What is pcos syndrome
Polycystic ovary syndrome (PCOS) - Care at Mayo Clinic
Polycystic ovary syndrome (PCOS) care at Mayo Clinic
Your Mayo Clinic care team
Mayo Clinic's care team for PCOS includes specialists trained in female reproductive medicine (gynecologists), hormone disorders (endocrinologists) and infertility (reproductive endocrinologists).
Specialists in the division of Reproductive Endocrinology and Infertility are frequently involved in care. Every staff doctor in that division is board certified in obstetrics and gynecology as well as reproductive endocrinology and infertility. These reproductive and infertility specialists work frequently with other specialists in endocrinology, metabolism and nutrition.
Mayo Clinic also has registered dietitians and certified diabetes care and education specialists to help with weight loss or diabetes prevention and treatment.
Having all of this expertise in a single place, focused on you, means that you're not just getting one opinion. Your care is discussed among the team, appointments are scheduled in coordination, and highly specialized PCOS experts work together to determine what's best for you.
Advanced diagnosis and treatment
Mayo Clinic has comprehensive diagnostic testing to identify PCOS. The disorder requires lifelong management to avoid complications such as diabetes and cardiovascular disease. Mayo Clinic has the multispecialty expertise to treat all of your health concerns, including infertility.
Many Mayo Clinic doctors who treat PCOS are also active researchers. They are working to improve treatment of PCOS. When you seek care at Mayo Clinic, you have access to the expertise of these Mayo Clinic care providers and researchers.
Nationally recognized expertise
Mayo Clinic in Rochester, Minnesota, ranks among the Best Hospitals for gynecology in the U. S. News & World Report Best Hospitals rankings.
S. News & World Report Best Hospitals rankings.
The Mayo Clinic experience and patient stories
Our patients tell us that the quality of their interactions, our attention to detail and the efficiency of their visits mean health care like they've never experienced. See the stories of satisfied Mayo Clinic patients.
Collaboration that changes lives
Elyn Simmons was 31 years old and eager to start a family with her husband, Guy. But in 2016, she was diagnosed with a hormonal disorder — PCOS, or polycystic ovary syndrome — that causes fertility problems. Then Elyn began experiencing other symptoms, including unexplained weight gain, increased body hair, migraines, and severe fatigue. Teamwork by Mayo Clinic clinicians and specialists in Mayo’s Department of Laboratory Medicine and Pathology found the source of Elyn's problem. In 2018, she was…
Expertise and rankings
- Experience. Mayo Clinic experts care for more than 2,100 women who have PCOS every year, using research-based treatments and teaching helpful lifestyle changes.

- Teamwork. Managing PCOS can require expertise in infertility, hirsutism, diabetes and cardiovascular care. Mayo Clinic experts work together closely to address all of your health concerns.
- Research. Mayo Clinic experts are continually studying how to improve the diagnosis and treatment of PCOS.
Learn more about Mayo Clinic's obstetrics and gynecology and endocrinology departments' expertise and rankings.
Locations, travel and lodging
Mayo Clinic has major campuses in Phoenix and Scottsdale, Arizona; Jacksonville, Florida; and Rochester, Minnesota. The Mayo Clinic Health System has dozens of locations in several states.
For more information on visiting Mayo Clinic, choose your location below:
Mayo Clinic's campus in Arizona
Mayo Clinic's campus in Florida
Mayo Clinic's campus in Minnesota
Mayo Clinic Health System
Costs and insurance
Mayo Clinic works with hundreds of insurance companies and is an in-network provider for millions of people.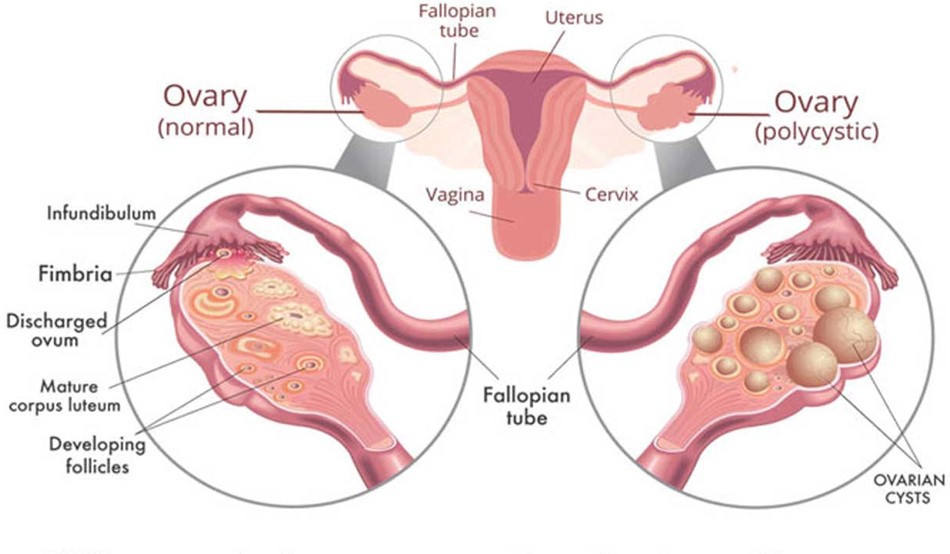
In most cases, Mayo Clinic doesn't require a physician referral. Some insurers require referrals, or may have additional requirements for certain medical care. All appointments are prioritized on the basis of medical need.
Learn more about appointments at Mayo Clinic.
Please contact your insurance company to verify medical coverage and to obtain any needed authorization prior to your visit. Often, your insurer's customer service number is printed on the back of your insurance card.
More information about billing and insurance:
Mayo Clinic in Arizona, Florida and Minnesota
Mayo Clinic Health System
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Polycystic Ovary Syndrome (PCOS) | Johns Hopkins Medicine
Polycystic ovary syndrome (PCOS) is a condition in which the ovaries produce an abnormal amount of androgens, male sex hormones that are usually present in women in small amounts. The name polycystic ovary syndrome describes the numerous small cysts (fluid-filled sacs) that form in the ovaries. However, some women with this disorder do not have cysts, while some women without the disorder do develop cysts.
However, some women with this disorder do not have cysts, while some women without the disorder do develop cysts.
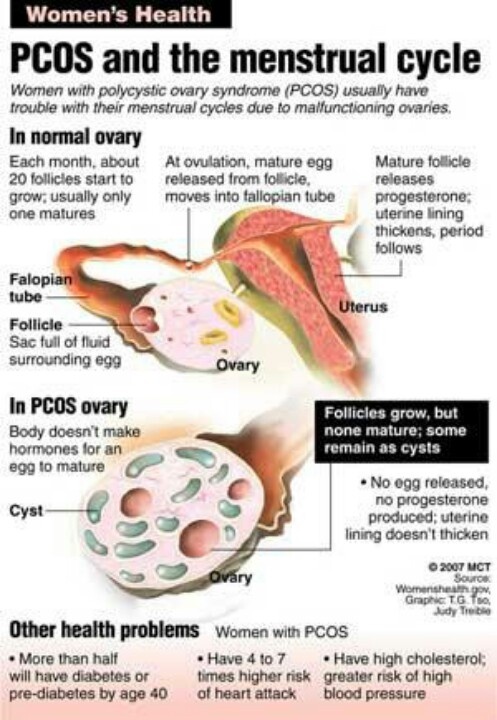
Ovulation occurs when a mature egg is released from an ovary. This happens so it can be fertilized by a male sperm. If the egg is not fertilized, it is sent out of the body during your period.
