Period like cramps at 35 weeks
Pregnancy at week 35 | Pregnancy Birth and Baby
Pregnancy at week 35 | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Your baby
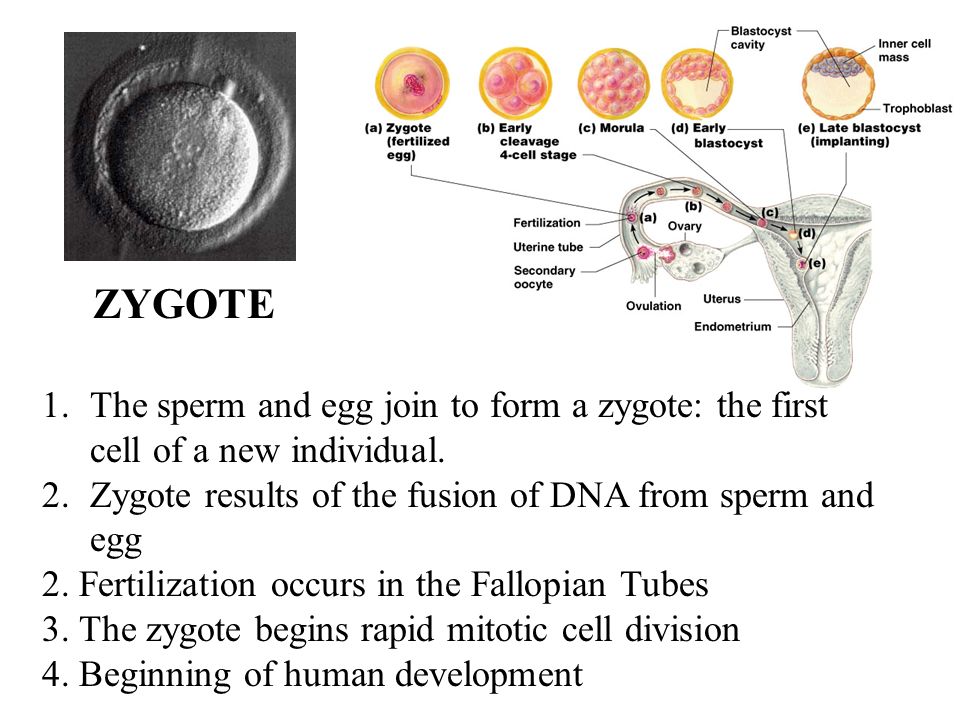
Your baby now weighs more than 2.3kg and measures about 32cm from head to bottom. They are quite cramped and their legs are bent up into their chest, but they can still change position and kick you. They can swallow about a litre of amniotic fluid every day, which is passed as urine.
Don’t worry if your baby is still in the breech position (head up, feet down) – most babies will gradually turn into the head-down position during the last month. If your baby is still in the breech position during the next week or two, your doctor or midwife may try to turn them using a procedure known as External Cephalic Version (ECV).
Your baby at 35 weeks
| Length: | 32cm (head to bottom) |
| Weight: | 2.3kg |
Your body
You may be having a lot of Braxton Hicks contractions by now. They feel like a tightening or cramping in your tummy, and they can happen as often as every 10 to 20 minutes in late pregnancy. They are your body’s way of preparing for the birth and are nothing to be worried about. You can tell if they’re Braxton Hicks and not real contractions because they normally go away if you move position.
They may be real contractions if:
- they get stronger or closer together
- they last longer as time goes by
- they are stronger when you walk
- you feel pain or pressure in your pelvis, abdomen or lower back
If you went into labour now it would be considered premature labour and you would need medical attention straight away. If you’re in doubt, contact your doctor or midwife.
If you’re in doubt, contact your doctor or midwife.
Things to remember
If your pregnancy is high risk, your doctor or midwife will probably want to see you more often from now on.
One serious complication that can develop in late pregnancy is pre-eclampsia. This is usually diagnosed if your doctor notices you have high blood pressure or protein in your urine.
