Where is umbilical cord attached to in the mother
What is the placenta? | Pregnancy Birth and Baby
beginning of content4-minute read
Listen
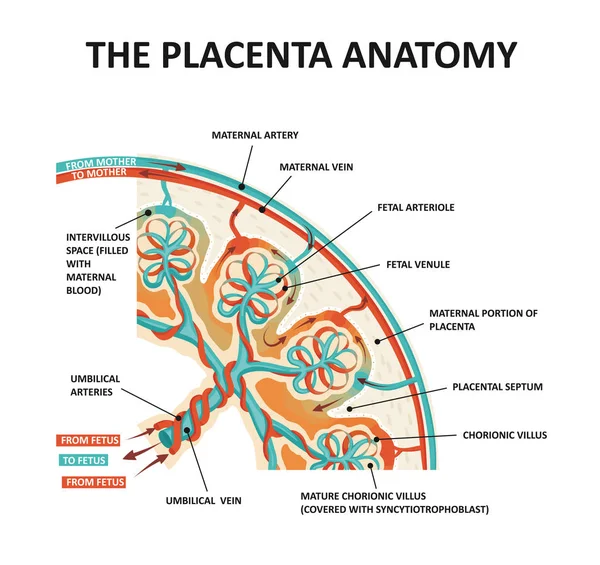
The placenta is crucial to keeping your baby alive and well during pregnancy. It is an organ attached to the lining of the womb that delivers oxygen and nutrients to the growing baby.
About the placenta
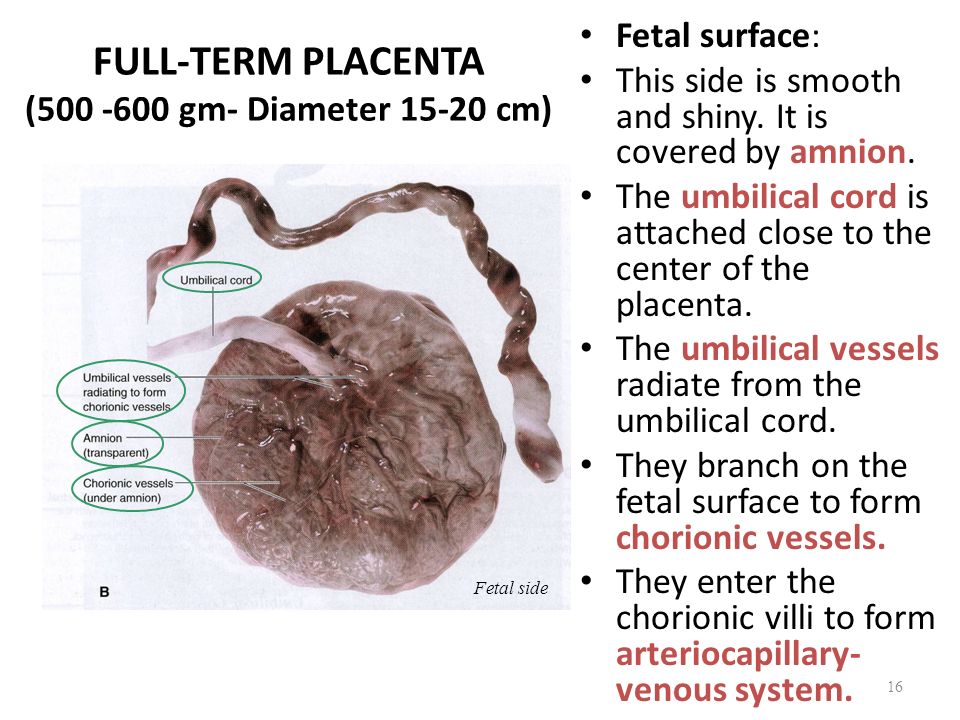
The placenta is a large organ that develops during pregnancy. It is attached to the wall of the uterus, usually at the top or side. The umbilical cord connects the placenta to your baby.
Blood from the mother passes through the placenta, filtering oxygen, glucose and other nutrients to your baby via the umbilical cord. The placenta also filters out substances that could be harmful to your baby and removes carbon dioxide and waste products from your baby’s blood.
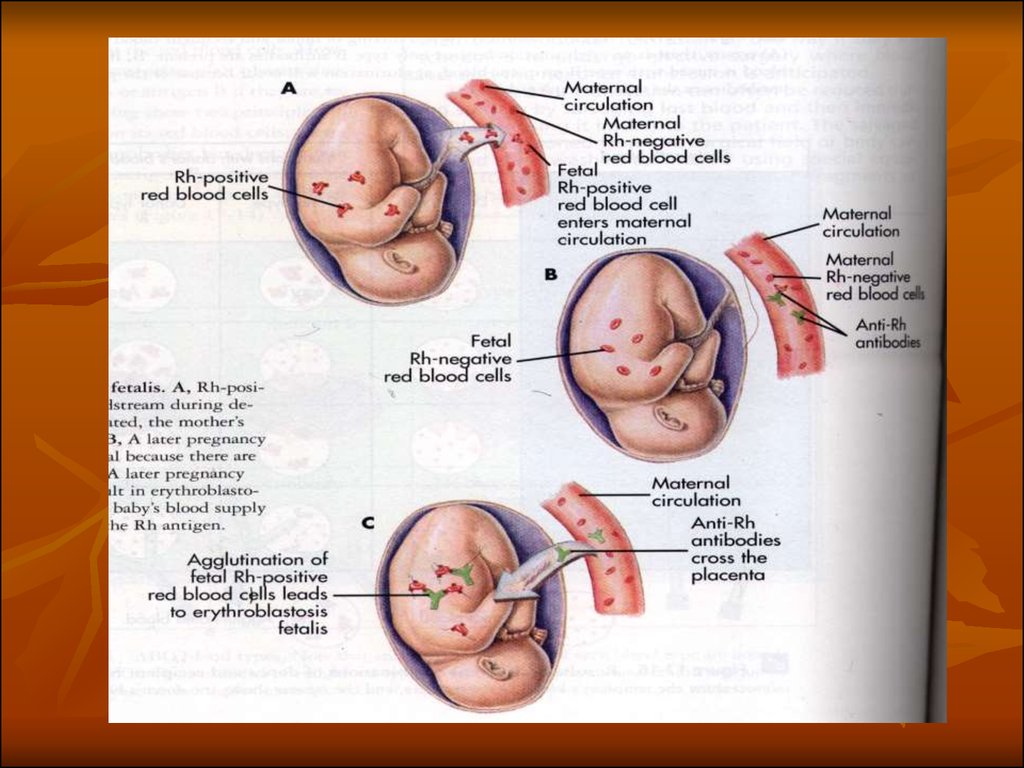
The placenta produces a number of hormones that are needed during pregnancy, such as lactogen, oestrogen and progesterone. It keeps the mother’s blood separate from the baby’s blood to protect the baby against infections. Towards the end of the pregnancy, the placenta passes on antibodies to protect the baby after birth.
