How to determine miscarriage
Miscarriage Symptoms, Causes, Diagnosis, and Treatment
Written by WebMD Editorial Contributors
In this Article
- What Is a Miscarriage?
- Miscarriage Symptoms
- Miscarriage Causes and Risk Factors
- Miscarriage Types
- Miscarriage Diagnosis
- Miscarriage Treatments
- Symptoms Following a Miscarriage
- Pregnancy Following a Miscarriage
- When to Try to Conceive After a Miscarriage
- Miscarriage Prevention
What Is a Miscarriage?
A miscarriage is the loss of a baby before the 20th week of pregnancy. The medical term for a miscarriage is spontaneous abortion. But it isn’t an abortion in the common meaning of the term.
As many as 50% of all pregnancies end in miscarriage -- most often before a woman misses a menstrual period or even knows they’re pregnant. About 15%-25% of recognized pregnancies will end in a miscarriage.
More than 80% of miscarriages happen within the first 3 months of pregnancy. Miscarriages are less likely to happen after 20 weeks. When they do, doctors call them late miscarriages.
Miscarriage Symptoms
Symptoms of a miscarriage include:
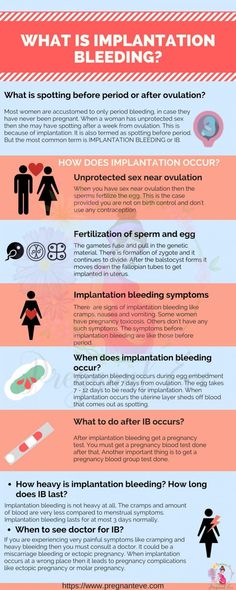
- Bleeding that goes from light to heavy
- Severe cramps
- Belly pain
- Weakness
- Worsening or severe back pain
- Fever with any of these symptoms
- Weight loss
- White-pink mucus
- Contractions
- Tissue that looks like blood clots passing from your vagina
- Fewer signs of pregnancy
If you have these symptoms, contact your doctor right away. They’ll tell you whether to come to the office or go to the emergency room.
Miscarriage Causes and Risk Factors
Most miscarriages happen when the unborn baby has fatal genetic problems. Usually, these problems are not related to the mother.
Usually, these problems are not related to the mother.
Other problems that can increase the risk of miscarriage include:
- Infection
- Medical conditions in the mother, such as diabetes or thyroid disease
- Hormone problems
- Immune system responses
- Physical problems in the mother
- Uterine abnormalities
- Smoking
- Drinking alcohol
- Using street drugs
- Exposure to radiation or toxic substances
A woman has a higher risk of miscarriage if they:
- Are over age 35
- Have certain diseases, such as diabetes or thyroid problems
- Have had three or more miscarriages
Cervical insufficiency. A miscarriage sometimes happens when the mother has a weakness of the cervix. Doctors call this a cervical insufficiency. It means the cervix can’t hold the pregnancy. This type of miscarriage usually happens in the second trimester.
Doctors call this a cervical insufficiency. It means the cervix can’t hold the pregnancy. This type of miscarriage usually happens in the second trimester.
There are usually few symptoms before a miscarriage caused by cervical insufficiency. You may feel sudden pressure, your water might break, and tissue from the baby and placenta could leave your body without much pain. Doctors usually treat an insufficient cervix with a "circling" stitch in the next pregnancy, usually around 12 weeks. The stitch holds your cervix closed until the doctor removes it around the time of delivery. If you never had a miscarriage but your doctor finds that you have cervical insufficiency they might add the stitch to prevent a miscarriage.
Miscarriage Types
There are different kinds of miscarriages, including:
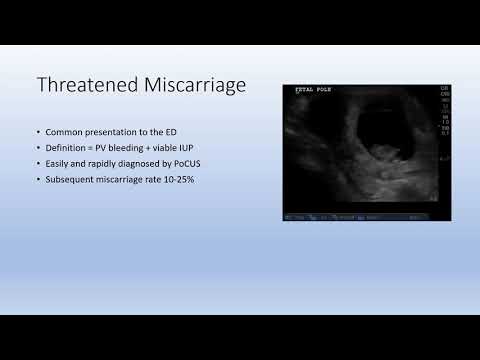
Threatened miscarriage. You’re bleeding and there’s the threat of a miscarriage, but your cervix hasn’t dilated. Your pregnancy will likely continue without any problems.
