A full term baby is born by emergency cesarean delivery
Emergency caesarean | Pregnancy Birth and Baby
Emergency caesarean | Pregnancy Birth and Baby beginning of content6-minute read
Listen
What is an emergency caesarean?
Even if you plan a vaginal birth, sometimes things don’t go as expected and you may need a caesarean. It may be the safest option if you or your baby is at risk. An emergency caesarean may need to be done very quickly, and there may not be time for you to consider all the options.
A caesarean section (C-section) is an operation to birth your baby. About 2 in every 5 caesareans are unplanned. These are known as emergency caesareans.
What are the reasons for an emergency caesarean?
An emergency C-section may be recommended if:
- there are concerns for the safety of you or your baby
- there is a life-threatening emergency for you or your baby
- your labour is not progressing normally
- there are complications, such as severe bleeding or severe pre-eclampsia
What happens if I need to have an emergency C-section?
Your doctor will explain why it is necessary to have a C-section. They will talk with you about the complications and risks.
You will be asked to complete a consent form for the operation. It is important to make an informed decision, so make sure you ask questions and discuss concerns with your doctor. Your partner or next of kin can give written permission if you can’t.
What is the difference between an emergency and a planned caesarean?
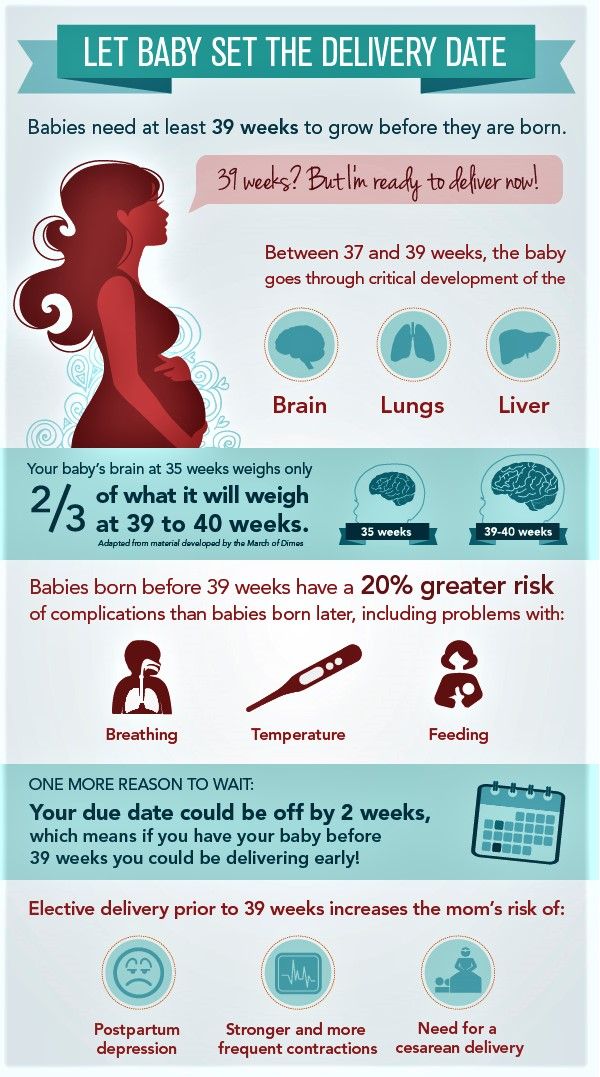
A C-section might be planned in advance (elective) if there is a reason that prevents your baby being born by a vaginal birth. The birth will usually happen before you go into labour.
Unplanned (emergency) caesareans can happen when there are problems either with your health or your baby’s health in your pregnancy or during your labour. An emergency caesarean may need to be done very quickly
How quickly will the caesarean be performed?
Your doctor has guidelines to identify how quickly your baby should be born by emergency C-section. It depends on the reasons for the operation.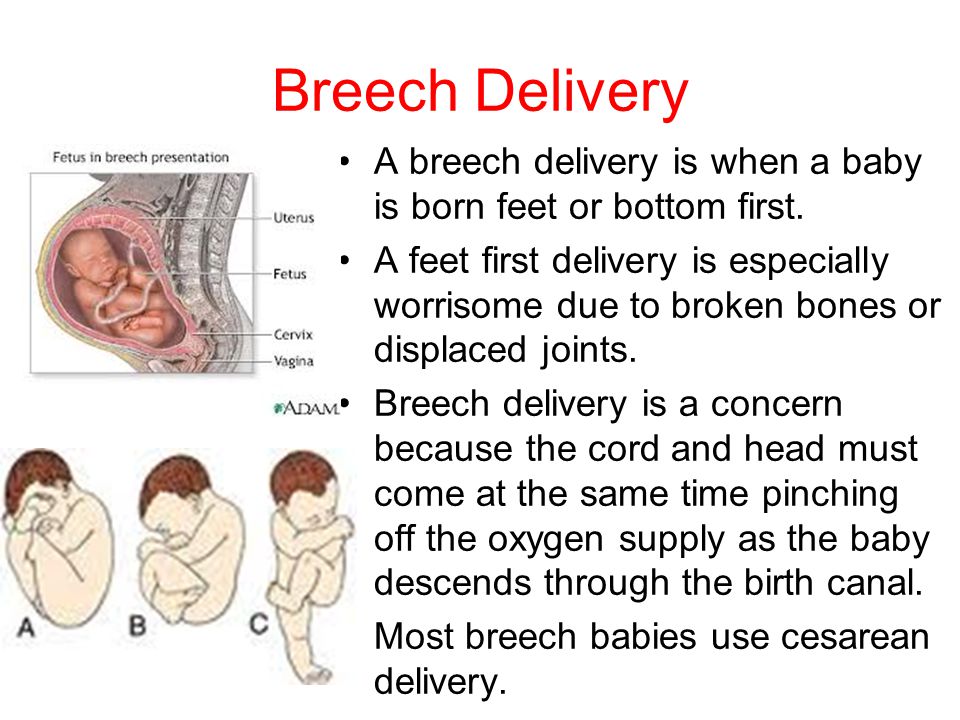
There are four categories that describe the urgency for caesarean section:
- Category 1 — immediate threat to the life of the mother or baby.
