Fever temp for infants
Fever (0-12 Months)
Is this your child's symptom?
- An abnormal high body temperature
- Fever is the only symptom. Your child has a true fever if:
- Rectal (bottom), Ear or Forehead temperature: 100.4° F (38.0° C) or higher
- Under the arm (armpit) temperature: 99° F (37.2° C) or higher
- Caution: Ear temperatures are not accurate before 6 months of age
- Caution: Forehead temperatures must be digital. Forehead strips are not accurate.
Causes of Fever
- Overview. Almost all fevers are caused by a new infection. Viruses cause 10 times more infections than bacteria. The number of germs that cause an infection are in the hundreds. Only a few common ones will be listed.
- Viral Infections. Colds, flu and other viral infections are the most common cause. Fever may be the only symptom for the first 24 hours. The start of viral symptoms (runny nose, cough, loose stools) is often delayed.
Roseola is the most extreme example. Fever may be the only symptom for 3 to 5 days. Then a rash appears.
- Bacterial Infections. A bladder infection is the most common cause of silent fever in girls.
- Vaccine Fever. Fever with most vaccines begins within 12 hours. It lasts 2 to 3 days. This is normal and harmless. It means the vaccine is working.
- Newborn Fever (Serious). Fever that occurs during the first 3 months of life can be serious. All of these babies need to be seen as soon as possible. The fever may be due to sepsis (a bloodstream infection). Bacterial infections in this age group can get worse quickly. They need rapid treatment.
- Meningitis (Very Serious). A bacterial infection of the membrane that covers the spinal cord and brain. The main symptoms are a stiff neck, headache and confusion. Younger children are lethargic or so irritable that they can't be consoled. If not treated early, can suffer brain damage.

- Overheated. The fever is usually low grade. Can occur during heat waves or from being overdressed. The temp becomes normal in a few hours after moving to a cooler place. Fever goes away quickly with rest and drinking extra fluids.
- Not Due to Teething. Research shows that "getting teeth" does not cause fevers.
Fever and Crying
- Fever on its own shouldn't cause much crying.
- Frequent crying in a child with fever is caused by pain until proven otherwise.
- Hidden causes can be ear infections, kidney infections, sore throats and meningitis.
Normal Temperature Range
- Rectal. A reading of 98.6° F (37° C) is just the average rectal temp. A normal low can be 96.8° F (36° C) in the morning. It can change to a high of 100.3° F (37.9° C) late in the day. This is a normal range.
When to Call for Fever (0-12 Months)
Call 911 Now
- Not moving
- Can't wake up
- Severe trouble breathing (struggling for each breath; can barely speak or cry)
- Purple or blood-colored spots or dots on skin
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Trouble breathing, but not severe
- Great trouble swallowing fluids or spit
- Fever in baby less than 12 weeks old.
 Caution: Do NOT give your baby any fever medicine before being seen.
Caution: Do NOT give your baby any fever medicine before being seen. - Fever over 104° F (40° C)
- Shaking chills (shivering) lasting more than 30 minutes
- Nonstop crying or cries when touched or moved
- Won't move an arm or leg normally
- Dehydration suspected. No urine in over 8 hours, dark urine, very dry mouth and no tears.
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Age 3-6 months old with fever
- Age 6-12 months old with fever that lasts more than 24 hours. There are no other symptoms (such as cough or diarrhea).
- Fever lasts more than 3 days
- Fever returns after gone for more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Fever with no other symptoms and your child acts mildly ill
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Fever
- What You Should Know About Fever:
- Having a fever means your child has a new infection.
- It's most likely caused by a virus.
- You may not know the cause of the fever until other symptoms develop. This may take 24 hours.
- For infants more than 3 months old, most fevers are good for sick children. They help the body fight infection.

- Use the ranges below to help put your child's level of fever into perspective:
- 100° - 102° F (37.8° - 39° C) Low grade fever: helpful, good range. Don't treat.
- 102° - 104° F (39 - 40° C) Average fever: helpful. Treat if causes discomfort.
- Over 104° F (40° C) High fever: causes discomfort, but harmless. Always treat.