See your doctor straight away if you develop:
- a bad headache
- pain in the tummy
- blurry vision
- sudden swelling of your hands or feet
Read next
Your pregnancy at 36 weeks
Learn about your pregnancy journey and what is happening to you and your baby.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Raising Children Network (Pregnancy week-by-week), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Breech Presentation at the End of your Pregnancy), NHS (You and your baby at 35 weeks pregnant), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: August 2020
Back To Top
Need more information?
Pregnancy at week 34
As at the start of your pregnancy, you’re probably feeling tired and emotional. The baby doesn't have much room to move, but you might feel them kick and roll.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 39
Your baby's weight gain should slow down since they are now ready to be born. You might soon start to notice the early signs of labour.
Read more on Pregnancy, Birth & Baby website
Pregnancy and travel - Better Health Channel
betterhealth.vic.gov.au
Read more on Better Health Channel website
Multiple birth - triplets or more
If you are pregnant with triplets or more, the birth will need careful planning. The main risk is that your babies will be born prematurely. Find out more here.
The main risk is that your babies will be born prematurely. Find out more here.
Read more on Pregnancy, Birth & Baby website
Episiotomy
An episiotomy is a procedure performed during labour to assist with the delivery of your baby.
Read more on Pregnancy, Birth & Baby website
The role of exercise in improving fertility, quality of life and emotional wellbeing
Being in the healthy weight range reduces the risk of infertility and improves the chance of conceiving spontaneously and with assisted reproductive technology (ART).
Read more on Your Fertility website
Undescended testicles - Better Health Channel
betterhealth. vic.gov.au
vic.gov.au
Read more on Better Health Channel website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.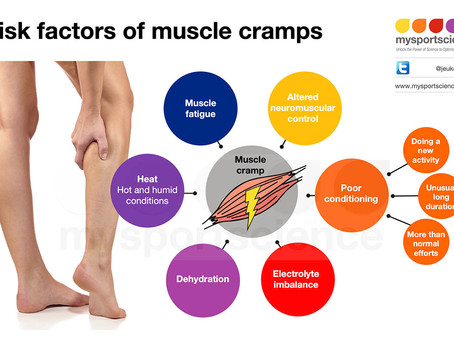
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Pregnancy Risk Preterm Labor
Preterm labor is defined as labor that begins before completion of 36 weeks of pregnancy.
Early warning signs of preterm labor may be subtle and develop slowly. Many symptoms are present during a normal pregnancy. You may not always be able to identify a specific problem; you may just feel that something is different from what you have previously experienced.
As you read the list of signs and symptoms, the question to keep in mind is whether a change has appeared from what has been usual for you:
- Menstrual-like cramps -You may feel dull, aching cramps in the lower part of your abdomen. They may be continuous or come and go in a rhythmic pattern.
- Low backache - The backache you experience in preterm labor is usually located in the lower back. It may come in waves and may travel to the front of your abdomen. This ache is not relieved by changing your position. It may come and go, or seem different from the normal backache you have felt at other times during your pregnancy.
- Abdominal cramps: Abdominal or intestinal cramps, with or without diarrhea. Persistent diarrhea may cause irritation of the uterus, which can lead to excessive uterine contractions.
- Pelvic pressure: Sometimes described as a feeling that the baby will “fall out”. You may feel you need to move your bowels, but with no result. This feeling of pressure may be constant or may come and go.
 You also may need to urinate more frequently.
You also may need to urinate more frequently. - Increase or change in vaginal discharge: Any of the following changes may be a sign of preterm labor:
- Change in type of discharge
- Change in consistency or feel of discharge
- Increased amount of discharge
- Change in color, especially to a brown or pink
- Contractions: A contraction is the tightening of the uterine muscle. The type of contractions that you feel in preterm labor may be different from those felt in term labor. You may feel only a tightening of the muscle. Sometimes, you may feel the contraction only if you have your fingers on the uterus to feel for the tightening.