In some cases, a woman doesn’t make enough of the hormones needed to ovulate. When ovulation doesn’t happen, the ovaries can develop many small cysts. These cysts make hormones called androgens. Women with PCOS often have high levels of androgens. This can cause more problems with a woman’s menstrual cycle. And it can cause many of the symptoms of PCOS.
Treatment for PCOS is often done with medication. This can’t cure PCOS, but it helps reduce symptoms and prevent some health problems.
What causes PCOS?
The exact cause of PCOS is not clear. Many women with PCOS have insulin resistance. This means the body can't use insulin well. Insulin levels build up in the body and may cause higher androgen levels. Obesity can also increase insulin levels and make PCOS symptoms worse.
Obesity can also increase insulin levels and make PCOS symptoms worse.
PCOS may also run in families. It's common for sisters or a mother and daughter to have PCOS.
What are the risks for PCOS?
You may be more likely to have PCOS if your mother or sister has it. You may also be more likely to have it if you have insulin resistance or are obese.
What are the symptoms of PCOS?
The symptoms of PCOS may include:
-
Missed periods, irregular periods, or very light periods
-
Ovaries that are large or have many cysts
-
Excess body hair, including the chest, stomach, and back (hirsutism)
-
Weight gain, especially around the belly (abdomen)
-
Acne or oily skin
-
Male-pattern baldness or thinning hair
-
Infertility
-
Small pieces of excess skin on the neck or armpits (skin tags)
-
Dark or thick skin patches on the back of the neck, in the armpits, and under the breasts
How is PCOS diagnosed?
Your health care provider will ask about your medical history and your symptoms.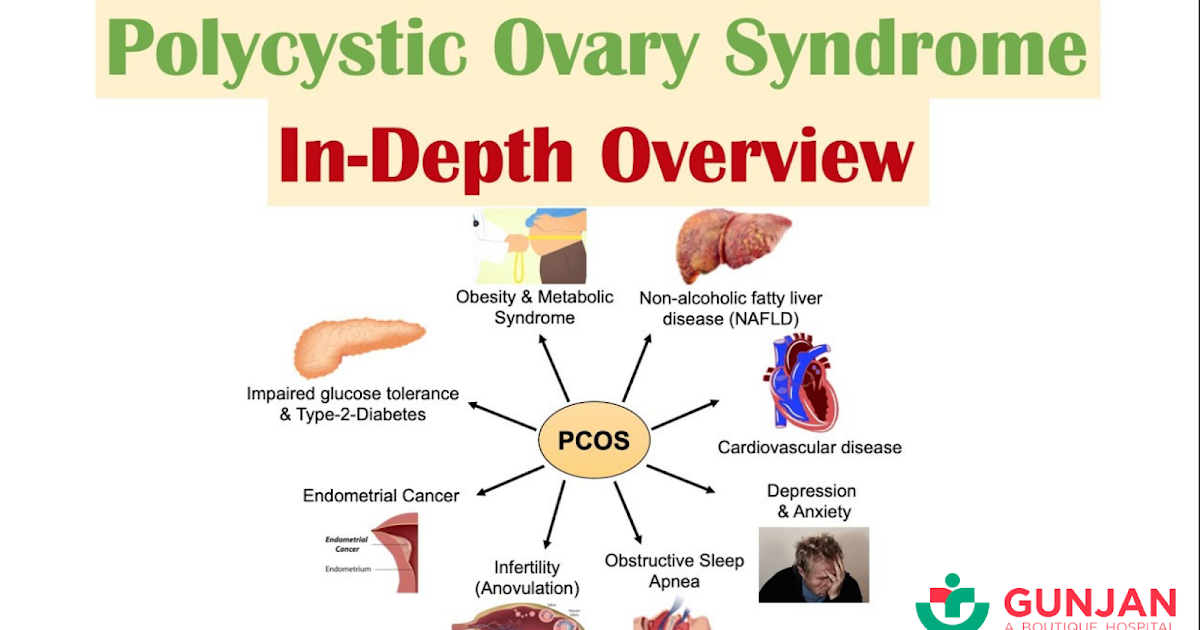 You will also have a physical exam. This will likely include a pelvic exam. This exam checks the health of your reproductive organs, both inside and outside your body.
You will also have a physical exam. This will likely include a pelvic exam. This exam checks the health of your reproductive organs, both inside and outside your body.
Some of the symptoms of PCOS are like those caused by other health problems. Because of this, you may also have tests such as:
-
Ultrasound. This test uses sound waves and a computer to create images of blood vessels, tissues, and organs. This test is used to look at the size of the ovaries and see if they have cysts. The test can also look at the thickness of the lining of the uterus (endometrium).
-
Blood tests. These look for high levels of androgens and other hormones. Your health care provider may also check your blood glucose levels. And you may have your cholesterol and triglyceride levels checked.
How is PCOS treated?
Treatment for PCOS depends on a number of factors. These may include your age, how severe your symptoms are, and your overall health. The type of treatment may also depend on whether you want to become pregnant in the future.
The type of treatment may also depend on whether you want to become pregnant in the future.
If you do plan to become pregnant, your treatment may include:
-
A change in diet and activity. A healthy diet and more physical activity can help you lose weight and reduce your symptoms. They can also help your body use insulin more efficiently, lower blood glucose levels, and may help you ovulate.
-
Medications to cause ovulation. Medications can help the ovaries to release eggs normally. These medications also have certain risks. They can increase the chance for a multiple birth (twins or more). And they can cause ovarian hyperstimulation. This is when the ovaries release too many hormones. It can cause symptoms such as abdominal bloating and pelvic pain.
If you do not plan to become pregnant, your treatment may include:
-
Birth control pills. These help to control menstrual cycles, lower androgen levels, and reduce acne.

-
Diabetes medication. This is often used to lower insulin resistance in PCOS. It may also help reduce androgen levels, slow hair growth, and help you ovulate more regularly.
-
A change in diet and activity. A healthy diet and more physical activity can help you lose weight and reduce your symptoms. They can also help your body use insulin more efficiently, lower blood glucose levels, and may help you ovulate.
-
Medications to treat other symptoms. Some medications can help reduce hair growth or acne.
What are the complications of PCOS?
Women with PCOS are more likely to develop certain serious health problems. These include type 2 diabetes, high blood pressure, problems with the heart and blood vessels, and uterine cancer. Women with PCOS often have problems with their ability to get pregnant (fertility).
