4Th trimester symptoms
The ‘fourth trimester’: Why women need health care after delivery | Your Pregnancy Matters
Prenatal care appointments can make it feel like you live at your Ob/Gyn’s office, especially in the third trimester as your due date approaches. Starting from the moment you find out you’re pregnant, you’re encouraged to see the Ob/Gyn regularly – and then some. Women typically are seen every four weeks for most of the first and second trimesters, then every two weeks for a period, and then every week in the later third trimester.
But for many women, after baby comes, the doctor-patient relationship becomes a vacuum. If you have a normal vaginal delivery, the standard post-delivery checkup is six weeks after your discharge from the hospital. After a C-section, which is a major medical procedure, it’s typically two weeks before women see the doctor again.
My colleagues and I call the postpartum period “the fourth trimester.” In this time, your body is healing from childbirth and trying to return to its pre-pregnancy state. Though a break from doctor appointments might sound like a good thing, it’s actually quite the opposite: The absence of health care after childbirth can lead to serious health implications, even death, for new moms.
Recent data has raised concerns regarding the maternal mortality rate in Texas. Fourth-trimester maternal care, also known as interconception care, can help reduce the risk of tragic medical issues after delivery and can be the first step towards optimizing your health, including for future pregnancies.
Health concerns we address in fourth-trimester health care
So many body transformations occur in new moms in the weeks and months after childbirth. The body’s adjustment from pregnancy to healing can cause uncomfortable side effects, including:
- General discomfort
- Hormone fluctuations
- Swelling for two to three weeks
- Postpartum bleeding for two to three weeks
Often, women either are unprepared for these side effects or perhaps expect that managing them will be easier than it turns out to be. Complicating recovery further, many women are diagnosed during pregnancy with health problems, such as diabetes or high blood pressure, that can last long after delivery. Depending on weight gain during and after pregnancy, women might face obesity-associated health risks. Some women are diagnosed with depression either during or after pregnancy. Depression that occurs after pregnancy is called postpartum depression.
Complicating recovery further, many women are diagnosed during pregnancy with health problems, such as diabetes or high blood pressure, that can last long after delivery. Depending on weight gain during and after pregnancy, women might face obesity-associated health risks. Some women are diagnosed with depression either during or after pregnancy. Depression that occurs after pregnancy is called postpartum depression.
These ongoing issues can be compounded by the sleep deprivation and stress that can accompany bringing home a newborn. In this sometimes-stressful time, it’s easy for women to overlook subtle emotional and physical signals that something more serious is wrong. This is especially true if the doctor sends you home with your newborn and says, “See you in six weeks!” without a thorough discussion of what to expect during recovery and what symptoms should alert you that something is wrong.
Gaps in fourth-trimester care
Unfortunately, even when a conversation about fourth-trimester health occurs, some women still don’t get that vital care. A study published in 2016 by the American College of Obstetricians and Gynecologists indicates that as many as 40 percent of women don’t go to their six-week postpartum exam. In Childbirth Connection’s Report of the Third National U.S. Survey of Women’s Childbearing Experiences, 44 percent of women surveyed who experienced depression symptoms had not met with their provider since giving birth.
A study published in 2016 by the American College of Obstetricians and Gynecologists indicates that as many as 40 percent of women don’t go to their six-week postpartum exam. In Childbirth Connection’s Report of the Third National U.S. Survey of Women’s Childbearing Experiences, 44 percent of women surveyed who experienced depression symptoms had not met with their provider since giving birth.
Statistics like these indicate a disconnect in doctor-patient relationships and communication. Doctors can’t expect overwhelmed new moms to know what should be expected and what could be a problem. That’s unreasonable.
We must explain that even if a woman experiences no unusual symptoms postpartum, attending the six-week appointment still is vital for her health. And a woman shouldn’t wait until her six-week checkup if symptoms or questions arise, or if something just doesn’t feel right. She should call an Ob/Gyn or primary care doctor and be seen, even if her six-week checkup is weeks away. This is a partnership.
This is a partnership.
Red flags during the fourth trimester
Seeking care from a doctor prior to the six-week checkup can help reduce the risk of complications. These symptoms might indicate that something is wrong, and you should seek the care of your Ob/Gyn immediately:
- Excessive fatigue
- Headaches
- Dizziness
- Extreme sadness or mood swings
- Thoughts of harming yourself or your baby
- Swelling or postpartum vaginal bleeding that lasts longer than two weeks
- Any sharp, persistent, or intense pain in the abdomen, particularly if you’ve had a C-section
During the fourth trimester, enlist the help of your partner, loved ones, and friends to not only help with the baby but also keep an eye on you. Pay attention to their thoughts regarding your health and behavior, and let them check in on you from time to time and ask how you’re feeling.
I recommend that every woman see a doctor annually to continually optimize her health and monitor health concerns. This is especially important to manage or resolve chronic health conditions diagnosed during pregnancy. If a woman chooses to get pregnant again in the future, going into the pregnancy healthy can decrease the risk of complications for both her and the baby.
This is especially important to manage or resolve chronic health conditions diagnosed during pregnancy. If a woman chooses to get pregnant again in the future, going into the pregnancy healthy can decrease the risk of complications for both her and the baby.
How primary care helps you in future pregnancies
A primary care doctor can help you achieve and maintain an ongoing healthier lifestyle, which can improve the chance for healthier pregnancies in the future. Ongoing primary care and healthy lifestyle choices can decrease the risk of complications such as birth defects, growth restriction, hypertension, diabetes, and other health concerns with your next pregnancy.
UT Southwestern maternal fetal medicine specialists (MFMs) like me are available on an outpatient basis to consult with women who have had or anticipate having complicated pregnancies. We will meet with you to create a plan to help optimize your health and potentially reduce preventable health risks to you and your baby. We also offer preconception counseling if you have a pre-existing condition that might make getting pregnant or having a healthy pregnancy difficult.