Occasionally, you may see the uterus tighten and appear to rise up like a ball. Contractions are normal during pregnancy, but you need to watch for an increase in frequency or contractions that come at regular intervals.
You should not have five or more contractions or tightenings in 1 hour, or contractions should not be less than 15 minutes apart while you are lying down. If you have fewer than five contractions an hour, this uterine activity is probably normal and needs only your careful observation.
If you have fewer than five contractions an hour, this uterine activity is probably normal and needs only your careful observation.
How to monitor:
- Lie down
- Tilt toward your left side
- Put a small pillow under your hip to support your back, if needed
- Using your fingertips, gently feel your uterus for tightening. (Ask your provider to work with you in practicing the steps until you have learned “the feel” of your own uterus and its contractions)
- Think of your uterus as divided into four sections, and feel over each of the four sections. You are monitoring especially to detect contractions that feel uniformly firm over all four sections of your uterus.
- When the uterus is relaxed, you will be able to indent it with your fingers.
- During a contraction, the uterus will feel firm to the touch. You will notice a definite pressure change.
- Sometimes you may feel the baby move.
- The uterus may feel firm on one side while the opposite side remains soft.
 You may also have localized contractions that cause a bulging on only one side of the uterus. This type of contraction does not cause equal pressure within the uterus and does not cause your cervix to change.
You may also have localized contractions that cause a bulging on only one side of the uterus. This type of contraction does not cause equal pressure within the uterus and does not cause your cervix to change.
If you feel uterine tightening, try to determine how often it is coming and how long it lasts. Start counting minutes from the time the uterus begins to tighten. The time from the beginning of a tightening until the uterus becomes soft again is the length, or duration, of a single contraction. The number of contractions in any given time period (for example, one hour) is the frequency of contractions.
What to do if you have frequent contractions
If you have five or more contractions in an hour, or the time between the beginning of one contraction and the beginning of the next is less than 15 minutes, do the following:
- Empty your bladder
- Drink some fluids
- Rest on your left side for an hour while re-checking your uterine activity.
If this uterine activity persists while you are resting, then you may be in preterm labor and you should contact your provider.
Remember, it is often not possible to determine true labor from false labor over the phone, so you may be asked to come into the clinic or hospital for observation and/or to have your cervix checked.
Adapted from: Preventing Preterm Birth: A Parent’s Guide, Editors: Michael Katz, Pamela Gill, Judith Turiel (Pages 28 – 32)
Pregnancy Problems
Pregnancy discharge | What are the discharge during pregnancy? | Blog
In the absence of menstruation, girls usually suspect that conception has occurred. However, during pregnancy, the female body may continue to secrete a secret of a different color and character. We recommend that you keep a close eye on everything that happens so as not to miss the development of adverse events. We will talk about how to recognize problem situations during pregnancy in the article.
What discharge can occur during conception
Many women note that immediately after the delay and in the later stages, the nature of the secretion changes. It can be:
- With or without scent.
- Depending on the color - transparent, white, cream, yellow, greenish, bloody.
- By consistency - thick, liquid, cheesy.
- As a symptom for assessing the state of health - threatening, safe.
During ovulation, the egg is released from the ovary, its membrane is deflated, a small amount of fluid is released - so it becomes ready for fertilization. At this time, the thick mucus that fills the cervical canal of the cervix becomes less viscous. This makes it easier for the spermatozoa to penetrate and move further into the tubes for fertilization. At this time, you may notice an abundance of clear mucous secretion.
After the fusion of the egg with the spermatozoon, movement into the uterus begins, which should end with implantation in the inner layer. During penetration, its slight detachment may occur - this causes damage to the blood vessels that abundantly penetrate the muscular layer of the uterus. You may see light brown discharge, which is common during pregnancy. The color is due to the fact that the blood has time to clot.
