Top food allergens for babies
Baby Food Allergies: Identifying and Preventing Them
Written by Gina Shaw
In this Article
- Start Gradually to Identify Any Food Allergies
- Babies and Allergies: The Top 8 Allergenic Foods
- Food Allergy Symptoms to Watch for in Your Baby
- Severe Food Allergy Symptoms: When to Call 911
- Dealing With Mild Food Allergies in Baby
- The Family Food-Allergy Connection
- Protecting Baby Against Food Allergies: Easy Does It
Starting to feed a baby solid foods is an exciting milestone for parents. However, it comes with a lot of questions and concerns, especially about food allergies. What foods are most likely to cause allergies in babies? How do you avoid them?
Emerging research has shown that introducing multiple foods together is safe, and may help the immune system have a lower risk of developing food allergies, but more studies are needed. Check with your doctor for what’s best for your baby.
Start Gradually to Identify Any Food Allergies
It’s most important to introduce a baby to new foods gradually, one at a time, in case of food allergies. If not, a parent may have trouble tying an allergy to a specific new food. For example, if you give your baby three new foods over the course of a day and they develop an allergic reaction, you won’t know which of the foods provoked it.
The type of food or the order in which food is introduced is not much of a concern, as long as the foods you are offering are healthy and well-balanced for the baby. Each time you offer a new food, you should wait three to five days before adding another new item to the menu. Don’t eliminate the other foods your baby is eating during that time; you already know these are safe because the child has not had any food reactions up until now. Just don’t add anything else new.
Babies and Allergies: The Top 8 Allergenic Foods
With any new food, you’ll want to be on the lookout for any allergic reactions. There are more than 160 allergenic foods; certain foods may be more allergenic than others. The following eight foods and food groups are known to possibly cause problems with allergic reactions possibly up to 90% of the time.
There are more than 160 allergenic foods; certain foods may be more allergenic than others. The following eight foods and food groups are known to possibly cause problems with allergic reactions possibly up to 90% of the time.
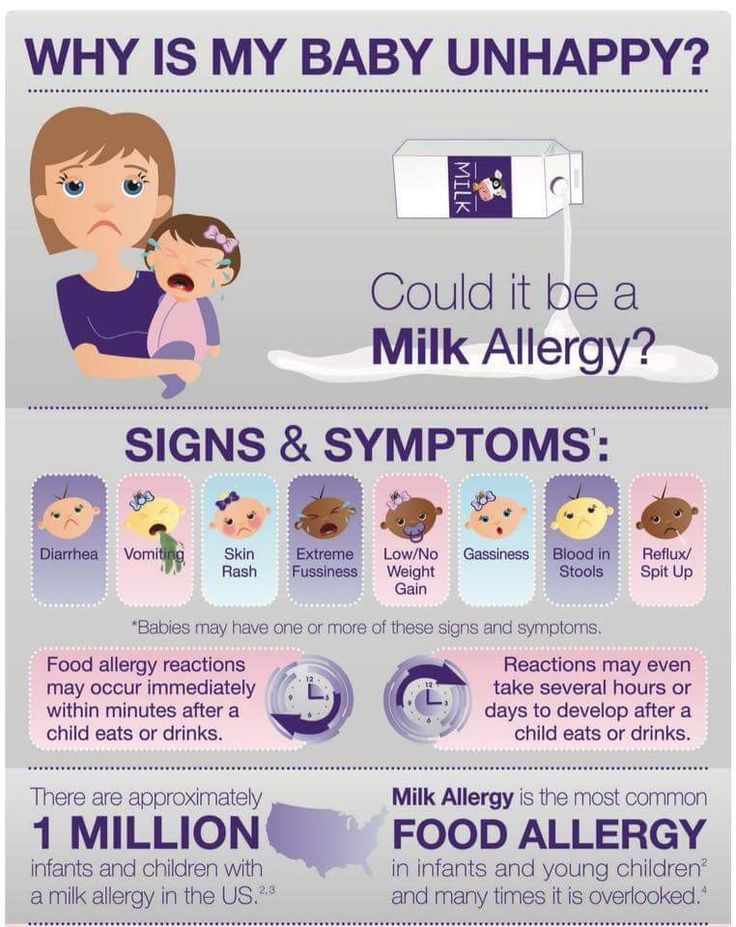
- Cow's milk
- Eggs
- Peanuts
- Tree nuts (such as walnuts or almonds)
- Fish
- Shellfish
- Soy
- Wheat
New nutrition guidelines from the American Academy of Pediatrics say it's okay to introduce these allergy-causing foods when your baby is ready to eat solids. There is no evidence that waiting until the baby is older prevents food allergy. If you believe your baby has an allergic reaction to a food, such as diarrhea, rash, or vomiting, talk with your child's doctor about the best choices for the diet.
Within a few months of starting solid foods, your baby's daily diet should include a variety of foods, such as breast milk, formula, or both; meats; cereal; vegetables; fruits; eggs; and fish.
Food Allergy Symptoms to Watch for in Your Baby
Food allergy symptoms usually appear very soon after the food is eaten -- within a few minutes to a couple of hours. If you’re introducing a new food to your baby, keep an eye out for these symptoms:
If you’re introducing a new food to your baby, keep an eye out for these symptoms:
- Hives or welts
- Flushed skin or rash
- Face, tongue, or lip swelling
- Vomiting and/or diarrhea
- Coughing or wheezing
- Difficulty breathing
- Loss of consciousness
Severe Food Allergy Symptoms: When to Call 911
Severe allergic reactions can be fatal very quickly. If your baby is having trouble breathing/wheezing, has swelling on their face/lips, or develops severe vomiting or diarrhea after eating, immediately call 911. You can inform your pediatrician at a later time.
Dealing With Mild Food Allergies in Baby
If you see mild symptoms, such as hives or a rash, contact your pediatrician for further evaluation. The doctor might refer you to an allergist (allergy specialist doctor), who will ask more questions and do a physical exam. The allergies may order diagnostic tests such as:
- A skin test. This test involves placing liquid extracts of food allergens on your child's forearm or back, pricking the skin, and waiting to see if reddish raised spots form within 15 minutes.
