A baby born three or more weeks early is called
Premature birth - Symptoms and causes
Overview
A premature birth is a birth that takes place more than three weeks before the baby's estimated due date. In other words, a premature birth is one that occurs before the start of the 37th week of pregnancy.
Premature babies, especially those born very early, often have complicated medical problems. Typically, complications of prematurity vary. But the earlier your baby is born, the higher the risk of complications.
Depending on how early a baby is born, he or she may be:
- Late preterm, born between 34 and 36 completed weeks of pregnancy
- Moderately preterm, born between 32 and 34 weeks of pregnancy
- Very preterm, born at less than 32 weeks of pregnancy
- Extremely preterm, born at or before 25 weeks of pregnancy
Most premature births occur in the late preterm stage.
Products & Services
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Mayo Clinic Guide to Your Baby's First Years
Symptoms
Your baby may have very mild symptoms of premature birth, or may have more-obvious complications.
Some signs of prematurity include the following:
- Small size, with a disproportionately large head
- Sharper looking, less rounded features than a full-term baby's features, due to a lack of fat stores
- Fine hair (lanugo) covering much of the body
- Low body temperature, especially immediately after birth in the delivery room, due to a lack of stored body fat
- Labored breathing or respiratory distress
- Lack of reflexes for sucking and swallowing, leading to feeding difficulties
The following tables show the median birth weight, length and head circumference of premature babies at different gestational ages for each sex.
| Weight, length and head circumference by gestational age for boys | |||
|---|---|---|---|
| Gestational age | Weight | Length | Head circumference |
| 40 weeks | 7 lbs. , 15 oz. , 15 oz.(3.6 kg) | 20 in. (51 cm) | 13.8 in. (35 cm) |
| 35 weeks | 5 lbs., 8 oz. (2.5 kg) | 18.1 in. (46 cm) | 12.6 in. (32 cm) |
| 32 weeks | 3 lbs., 15.5 oz. (1.8 kg) | 16.5 in. (42 cm) | 11.6 in. (29.5 cm) |
| 28 weeks | 2 lbs., 6.8 oz. (1.1 kg) | 14.4 in. (36.5 cm) | 10.2 in. (26 cm) |
| 24 weeks | 1 lb., 6.9 oz. (0.65 kg) | 12.2 in. (31 cm) | 8.7 in. (22 cm) |
| Weight, length and head circumference by gestational age for girls | |||
|---|---|---|---|
| Gestational age | Weight | Length | Head circumference |
| 40 weeks | 7 lbs.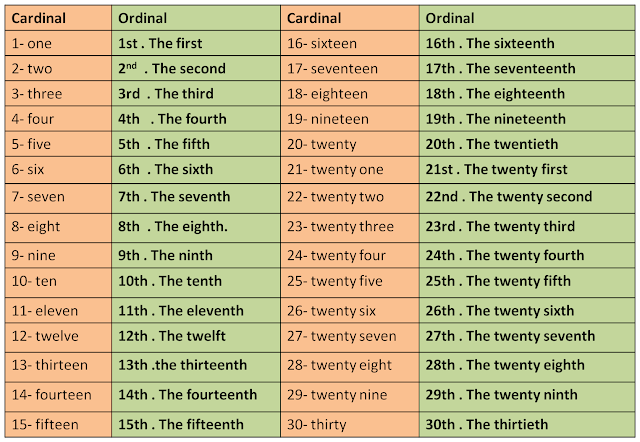 , 7.9 oz. , 7.9 oz.(3.4 kg) | 20 in. (51 cm) | 13.8 in. (35 cm) |
| 35 weeks | 5 lbs., 4.7 oz. (2.4 kg) | 17.7 in. (45 cm) | 12.4 in. (31.5 cm) |
| 32 weeks | 3 lbs., 12 oz. (1.7 kg) | 16.5 in. (42 cm) | 11.4 in. (29 cm) |
| 28 weeks | 2 lbs., 3.3 oz. (1.0 kg) | 14.1 in. (36 cm) | 9.8 in. (25 cm) |
| 24 weeks | 1 lb., 5.2 oz. (0.60 kg) | 12.6 in. (32 cm) | 8.3 in. (21 cm) |
Special care
If you deliver a preterm baby, your baby will likely need a longer hospital stay in a special nursery unit at the hospital. Depending on how much care your baby requires, he or she may be admitted to an intermediate care nursery or the neonatal intensive care unit (NICU).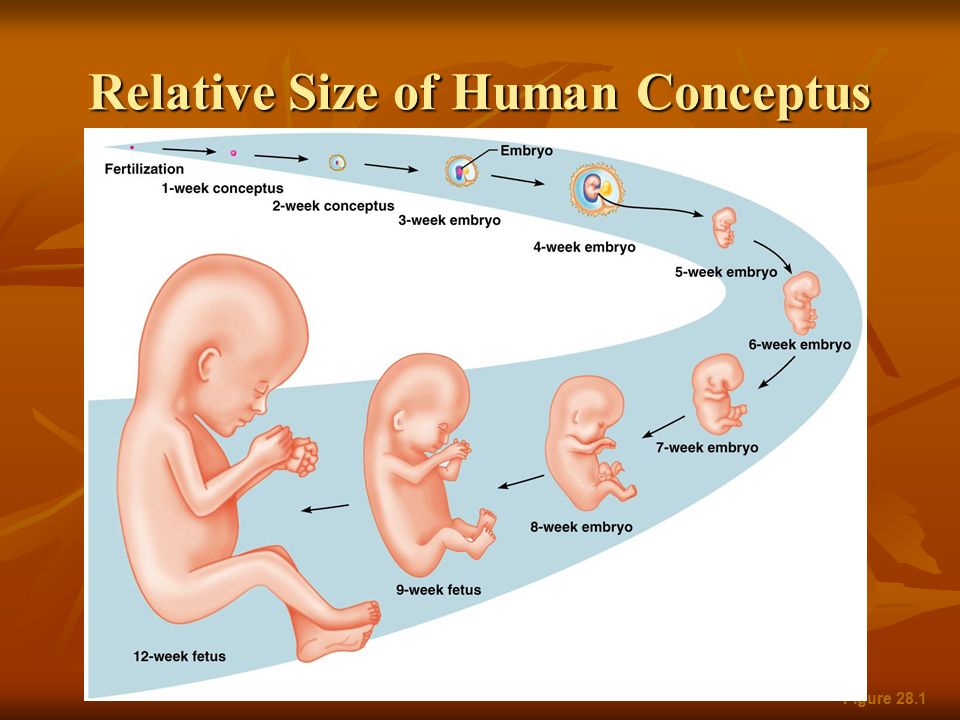 Doctors and a specialized team with training in taking care of preterm babies will be available to help care for your baby. Don't hesitate to ask questions.
Doctors and a specialized team with training in taking care of preterm babies will be available to help care for your baby. Don't hesitate to ask questions.
Your baby may need extra help feeding, and adapting immediately after delivery. Your health care team can help you understand what is needed and what your baby's care plan will be.
Request an Appointment at Mayo Clinic
Risk factors
Often, the specific cause of premature birth isn't clear. However, there are known risk factors of premature delivery, including:
- Having a previous premature birth
- Pregnancy with twins, triplets or other multiples
- An interval of less than six months between pregnancies
- Conceiving through in vitro fertilization
- Problems with the uterus, cervix or placenta
- Smoking cigarettes or using illicit drugs
- Some infections, particularly of the amniotic fluid and lower genital tract
- Some chronic conditions, such as high blood pressure and diabetes
- Being underweight or overweight before pregnancy
- Stressful life events, such as the death of a loved one or domestic violence
- Multiple miscarriages or abortions
- Physical injury or trauma
For unknown reasons, black women are more likely to experience premature birth than are women of other races.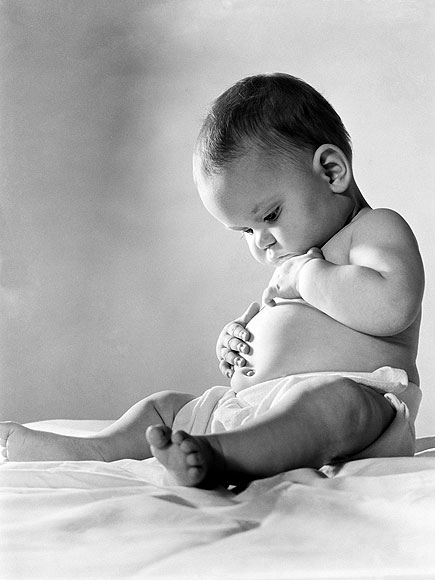 But premature birth can happen to anyone. In fact, many women who have a premature birth have no known risk factors.
But premature birth can happen to anyone. In fact, many women who have a premature birth have no known risk factors.
Complications
While not all premature babies experience complications, being born too early can cause short-term and long-term health problems. Generally, the earlier a baby is born, the higher the risk of complications. Birth weight plays an important role, too.
Some problems may be apparent at birth, while others may not develop until later.