Alcohol, nicotine and other drugs and medicines can cross the placenta and damage your baby.
What happens to the placenta during pregnancy?
The placenta often develops low in the womb but moves to the side or up as the womb stretches. The position of the placenta will be checked at your 18-week ultrasound.
The placenta is expelled from your body after the birth, usually about 5 to 30 minutes after your baby is born. This is called the third stage of labour.
After the baby is born you will continue to have mild contractions. You will have to give one more push to deliver the placenta. Sometimes your abdomen will be massaged or you will be given an injection of oxytocin and the umbilical cord will be gently pulled to help deliver the placenta.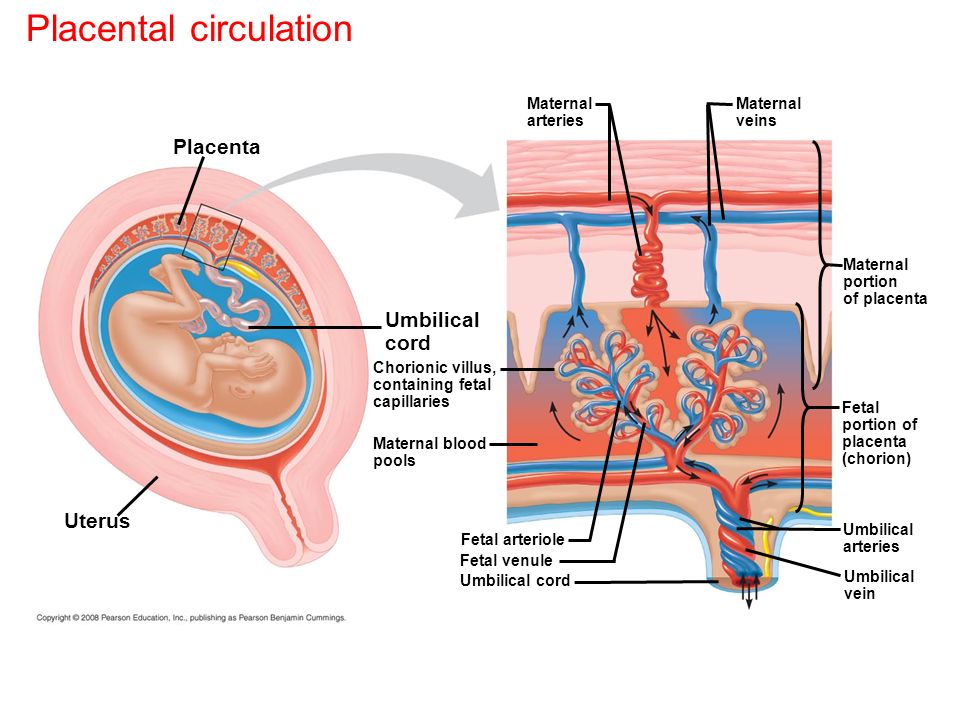
If you have a caesarean section, the doctor will remove the placenta at the same time.
It is important that the whole placenta comes out after pregnancy. If any fragments of the placenta stay inside, they will have to be surgically removed to prevent bleeding and infection.
How to keep your placenta healthy
It is important to visit your healthcare provider regularly during pregnancy to check for any problems with your placenta.
Tell your doctor if you have had problems with the placenta in a previous pregnancy, or if you have had any surgery to your womb.
Don’t smoke, drink alcohol or take illegal drugs during pregnancy because this increases the likelihood you will have problems with the placenta. Always consult your doctor before you take any medicines, including over-the-counter medicines, natural therapies and supplements, while you are pregnant.
Speak with your doctor or midwife if you have any concerns, or if you experience:
- severe abdominal or back pain
- vaginal bleeding
- contractions
- any trauma to your abdomen, for example from a fall or car accident
Placenta complications
Problems with the placenta can potentially be dangerous for both mother and baby:
- Placenta accreta: When the placenta grows too deeply into the wall of the uterus.
 This can lead to massive blood loss during or after delivery and can be life-threatening.
This can lead to massive blood loss during or after delivery and can be life-threatening. - Placental abruption: When the placenta peels away from the wall of the womb before delivery. This can cause bleeding and will mean your baby may not be getting all the nutrients they need. In some cases, an early delivery may be needed.
