Bump on baby back
Lipomyelomeningocele - Seattle Children's
What is a lipomyelomeningocele?
A lipomyelomeningocele (pronounced lipo-my-elo-men-IN-go-seal) is a birth defect that affects a child’s backbone (spine).
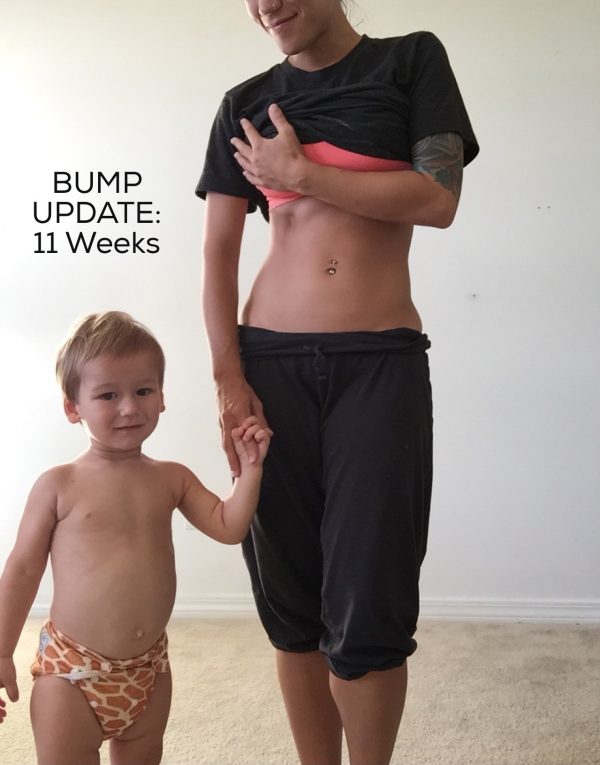
A lipomyelomeningocele is a fatty mass under the skin on the child’s back. It is usually in the middle of the back. The mass attaches to the spinal cord and may slowly pull on the cord.
A lipomyelomeningocele is covered by skin. You can usually see it on the outside of the child’s body. It looks like a large lump.
Lipomyelomeningocele in Children
Lipomyelomeningoceles are present when a baby is born (congenital).
Lipomyelomeningoceles happen in only 1 to 2 of every 10,000 babies born in the United States. It is slightly more common in girls.
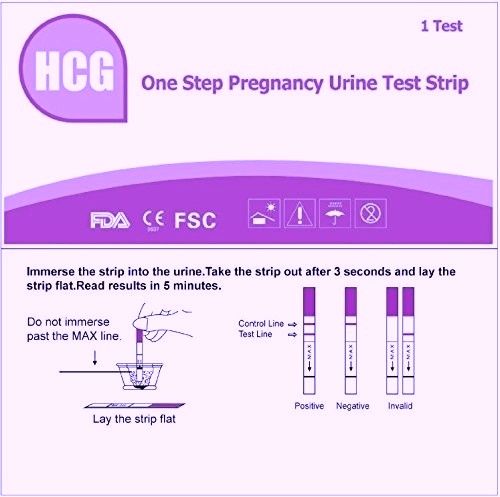
Babies develop lipomyelomeningoceles early in their mother’s pregnancy – during the fourth to sixth week. There is no known cause. The genes babies get from their parents do not play a role. It is not caused by mothers getting too little folic acid during pregnancy.
Lipomyelomeningocele at Seattle Children’s
We have a great deal of experience caring for babies and children with lipomyelomeningoceles.
Children with this condition often have complex problems that need special care. At Seattle Children’s, we bring many experts together in one clinic to treat your child. Neurosurgery is one part of your child’s medical team. Based on your child’s needs, the team may also include experts from Urology, Neurodevelopmental, Orthopedics and Rehabilitation.
Doctors outside of Seattle Children’s refer babies and children with lipomyelomeningoceles to us each year. Our neurosurgeons have a great deal of experience closing and repairing lipomyelomeningoceles. We use the latest and best neuromonitoring equipment during your child’s surgery.