Short-term complications
In the first weeks, the complications of premature birth may include:
-
Breathing problems. A premature baby may have trouble breathing due to an immature respiratory system. If the baby's lungs lack surfactant — a substance that allows the lungs to expand — he or she may develop respiratory distress syndrome because the lungs can't expand and contract normally.
Premature babies may also develop a lung disorder known as bronchopulmonary dysplasia.
 In addition, some preterm babies may experience prolonged pauses in their breathing, known as apnea.
In addition, some preterm babies may experience prolonged pauses in their breathing, known as apnea. - Heart problems. The most common heart problems premature babies experience are patent ductus arteriosus (PDA) and low blood pressure (hypotension). PDA is a persistent opening between the aorta and pulmonary artery. While this heart defect often closes on its own, left untreated it can lead to a heart murmur, heart failure as well as other complications. Low blood pressure may require adjustments in intravenous fluids, medicines and sometimes blood transfusions.
- Brain problems. The earlier a baby is born, the greater the risk of bleeding in the brain, known as an intraventricular hemorrhage. Most hemorrhages are mild and resolve with little short-term impact. But some babies may have larger brain bleeding that causes permanent brain injury.
-
Temperature control problems.
 Premature babies can lose body heat rapidly. They don't have the stored body fat of a full-term infant, and they can't generate enough heat to counteract what's lost through the surface of their bodies. If body temperature dips too low, an abnormally low core body temperature (hypothermia) can result.
Premature babies can lose body heat rapidly. They don't have the stored body fat of a full-term infant, and they can't generate enough heat to counteract what's lost through the surface of their bodies. If body temperature dips too low, an abnormally low core body temperature (hypothermia) can result.Hypothermia in a premature baby can lead to breathing problems and low blood sugar levels. In addition, a premature infant may use up all of the energy gained from feedings just to stay warm. That's why smaller premature infants require additional heat from a warmer or an incubator until they're larger and able to maintain body temperature without assistance.
- Gastrointestinal problems. Premature infants are more likely to have immature gastrointestinal systems, resulting in complications such as necrotizing enterocolitis (NEC). This potentially serious condition, in which the cells lining the bowel wall are injured, can occur in premature babies after they start feeding.
 Premature babies who receive only breast milk have a much lower risk of developing NEC.
Premature babies who receive only breast milk have a much lower risk of developing NEC. -
Blood problems. Premature babies are at risk of blood problems such as anemia and newborn jaundice. Anemia is a common condition in which the body doesn't have enough red blood cells. While all newborns experience a slow drop in red blood cell count during the first months of life, the decrease may be greater in premature babies.
Newborn jaundice is a yellow discoloration in a baby's skin and eyes that occurs because the baby's blood contains excess bilirubin, a yellow-colored substance, from the liver or red blood cells. While there are many causes of jaundice, it is more common in preterm babies.
- Metabolism problems. Premature babies often have problems with their metabolism. Some premature babies may develop an abnormally low level of blood sugar (hypoglycemia). This can happen because premature infants typically have smaller stores of stored glucose than do full-term babies.
 Premature babies also have more difficulty converting their stored glucose into more-usable, active forms of glucose.
Premature babies also have more difficulty converting their stored glucose into more-usable, active forms of glucose. - Immune system problems. An underdeveloped immune system, common in premature babies, can lead to a higher risk of infection. Infection in a premature baby can quickly spread to the bloodstream, causing sepsis, an infection that spreads to the bloodstream.
Long-term complications
In the long term, premature birth may lead to the following complications:
- Cerebral palsy. Cerebral palsy is a disorder of movement, muscle tone or posture that can be caused by infection, inadequate blood flow or injury to a newborn's developing brain either early during pregnancy or while the baby is still young and immature.
- Impaired learning. Premature babies are more likely to lag behind their full-term counterparts on various developmental milestones. Upon school age, a child who was born prematurely might be more likely to have learning disabilities.

- Vision problems. Premature infants may develop retinopathy of prematurity, a disease that occurs when blood vessels swell and overgrow in the light-sensitive layer of nerves at the back of the eye (retina). Sometimes the abnormal retinal vessels gradually scar the retina, pulling it out of position. When the retina is pulled away from the back of the eye, it's called retinal detachment, a condition that, if undetected, can impair vision and cause blindness.
- Hearing problems. Premature babies are at increased risk of some degree of hearing loss. All babies will have their hearing checked before going home.
- Dental problems. Premature infants who have been critically ill are at increased risk of developing dental problems, such as delayed tooth eruption, tooth discoloration and improperly aligned teeth.
- Behavioral and psychological problems. Children who experienced premature birth may be more likely than full-term infants to have certain behavioral or psychological problems, as well as developmental delays.
- Chronic health issues. Premature babies are more likely to have chronic health issues — some of which may require hospital care — than are full-term infants. Infections, asthma and feeding problems are more likely to develop or persist. Premature infants are also at increased risk of sudden infant death syndrome (SIDS).
Prevention
Although the exact cause of preterm birth is often unknown, there are some things that can be done to help women — especially those who have an increased risk — to reduce their risk of preterm birth, including:
- Progesterone supplements. Women who have a history of preterm birth, a short cervix or both factors may be able to reduce the risk of preterm birth with progesterone supplementation.
-
Cervical cerclage. This is a surgical procedure performed during pregnancy in women with a short cervix, or a history of cervical shortening that resulted in a preterm birth.

During this procedure, the cervix is stitched closed with strong sutures that may provide extra support to the uterus. The sutures are removed when it's time to deliver the baby. Ask your doctor if you need to avoid vigorous activity during the remainder of your pregnancy.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
When Your Baby's Born Premature (for Parents)
What Is Prematurity?
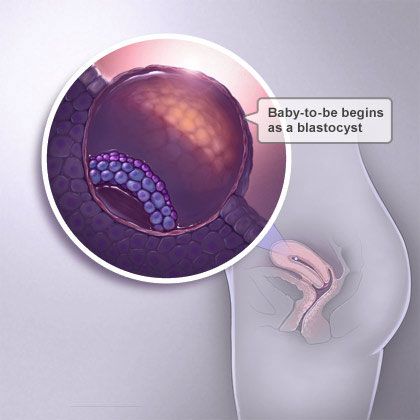
Babies born more than 3 weeks earlier than their expected due date are called "premature." Premature babies (preemies) didn't have enough time to grow and develop as much as they should have before birth.
Why Was My Baby Born Early?
Most of the time, doctors don't know why babies are born early. When they do know, it's often because a mother has a health problem during pregnancy, such as:
- diabetes (high blood sugar)
- hypertension (high blood pressure)
- heart or kidney problems
- an infection of the amniotic membranes or vaginal or urinary tracts
Babies also may be born early if:
- there's bleeding, often due to a low-lying placenta (placenta previa) or a placenta that separates from the womb (placental abruption)
- the mother's womb is not shaped typically
- they're part of a multiple birth (twins, triplets, or more)
- their mother was underweight before pregnancy or didn't gain enough weight during pregnancy
- their mother smoked, used drugs, or drank alcohol while pregnant
Does My Baby Need Special Care?
Yes, preemies may have many special needs. Younger and smaller babies tend to have more health problems than babies born closer to their due dates. So they often need care in a neonatal intensive care unit (NICU).
Younger and smaller babies tend to have more health problems than babies born closer to their due dates. So they often need care in a neonatal intensive care unit (NICU).
Why Must My Baby Stay Warm?
Preemies don't have enough body fat to hold their body temperature. Incubators or radiant warmers keep them warm in the NICU:
- Infant warmers: These small beds with heaters over them help babies stay warm while being monitored. Because they are open, the team has easy access to babies to provide care.
- Incubators: These small beds are enclosed by clear, hard plastic. Temperature in the incubator is controlled to keep a baby's body temperature where it should be. Doctors, nurses, and others can give care to the baby through holes in the sides of the incubator.
What Are My Baby's Nutritional Needs?
Breast milk is the best nutrition for all babies, especially preemies. It has proteins that help fight infection. Most preemies can't feed straight from the breast or bottle at first. Mothers pump their milk and it's given to babies through a tube that goes through the nose or mouth and into the stomach.
Most preemies can't feed straight from the breast or bottle at first. Mothers pump their milk and it's given to babies through a tube that goes through the nose or mouth and into the stomach.
If that is not an option, doctors may suggest giving the baby donor milk from a milk bank, which is safe.
If you don't breast feed or pump milk, your baby will get formula. Preemies need more calories, proteins, and other nutrients than full-term babies do. So extra nutrients called fortifiers may be added to pumped milk or specially designed preterm formulas may be used to help your baby grow.
Preemies are fed slowly because they can get necrotizing enterocolitis (NEC), a serious intestinal problem that affects preemies.
Some babies who are very small or very sick get their nutrition through intravenous (IV) feedings called total parenteral nutrition (TPN). TPN has a special mix of nutrients like proteins, carbohydrates, fats, vitamins, and minerals that can fully support a baby’s growth until they can feed.
Doctors and dietitians watch the diets of preemies very carefully and make changes when needed to make sure the babies get the nutrients needed to grow.