- Category 2 — there are problems affecting the health of the mother and/or baby but they are not immediately life threatening.
- Category 3 — the baby needs to be born early but there is no immediate risk to mother or baby.
- Category 4 — the operation will take place at a time that suits the woman and the caesarean section team.
If several women need caesareans at the same time, they will be prioritised according to the level of risk. This means you may have to wait a while, even if you have been told it is an emergency.
Most emergency caesarean births are Category 2 and are mostly done about an hour after the decision is made. Life threatening Category 1 caesareans aim to be done within 30 minutes.
What happens during an emergency caesarean?
Caesarean surgery usually takes 30-60 minutes, although it might be several hours before you’re back in the maternity ward with your baby.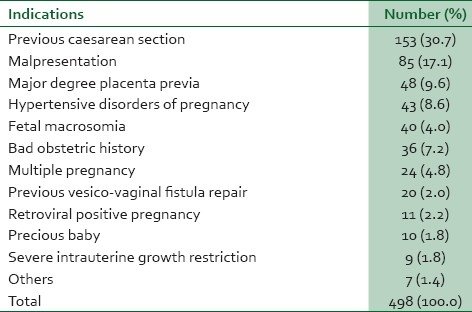
In an emergency, there might not be time to give you epidural or spinal block. You may need a general anaesthetic, although this is rare. When you wake up you may feel dizzy, nauseous, and you may have a sore throat.
In most cases your partner or support person can be with you. You will also usually have a midwife that stays with you. They will look after you and your baby in the theatre and recovery area.
Emotional support after an emergency caesarean
Some women feel happy after having a caesarean birth, but others can feel a range of overwhelming emotions, particularly if it was unexpected. Very urgent caesareans (Category 1) happen very quickly and can be a traumatic experience for parents and support people.
- talk to a midwife immediately after the birth about your experience
- talk to your doctor, midwife or maternal child health nurse at any time, about how you feel
- ask for practical and emotional support from friends and family
If the birth was very traumatic, it is possible to develop post-traumatic stress disorder (PTSD). or postnatal depression.
or postnatal depression.
If you have negative feelings about your birth, it’s important to seek help as early as possible. You doctor will be able to guide you to the appropriate support. If needed, therapy or medicines can be used as treatment.
You can also call:
- Pregnancy, Birth and Baby on 1800 882 436 to speak to a maternal child health nurse
- Lifeline on 13 11 14
- beyondblue on 1300 22 4636
- PANDA on 1300 726 306
Support is also available for partners and support people.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
The Royal Women's Hospital (Caesarean birth), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Categorisation of Urgency for Caesarean Section), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Caesarean section)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2022
Back To Top
Related pages
- Planned or elective caesarean
- Recovery after a caesarean
- Vaginal birth after caesarean (VBAC)
Need more information?
Vaginal birth after caesarean (VBAC)
If you've delivered a baby by caesarean (C-section), you may have a choice with your next pregnancy - a vaginal birth after caesarean (VBAC) or a planned (elective) caesarean.
Read more on Pregnancy, Birth & Baby website
Vaginal Birth after Caesarean Section
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Having a caesarean
A caesarean is an operation to deliver a baby through a cut in the abdomen (tummy) and uterus (womb). It might be planned (elective) or an emergency procedure.
It might be planned (elective) or an emergency procedure.
Read more on Pregnancy, Birth & Baby website
Recovery after a caesarean
Recovery after a caesarean section - whether it's an emergency or planned - will take several weeks. Find out what to expect after you have had your baby.
Read more on Pregnancy, Birth & Baby website
Caesarean section - Better Health Channel
A caesarean section is usually performed when it is safer for the mother or the baby than a vaginal birth.
Read more on Better Health Channel website
Caesarean Section
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Elective caesarean birth: what to expect | Raising Children Network
Having a planned or elective caesarean birth? As with any major surgery, it helps to know what to expect during a caesarean section.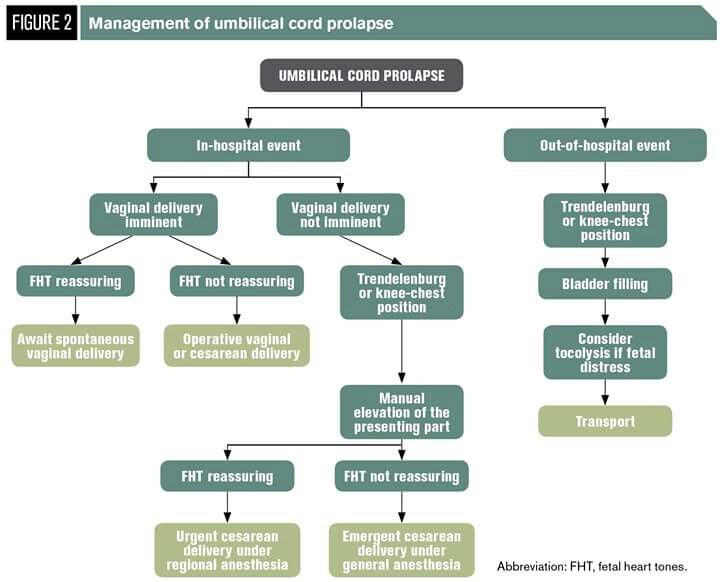 Our guide explains.