 A positive test to a food only shows that your child might be sensitive to that food.
A positive test to a food only shows that your child might be sensitive to that food. - Blood tests to check the blood for IgE antibodies to specific foods
Remember, just because a baby’s initial allergic reaction to a new food may be mild, it may get worse upon following exposures. Talk to your pediatrician about any food allergy symptoms in your baby.
Some allergies go away with time. Egg and milk allergies often go away as children get older, but peanut, tree nut, and shellfish allergies tend to persist. That said, research shows that in the case of peanut allergies, peanut immunotherapy drops administered under the tongue are safe and effective as treatment for peanut allergy, even in children as young as 1. They were also found to help significantly desensitize the patients to peanuts.
The Family Food-Allergy Connection
If there is a family food allergies, your baby has an increased risk of also developing allergies, although it is not a certainty.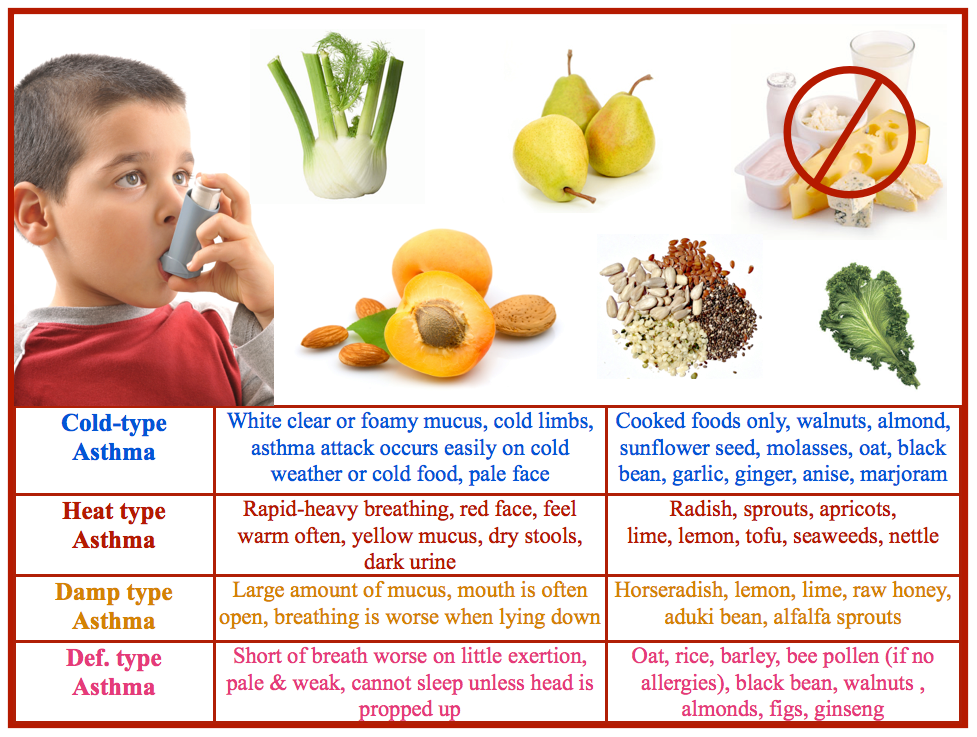 If you have the allergies, the odds are 50-50 for them to have them as well.
If you have the allergies, the odds are 50-50 for them to have them as well.
It’s best to introduce the 8 allergens gradually, at one-to-two week intervals over time so that you can recognize if an allergy develops.
Protecting Baby Against Food Allergies: Easy Does It
In a reversal of earlier policy, the American Academy of Pediatrics is now recommending that potential allergens be introduced to your infant earlier rather than later. In doing so, the move may actually help prevent them from developing allergies to those foods.
Breastfeeding you baby for 4-6 months is the best way to prevent a milk allergy. Remember that breast milk or formula is higher in nutrition. When you begin to introduce whole milk, you should do so under a doctor’s supervision. Yogurt and soft cheeses are fine, because the proteins in these dairy products are broken down and less likely to cause tummy trouble.
The AAP now advises that, in the case of infants who are at high risk of allergies, peanuts should be introduced between 4-6 months. Infants at highest risk of developing peanut allergies are those with eczema or egg allergies or both. It was originally believed that introducing your baby to the foods when they are older might make any reactions more manageable.
Infants at highest risk of developing peanut allergies are those with eczema or egg allergies or both. It was originally believed that introducing your baby to the foods when they are older might make any reactions more manageable.
Other potential allergens such as tree nuts and fish should be introduced over a period of time as you introduce your baby to solid foods, between 6 and 9 months
You should wait until at least age 1 (some experts say age 2) to introduce honey, which can cause a potentially serious disease called infant botulism. Ask your pediatrician for guidance.
Common food allergens and kids
Share:
Sharing new foods with your baby is an exciting milestone. Unfortunately, amongst the fun of watching your child experience new tastes remain questions and fears about food allergies. Recommendations of when to introduce certain foods seem to change often, and for many parents, it can be confusing to know what is best for your child at each age.
April Clark, registered dietitian with the Food Allergy Center at Children’s Health℠, offers tips on when and how to introduce the top allergenic foods.
How to decrease the chance of food allergies in kids
The eight most common food allergens include: cow’s milk, eggs, peanuts, soy, tree nuts, finned fish, shellfish and wheat (gluten). According to the FDA, they account for approximately 90% of all food allergies in the United States.
Previously, the American Academy of Pediatrics (AAP) recommended that the introduction of certain highly allergenic foods be delayed in high-risk children. However, the AAP now recognizes that early introduction of peanuts decreases the chance of developing peanut allergies. Clark recommends following new guidelines to slowly introduce allergenic foods after the addition of solid foods, which often occurs during a baby’s first 4 to 6 months.