- Over 106° F (41.1° C) Very high fever: important to bring it down. Rare to go this high.
- Over 108° F (42.3° C) Dangerous fever: fever itself can be harmful.
- Treatment for All Fevers - Extra Fluids:
- Fluids alone can lower the fever. Reason: being well hydrated helps the body give off heat through the skin.
- For shivering (or the chills), give your child a blanket. Make them comfortable.
- Offer your child extra water or other fluids by mouth. Cold fluids are better. Until 6 months old, only give extra formula or breastmilk.
- For all children, dress in 1 layer of light weight clothing, unless shivering.
 Reason: also helps heat loss from the skin.
Reason: also helps heat loss from the skin. - For shivering (or the chills), give your child a blanket. Make them comfortable.
- Caution: if a baby under 1 year has a fever, never overdress or bundle up. Reason: Babies can get over-heated more easily than older children.
- Fever Medicine:
- Caution: Do not give a baby under 3 months any fever medicine. Most of these babies will need to be seen.
- For fevers 100°-102° F (37.8° - 39°C), fever meds are not needed. Reason: fevers in this range help the body fight the infection. Fevers turn on the body's imune system. Fevers don't cause any discomfort. Fever meds are mainly needed for fevers higher than 102° F (39° C).
- Give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil) if over 6 months old.
- Goal of treatment: keep the fever at a helpful level. Most often, the fever meds lower the fever by 2° to 3° F (1 - 1.
 5° C). They do not bring it down to normal. It takes 1 or 2 hours to see the effect.
5° C). They do not bring it down to normal. It takes 1 or 2 hours to see the effect. - Do not use aspirin. Reason: Risk of Reye syndrome, a rare but serious brain disease.
- Do not use both acetaminophen and ibuprofen together. Reason: Not needed and a risk of giving too much.
- Pain: fever does not cause pain. If your child also has pain, it's from the infection. It may be a sore throat or muscle pain. Treat the pain, if it's more than mild.
- Return to Child Care:
- Your child can return to child care after the fever is gone. Your child should feel well enough to join in normal activities.
- What to Expect:
- Most fevers with viral illnesses range between 101° and 104° F (38.4° and 40° C).
- They may last for 2 or 3 days.
- They are not harmful.
- Call Your Doctor If:
- Your child looks or acts very sick
- Any serious symptoms occur such as trouble breathing
- Fever goes above 104° F (40° C)
- Any fever occurs if less than 12 weeks old
- Fever without other symptoms lasts more than 24 hours
- Fever lasts more than 3 days (72 hours)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.

Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 10/31/2022
Last Revised: 09/18/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
Fevers (for Parents) - Nemours KidsHealth
All kids get a fever from time to time. A fever itself usually causes no harm and can actually be a good thing — it's often a sign that the body is fighting an infection.
But when your child wakes in the middle of the night flushed, hot, and sweaty, it's easy to be unsure of what to do next. Should you get out the thermometer? Call the doctor?
Here's more about fevers, including when to contact your doctor.
What Is a Fever?
Fever happens when the body's internal "thermostat" raises the body temperature above its normal level. This thermostat is found in a part of the brain called the hypothalamus. The hypothalamus knows what temperature your body should be (usually around 98. 6°F/37°C) and will send messages to your body to keep it that way.
6°F/37°C) and will send messages to your body to keep it that way.
Most people's body temperatures change a little bit during the course of the day: It's usually a little lower in the morning and a little higher in the evening and can vary as kids run around, play, and exercise.
Sometimes, though, the hypothalamus will "reset" the body to a higher temperature in response to an infection, illness, or some other cause. Why? Researchers believe that turning up the heat is a way for the body to fight the germs that cause infections, making it a less comfortable place for them.
What Causes Fevers?
It's important to remember that fever by itself is not an illness — it's usually a sign or symptom of another problem.
Fevers can be caused by a few things, including:
Infection: Most fevers are caused by infection or other illness. A fever helps the body fight infections by stimulating natural defense mechanisms.
Overdressing: Infants, especially newborns, may get fevers if they're overbundled or in a hot environment because they don't regulate their body temperature as well as older kids. But because fevers in newborns can indicate a serious infection, even infants who are overdressed must be checked by a doctor if they have a fever.