Our guide explains.
Read more on raisingchildren.net.au website
Planned or elective caesarean
There are important things to consider if you are having a planned, or elective, caesarean.
Read more on Pregnancy, Birth & Baby website
VBAC: vaginal birth after caesarean | Raising Children Network
For many women, vaginal birth after caesarean – VBAC – is a safe and positive way to have a baby. Our guide explains VBAC’s possible benefits and risks.
Read more on raisingchildren.net.au website
Caesarean Section - Birth Trauma
Being abdominal surgery, pain in the early months is very common after a caesarean section (C-section) and needs to be managed with rest, pain relief, and
Read more on Australasian Birth Trauma Association website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Why They're Needed and What to Expect
Congratulations, you’re expecting! This exciting time includes a lot of changes for you, as well as planning for the arrival of your baby and the not-so-distant future. It can also mean lots of anxiety and trying to make your birth plan just right.
Sometimes we plan, and the universe gently smiles.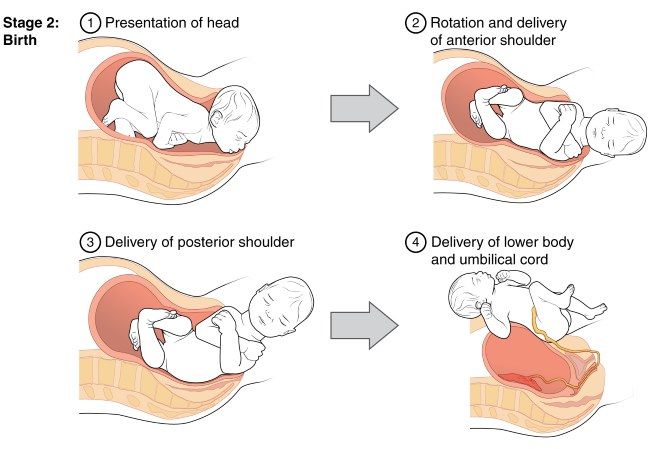 For many reasons, your birth plan may change — sometimes in regards to its smaller details, and other times in regards to its bigger ones, including how you want to give birth.
For many reasons, your birth plan may change — sometimes in regards to its smaller details, and other times in regards to its bigger ones, including how you want to give birth.
Whether your plans are for a vaginal birth or scheduled cesarean delivery (also called a C-section), both of these options will be off the table if you need an emergency C-section.
Don’t worry. You and your baby are in expert hands. Although almost 32 percent of births in the United States occur by C-section, you’re less likely to need an emergency C-section, which only happens when it’s the safest option for you and your baby.
An emergency C-section is one that happens very quickly due to immediate concern for the health of the mother and/or baby. The goal is that no more than 30 minutes pass between the decision to perform an emergency C-section and delivery, but it can take up to 75 minutes.
Any kind of C-section is a major surgery that requires a room full of healthcare professionals and a great deal of organizing. This means that when a patient needs an emergency C-section, a lot of doctors and nurses have to get ready faster than normal.
This means that when a patient needs an emergency C-section, a lot of doctors and nurses have to get ready faster than normal.
You can end up having an emergency C-section even if you already had a scheduled, planned, or even unplanned C-section in the works. All of these are sometimes called medical C-sections, as they happen for health reasons. In comparison, an elective C-section is one that you choose to have.
What’s the difference between the types of C-sections?
- Scheduled C-section. This is when you and your doctor decide that it’s safest for you and your baby to deliver via C-section, potentially because you’ve had a C-section before. Your doctor will schedule a C-section date around your estimated delivery date, possibly months in advance.
- Unplanned C-section. This is when you were planning to have a vaginal birth, but a little while before your delivery your doctor decides that a C-section is best for you and your baby.
 This decision can be made a few weeks, days, or even hours before you’re about to give birth. With an unplanned C-section, there’s no emergency, but the change in plans is made to get you and baby onto the safest birth route.
This decision can be made a few weeks, days, or even hours before you’re about to give birth. With an unplanned C-section, there’s no emergency, but the change in plans is made to get you and baby onto the safest birth route.
- Emergency C-section. This happens when delivery must occur urgently to make sure both you and baby are safe. This can happen whether you’re planning to have a vaginal birth or a C-section.
They might seem like the same thing, but not all C-section experiences are created equal. Your experience, as well as the actual procedure for an emergency C-section, will be different than those of a scheduled or unplanned C-section.
What will happen during an emergency C-section?
One main difference is how you might be prepared for it. Everything must move quickly, including administering pain medications and getting the baby delivered.
Most scheduled C-sections are performed with local or regional numbing (anesthesia).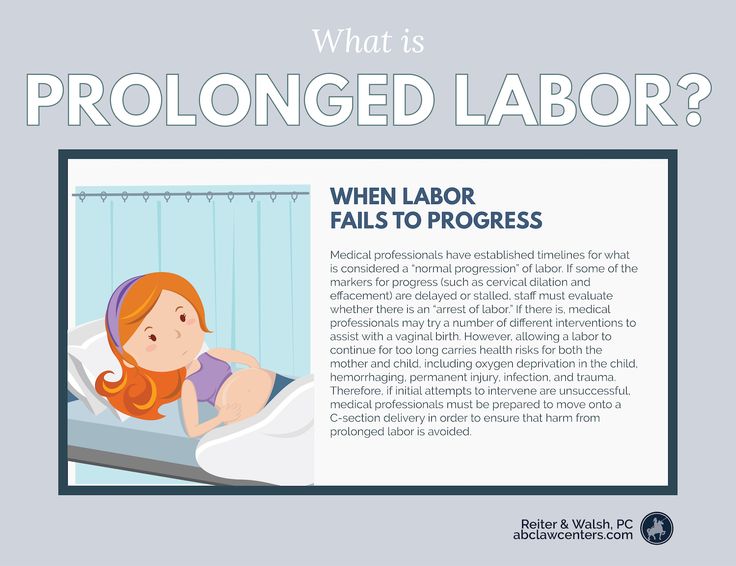 This means you’ll still be awake, but you won’t feel pain during the procedure. Local anesthesia is usually administered via a spinal injection, and this can take time.