We also offer preconception counseling if you have a pre-existing condition that might make getting pregnant or having a healthy pregnancy difficult.
In addition to seeing an Ob/Gyn, it’s important to see a primary care or family medicine doctor on a regular basis. These doctors often have training in a variety of areas, including pediatrics and women’s health concerns. These doctors can help you with questions about birth control, breastfeeding, and managing chronic concerns such as diabetes and high blood pressure.
Just as we encourage women in the third trimester to think about getting diapers and a car seat prepared, we encourage adding “find a primary care doctor” to the pre-baby to-do list. You can look on your own or request references from friends and family members, or we can recommend providers we know and trust who can take care of you going forward.
If you have medical conditions that made your pregnancy difficult, such as a heart problem, diabetes, obesity, or high blood pressure, your primary care doctor can help you optimize your health and straighten out your medications after pregnancy and as your health improves over time. Think about bringing your new child into the world as a chance to reset your own health as well.
Think about bringing your new child into the world as a chance to reset your own health as well.
The better your chronic conditions are controlled, the healthier you will be and the more energy you will have to care for your newborn – and the healthier you will be if you choose to get pregnant again.
Looking for a primary care doctor? Find a UT Southwestern doctor online or call 214-645-8300.
A Mother’s Guide to the Fourth Trimester
The fourth trimester—the 12 weeks after giving birth—is just as important for a mother’s health as the first three trimesters. Yet this is often when mothers have the least interaction with their health care team, a time when, some experts argue, mothers need it the most.
The American College of Obstetricians and Gynecologists (ACOG) recommends that mothers have initial contact with their OB-GYN within three weeks after delivery, followed by ongoing care as needed, and a comprehensive postpartum visit no later than 12 weeks after delivery. They also recommend that a postpartum care plan be developed during pregnancy, so that mothers are better prepared when they go home.
They also recommend that a postpartum care plan be developed during pregnancy, so that mothers are better prepared when they go home.
“Those 12 weeks after giving birth are a critical time to focus on Mom and make sure that she is healthy moving forward,” says Mary Rosser, MD, PhD, assistant professor of obstetrics & gynecology at Columbia University Vagelos College of Physicians and Surgeons and an OB-GYN at Columbia University Irving Medical Center/NewYork-Presbyterian. “We want to make sure it is not just a one-off checkup but that we’re giving mothers holistic care and support for their growing family. Postpartum care sets the stage for lifelong health and well-being.”
Postpartum Visits
Just 40% of moms attend their postpartum follow-up visit, says Rosser, who helped develop post-birth recommendations as a member of ACOG’s Presidential Task Force on Redefining the Postpartum Visit. “It’s an overwhelming time, so what often happens is this visit gets pushed aside, but it absolutely should not,” she says. “It impedes the management of chronic health conditions, discussing family planning and contraception, assessing mental health and well-being, and physical recovery.”
“It impedes the management of chronic health conditions, discussing family planning and contraception, assessing mental health and well-being, and physical recovery.”
Rather than the traditional single checkup at around six weeks, Rosser says that “postpartum care should be an ongoing process, with tailored services to support each mother’s individual needs.”
ACOG recommends a postpartum visit within one to three weeks and another within 12 weeks of giving birth.
Those who are considered high risk should check in within the first week or two, says Rosser. The first check-in—which often can be done over the phone or via telehealth—is to make sure Mom is doing well physically and emotionally and baby is feeding properly and gaining weight. It is important to discuss with your health care provider, Rosser says, whether this initial visit can be done via video or should be in person.
Within 12 weeks mothers should have an in-person, comprehensive care visit to discuss any medical concerns that may need addressing, as well as the mother’s physical health, mental and emotional health, and infant care and feeding. This also is a time when practitioners and patients can develop a road map for future health.
This also is a time when practitioners and patients can develop a road map for future health.
It is important to note that, depending on a mother’s personal history and individual needs, they should receive ongoing postpartum care as needed. “It really is no longer a one-size-fits-all approach,” says Rosser.
A Comprehensive Postpartum Checklist
1. Physical recovery
After delivery, there is a lot of soreness and healing that takes place. It is important for patients to have a full physical exam during their postpartum visit. A patient who had a tear during a vaginal delivery will need a thorough exam to make sure everything is healed. For C-section deliveries, the stitches need to be looked at to ensure they’re healing. “I’ll listen to the heart and the lungs, especially if they have had hypertension, do an abdominal exam, check to see if their thyroid is OK,” says Rosser. “You’re going from top to bottom, just like you would for any comprehensive exam, but you are targeting and individualizing it to that individual woman. ”
”
2. Infant care and feeding
Postpartum appointments also are a chance to assess how a baby is doing and whether they are feeding properly. Breastfeeding is healthy for both infants and moms, but not everyone has instant success. If, after two or three days, there is a lot of pain, Mom is unable to breastfeed, or the baby is not gaining weight, seek support from a lactation consultant.
3. Sleep and fatigue
Mothers will be very fatigued in the first few weeks after delivering a baby. Experts advise new mothers fit in sleep whenever possible, such as when the baby is sleeping. Resist the urge to do chores around the house when your newborn is sleeping; instead, take a nap yourself. Consider enlisting your partner in nighttime feedings so that you can get a good night’s sleep. Perhaps a family member or friend can help with babysitting once or twice a week or running errands while you get some much-needed rest. Don’t be afraid to ask for help if you are not getting enough sleep to function. Sleep deprivation should slowly get better over time. If it does not and instead gets worse, call your doctor.