But because fevers in newborns can indicate a serious infection, even infants who are overdressed must be checked by a doctor if they have a fever.
Immunizations: Babies and kids sometimes get a low-grade fever after getting vaccinated.
Although teething may cause a slight rise in body temperature, it's probably not the cause if a child's temperature is higher than 100°F (37.8°C).
When Is a Fever a Sign of Something Serious?
In healthy kids, not all fevers need to be treated. High fever, though, can make a child uncomfortable and make problems (such as dehydration) worse.
Doctors decide on whether to treat a fever by considering both the temperature and a child's overall condition.
Kids whose temperatures are lower than 102°F (38.9°C) often don't need medicine unless they're uncomfortable. There's one important exception: If an infant 3 months or younger has a rectal temperature of 100.4°F (38°C) or higher, call your doctor or go to the emergency department immediately. Even a slight fever can be a sign of a potentially serious infection in very young babies.
Even a slight fever can be a sign of a potentially serious infection in very young babies.
If your child is between 3 months and 3 years old and has a fever of 102.2°F (39°C) or higher, call to see if your doctor needs to see your child. For older kids, take behavior and activity level into account. Watching how your child behaves will give you a pretty good idea of whether a minor illness is the cause or if your child should be seen by a doctor.
The illness is probably not serious if your child:
- is still interested in playing
- is eating and drinking well
- is alert and smiling at you
- has a normal skin color
- looks well when his or her temperature comes down
And don't worry too much about a child with a fever who doesn't want to eat. This is very common with infections that cause fever. For kids who still drink and urinate (pee) normally, not eating as much as usual is OK.
Is it a Fever?
A gentle kiss on the forehead or a hand placed lightly on the skin is often enough to give you a hint that your child has a fever. However, this method of taking a temperature (called tactile temperature) won't give an accurate measurement.
However, this method of taking a temperature (called tactile temperature) won't give an accurate measurement.
Use a reliable digital thermometer to confirm a fever. It's a fever when a child's temperature is at or above one of these levels:
- measured orally (in the mouth): 100°F (37.8°C)
- measured rectally (in the bottom): 100.4°F (38°C)
- measured in an axillary position (under the arm): 99°F (37.2°C)
But how high a fever is doesn't tell you much about how sick your child is. A simple cold or other viral infection can sometimes cause a rather high fever (in the 102°–104°F/38.9°–40°C range), but this doesn't usually mean there's a serious problem. In fact, a serious infection, especially in infants, might cause no fever or even a low body temperature (below 97°F or 36.1°C).
Because fevers can rise and fall, a child might have chills as the body's temperature begins to rise. The child may sweat to release extra heat as the temperature starts to drop.
The child may sweat to release extra heat as the temperature starts to drop.
Sometimes kids with a fever breathe faster than usual and may have a faster heart rate. Call the doctor if your child has trouble breathing, is breathing faster than normal, or is still breathing fast after the fever comes down.
p
How Can I Help My Child Feel Better?
Again, not all fevers need to be treated. In most cases, a fever should be treated only if it's causing a child discomfort.
Here are ways to ease symptoms that often accompany a fever:
Medicines
If your child is fussy or uncomfortable, you can give acetaminophen or ibuprofen based on the package recommendations for age or weight. (Unless instructed by a doctor, never give aspirin to a child due to its association with Reye syndrome, a rare but potentially fatal disease.) If you don't know the recommended dose or your child is younger than 2 years old, call the doctor to find out how much to give.
Infants younger than 2 months old should not be given any medicine for fever without being checked by a doctor. If your child has any medical problems, check with the doctor to see which medicine is best to use. Remember that fever medicine can temporarily bring a temperature down, but usually won't return it to normal — and it won't treat the underlying reason for the fever.
If your child has any medical problems, check with the doctor to see which medicine is best to use. Remember that fever medicine can temporarily bring a temperature down, but usually won't return it to normal — and it won't treat the underlying reason for the fever.
Home Comfort Measures
Dress your child in lightweight clothing and cover with a light sheet or blanket. Overdressing and overbundling can prevent body heat from escaping and can cause the temperature to rise.
