5 week miscarriage sac
Miscarriage - what you might actually see and feel
Miscarriage - what you might actually see and feel | Pregnancy Birth and Baby beginning of content7-minute read
Listen
WARNING — This article contains some graphic descriptions of what you might see during a miscarriage.
A miscarriage requires prompt medical care. If you think you are having a miscarriage, call your doctor or midwife for advice and support. Go to the Emergency Department if:
- you are bleeding very heavily (soaking more than 2 pads per hour or passing clots larger than golf balls)
- you have severe pain in your tummy or shoulder
- you have a fever (a temperature above 38 degrees C)
- you are dizzy, fainting or feel like fainting
- you notice fluid coming from your vagina that smells bad
- you have diarrhoea or pain when you have a bowel motion (do a poo)
Miscarriage is a very unfortunate and sad outcome of pregnancy that takes a significant emotional and physical toll on a woman. It also happens more frequently than many people think. It's important to recognise that there's no right or wrong way to feel about a miscarriage.
Despite close to one in 5 pregnancies ending in miscarriage, what actually happens and what a woman needs to know and do when faced with a possible miscarriage are subjects that rarely get discussed.
This article aims to give you an idea of what happens and what a woman needs to know and do at different stages in her pregnancy.
Please call Pregnancy, Birth and Baby on 1800 882 436 if you have any concerns or wish to discuss the topic further.
What might I feel during a miscarriage?
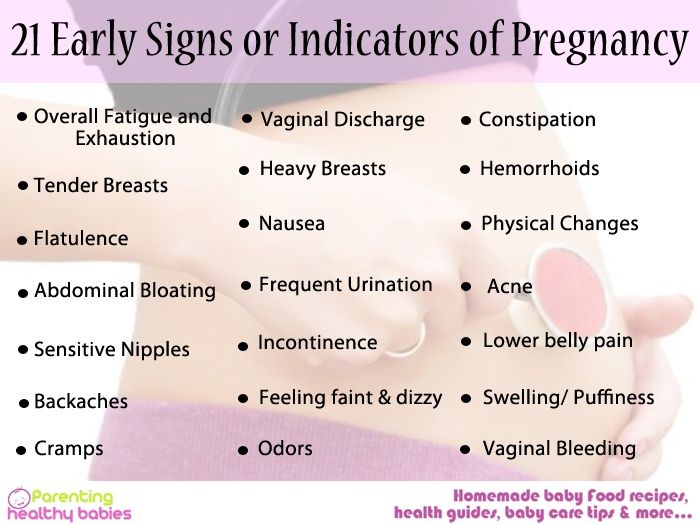
Many women have a miscarriage early in their pregnancy without even realising it. They may just think they are having a heavy period. If this happens to you, you might have cramping, heavier bleeding than normal, pain in the tummy, pelvis or back, and feel weak. If you have started spotting, remember that this is normal in many pregnancies — but talk to your doctor or midwife to be safe and for your own peace of mind.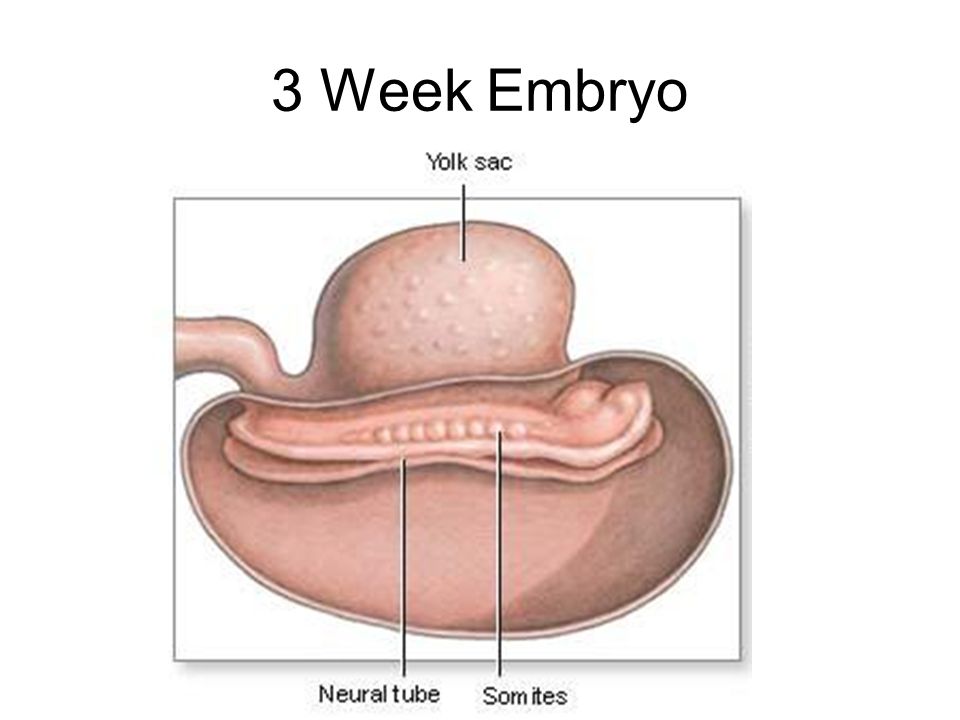
Later in your pregnancy, you might notice signs like cramping pain, bleeding or passing fluid and blood clots from your vagina. Depending on how many weeks pregnant you are, you may pass tissue that looks more like a fetus, or a fully-formed baby.
In some types of miscarriage, you might not have any symptoms at all — the miscarriage might not be discovered until your next ultrasound. Or you might just notice your morning sickness and breast tenderness have gone.
It is normal to feel very emotional and upset when you realise you’re having a miscarriage. It can take a while to process what is happening. Make sure you have someone with you, for support, and try to be kind to yourself.
What happens during a miscarriage?
Unfortunately, nothing can be done to stop a miscarriage once it has started. Any treatment is to prevent heavy bleeding or an infection.
