugs can cause serious side effects that are incomparable to their antipyretic effect.
Usually a decrease in temperature by 0.5-1˚ C is sufficient to improve the child's well-being, it is not necessary to achieve a decrease in temperature to normal numbers. Large diurnal fluctuations in temperature may have a more significant negative effect than the fever itself.
We have already said above that fever in children is most often accompanied by acute infectious diseases, which can be both viral and bacterial etiology. In the vast majority of cases, a viral infection does not require the appointment of an antibiotic (antibiotics do not act on viruses), children are treated with symptomatic agents and, if necessary, reduce the temperature. In the case of a proven bacterial etiology of the disease, it is necessary to prescribe antibiotic therapy. It is up to the doctor to decide what exactly the child is sick with, and, accordingly, how to treat him. However, if the disease begins with fever, runny nose and cough, the child's condition suffers slightly, with a high degree of probability one can think about the development of a respiratory viral infection and treat the child symptomatically. If the temperature persists for more than 3 days, of course, it is necessary to consult a doctor, control a blood test, if urine is needed, with a decision on the advisability of prescribing an antibiotic. A disease that is not accompanied by catarrhal symptoms, a runny nose, should be more alert to both parents and doctors, due to the higher likelihood of any bacterial infection that needs to be diagnosed and treated in time.
In the vast majority of cases, a viral infection does not require the appointment of an antibiotic (antibiotics do not act on viruses), children are treated with symptomatic agents and, if necessary, reduce the temperature. In the case of a proven bacterial etiology of the disease, it is necessary to prescribe antibiotic therapy. It is up to the doctor to decide what exactly the child is sick with, and, accordingly, how to treat him. However, if the disease begins with fever, runny nose and cough, the child's condition suffers slightly, with a high degree of probability one can think about the development of a respiratory viral infection and treat the child symptomatically. If the temperature persists for more than 3 days, of course, it is necessary to consult a doctor, control a blood test, if urine is needed, with a decision on the advisability of prescribing an antibiotic. A disease that is not accompanied by catarrhal symptoms, a runny nose, should be more alert to both parents and doctors, due to the higher likelihood of any bacterial infection that needs to be diagnosed and treated in time.