What Health Problems Can Happen?
Because their organs aren't fully ready to work on their own, preemies are at risk for health problems. In general, the earlier a baby was born, the greater their chances of health problems.
These problems include:
- anemia, when babies don't have enough red blood cells
- apnea, when a baby stops breathing for a short time; the heart rate may lower; and the skin may turn pale or blue
- bronchopulmonary dysplasia and respiratory distress syndrome, problems with breathing
- hyperbilirubinemia, when babies have high levels of bilirubin, which is produced by the normal breakdown of red blood cells. This leads to jaundice, a yellowing of the skin and whites of the eyes.

- necrotizing enterocolitis, a serious disease of the intestines
- patent ductus arteriosus, a problem with the heart
- retinopathy of prematurity, a problem with the eye's retina
- sepsis infections that babies can get before, during, or after birth
What Else Should I Know?
Preemies often need special care after leaving the NICU, sometimes in a high-risk newborn clinic or early intervention program. Depending on their health, they may need care from specialists, such as doctors who treat problems with the brain and nervous system (neurologists), eyes (ophthalmologists), and lungs (pulmonologists).
Preemies must go to all doctor visits (including well-child checkups), get the vaccines that all babies need to stay healthy, and have routine hearing and eye exams. As your little one grows, doctors will check your baby's:
- growth
- development, including speech and language, learning, and motor skills
- muscle tone, strength, and reflexes
Looking Ahead
Caring for a preemie can be more demanding than caring for a full-term baby.
Take care of yourself by eating well, resting when you can, and getting exercise. Spend one-on-one time with your other children when you can, and get help from others. Look for support from friends, family, and support groups. You also can get support online from groups such as:
- March of Dimes
- Graham's Foundation
- Life's Little Treasures Foundation
- Hand to Hold
Reviewed by: Lynn M. Fuchs, MD
Date reviewed: October 2021
Perinatal Center of the Republic of Tuva - Preterm birth
Normal pregnancy lasts from 37 to 42 weeks, 40 weeks on average. A child born during this period is considered full-term. The date of birth is determined by the first day of the last menstruation and normally occurs 280-282 days after it. The frequency of preterm birth in developed countries is 5-7%, neonatal mortality - 28%. Every year, 15 million premature babies are born in the world. Premature birth (PR) is a complex medical and social problem associated with solving the problems of improving the quality of the subsequent life of children born prematurely and associated with material and economic costs, both for the family and the state as a whole.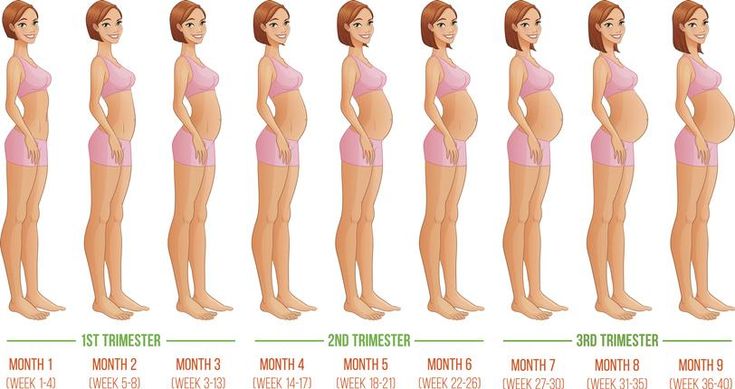 The severity of complications associated with prematurity is proportional to the gestational age of preterm birth
The severity of complications associated with prematurity is proportional to the gestational age of preterm birth
Classification of preterm birth (PR) according to gestational age
- 22-28 weeks (27 weeks 6 days inclusive) - very early PR, 5% of all preterm births. At the same time, newborns are deeply premature, have extremely low body weight (up to 1000 g), pronounced immaturity of the lungs (in some cases, RDS prevention is not very effective). The prognosis for them is extremely unfavorable. Morbidity and mortality rates in newborns are extremely high.
· 28-30 weeks 6 days - early PB, about 15% of all preterm births. Newborns (severe prematurity) are characterized by very low body weight (up to 1500 g), the lungs of the fetus are immature, with the help of corticosteroids it is sometimes possible to achieve their accelerated maturation. The outcome of childbirth for the fetus and postnatal prognosis are more or less favorable.
· 31-33 weeks 6 days - preterm birth, about 20% of all preterm births. Newborns have moderate prematurity.
Newborns have moderate prematurity.
- 34-36 weeks 6 days - late preterm birth, 70% of all preterm births. Infectious incidence of newborns born at 34-37 weeks of pregnancy is significantly lower than those born at an earlier date. Prolongation of pregnancy at this period does not have a significant effect on neonatal mortality rates.
Why are some babies born prematurely?
It is not at all surprising that we do not know the answer to this question, because we still do not know what causes childbirth. How does the fetus know that it is time to leave the mother's body and start an independent life?
Causes of fetal growth retardation:
ü complications of pregnancy; placental insufficiency;
infections in the mother and/or fetus;
diseases/malformations/chromosomal disorders; mother smoking.
The most obvious causes of preterm labor are known. The most important are preeclampsia, bleeding during pregnancy, stress or strenuous physical work, infections in the woman, cervical weakness, multiple pregnancies, premature rupture of water, malformations, infections (especially viral) or other fetal diseases. High blood pressure and pregnancy complications can also lead to preterm labor. According to some reports, the tendency to early birth can be inherited: mothers who were born prematurely are more likely to have a premature birth. However, in about half of the cases, the cause of preterm labor remains unknown. Stress and hard physical work can hardly be quantified. However, there are studies that show that stress (for example, the death of close relatives, job loss or divorce) can lead to premature birth.
High blood pressure and pregnancy complications can also lead to preterm labor. According to some reports, the tendency to early birth can be inherited: mothers who were born prematurely are more likely to have a premature birth. However, in about half of the cases, the cause of preterm labor remains unknown. Stress and hard physical work can hardly be quantified. However, there are studies that show that stress (for example, the death of close relatives, job loss or divorce) can lead to premature birth.
Causes of preterm birth:
- bleeding during pregnancy;
stress;
complications of pregnancy;
heavy physical work;
weakness of the cervix;
infections in mother and fetus;
multiple pregnancy; early discharge of water;
ü heredity
ü and others.
Infection in women, especially urinary tract infection, may precipitate preterm labour. Often, such infections are asymptomatic and the woman does not know that she is sick. It is possible that certain types of bacteria release chemicals that increase prostaglandin production in the uterus. Prostaglandins are lipid substances and can be found in various parts of the body. They act on the involuntary muscles and cause contraction or relaxation. In other words, they can cause contraction of the muscles of the uterus and provoke the onset of preterm labor. Prostaglandins have other functions, in particular, they are involved in the development of fetal circulation. Weakness of the cervix causes preterm birth in about 20% of cases. In the presence of such a diagnosis, it is possible to strengthen the surrounding tissues with a thin thread (circle). This prevents premature opening of the cervix. Pregnancy with three or four fetuses also increases the chance of preterm birth. The frequency of multiple pregnancies increases with the use of certain fertility treatments. There is too little space for the fetus in the uterus, which can lead to an earlier than normal start of labor.
It is possible that certain types of bacteria release chemicals that increase prostaglandin production in the uterus. Prostaglandins are lipid substances and can be found in various parts of the body. They act on the involuntary muscles and cause contraction or relaxation. In other words, they can cause contraction of the muscles of the uterus and provoke the onset of preterm labor. Prostaglandins have other functions, in particular, they are involved in the development of fetal circulation. Weakness of the cervix causes preterm birth in about 20% of cases. In the presence of such a diagnosis, it is possible to strengthen the surrounding tissues with a thin thread (circle). This prevents premature opening of the cervix. Pregnancy with three or four fetuses also increases the chance of preterm birth. The frequency of multiple pregnancies increases with the use of certain fertility treatments. There is too little space for the fetus in the uterus, which can lead to an earlier than normal start of labor. In a pregnancy with three or four fetuses, delivery usually occurs by caesarean section 6 or more weeks before the term, depending on the condition of the fetuses.
In a pregnancy with three or four fetuses, delivery usually occurs by caesarean section 6 or more weeks before the term, depending on the condition of the fetuses.
Diseases and injuries in premature babies
The boundary between disease and damage in a premature baby is very arbitrary, since the child is not yet mature and can easily be damaged by the treatment used for certain diseases. We know that too much oxygen can sometimes be dangerous for a child's eyes, and the use of a ventilator can damage the lungs. At the same time, it is known that in some children, damage occurs regardless of the use of oxygen or artificial ventilation. Therefore, it is not always possible to say what occurs due to the disease, and what is independent of it.