Living with PCOS
Some women struggle with the physical symptoms of PCOS, such as weight gain, hair growth, and acne.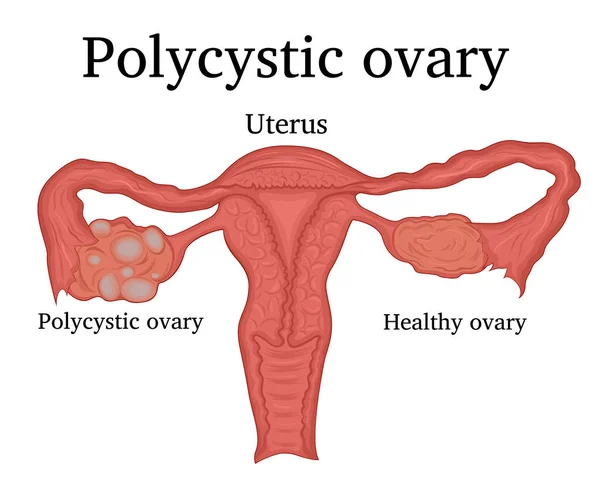 Cosmetic treatments, such as electrolysis and laser hair removal, may help you feel better about your appearance. Talk with your health care provider about the best ways to treat the symptoms that bother you.
Cosmetic treatments, such as electrolysis and laser hair removal, may help you feel better about your appearance. Talk with your health care provider about the best ways to treat the symptoms that bother you.
When should I seek medical care?
If you have missed or irregular periods, excess hair growth, acne, and weight gain, call your doctor for an evaluation.
Key points
-
PCOS is a very common hormone problem for women of childbearing age.
-
Women with PCOS may not ovulate, have high levels of androgens, and have many small cysts on the ovaries.
-
PCOS can cause missed or irregular menstrual periods, excess hair growth, acne, infertility, and weight gain.
-
Women with PCOS may be at higher risk for type 2 diabetes, high blood pressure, heart problems, and endometrial cancer.
-
The types of treatment for PCOS may depend on whether or not a woman plans to become pregnant.
 Women who plan to become pregnant in the future may take different kinds of medications.
Women who plan to become pregnant in the future may take different kinds of medications.
Next steps
Tips to help you get the most from a visit to your health care provider:
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells you.
-
At the visit, write down the names of new medicines, treatments, or tests, and any new instructions your provider gives you.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your provider if you have questions.
Polycystic ovary syndrome - symptoms, causes, features, diagnosis and treatment in medical centers "K + 31
Causes of polycystic ovary syndrome
PCOS is a dyshormonal disease that leads to the formation of a dense membrane around the ovaries that prevents the release of an egg (ovulation) . For the first time, the clinical picture of this pathology was described by Stein and Leventhal in the last century. For this reason, PCOS is also called Stein-Leventhal syndrome.
For the first time, the clinical picture of this pathology was described by Stein and Leventhal in the last century. For this reason, PCOS is also called Stein-Leventhal syndrome.
The mechanisms by which PCOS develops are not fully understood. At present, the role of hereditary factors in its occurrence has been proven. With PCOS, the conversion of male sex hormones into female sex hormones is disrupted in the ovaries. As a result, an excess of androgens appears in the blood, the maturation of follicles in the ovaries stops, many cysts form, and their albuginea thickens.
These disorders are based on increased activity of insulin during puberty, the effect of which on the ovaries is mediated through the main regulatory center - the pituitary gland and its hormones: follicle-stimulating (FSH) and luteinizing (LH).
How does polycystic ovary syndrome manifest itself?
Violation of the production of sex hormones in the ovaries leads to a decrease in estrogen levels.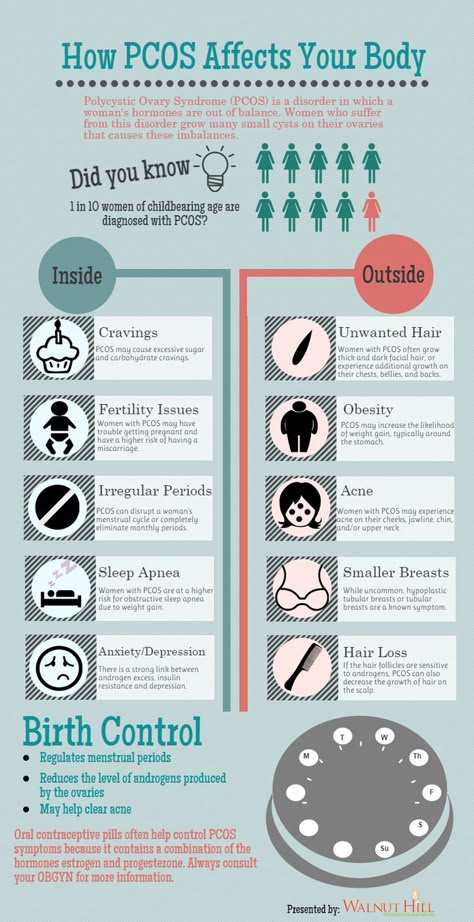 As a result, menstruation becomes rare until their complete disappearance. In some cases, on the contrary, uterine bleeding is noted due to the formed hyperplastic process of the endometrium.
As a result, menstruation becomes rare until their complete disappearance. In some cases, on the contrary, uterine bleeding is noted due to the formed hyperplastic process of the endometrium.
An excess of androgens in the body leads to the development of hirsutism (excessive growth of hair on the body and face). At the same time, there may even be baldness or hair loss with bald patches on the sides of the forehead and on the top of the head. Many women develop acne, seborrhea, the skin becomes oily. One of the main reasons for patients with PCOS to see a doctor is infertility due to the lack of ovulation.
A characteristic symptom of polycystic ovaries is male-type obesity, in which the bulk of adipose tissue is deposited in the lower abdomen and in the abdominal cavity. As a result of a rapid increase in body weight against the background of hormonal imbalance, stretch marks appear on the skin of the abdomen, hips, buttocks - striae.
Patients with PCOS often experience:
- depression,
- decreased libido,
- irritability,
- nervousness,
- aggressiveness,
- often drowsiness,
- lethargy,
- complaints about "fog in the head".
With this pathology, there is a dysfunction not only of the ovaries, but also of other organs: the hypothalamus, pituitary gland, adrenal glands, thyroid gland. Therefore, the clinical picture and the severity of manifestations are very diverse.
Absence of ovulation
Any woman may suspect the presence of polycystic ovaries. As we said, with PCOS, a dense capsule forms around the ovary, which prevents ovulation. Its absence can be registered using the basal temperature (BT) chart, which is recommended for a patient with infertility to be measured within 3-6 months. With PCOS, the BBT schedule will be monotonous without a characteristic ovulatory peak in the middle of the cycle throughout the entire observation period.