Inevitable miscarriage. You’re bleeding and cramping. Your cervix is dilated. A miscarriage is likely.
Incomplete miscarriage. Some tissue from the baby or the placenta leaves your body, but some stays in your uterus.
Complete miscarriage. All the pregnancy tissues leave your body. This type of miscarriage usually happens before the 12th week of pregnancy.
Missed miscarriage. The embryo dies or was never formed, but the tissues stay in your uterus.
Recurrent miscarriage (RM). You lose three or more pregnancies in a row during the first trimester. This type of miscarriage only affects about 1% of couples trying to have a baby.
Miscarriage Diagnosis
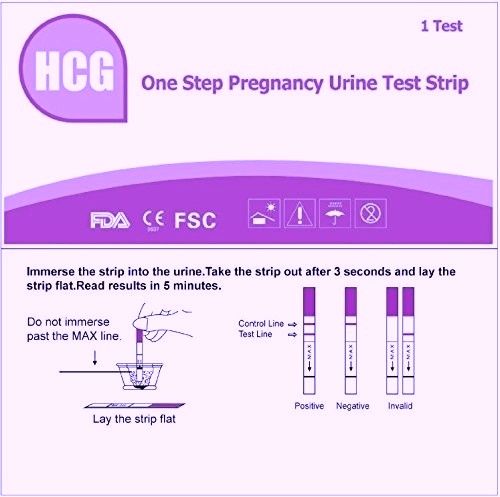
To check whether you've had a miscarriage, your doctor will do:
- A pelvic exam. They’ll check to see if your cervix has started to dilate.
- An ultrasound test. This test uses sound waves to check for a baby’s heartbeat.
 If the results aren’t clear, you may go back for another test in a week.
If the results aren’t clear, you may go back for another test in a week. - Blood tests. The doctor uses them to look for pregnancy hormones in your blood and compare it to past levels. They may also test you for anemia if you’ve been bleeding a lot.
- Tissue tests. If tissue left your body, the doctor may send it to a lab to confirm that you had a miscarriage. It can also help make sure there wasn’t another cause for your symptoms.
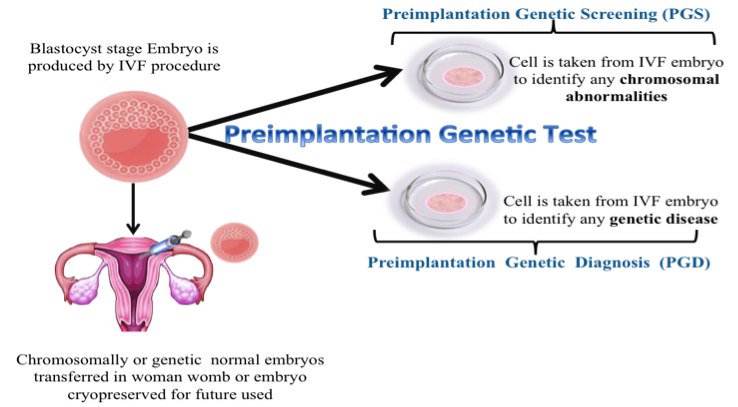
- Chromosome tests. If you’ve had two or more miscarriages, the doctor might do these tests to see if you or your partner’s genes are the cause.
Miscarriage Treatments
If the miscarriage is complete and your uterus is empty, you probably won’t need further treatment.
Sometimes all the tissue doesn’t come out. If that happens, your doctor might do a dilation and curettage (D&C) procedure. They’ll dilate your cervix and gently remove any remaining tissue. There are also medications you can take that cause any tissue left in your uterus to leave your body. This may be a better option if you want to avoid surgery.