Make sure your child's bedroom is a comfortable temperature — not too hot or too cold.
While some parents use lukewarm sponge baths to lower fever, this method only helps temporarily, if at all. In fact, sponge baths can make kids uncomfortable. Never use rubbing alcohol (it can cause poisoning when absorbed through the skin) or ice packs/cold baths (they can cause chills that can raise body temperature).
Food and Drinks
Offer plenty of fluids to avoid dehydration because fevers make kids lose fluids more rapidly than usual. Water, soup, ice pops, and flavored gelatin are all good choices. Avoid drinks with caffeine, including colas and tea, because they can make dehydration worse by increasing urination (peeing).
Water, soup, ice pops, and flavored gelatin are all good choices. Avoid drinks with caffeine, including colas and tea, because they can make dehydration worse by increasing urination (peeing).
If your child also is vomiting and/or has diarrhea, ask the doctor if you should give an electrolyte (rehydration) solution made especially for kids. You can find these at drugstores and supermarkets. Don't offer sports drinks — they're not made for younger children and the added sugars can make diarrhea worse. Also, limit your child's intake of fruits and apple juice.
In general, let kids eat what they want (in reasonable amounts), but don't force it if they don't feel like it.
Taking it Easy
Make sure your child gets plenty of rest. Staying in bed all day isn't necessary, but a sick child should take it easy.
It's best to keep a child with a fever home from school or childcare. Most doctors feel that it's safe to return when the temperature has been normal for 24 hours.
When Should I Call the Doctor?
The exact temperature that should trigger a call to the doctor depends on a child's age, the illness, and whether there are other symptoms with the fever.
Call your doctor if you have an:
- infant younger than 3 months old with a rectal temperature of 100.4°F (38°C) or higher
- older child with a temperature of higher than 102.2°F (39°C)
Also call if an older child has a fever of lower than 102.2°F (39°C) but also:
- refuses fluids or seems too ill to drink adequately
- has lasting diarrhea or repeated vomiting
- has any signs of dehydration (peeing less than usual, not having tears when crying, less alert and less active than usual)
- has a specific complaint (like a sore throat or earache)
- still has a fever after 24 hours (in kids younger than 2 years old) or 72 hours (in kids 2 years or older)
- is getting fevers a lot, even if they only last a few hours each night
- has a chronic medical problem, such as heart disease, cancer, lupus, or sickle cell disease
- has a rash
- has pain while peeing
Get emergency care if your child shows any of these signs:
- crying that won't stop
- extreme irritability or fussiness
- sluggishness and trouble waking up
- a rash or purple spots that look like bruises on the skin (that were not there before your child got sick)
- blue lips, tongue, or nails
- infant's soft spot on the head seems to be bulging out or sunken in
- stiff neck
- severe headache
- limpness or refusal to move
- trouble breathing that doesn't get better when the nose is cleared
- leaning forward and drooling
- seizure
- moderate to severe belly pain
Also, ask if your doctor has specific guidelines on when to call about a fever.
What Else Should I Know?
All kids get fevers, and in most cases they're completely back to normal within a few days. For older babies and kids, the way they act can be more important than the reading on your thermometer. Everyone gets a little cranky when they have a fever. This is normal and should be expected.
But if you're ever in doubt about what to do or what a fever might mean, or if your child is acting ill in a way that concerns you even if there's no fever, always call your doctor for advice.
Reviewed by: Joanne Murren-Boezem, MD
Date reviewed: September 2018
Fever in children - NCCH
36.6˚ is the average normal body temperature for an adult. In children, the average body temperature is 0.3-0.4˚ C higher than in adults. In addition, the temperature in children is characterized by significant lability and its average fluctuations in newborns can be about 0.4 ° C, and in older children up to 1 ° C. Factors such as food intake, hunger, movement, restlessness, alternation of sleep and wakefulness. It must be remembered that there are daily fluctuations in temperature, in the evening it is usually slightly higher. In young children with insufficient maturity of thermoregulation processes, environmental factors have a significant impact, it is important to remember that children are very easy to both overcool and overheat, so the air temperature in the room, the quantity and quality of clothes on the child, etc. are important. If the child seemed hot to you, and you decided to measure the temperature, you must wait 15-20 minutes after sleep or physical activity, uncover the child. The temperature should not be measured in the hands of the mother, but in a calmly sitting or lying child. When measuring the temperature in the armpit, you just need to hold the child's hand with a thermometer with your hand or use an ear infrared thermometer.