- Placenta praevia: When the placenta partially or totally covers the cervix, the opening through which the baby will come out. This condition is more common early in pregnancy and often resolves as the placenta moves higher in the uterus as the uterus grows. If the placenta is still covering the cervix close to the time of delivery, a caesarean section will be necessary.
- Placental insufficiency: When the placenta doesn’t work properly during pregnancy, depriving the baby of oxygen and nutrients. This can affect the growth of the baby.
- Retained placenta: The placenta may not come out after the birth because it is blocked by the cervix or it is still attached to the uterus.
 This can cause severe infection or blood loss, and can be life-threatening.
This can cause severe infection or blood loss, and can be life-threatening.
Options for the placenta after the birth
In some cultures, families bury the placenta in a special place.
There is also a rare practice, known as placentophagy, in which women cook and eat the placenta. Some commercial service providers will offer to turn your placenta into capsules for you to swallow.
However, these practices should be treated with caution since there is no regulation in Australia either of these products or the providers of placenta pills.
Recent research shows there are no known health benefits from eating the placenta, but there may be a risk of infection from poor production standards.
Sources:
Mayo Clinic (Is it safe to eat my placenta?), Archives of Women’s Mental Health (Placentophagy: therapeutic miracle or myth?), Women’s and Children’s Health Network (Routine antenatal tests), RANZCOG (Placenta accreta), Mayo Clinic (Placenta: how it works, what's normal)Learn more here about the development and quality assurance of healthdirect content.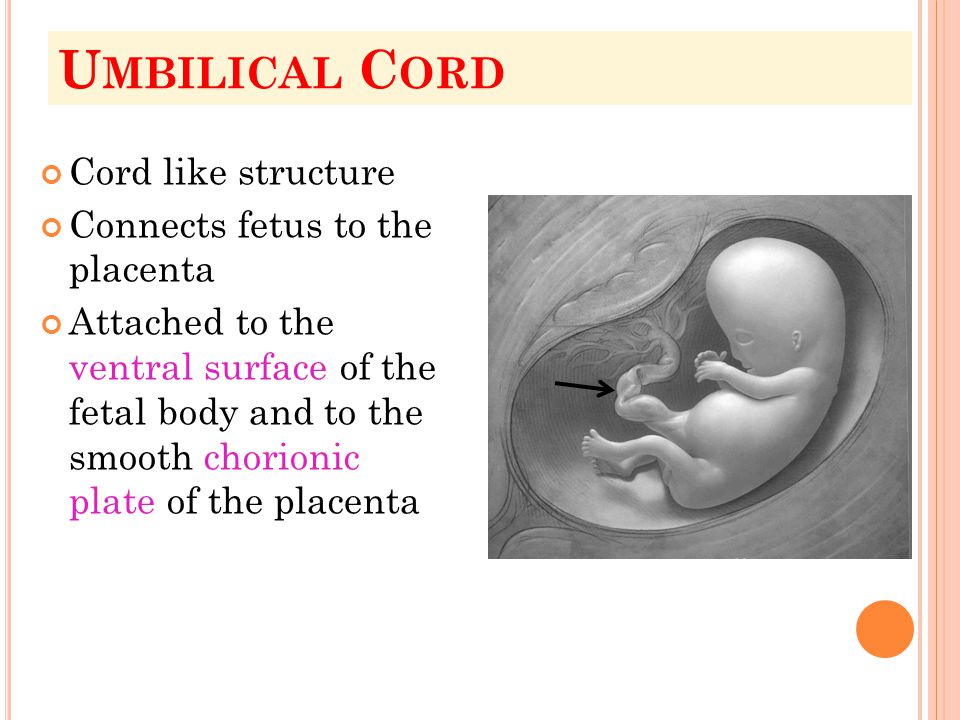
Last reviewed: August 2020
Back To Top
Related pages
- Mum's first 24 hours after birth
- Giving birth - stages of labour
- Placenta complications in pregnancy
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.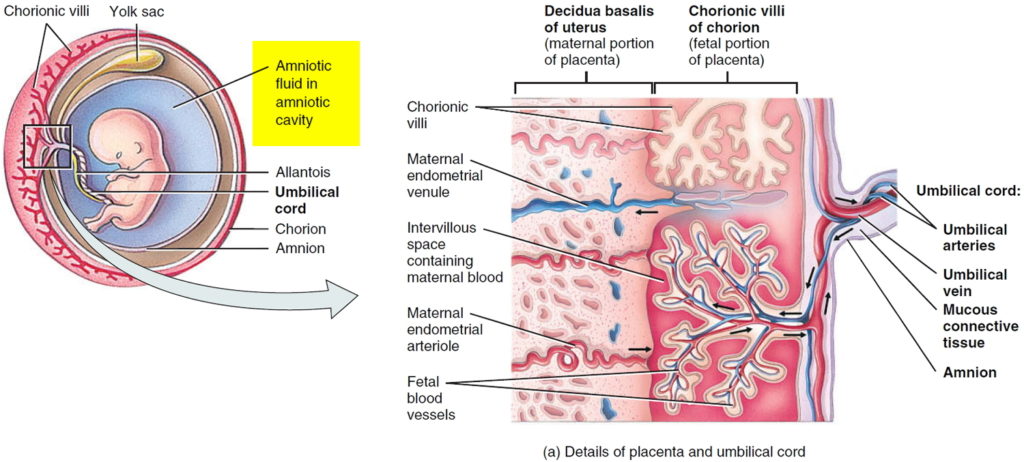
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Umbilical cord abnormalities | March of Dimes
What's happening in your area
Find out about local events, news, programs, and more.