The greatest danger for premature babies is pulmonary disorders. The most common respiratory distress syndrome (RDS) occurs due to the immaturity of the lungs. Other lung diseases include pneumonia and bronchopulmonary dysplasia (BPD). BPD is lung damage that occurs, among other things, as a reaction to artificial ventilation and the use of oxygen. As we already know, the lungs can provide respiratory function starting from the 22-24th week of pregnancy. At 28–30 weeks, alveoli begin to develop. The number of alveoli continues to increase, and the lungs grow until the age of 8–10 years of age. This is what causes lung function to improve with age, even if it was damaged in the neonatal period
BPD is lung damage that occurs, among other things, as a reaction to artificial ventilation and the use of oxygen. As we already know, the lungs can provide respiratory function starting from the 22-24th week of pregnancy. At 28–30 weeks, alveoli begin to develop. The number of alveoli continues to increase, and the lungs grow until the age of 8–10 years of age. This is what causes lung function to improve with age, even if it was damaged in the neonatal period
Pneumothorax - air in the pleural cavity As is well known, mechanical ventilation can have a damaging effect. Too much pressure with which air and oxygen enter the lower respiratory tract can lead to rupture of the alveoli. In this case, the air flows into the thin space between the alveoli. If this continues long enough, a hole may develop in the lung sac (pleura) and air will begin to accumulate in this space. In this case, a so-called pneumothorax occurs. The lungs collapse and oxygen saturation drops sharply within minutes. Pneumothorax occurs not only as a complication of treatment, but also spontaneously, including in children who have not received artificial ventilation.
Pneumothorax occurs not only as a complication of treatment, but also spontaneously, including in children who have not received artificial ventilation.
Arterial duct. The earlier a child is born, the more difficult it is for him to close the ductus arteriosus (see p. 25, Fig. 5). If at the same time the lungs of a premature baby have not matured and he needs artificial ventilation, the closure of the ductus arteriosus is even more difficult. Immediately after delivery, pulmonary artery pressure continues to be high. This prevents large amounts of blood from entering the lungs. However, 4-5 days after birth, the pressure in the pulmonary vessels drops, and if at this moment the ductus arteriosus is still open, blood flows from the aorta to the lungs and heart. This causes the blood flow to the lungs to increase, and this greatly increases the workload on the lungs and heart. If the child is connected to a ventilator, then the doctor often has to increase the airway pressure and oxygen concentration.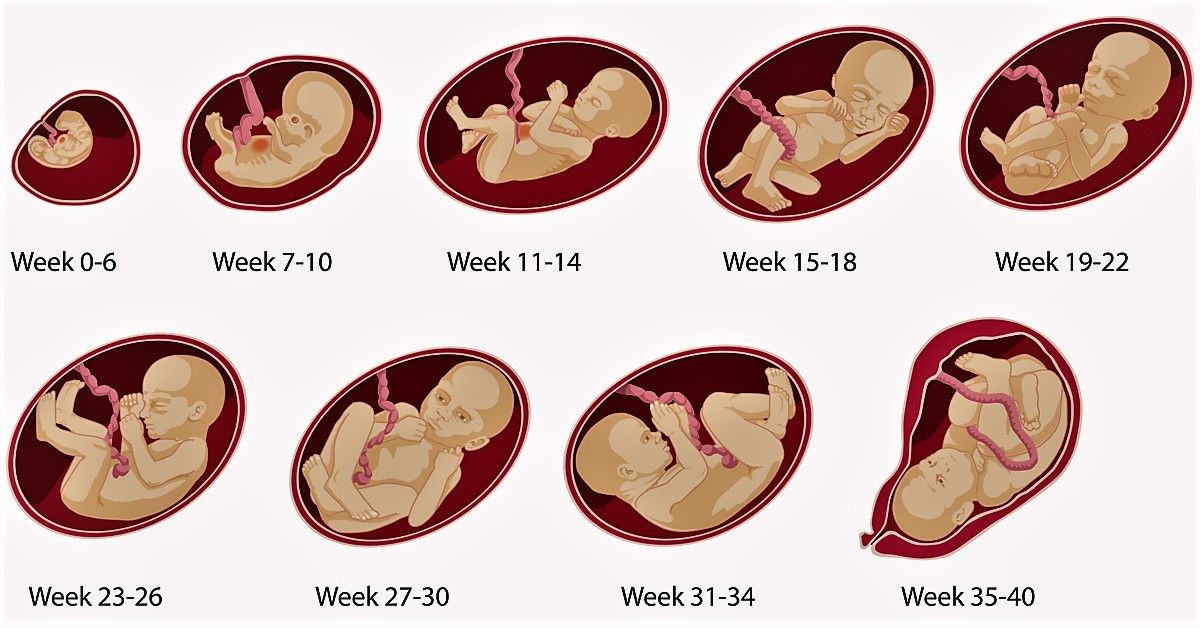 The condition of children often becomes unstable; they experience drops in heart rate, and they endure swaddling and other procedures worse than before.
The condition of children often becomes unstable; they experience drops in heart rate, and they endure swaddling and other procedures worse than before.
Respiratory arrest (apnea). In premature babies, the respiratory center in the brain is often not fully formed. Respiratory movements originate and are regulated in the respiratory center of the brainstem. If a person does not breathe often enough, as a rule, this is compensated by deeper breathing. In premature babies, this skill is not yet developed. Therefore, they often stop breathing. All babies, both premature and full-term, breathe unevenly. They have periods when they breathe too fast, and after that there is a period of slow breathing. This is fine. If the pauses in breathing last more than 10-15 seconds, this is called apnea. If apnea occurs very often, it can be dangerous for the child. Most often they occur in the 1st-2nd week of life and in some children they can last quite a long time. However, eventually the child grows up and the apnea stops.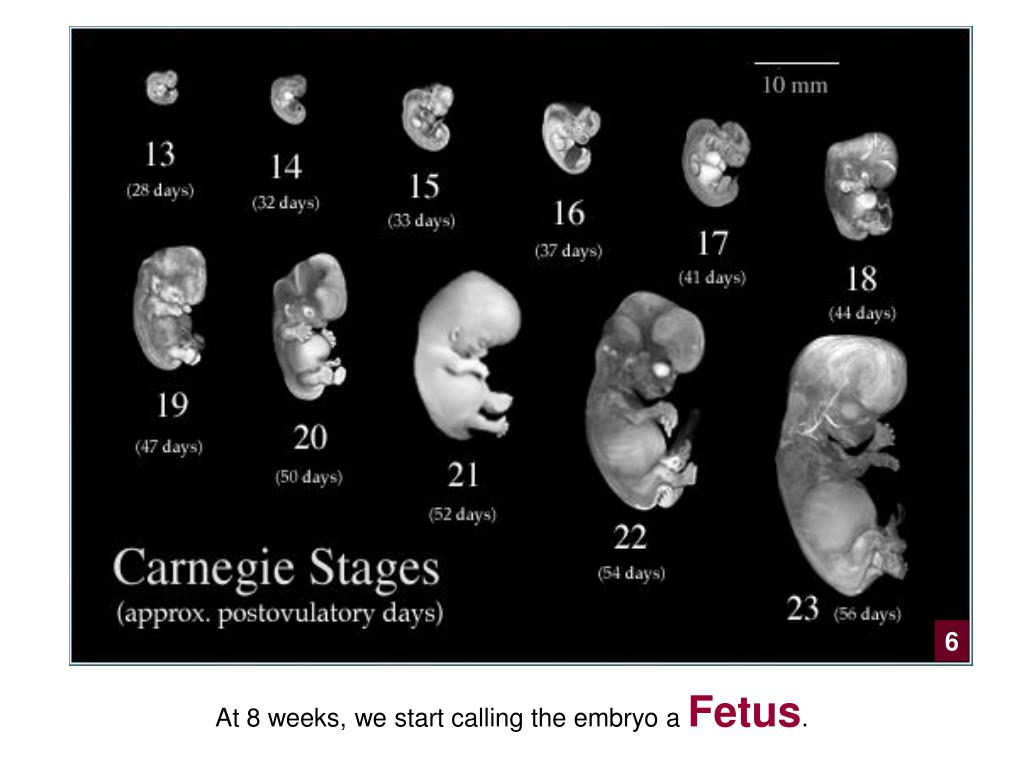
Infections. Inflammation of the lungs and sepsis (blood bacterial infection) Premature babies are more likely to develop infections than anyone else. One reason for this is the immaturity of the immune response. The body's own antibodies (immunoglobulins) are not produced in sufficient quantities, and compared to full-term babies, premature babies receive relatively few antibodies from their mothers. Full-term babies receive large amounts of antibodies from their mother a week before birth; if the baby is born earlier, the amount of antibodies remains low. White blood cells, which play an important role in protecting against infection, may also not fully mature. In addition, it is known that many preterm births are caused by infection; therefore, some babies are already infected at birth. Symptoms may appear gradually and may include decreased appetite and slow weight gain; perhaps the child needs more oxygen and is unstable.