Symptoms of Lipomyelomeningocele
All babies with a lipomyelomeningocele have a spinal cord that is stuck (tethered) into the fatty mass on their back. This may pull the spinal cord downward. Tethered spinal cord can cause symptoms, including:
Tethered spinal cord can cause symptoms, including:
- Back and leg pain
- Weak and numb legs
- Changes in bladder and bowel control
Diagnosing Lipomyelomeningocele
Usually, doctors can see a lipomyelomeningocele when a baby is born. They may see a lump or some other type of mark on your baby’s back, such as a fat pad, birthmark, dimple or tuft of hair.
Your child’s doctor will ask for a magnetic resonance imaging (MRI) of the spine to get a better view of your baby’s spinal cord and any problems that relate to it.
Sometimes, there is no lump or other mark on the baby’s back, and the child has no symptoms early on or never has symptoms at all. These cases may be diagnosed later in life, if symptoms develop, or if a scan done for some other reason shows the lipomyelomeningocele.
Treating Lipomyelomeningocele
Most babies with a lipomyelomeningocele need surgery.
Some lipomyelomeningoceles are not diagnosed until later in life because they caused no signs or symptoms earlier. These cases may not require surgery, unless the condition starts to cause pain or other problems.
These cases may not require surgery, unless the condition starts to cause pain or other problems.
Even after surgery to repair a lipomyelomeningocele, the spinal cord can become tethered. This can lead to neurological damage over time, especially during growth, because growth can stretch the tethered spinal cord. Slowly, the child may lose sensory and motor function. The feet may get weaker. Bladder and bowel function may get worse or be lost. These changes may last forever.
About 2 in 10 children in the United States who have had surgery for lipomyelomeningocele develop a tethered spinal cord and need more surgeries.
Treatment Options for Lipomyelomeningocele
Most often, babies treated at Seattle Children’s have lipomyelomeningocele surgery before age 1.
Your child’s neurosurgeon begins with a surgery called a laminectomy. The neurosurgeon removes parts of some bones in the spine (vertebrae). This lets the neurosurgeon get to the spinal cord or spinal nerve roots that need repair.
Next neurosurgeons remove some of the fatty mass (sometimes using a laser), and they free the spinal cord. Then they close the hole where the fatty mass enters your baby’s spinal canal. We monitor your child’s nerve function electrically during the surgery.
Skin Lump
Is this your child's symptom?
- A skin lump or bump covered by normal skin
- Skin swelling just in one spot (localized) is also included
Causes of Skin Lumps
- Insect Bites. The most common cause of an itchy bump is a mosquito bite. Other insects can also cause little bumps.
- Stings. A bee sting can cause a painful bump. The swelling can become quite large.
- Lymph Nodes. Most common cause of a lump or mass felt under the skin. Commonly found in the neck or groin. Nodes have a boundary or edge and are movable. This is not the case for the swelling seen with insect bites. Lymph nodes become larger with infections.

- Scalp Hematoma. The most common cause of a lump on the head is a scalp hematoma (goose egg). In a child under 2 years of age the injury may not have been seen.
- Injuries. New lumps anywhere can be caused by an injury that wasn't observed. A bruise is often present with the swelling.
- Callus. Broken bones heal with new bone formation. The medical term is callus. The callus feels like a bony knot that is larger than the bone itself. A callus is most commonly felt after a collarbone fracture.
- Boils. A boil is a skin abscess. It causes a very painful red lump.
Lumps that are a Normal Part of the Body
- Breast Bud. A small disc-shaped lump felt under the nipple. It indicates the onset of puberty in 7-12 year old girls.
- External Occipital Protuberance. The bony lump felt at the base of the skull in back.
- Mastoid Process.
 The bony lump felt behind each lower ear.
The bony lump felt behind each lower ear. - Xiphoid Process. A small hard lump felt at the lower end of the sternum (breastbone).