Close X
Now playing: Bleeding and spotting during pregnancyGestational diabetesGestational hypertension and preeclampsiaSeasonal flu and pregnancy
Topics
In This TopicView More
The umbilical cord is a narrow tube-like structure that connects the developing baby to the placenta.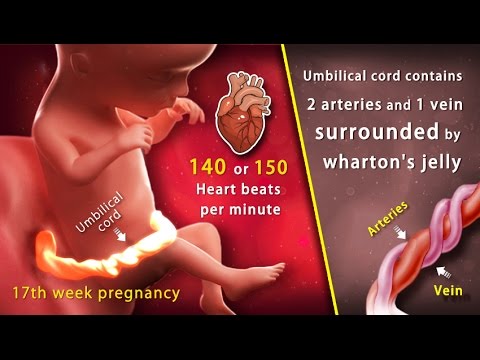 The cord is sometimes called the baby's “supply line” because it carries the baby's blood back and forth, between the baby and the placenta. It delivers nutrients and oxygen to the baby and removes the baby's waste products.
The cord is sometimes called the baby's “supply line” because it carries the baby's blood back and forth, between the baby and the placenta. It delivers nutrients and oxygen to the baby and removes the baby's waste products.
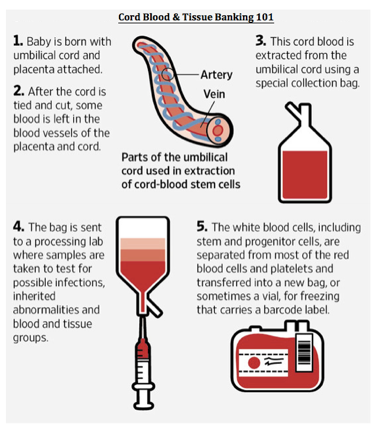
The umbilical cord begins to form at 5weeks after conception. It becomes progressively longer until 28 weeks of pregnancy, reaching an average length of 22 to 24 inches (1). As the cord gets longer, it generally coils around itself. The cord contains three blood vessels: two arteries and one vein.
- The vein carries oxygen and nutrients from the placenta (which connects to the mother's blood supply) to the baby.
- The two arteries transport waste from the baby to the placenta (where waste is transferred to the mother's blood and disposed of by her kidneys).
A gelatin-like tissue called Wharton's jelly cushions and protects these blood vessels.
A number of abnormalities can affect the umbilical cord. The cord may be too long or too short.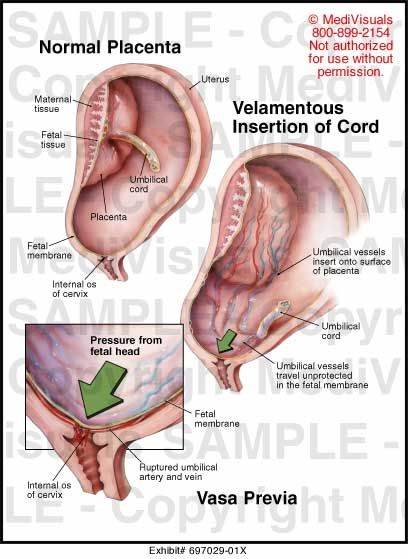 It may connect improperly to the placenta or become knotted or compressed. Cord abnormalities can lead to problems during pregnancy or during labor and delivery.
It may connect improperly to the placenta or become knotted or compressed. Cord abnormalities can lead to problems during pregnancy or during labor and delivery.
In some cases, cord abnormalities are discovered before delivery during an ultrasound. However, they usually are not discovered until after delivery when the cord is examined directly. The following are the most frequent cord abnormalities and their possible effects on mother and baby.
What is a single umbilical artery?
About 1 percent of singleton and about 5 percent of multiple pregnancies (twins, triplets or more) have an umbilical cord that contains only two blood vessels, instead of the normal three. In these cases, one artery is missing (2). The cause of this abnormality, called single umbilical artery, is unknown.
Studies suggest that babies with single umbilical artery have an increased risk for birth defects, including heart, central nervous system and urinary-tract defects and chromosomal abnormalities (2, 3). A woman whose baby is diagnosed with single umbilical artery during a routine ultrasound may be offered certain prenatal tests to diagnose or rule out birth defects. These tests may include a detailed ultrasound, amniocentesis (to check for chromosomal abnormalities) and in some cases, echocardiography (a special type of ultrasound to evaluate the fetal heart). The provider also may recommend that the baby have an ultrasound after birth.
A woman whose baby is diagnosed with single umbilical artery during a routine ultrasound may be offered certain prenatal tests to diagnose or rule out birth defects. These tests may include a detailed ultrasound, amniocentesis (to check for chromosomal abnormalities) and in some cases, echocardiography (a special type of ultrasound to evaluate the fetal heart). The provider also may recommend that the baby have an ultrasound after birth.
What is umbilical cord prolapse?
Umbilical cord prolapse occurs when the cord slips into the vagina after the membranes (bag of waters) have ruptured, before the baby descends into the birth canal. This complication affects about 1 in 300 births (1). The baby can put pressure on the cord as he passes through the cervix and vagina during labor and delivery. Pressure on the cord reduces or cuts off blood flow from the placenta to the baby, decreasing the baby's oxygen supply. Umbilical cord prolapse can result in stillbirth unless the baby is delivered promptly, usually by cesarean section.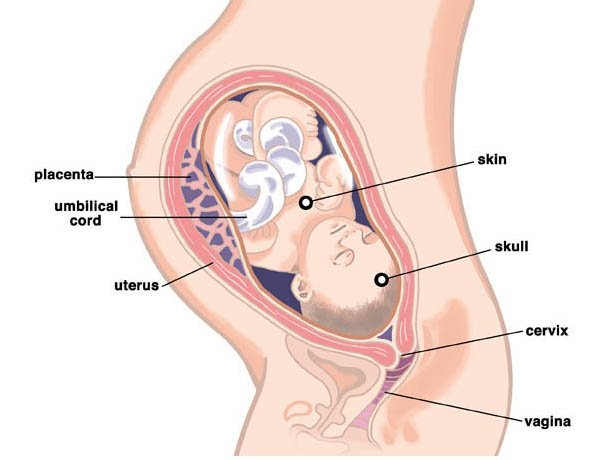
If the woman's membranes rupture and she feels something in her vagina, she should go to the hospital immediately or, in the United States, call 911. A health care provider may suspect umbilical cord prolapse if the bay develops heart rate abnormalities after the membranes have ruptured. The provider can confirm a cord prolapse by doing a pelvic examination. Cord prolapse is an emergency. Pressure on the cord must be relieved immediately by lifting the presenting fetal part away from the cord while preparing the woman for prompt cesarean delivery.