Sleep deprivation should slowly get better over time. If it does not and instead gets worse, call your doctor.
4. Mental health and well-being
It is normal to feel a bit of sadness seven to 14 days after birth—as many as 80% of women experience these “baby blues.” After all, a mother’s hormones are shifting, there is lack of sleep, and mothers are adapting to a new baby. “But if it goes beyond 10 to 14 days and people feel an overwhelming sadness or hopelessness, or a mother has so much anxiety or worry that they even think about not existing anymore, that may be a sign of postpartum depression,” says Rosser. “Those are reasons to get help immediately.”
5. Sex and family planning
Returning to sex should be a personal decision. “Usually, it’s OK at six to eight weeks if everything is healed, or whenever Mom feels ready,” says Rosser. “What is important is that partners have open communication. Sex may be a bit different, so it is good to be open to it being different and take your time. ”
”
When it comes to contraception and family planning, Rosser urges patients to have a plan in place before the baby arrives. Do not consider breastfeeding a form of contraception. “Before you become sexually active again, talk with your provider about birth control. Many patients will opt for an IUD right after delivery so that they don’t have to worry about an unplanned pregnancy immediately after birth.”
6. Diet and exercise
It is important for new moms to nourish their bodies with healthy, whole foods (lots of fresh fruits and vegetables, lean protein, and whole grains), drink plenty of water, and begin moving their bodies as they feel ready. For those who have had a vaginal delivery or a C-section, an excellent place to start is simply walking: Go outside and walk around the block. Ease into it and build up your physical activity. Those who have had a C-section should check with their doctor about when to resume more strenuous physical activity.
Eating well and moving helps the body heal and recover. Healthy babies need healthy, well-adjusted mothers. “If Mom is not well, then she is not going to be able to care for her baby and her family the way that she might want,” says Rosser.
Healthy babies need healthy, well-adjusted mothers. “If Mom is not well, then she is not going to be able to care for her baby and her family the way that she might want,” says Rosser.
7. Chronic disease management
Postpartum visits are an opportunity to recognize risk factors for conditions like heart disease or obesity and to check that complications during pregnancy such as high blood pressure or diabetes are resolving. “We can provide risk reduction strategies and early intervention,” Rosser says. “It’s about educating, empowering, and motivating the patient and encouraging a healthy lifestyle that is consistent.”
8. Know the warning signs
One-third of maternal deaths occur after the birth of the baby, from one week through one year after delivery, according to the Centers for Disease Control and Prevention. Black women are three to four times more likely to die of a pregnancy-related cause than white women. It’s a sobering statistic that OB-GYN experts are working diligently to change by raising awareness of certain warning signs.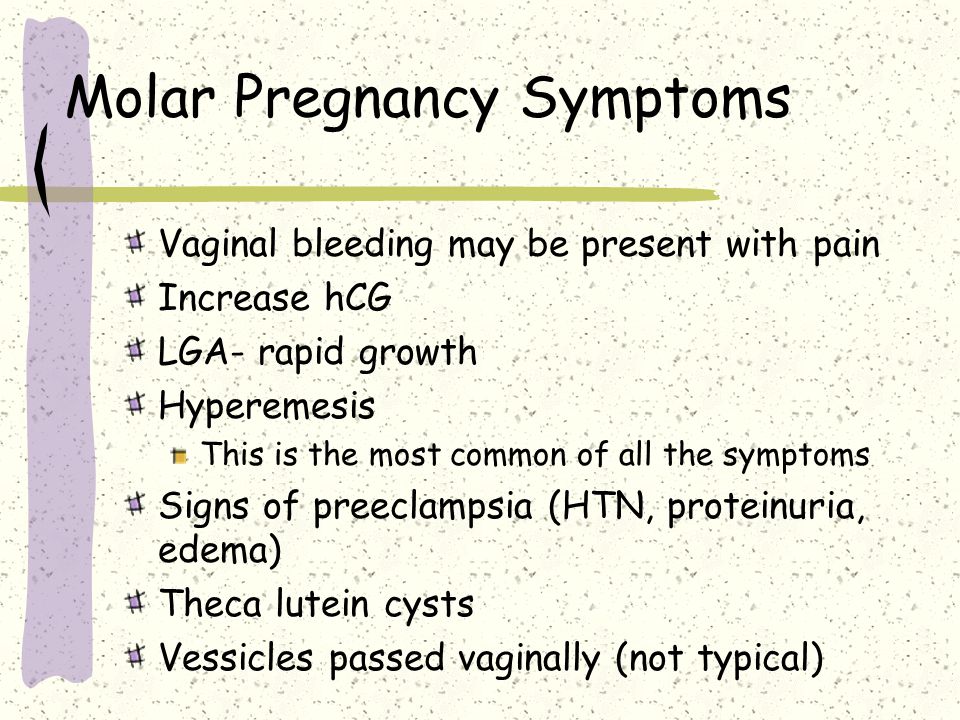
Seek medical attention immediately if you have any of the following symptoms:
- Fever or chills. This could indicate an infection vaginally (if there was a significant tear), in the womb, or of the C-section. Urinary tract infections can also be very common.
- Heavy, brisk, bright-red bleeding. Postpartum women may bleed up to four to six weeks; however, if it is heavy all at once, it could be postpartum hemorrhage. “I tell women, if you saturate a pad every hour and that’s consistent for several hours, we want to see you,” says Rosser.
- Dizziness. A symptom associated with loss of blood.
- Shortness of breath or chest pain. This might signal a blood clot like deep venous thrombosis or a pulmonary embolism.
- Severe headache. Sometimes associated with preeclampsia, which is a pregnancy complication characterized by high blood pressure or stroke.
- Swelling of the legs and feet.
 May be a sign of preeclampsia.