There are also medications you can take that cause any tissue left in your uterus to leave your body. This may be a better option if you want to avoid surgery.
If it’s later in the pregnancy and the fetus has died in the womb, the doctor will induce labor and delivery.
When the bleeding stops, you should be able to go back to your normal activities. If your cervix dilated on its own but you’re still pregnant, you could have a condition known as incompetent cervix. Your doctor might do a procedure to close it called cerclage.
If your blood type is Rh negative, the doctor may give you a blood product called Rh immune globulin (Rhogam). This prevents you from developing antibodies that could harm your baby or any future pregnancies.
You may get blood tests, genetic tests, or medication if you’ve had more than two miscarriages in a row (recurrent miscarriage). To diagnose this condition, your doctor might use tests like:
- Pelvic ultrasound
- Hysterosalpingogram, An X-ray of the uterus and fallopian tubes
- Hysteroscopy.
 The doctor uses a thin, telescope-like device inserted through your vagina and cervix to look inside your uterus
The doctor uses a thin, telescope-like device inserted through your vagina and cervix to look inside your uterus
If you've had two miscarriages in a row, use a form of birth control and talk to your doctor about tests to find the cause
Symptoms Following a Miscarriage
Bleeding and mild discomfort are common symptoms after a miscarriage. If you have heavy bleeding with fever, chills, or pain, contact your doctor right away. These may be signs of an infection.
Besides the physical effects, you may also feel a range of emotions, from sadness and guilt to grief and worry about future pregnancies. What you’re feeling is normal. Let yourself grieve.
If you’re up to it, talk to people in your life who are supportive like your partner, a friend, or family member. You can also talk to a professional mental health counselor. Pregnancy loss support groups may also be a valuable resource to you and your partner. Ask your doctor for more information about these resources. And remember that everyone heals at a different pace and in different ways.
And remember that everyone heals at a different pace and in different ways.
Pregnancy Following a Miscarriage
You can get pregnant after a miscarriage. At least 85% of women who have one go on to have normal pregnancies and births. Having a miscarriage doesn’t mean you have a fertility problem. On the other hand, about 1%-2% of women may have repeated miscarriages (three or more). Some researchers believe this is related to an autoimmune response.
If you've had two miscarriages in a row, you should stop trying to conceive, use a form of birth control, and ask your doctor to do tests to figure out what’s causing the miscarriages.
When to Try to Conceive After a Miscarriage
Discuss the timing of your next pregnancy with your doctor. Some experts say you should wait a certain amount of time (from one menstrual cycle to 3 months) before you try again. While this is not a widespread practice, to prevent another miscarriage the doctor may suggest treatment with progesterone, a hormone that helps the embryo implant and supports early pregnancy in your uterus.
Taking time to heal both physically and emotionally after a miscarriage is important. Above all, don't blame yourself. Counseling is available to help you handle your loss.
Miscarriage Prevention
Most miscarriages happen because there’s a problem with the pregnancy. You can’t prevent them. If your doctor does testing and finds a problem, treatment options may be available.
If you have an illness, treating it can improve your chances for a successful pregnancy. One step you can take is to get as healthy as you can before you try to have a baby:
- Get regular exercise.
- Eat a healthy, well-balanced diet.
- Maintain a healthy weight.
- Avoid infections.
- Don’t smoke, drink alcohol, or take illegal drugs.
- Cut back on caffeine.
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Miscarriage - Diagnosis and treatment
Diagnosis
Your health care provider might do a variety of tests:
- Pelvic exam.
 Your health care provider might check to see if your cervix has begun to dilate.
Your health care provider might check to see if your cervix has begun to dilate. - Ultrasound. During an ultrasound, your health care provider will check for a fetal heartbeat and determine if the embryo is developing as it should be. If a diagnosis can't be made, you might need to have another ultrasound in about a week.