Tips on introducing new foods
Clark recommends that any of the foods noted below should be introduced one at a time, and parents should carefully observe their child’s reactions. Foods should first be given as single ingredients – not as part of a recipe like eggs in a baked good. They can also be given with complementary fruits and vegetables that have already been proven safe.
Foods should first be given as single ingredients – not as part of a recipe like eggs in a baked good. They can also be given with complementary fruits and vegetables that have already been proven safe.
If there isn’t an allergic reaction once a food is introduced, continue including it at least three times a week in your child’s meals to ensure the best results. There isn’t a firm deadline to stop serving the foods. Instead, Clark notes that a healthy, well-balanced diet should normally contain variations of these common foods.
- Cow’s milk (dairy) may be one of the first allergies to be noticed, as many formulas are made with milk. Unlike the other foods listed, experts recommend waiting until after age 1 to introduce cow’s (whole) milk into a child’s diet. Instead, Clark notes babies eating solid foods should try yogurt or cheeses.
- Eggs are an excellent source of protein for growing children. Clark recommends either scrambled eggs or pieces of hard-boiled eggs.
 Depending on the child, they may enjoy the squishy texture and prefer to feed themselves.
Depending on the child, they may enjoy the squishy texture and prefer to feed themselves. - Peanuts or peanut butter are another reliable source of protein. Do not give whole or even peanut pieces, as they can be a choking hazard; instead, peanut butter is a safer alternative, but the thick consistency can be difficult for most children to swallow. Clark recommends melting down the peanut butter with warm water or adding it to a fruit or veggie puree. If a child has severe eczema, and/or already has been diagnosed with egg allergy, they should be evaluated prior to peanut introduction.
- Soy is another allergy that is noticed early due to formulas with a soy base. Protein-packed tofu and edamame (soy beans) can be introduced when your child is ready. They are great options for self-feeding. Like cow’s milk, Clark says parents should not offer soy milk until after age 1.
- Finned fish and shellfish (shrimp, crab, clams, etc.
 ) can be introduced as a puree around the 4 to 6-month mark, or in bite-size pieces once your child is ready. In addition to possible allergies, the AAP warns parents not to serve raw or undercooked items due to possible bacteria or viruses that can make your child seriously ill. Also, the AAP notes children shouldn’t eat more than 12 ounces of fish a week due to concerns about traces of mercury in fish or shellfish.
) can be introduced as a puree around the 4 to 6-month mark, or in bite-size pieces once your child is ready. In addition to possible allergies, the AAP warns parents not to serve raw or undercooked items due to possible bacteria or viruses that can make your child seriously ill. Also, the AAP notes children shouldn’t eat more than 12 ounces of fish a week due to concerns about traces of mercury in fish or shellfish. - Tree nuts (almonds, cashews or walnuts) follow the same guidelines as peanut and peanut butter above.
- Wheat (gluten) can be introduced as finger foods in teething biscuits, puffs and crackers that contain wheat.
Signs of a food allergy
Clark notes children with a first-degree relative (parent or sibling) with allergies are more likely to also have food allergies. Children (and their parents) who have a history of severe or recurring eczema and/or asthma are also at a higher risk to develop food allergies. If your child has any of these factors, you many want to consult your pediatrician for guidance on the best way to proceed.
If your child has any of these factors, you many want to consult your pediatrician for guidance on the best way to proceed.
Allergy symptoms and reactions can vary between children and may appear differently, depending on the age. Reactions can develop minutes after the food is ingested, or there may be a delayed reaction a few hours later. Clark cautions anyone can have a severe reaction at any time, and recommends following guidelines developed by Food Allergy Research & Education (FARE) to identify an allergic reaction. See FARE's list of symptoms here.
What to do if an allergic reaction occurs
Contact your pediatrician if your child has a mild allergic reaction and it is not an emergency. Call 911 immediately for severe and life-threatening reactions.
If you suspect your child has a food allergy, Clark recommends seeing a board-certified allergist to discuss your concerns. Bring any information about the food, the reaction and your family history to the appointment.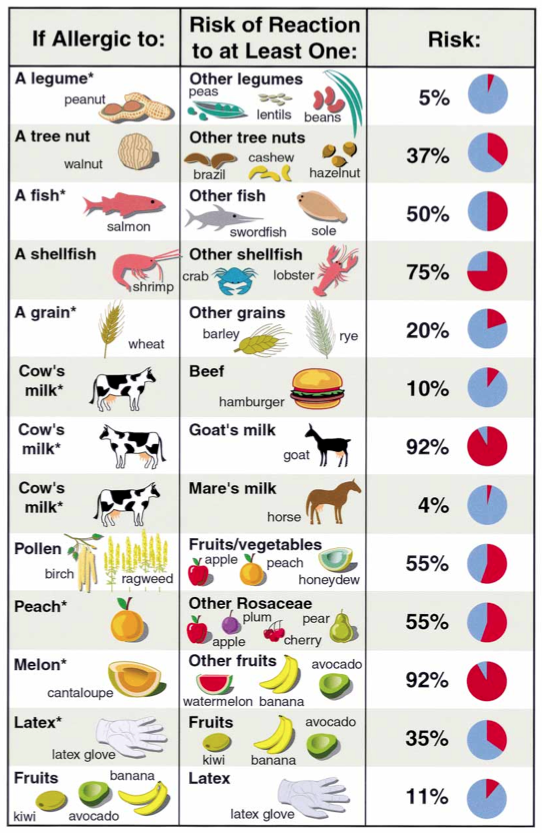 The physician will likely take a detailed medical and diet history, and recommend appropriate testing that’s specific to your child’s symptoms and suspected food allergens. Your allergist will be able to manage the diagnosis and answer any questions. Specialists can also provide useful information like recipes and food allergy guidelines.
The physician will likely take a detailed medical and diet history, and recommend appropriate testing that’s specific to your child’s symptoms and suspected food allergens. Your allergist will be able to manage the diagnosis and answer any questions. Specialists can also provide useful information like recipes and food allergy guidelines.