May be a sign of preeclampsia. - Deep sadness, thoughts of hopelessness, or thoughts about death, suicide, or harming oneself or the baby. Postpartum depression affects one in 10 mothers and is very serious.
“These symptoms can be life-threatening,” says Rosser. “Don’t ignore them or chalk them up to just being tired and postpartum. If it’s something that is out of the ordinary, please contact your doctor or go to the emergency room.”
Mothers who are considered high risk—those with diabetes, high blood pressure, obesity, or another chronic health condition—should be extra vigilant about any signs and symptoms that are not normal.
“Just as babies need care and attention during the fourth trimester, so too do mothers,” says Rosser. “Postpartum care is a crucial time to make sure Mom is safe and healthy so that the baby can be supported in the best possible way.”
Toxemia, Intestinal Problems, and Heartburn
Find out how pregnancy affects your digestive tract, which trimesters are more likely to cause indigestion and nausea, and what to do to manage them.

During pregnancy, the burden on the mother's body increases. The body needs more nutrients, the body produces additional hormones. And the growing fetus puts pressure on neighboring organs, including the stomach and intestines. We tell you what symptoms are observed in each trimester, how to cope with toxicosis and get rid of heartburn.
Contents:
- 2. Toxicosis and pregnancy
- 3. Causes, risks and treatment of diarrhea during pregnancy
- 4. Heartburn and stomach pain during pregnancy
- 5. Bloating, constipation and microbiota during pregnancy
- 6. Note
Changes in the work of the gastrointestinal tract by trimesters of pregnancy
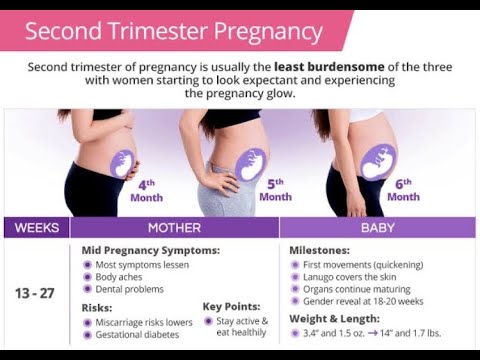
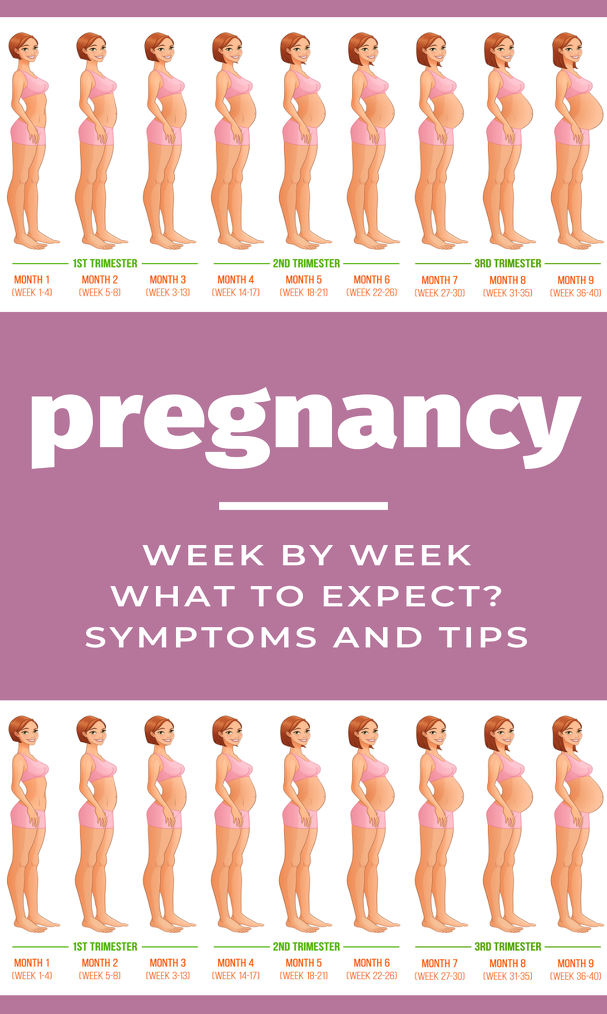
The average duration of pregnancy is 40 weeks, which are usually divided into trimesters in accordance with the stages of intrauterine development of the child.