You can also detect anovulation with home tests, which are carried out starting from the 17th day before the expected period. With PCOS, all tests will be negative. The absence of ovulation according to BT and tests for several months requires further examination, first of all, ultrasound.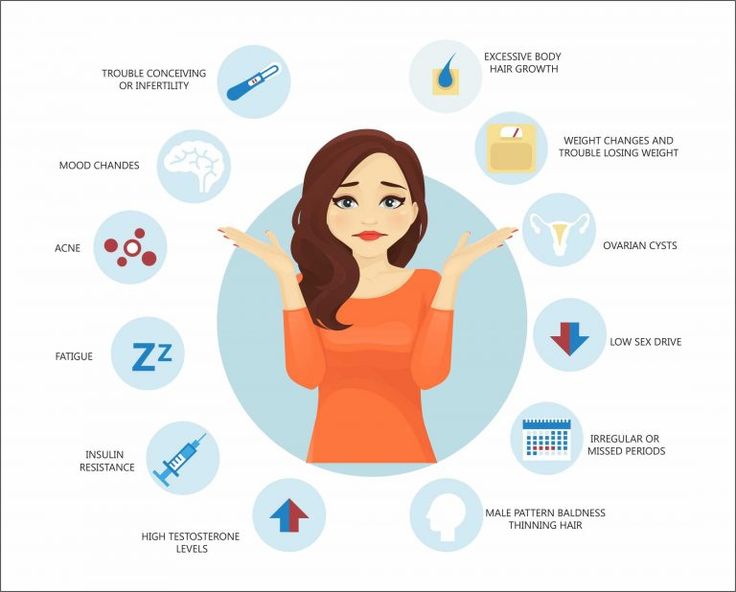
What will the ultrasound show?
Ultrasound can detect the following signs of PCOS:
- bilateral ovarian enlargement 2-3 times;
- many small cysts (more than 10) on the periphery of the ovaries, which look like a "pearl necklace", an accumulation of whitish bubbles or "fruit seeds";
- thickened to 5 mm or more capsule;
- reduction in the size of the uterus.
Ultrasound is highly informative for PCOS. However, the data of this method alone is not enough to establish a diagnosis. A laboratory study of the patient's blood is necessary.
Hormonal disorders
An important step in the examination of patients with suspected PCOS is the study of the hormonal profile, which is carried out on the 2nd-4th day of the menstrual cycle. With this pathology in the serum, there is an increase in the level of LH, testosterone, dehydroepiandrosterone (DHEA), estradiol deficiency.
Patients with PCOS also often have decreased thyroid function.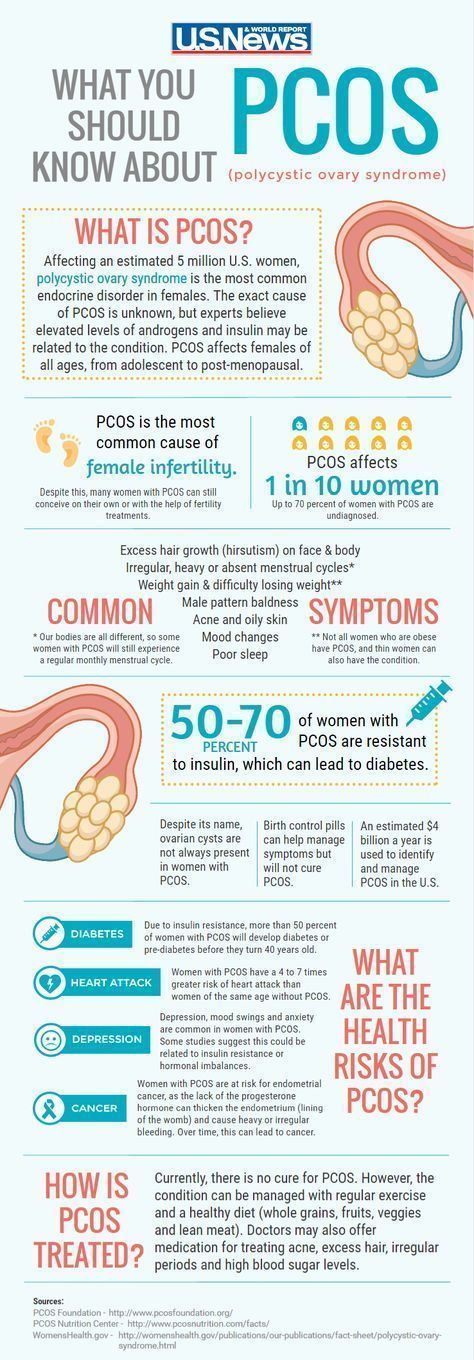 Therefore, the concentrations of thyroid-stimulating hormone (TSH), thyroxine (T4) and prolactin should be additionally assessed, which can be changed.
Therefore, the concentrations of thyroid-stimulating hormone (TSH), thyroxine (T4) and prolactin should be additionally assessed, which can be changed.
An anti-Mullerian hormone (AMH) test plays an important role in the detection of PCOS. Normally, its level is 1-2.5 ng / ml. With polycystic it increases.
How to distinguish between PCOS and adrenal pathology?
Often, PCOS has to be distinguished from adrenogenital syndrome (AGS) - a hereditary pathology of the adrenal glands, which also increases the content of male sex hormones. But with PCOS, unlike AGS, they are synthesized in the ovaries, and not in the adrenal glands.
To establish the diagnosis, tests with glucocorticoids (prednisolone, dexamethasone, cortisone) are carried out, the deficiency of which is present in adrenogenital syndrome and absent in PCOS. In the pathology of the adrenal glands, after the introduction of the missing glucocorticoid, the levels of androgens, their intermediate products and metabolites (DHEA, 17-OK, 17-OP) are normalized.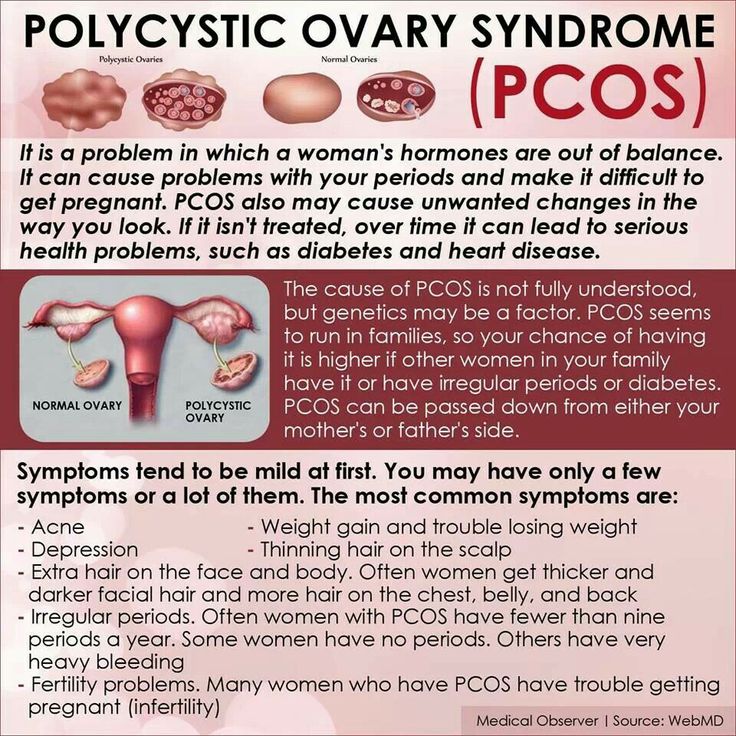 With PCOS, this effect is absent.