It must be remembered that there are daily fluctuations in temperature, in the evening it is usually slightly higher. In young children with insufficient maturity of thermoregulation processes, environmental factors have a significant impact, it is important to remember that children are very easy to both overcool and overheat, so the air temperature in the room, the quantity and quality of clothes on the child, etc. are important. If the child seemed hot to you, and you decided to measure the temperature, you must wait 15-20 minutes after sleep or physical activity, uncover the child. The temperature should not be measured in the hands of the mother, but in a calmly sitting or lying child. When measuring the temperature in the armpit, you just need to hold the child's hand with a thermometer with your hand or use an ear infrared thermometer.
Fever is an increase in body temperature ≥38˚ C, in most cases it is not dangerous, it is a normal physiological reaction of the body to infectious and non-infectious diseases. In young children, febrile illnesses are common and are usually caused by viral infections.
In young children, febrile illnesses are common and are usually caused by viral infections.
In the body, the role of the thermoregulation center is performed by the hypothalamus, the mechanism of its action is based on achieving a balance between heat production and heat loss.
Febrile convulsions are genetically determined, develop in 3-4% of children, as a rule, are not accompanied by epileptic activity of the brain, do not affect the further development of the child and do not recur after 6 years. In almost 50% of cases, febrile convulsions are single, however, if they are present in the history of the child, antipyretics are recommended for him at lower fever numbers.
Of course, one can understand the excitement of parents and grandparents when a child has a fever, but they need to remember that by lowering the temperature, especially low values, they calm themselves more than help the child. So, in most viral infections, only during an increase in temperature, antibodies to the virus and various active substances are produced that are responsible for the immune response and immunological memory. Therefore, an artificial decrease in temperature can lengthen the period of the disease. If a child has started antibiotic therapy for a bacterial infection, it is important to evaluate the effectiveness of the antibiotic, which can be seen primarily by self-reduction of body temperature. Against the background of antipyretics, this is quite difficult to do, and the sooner the child receives the correct treatment, the lower the risk of possible complications. Taking into account all of the above, international recommendations have been developed for the appointment of antipyretics. They are indicated in initially healthy children under the age of 3 months with an increase in body temperature above 38 °C. For children older than 3 months, antipyretics are prescribed at a temperature above 39-39.5˚С. For children at risk (with congenital heart defects, diseases of the central nervous system, etc.), as well as with previously identified febrile convulsions, the temperature is reduced to a lower temperature - 37.
Therefore, an artificial decrease in temperature can lengthen the period of the disease. If a child has started antibiotic therapy for a bacterial infection, it is important to evaluate the effectiveness of the antibiotic, which can be seen primarily by self-reduction of body temperature. Against the background of antipyretics, this is quite difficult to do, and the sooner the child receives the correct treatment, the lower the risk of possible complications. Taking into account all of the above, international recommendations have been developed for the appointment of antipyretics. They are indicated in initially healthy children under the age of 3 months with an increase in body temperature above 38 °C. For children older than 3 months, antipyretics are prescribed at a temperature above 39-39.5˚С. For children at risk (with congenital heart defects, diseases of the central nervous system, etc.), as well as with previously identified febrile convulsions, the temperature is reduced to a lower temperature - 37.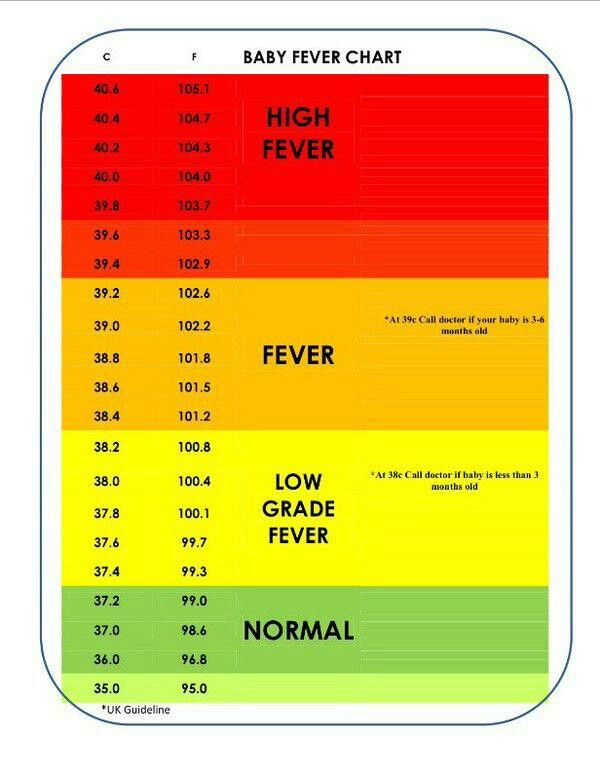 5-38 ° C. If the child feels unwell with a fever, refuses to eat and drink, parents can begin to lower the temperature to a lower temperature. No guideline for the management of children with fever recommends the use of antipyretics solely to reduce fever.