This means you’ll still be awake, but you won’t feel pain during the procedure. Local anesthesia is usually administered via a spinal injection, and this can take time.
In an emergency C-section, the timing and details of your situation, along with hospital policies, can affect your options for anesthesia.
Your doctor and the anesthesiologist may decide that there’s time to administer a spinal injection. Or, you may already have an epidural in place, which helps with the surgery preparations. However, depending on multiple factors, some of these options may not be possible.
Alternatively, you may have general anesthesia, using both injected and inhaled drugs to make sure you’re pain-free during the surgery. This will allow the C-section to happen more quickly, but this combination means you’re not able to be awake during the procedure.
Another difference may be the incision used during the surgery. In non-emergency C-sections, a horizontal (bikini) cut is typically performed. If you’re at term, you’ll likely have this type of incision, even in an emergency.
If you’re at term, you’ll likely have this type of incision, even in an emergency.
However, during an emergency surgery in which your baby’s health needs immediate attention, the surgeon may opt to use a vertical incision on your uterus to get to your baby faster. This type of incision may be necessary in cases of preterm birth, as well as due to adhesions from previous surgeries or fibroids that may be in the way of the uterus.
Again, this is dependent on the circumstances of your birth. Your surgeon’s training, as well as your and your baby’s health needs, are taken into consideration.
The reasons you might need an emergency C-section are also different than the reasons you might have a scheduled C-section.
Basically, an emergency C-section means that your baby isn’t cooperating with the planned exit or decides they want to come out before a scheduled or unplanned C-section. It may also mean that your health is a concern and waiting for progress isn’t the right choice.
In most cases, there’s nothing you or your doctor can do to change the need for an emergency C-section.
The following are several reasons why this might happen:
Very long labor
Prolonged or delayed labor is when labor goes on for much longer than normal. This can sometimes cause health problems for both baby and mom. Prolonged labor is the most common reason for an emergency C-section. About 8 percent of pregnant women who are about to give birth have a prolonged labor.
When this happens, your doctor may decide that it’s much healthier for you and your baby to have an emergency C-section than to try to deliver vaginally. You might have a prolonged labor because:
- Your labor didn’t really start. Sometimes you’ve had contractions for ages, but they don’t seem to be doing anything. Plus, you may not be dilating as you should.
- Your labor stalls. Everything might be on track as you start having contractions and even begin dilating, but then everything stops.
 Sometimes this happens because your baby’s head cannot fit through your pelvis.
Sometimes this happens because your baby’s head cannot fit through your pelvis.
Baby’s position
Your baby’s position might have already been a concern when your labor began, or an external cephalic version might have seemed successful, only to have baby return to a breech position at the last minute. Whatever the circumstances, labor may not progress as expected if your little one can’t be coaxed into turning around into a cooperative position.
If your baby is positioned with their behind first (breech), feet first, or stretched out sideways straight across your stomach (transverse), a vaginal delivery may not be possible. Your doctor may try to coax baby into position by turning your baby under controlled conditions, but this doesn’t always work.
Exhaustion
Sometimes all the pushing and trying in the world doesn’t seem like enough. Your doctor may have pulled out all the stops, even trying a vacuum-assisted delivery, to no avail.
At this stage you’ve likely been pushing for ages and are too exhausted to push any more. Your health may begin to show signs of distress, suggesting continued pushing is not an option.
Your health may begin to show signs of distress, suggesting continued pushing is not an option.
At the same time, the fetal monitor might show that your baby’s heart is beating too fast or too slow. Your doctor may decide that it’s no longer safe for you and your baby to keep this up.
Health condition
If mama has a health condition or infection that comes up during labor, an emergency C-section might be recommended. For example, a herpes infection or other infection in the vaginal area can suddenly become active and harm the baby.
Alternatively, if your blood pressure or heart rate gets too high, it may not be a good idea to keep pushing. Also, if you have any kind of sudden heart or brain health issue, you may need an emergency C-section.
Tangled umbilical cord
If the umbilical cord gets compressed, tangled, or tries to come out before your baby, you’ll likely need an emergency C-section.
A prolapsed umbilical cord is a very rare complication that happens when the cord slides into the birth canal ahead of your baby.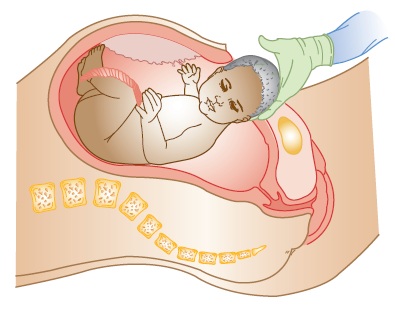 When this happens there’s a risk that it’ll be squeezed too much while your baby is trying to make their grand entrance. This can cut off baby’s blood supply.