Urinary and other infections. Urinary tract infections may occur in premature babies. In rare cases, this occurs due to congenital anomalies of the kidneys and urinary tract. If an infection is suspected, the urine is always tested for bacteria, and if a urinary tract infection is present, a thorough examination, such as by ultrasound, is always done. Also, the child may develop inflammation of the meninges and other infections. If inflammation of the meninges is suspected, which occurs in rare cases, a lumbar puncture (a puncture into the spinal canal) is performed and the cerebrospinal fluid is examined for the presence of bacteria and white blood cells. The principle treatment of these infections coincides with the treatment of pneumonia and sepsis. One reason for this is that localized infections such as pneumonia and urinary tract infections in preterm infants often become generalized and end in sepsis (bacteria in the blood). That is why it is often impossible to differentiate different infections (such as pneumonia, sepsis, urinary tract infections or inflammation of the meninges) from each other, the symptoms of the diseases are very similar.
Urinary tract infections may occur in premature babies. In rare cases, this occurs due to congenital anomalies of the kidneys and urinary tract. If an infection is suspected, the urine is always tested for bacteria, and if a urinary tract infection is present, a thorough examination, such as by ultrasound, is always done. Also, the child may develop inflammation of the meninges and other infections. If inflammation of the meninges is suspected, which occurs in rare cases, a lumbar puncture (a puncture into the spinal canal) is performed and the cerebrospinal fluid is examined for the presence of bacteria and white blood cells. The principle treatment of these infections coincides with the treatment of pneumonia and sepsis. One reason for this is that localized infections such as pneumonia and urinary tract infections in preterm infants often become generalized and end in sepsis (bacteria in the blood). That is why it is often impossible to differentiate different infections (such as pneumonia, sepsis, urinary tract infections or inflammation of the meninges) from each other, the symptoms of the diseases are very similar.
Jaundice . All newborns have a tendency to develop jaundice. It usually appears after a couple of days and peaks at 2–4 days of life in term infants and 5–7 days of life in premature infants. Jaundice occurs in approximately 80% of preterm infants, and the incidence correlates with the degree of prematurity. There are three main causes of neonatal jaundice. First, a child is born with a much larger number of red blood cells (erythrocytes) than remains in a person later in life. Second, a newborn baby's red blood cells are destroyed much faster than those of older children and adults. In the process of destruction, a yellow dye is formed - bilirubin. Hemoglobin is a protein that fills red blood cells and is necessary for the transport of oxygen. When destroyed, this substance turns into bilirubin, which is further converted in the liver into a water-soluble form and excreted through the gallbladder into the intestine. Bilirubin gives color to feces. During fetal development, bilirubin is excreted through the placenta. The third reason for the development of jaundice in newborns is the immaturity of the liver and, accordingly, the inability to convert and remove all bilirubin through the biliary tract. Bilirubin then enters the blood and tissues of the body, such as the skin, and gives them a yellow tint. Premature babies have even more immature livers and are therefore more prone to jaundice than full-term babies.
The third reason for the development of jaundice in newborns is the immaturity of the liver and, accordingly, the inability to convert and remove all bilirubin through the biliary tract. Bilirubin then enters the blood and tissues of the body, such as the skin, and gives them a yellow tint. Premature babies have even more immature livers and are therefore more prone to jaundice than full-term babies.
Low hemoglobin level in premature babies . The level of hemoglobin in premature and full-term babies is almost the same, but in very preterm babies it is usually slightly lower. Within a few hours after birth, the hemoglobin level rises slightly and on the first day of life averages 184 g / l. After that, the hemoglobin level slowly decreases and reaches a minimum at the 6-8th week after birth.
Anemia of prematurity. In premature babies, the hemoglobin level decreases faster and more severely than in babies born at term. This is because the lifespan of blood cells in preterm infants is shorter compared to blood cells in term infants. In addition, preterm infants may have lower levels of erythropoietin production. Erythropoietin is a hormone that stimulates the formation of red blood cells. The low rate of formation leads to the development of a form of anemia, which is called anemia of prematurity.
In addition, preterm infants may have lower levels of erythropoietin production. Erythropoietin is a hormone that stimulates the formation of red blood cells. The low rate of formation leads to the development of a form of anemia, which is called anemia of prematurity.
Inflammation of the intestine - necrotizing enterocolitis (NEC). Premature babies are predisposed to developing intestinal inflammation (necrotizing enterocolitis - NEC). The reason for this phenomenon is unknown. The disease is more common in the US than in Scandinavia. This may be because children in Scandinavia are more likely to be breastfed than in the United States. Studies have shown that necrotizing enterocolitis is more likely to occur in children who receive formula (artificial nutrition) instead of mother's milk. In addition, it is suggested that infections can also contribute to the development of the disease.
Cerebral hemorrhage. The greater the degree of prematurity, the higher the risk of hemorrhage. One of the reasons for this is the tight fit of the area around the cavity of the brain ventricle to the blood vessels during fetal development. Vessels are very fragile, and very little force is required to break them. This vascular system undergoes reverse development around the 35th week of pregnancy and most often completely disappears by childbirth. Therefore, most babies born before the 35th week of pregnancy are prone to hemorrhages. Initially, it was believed that with a hemorrhage in a child, brain damage necessarily occurs. Later it was found that in most cases no lesions develop.
One of the reasons for this is the tight fit of the area around the cavity of the brain ventricle to the blood vessels during fetal development. Vessels are very fragile, and very little force is required to break them. This vascular system undergoes reverse development around the 35th week of pregnancy and most often completely disappears by childbirth. Therefore, most babies born before the 35th week of pregnancy are prone to hemorrhages. Initially, it was believed that with a hemorrhage in a child, brain damage necessarily occurs. Later it was found that in most cases no lesions develop.
Eye damage - retinopathy of prematurity (RP). it is known that too high an oxygen concentration can cause eye damage in premature babies. In the most severe cases, damage can lead to blindness (called cavern blindness). Initially, the condition was called retrolental fibroplasia, which means the ingrowth of fibrous tissue into the lens of the eye. The condition was later determined to vary in severity, from mild to severe, in the form of blindness. Currently, the disease is called "retinopathy of prematurity" (English retinopathy of prematurity, abbreviated RH). This means that the disease primarily affects the retina of the eye (retina) of premature babies.
Currently, the disease is called "retinopathy of prematurity" (English retinopathy of prematurity, abbreviated RH). This means that the disease primarily affects the retina of the eye (retina) of premature babies.
What is the department of pathology of newborns and premature babies?
The Department of Pathology of Newborns and Premature Babies provides specialized round-the-clock care for newborn premature babies and children with any diseases.
Why is it necessary to place a child in a neonatal and premature infant pathology unit?
Premature babies need extra care and attention to catch up with the growth and development that should have taken place in utero. For example, it is more difficult for a premature baby to keep warm because the baby is not yet able to regulate its own body temperature. This requires a special crib or incubator.
If the baby is still too small, weak and unable to eat, he can receive the necessary nutrition through intravenous drip or through a tube that brings milk into the baby's stomach.
Premature babies also need additional monitoring, treatment and care. They are still very vulnerable and can have serious health problems. Common health problems in premature babies:
- breathing problems;
- cerebral hemorrhage;
- unsatisfactory condition of the heart;
- bowel disorder, indigestion;
- vision problems;
- jaundice;
- anemia;
- infections.
Who will take care of the baby in the department of pathology of newborns and premature babies?
- Senior nurse.
- Neonatologists who see your baby.
- Other specialized doctors, such as surgeons, radiologists, who are called from other departments for consultations.
- Nurses caring for children.
- Mistress and junior staff who also help and support the work of the department, wash, generals, prepare diapers, feed mothers, etc.
- Other specialized support units such as kitchen, laundry, housekeeping, etc.

- Last but not least on the list - parents, relatives. Parents are the main responsible for taking care of the child. Doctors understand this and treat them as part of a team. Mothers should be more actively involved in child care.
Here is a list of some of the equipment used to bring premature babies to the neonatal and preterm infant pathology department:
Baby warmers
humidity. Some types of incubators have a lid. Some incubators are equipped with an additional heating element, which is located above the baby.
Tubes
A thin surgical needle can be inserted into a child's vein and connected to a tube to inject fluids, medicines, and nutrition that the baby needs.
An infusion pump is a device that helps inject the necessary drugs and liquids through a tube at a certain rate and frequency.
If the baby is not yet ready to be fed from mother's breast or from a bottle, a stomach tube will deliver milk directly to the baby's tummy. The nurse will gently insert a soft, flexible tube through the child's mouth or nose into the stomach when the child does not yet know how to swallow or synchronize breathing with swallowing.
The nurse will gently insert a soft, flexible tube through the child's mouth or nose into the stomach when the child does not yet know how to swallow or synchronize breathing with swallowing.
Special light beams
Most premature babies develop jaundice, which can be treated with phototherapy. Their skin turns yellow because a substance called bilirubin is produced faster than the baby's body can excrete it.
Under the influence of these rays, the bilirubin produced in the baby's body is converted into a harmless substance until the baby's body is able to do it on its own. With the help of phototherapy, bilirubin is converted into a form that is much faster excreted from the body. During this procedure, the child is placed under a phototherapy lamp, a special mask is put on to protect the eyes.
Kangaroo method
As soon as the baby gets stronger, one of the effective ways to help him will be the so-called kangaroo method. The parent simply holds the child under their clothing, ensuring skin-to-skin contact. When using the kangaroo method, the baby calms down, his well-being improves, development processes are accelerated.