With PCOS, this effect is absent.
Currently, to establish the diagnosis of AGS, genotyping of the 21-hydroxylase gene (CYP21A2) mutation is performed, which makes it possible to identify the deficiency of this enzyme, which is the cause of congenital adrenal pathology.
Run diagnostics
Assessing glucose tolerance
A distinctive feature of PCOS is insulin resistance - a violation of insulin susceptibility by tissues. A similar condition occurs in type 2 diabetes.
For this reason, patients with PCOS have a glucose tolerance test.
With PCOS, there is often a change in the blood lipid spectrum with a predominance of atherogenic components: cholesterol, triglycerides, low and very low density lipoproteins (LDL and VLDL).
We normalize carbohydrate metabolism
Women with PCOS and overweight are advised to change their lifestyle and diet. It is necessary to follow a diet (eating enough pure protein, vegetables, limiting carbohydrates), doing fitness and sports.
Given the decrease in tissue sensitivity to insulin, as in type 2 diabetes, gynecologists-endocrinologists of the gynecology department of the K + 31 Clinic in PCOS prescribe metformin (MF), which increases the susceptibility of cells to insulin. Against the background of taking the drug, carbohydrate metabolism is normalized, the number of male sex hormones in the blood decreases, and ovarian function is restored.
We stimulate ovulation
An important step in the treatment of PCOS is the normalization of the menstrual cycle. For this purpose, combined oral contraceptives (COCs) are used, which include antiandrogens that block the effects of male sex hormones. Taking COCs prevents further progression of the disease. After the withdrawal of hormones, the patient ovulates and there is a chance to become pregnant.
If at the end of the COC course the ovarian function has not returned to normal, and the woman is interested in pregnancy, it is necessary to induce (stimulate) ovulation with special hormonal preparations (clostilbegyt).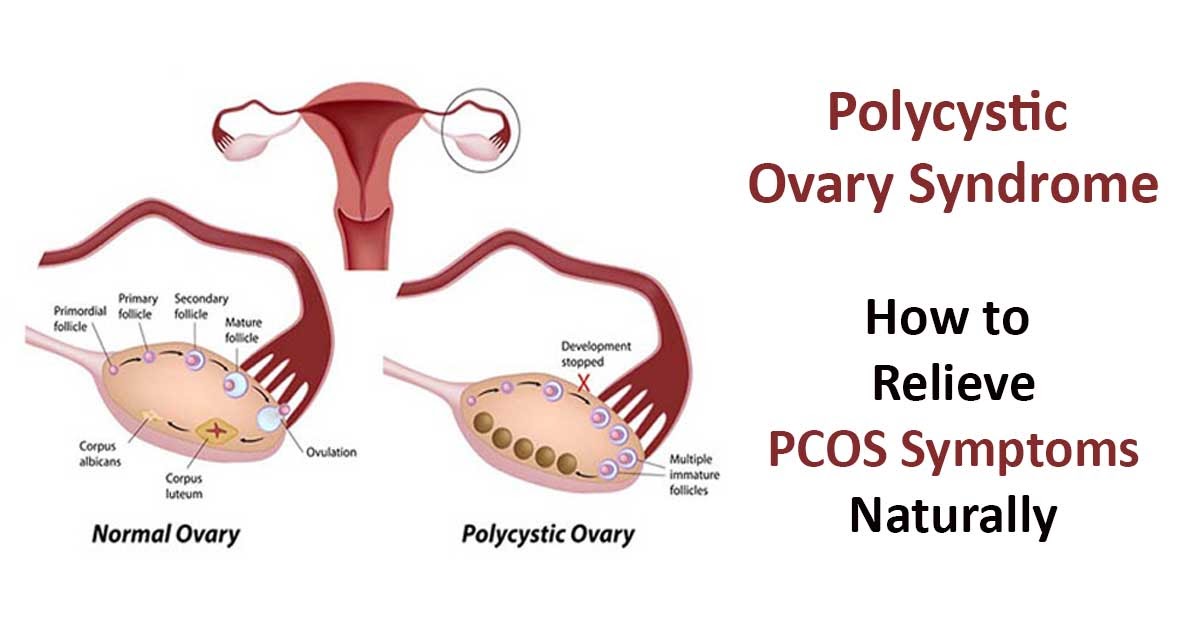 The scheme is selected by the doctor. Usually, treatment is started with a low dose and, in the absence of a result, it is increased.
The scheme is selected by the doctor. Usually, treatment is started with a low dose and, in the absence of a result, it is increased.
Also, in order to correct hyperandrogenism, cyproterone acetate (androkur) and spironolactone (veroshpiron), which have an antiandrogenic effect, are additionally used. Against the background of their intake, the greasiness of the skin decreases, acne disappears, and hair growth improves.
Surgical treatment of polycystic ovary syndrome (PCOS)
If ovulation still does not occur despite 3-6 months of hormone therapy, surgery is performed. When choosing an access, preference is given to laparoscopy. During the operation, either small incisions (wedge resection) or holes (cauterization) are made in the dense shell of the ovaries, through which the egg can leave the ovary and be fertilized. After the intervention, the menstrual cycle becomes ovulatory. This effect lasts up to a year, during which a woman can become pregnant.
Treatment of PCOS takes a long time - from 3 to 12 months. But if it is chosen correctly, the effect is good, and pregnancy occurs in most patients.
But if it is chosen correctly, the effect is good, and pregnancy occurs in most patients.
PCOS is not a tragedy, not a sentence, but just a barrier that temporarily prevents the achievement of an important goal in life. However, thanks to modern advances in medicine, you will be able to overcome this barrier. You just need to contact the leading specialists, be patient, and the meeting with the baby will take place!
* Prices are for guidance only.
Registration for service
I agree to the processing of my personal data
I am familiar with the internal regulations
User agreement for the services of JSC "K + 31"
By using the site, you consent to the use of cookies, as well as consent to the processing of personal data.