Each trimester is accompanied by a number of changes in the body, including in the gastrointestinal tract:
| The first trimester 1–13 weeks | 900 26 weeks | Third trimester of pregnancy 27–40 weeks |
| Morning sickness Morning sickness Zapor Intestinal disorder increased appetite TREAM to certain products Acid reflux | Constipation Acid Office 9000 9000 9000 9000 Flatulence Constipation Heartburn Violation of the outflow of bile Hemorrhoids |
The Atlas genetic test will help you find out how your genes affect the level of female sex hormones necessary for fertility and pregnancy.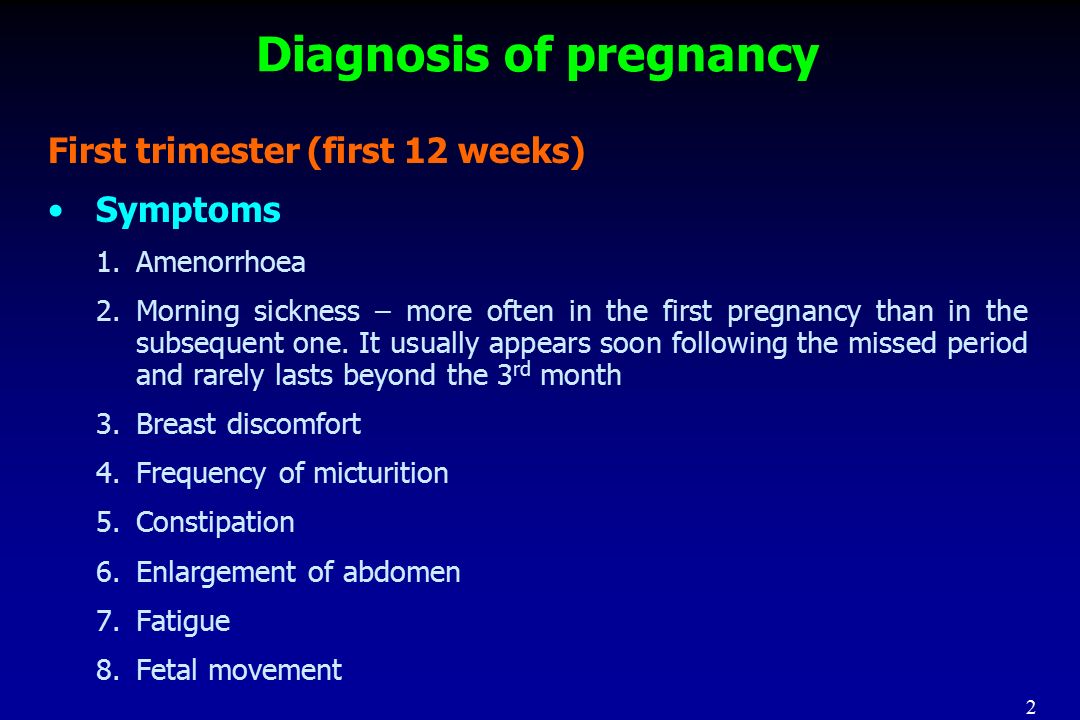
Causes of gastrointestinal problems during pregnancy
Every pregnancy is accompanied by inevitable changes in the functioning of the digestive system. They are most often caused by hormonal changes and increased stress on the organs, but they can also be associated with lifestyle and health conditions, for example:
- Sedentary lifestyle and unbalanced diet;
- Certain drugs, including calcium or aluminum antacids;
- Viral and bacterial infections;
- Intolerance to certain nutrients and allergic reactions;
- Stress;
- Diseases of the thyroid gland.
If you have chronic diseases of the gastrointestinal tract and you are planning a pregnancy, try to consult your doctor in advance. Symptoms of conditions such as irritable bowel syndrome (IBS) or acid reflux are more likely to get worse during pregnancy. Your doctor will help prepare your body and create a prevention plan to help relieve symptoms during this time.
Irritable bowel syndrome, or IBS, is a functional bowel disease that causes frequent abdominal pain, impaired peristalsis, bloating, constipation, or diarrhea.
Morning sickness, vomiting and general malaise during pregnancy
Morning sickness and morning sickness during early pregnancy are common, because the body undergoes important changes necessary for the development of the child.
up to 90%
women experience nausea during pregnancy
Doctors find it difficult to say with certainty why pregnant women feel sick in the morning. The main theory is hormonal changes. But there are some patterns associated with an increased risk of morning sickness:
- Multiple pregnancy;
- Toxicosis during previous pregnancy;
- History of morning sickness during pregnancy in close relatives;
- Tendency to motion sickness in transport;
- Use of oral contraceptives containing estrogen before pregnancy;
- Frequent migraines;
- BMI 30 and above;
- Elevated levels of stress hormones
Risks of severe morning sickness and how to reduce nausea
Nausea and vomiting are usually not associated with a risk for mother and child and disappear by 16-20 weeks of pregnancy, but it is not necessary to wait so long - there are ways that can help reduce nausea and enjoy the process of waiting for a new person:
- Get plenty of rest - fatigue increases toxicosis;
- Avoid smells and foods that cause nausea;
- Eat something right after waking up.
 A toast or a slice of bread will help reduce nausea;
A toast or a slice of bread will help reduce nausea; - Avoid hunger - empty stomach increases nausea. Eat small meals often, prefer low-fat, high-carbohydrate foods;
- Try ginger - studies show it helps with nausea;
- Sip as often as possible and prefer still water.
In rare cases, pregnant women may develop hyperemesis gestationis or excessive vomiting. This is a serious condition that can lead to dehydration, kidney damage, seizures, abnormal heart rhythms, and even death.
Signs of dehydration include dry mouth, dizziness, dark urine, infrequent urination and/or dizziness.
Symptoms of excessive pregnancy vomiting:
- frequent nausea for a long time and regular vomiting after meals;
- dry skin and lips;
- sudden weight loss;
- low blood pressure (below 90/60).
If symptoms of excessive pregnancy vomiting occur, do not wait until the condition resolves on its own.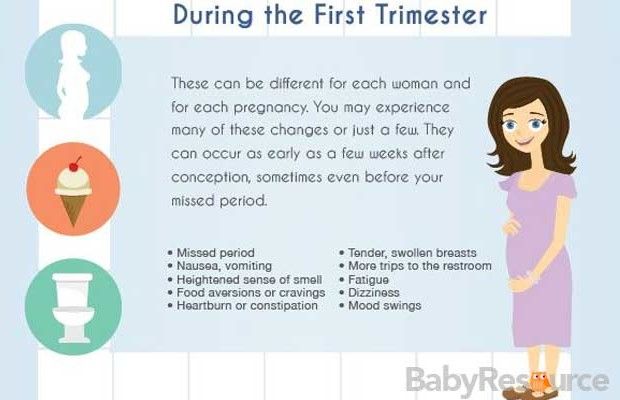 It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
0.5–2%
pregnant women experience excessive vomiting
Diarrhea in pregnancy
The word "diarrhea" comes from the Greek language and literally means "to flow through". This is a condition during which bowel movements or bowel movements occur three times a day or more often. This phenomenon is especially typical for the third trimester of pregnancy, but it can also occur earlier.