When using the kangaroo method, the baby calms down, his well-being improves, development processes are accelerated.
Research has shown that using the kangaroo method can reduce the risk of infections, help you breastfeed and bond with your baby.
Feeding the baby
Nurses help the mother to express breast milk until the baby is strong. Breastfeeding a premature baby can help develop his brain and help fight disease. Breastfed babies are discharged from the hospital earlier.
Caring for the baby
It may take a long time for the baby to get stronger and parents to be able to do their normal parenting duties such as feeding, changing, helping with bathing and grooming, changing diapers.
When can my child be discharged from the hospital?
It depends on the condition of the individual baby. The condition of children, whose weight (weight) and sizes are smaller, who were born earlier, as a rule, is associated with a large number of problems. They, in most cases, stay in the department of pathology of newborns and premature babies longer.
They, in most cases, stay in the department of pathology of newborns and premature babies longer.
A premature baby who, on the contrary, feels better, usually stays in the pathology of newborns and premature babies until the expected date of birth. If the child's condition is really good, he can be discharged earlier.
Criteria for Prematurity
When a baby is born prematurely, it does not have one age like a normal baby, but three.
1) According to the child's birth certificate, say, a month, this is official data.
2) The second age is called post-conceptual: we consider the duration of pregnancy, which should not yet end in childbirth. If the baby was born at the 28th week of pregnancy, in a month we consider that the 32nd week is coming.
3) Then, when he grows up to the day he was supposed to be born, we will start counting the third age, corrected. That is, a child can be three months old according to the birth certificate, and his corrected age is one week.
Neonatologists have complicated calculations. They are needed to make discounts for development. A child who was born at 28 weeks has the right to not be able to do what a full-term baby can do in three months. Up to a year, these things are taken into account necessarily. Of course, children weighing less than a kilogram are the most difficult. They necessarily go through the stage of resuscitation until they are able to provide for themselves to a certain extent. When the apparatus no longer breathes for them, when they are fed through the stomach, and not through the vein, when the heart works as expected, they come to our department. Parents are harder to work with than kids. Sometimes there are often more problems with the health of the mother (including mental health in the postpartum period of premature birth) than the child. All people are different. Parental maturity does not always depend on age. There are 18-year-old mothers who are ready for motherhood. It happens that women in their thirties or forties do not understand either do not want to understand and accept the child's illness, and this harms him, often refusing treatment or staying next to the child in the neonatal pathology department, thereby further exacerbating the difficulties already existing in their family. A child with such an attitude of his mother towards him, even if he is fed and cared for in time, will not recover well. He needs to feel that his mother is taking care of him. Even a little contact between mother and child, even if it is important in the incubator. The source of the material are:
A child with such an attitude of his mother towards him, even if he is fed and cared for in time, will not recover well. He needs to feel that his mother is taking care of him. Even a little contact between mother and child, even if it is important in the incubator. The source of the material are:
- National Guide to Neonatology \ \ N. N. Volodin-M.-2017
- Manual of perinatology / ed. BEFORE. Ivanov - St. Petersburg: Inform - Navigator, 2015
- Maternal and child health service in 2016 / Collection of the Ministry of Health of the Russian Federation.
- Shabalov, N. P. Neonatology - M. : MEDpress-inform, 2016.
- Sources from the Internet.
"His organs and systems are not ready" Why in Russia they are trying to save children who have almost no chance to survive and be healthy: Society: Russia: Lenta.ru
In Russia, it was proposed to register only from the seventh day babies who were born very early (less than 22 weeks) and with extremely low birth weight (less than 500 grams). This happened after a series of criminal cases that the Investigative Committee initiated against obstetricians. So, neonatologist Elina Sushkevich from Kaliningrad was accused of killing a 22-week-old boy. Why are they trying to save 500-gram children in Russia at all today, what are their chances of surviving and whether they can grow up healthy - Lenta.ru learned from the doctor of medical sciences, head of the scientific department of neonatology and pathology of young children at the Research Clinical Institute of Pediatrics named after Yu.E. Veltishchev Elena Keshishyan.
This happened after a series of criminal cases that the Investigative Committee initiated against obstetricians. So, neonatologist Elina Sushkevich from Kaliningrad was accused of killing a 22-week-old boy. Why are they trying to save 500-gram children in Russia at all today, what are their chances of surviving and whether they can grow up healthy - Lenta.ru learned from the doctor of medical sciences, head of the scientific department of neonatology and pathology of young children at the Research Clinical Institute of Pediatrics named after Yu.E. Veltishchev Elena Keshishyan.
***
Lenta.ru: Now the minimum criteria for saving premature babies are 22-23 weeks and 500 grams of weight. Why?
Elena Keshishyan : In order to understand the limit of possibilities both in technical terms (creation of an environment close to intrauterine), and in terms of the maturity of the child's brain, which is able to develop out of utero, attempts were made in the world to give birth to premature babies of different ages. The greatest successes in this were achieved by the Japanese. They tried out babies born at 20 weeks. That is, the approximate gestational age was five months. The Japanese succeeded, but in isolated cases. And they saw that in children born at this age there is no differentiation of the brain, division into gray and white matter. Roughly speaking, this process determines the ability to think, to feel. This is called higher nervous activity. It is this ability that distinguishes man from animals.
The greatest successes in this were achieved by the Japanese. They tried out babies born at 20 weeks. That is, the approximate gestational age was five months. The Japanese succeeded, but in isolated cases. And they saw that in children born at this age there is no differentiation of the brain, division into gray and white matter. Roughly speaking, this process determines the ability to think, to feel. This is called higher nervous activity. It is this ability that distinguishes man from animals.
Therefore, guided by research data and on the basis of a humanistic idea, the World Health Organization has established this limit for human live birth - 23 weeks, which corresponds to approximately 500 grams of weight. This is the minimum age at which the brain can differentiate into gray and white matter. And, accordingly, there is hope that it will already be a human person with mental abilities.
Countries with technological capabilities, including Russia, have agreed that those born at this gestational age can legally be considered human. That is, they have all human rights, including medical care.
That is, they have all human rights, including medical care.
Since 2012, Russia has moved to the WHO criteria for nursing premature babies. How many of these children have been saved during this time?
As a percentage of all those born, this is a minuscule amount. I don't have exact numbers. But I want to say that the body of children born almost half prematurely is very immature. And their survival rate, conditionally, is one in a hundred. Still, 22-23 weeks is not childbirth in the full sense. From the point of view of nature, this is a miscarriage, this is a critical situation that may be associated with the health of the mother or the sick child herself. Therefore, the readiness for independent existence in such fruits is close to zero. Even if we assume that the maximum efforts of doctors are thrown to save the child, all the necessary equipment is connected, the chance that he will get out is very small. In such an infant, the kidneys, gastrointestinal tract, heart and other organs may not work. This is a very, very complex, jewelry work of doctors.
This is a very, very complex, jewelry work of doctors.
One of the smallest surviving premature babies in the world. Amilya Taylor was born in 2006 in Miami, USA. She spent only 22 weeks in the womb and was born with a weight of 284 grams and a height of 24 centimeters.
Photo: Baptist Health South Florida / Reuters
And dear?
Of course. A day in a well-equipped neonatal intensive care unit costs several thousand dollars. And to leave such a child, months are needed. But I want to emphasize that the number of survivors in this period is minimal. And it is minimal in almost all countries where the WHO criteria apply.
If these children are not viable, cost too much, then why were these criteria established?
The medical task here is not at all to save without exception all children born at a term of five months. It is clear that there is not a single person who does not understand that this child is at risk of being blind, deaf and immobilized. The task of medicine in this situation is to acquire knowledge and experience.
The task of medicine in this situation is to acquire knowledge and experience.
Obstetricians learn how to prolong pregnancy as much as possible. There is a whole range of activities: prenatal diagnosis of genetic chromosomal diseases, various fetal malformations, identification of risk groups among pregnant women, their special monitoring, prenatal logistics and routing. They also hone the ability to properly take birth at this time. This must be done as carefully as possible and do not forget about the "golden hour". It is necessary to have time to give the child, without waiting until his condition worsens, what he could not get from his mother. That is, even if the child screamed, you need to understand that soon he will stop doing this and will not be able to breathe. The "golden hour" essentially determines whether or not there will be damage to brain cells. This means whether or not a child will have a full life.
And the qualifications of resuscitators working with such children are growing today. All this led to an important point: the quality of nursing of children born a little later, at 26-28 weeks, has become much better. I see these babies regularly. And I can say that over time, many of them are no different from their peers.
All this led to an important point: the quality of nursing of children born a little later, at 26-28 weeks, has become much better. I see these babies regularly. And I can say that over time, many of them are no different from their peers.
And before?
About 30 years ago, about six or seven out of ten children would have become severely disabled. And today I had three 26-week-old babies at my appointment. And everyone is developing quite well, there is a slight backlog, but they will catch up. These children no longer have those possible malformations that, unfortunately, would have necessarily arisen in past years.