Your doctor might advise you that no treatment is necessary. This is called 'expectant management', and you just wait to see what will happen.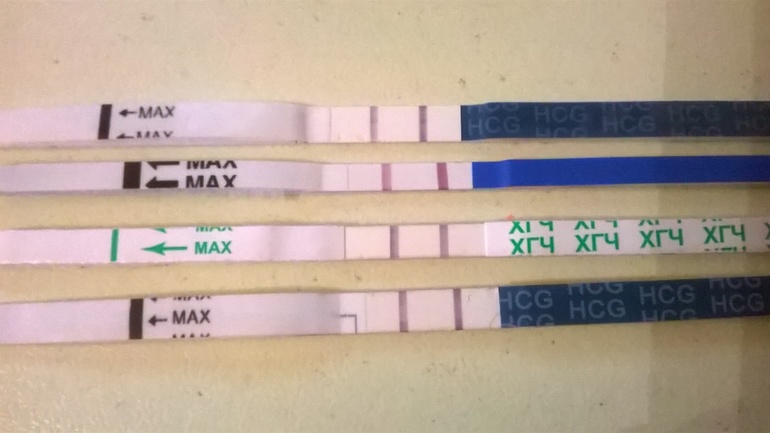 Eventually, the pregnancy tissue (the fetus or baby, pregnancy sac and placenta) will pass naturally. This can take a few days or as long as 3 to 4 weeks.
Eventually, the pregnancy tissue (the fetus or baby, pregnancy sac and placenta) will pass naturally. This can take a few days or as long as 3 to 4 weeks.
It can be very hard emotionally to wait for the miscarriage because you don’t know when it will happen. When it starts, you will notice spotting and cramping and then, fairly quickly, you will start bleeding heavily. The cramps will get worse until they feel like contractions, and you will pass the pregnancy tissue.
Some women opt to have medicine to speed up the process. In this case, the pregnancy tissue is likely to pass within a few hours.
If not all the tissue passes naturally or you have signs of infection, you may need to have a small operation called a ‘dilatation and curettage’ (D&C). You may need to wait some time for your hospital appointment. The operation only takes 5 to 10 minutes under general anaesthetic, and you will be able to go home the same day.
While you are waiting for a miscarriage to finish, it’s best to rest at home — but you can go to work if you feel up to it. Do what feels right for you. You can use paracetamol for any pain. If you are bleeding, use sanitary pads rather than tampons.
Do what feels right for you. You can use paracetamol for any pain. If you are bleeding, use sanitary pads rather than tampons.
What might I see during a miscarriage?
In the first month of pregnancy, the developing embryo is the size of a grain of rice so it is very hard to see. You may pass a blood clot or several clots from your vagina, and there may be some white or grey tissue in the clots. The bleeding will settle down in a few days, although it can take up to 2 weeks.
At 6 weeks
Most women can’t see anything recognisable when they have a miscarriage at this time. During the bleeding, you may see clots with a small sac filled with fluid. The embryo, which is about the size of the fingernail on your little finger, and a placenta might be seen inside the sac. You might also notice something that looks like an umbilical cord.
At 8 weeks
The tissue you pass may look dark red and shiny — some women describe it as looking like liver. You might find a sac with an embryo inside, about the size of a small bean. If you look closely, you might be able to see where the eyes, arms and legs were forming.
If you look closely, you might be able to see where the eyes, arms and legs were forming.
At 10 weeks
The clots that are passed are dark red and look like jelly. They might have what looks like a membrane inside, which is part of the placenta. The sac will be inside one of the clots. At this time, the developing baby is usually fully formed but still tiny and difficult to see.
At 12 to 16 weeks
If you miscarry now, you might notice water coming out of your vagina first, followed by some bleeding and clots. The fetus will be tiny and fully formed. If you see the baby it might be outside the sac by now. It might also be attached to the umbilical cord and the placenta.
From 16 to 20 weeks
This is often called a 'late miscarriage'. You might pass large shiny red clots that look like liver as well as other pieces of tissue that look and feel like membrane. It might be painful and feel just like labour, and you might need pain relief in hospital. Your baby will be fully formed and can fit on the palm of your hand.
After the miscarriage
You will have some cramping pain and bleeding after the miscarriage, similar to a period. It will gradually get lighter and will usually stop within 2 weeks.
The signs of your pregnancy, such as nausea and tender breasts, will fade in the days after the miscarriage. If you had a late miscarriage, your breasts might produce some milk. You will probably have your next period in 4 to 6 weeks.
Remember, it’ll be normal to feel very emotional and upset at this time.
More information
Read more about miscarriage:
- What is a miscarriage?
- What happens after a miscarriage
- Emotional support after miscarriage
- Fathers and miscarriage
- Experiencing a pregnancy loss
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
KidsHealth (Understanding miscarriage), The Royal Women's Hospital (Treating miscarriage), Pink Elephants Support Network (Sorry for your loss), Women’s and Children’s Health Network (Miscarriage), Patient.com (Miscarriage and bleeding in early pregnancy), Pink Elephants Support Network (Treatments and procedures), New Kids Center (Blood Clots of Miscarriage: What It Looks Like?), Babycenter Australia (Understanding late miscarriage)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: March 2022
Back To Top
Related pages
- Fathers and miscarriage
- Emotional support after miscarriage
- What happens after miscarriage
- Miscarriage
- Experiencing a pregnancy loss
Need more information?
Miscarriage
Miscarriage Despite being common and widespread, miscarriage can be a heartbreaking experience – with up to one in five pregnancies ending before week 20
Read more on Gidget Foundation Australia website
Miscarriage
A miscarriage is the loss of a baby, usually during the first three months or first trimester of pregnancy.
Read more on Pregnancy, Birth & Baby website
Fathers and miscarriage
A miscarriage can be a time of great sadness for the father as well as the mother.
Read more on Pregnancy, Birth & Baby website
Emotional support after miscarriage
It is important to know that there is no right or wrong way to feel after experiencing a miscarriage.