Using cookies, working with data.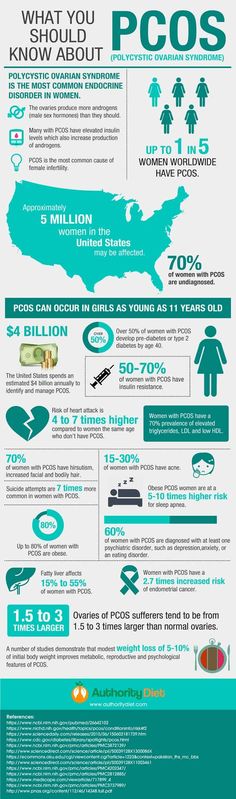
I accept
Long-term effects of polycystic ovary syndrome
AH — arterial hypertension
BP - blood pressure
GDM - gestational diabetes mellitus
CI - confidence interval
BMI - body mass index
IR - insulin resistance
HDL - high density lipoproteins
NTG - glucose tolerance
FROM - waist circumference
OGTT - oral glucose tolerance test
breast cancer - breast cancer
RE - endometrial cancer
OC - ovarian cancer
DM - diabetes mellitus
PCOS - polycystic ovary syndrome
CVD - cardiovascular disease
UGK - blood glucose level
FR - risk factor
Polycystic ovary syndrome (PCOS) is a chronic disease that is the most common endocrinological disorder in women. At a young reproductive age, the most common symptoms are menstrual irregularities, hyperandrogenism, and/or infertility. At the same time, one should not forget about the long-term consequences of PCOS: with age, metabolic disorders begin to predominate. Late reproductive age increases the risk of pregnancy complications, obesity, impaired glucose tolerance (IGT) or type 2 diabetes mellitus (DM), cardiovascular disease (CVD), and reproductive cancer (see figure) .
At the same time, one should not forget about the long-term consequences of PCOS: with age, metabolic disorders begin to predominate. Late reproductive age increases the risk of pregnancy complications, obesity, impaired glucose tolerance (IGT) or type 2 diabetes mellitus (DM), cardiovascular disease (CVD), and reproductive cancer (see figure) .
Age dynamics of PCOS.
Complications of pregnancy. Women with PCOS have a high risk of developing complications during pregnancy, such as gestational DM - GDM (relative risk - RR 2.94) and associated fetal macrosomia [1, 2]. In addition, the incidence of gestational arterial hypertension (AH) increases (preeclampsia, RR 3.67; AH in pregnant women, RR 3.47) [1]. Finally, women with PCOS have a higher risk of preterm birth (RR 1.75) and perinatal mortality (RR 3.07) [1]. Obesity, impaired glucose metabolism, and reduced uterine blood flow are thought to be the underlying causes of these complications. Since it has been proven that the use of metformin before conception or during pregnancy does not give a positive effect, its use in clinical practice before the IGT stage is not recommended [3].
Although there are no official guidelines for the management of pregnancy in women with PCOS, fasting blood glucose (FG) is indicated in the first trimester to screen for GDM. In addition, careful monitoring of blood pressure (BP) and, possibly, regular assessment of uteroplacental circulation in the second trimester are advisable (see table).
Table 1 Complications of PCOS and suggested screening tests Note. FROM - waist circumference; OGTT, oral glucose tolerance test; BMI - body mass index.
Obesity and its consequences. The incidence of overweight (BMI 25–29.9 kg/m 2 ) or obesity (BMI >30 kg/m 2 ) in women with PCOS varies from country to country. Thus, in the UK, about 90% of women with PCOS have a BMI >25 kg/m 2 , while in China - only 20%. The highest prevalence of obesity in women with PCOS is in the USA (61%) and Australia (76%) [3].
Women with PCOS are more likely to have abdominal obesity, which is associated with metabolic diseases. Abdominal obesity is directly related to insulin resistance (IR). Measurement O.T. - an informative and simple anthropometric method that allows you to identify metabolic disorders, since this indicator directly correlates with the amount of abdominal fat. In addition, women with PCOS have a more pronounced IR and a degree of obesity, which leads to a complicated course of PCOS.
Abdominal obesity is directly related to insulin resistance (IR). Measurement O.T. - an informative and simple anthropometric method that allows you to identify metabolic disorders, since this indicator directly correlates with the amount of abdominal fat. In addition, women with PCOS have a more pronounced IR and a degree of obesity, which leads to a complicated course of PCOS.
Obesity may be associated with hypertension, obstructive sleep apnea, dyslipidemia, etc. In PCOS, these associated disorders are more common and more severe due to more pronounced IR.
NTG and type 2 diabetes. IR is an important component of the SES. IGT develops in 40% of women with PCOS older than 40 years, and in 50% of them it progresses to DM within 6 years [4]. According to the results of recent meta-analyses, with an equal BMI, the presence of PCOS in women increases the risk of developing IGT and type 2 diabetes by 2.5 and 4.1 times, respectively [4].
Even with a normal BMI, women with PCOS have an increased risk of developing IGT and type 2 diabetes.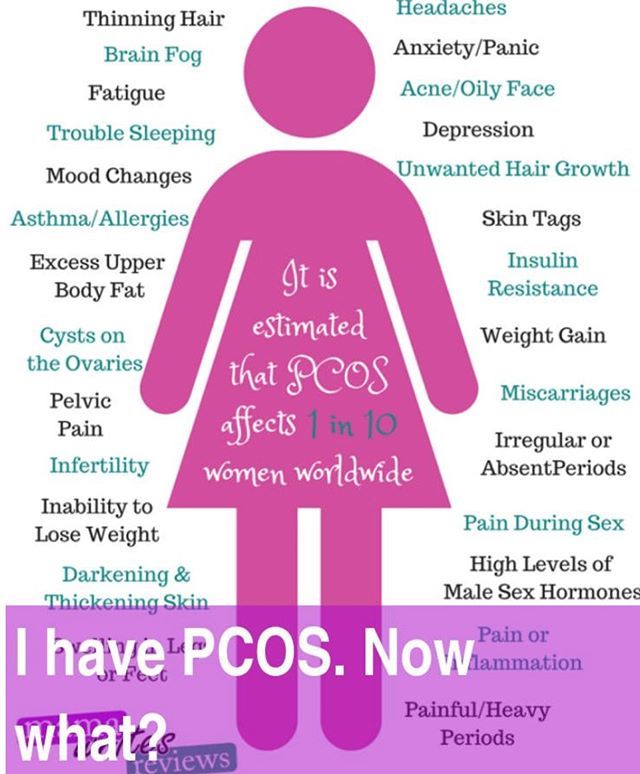 In women suffering from PCOS with hyperandrogenism and anovulation, IR develops more often and is more severe; the risk of developing IGT or type 2 diabetes is higher, the more pronounced obesity.
In women suffering from PCOS with hyperandrogenism and anovulation, IR develops more often and is more severe; the risk of developing IGT or type 2 diabetes is higher, the more pronounced obesity.