And this became possible thanks to the experience, the accumulation of knowledge about how such babies develop. There are no small things. This applies to everything - how to evaluate the heartbeat, how to interpret blood tests, and so on. Caring for a premature baby, both in the neonatal period and later, in the first or second year of life, is not the same as managing a normal, full-term baby. But knowledge allows timely adjustment of development, without even waiting for problems.
But knowledge allows timely adjustment of development, without even waiting for problems.
Photo: Science Photo Library / East News
It is important to understand that a premature baby is not a small copy of a normal one. This is a child who is forced to adapt to extrauterine life, when physiologically he should not do this. Its organs and systems are not prepared to function in the new conditions.
"This is painful love at the level of deep depression"
What do such children most often suffer from?
One of the typical pathologies is retinopathy of prematurity. In children, the mechanism that protects the eye from light has not yet matured. And they experience a real shock, suddenly falling into our bright world. Photons of light and the flow of oxygen begin to act on the retina, its vessels begin to grow rapidly, penetrate all the media of the eye, and, ultimately, exfoliate the retina, leading to total blindness. Earlier, even when I was just starting to work, although we knew about such a disease as retinopathy of prematurity, there were few children born and surviving at gestational ages of less than 30 weeks. Therefore, no one knew how to treat this disease. It's scary to remember, but premature babies were in wards with round-the-clock lighting. The light was needed so that doctors and nurses could observe the baby's condition and notice changes in time. At that time, six out of ten children whose birth weight was less than a kilogram went blind. Just then, the borders were opened in Russia, and we were amazed that in Europe, a maximum of two out of ten newborns had blindness.
Therefore, no one knew how to treat this disease. It's scary to remember, but premature babies were in wards with round-the-clock lighting. The light was needed so that doctors and nurses could observe the baby's condition and notice changes in time. At that time, six out of ten children whose birth weight was less than a kilogram went blind. Just then, the borders were opened in Russia, and we were amazed that in Europe, a maximum of two out of ten newborns had blindness.
But we started learning very quickly. Now in perinatal centers in all intensive care units for premature babies - twilight. The cuveuses are completely covered with dark blankets. The staff does not need to watch the baby all the time - all readings are automatically recorded by special devices. In good ICUs, nurses who approach babies have headlights. This is to avoid disturbing other children. In many intensive care units, a large “ear” hangs. If the decibel level in the room begins to exceed the allowable limit, the device lights up red.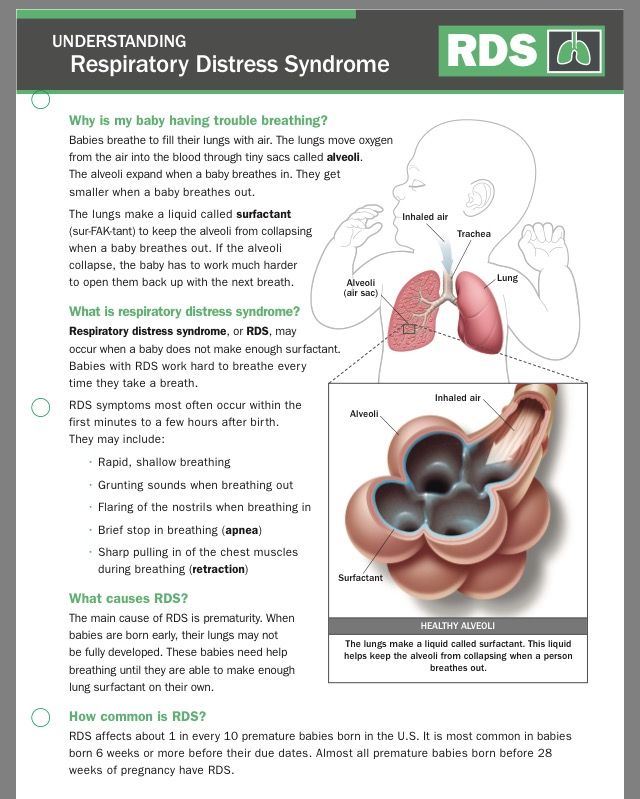
After the birth of the child, every week they begin to look at the eyes with a special method. If there is proliferation of blood vessels, laser coagulation of the retina is performed. There are specialists in such operations in almost every major city.
Approximately 400-600 babies pass through me every year, born at 26-28 weeks. Over the past few years, not a single blind person has been among them. Although earlier in hospitals for such newborns it was necessary to open entire departments.
Is there any data on how many premature babies later became healthy?
Now, among premature babies born at five or six months (25-26 weeks of pregnancy), 25-30 percent become disabled. The same is true in developed countries. And even 20-30 years ago there were 75-80 percent of them.
The risks for these children are still very high. They require long-term observation and treatment. But still today they have incommensurably or better chances than before.
Photo: East News
Do unfortunate parents regret insisting on resuscitation at all costs?
As a doctor, no one has ever told me this. Naturally, the families had very different hopes for childbirth. In the doctor's office they cry, but they don't moan. These children are madly loved. But this is painful love at the level of deep depression. Probably, some of these mothers may think at night what would happen if they knew in advance how everything would turn out. Perhaps they voice this to their mothers, husbands, girlfriends ... But not to doctors. This is where people prefer to stay.
When a child is one or two years old, from a moral point of view, the situation is more difficult than in three days. Newborns are all wonderful bags, it is only then that children begin to differ from each other. These families have a very specific and difficult life. When a child lies at home, does not move, does not swallow, never looks at you, does not speak - this is very difficult. And parents need to be helped to turn their life into at least a relatively social one, not to make them outcasts.
And parents need to be helped to turn their life into at least a relatively social one, not to make them outcasts.
What family support can I expect now?
When Russia switched to WHO standards, doctors began to say that if we started caring for such children, there would be a high incidence of cerebral palsy, mental retardation and other pathologies leading to severe disability. Without the development of a specialized service that will help such children, we will inflict enormous damage on a society that will not accept such an increase in the number of people with disabilities. Then a follow-up system for premature babies began to develop, which leads them up to three years. Because in the usual polyclinic network there are not always doctors who understand how a child born with low or extremely low body weight grows and develops. In parallel with this, the system of medical rehabilitation is developing quite rapidly.
The worst situation is with the social service. Help for these children is minimal. Few people explain to families how to care for such a child, how to develop him, how to maintain motor skills. If in large cities at least some minuscule can be achieved, then what can we say about the province? All this turns one of the parents out of social life. There are no places where it would be possible to transfer such a child at least for a week, a month, so that the parents could have a little rest. Since the state has taken such a step, since we have legally recognized a 500-gram fetus as a person, then they themselves also need to act humanly in the future with his family.
Help for these children is minimal. Few people explain to families how to care for such a child, how to develop him, how to maintain motor skills. If in large cities at least some minuscule can be achieved, then what can we say about the province? All this turns one of the parents out of social life. There are no places where it would be possible to transfer such a child at least for a week, a month, so that the parents could have a little rest. Since the state has taken such a step, since we have legally recognized a 500-gram fetus as a person, then they themselves also need to act humanly in the future with his family.
Is there a support system in other countries?
I know that in Europe and in the USA it is built very well. The emphasis is not on medical rehabilitation, but on social rehabilitation. They have social workers who come and relieve these families of a significant part of their worries. Somewhere there are social centers where a child can be taken to a kindergarten. Moreover, they are zoned - parents do not need to go to the other end of the city.
Moreover, they are zoned - parents do not need to go to the other end of the city.
Photo: Alexander Kondratyuk / RIA Novosti
“Even if it is clear that a child has pathologies that are incompatible with life, they must be saved to the last”
You say that some time ago, kilogram premature babies were also considered “non-residents”, but now they are quite promising. Is it possible that in 30-40 years the same can be said about 500-gram ones?
Indeed, even 30-40 years ago, when it was not possible to maintain breathing, children born before seven months of age survived very rarely.