During penetration, its slight detachment may occur - this causes damage to the blood vessels that abundantly penetrate the muscular layer of the uterus. You may see light brown discharge, which is common during pregnancy. The color is due to the fact that the blood has time to clot.
Sometimes the discharge is brightly colored and some women mistake it for a period that has started too early. But in this case, a short duration is characteristic, a different shade (dark or scarlet), a slight mark on the linen.
With some features of the structure of the female genital organs (for example, with a bicornuate uterus), after implantation of the embryo in one part, rejection of the endometrium may begin in the other, as usually occurs during menstruation. This rarely happens.
Characteristics of discharge in the event of a threatened miscarriage
Spontaneous abortion is the rejection of an embryo in the early stages after conception. If at the first signs of pregnancy, you notice spotting, there is a high probability that a miscarriage begins.
Also, miscarriage symptoms include:
- pulling or pressing on the lower abdomen, sacrum, lower back;
- the muscles of the uterus are tense.
The woman may feel cramps. This continues all the time or intermittently. From the vagina there are scarlet or brown discharge during pregnancy, which was previously confirmed. Sometimes the period may be still small, and the first signs did not have time to appear.
After 22 weeks, this phenomenon is called preterm labor. The child in this case is still weak, the organs are not sufficiently developed, and there is little chance of survival.
The following factors increase the risk of miscarriage:
- various diseases;
- progesterone deficiency;
- nervous and physical overexertion;
- pathologies in the genitals;
- fetal developmental defects.
To confirm the diagnosis, the doctor prescribes an ultrasound scan. If it shows that the fetal heart rate is disturbed, the tone of the uterus is increased, its size differs from normal for this period, hospitalization will be recommended to maintain pregnancy.
What discharge during pregnancy is considered normal
This secretion does not pose a threat to health:
- transparent;
- whitish;
- yellowish;
- odor free;
- mucous;
- without itching, burning, redness of the genitals.
Clear fluid on underwear is a symptom of ovulation. During pregnancy, the activity of ongoing processes in the body increases, so the amount of secretion secreted may increase. However, a violation of the norm is the leakage of amniotic fluid. You can determine the problem with the help of special diagnostic tests that the doctor will prescribe if he has suspicions.
White color, small amount, homogeneous structure should also not cause concern. The increased volume of fluid in this case is associated with increased hormonal activity.
One of the variants of the norm is mucous discharge, which smells of slight sourness. If there is no pain, discomfort, there is nothing to worry about.
Yellow discharge, there are signs of pregnancy, there is no unpleasant odor - you are all right. Some women had this color before conception, only they did not pay attention. Now there are more of them, therefore more noticeable.
Sometimes a woman observes that the laundry gets wet and there is a smell of urine. This may indicate incontinence due to the constant pressure of the growing uterus. In this case, it is recommended to go to the toilet more often, change underpants twice a day.
What discharge during pregnancy is considered a sign of infection?
White discharge during pregnancy with a cheesy texture is a symptom of thrush (candidiasis). In pregnant women, it is diagnosed quite often - the reason is a change in hormonal levels. The disease is accompanied by itching, redness of the vulva, a strong sour smell. Sometimes external manifestations are not detected, then treatment is not carried out.
Infection is indicated by pain, pain, skin irritation, ulcers, smell of rot or fish, gray or green color, frothy discharge, increased nervousness, large inguinal lymph nodes. The reason may lie in sexually transmitted infections. This includes syphilis, gonorrhea, trichomoniasis, chlamydia and others. They are dangerous because they cause premature birth and fetal developmental defects.
The reason may lie in sexually transmitted infections. This includes syphilis, gonorrhea, trichomoniasis, chlamydia and others. They are dangerous because they cause premature birth and fetal developmental defects.
What kind of discharge during pregnancy should I pay special attention to and should I consult a doctor?
The following indicates that pregnancy is at risk:
- Severe pain in the perineum, bleeding, difficulty defecation, convulsions - these may be injuries to the vaginal mucosa.