Download your guide to allergen-free lunches
Looking for tips to pack allergy-friendly school lunches? Download the Parents' Guide to Allergen-Free Lunches for kid-friendly recipes that are free of the top eight food allergens. Download now.
Learn more
Food allergy experts at Children’s Health can help with testing, questions and offer patient resources. Learn more about our program and services.
For more information, please see the following additional references:
- Food Allergy Research & Education (FARE)
- Instructions for feeding peanut butter and recipes
- Additional information about introducing peanut butter
- LEAP study in the U.
 K. (Learning Early About Peanuts)
K. (Learning Early About Peanuts) - Recommendations from the AAP for introducing food
Thank you!
You are now subscribed to the Children's Health Family Newsletter.
Children's Health will not sell, share or rent your information to third parties. Please read our privacy policy.
Children's Health Family Newsletter
Get health tips and parenting advice from Children's Health experts sent straight to your inbox twice a month.
Please enter a valid email address
Food allergies in children
What you need to know about feeding young children with food allergies
Food allergies are the earliest form of allergic diseases and can manifest themselves from the first months of life. Its detrimental effect on health is associated not only with the immediate signs of food allergies in children, which in themselves can be painful for the baby, for example, skin itching or intestinal colic, but also with the fact that due to the forced restriction of nutrition, there is a threat to normal development child.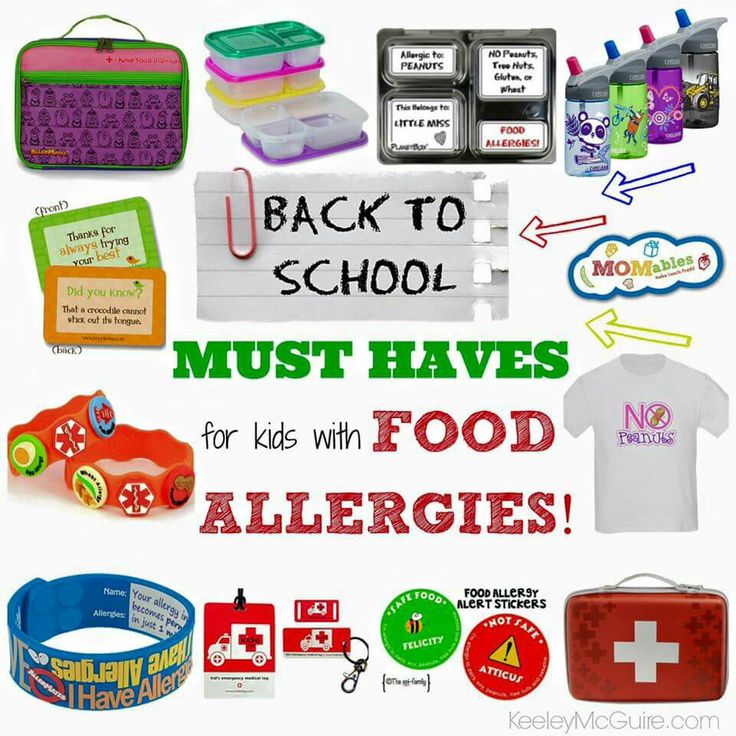 On the other hand, the current food allergy in children creates conditions for the rapid formation of subsequent forms of allergic diseases, including such severe ones as bronchial asthma.
On the other hand, the current food allergy in children creates conditions for the rapid formation of subsequent forms of allergic diseases, including such severe ones as bronchial asthma.
Causes of food allergies
The main cause of food allergies lies in the violation of the fundamental mechanism of the nutrition process, which in the language of specialists is called food tolerance. Its biological meaning is that, on the one hand, it allows various natural substances to penetrate into the internal environment of the body as part of food, in order to then build tissues and organs from them. On the other hand, the same mechanism provides a powerful barrier to the penetration of those substances that can violate the genetic integrity of the human body. This mechanism belongs to the domain of the immune system. Due to its extreme importance, it begins to form very early, already from the 7th week of intrauterine development. Interestingly, its improvement occurs under the direct control of the nutrients themselves, which first penetrate the fetus through the cord blood into the baby's body with mother's milk, and then through the child's independent nutrition.
All the main components of food, namely: proteins, fats, carbohydrates, trace elements, vitamins have a strong effect on the immune system. They regulate the work of immune cells, cooperate with the interaction of various participants in the immune process, and are even able to change the activity of genes responsible for the immune response. This influence is especially powerful in the first months and years of life, but is not lost in all other periods of a person's life. An active role in the formation of food tolerance is played by beneficial intestinal microorganisms. They provide the right balance of individual participants in the immune system, enhance the production of protective immune proteins and support the overall activity of the immune system with the help of their waste products.
What foods cause food allergies in children?
Food allergies can occur after eating a variety of foods that have allergenic properties.