Read more on Pregnancy, Birth & Baby website
What happens after miscarriage
There are a number of things you may need to consider after a miscarriage.
Read more on Pregnancy, Birth & Baby website
Miscarriage | SANDS - MISCARRIAGE STILLBIRTH NEWBORN DEATH SUPPORT
Helping you understand the complex range of emotions you may experience during fertility treatment or after miscarriage or early pregnancy loss
Read more on Sands Australia website
Miscarriage: a guide for men | Raising Children Network
This Dads Guide to Pregnancy covers miscarriage, the grief men might experience after miscarriage, and how to support partners after pregnancy loss.
Read more on raisingchildren.net.au website
The Pink Elephants Support Network - Medical Options for Recurrent Miscarriage
In some cases, a medical reason for miscarriage or recurrent miscarriage can be found through testing
Read more on Pink Elephants Support Network website
New research on vitamin B3 and miscarriages
Pregnant women are being warned not to start taking vitamin B3 supplements, despite a recent study that suggests it might reduce the risk of miscarriages and birth defects.
Read more on Pregnancy, Birth & Baby website
Pregnancy: miscarriage & stillbirth | Raising Children Network
Have you experienced a miscarriage or stillbirth? Find articles and videos about coping with the grief of losing a pregnancy or having a stillbirth.
Read more on raisingchildren.net.au website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
What to Expect, What You'll See, and More
If you’re 5 weeks pregnant, you’re undergoing some major changes.
But you likely won’t notice any differences to your body on the outside. On the other hand, your body is already working to nurture a growing embryo, which is quickly developing important things like the brain, heart, spinal cord, and blood vessels.
It’s normal to want to get a glimpse of your baby as soon as you can. With that being said, if you haven’t had previous complications in pregnancy and you’re relatively healthy, it’s better to wait until at least 12 to 14 weeks into pregnancy to schedule your first ultrasound. This is because it’s too early to see the baby’s limbs and organs before this point.
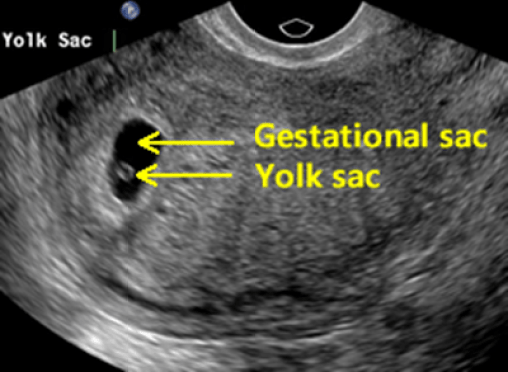
In fact, at 5 weeks, you’ll likely only see the yolk sac and the gestational sac — and many not even that. What you don’t see may unnecessarily worry you, but it’s perfectly normal.
Some women may get an early ultrasound during their first trimester to estimate the age of the gestational sac, which usually becomes visible in an ultrasound during the fifth week.
If you have a history of ectopic pregnancy or miscarriage, or if you’ve conceived via in vitro fertilization, your doctor may also want you to have an early ultrasound. In addition, bleeding after a positive pregnancy test might warrant a look at your uterus.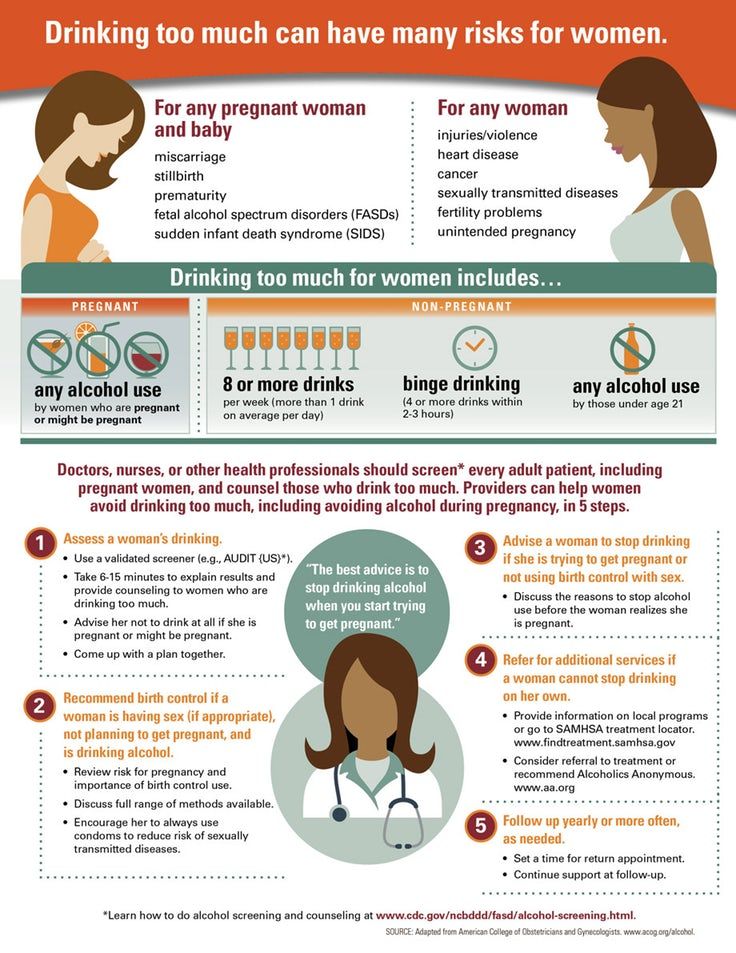
If you’re 5 weeks pregnant, your ultrasound will be done via the vagina as opposed to transabdominal ultrasounds that are typically performed later on in pregnancy.
During a transvaginal ultrasound, a lubricated wand is inserted into your vagina and images translate back to a screen. It shouldn’t be painful, but it may be a little uncomfortable.