Then, when some first mechanisms appeared, the bar was raised until the 28th week of pregnancy, which is about six months. But technological progress is always moving forward, and this has allowed us to further gradually reduce the age of survival. We can now at least partially simulate intrauterine conditions. For example, when a child is not born on time, he does not yet have a substance in his lungs, thanks to which he can breathe - surfactants.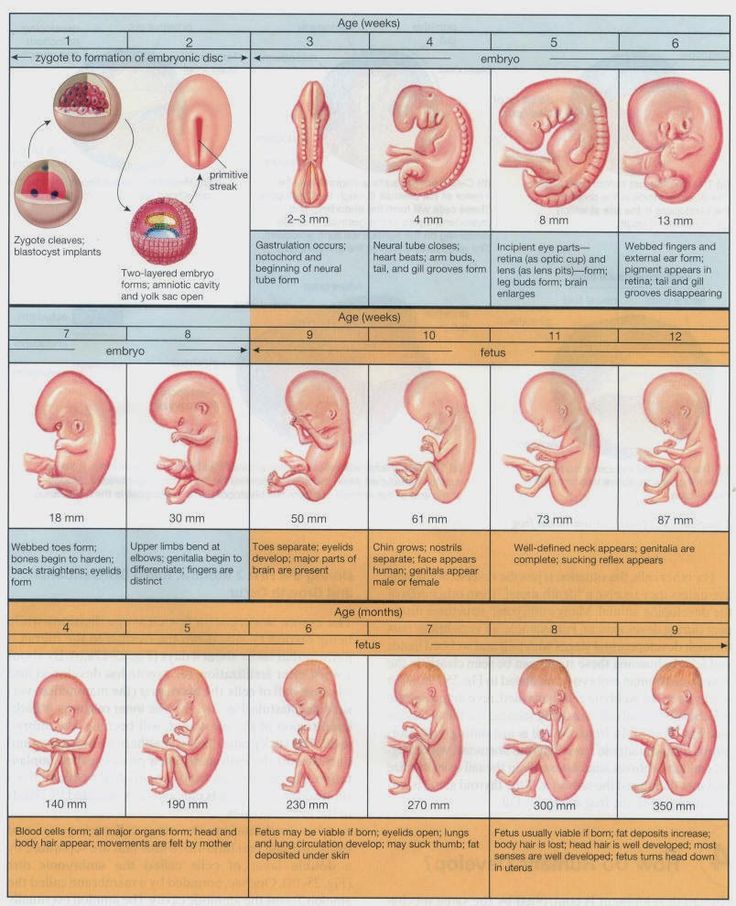 They can be introduced immediately at birth, start artificial ventilation of the lungs and thereby support gas exchange. It also became possible to give nutritional subsidies not through the gastrointestinal tract, but through a vein with special substances that are already ready for inclusion in metabolism. There are many other adaptations: the creation of a thermal regime, humidity close to intrauterine.
They can be introduced immediately at birth, start artificial ventilation of the lungs and thereby support gas exchange. It also became possible to give nutritional subsidies not through the gastrointestinal tract, but through a vein with special substances that are already ready for inclusion in metabolism. There are many other adaptations: the creation of a thermal regime, humidity close to intrauterine.
Technologically, the frontier could move indefinitely. If desired, you can simulate a situation where a woman is not needed at all to bear a child. But I have already said that scientists have established that the age of 22-23 weeks is the minimum period at which the cells of the cerebral cortex can develop postnatally. Still, the main criterion for the normal development of a child is not technological achievements, but the capabilities of the brain.
Is it true that they try to save all 500-gram children only in Russia and Turkey, and in other countries - only if the child has high chances for a normal life?
This is not true. In all countries where the WHO concept has been adopted, these children are subject to mandatory medical care. But there are nuances. If the baby was born between the 23rd and 25th weeks, parents can refuse resuscitation. To do this, in many countries there is a legal standard, reminiscent of the law on euthanasia.
In all countries where the WHO concept has been adopted, these children are subject to mandatory medical care. But there are nuances. If the baby was born between the 23rd and 25th weeks, parents can refuse resuscitation. To do this, in many countries there is a legal standard, reminiscent of the law on euthanasia.
There is a special service in perinatal centers. When it becomes clear that preterm labor has begun, representatives approach relatives - the father and, if possible, the mother. “We assume that a baby will be born with such and such parameters. In this case, there are such and such development risks ... You have the right to choose either full resuscitation or palliative care. And depending on what the parents decide, the doctors act.
Photo: Sergey Pyatakov / RIA Novosti
In Russia, you can also choose a palliative today, right?
This is not prescribed by law. Today, even if it is clear that a child has pathologies incompatible with life, they must be saved to the last. It happens that parents can sign a paper on their own that they would not like resuscitation, but this has no legal force. Parents can say, “Look, he is breathing, breathing. He opened his eyes. Let's revive him now!" And we lost time, which in this case is very important. This child initially has little chance, but it has become even less. And a situation may arise when parents accuse the doctors that their child was not specially treated, “talking teeth”.
It happens that parents can sign a paper on their own that they would not like resuscitation, but this has no legal force. Parents can say, “Look, he is breathing, breathing. He opened his eyes. Let's revive him now!" And we lost time, which in this case is very important. This child initially has little chance, but it has become even less. And a situation may arise when parents accuse the doctors that their child was not specially treated, “talking teeth”.
The medical community is very concerned about this ambiguous position of doctors. And we have a number of proposals to solve the problem of their protection.
What exactly is offered?
Legislative initiative to allow parents to independently decide whether resuscitation care is appropriate for a child born between the 23rd and 25th weeks. Naturally, all this should be discussed. It is necessary to involve the public in the discussion: these are lawyers, doctors, patient communities, representatives of religious denominations.
The Ministry of Health has now prepared new criteria for newborns born too early. In particular, it is proposed not to register such a child until he has lived seven days. Maybe this will fix the situation, protect doctors from murder charges?
There are a lot of pitfalls here. In Russia, there was a similar law on kilogram children. They were assisted from birth, but until the age of seven days the child was considered a fetus. If he died, then his mortality already went into other criteria, it was not considered the death of a newborn.
There are not many children born with extremely low rates, they simply cannot influence the demographic structure in any way. But if there is such a situation that you can not register for up to seven days, it seems to me that even more claims may arise against doctors regarding the failure to provide assistance.
These are very difficult questions. On the one hand, parents can say: you did not save the child. And others, on the contrary, will say: why are you torturing him in vain? And imagine a resuscitator who may be faced with an ethical choice: he has only one ventilator in the hospital, and a 23-week-old baby has been on it for the 40th day. And then a 32-week-old is born in the hospital. He needs help, hold him for three days on the device, and then the baby will cope on his own. In the first case, there will certainly be a disabled person. And in the second - almost healthy. And what should a doctor do?
And then a 32-week-old is born in the hospital. He needs help, hold him for three days on the device, and then the baby will cope on his own. In the first case, there will certainly be a disabled person. And in the second - almost healthy. And what should a doctor do?
Are you speaking theoretically now or do such situations occur?
We cannot have this in federal centers. We have enough equipment. I just illustrated with an example that the issue of nursing such children is the most difficult, all aspects are in common in it - from medical to ethical and religious.
Photo: Sergei Krasnoukhov / RIA Novosti
“The issue of infant mortality has always been political”
The issue of infant mortality has recently become political. Perhaps that is why patient scandals associated with maternity hospitals are developing so sharply?
The issue of infant mortality has always been political. This is a socially significant parameter that determines the position of the country in terms of development. In our country as a whole, infant mortality has significantly decreased over ten years. However, in the last two years the rate of decline has slowed down. Our government says it's bad. From the point of view of doctors, this is not entirely true. There are objective reasons that cannot be overcome with a swoop.
In our country as a whole, infant mortality has significantly decreased over ten years. However, in the last two years the rate of decline has slowed down. Our government says it's bad. From the point of view of doctors, this is not entirely true. There are objective reasons that cannot be overcome with a swoop.
The primary decrease in mortality occurred due to the high-quality saturation of hospitals with equipment, due to the construction of perinatal centers. This gave immediate results. And now these figures have reached a plateau. Another thing is that a plateau, for example, in Kaliningrad, St. Petersburg, is one thing. There mortality rates are at the European level. That is very low. And there are regions where mortality is high - the Altai Territory, the Jewish Autonomous Region, Magadan. There is a lack of doctors, a lack of equipment, very long distances, routing difficulties. And it's very difficult to do anything about it.
We are not compact Switzerland. We have a huge country with difficult geographical conditions. There are regions where we cannot even deliver a woman by helicopter. At one time I spent a lot of time in Chukotka, watching the obstetric service. Often, if a premature baby is born there, you will not help him in any way.
There are regions where we cannot even deliver a woman by helicopter. At one time I spent a lot of time in Chukotka, watching the obstetric service. Often, if a premature baby is born there, you will not help him in any way.
There are no good hospitals there?
Everything is there, but in one city - in Anadyr. And if a woman gave birth in another place, then often she can be cut off from the world. There are periods when even planes do not fly: a snowstorm, something else. And with routing too you will not guess. Because when you are expecting your first child, you are not going to give birth at 24 weeks. This is if the situation with childbirth repeats, then you can plan something, come closer to specialized care at the “dangerous” time ...
Is it true that there have been more premature births lately?
No, their number is stable. This is approximately 7-10 percent of all newborns. Significantly increased their survival rate.
One of the most "inciting" topics on parenting Internet forums is that children who are "culled out" by nature have a bad effect on the quality of the gene pool. Is there any reason to think so?
Is there any reason to think so?
In order for "survivors" to be able to influence the population, there must be a lot of them in percentage terms. For example, there are very few 26-week-olds - no more than two percent of all births. It can't affect anything in any way.
I know that at one time they discussed: what will happen if my child marries in the future someone who was once premature, will the gene pool suffer? Firstly, I can say that, as for children born after the 30th week, they are completely healthy, adapted and no different from others. They themselves give birth to beautiful healthy children, we have already seen many generations. The risk of preterm birth is not inherited. And usually premature babies are shaken, they are a lot of work. So in terms of development, these children can give odds to others.
As for children born at 5-6 months old, when they catch up with their peers, it is important that parents continue their active life with them, and not engage in a protective regime.