Animal food proteins are considered the most allergenic, especially those whose structure differs significantly (more than 55%) from the structure of human proteins.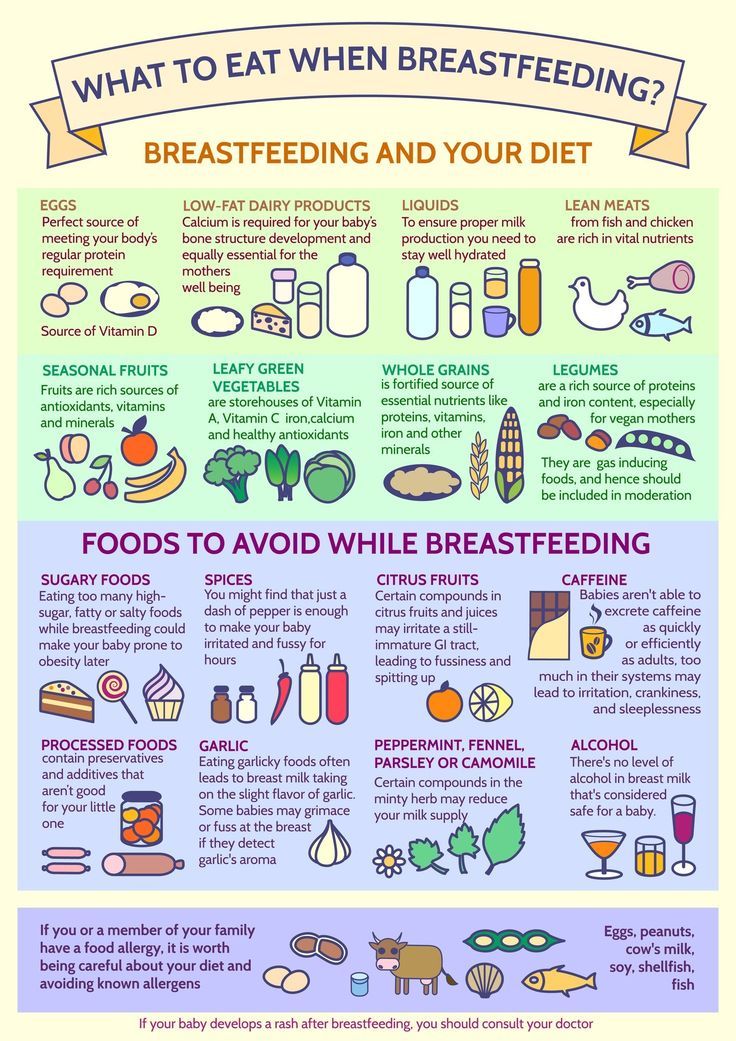 These include proteins in the muscle tissue of crustaceans, fish, mammalian milk, chicken eggs. At the age of the first 3 years, especially in the first year of life, the most important allergens are animal milk proteins (cow, goat). There are more than 200 of them in milk. Each of them or several proteins at the same time can become allergenic for a child, so it is not practical to consider that some milk is less allergenic than another.
These include proteins in the muscle tissue of crustaceans, fish, mammalian milk, chicken eggs. At the age of the first 3 years, especially in the first year of life, the most important allergens are animal milk proteins (cow, goat). There are more than 200 of them in milk. Each of them or several proteins at the same time can become allergenic for a child, so it is not practical to consider that some milk is less allergenic than another.
Plant foods also have a number of allergenic properties. Its allergenic potential is largely determined by the presence of so-called "plant protection proteins". These substances are able to break down insect chitin, protect the plant from microbes and fungi, and help it fight chemical and mechanical damage. Under unfavorable plant growth conditions or improper storage conditions for food raw materials (vegetables, fruits, cereals, nuts), their concentration can be very high, therefore, cutting off the damaged part of the fruit, you will slightly reduce its allergenic properties.
Seed germ proteins, cereals and gluten components are also highly allergenic. From a practical point of view, it is important that the allergens of some plants have a certain similarity with each other. This leads to the fact that at the same time the child may have intolerance to antigenically related pollens (for example, birch and wormwood pollen), vegetables (for example, carrots) and fruits (for example, apples). For the ability to cross-react, such allergens are called "panallergens". The same property of plant allergens is associated with the regular formation of pollen allergy (hay fever) in a child who has a food allergy to plant foods.
Is it possible to reduce the allergenic properties of food?
Studies have proven the failure of attempts to reduce the allergenic properties of food through culinary or industrial processing. Since the 60s of the last century, it has become known that if the protein is not acted too aggressively, then it temporarily changes its “architecture”, but then spontaneously restores it when the environment “normalizes” (Anfinsena K. B., 1972, Nobel Prize) . For example, during the industrial production of infant milk formulas, during pasteurization, drying, and other influences, milk protein reduces its allergenic properties, but when the dry milk formula is diluted with water, it regains it. In some cases, prolonged heat treatment can lead to a significant increase in the allergenic properties of the protein. So, in the process of preparing boiled condensed milk, beloved by children, milk protein combines with sugar and forms an aggressive chemical compound that can cause severe manifestations of food allergies. Similar compounds are also formed during long-term storage of the opened package of dry infant formula, which exceeds the recommended time.
B., 1972, Nobel Prize) . For example, during the industrial production of infant milk formulas, during pasteurization, drying, and other influences, milk protein reduces its allergenic properties, but when the dry milk formula is diluted with water, it regains it. In some cases, prolonged heat treatment can lead to a significant increase in the allergenic properties of the protein. So, in the process of preparing boiled condensed milk, beloved by children, milk protein combines with sugar and forms an aggressive chemical compound that can cause severe manifestations of food allergies. Similar compounds are also formed during long-term storage of the opened package of dry infant formula, which exceeds the recommended time.
There are foods that do not lose their high allergenicity either during cooking or during digestion and can cause food allergies, cause allergic reactions even when consumed in small quantities. Such products include fish, caviar, shrimp, eggs, nuts, honey, mushrooms, citrus fruits, strawberries, coffee, cocoa, chocolate. They are called obligate allergens and are mandatory removed from the children's diet for food allergies.
They are called obligate allergens and are mandatory removed from the children's diet for food allergies.
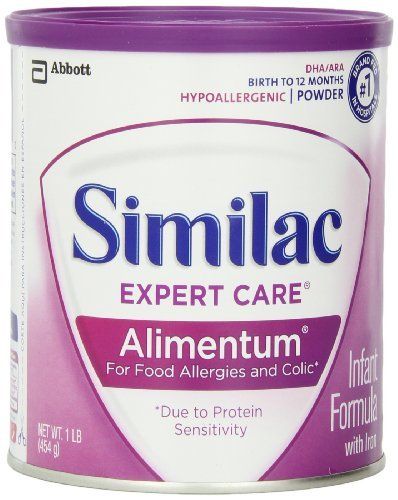
Recommendations of a pediatric allergist
The risk of food allergies in a small child is also associated with high intestinal permeability. It is especially high in a child in the first months of life. In breastfeeding conditions, this is not dangerous, since the intake of food allergens through mother's milk is extremely small, and besides, breast milk itself has powerful anti-allergic properties. At the same time, early artificial feeding can lead to inadequately high penetration of proteins with high allergenic properties into the body. So with 40g of a standard milk formula, a child will receive the same amount of the most allergenic milk protein (ß-lactoglobulin) as it is contained in 8000l of breast milk! In conditions of an immature immune system, and especially if the child has a hereditary predisposition to allergies, this leads to the rapid formation of food allergies in children. The same undesirable effect occurs with unreasonably early introduction of complementary foods, especially if they contain highly allergenic components.