When this happens there’s a risk that it’ll be squeezed too much while your baby is trying to make their grand entrance. This can cut off baby’s blood supply.
Similarly, your baby might not be getting enough oxygen if the umbilical cord gets kinked or tangled like a garden hose.
Placental problems
Like the umbilical cord, the placenta can also complicate delivery.
Part or all of the placenta can come away from the lining of the womb. This is called placental abruption. When this happens your baby can’t get the necessary nutrients and oxygen inside the womb, and you may need an emergency C-section.
Womb tear
In very rare cases, the increased pressure on your body during birth can tear or rupture the womb. Having had a prior C-section increases your risk. If you have a womb or uterus tear (uterine rupture), you’ll need an emergency C-section.
Most of the risks of an emergency C-section are similar to those of any type of C-section.
Risks to your health include:
- an infection inside the womb or at the opening site
- opening or splitting stitches
- injury to the organs, nerves, or blood vessels near the uterus
- blood loss during the surgery
- heavy bleeding afterward
- blood clots
- a reaction to the anesthesia
- not being able to deliver vaginally in the future
Risks to your baby’s health include:
- accidental injury during the C-section
- temporary breathing problems for a few days after birth
There are also some risks to consider after the delivery is over.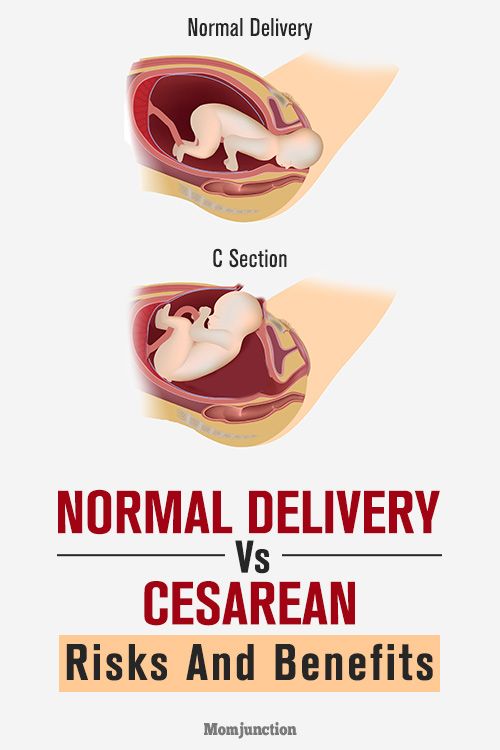
If you’re asleep for the emergency C-section, you’ll likely not be able to have skin-to-skin contact with your baby right after birth. Also, the effects of the medications you were administered might make breastfeeding challenging for a while.
This does not mean that breastfeeding or bonding is impossible. You can begin a solid and satisfying breastfeeding relationship after an emergency delivery. Know that support is available, and you can work with a lactation consultant and your provider to meet your goals.
You may also be at higher risk of post-traumatic stress and its related effects. It’s important to spend time caring for yourself and your mental health. Discuss any issues or concerns you have with your provider or a mental health professional.
Like other major surgeries, you’ll need time to rest and recover after any kind of C-section. This could mean bed rest and not being able to climb stairs or lift anything heavy for a while.
It’s important to avoid putting too much pressure on the incision site to help it heal well. You might not be able to pick up or hold your baby for too long if you’re sore. You’ll need to change the bandages and see your doctor for follow-up visits to make sure the area is not infected.
You might not be able to pick up or hold your baby for too long if you’re sore. You’ll need to change the bandages and see your doctor for follow-up visits to make sure the area is not infected.
You’ll also likely need a dose of antibiotics to prevent infection. And if you need pain meds to stay comfortable, you may not be able to breastfeed your little one until you stop taking them. Ask your doctor about when it’s safe to breastfeed.
Also, unlike other C-sections and most surgeries, your doctor decided to do an emergency C-section at the eleventh hour. This means you may not have felt emotionally or mentally prepared for it.
Again, an emergency C-section may lead to post-traumatic stress disorder (PTSD). Talk to your doctor if you’re having difficulty dealing with your birth experience or feel you may have postpartum depression.
You might need an emergency C-section if your doctor decides that it’s the best option for you to deliver a healthy baby, and the need may arise due to a number of reasons.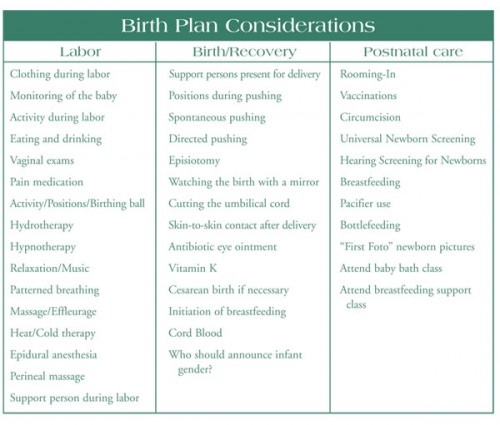
Neither you nor your doctor can control this outcome. While a C-section might be a major detour from your birth plan, the important thing is that you and your baby remain healthy and safe.
Caesarean section or vaginal delivery for preterm birth in women with singleton pregnancies
There is not enough evidence to show the effects of a policy of planned immediate caesarean section, or a policy of planned vaginal birth in preterm births (preterm births).
A caesarean section is an operation performed to remove the baby through an incision in the abdomen and uterus. Elective caesarean section in women who are assessed as being in preterm labor may have a protective effect on the baby and may also prevent emergency labor with associated complications. However, it can also be traumatic for both the mother and her baby. More often than not, women who are assessed as being in preterm labor will give birth a few weeks later, most often at term. Therefore, there is a real possibility that a policy of elective caesarean section may increase the number of infants who are removed prematurely.