5-38 ° C. If the child feels unwell with a fever, refuses to eat and drink, parents can begin to lower the temperature to a lower temperature. No guideline for the management of children with fever recommends the use of antipyretics solely to reduce fever.
Temperature reduction is carried out by physical cooling methods and, if necessary, medication. If the child does not have chills, marbling of the skin, the room should be ventilated, the child is open. With cold hands and feet, they must be rubbed to redness or given a no-shpu in order to expand the peripheral vessels for an adequate heat transfer process. The drugs of choice among antipyretics for children are paracetamol and ibuprofen with many convenient dosage forms for the child. A single dose is calculated on body weight and is 10-15 mg / kg (every 6 hours, if necessary) for paracetamol and 5-10 mg / kg (every 6 hours, if necessary) for ibuprofen. If the dose of antipyretics is insufficient, the effect of them may not be. In the presence of vomiting, the form in candles is convenient. A decrease in temperature, as a rule, can be expected 30-60 minutes after taking the drug (somewhat longer with rectal use) and the effect lasts up to 3-8 hours. If the temperature is very high, physical cooling methods can be used until the antipyretic begins to take effect or until the time of the next dose of the drug. Vinegar and vodka, when rubbed, can have both a local irritant effect and a toxic effect when absorbed through the skin. Therefore, the simplest and safest way is to wipe the child with ordinary water at 25-30˚ C. It is necessary to wipe the neck, back of the head, inguinal and axillary folds, forehead, and then other surfaces.
In the presence of vomiting, the form in candles is convenient. A decrease in temperature, as a rule, can be expected 30-60 minutes after taking the drug (somewhat longer with rectal use) and the effect lasts up to 3-8 hours. If the temperature is very high, physical cooling methods can be used until the antipyretic begins to take effect or until the time of the next dose of the drug. Vinegar and vodka, when rubbed, can have both a local irritant effect and a toxic effect when absorbed through the skin. Therefore, the simplest and safest way is to wipe the child with ordinary water at 25-30˚ C. It is necessary to wipe the neck, back of the head, inguinal and axillary folds, forehead, and then other surfaces.