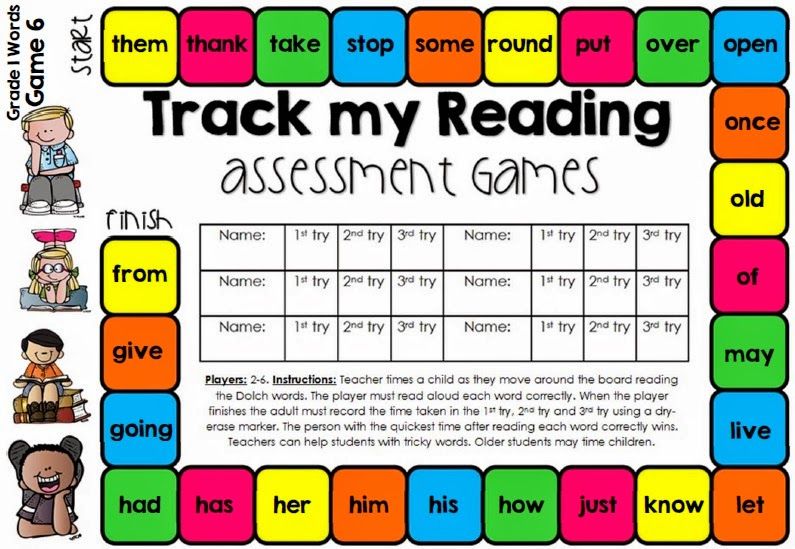
Common Objects Used to Guess the Size
- Pea or pencil eraser: ¼ inch or 6 mm
- Dime: ¾ inch or 1.8 cm
- Quarter: 1 inch or 2.5 cm
- Golf ball: 1 ½ inches or 3.8 cm
- Tennis Ball: 2 ½ inches or 6.4 cm
When to Call for Skin Lump
Call Doctor or Seek Care Now
- Redness spreading from the lump with fever
- Groin swelling and painful
- Age less than 12 months and on scalp. Exception: normal bump in back at base of skull.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Redness spreading from the lump without fever
- Boil suspected (painful, non-itchy, red lump)
- Age 12 months or older and on scalp. Exception: normal bump in back at base of skull.

- Can't move nearest joint normally (bend and straighten completely)
- Swelling is painful and cause not known
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- Large lump more than 1 inch (2.5 cm) and cause not known
- Small lump lasts more than 7 days and cause not known
- You have other questions or concerns
Self Care at Home
- Small lump present 7 days or less and cause not known. Reason: probably due to insect bite not observed.
- Breast bud - normal lump under the nipple
- External occipital protuberance - normal lump on back of head
- Mastoid process - normal lump behind each lower ear
- Xiphoid process - normal lump at bottom of breastbone
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice
Treatment for a Small Lump or Swelling
- What You Should Know:
- Most new swellings are due to insect bites.
 Mosquito bites account for 90% of them. Your child may not even know that he got bit.
Mosquito bites account for 90% of them. Your child may not even know that he got bit. - Suspect an insect bite if there are bites on other parts of the body.
- While most insect bites cause a small red bump, some are larger (like a hive).
- This does not mean your child has an allergy or the bite is infected.
- Here is some care advice that should help.
- Most new swellings are due to insect bites.
- Cold Pack for Swelling:
- Apply a cold pack or cold wet washcloth for 20 minutes.
- Steroid Cream for Itching:
- If the swelling is itchy, use 1% hydrocortisone cream (such as Cortaid). No prescription is needed.
- Do this 3 times per day.
- Allergy Medicine for Itching:
- If itching becomes severe, give a dose of Benadryl.
- No prescription is needed. Age limit: 1 and older.
- What to Expect:
- Most insect bites itch or hurt for 1 or 2 days.
- The swelling usually peaks in 2 days, but may last a week.

- If the swelling becomes larger or doesn't go away, it needs to be examined.
- Call Your Doctor If:
- Swelling becomes very painful
- Fever occurs
- Swelling becomes large (over 1 inch or 2.5 cm)
- Swelling lasts over 7 days
- You think your child needs to be seen
- Your child becomes worse
Lumps that are a Normal Part of the Body
- Breast Buds - Normal Lump Under the Nipple:
- Breast buds are normal, small disc-shaped rubbery lumps felt under the nipple.
- Age. They normally occur in 8-12 year old girls and are the first sign of puberty. Sometimes, they are even normal in 7 year olds.
- One Side. They sometimes start just on one side. Don't worry about that. Within 2 or 3 months, a breast bud will also appear on the other side.