We included six randomized trials (involving 122 pregnant women) but only four studies (involving 116 women) were included in the analyses. Our review found that there is not enough conclusive evidence to compare elective caesarean section with elective vaginal delivery. Sometimes an elective caesarean cannot be performed because labor progresses too quickly, and sometimes, even when a vaginal birth is planned, complications that develop during labor may necessitate a caesarean section. The results of the review showed that an insufficient number of women were included in these trials and therefore the decision on how best to deliver a premature baby, whether in cephalic or breech presentation, remains based on the opinion and accepted practice in each hospital, and not on scientific evidence.
All four trials were terminated early due to difficulties in enrolling women in the studies. There were no reports of serious maternal complications, including transfer to the intensive care unit. However, seven cases of severe maternal postpartum complications (gaping wound, deep vein thrombosis, endotoxic shock, and puerperal sepsis) were reported in the elective caesarean section group, and there were no complications in the group of women randomized to elective vaginal delivery. There was no clear difference between the two groups in the number of cases of excessive blood loss from the birth canal after childbirth (postpartum hemorrhage), as well as in the number of birth asphyxia or respiratory distress syndrome, or childbirth injuries.
However, seven cases of severe maternal postpartum complications (gaping wound, deep vein thrombosis, endotoxic shock, and puerperal sepsis) were reported in the elective caesarean section group, and there were no complications in the group of women randomized to elective vaginal delivery. There was no clear difference between the two groups in the number of cases of excessive blood loss from the birth canal after childbirth (postpartum hemorrhage), as well as in the number of birth asphyxia or respiratory distress syndrome, or childbirth injuries.
Translation notes:
Translation: Li Yun. Editing: Ziganshina Lilia Evgenievna. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center on the basis of Kazan Federal University). For questions related to this translation, please contact us at: [email protected]; [email protected]
Caesarean section in preterm pregnancy
The search for adequate methods of delivery in preterm pregnancy is of great relevance. Only 25% of pregnant women in terms of 28-37 weeks of gestation are delivered through the natural birth canal. These are, as a rule, premature births, uncomplicated by serious extragenital or obstetric pathology. In 75% of cases, pregnancy within the indicated time frame ends with an emergency or planned caesarean section [1].
Only 25% of pregnant women in terms of 28-37 weeks of gestation are delivered through the natural birth canal. These are, as a rule, premature births, uncomplicated by serious extragenital or obstetric pathology. In 75% of cases, pregnancy within the indicated time frame ends with an emergency or planned caesarean section [1].
The most serious consequence of childbirth for a premature baby is birth trauma, which occurs 7 times more often in premature births than in timely ones.
Material and research methods
We analyzed 260 cases of caesarean section in preterm pregnancy, performed in the clinical maternity hospital No. 1 of Kazan. Of these, 12 (4.6%) operations were performed at 22-27 weeks of gestation, 86 (33.08%) operations - at 28-33 weeks, 162 (62.31%) operations - at 34-37 weeks.
In the structure of indications for abdominal delivery, those from the mother's side prevailed (about 60%). The most frequent of them were bleeding and preeclampsia.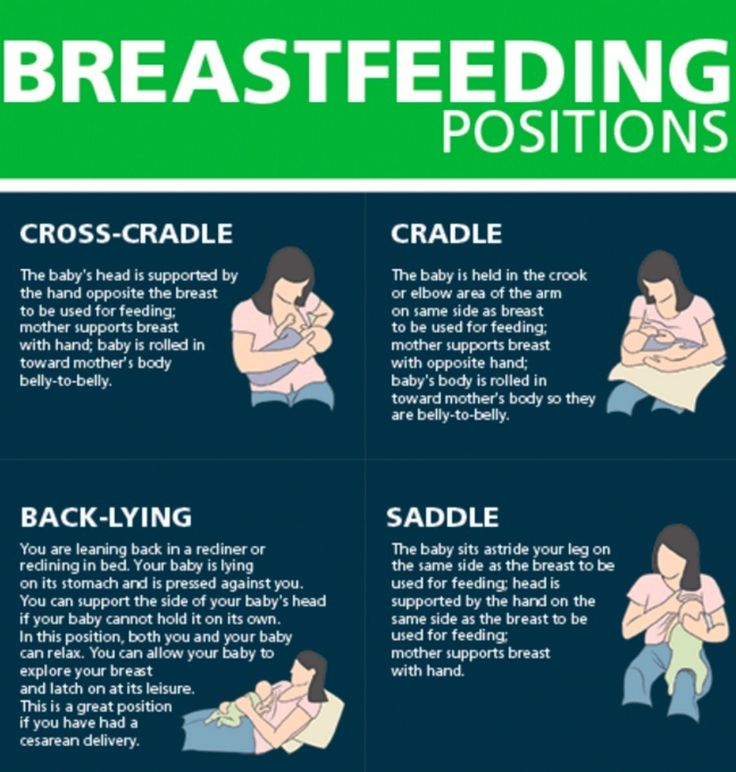 In second place were indications from the fetus (about 40%), the common reason for which was the reduction of birth trauma for an immature and underweight child. In 71.2%, these were emergency operations and only in 28.8% of cases - planned ones. The outcomes of abdominal delivery were better if it was planned. Survival of premature babies after caesarean section was also determined by the body weight of newborns and the timeliness of the operation.
In second place were indications from the fetus (about 40%), the common reason for which was the reduction of birth trauma for an immature and underweight child. In 71.2%, these were emergency operations and only in 28.8% of cases - planned ones. The outcomes of abdominal delivery were better if it was planned. Survival of premature babies after caesarean section was also determined by the body weight of newborns and the timeliness of the operation.