The same undesirable effect occurs with unreasonably early introduction of complementary foods, especially if they contain highly allergenic components.
Mistakes in child nutrition create a high risk of developing food allergies. At the same time, with proper management, it is nutrition that becomes a powerful and effective therapeutic and preventive measure.
Diet for children with food allergies
Features of the organization of a diet for food allergies in a child, of course, depend on age, but there are general rules that ensure its effectiveness: For a child of the first year of life, this is, of course, long-term (at least 6 months) breastfeeding. In those rare cases when allergens that penetrate breast milk cause allergy symptoms in the child, it is necessary to organize a hypoallergenic diet for the mother with the exception of obligate food allergens, foods that cause allergic reactions in the child (most often, these are dairy products), irritating dishes.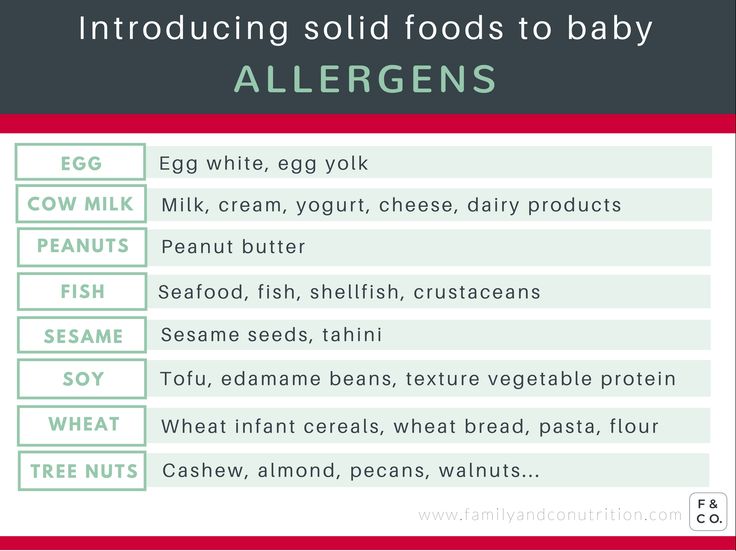 In conditions of artificial feeding, the diet for children with food allergies is based on highly effective medicinal products in which milk protein is split into non-allergenic substances. They are called complete hydrolysates. Their choice is quite wide. Such mixtures can even be tailored to a particular clinical manifestation, such as a predominant skin or gastrointestinal tract lesion. They contain everything necessary for the good development of the child and can be used for a long time. If a child has signs of a food allergy to cow's milk proteins, in no case should therapeutic mixtures be replaced with fermented milk products or so-called hypoallergenic mixtures, which are intended only for the prevention of food allergies if there is a risk of its development.
In conditions of artificial feeding, the diet for children with food allergies is based on highly effective medicinal products in which milk protein is split into non-allergenic substances. They are called complete hydrolysates. Their choice is quite wide. Such mixtures can even be tailored to a particular clinical manifestation, such as a predominant skin or gastrointestinal tract lesion. They contain everything necessary for the good development of the child and can be used for a long time. If a child has signs of a food allergy to cow's milk proteins, in no case should therapeutic mixtures be replaced with fermented milk products or so-called hypoallergenic mixtures, which are intended only for the prevention of food allergies if there is a risk of its development.
The timing and correct sequence of complementary foods are very important. In children with food allergies, complementary foods are introduced no earlier than 4.5 and no later than 6 months. life. It is more profitable to start with vegetables, since their overall allergenic potential is lower than that of cereals. The optimal first choice is mono-component mashed potatoes from zucchini, cauliflower, broccoli without salt and sugar. From 5 months pumpkin puree, carrots and vegetable mixtures can be introduced, then vegetable stews and vegetables supplemented with cereals, such as rice. At the severity of the disease, potatoes are not recommended. Its main allergen (Sola t1) is resistant to digestion and heat treatment and can cause a reaction. Starch does not contain this allergen. The first porridge should be not only monocomponent, but also gluten-free (low-allergenic buckwheat, rice, corn). Early introduction of cereals containing gluten (for example, semolina) can cause allergic inflammation of the intestinal mucosa and increase its permeability. The absence of gluten-containing admixtures can only be guaranteed by cereals of industrial production. Their advantages, which are important for a child with allergies, include supplementation with substances useful for immunity - dietary fiber, fatty acids, vitamins and minerals.
The optimal first choice is mono-component mashed potatoes from zucchini, cauliflower, broccoli without salt and sugar. From 5 months pumpkin puree, carrots and vegetable mixtures can be introduced, then vegetable stews and vegetables supplemented with cereals, such as rice. At the severity of the disease, potatoes are not recommended. Its main allergen (Sola t1) is resistant to digestion and heat treatment and can cause a reaction. Starch does not contain this allergen. The first porridge should be not only monocomponent, but also gluten-free (low-allergenic buckwheat, rice, corn). Early introduction of cereals containing gluten (for example, semolina) can cause allergic inflammation of the intestinal mucosa and increase its permeability. The absence of gluten-containing admixtures can only be guaranteed by cereals of industrial production. Their advantages, which are important for a child with allergies, include supplementation with substances useful for immunity - dietary fiber, fatty acids, vitamins and minerals. Meat complementary foods are introduced to children with food allergies on time (7-8 months) and in full, because. it ensures the intake of sufficient quantities of nutrients important for the development of immunity, such as protein, iron and zinc. When choosing a type of meat, one should be guided by its allergenic properties. Horse meat, rabbit, turkey, pork, beef are preferred. During a diet with food allergies, fish, caviar, eggs are not given (sometimes chicken eggs can be replaced with quail eggs), nuts, honey, cocoa, chocolate (they can be a component of some children's cereals and cookies), strawberries, strawberries, citrus fruits.