Symptoms of diarrhea:
- Three or more bowel movements per day
- Urgent urge to have a bowel movement
- Abdominal pain and cramps
- Bloating
Causes of diarrhea during pregnancy poisoning, dysbacteriosis, bacterial and viral infections:
| Gastroenteritis | Use of lactose and gluten in case of intolerance to these nutrients |
| Bacterial infections: listeriosis or salmonella | Chronic gastrointestinal diseases: Crohn's disease, IBS, ulcerative colitis |
| Certain antibiotics and antacids to reduce acidity | Laxatives |
| Sugar substitutes such as sorbitol | Overconsumption of certain foods |
Tip: If you have recently returned from a holiday in an exotic country with nausea and diarrhea and find out you are pregnant, see your doctor as soon as possible.
Gastroenteritis
One common cause of diarrhea during pregnancy is gastroenteritis or stomach flu. It is caused by bacterial or viral infections: norovirus, rotavirus, E. coli, salmonella, which enter the body through contact with contaminated surfaces, dishes, food and water.
Gastroenteritis usually lasts about three days. However, severe illness is a health hazard, especially during pregnancy, as it can cause dehydration, electrolyte imbalance, and lead to preterm labor.
The main symptoms of gastroenteritis are diarrhea without blood, nausea and vomiting, stomach cramps and pain, slight fever, headache and muscle pain.
Take extra precautions to reduce your risk of getting sick: frequent handwashing and surface disinfection. If the expectant mother has small children, they are not recommended to use the same cutlery.
Risks of diarrhea during pregnancy
Usually diarrhea during pregnancy is not a cause for concern. However, you should consult a doctor if the following symptoms occur during this period:
However, you should consult a doctor if the following symptoms occur during this period:
- Diarrhea for more than two days;
- Blood or mucus stools;
- Sudden weight loss;
- Pain in the abdomen;
- Dehydration.
How to treat diarrhea during pregnancy
If you have diarrhea during pregnancy, drink plenty of fluids, avoid foods high in fat and sugar, avoid dairy products, and caffeinated drinks.
Dehydration is a serious risk, especially during pregnancy, so electrolyte balance should be restored first with fluids and simple foods:
| Moderate fruit juices | Drinks without alcohol and caffeine |
| Bananas | Potato |
| Rice | Toast |
| Rusks | Light soups and broths |
| Pasta | Applesauce |
Find out about your body's ability to break down lactose and gluten with the Atlas Microbiota Test.
Stomach pain and heartburn during pregnancy
Many women experience stomach pain during pregnancy, especially the upper part of the stomach, as well as heartburn - a burning sensation in the chest and esophagus.
This is more common in the third trimester, after about 27 weeks. This is an unpleasant but natural phenomenon during pregnancy: the baby grows inside the uterus and presses on other organs, including the stomach. And hormones cause the muscles to relax, which causes acid from the stomach to enter the esophagus and irritate it. In addition, pain can be caused by problems with certain organs such as the gallbladder, or inflammation of the pancreas.
Symptoms of heartburn during pregnancy:
- Burning in chest and esophagus;
- Feeling of overeating, heaviness or bloating;
- Belching, including with acid and/or food particles;
- Nausea.
It is unlikely that you will be able to avoid cramps and heartburn during pregnancy. However, some tips can help reduce their frequency:
However, some tips can help reduce their frequency:
Nutrition : try to avoid overeating - eat easily digestible food in small portions; do not eat three hours before bedtime; watch your posture while eating - so the pressure on your stomach will be less.
Smoking and alcohol: In addition to known harms to mothers and babies, tobacco smoke also relaxes the muscles in the lower esophagus, allowing acid to enter the esophagus. And alcohol provokes heartburn and acid reflux.
Although stomach pain and heartburn often accompany pregnancy, abdominal pain, especially in the third trimester, should be taken seriously. It can be a sign of preterm labor or placental abruption, and puts mother and baby at risk.
If you experience severe abdominal pain during pregnancy that is accompanied by the following symptoms, seek medical attention as soon as possible:
| Abdominal pain and fever | Bleeding |
| Regular convulsions | Unusual vaginal discharge / spotting |
| Vomiting | Low back pain |
| Pain or burning when urinating | Severe pain that lasts 30-60 minutes |
Bloating, constipation and microbiota during pregnancy
Excessive gas and constipation during pregnancy can be caused by hormonal changes, such as increased production of progesterone.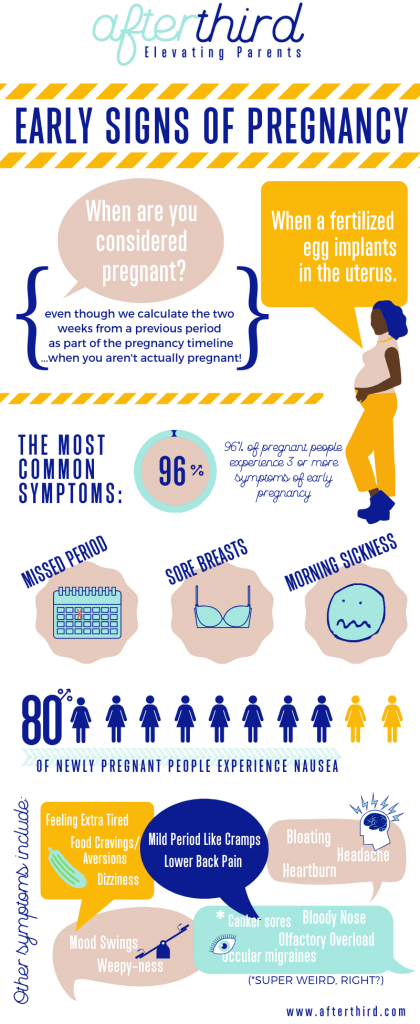 This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
Flatulence - bloating of the abdomen due to the accumulation of gases.