Don’t be worried if you can’t see your baby! The embryo is only the size of a peppercorn right now — about 2 millimeters (mm).
At this stage, the only things you’ll likely see are the yolk sac and the gestational sac.
It’s possible that the sonographer might be able to point out the embryo, which at this stage is likely a tiny white curled object.
Surrounding the embryo is the yolk sac, which will look like a small white circle. The yolk sac nourishes the embryo and also helps produce blood cells during the early stages of pregnancy.
The yolk sac is surrounded by a larger black area, known as the gestational sac. The gestational sac contains amniotic fluid and surrounds the embryo. You may see the gestational sac in an ultrasound as early as 4 1/2 to 5 weeks.
The gestational sac contains amniotic fluid and surrounds the embryo. You may see the gestational sac in an ultrasound as early as 4 1/2 to 5 weeks.
The gestational sac increases in diameter by 1.13 mm per day and initially measures 2 to 3 mm in diameter, according to the National Center for Biotechnology Information.
You may get to see the flicker of a little heartbeat, but again, don’t stress if the sonographer can’t see it yet. It’s more common to see the heartbeat at 6 weeks or even later.
Patience is key during pregnancy. Some women may go in for a 5-week ultrasound only to hear that their gestational sac isn’t showing up yet.
There are a few possibilities as to why the gestational sac doesn’t show up during a 5-week ultrasound.
It’s too early
You may have counted the days incorrectly if you’re unable to see the gestational sac. Something as simple as getting the dates wrong may be the reason why you don’t see anything during a 5-week ultrasound.
This is common and has everything to do with your human chorionic gonadotropin (hCG) levels. HCG is the same hormone that confirms pregnancy from urine on a pregnancy test.
Your hCG levels should be around 1,500 to 2,000 at 5 weeks pregnant, but it may be difficult to see anything until hCG exceeds 2,000.
Ectopic pregnancy
An ectopic pregnancy may be the reason why you don’t see anything during a 5-week ultrasound. This is less common than having the dates wrong and may be life threatening if not treated.
An ectopic pregnancy happens when fertilized eggs implant and grow on the outside main cavity of the uterus. These pregnancies require treatment and may cause heavy bleeding inside the abdomen. Most ectopic pregnancies occur in a Fallopian tube.
See your doctor if you notice any vaginal bleeding or pain in the pelvic area while pregnant.
Miscarriage
Falling hCG levels and the inability to find a gestational sac may also point to an early miscarriage. A miscarriage happens when a fertilized egg doesn’t form properly form an embryo.
A miscarriage happens when a fertilized egg doesn’t form properly form an embryo.
Vaginal bleeding is a common sign of a miscarriage but isn’t a unique symptom for miscarriages — vaginal bleeding may mean something else in your pregnancy.
In more rare cases, miscarriages may occur because of problems with your uterus or cervix. See your doctor if you have questions or concerns about miscarriage.
Pregnancy symptoms are impacted by your hCG levels. Common symptoms during the fifth week of pregnancy include:
- metallic taste in your mouth
- tender breasts
- morning sickness
- mood swings
- unusual pregnancy cravings
- constipation
- expanded sense of smell
- increased urination
- white vaginal discharge
- light spotting
- abdominal cramps
- thicker and shinier hair
- bloating
- missed period
You may want to wait a couple of weeks to get your first ultrasound to increase the chances of seeing the gestational sac and embryo.
While most women can expect to see something in a 5-week ultrasound, no two pregnancies are the same. Your doctor may recommend more frequent ultrasounds if you have existing health conditions.
No matter what, it’s very important to monitor your health and the health of the baby by keeping up with your recommended prenatal appointments.
Miscarriage, how to avoid - Planning and management of pregnancy in the gynecology of the Literary Fund polyclinic after a miscarriage
- Gallery
- News
- Blog
- Reviews
- Jobs
- Licenses
- Insurance partners
- Controlling organizations
- Schedule of reception of citizens on personal appeals
- What you need to know about coronavirus infection?
- Rules for patients
- Online doctor's consultation
- to corporative clients
- The documents
A miscarriage is always associated with severe consequences for the whole body of a woman and for her reproductive organs in particular, it also affects the family situation, disrupts the woman's work schedule.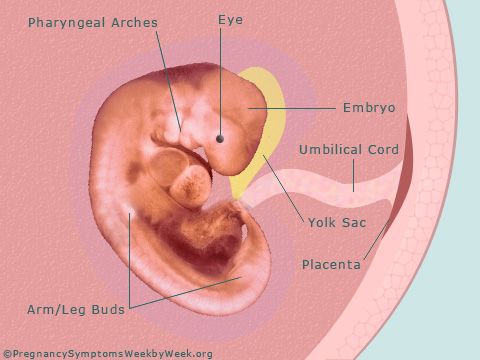 An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
Any competent gynecologist will tell you that the problem of miscarriage can be solved. With proper preparation for pregnancy and its management, the next time you will have a successful pregnancy. Most girls after a miscarriage go to extremes: they try to get pregnant again as soon as possible. And if this succeeds, then the miscarriage is very often repeated. And you need to give the body a rest for 2-3 months, then identify and eliminate the cause. And only then try.
Causes of miscarriage
Many are convinced that miscarriages are due to a fall, bruise, or some other physical shock. Any woman who has had a miscarriage can remember that not long before she either fell or lifted something heavy. And I am sure that she lost her unborn child precisely because of this. However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
The woman's body is almost always to blame for the other half of miscarriages. They are caused by various known and unknown factors, such as: acute infectious diseases suffered in the first trimester of pregnancy, poor environment or difficult working conditions, excessive psychological or physical stress, abnormal development of the uterus, radiation, alcohol, smoking and certain types of drugs.