It is not recommended to alternate paracetamol and ibuprofen, as well as to give their combined preparations, this combination is no more effective than monotherapy, but is fraught with serious side effects and can lead to acute renal failure. Also, nimesulide, acetylsalicylic acid preparations are not used in children with an antipyretic purpose, and metamizole (analgin) can only be administered intramuscularly in order to quickly reduce the temperature.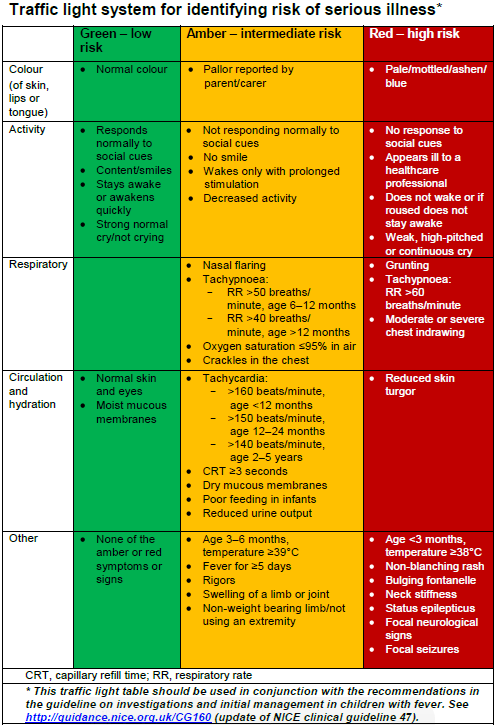 All of these drugs can cause serious side effects that are incomparable to their antipyretic effect.
All of these drugs can cause serious side effects that are incomparable to their antipyretic effect.
Usually a decrease in temperature by 0.5-1˚ C is sufficient to improve the child's well-being, it is not necessary to achieve a decrease in temperature to normal numbers. Large diurnal fluctuations in temperature may have a more significant negative effect than the fever itself.
We have already said above that fever in children is most often accompanied by acute infectious diseases, which can be of both viral and bacterial etiology. In the vast majority of cases, a viral infection does not require the appointment of an antibiotic (antibiotics do not act on viruses), children are treated with symptomatic agents and, if necessary, reduce the temperature. In the case of a proven bacterial etiology of the disease, it is necessary to prescribe antibiotic therapy. It is up to the doctor to decide what exactly the child is sick with, and, accordingly, how to treat him. However, if the disease begins with fever, runny nose and cough, the child's condition suffers slightly, with a high degree of probability one can think about the development of a respiratory viral infection and treat the child symptomatically. If the temperature persists for more than 3 days, of course, it is necessary to consult a doctor, control a blood test, if urine is needed, with a decision on the advisability of prescribing an antibiotic. A disease that is not accompanied by catarrhal symptoms, a runny nose, should be more alert to both parents and doctors, due to the higher likelihood of any bacterial infection that needs to be diagnosed and treated in time. Although some viral infections, such as enterovirus, can also occur without any symptoms other than high fever.
If the temperature persists for more than 3 days, of course, it is necessary to consult a doctor, control a blood test, if urine is needed, with a decision on the advisability of prescribing an antibiotic. A disease that is not accompanied by catarrhal symptoms, a runny nose, should be more alert to both parents and doctors, due to the higher likelihood of any bacterial infection that needs to be diagnosed and treated in time. Although some viral infections, such as enterovirus, can also occur without any symptoms other than high fever.
Remember that antipyretics are also drugs! They have their side effects! In addition, the imaginary improvement in the child's well-being against the background of antipyretics should not be a reason for refusing timely examination by a pediatrician and prescribing the necessary treatment.
Site map - Nizhnevartovsk city emergency medical station
Version for the visually impaired
- Home
- About the establishment
- Documents
- Structure of the institution
- Community Council
- Information about medical workers
- Availability indicators
- Working hours of a medical organization
- Paid services
- Vacancies
- Supervisory authorities
- Photo reports
- Activity
- Information about work in the MHI system
- Unified portal of public services
- Career guidance.
 Targeted learning. Employment of graduates
Targeted learning. Employment of graduates - Anti-corruption activities
- Information for patients
- Social services to the population
- Patient Questionnaire
- How to get high-tech medical care
- Internal regulations for the consumer of services
- Standards for the scope of medical care
- Information for citizens in need of pain relief
- Target values of the criteria for the availability and quality of medical care
- Conditions and procedure for the provision of medical care established by the territorial CHI program
- Information materials on the implementation of the state guarantees program
- List of medicines, medical devices and specialty health foods
- List of types, forms and conditions for the provision of medical care, the provision of which is carried out free of charge
- List of drugs used in the outpatient treatment of children from large families
- Rights and obligations of citizens in the field of health care
- Rights and obligations of insured persons
- Contacts
- Make an appointment with a doctor
- For specialists
- Telephone directory
- Vacancies
- Information for medical staff
|