The risk of umbilical cord prolapse increases if:
- The baby is in a breech (foot-first) position.
- The woman is in preterm labor.
- The umbilical cord is too long.
- There is too much amniotic fluid.
- The provider ruptures the membranes to start or speed up labor.
- The woman is delivering twins vaginally. The second twin is more commonly affected.
What is vasa previa?
Vasa previa occurs when one or more blood vessels from the umbilical cord or placenta cross the cervix underneath the baby. The blood vessels, unprotected by the Wharton's jelly in the umbilical cord or the tissue in the placenta, sometimes tear when the cervix dilates or the membranes rupture. This can result in life-threatening bleeding in the baby. Even if the blood vessels do not tear, the baby may suffer from lack of oxygen due to pressure on the blood vessels. Vasa previa occurs in 1 in 2,500 births (4).
When vasa previa is diagnosed unexpectedly at delivery, more than half of affected babies are stillborn (4). However, when vasa previa is diagnosed by ultrasound earlier in pregnancy, fetal deaths generally can be prevented by delivering the baby by cesarean section at about 35 weeks of gestation (4).
Pregnant women with vasa previa sometimes have painless vaginal bleeding in the second or third trimester. A pregnant woman who experiences vaginal bleeding should always report it to her health care provider so that the cause can be determined and any necessary steps taken to protect the baby.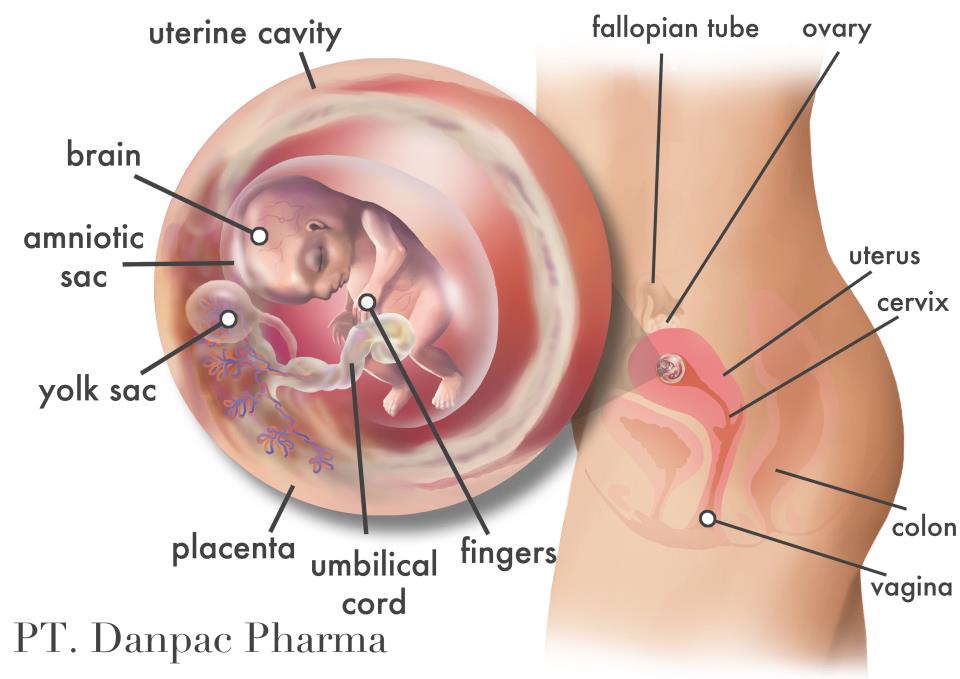
A pregnant woman may be at increased risk for vasa previa if she:
- Has a velamentous insertion of the cord (the umbilical cord inserts abnormally into the fetal membranes, instead of the center of the placenta)
- Has placenta previa (a low-lying placenta that covers part or all of the cervix) or certain other placental abnormalities
- Is expecting more than one baby
What is nuchal cord?
About 25 percent of babies are born with a nuchal cord (the umbilical cord wrapped around the baby's neck) (1). A nuchal cord, also called nuchal loops, rarely causes any problems. Babies with a nuchal cord are generally healthy.