The causes of early and late miscarriage may differ, although they may overlap.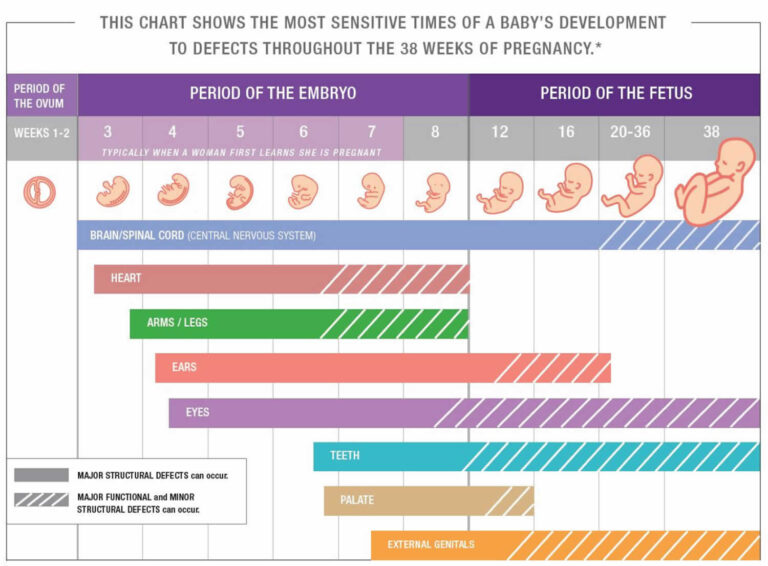 The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
Miscarriage
Miscarriage statistics also include “missed pregnancy”. Sometimes it happens that the embryo dies and lingers in the uterine cavity. Most often, this fact is detected by ultrasound. The dead fetus may begin to decompose, and this, thereby, will lead to poisoning of the mother's body.
Doctors resort to surgical curettage, which is associated with a risk of inflammation and complications. With such a miscarriage, the next pregnancy is planned after the body is fully restored - not earlier than a year. During this year, you will have to find out the cause of the missed pregnancy and treat it.
Miscarriage up to 6 weeks
The main causes of miscarriage on this line are malformations of the embryo itself. Statistics say that from 70-90% of embryos had chromosomal abnormalities: they are random and will not occur in other pregnancies. You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
The human body is perfect and finds a way to correct the situation by miscarriage. Today is a tragedy for you. The real tragedy would be the preservation and birth of a sick, non-viable child. So don’t cry and understand: everything is for the best, you won’t help grief with tears ... And after three months, try again - it will almost certainly turn out to be successful.
It should also be noted that the fact of a miscarriage does not mean that you have lost something. So for a period of 7-8 weeks, the absence of an embryo in the fetal egg is found - "anembryony". It is believed that in 80-90% of cases, miscarriages are undiagnosed non-developing pregnancies.
Miscarriage between 6 and 12 weeks
Miscarriage in this period is also considered early. Its most common causes are:
Endocrine disorders
Endocrine disorders, when the ovaries do not synthesize enough hormones to keep the fetus in the womb, or the amount of male sex hormones is increased, is one of the most common causes of miscarriage and miscarriage.
Imbalance of hormones in a woman's body is very likely to lead to an early termination of pregnancy. With a lack of the main hormone progesterone produced by the ovaries, this happens most often. Another hormonal problem is an increase in the tone of the uterus, which provokes the expulsion of the fetus.
Progesterone prepares the uterine mucosa for implantation and is the hormone for maintaining pregnancy in the first months. If conception occurs, the fetus cannot properly establish itself in the uterus. As a result, the fertilized egg is rejected. But pregnancy can be saved with the help of progesterone preparations if this problem is detected in time.
An excess of male sex hormones that suppress the production of estrogen and progesterone can also be the cause of an early miscarriage. Often, the cause of recurrent miscarriages are androgens that affect the formation and development of pregnancy; as well as thyroid and adrenal hormones. Therefore, a change in the function of these glands can lead to miscarriage.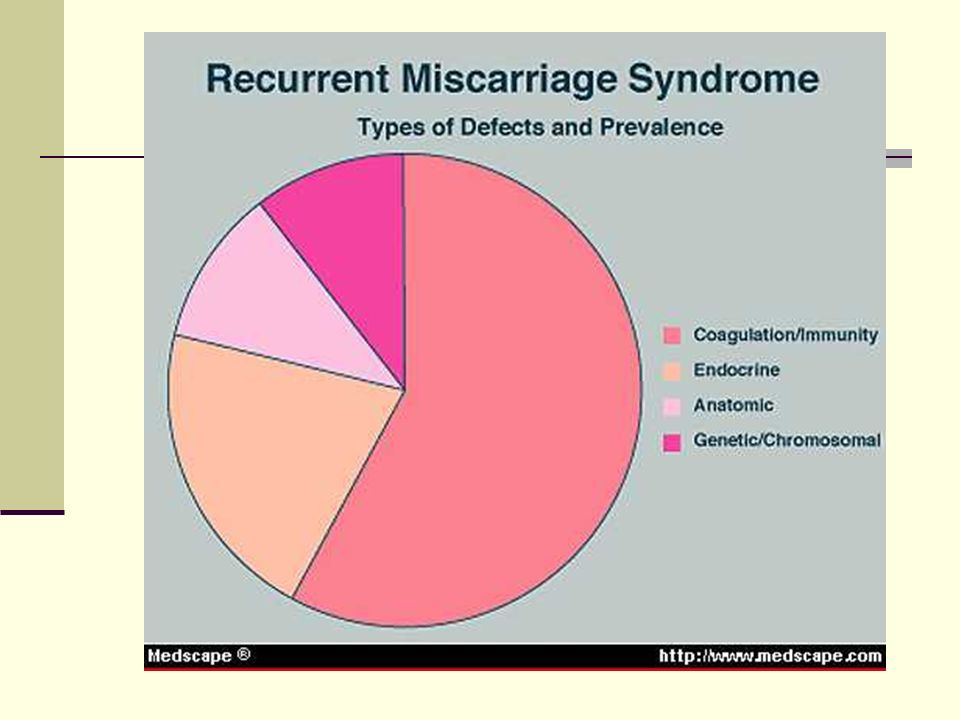
Undertreated sexual infections
This problem must be solved before conception. Often the cause of miscarriage is sexually transmitted infections: syphilis, trichomoniasis, toxoplasmosis, chlamydia, cytomegalovirus and herpetic infections. Their effect on the fetus and the course of pregnancy is different for each woman and depends on the timing of infection, the activity of the microorganism, the degree of immune protection and the presence of other adverse factors. Depending on the situation, they can lead to the formation of fetal malformations, intrauterine infection, feto-placental insufficiency, early miscarriage or premature birth. Infection of the fetus and damage to the membrane of the fetus leads to miscarriage. To avoid this, infections should be treated before pregnancy. The use of therapy is possible during pregnancy as prescribed by a doctor.