The 2012 Amsterdam Consensus (consensus document of the European Society for Human Reproduction and Embryology - ESHRE and the American Society for Reproductive Medicine - ASRM) recommends screening for carbohydrate metabolism in women with PCOS with one or more of the following risk factors (RF): BMI >30 kg/ m 2 , WC more than 88 cm, acanthosis nigricans, heredity burdened by type 2 diabetes, history of GDM [3] (see table). As a screening research method, it is recommended to use OGTT with 75 g of anhydrous glucose and the determination of UGC before and 2 hours after its administration. The Amsterdam Consensus suggests that OGTT also be performed for menstrual irregularities and hyperandrogenism, as some studies suggest a correlation between the number of PCOS symptoms and the detection of IGT or type 2 diabetes.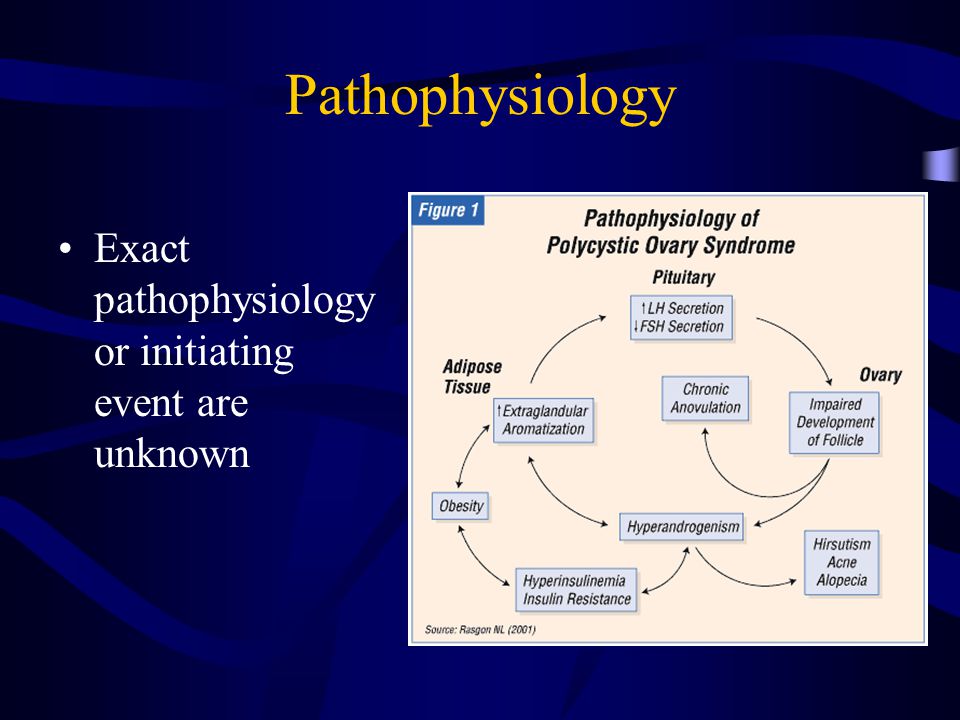
Treatment of IGT begins with recommendations for lifestyle changes. In the absence of the effect of non-drug therapy in confirmed IGT, metformin may be prescribed.
Cardiovascular complications. The results of observational studies on the study of diseases of the cardiovascular system in women with PCOS are contradictory. For example, in the review by M. Rizzo et al. [6] reviewed 5 studies that showed an increase in the risk of developing CVD in women with PCOS, but according to other 3 studies, there was no such increase in risk. It should be noted that each study used its own definition of PCOS, differed in cardiovascular outcomes and the average age of patients. Some studies have been small in size, others have included patients who are too young, in whom the risk of developing CVD is minimal, or in menopausal patients, when it is difficult to make a retrospective diagnosis of PCOS. A recent meta-analysis by R. Groot et al. [7], based on 5 cohort studies that also used different definitions of PCOS, showed an increased risk of developing CVD and cerebrovascular disease in women with PCOS compared with the control group (effect size 2 at 95% confidence interval - CI from 1.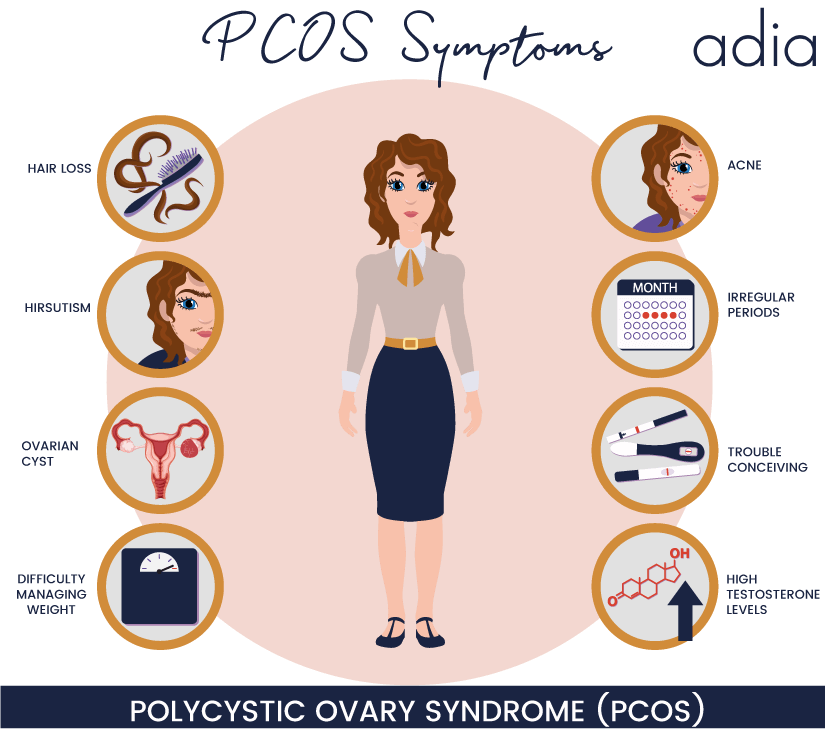 47 to 2.76). According to a large retrospective study published in 2013 by N. Mani et al. [8] with more than 2000 women with PCOS followed up for many years, there is an age-dependent increase in the risk of developing myocardial infarction and angina pectoris. Nevertheless, the overall prevalence of myocardial infarction and angina pectoris in patients of this category did not differ from the general population, which the authors of the study attribute to the young age of the patients included in the study (more than 80% under 45 years of age). Finally, according to the analysis of the largest database in the UK (21,000 women with PCOS), an increase in the incidence of CVD was not detected, although the young age of patients and the doubtful diagnosis of PCOS should also be noted [9].
47 to 2.76). According to a large retrospective study published in 2013 by N. Mani et al. [8] with more than 2000 women with PCOS followed up for many years, there is an age-dependent increase in the risk of developing myocardial infarction and angina pectoris. Nevertheless, the overall prevalence of myocardial infarction and angina pectoris in patients of this category did not differ from the general population, which the authors of the study attribute to the young age of the patients included in the study (more than 80% under 45 years of age). Finally, according to the analysis of the largest database in the UK (21,000 women with PCOS), an increase in the incidence of CVD was not detected, although the young age of patients and the doubtful diagnosis of PCOS should also be noted [9].