Although caesarean section has advantages over spontaneous delivery in a number of clinical situations, it does not solve the problem of preventing birth injuries in preterm pregnancy. By reducing mortality, operative delivery has little effect on the incidence of low birth weight children [3]. Improving the technique of caesarean section in preterm pregnancy is of great relevance.
In 1988, H. Hillemans proposed a caesarean section technique, which involves the extraction of the fetus in whole membranes [cit. by 2]. In Russia, this operation has found application in some obstetric clinics for preterm birth.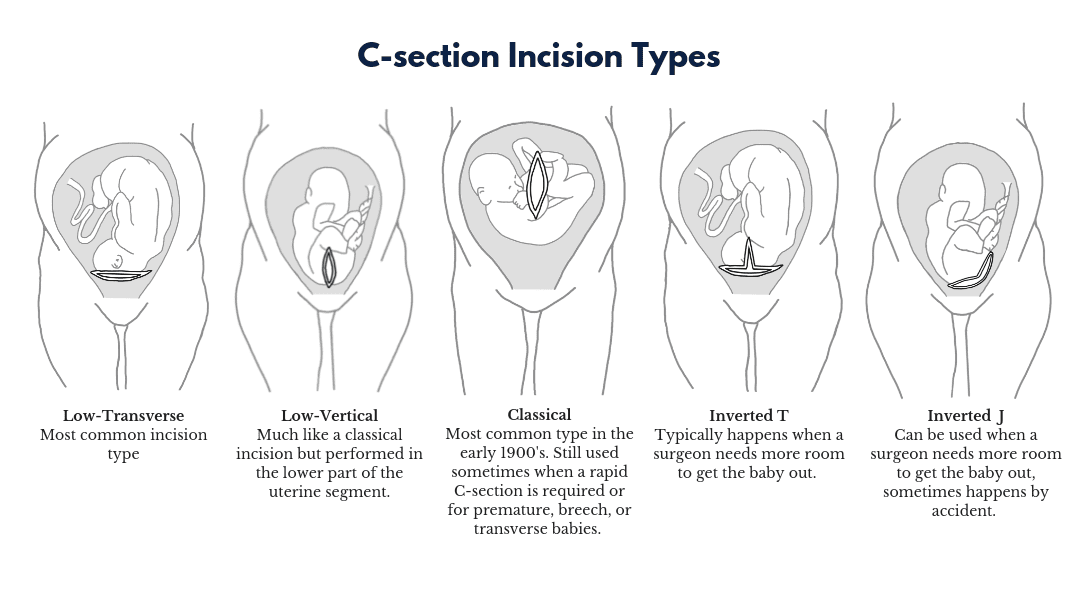 We have proposed an original method of caesarean section with the extraction of the fetus in the whole amniotic sac, and also conducted a comparative study of the effectiveness of this technique, taking into account the outcomes of delivery for a child with low body weight.
We have proposed an original method of caesarean section with the extraction of the fetus in the whole amniotic sac, and also conducted a comparative study of the effectiveness of this technique, taking into account the outcomes of delivery for a child with low body weight.
The operation technique consists in maintaining the integrity of the fetal bladder when making an incision on the uterus and creating a kind of "hydraulic protection" when removing the child. After laparotomy (according to Joel-Kohen or Pfannenstiel), the incision on the uterus is made with a scalpel to the fetal membranes without damaging them, then continues with scissors in an arcuate transverse direction under the control of two fingers inserted between the wall of the uterus and the membranes, to a length sufficient to extract the fetus. In very early preterm labor (22-27 weeks) and an unformed lower segment, a longitudinal isthmic-corporal incision of the uterus is justified. The subsequent stages of the operation consist in carefully exfoliating the fetal bladder from the walls of the uterus by hand, removing the fetal head from the uterine cavity using gentle and smooth pressure through the anterior abdominal wall to the bottom of the uterus, extracting the fetus in the whole fetal bladder to the shoulder girdle or in its entirety, opening the membranes and crossing umbilical cord (Fig. 1, 2). Figure 1. Exfoliation of the amniotic sac from the walls of the uterus. Figure 2. Extraction of the fetus in the whole amniotic sac.
1, 2). Figure 1. Exfoliation of the amniotic sac from the walls of the uterus. Figure 2. Extraction of the fetus in the whole amniotic sac.
In total, 80 newborns born at 28-37 weeks of gestation were examined, of which 40 children were removed in the fetal bladder (main group), 40 were born by traditional caesarean section (comparison group). The study was conducted using the copy-pair method. The selection of copies was carried out according to the main diagnosis, gestational age, body weight of the newborn. Prevention of the syndrome of respiratory disorders and endotracheal administration of surfactant were taken into account. The following inclusion criteria were used in the study: gestational age 28-36 weeks, fetal weight from 1000 to 2500 g, whole amniotic sac, cephalic presentation. Exclusion criteria: first or second stage of labor, severe fetal hypoxia, polyhydramnios, complete placenta previa, total placental abruption.
Research results and discussion
In the main group, 8 (20%) newborns were born at 28-30 weeks, 22 (55%) - at 31-33 weeks, 10 (25%) - at 34-37 weeks, in the comparison group, respectively, 9 (22, 5%), 21 (52. 5%) and 10 (25%) children.
5%) and 10 (25%) children.
In the whole fetal bladder with a birth weight of 1000-1499 g, 19 newborns were removed, with a body weight of 1500-2500 g - 21 infants. There were no newborns weighing 500-999 g in any group.