Viral infections and other diseases
Any disease accompanied by intoxication and fever above 38 about C can lead to a miscarriage. Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Extremely dangerous during pregnancy rubella - it leads to severe fetal malformations, so infection during pregnancy is an indication for medical abortion.
Any disease during pregnancy can lead to non-viability of the fetus. And the body, through a miscarriage, insures you against unwanted offspring. With such a miscarriage, the next pregnancy has every chance of going well.
Immune causes of miscarriage
Sometimes antibodies that are hostile to the fetus are formed in the blood of a pregnant woman. This cause can be predicted and eliminated in advance. Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Reduced immunity
Reduced immunity during pregnancy also refers to immune causes. The body is simply not able to grow a new life in itself. You need to take care of yourself and recover before the next conception.
Anatomical causes of miscarriage
Anatomical causes of miscarriage are the most intractable. Malformations of the uterus are a serious reason for miscarriage. Sometimes you just have to deal with it.
Miscarriage between 12 and 22 weeks
Such a miscarriage is considered late. Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
At this time, miscarriage also occurs due to isthmic-cervical insufficiency - a weak cervix cannot hold the fetus and opens. For this reason, a miscarriage can occur in the 2nd or 3rd trimester. Isthmic-cervical insufficiency is observed in 15.0-42.7% of women suffering from miscarriage. Careful monitoring of the pregnant woman allows you to identify the problem in time and make surgical correction of the cervix before the onset of childbirth.
In isthmic-cervical insufficiency, there is only one method of treatment - mechanical narrowing of the cervical canal. To do this, the neck is either sewn up or a special ring is put on it. However, the latter method is less efficient, because the ring can easily slide off the neck, then it will no longer hold back the process of opening it.
After suturing, if necessary, it is possible to use antibiotics and drugs that normalize the microflora of the vagina.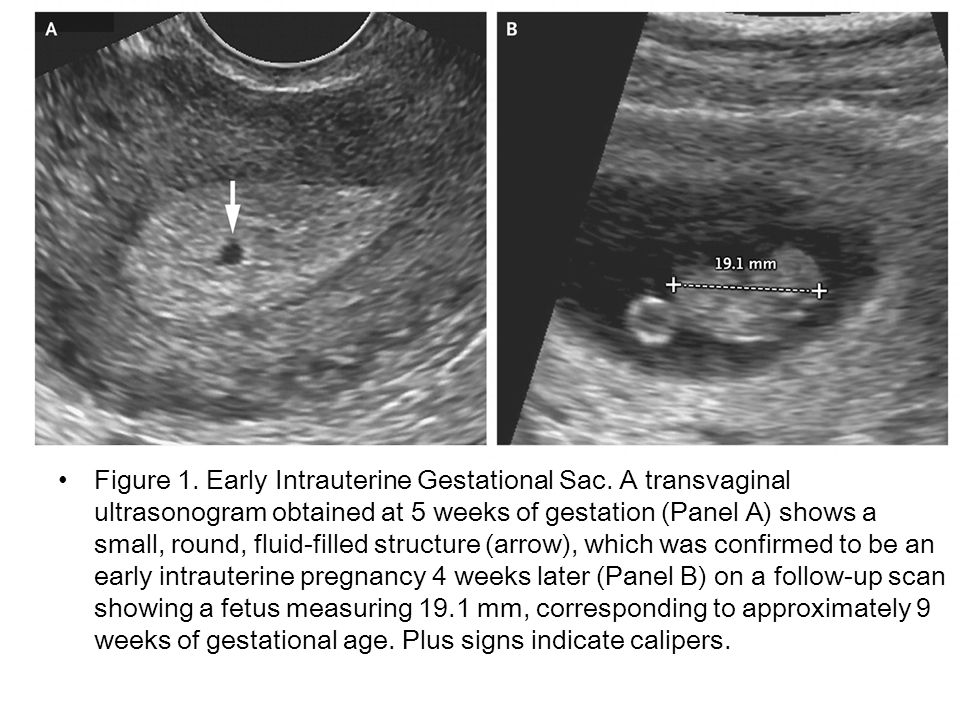 The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
Isthmic-cervical insufficiency may be primary (for no apparent reason), may be the result of abortion or hormonal disorders (increased levels of androgens - male sex hormones or their precursors).
Miscarriage after 22 weeks
Such a loss is hard to forget. Obstetricians talk about premature birth after the 28th week of pregnancy. Traditionally, a child born after this period is considered viable. But medicine knows many cases when it was possible to save the life of earlier children.
We recommend that you be carefully examined for miscarriage, check the above factors. In addition to them, the cause of a miscarriage can be antiphospholipid syndrome, while the woman's body perceives the child as something alien and rejects it. This disease, like the others listed, can be corrected; you have a very real chance of bearing a child.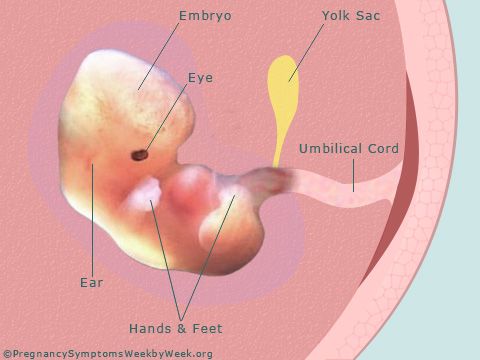
Miscarriages due to hemostasis disorders
All of the above causes account for only 30-40%. Up to 70% of miscarriages are caused by disorders in the blood coagulation system (hemostasis).