- Importance. The entire breast develops entirely from the breast bud, taking 2 or 3 years to completion.
- Symptoms. Breast buds normally can be somewhat tender.
- Caution: Never squeeze or massage breast buds. Reason: Can cause a serious infection.
- Risks. None. Breast buds have no risk of turning into cancer.
- Follow-up. You can have your child's doctor check the breast bud during the next regular office visit.
- External Occipital Protuberance - Normal Lump on Back of Head:
- The lump you feel at the base of the skull in back is normal. It is a bony part of the skull that sticks out and feels hard.
- If you feel carefully, you will find one on yourself or other children.
- This is not caused by any injury.
- Mastoid Process - Normal Lump Behind the Ear:
- The mastoid process is a bony lump you can feel behind the lower ear.
- Muscles that turn the neck attach to the mastoid process.
- The process is larger in men because of larger neck muscles.

- The mastoid is filled with air cells that connect to the inner ear.
- Xiphoid Process - Normal Lump at Bottom of Breastbone:
- The small hard lump at the lower end of the sternum (breastbone) is normal. It is called the xiphoid process. You can feel it.
- It is more prominent in babies and slender children. Sometimes, it's more visible when breathing in.
- If you feel carefully, you will find one on yourself or other children.
- It's made of cartilage, but turns to bone in adults.
- Call Your Doctor If:
- You have other questions or concerns
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 10/31/2022
Last Revised: 01/13/2022
Copyright 2000-2022. Schmitt Pediatric Guidelines LLC.
Schmitt Pediatric Guidelines LLC.
Injuries in children. First aid and further actions - DMC UDP
Injuries in the summer are an integral part of childhood. Unfortunately, it is impossible to completely protect a child from injuries, but every adult is able to competently provide first aid. The most important rule is not to panic! If a child is injured, it is necessary to give him first aid and show him or consult a doctor. Depending on the nature of the damage, the scope of primary measures will be different.
The following types of injuries are distinguished:
Contusion in a child
The most common injury in children. As a result of a bruise, the skin is not damaged, but swelling and hemorrhage (bruising) appear at the site of impact. Ice or a chilled object must be applied to the injury site. You can do this several times during the first day in the form of applications for 5-7 minutes. With an increase in bruising, it is necessary to contact a traumatologist.
Dislocation in a child
This is an injury in which one of the bones that make up the joint is displaced outside the joint cavity. In childhood, dislocations often occur in the elbow joint and in the joints of the fingers. Any attempt to “set” a dislocation at the scene of an accident is strictly prohibited, even if a person with a medical education is trying to do it!
Ligament and tendon injury
This is a condition in which there is a partial rupture of the tendons or sprain of the ligaments. The most vulnerable places are the limbs.
Fracture
This is a type of injury that breaks the integrity of the bone. Distinguish between open and closed fractures. In the latter case, damage to the skin in the area of the fracture occurs.
First aid consists only in fixing the injured limb and transporting the child to the nearest medical facility. If the upper limb is damaged, the arm is fixed with a scarf bandage, if the lower limb is damaged, it is fixed with a splint along the entire length of the leg, using any available material for manufacturing. In case of an open fracture, it is necessary to cover the wound with a clean napkin; if possible, it is permissible to moisten the napkin with an antiseptic solution to avoid infection. It is optimal to fix the napkin with a band-aid or grab it with a bandage.
If the upper limb is damaged, the arm is fixed with a scarf bandage, if the lower limb is damaged, it is fixed with a splint along the entire length of the leg, using any available material for manufacturing. In case of an open fracture, it is necessary to cover the wound with a clean napkin; if possible, it is permissible to moisten the napkin with an antiseptic solution to avoid infection. It is optimal to fix the napkin with a band-aid or grab it with a bandage.
It is strictly forbidden to eliminate the displacement of bone fragments at the scene of the incident!
Abrasion
This is a superficial injury to the skin. In most cases, it is enough to treat the abrasion with any antiseptic solution. However, if redness occurs around the abrasion, swelling, fluid discharge of the child, it is necessary to show it to a pediatric surgeon.