Indications for caesarean section in the groups did not differ significantly: gestosis (in 22 women in the main group and 22 in the comparison group), partial premature detachment of a normally located placenta (in 10 and 10 women), failure of the uterine scar (in 4 and 4), premature rupture of amniotic fluid (in 4 and 4), high myopia in preterm birth and intrauterine growth retardation of the fetus II degree (in 1 and 1 women, respectively).
Assessment of the state of the newborn at birth was carried out according to the Silverman and Apgar scales, the neurological status was determined. Of the special research methods, neurosonography using an Aloka SSD 1400 sonograph, Dopplerography with an assessment of cerebral blood flow, and fundus examination were used. The incidence of children in the first year of life was studied.
The incidence of children in the first year of life was studied.
According to the neurological examination, all premature infants had manifestations of perinatal lesions of the central nervous system, however, the degree of their severity in the main group and the comparison group was different. Newborns of the main group did not have such severe clinical disorders as bilateral pyramidal insufficiency, rubral tremor.
According to special research methods, intraperiventricular hemorrhages (IPVC) were diagnosed in 10 (25%) newborns of the main group and 32 (80%) of the comparison group (p<0.05). III degree PVVC were not detected in the main group, in the comparison group they were diagnosed in one (2.5%) newborn, degree II PVVC was found in 8 (20%) and 24 (60%) children, respectively, degree I PVVC - in one (2.5%) and 3 (7.5%) newborns, respectively (p<0.05) (Fig. 3).
Signs of cerebral ischemia were detected in 26 (65%) newborns of the main group and in 30 (75%) in the comparison group (p<0. 05). Cerebral ischemia of I degree was diagnosed in 10 and 6 children, II degree - in 16 and 20 newborns, respectively. In children of the main group III, the degree of ischemia was not observed; in the comparison group, it was diagnosed in 10 newborns.
05). Cerebral ischemia of I degree was diagnosed in 10 and 6 children, II degree - in 16 and 20 newborns, respectively. In children of the main group III, the degree of ischemia was not observed; in the comparison group, it was diagnosed in 10 newborns.
There were no traumatic intracranial lesions of the nervous system in children born by caesarean section.
The duration of respiratory support in the main group averaged 5.56±3.44 days, in the comparison group - 8.59±3.92 days (p<0.05). The length of stay of newborns both at the first and second stages of nursing was also significantly less in children of the main group and amounted to 8.30±4.48 days at the first stage of nursing, and 21.30±12.3 days at the second stage. In the comparison group, the duration of the first stage was 12.8±5.07 days, the second stage - 30±12.7 days (p<0.05).
These data indicate a difference in the neurological status of newborns in both groups, which was manifested in a decrease in the number and severity of PVVC, a decrease in the severity of cerebral ischemia and perinatal lesions of the central nervous system.
The results of the analysis of infant morbidity are indicative. Children in the comparison group had a significantly higher level of morbidity compared to that in the main group (Fig. 4). Despite some positive dynamics, these differences persisted by the end of the first year of life.
Thus, caesarean section with fetal retrieval in the whole amniotic sac provides more favorable immediate and long-term results for the health and development of children. With low and very low body weight of the fetus, as a rule, there are no difficulties in extracting it in the fetal bladder, while the obstetrician's hand does not come into direct contact with the fetal head. Her birth takes place under conditions of "hydraulic protection" by amniotic fluid. With a very low weight of the fetus, it "rolls out" or floats out along with the amniotic fluid. The moment of traction is excluded, which is fraught with excessive load on the spine of a premature baby. The advantages of this technique of caesarean section should also include the minimized risk of damage to the fetus with a scalpel.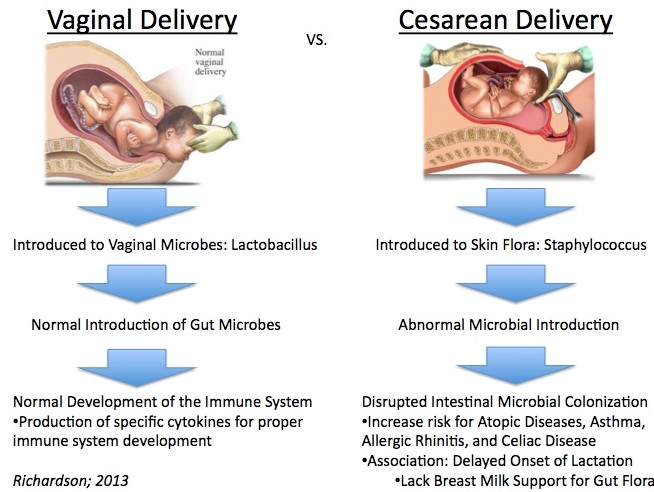 This complication of caesarean section occurs in 2% of cases [4].
This complication of caesarean section occurs in 2% of cases [4].
Experience has shown that the retrieval time for this operation is slightly longer than for the traditional technique. This is due to the peculiarities of dissection of the uterine wall to the membranes, exfoliation of the fetal bladder from the walls of the uterus. At the same time, under conditions of regional anesthesia, this did not significantly affect the condition of the mother and child.
Obviously, caesarean section does not eliminate the influence of factors that are associated with the immaturity of a premature baby, and does not solve the fundamental problem of safe delivery in preterm pregnancy. Pulmonary atelectasis, pulmonary distress, respiratory disorders and hypoxia, and other conditions characteristic of prematurity largely determine the condition of the child and the need for therapeutic measures. The main thing remains for the whole complex of preventive, therapeutic, surgical, resuscitation and rehabilitation measures, including the proper management of preterm labor.