- Blood tests. Your health care provider might check the level of the pregnancy hormone, human chorionic gonadotropin (HCG), in your blood and compare it to previous measurements. If the pattern of changes in your HCG level is abnormal, it could indicate a problem. Your health care provider might check to see if you're anemic — which could happen if you've experienced significant bleeding — and may also check your blood type.
- Tissue tests. If you have passed tissue, it can be sent to a lab to confirm that a miscarriage has occurred — and that your symptoms aren't related to another cause.
- Chromosomal tests. If you've had two or more previous miscarriages, your health care provider may order blood tests for both you and your partner to determine if your chromosomes are a factor.
Possible diagnoses include:
- Threatened miscarriage. If you're bleeding but your cervix hasn't begun to dilate, there is a threat of miscarriage. Such pregnancies often proceed without any further problems.
- Inevitable miscarriage. If you're bleeding, cramping and your cervix is dilated, a miscarriage is considered inevitable.
- Incomplete miscarriage. If you pass fetal or placental material but some remains in your uterus, it's considered an incomplete miscarriage.
- Missed miscarriage. In a missed miscarriage, the placental and embryonic tissues remain in the uterus, but the embryo has died or was never formed.
- Complete miscarriage.
 If you have passed all the pregnancy tissues, it's considered a complete miscarriage. This is common for miscarriages occurring before 12 weeks.
If you have passed all the pregnancy tissues, it's considered a complete miscarriage. This is common for miscarriages occurring before 12 weeks. - Septic miscarriage. If you develop an infection in your uterus, it's known as a septic miscarriage. This can be a severe infection and demands immediate care.
More Information
- Pelvic exam
- Ultrasound
Treatment
Threatened miscarriage
For a threatened miscarriage, your health care provider might recommend resting until the bleeding or pain subsides. Bed rest hasn't been proved to prevent miscarriage, but it's sometimes prescribed as a safeguard. You might be asked to avoid exercise and sex, too. Although these steps haven't been proved to reduce the risk of miscarriage, they might improve your comfort.
In some cases, it's also a good idea to postpone traveling — especially to areas where it would be difficult to receive prompt medical care. Ask your health care provider if it would be wise to delay any upcoming trips you've planned.
Miscarriage
With ultrasound, it's now much easier to determine whether an embryo has died or was never formed. Either finding means that a miscarriage will definitely occur. In this situation, you might have several choices:
- Expectant management. If you have no signs of infection, you might choose to let the miscarriage progress naturally. Usually this happens within a couple of weeks of determining that the embryo has died. Unfortunately, it might take up to three or four weeks. This can be an emotionally difficult time. If expulsion doesn't happen on its own, medical or surgical treatment will be needed.
- Medical treatment. If, after a diagnosis of certain pregnancy loss, you'd prefer to speed the process, medication can cause your body to expel the pregnancy tissue and placenta. The medication can be taken by mouth or by insertion in the vagina. Your health care provider might recommend inserting the medication vaginally to increase its effectiveness and minimize side effects such as nausea and diarrhea.
 For about 70 to 90 percent of women, this treatment works within 24 hours.
For about 70 to 90 percent of women, this treatment works within 24 hours. - Surgical treatment. Another option is a minor surgical procedure called suction dilation and curettage (D&C). During this procedure, your health care provider dilates your cervix and removes tissue from the inside of your uterus. Complications are rare, but they might include damage to the connective tissue of your cervix or the uterine wall. Surgical treatment is needed if you have a miscarriage accompanied by heavy bleeding or signs of an infection.
Physical recovery
In most cases, physical recovery from miscarriage takes only a few hours to a couple of days. In the meantime, call your health care provider if you experience heavy bleeding, fever or abdominal pain.
You may ovulate as soon as two weeks after a miscarriage. Expect your period to return within four to six weeks. You can start using any type of contraception immediately after a miscarriage. However, avoid having sex or putting anything in your vagina — such as a tampon — for two weeks after a miscarriage.
However, avoid having sex or putting anything in your vagina — such as a tampon — for two weeks after a miscarriage.