Meat complementary foods are introduced to children with food allergies on time (7-8 months) and in full, because. it ensures the intake of sufficient quantities of nutrients important for the development of immunity, such as protein, iron and zinc. When choosing a type of meat, one should be guided by its allergenic properties. Horse meat, rabbit, turkey, pork, beef are preferred. During a diet with food allergies, fish, caviar, eggs are not given (sometimes chicken eggs can be replaced with quail eggs), nuts, honey, cocoa, chocolate (they can be a component of some children's cereals and cookies), strawberries, strawberries, citrus fruits.
- Correction of emerging nutritional deficiencies. Depriving a child for a long time of important food for his age can lead to the formation of nutritional deficiencies, primarily mineral salts and vitamins. Under the conditions of the use of specialized therapeutic mixtures, this does not happen, but only if their daily volume is sufficient.
 If they are not used in the diet of children with food allergies, or their volume is too small, then additional correction with multivitamin and mineral complexes may be necessary. Vitamins A, E, C, B6, B12, folates, minerals zinc and selenium are especially important for maintaining immunity. Their combination with polyunsaturated fatty acids (omega acids) is optimal.
If they are not used in the diet of children with food allergies, or their volume is too small, then additional correction with multivitamin and mineral complexes may be necessary. Vitamins A, E, C, B6, B12, folates, minerals zinc and selenium are especially important for maintaining immunity. Their combination with polyunsaturated fatty acids (omega acids) is optimal. - Ensuring environmentally friendly products. Unfortunately, modern food products are characterized by a high degree of environmental pollution. These can be antibiotics, hormone-like substances, traces of fertilizers and pesticides, molds that release toxic substances. Industrial production of food products, their transportation and storage are inconceivable without the so-called food additives. It turned out that many of them provoke the manifestation of food allergies in children. This happens especially often when using products containing benzoic acid and benzoates (E 210-213), butylated hydroxyanisole (E 320), butylated hydroxytoluene (E 321), gallates (E 310-313), sodium glutamate (E 621), diphenyl (E 230 ) and some others.
 All these undesirable impurities are found in abundance in general-purpose industrial products, so you should never feed a small child with dishes from a common family table. This food does not correspond to the digestive and immune capabilities of the child and always puts him on the brink of illness. The only reliable choice is industrial children's products made in an environmentally friendly manner.
All these undesirable impurities are found in abundance in general-purpose industrial products, so you should never feed a small child with dishes from a common family table. This food does not correspond to the digestive and immune capabilities of the child and always puts him on the brink of illness. The only reliable choice is industrial children's products made in an environmentally friendly manner.
Eating a child with food allergies is a troublesome and painstaking task. It requires strict adherence to the recommendations of a pediatric allergist, utmost care in choosing food, and adherence to the duration of a therapeutic diet. Be patient. Change takes time, but you will be rewarded by bringing significant relief to your child, and sometimes a full recovery.
See also:
- Ambulatory ECG and BP monitoring
- Treatment of insomnia in St. Petersburg
- Ultrasound examination of the gallbladder
- Vocational rehabilitation center in St.
 Petersburg
Petersburg
6 food allergens that should not be given to a child
Other related articles: pediatrician,
8 proper nutrition
adenovirus infection
Adenoids
Autism
Autism (RAS)
Bronchitis in children
Chickenpox
windmill parties
coxsackie virus
Questions to the pediatrician
All about diets
Flu and SARS
Breast milk
Dacryocystitis
Children's painkillers
Diet for nursing
Medical examination at 1 year
Diphtheria in children
For expectant mothers
hardening
Hardening of children
Constipation in children
Foreign body of the bronchi
Infectious mononucleosis
Whooping cough
Measles in children
Rubella in children
Deprive a child
false croup
Tangerines for children
Children's massage
Meningococcal infection
Pediatrician at home
First year of life
Baby's first year
Nutrition for children 1-3 years old
Child nutrition
food allergy
Defeat the Flu
Preparation for vaccination
Complementary foods for children
Child's bite
Walks in the cold
Products for longevity
Allergen products
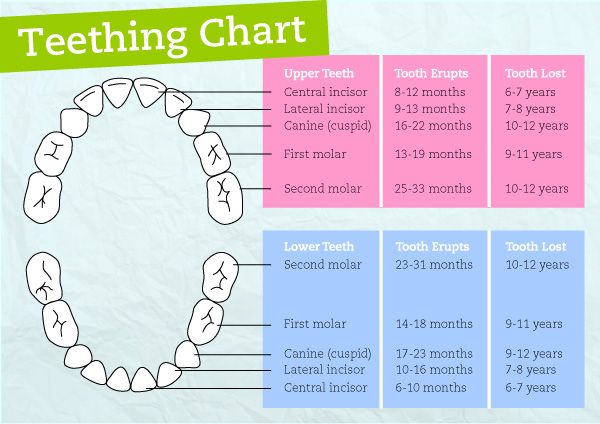
Teething
Rickets in children
Child is sick
Rotavirus infection
mumps in children
Scarlet fever in children
Sleep with animals
Baby care
Phytotherapy in children
Enuresis
Any food is capable of causing an allergic reaction, and we cannot exclude absolutely everything. But when we talk about food allergies, we immediately remember the big eight allergens:
But when we talk about food allergies, we immediately remember the big eight allergens:
- Eggs
- Milk
- Soya
- Peanuts
- Nuts
- Wheat
- Fish
- Mollusks and crustaceans
Let's take a look at each product individually.
So, eggs. Eggs are recommended to be introduced into the diet from 6-8 months of age. Only fully cooked eggs should be given to children.
Milk. Milk is not recommended for use in children under one year of age. After a year and up to 5 years, you can include milk in the menu daily.