Blood coagulation disorders leading to pregnancy loss can be divided into thrombophilic (increased clotting) and hemorrhagic (bleeding tendencies). Both of these extremes are dangerous to the fetus. Various disorders leading to the formation of small blood clots lead to the fact that the fetus loses sufficient blood supply, development is disturbed and the fetus is rejected.
The main hemorrhagic changes can appear even in childhood in the form of increased bleeding during cuts, tooth extractions, the onset of menstruation. But sometimes they declare themselves only during pregnancy and are the cause of a miscarriage. Bleeding in the early stages and detachment of the chorion is difficult to stop.
You may not guess, but incomprehensible headaches, weakness, fatigue, temporary loss of smell or hearing may be symptoms of disorders in the blood coagulation system.
When planning a pregnancy, a genetic examination should be carried out and, if necessary, treatment should be initiated.
It is advisable to be examined for hidden hemostasis defects even for those who consider themselves healthy. This will allow you to predict the occurrence of complications and prevent loss. Early therapy can prevent miscarriage at 98% of cases. If defects in hemostasis are already detected during pregnancy, it can be difficult to maintain it.
What to do after a miscarriage?
Find the cause! The ideal option is to be examined by future parents: it is much more reasonable to postpone conception and spend two or three months to identify the causes than to risk getting pregnant again, spend two months waiting, and then lose everything again and still go to the doctors.
Until you understand the reason, it will not evaporate. In most cases, the answers lie on the surface. Take care of your health and your future baby.
Sign up for a consultation with an obstetrician-gynecologist by phone +7 (495) 150-60-01
Tyan Oksana Alexandrovna
Head of the department, obstetrician-gynecologist Doctor of the highest category Work experience: 26 years
Volkova Polina Dmitrievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the highest category Experience: 35 years
Postnikova Nadezhda Anatolyevna
Obstetrician-gynecologist, ultrasound specialist Work experience: 35 years
Moiseeva Alla Vitalievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the first category Work experience: 37 years
Zabolotnova Olga Valentinovna
Obstetrician-gynecologist Doctor of the first category Experience: 25 years
Shchelokova Elena Nikolaevna
Obstetrician-gynecologist Doctor of the highest category Work experience: 38 years
Pass or medical card number:
Contact phone: *
Select the day of your appointment:
Additional information:
I am not a robot
By clicking the "Submit Application" button, you agree to the terms Privacy Policy and User Agreement
Spontaneous miscarriage and miscarriage
Over the past 10 years, the number of spontaneous miscarriages has been growing rapidly.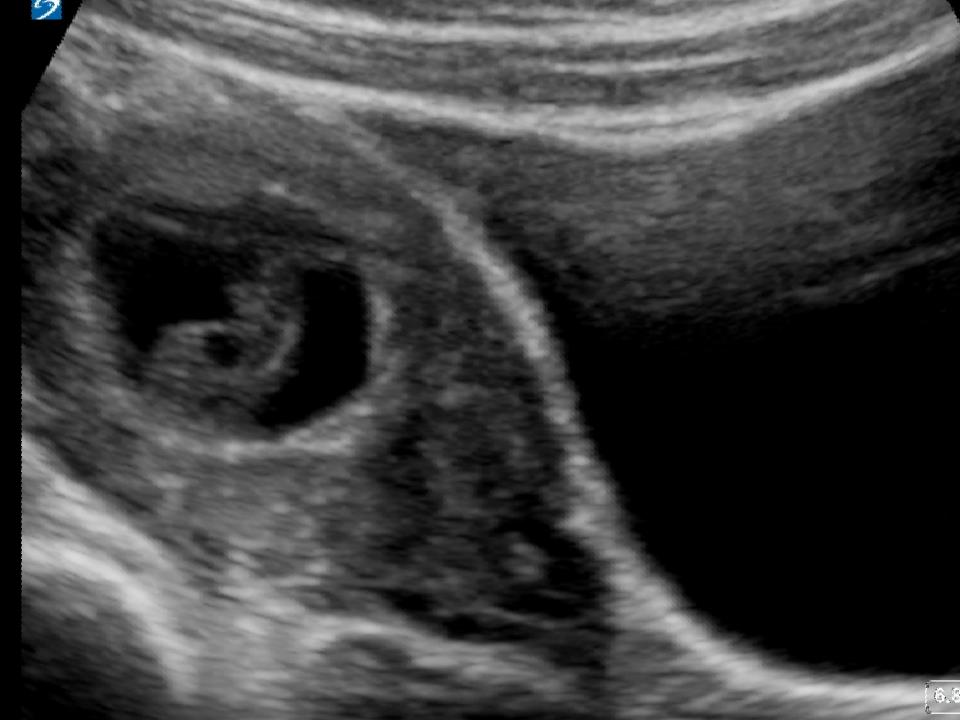 The International Histological Classification Organization (FIGO) has declared an epidemic of the situation with an increase in the frequency of miscarriages.
The International Histological Classification Organization (FIGO) has declared an epidemic of the situation with an increase in the frequency of miscarriages.
Spontaneous miscarriage is the termination of pregnancy before the fetus reaches a viable term (up to 22 weeks of pregnancy and fetal weight 500g.).
Most miscarriages (about 80%) occur before 12 weeks of gestation. Moreover, in the early stages up to 8 weeks of pregnancy, the cause of miscarriage is chromosomal abnormalities in 50% of cases. It turns out that nature eliminates the defective product of conception. And these causes are difficult to prevent, especially in the presence of hereditary diseases. Fortunately, accidental breakdowns are much more common than genetically determined ones. Therefore, subsequent pregnancies usually end happily. But the remaining 50% of miscarriages have completely real and removable causes. They can be easily identified at the stage of preparation for pregnancy by a gynecologist.