Future pregnancies
It's possible to become pregnant during the menstrual cycle immediately after a miscarriage. But if you and your partner decide to attempt another pregnancy, make sure you're physically and emotionally ready. Ask your health care provider for guidance about when you might try to conceive.
Miscarriage is usually a one-time occurrence. Most women who miscarry go on to have a healthy pregnancy after miscarriage. Less than 5 percent of women have two consecutive miscarriages, and only 1 percent have three or more consecutive miscarriages.
If you experience multiple miscarriages, generally two or three in a row, consider testing to identify any underlying causes. Such causes could include problems with the uterus, blood clotting or chromosomes. If the cause of your miscarriages can't be identified, don't lose hope. About 60 to 80 percent of women with unexplained repeated miscarriages go on to have healthy pregnancies.
More Information
- Dilation and curettage (D&C)
Request an Appointment at Mayo Clinic
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
Emotional healing can take much longer than physical healing. Miscarriage can be a heart-wrenching loss that others around you might not fully understand. Your emotions might range from anger and guilt to despair. Give yourself time to grieve the loss of your pregnancy, and seek help from loved ones.
You'll likely never forget your hopes and dreams surrounding this pregnancy, but in time acceptance might ease your pain. Talk to your health care provider if you're feeling profound sadness or depression.
Preparing for your appointment
If you have signs or symptoms of miscarriage, contact your health care provider right away. Depending on the circumstances, you might need immediate medical care.
Here's some information to help you get ready for your appointment, and what to expect from your health care provider.
What you can do
Before your appointment, you might want to:
- Ask about pre-appointment restrictions. In most cases you'll be seen immediately. If that's not the case, ask whether you should restrict your activities while you wait for your appointment.
- Find a loved one or friend who can join you for your appointment. Fear and anxiety might make it difficult to focus on what your health care provider says. Take someone along who can help remember all the information.
- Write down questions to ask your health care provider. That way, you won't forget anything important that you want to ask, and you can make the most of your time with your health care provider.
Below are some basic questions to ask your health care provider about miscarriage:
- What are the treatment options?
- What kinds of tests do I need?
- Can I continue to do my usual activities?
- What signs or symptoms should prompt me to call you or go to the hospital?
- Do you know what caused my miscarriage?
- What are my chances for a successful future pregnancy?
In addition to the questions you've prepared, don't hesitate to ask other questions during your appointment — especially if you need clarification or you don't understand something.
What to expect from your health care provider
Your health care provider is likely to ask you a number of questions, too. For example:
- When was your last menstrual period?
- Were you using any contraceptive methods at the time you likely conceived?
- When did you first notice your signs or symptoms?
- Have your symptoms been continuous or occasional?
- Compared with your heaviest days of menstrual flow, is your bleeding more, less or about the same?
- Have you had a miscarriage before?
- Have you had any complications during a previous pregnancy?
- Do you have any other health conditions?
- Do you know your blood type?
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Early miscarriage - symptoms and how to prevent it
The term "early miscarriage" refers to a spontaneous abortion that occurs in the first 6-8 weeks of pregnancy. It can occur before 20 weeks of pregnancy for reasons related to the natural states of the fair sex. According to statistics, the logical outcome of every fifth pregnancy is a miscarriage. However, quite often a woman does not even know that she was pregnant by the time the fetus is rejected by the body.
It can occur before 20 weeks of pregnancy for reasons related to the natural states of the fair sex. According to statistics, the logical outcome of every fifth pregnancy is a miscarriage. However, quite often a woman does not even know that she was pregnant by the time the fetus is rejected by the body.
In addition, a curious pattern was revealed: more often than a natural one, a pregnancy induced artificially ends in a miscarriage. For example, in vitro fertilization, unfortunately, does not always lead to a successful pregnancy and the birth of a baby on time.
Why can an early miscarriage occur?