Soy. Soya is also recommended for consumption from one year. It is worth recalling that any plant milk is not a complete replacement for regular cow's milk.
Peanuts. Peanuts are a common allergen in many developed countries. At the same time, there are a large number of studies that have shown that the introduction of peanut butter at the age of 4-6 months reduces the risk of developing an allergy to it at an older age. So peanut butter can be consumed from six months.
So peanut butter can be consumed from six months.
Nuts. Nuts are introduced into the diet from the year. It must be remembered that whole nuts or peanuts should not be given to children under five years of age due to the high risk of suffocation.
Wheat. Introduced into the diet from 8-10 months in the form of cereals, pasta, bread, baby cookies.
Fish. We add it to the child's diet from 8-10 months, starting with white fish, from the year you can start introducing red.
Mollusks and crustaceans. "Seafood" can be introduced into the diet of a child from the age of one. The main thing is that they are thermally fully cooked.
Thus, all the most important food allergens of this world can and should be consumed. If you suspect that your child is allergic to any product, you should consult a doctor to understand this issue. But you definitely shouldn’t exclude entire food groups from your child’s diet, since the most varied diet is the key to good health.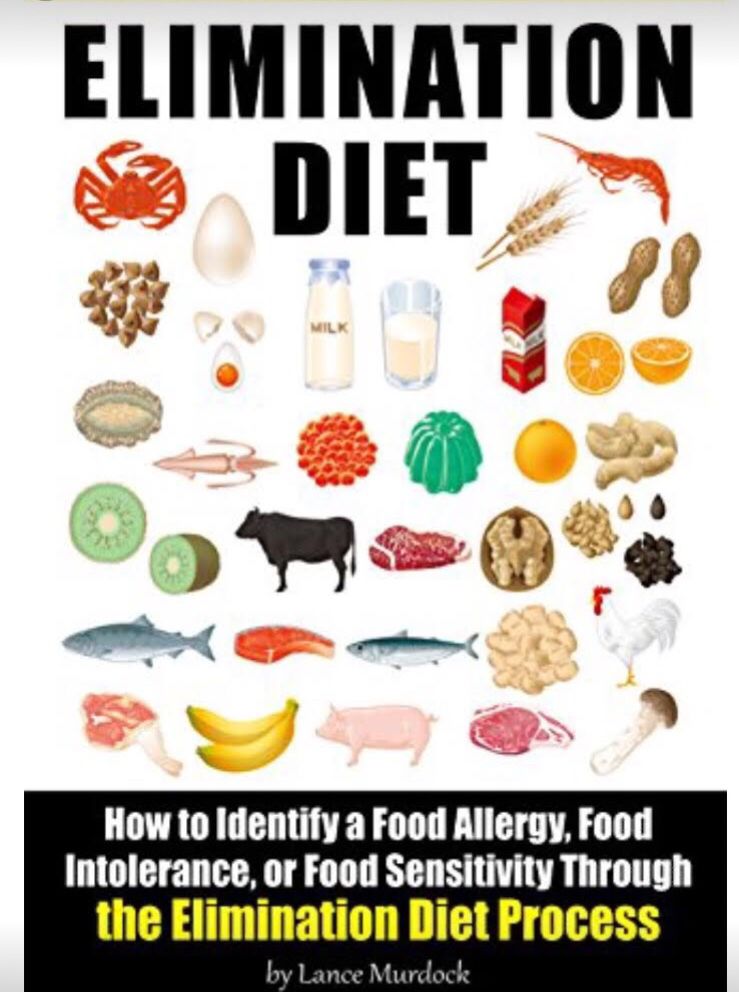
To be fair, there are also foods that contain high levels of histamine or cause it to be released in the body. When eating large amounts of these foods, some children may experience an allergic-like reaction. But this is not a true allergy, and the effect in this case is dose-dependent, that is: if a child eats two tomatoes, and not a kilogram, then nothing will happen.
These products include:
- Eggplant
- Tomatoes
- Pineapple, plum, banana, papaya, kiwi
- Almost all citrus fruits: lemon, lime, orange
- Pickled or preserved foods
- Hard cheeses, aged cheeses
- Smoked products, deli meats: salami, ham, sausages
- Shellfish, seafood
- Beans and legumes, chickpeas, soy flour
- Hazelnuts, walnuts, pine nuts, peanuts, cashews, almonds, pistachios
- Chocolate and other cocoa products
- Most vinegars
If you notice a reaction to any of the above foods, you can try reducing the amount in your diet and find a dose that your child can tolerate.
Food allergies are not that common in practice. This disease occurs in 6-8% of children and 3% of adults. At the same time, most children “outgrow” their allergies, and in adulthood they can safely eat foods previously excluded from the diet.
Still, there is something that should be excluded from the child's diet:
- Sugar up to two years. WHO clearly does not recommend foods containing added sugar for children under two years of age. After two years, it is worth focusing on age norms.
- Salt. It is not recommended to add it to the diet before 9 months. Up to three years - no more than two grams per day. Older than three years - no more than five.
- Honey up to a year. This is not due to its allergenicity, but to the risk of containing spores of the bacterium that causes botulism.
- Nuts, peanuts, whole grapes. Young children are at risk of suffocation with these products.

- Caffeine up to 4-5 years. Not recommended due to its stimulating effect.
- Rice milk up to 5 years. This milk may contain a high concentration of arsenic. This does not apply to rice itself and dishes from it.
- Trans fats. They are not recommended for children, as well as adults, because they increase the risk of CVD, a carcinogenic effect.
- Unwashed vegetables, raw eggs, meat.
- Products with a large amount of preservatives, dyes. It is not recommended to use up to 5-7 years, after - their content in the diet should be minimized.
In summary, we can say that there are no allergenic foods that need to be excluded from a child's diet. The diagnosis of food allergy is confirmed by the doctor, he also recommends a certain diet. And trying to delay the introduction of the most common allergens is not food allergy prevention.