Here are a few simple rules that will help improve intestinal motility and avoid constipation and bloating:
- If you don't usually eat a lot of fiber and indigestible foods like legumes, try to gradually introduce them into your diet;
- Avoid carbonated drinks and fatty foods;
- Move more;
- Drink plenty of fluids.
If bloating and constipation are accompanied by severe pain that lasts more than 30 minutes, or if you have been constipated for two or more weeks, see your doctor.
Gut microbiota and bacteria during pregnancy
A woman's body goes through many changes during pregnancy, and this can affect the microbiota, the bacterial ecosystem that lives in the gut.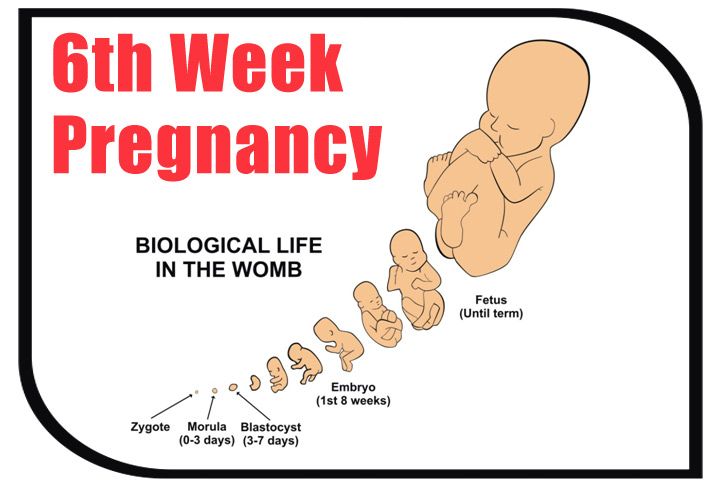 Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
The additional influx of female hormones that accompanies pregnancy alters gut function and affects the microbiota. This is good, because the bacterial community is constantly adjusting to external and internal conditions in order to keep up with the needs of the body.
To keep your gut bacteria running smoothly, they need your help. Provide them with healthy foods and plant fibers. Fruits, vegetables, whole grains, nuts, and seeds contain prebiotics, special substances that beneficial bacteria feed on. When properly balanced, the bacteria even increase your body's defenses against harmful microorganisms that can cause gastroenteritis during pregnancy.
The Atlas Microbiota Test helps you understand how to prepare your gut for future pregnancies and reduce the risk of digestive problems.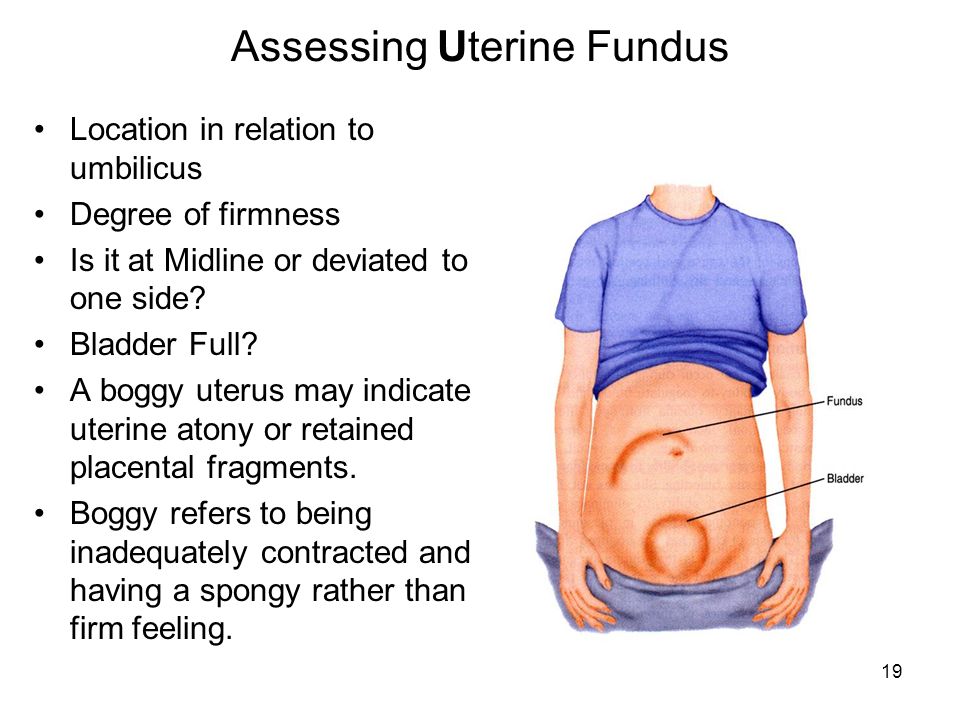
☝️ Take note
Now you have all the necessary knowledge and tools to help you deal with digestive problems during pregnancy. They are quite varied and quite natural, but in some cases it is necessary to immediately seek medical help:
- Vomiting blood;
- Blood in stool;
- Diarrhea for more than two days;
- Constipation for more than two weeks;
- Sudden weight loss;
- Severe pain interfering with daily activities;
- Difficulty breathing;
- Pain when swallowing or difficulty swallowing;
- Excessive fatigue.
More articles on the causes of digestive problems on the blog:
- 7 foods that cause gas and bloating
- Leaky intestines
- When the intestines are upset
- 08 Mayo Clinic, sick0108
- Lindsey J Wegrzyniak, Treatment of Hyperemesis Gravidarum, 2012
- Edwards A. et al., The Maternal Gut Microbiome During Pregnancy, 2018
- National Health and Safety (NHS), Vomiting and morning sickness in pregnancy
- Kudzai Kanhutu, Travel and pregnancy: an infectious diseases perspective, 2011
- CDC, Pregnant travelers
- U.