Sometimes fetal monitoring shows heart rate abnormalities during labor and delivery in babies with a nuchal cord. This may reflect pressure on the cord. However, the pressure is rarely serious enough to cause death or any lasting problems, although occasionally a cesarean delivery may be needed.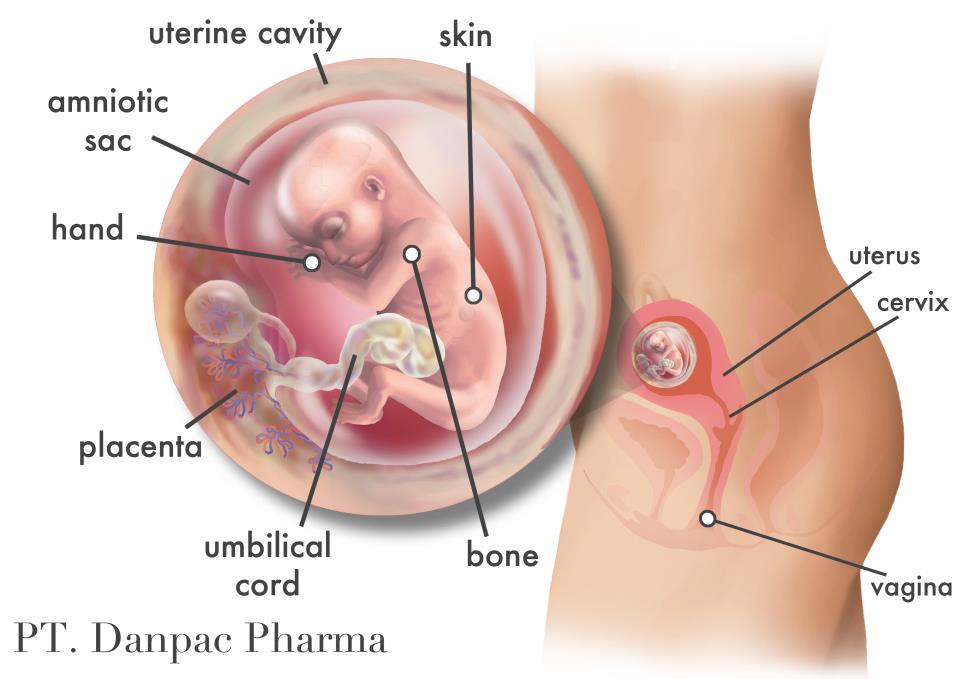
Less frequently, the umbilical cord becomes wrapped around other parts of the baby's body, such as a foot or hand. Generally, this doesn't harm the baby.
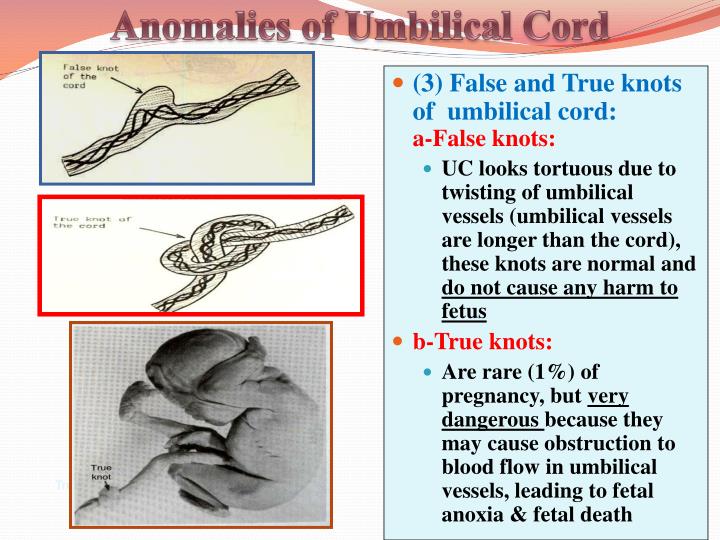
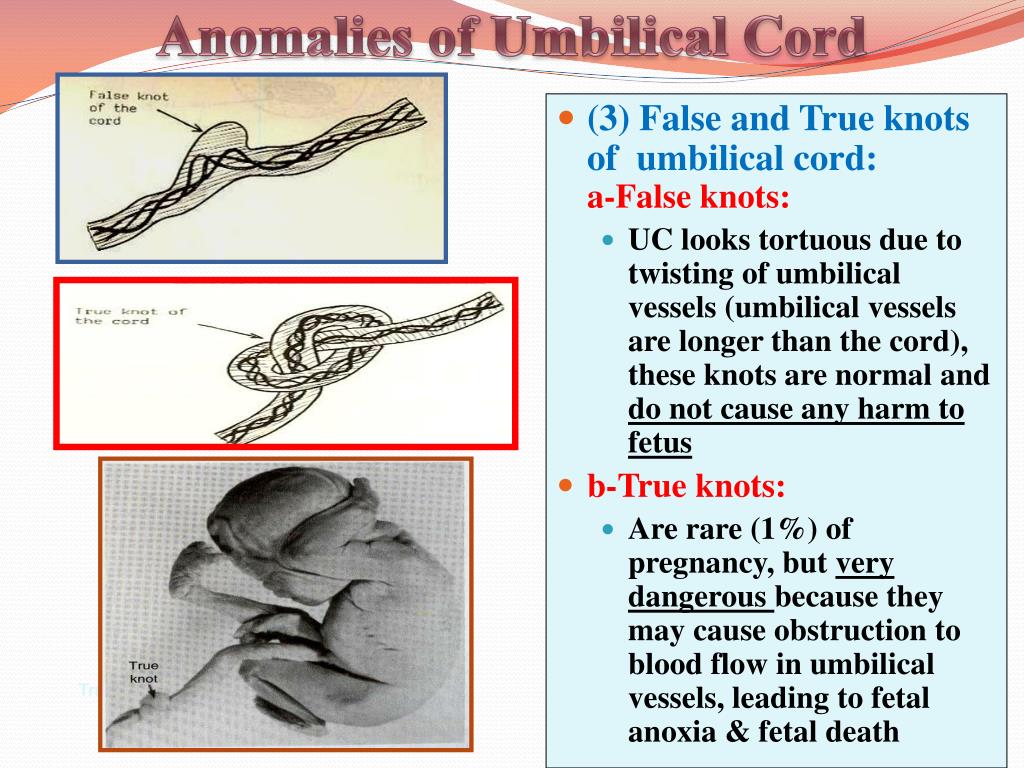
What are umbilical cord knots?