The incidence of cerebrovascular disease, on the contrary, is unambiguously higher in women with PCOS (RR 2.8, and BMI-adjusted RR 3.4) [10].
Although there is no evidence of increased morbidity and mortality from CVD in patients with PCOS, clinical manifestations of hyperandrogenism or a history of menstrual irregularities in postmenopausal women increase the risk of developing CVD [11, 12]. At the present stage, large prospective studies are needed to answer the question of whether the incidence of CVD in women with PCOS is increased compared to women of comparable BMI and age without PCOS.
At the present stage, large prospective studies are needed to answer the question of whether the incidence of CVD in women with PCOS is increased compared to women of comparable BMI and age without PCOS.
Subclinical vascular disease. Although there is no evidence of an increased incidence of CVD in PCOS, subclinical vascular disease is significantly more common than in women of the same age and BMI but without PCOS. Carotid intima-media thickness, arterial stiffness, and coronary calcification are major markers of vascular disease used in clinical studies. All three indicators in women with PCOS are higher than in women in the control group [13–17].
Classic risk factors for CVD development. Logically, the increased incidence of arterial disease should be associated with a higher prevalence of classic risk factors for CVD in PCOS. Indeed, hypertension, atherogenic dyslipidemia with elevated low-density lipoprotein levels, IR, type 2 diabetes, and obesity (especially abdominal) are more common in women with PCOS than those without PCOS.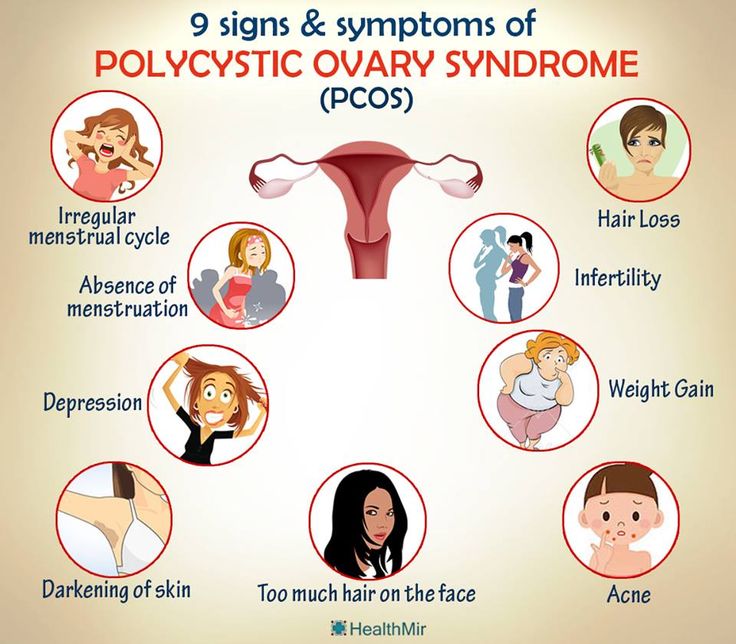 Abdominal obesity (OT greater than 80 cm) and a decrease in high-density lipoprotein (HDL) levels develop earlier than others, so appropriate screening should be performed first. Regardless of BMI, patients with PCOS are 5 times more likely to have obstructive sleep apnea/hypopnea syndrome [18].
Abdominal obesity (OT greater than 80 cm) and a decrease in high-density lipoprotein (HDL) levels develop earlier than others, so appropriate screening should be performed first. Regardless of BMI, patients with PCOS are 5 times more likely to have obstructive sleep apnea/hypopnea syndrome [18].
Some of these risk factors are included in the concept of "metabolic syndrome", which is defined as a combination of 3 of the following conditions or more: abdominal obesity, decreased HDL levels, increased triglycerides, hypertension, IGT. At the same time, the presence of any of these conditions itself increases the risk of developing cardiovascular complications [19]. The number of these risk factors increases with the number of clinical manifestations of PCOS [20].
As recommended by the 2012 Amsterdam Consensus, screening for CVD risk factors in PCOS, regardless of age, should include BP, WC, BGD, lipid profile, physical activity, nutritional status, and smoking status (see . table) [3].
table) [3].
Although there is currently no evidence of an increase in the incidence of CVD in PCOS, the high prevalence of risk factors for their development and metabolic disorders in these patients may lead to the development of CVD with age, especially in postmenopausal women.
Oncological diseases of the female reproductive system. Endometrial cancer (EC). Chronic anovulation leading to prolonged estrogen excess may cause hyperplasia and EC. A meta-analysis showed an increased risk of EC in women with PCOS (RR 2.7 vs 95% CI from 1.00 to 7.29) [21]. In a study by S. Wild et al. [10] showed an increase in the risk of developing EC in women with PCOS by 5.3 times and by 6.1 times with concomitant obesity. In most cases, these women develop a highly differentiated prognostically favorable EC.
Ultrasonography or endometrial biopsy is recommended in PCOS women with prolonged amenorrhea, depending on the clinical presentation (Amsterdam Consensus, 2012). To prevent the development of endometrial hyperplasia, withdrawal bleeding should be induced at least 4 times a year (every 3 months) [3, 22] (see table).
To prevent the development of endometrial hyperplasia, withdrawal bleeding should be induced at least 4 times a year (every 3 months) [3, 22] (see table).
Breast cancer (BC). Data on the association of breast cancer and PCOS are scarce. In a meta-analysis by V. Chittenden et al. [21], based on three PCOS studies, showed no relationship between PCOS and breast cancer risk. Therefore, the examination and observation of patients with PCOS for the diagnosis or prevention of breast cancer is not regulated in current guidelines.
Ovarian cancer (OC). So far, only one study has been performed aimed at assessing the relationship between PCOS and OC [23]. Although a lower frequency of ovulation is thought to reduce the likelihood of developing OC, this study demonstrated a 2.5-fold increase in the risk of developing OC in patients with PCOS compared with control women. At the same time, the number of women with PCOS in this study was very small. Opposite data were obtained in a study by T. Pierpoint et al. [24]: in patients with PCOS, there was a decrease in mortality from OC compared with a group of women without PCOS.
Pierpoint et al. [24]: in patients with PCOS, there was a decrease in mortality from OC compared with a group of women without PCOS.
Such limited data do not allow a definitive conclusion regarding the risk of developing OC in patients with PCOS. However, it should be remembered that in PCOS there are risk factors for the development of OC, such as no history of pregnancy, infertility and treatment for this, anovulation, and obesity. There are no guidelines for screening patients with PCOS for OC.
PCOS is a chronic disease. Obesity and impaired glucose metabolism are the most frequent companions of this syndrome. Metabolic disorders in patients with PCOS lead to a complicated course of pregnancy. There is not enough data yet to establish whether cardiovascular morbidity and mortality are increased in PCOS. The long-term studies currently presented are characterized by insufficient standardization and inconsistent diagnostic criteria for PCOS. Awareness about PCOS is extremely important as it helps to prevent its long-term complications, including metabolic disorders and EC, which can be successfully treated in the early stages.