Wounds
The most diverse type of injury. This is quite deep compared to an abrasion, skin damage, accompanied by bleeding. The main pre-medical measure for wounds is to stop bleeding. To do this, a pressure bandage is applied to the wound, previously, if possible, washing with water to remove foreign objects and treating with an antiseptic solution. It is forbidden to remove foreign bodies from the wound with your hands, since there is a possibility of displacing them inside the wound.
The main pre-medical measure for wounds is to stop bleeding. To do this, a pressure bandage is applied to the wound, previously, if possible, washing with water to remove foreign objects and treating with an antiseptic solution. It is forbidden to remove foreign bodies from the wound with your hands, since there is a possibility of displacing them inside the wound.
In case of abrasions and wounds, the issue of emergency vaccination against tetanus must be resolved, the need and amount of which is determined by the doctor.
Bites
Bites come from insects and animals. With minor insect bites, the doctor prescribes antihistamines, with a bite of a stinging insect (wasp, bee) - you must contact a medical institution for possible removal of the insect sting and treatment of the wound.
In the event of a tick bite, contacting a pediatric surgeon or orthopedic traumatologist is mandatory. You should not attempt to remove the tick yourself, as this increases the risk of infection with tick-borne encephalitis or borreliosis. You can protect your child and get vaccinated against tick-borne encephalitis at our children's medical center.
You can protect your child and get vaccinated against tick-borne encephalitis at our children's medical center.
If bitten by an animal, including a domestic animal, cover the bite with a clean bandage and seek immediate medical attention. When bitten by animals, children are prescribed a course of vaccinations aimed at preventing rabies.
Burn
Type of injury resulting from skin exposure to very high temperatures, chemicals, or combinations thereof. Most often, children get burned by fire or boiling water. There are several degrees of burns from mild, characterized by reddening of the skin, to severe, in which deep lesions of soft tissues are noted. With these injuries, it is necessary to stop the action of heat and chemical compounds as soon as possible and cool the affected area either under a stream of cold water or with wet, cold, frequently replaced wipes. Regardless of the degree of the burn, the child must be shown to the pediatric surgeon.
Electric shock or electric shock
This type of injury occurs when a child comes into contact with sockets, electrical appliances and wires. With such an injury, along with the occurrence of a burn at the point of contact, there is a violation in the work of the cardiovascular system in the form of an arrhythmic heartbeat and intermittent breathing. If you receive an electrical injury, you must immediately call an ambulance. Such children require medical supervision for several days.
With such an injury, along with the occurrence of a burn at the point of contact, there is a violation in the work of the cardiovascular system in the form of an arrhythmic heartbeat and intermittent breathing. If you receive an electrical injury, you must immediately call an ambulance. Such children require medical supervision for several days.
Treatment of bruising in the back
Bruising in the back is soft tissue damage caused by a strong blow, fall, accident, etc. Such injuries are fraught with serious danger, since there are not many soft tissues in the back area that could reduce the effects of the blow by taking it upon themselves. On the contrary, there is a high risk of damaging the spine and causing irreparable harm to health.
Symptoms
- severe pain, especially during movement;
- throbbing pain;
- edema;
- the appearance of a hematoma in the area of injury;
Otherwise, it all depends on which particular part of the back was injured.
Types of bruises
Depending on the location of the injury, there is the following classification of back bruises and their consequences:
- In case of bruising of the upper back , the cervical vertebrae may be affected. Sometimes this entails respiratory failure, paralysis, decreased tone and paresis of the muscles, impaired sensitivity.
- Contusion mid back may cause loss of coordination and sensation in the limbs. The victim may feel pain in the heart, experience discomfort during breathing.
- Injuries to the lower back are fraught with urination disorders and reduced sensation in the legs.
Bruises involving the spinal cord are the most dangerous. The consequences of such an injury can be varied: from circulatory disorders to rupture of nerve endings and paralysis.
Complications
In case of back bruises, the following complications are possible: bruising of the kidney, spine, lungs; fractures of the ribs, vertebrae; exacerbation of osteochondrosis; retroperitoneal hematoma;
Treatment of a bruise in the back
Regardless of the severity of the injury, the patient is prescribed bed rest.