Here are the most common causes, each of which significantly increases the risk of miscarriage:
- the expectant mother has certain infectious diseases, as well as STDs;
- intoxication of a woman's body for various reasons, including as a result of her living in an ecologically unfavorable region;
- all kinds of metabolic disorders in the body;
- hormonal disruptions, including those caused by a malfunction of the thyroid gland;
- various neoplasms in the uterus and others, as well as the cervix, pathologies;
- maintenance by the future mother of a life far from a healthy lifestyle.
 May include drinking alcohol, smoking, taking psychotropic and narcotic drugs, as well as malnutrition;
May include drinking alcohol, smoking, taking psychotropic and narcotic drugs, as well as malnutrition; - obesity;
- immune status disorders;
- cardiac diseases;
- diabetes mellitus;
- too early for pregnancy or, conversely, the patient's overly mature age at times increases the risk of miscarriage;
- all kinds of pathologies of chromosomes and genes;
- prolonged exposure to stress or severe psycho-emotional trauma in a woman.
The timing of a miscarriage may depend, among other things, on the patient's genetic predisposition to miscarriage. Finally, often its specific cause remains unexplained to the end.
Symptoms of miscarriage
A pregnant woman should urgently seek medical help if she has the following warning signs:
- bleeding from the vagina;
- spotting discharge from the genital tract. They can have both light pink and intense red or brownish tint;
- convulsions;
- severe pain in the lumbar region;
- abdominal pain, etc.

All of the above signs can be symptoms of a miscarriage. Timely provision of qualified medical care is the key to maintaining pregnancy.
Life after miscarriage
If a woman could not bear the pregnancy - an early miscarriage crossed out all her plans - then she needs to calm down and take all measures to prevent such complications in the future. Usually obstetricians-gynecologists recommend planning a new pregnancy no earlier than six months after a miscarriage. During this time, a woman needs to be examined and find out if she has any pathology in her body that could lead to an abortion. It can be various STDs and infectious diseases. In the presence of chronic diseases that can provoke spontaneous abortion, it is necessary to throw all your efforts into their treatment.
Gynecologists of the corresponding department of our private clinic in Ryazan will help you find out what could have caused the miscarriage, as well as make recommendations on how to prepare for pregnancy. They usually include a set of physical exercises suitable for a woman, a diet rich in everything necessary for bearing a healthy baby, no stress, and measures to maintain a normal body mass index. Can't recover or get pregnant after a miscarriage? Contact "ON CLINIC in Ryazan" - here you will definitely be helped!
They usually include a set of physical exercises suitable for a woman, a diet rich in everything necessary for bearing a healthy baby, no stress, and measures to maintain a normal body mass index. Can't recover or get pregnant after a miscarriage? Contact "ON CLINIC in Ryazan" - here you will definitely be helped!
miscarriage, symptoms - Health Clinic 365 G. Yekaterinburg
Causes of miscarriage
Questions to the doctor about miscarriages
Diagnostics of miscarriage
Treatment and prevention of miscarriage
Pereki - this is spontaneous termination of pregnancy up to 20 weeks. According to statistics, 10 to 20% of all pregnancies end in miscarriage. However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy. Most miscarriages happen due to abnormal development of the fetus.
Miscarriage is quite common, but this fact does not make things any easier. It is always difficult to cope with the realization that there was a pregnancy, but no child. Try to deal with the situation psychologically and understand what could be causing the miscarriage, what increases the risk of it, and what type of treatment might be needed.
It is always difficult to cope with the realization that there was a pregnancy, but no child. Try to deal with the situation psychologically and understand what could be causing the miscarriage, what increases the risk of it, and what type of treatment might be needed.
Symptoms of miscarriage .
Most miscarriages occur before 12 weeks. Signs and symptoms of a miscarriage include:
- Vaginal bleeding or spotting (although quite common in early pregnancy)
- Pain or cramps in the abdomen or lower back
- Fluid vaginal discharge or tissue fragments
It is important to consider the fact that in early pregnancy, spotting or vaginal bleeding is quite common. In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage.
Some women who have a miscarriage develop an infection in the uterus.