What are the reasons?
- chronic diseases: inflammatory diseases of the uterus and appendages, polycystic ovary syndrome, uterine fibroids, endometriosis, malformations of the genital organs.
- infections: toxoplasmosis, listeriosis, genital tuberculosis, sexual infections - chlamydia, mycoplasma, ureaplasma, syphilis.
- antiphospholipid syndrome.
- endocrine diseases: diabetes, thyroid disease.
- metabolic disorders in the body: obesity, folic acid deficiency, iron deficiency, vitamin D deficiency.
- male factor.
Of course, these causes are identified and eliminated before the planned conception.
There are harmful factors that can affect the development of the fetus in the early stages of pregnancy and lead to miscarriage:
- alcohol consumption.
- use of caffeine (4-5 cups of coffee per day).
- smoking (more than 10 cigarettes per day).
- drug use.
- taking medications with a teratogenic effect (for example: aspirin, nise and others from this group of drugs; antifungals; antidepressants; some antibiotics and a number of other drugs).
- toxins and occupational hazards: ionizing radiation, pesticides, inhalation of anesthetic gases.
What are the signs of possible pregnancy loss?
These are complaints of pain in the lower abdomen and lower back, bloody discharge from the genital tract. It is necessary to consult a doctor to rule out an ectopic pregnancy and conduct an additional examination (hCG test, blood test for progesterone, ultrasound).
In early pregnancy, with dubious ultrasound data or suspected non-developing (missing) pregnancy, expectant management is chosen with a repetition of a gynecologist's examination, ultrasound, tests after 7-10 days. If a the diagnosis was made and the fact of uterine pregnancy was confirmed, with a threatened miscarriage, preservation therapy is carried out in an outpatient day hospital. A miscarriage that has begun requires hospitalization in the gynecological department. In the case of a non-developing pregnancy, an abortion is performed.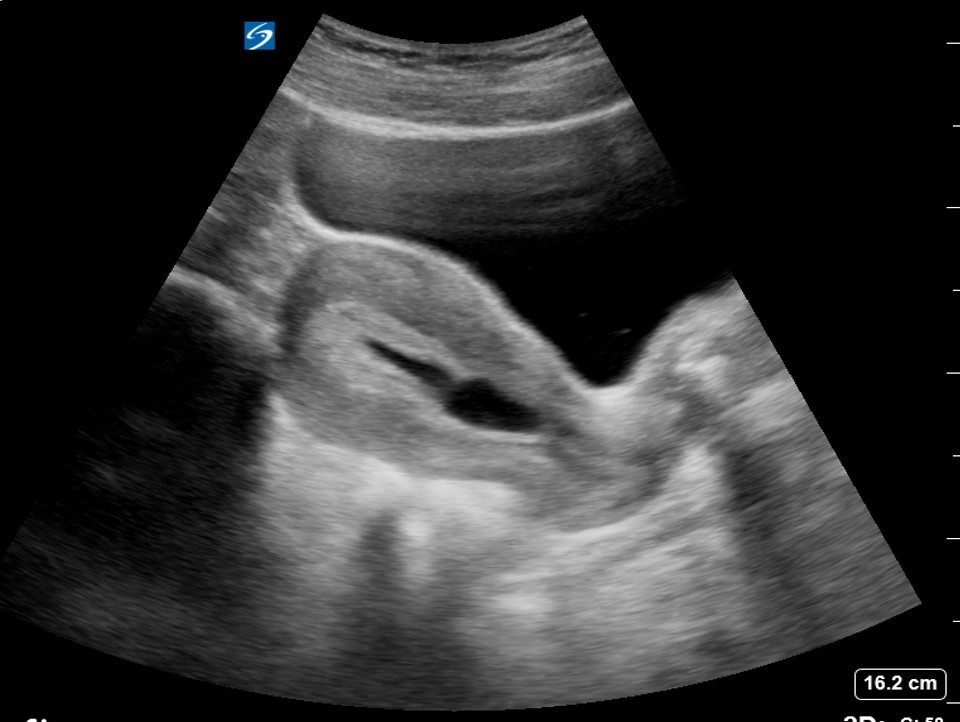
In accordance with the clinical treatment protocol approved by the Ministry of Health of the Russian Federation dated 07.06.2016. Preference is given to drug therapy aimed at terminating pregnancy with prostaglandin analogues (misoprostol) with or without prior use of an antiprogestin (mifepristone). In case of need for surgical treatment (with incomplete miscarriage with infected miscarriage), it is recommended to use aspiration curettage (with an electric vacuum source or a manual vacuum aspirator). What has a significant advantage over curettage of the uterine cavity because it is less traumatic and can be performed on an outpatient basis.
All women who have had a miscarriage need treatment to prevent complications and prevent recurrent miscarriages. Why is rehabilitation therapy necessary?
According to the decision of the XVIII World Congress of Obstetricians and Gynecologists , the diagnosis of chronic endometritis should be made to absolutely all women who have had an undeveloped pregnancy. Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy.
Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy.
If time is lost, it is necessary to carry out additional diagnostics: a pipel biopsy of the endometrium with a histological examination and a study for infections, including tuberculosis. Then, taking into account the results obtained, symptomatic anti-inflammatory therapy is carried out (immunomodulators, antibacterial drugs, physiotherapy, gynecological massage, mud therapy). In parallel, an examination is prescribed to identify other causes of miscarriage (male factor, chronic maternal diseases, genital infections, antiphospholipid syndrome).
In the medical center "Mifra-Med" at the level of modern requirements of medicine, all the possibilities of a complete adequate examination have been created: all types of tests, ultrasound, hysteroscopy, aspiration biopsy, consultations of narrow specialists (endocrinologist, therapist, neurologist, urologist).