- Nausea, profuse vomiting, edema, headaches, cough, hypertension, bright red secretion are symptoms of hydatidiform mole (abnormal development of the embryo).
- A drop in blood pressure, pallor, weakness, sweating, pulling sensations, bleeding during pregnancy against the background of a lack of growth of hCG in the blood - this is how ectopic attachment manifests itself.
- Isolation of clots, sharp pain, vomiting, diarrhea may indicate a frozen fetus.
If you experience any of these symptoms, contact your doctor immediately.
It is also necessary to go to the clinic if you have been physically abused, had rough sex, had an accident, fell, hit. The likelihood that the situation will be resolved successfully is much higher if you do not delay the visit, listen to the symptoms and take good care of your health.
Remember, despite the fact that pregnancy is a normal state of health of the female body, the diagnosis and treatment tactics are still different, due to the many restrictions on manipulations and medications during pregnancy. That is why diagnosis and treatment during pregnancy should take place only under the supervision of a doctor. By ignoring the symptoms or self-medicating, a pregnant woman risks not only her health, but also the health of her child.
Doctors of the Leleka maternity hospital manage pregnancies of any complexity, including those aggravated by infections, pathologies, and the threat of miscarriage. Our own diagnostic laboratory allows us to accurately and in the shortest possible time to obtain the results of the tests. Thanks to constant medical supervision throughout the entire period, the chances of a successful birth are greatly increased.
Our own diagnostic laboratory allows us to accurately and in the shortest possible time to obtain the results of the tests. Thanks to constant medical supervision throughout the entire period, the chances of a successful birth are greatly increased.
Trust the life and health of your child to Leleka doctors, and we will make sure that you are satisfied.
Interventions for leg cramps during pregnancy
What is the problem?
Leg cramps manifest themselves as sudden, intense involuntary contractions of the leg muscles. This is a common problem during pregnancy, especially in the third trimester. They are painful and can interfere with daily activities, disrupt sleep, and reduce quality of life. Various types of interventions are used to treat leg cramps during pregnancy, including medications, electrolytes (magnesium, calcium, sodium) and vitamins, as well as non-drug therapies such as muscle stretching.
Why is this important?
The purpose of this review was to find out which treatment for leg cramps during pregnancy is effective and safe.
What evidence did we find?
In September 2019, we searched for evidence and identified eight randomized controlled trials in 576 women 14 to 36 weeks gestation comparing magnesium, calcium, calcium with vitamin D, or B vitamins versus placebo or no treatment, and compared vitamin C with calcium. All drugs were given as tablets to chew or swallow.
Magnesium supplements may reduce the incidence of leg cramps in women compared with placebo or no treatment, although studies have not been consistent. Different studies have assessed the effect of magnesium supplementation differently. Some studies have shown magnesium to help reduce the incidence of leg cramps, while others have shown little or no effect. Data on the effect of magnesium on pain reduction was also inconclusive, with only one study showing a reduction in pain intensity, while others showed no difference. Differences in the occurrence of side effects such as nausea and diarrhea were negligible or non-existent.
Differences in the occurrence of side effects such as nausea and diarrhea were negligible or non-existent.
Calcium did not always reduce the incidence of leg cramps in women after treatment compared to those who did not receive any treatment. It also found that the evidence was of very low quality, so we cannot be sure of the results.
More women who received B-vitamin supplements made a full recovery compared to those who received no treatment; however, these results were based on a small sample size and the study had design limitations.
The frequency of leg cramps did not differ between women receiving calcium and women receiving vitamin C. with placebo.
What does this mean?
The quality of the evidence was low to very low. This was mainly due to small study sample sizes and study design weaknesses. Four studies were well-conducted and presented their reports. The remaining four had flaws in their design: in several studies, women were not best assigned to different treatment groups, and in two studies, women knew whether they were receiving treatment or not.