About 1 percent of babies are born with one or more knots in the umbilical cord (1). Some knots form during delivery when a baby with a nuchal cord is pulled through the loop. Others form during pregnancy when the baby moves around. Knots occur most often when the umbilical cord is too long and in identical-twin pregnancies. Identical twins share a single amniotic sac, and the babies' cords can become entangled.
As long as the knot remains loose, it generally does not harm the baby. However, sometimes the knot or knots can be pulled tight, cutting off the baby's oxygen supply. Cord knots result in miscarriage or stillbirth in 5 percent of cases (1). During labor and delivery, a tightening knot can cause the baby to have heart rate abnormalities that are detected by fetal monitoring.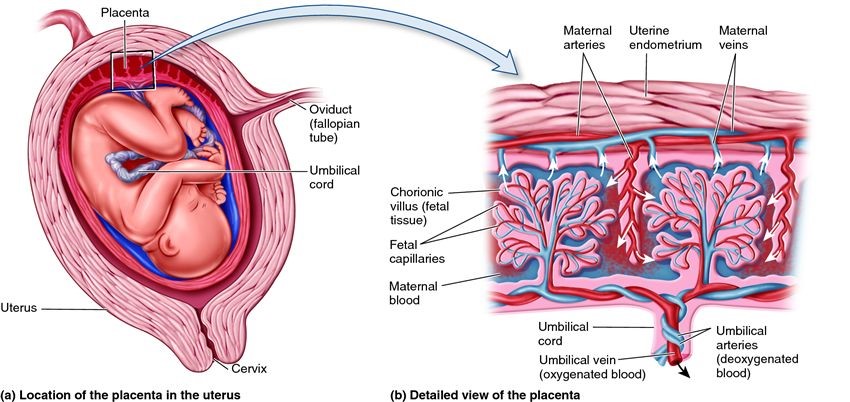 In some cases, a cesarean delivery may be necessary.
In some cases, a cesarean delivery may be necessary.
What is an umbilical cord cyst?
Umbilical cord cysts are outpockets in the cord. They are found in about 3 percent of pregnancies (2).
There are true and false cysts:
- True cysts are lined with cells and generally contain remnants of early embryonic structures.
- False cysts are fluid-filled sacs that can be related to a swelling of the Wharton's jelly.
Studies suggest that both types of cysts are sometimes associated with birth defects, including chromosomal abnormalities and kidney and abdominal defects (2). When a cord cyst is found during an ultrasound, the provider may recommend additional tests, such as amniocentesis and a detailed ultrasound, to diagnose or rule out birth defects.
Does the March of Dimes support research on umbilical cord abnormalities?
The March of Dimes continues to support research aimed at preventing umbilical cord abnormalities and the complications they cause.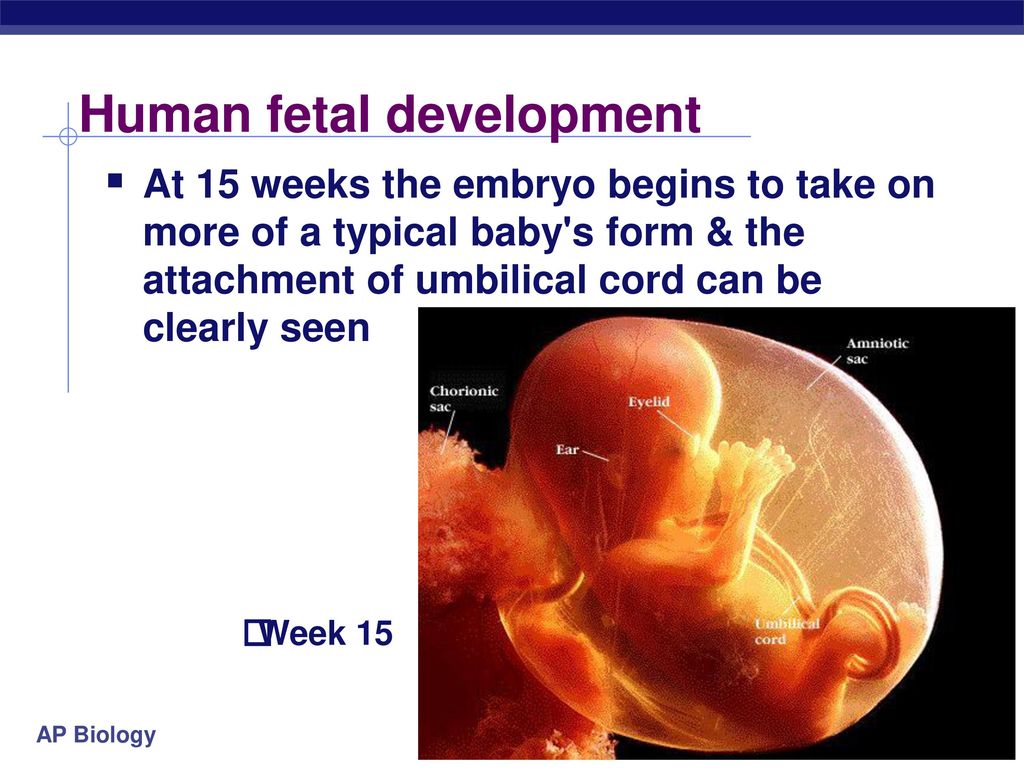 One grantee is studying the development of blood vessels in the umbilical cord for insight into the causes of single umbilical artery and other cord abnormalities. The goals of this study are to:
One grantee is studying the development of blood vessels in the umbilical cord for insight into the causes of single umbilical artery and other cord abnormalities. The goals of this study are to:
- Develop a better understanding of the causes of birth defects
- Develop treatments to help prevent oxygen deprivation before and during delivery, which may contribute to cerebral palsy and other forms of brain damage
- Cruikshank, D.W. Breech, Other Malpresentations, and Umbilical Cord Complications, in: Scott, J.R., et al. (eds.), Danforth's Obstetrics and Gynecology, 9th Edition. Philadelphia, Lippincott Williams and Wilkins, 2003, pages 381-395.