 S. Department of Health and Human Services, Agency for healthcare research and quality, Abdominal Pain in Early Pregnancy
S. Department of Health and Human Services, Agency for healthcare research and quality, Abdominal Pain in Early Pregnancy - Robyn Horsager-Boehrer, M.D., UT Southwestern Medical Center, Should pregnant moms be concerned about gastroenteritis?, 2018
- International Foundation for Gastrointestinal Disorders, Pregnancy and Irritable Bowel Syndrome, 2016
- NHS Vomiting and morning sickness in pregnancy
- NHS, Severe vomiting in pregnancy
- Lindsey J Wegrzyniak et al., Treatment of Hyperemesis Gravidarum, 2012
- Karen Miles, Diarrhea during pregnancy, 2020
- Cleveland Clinic, Diarrhea
- You and your hormones, Progesterone
- Traci C. Johnson, MD, Pregnancy, Bloating, 2020
Critical stages of pregnancy - why are they dangerous?
Services
Virtual tour. Clinic "ARNIKA"
The wonderful period of waiting for a baby for almost every woman is far from serene: how many anxieties, worries and doubts arise in expectant mothers at this time - they simply cannot be counted. In most cases, all fears are in vain - the baby develops and grows safely. However, it must be remembered that there are also so-called critical periods of pregnancy, when inattention to oneself and one's body can lead to a disastrous result - its spontaneous termination.
In most cases, all fears are in vain - the baby develops and grows safely. However, it must be remembered that there are also so-called critical periods of pregnancy, when inattention to oneself and one's body can lead to a disastrous result - its spontaneous termination.
First trimester
The beginning of a new life in a woman's body, or 2-3 weeks of pregnancy, is considered the first critical period. This is due to the fact that the egg can be fertilized, but due to changes as a result of inflammation, hormonal imbalances, the presence of nodes, scars, fibroids or synechia on the inner mucous membrane of the uterus, implantation does not occur, the embryo dies and is removed from the mother's body during menses. However, even if implantation has occurred, the embryo may stop developing and spontaneous miscarriage at an early stage , and the main reason for this course of events is chromosomal abnormalities.
The second critical period of the first trimester begins at 8 and ends at 12 weeks of gestation. At this time, the main cause of interruption is considered to be hormonal deficiency, which disrupts the process of placental formation. This condition may be associated with reduced work of the corpus luteum of the ovaries, excessive production of androgens by the adrenal glands - male sex hormones, as well as malfunctions of the pituitary gland or thyroid gland. The threat of abortion can be eliminated with the help of properly selected and timely prescribed hormonal treatment, which will allow the baby to safely reach the due date.
At this time, the main cause of interruption is considered to be hormonal deficiency, which disrupts the process of placental formation. This condition may be associated with reduced work of the corpus luteum of the ovaries, excessive production of androgens by the adrenal glands - male sex hormones, as well as malfunctions of the pituitary gland or thyroid gland. The threat of abortion can be eliminated with the help of properly selected and timely prescribed hormonal treatment, which will allow the baby to safely reach the due date.
In addition, throughout the first trimester of pregnancy, the fetus may stop developing due to the following adverse environmental factors:
- harmful working conditions
- bad habits
- physical effects - radiation, vibration, intense sports training, etc.
- acute infectious diseases (influenza, cytomegalovirus, herpes, rubella and others)
- severe stressful situations
And even if the fetus develops further, the negative impact of most of these factors can appear after a few months of pregnancy or even after the baby is born: these can be anatomical disorders or severe malformations. Therefore, the entire first trimester of the development of a new life can be considered "critical".
Therefore, the entire first trimester of the development of a new life can be considered "critical".
Second trimester
The third critical period of pregnancy occurs at 18-24 weeks of pregnancy and is largely associated with the active growth of the uterus. At this time, spontaneous interruption most often occurs due to isthmic-cervical insufficiency (ICI), as a result of which the fetal egg descends under the influence of gravity, loses its integrity and triggers the mechanism of labor activity. However, shortening and expansion of the cervical canal, detected in time, allows suturing the cervix or installing an obstetric pessary and safely prolonging the pregnancy. Here we should also remember about infectious diseases, including intrauterine infection, which can disrupt the functions of the placenta, lead to the outflow of water from the fetal bladder and late miscarriage.
Another common reason for interrupting the process of bearing a fetus at this time is placenta previa or its low location: for various reasons, it can exfoliate, cause severe bleeding and death of the fetus. In addition, at this time, pregnancy may stop developing due to violations in the development of the brain and the most important functional systems of the baby, caused by the harmful effects of various negative factors on them in the first trimester.
In addition, at this time, pregnancy may stop developing due to violations in the development of the brain and the most important functional systems of the baby, caused by the harmful effects of various negative factors on them in the first trimester.
Third trimester
In this trimester - at 28-32 weeks - the fourth critical period takes place. The threat of premature birth may occur due to insufficiency of the placenta, its premature detachment, severe forms of late toxicosis of pregnant women, ICI and various hormonal disorders. In addition, due to the overdistension of the uterus, most multiple pregnancies end at this time. Children born during this period are already viable, but they need long-term qualified medical care.
In addition to all the periods listed above, the critical periods for women who have had reproductive losses in the past are the days of planned menstruation, miscarriages or “fading” of pregnancies. Doctors believe that during these periods the body can “remember” the need for hormonal changes, so they carefully monitor the condition of the expectant mother and baby and prescribe treatment in a timely manner if any threat arises.