- Morgan, B.L.G. and Ross, M.G. Umbilical Cord Complications. emedicine.com, March 1, 2006.
- Gossett, D.R., et al. Antenatal Diagnosis of Single Umbilical Artery: Is Fetal Echocardiography Warranted? Obstetrics and Gynecology, volume 100, number 5, November 2002, pages 903-908.
- Oyelese, Y. and Smulian, J.C. Placenta Previa, Placenta Accreta, and Vasa Previa. Obstetrics and Gynecology, volume 107, number 4, April 2006, pages 927-941.
Last reviewed: February, 2008
The umbilical cord is a narrow tube-like structure that connects the developing baby to the placenta. The cord is sometimes called the baby's “supply line” because it carries the baby's blood back and forth, between the baby and the placenta. It delivers nutrients and oxygen to the baby and removes the baby's waste products.
The umbilical cord begins to form at 5weeks after conception. It becomes progressively longer until 28 weeks of pregnancy, reaching an average length of 22 to 24 inches (1). As the cord gets longer, it generally coils around itself. The cord contains three blood vessels: two arteries and one vein.
- The vein carries oxygen and nutrients from the placenta (which connects to the mother's blood supply) to the baby.
- The two arteries transport waste from the baby to the placenta (where waste is transferred to the mother's blood and disposed of by her kidneys).
A gelatin-like tissue called Wharton's jelly cushions and protects these blood vessels.
A number of abnormalities can affect the umbilical cord. The cord may be too long or too short. It may connect improperly to the placenta or become knotted or compressed. Cord abnormalities can lead to problems during pregnancy or during labor and delivery.
In some cases, cord abnormalities are discovered before delivery during an ultrasound. However, they usually are not discovered until after delivery when the cord is examined directly. The following are the most frequent cord abnormalities and their possible effects on mother and baby.
What is a single umbilical artery?
About 1 percent of singleton and about 5 percent of multiple pregnancies (twins, triplets or more) have an umbilical cord that contains only two blood vessels, instead of the normal three.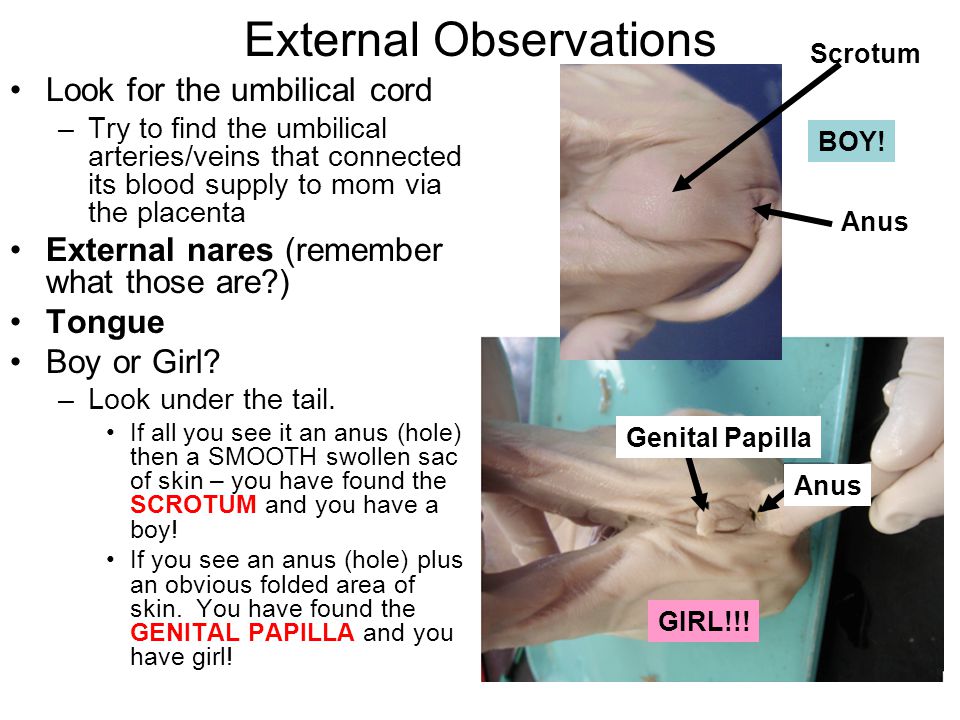 In these cases, one artery is missing (2). The cause of this abnormality, called single umbilical artery, is unknown.
In these cases, one artery is missing (2). The cause of this abnormality, called single umbilical artery, is unknown.
Studies suggest that babies with single umbilical artery have an increased risk for birth defects, including heart, central nervous system and urinary-tract defects and chromosomal abnormalities (2, 3). A woman whose baby is diagnosed with single umbilical artery during a routine ultrasound may be offered certain prenatal tests to diagnose or rule out birth defects. These tests may include a detailed ultrasound, amniocentesis (to check for chromosomal abnormalities) and in some cases, echocardiography (a special type of ultrasound to evaluate the fetal heart). The provider also may recommend that the baby have an ultrasound after birth.
What is umbilical cord prolapse?
Umbilical cord prolapse occurs when the cord slips into the vagina after the membranes (bag of waters) have ruptured, before the baby descends into the birth canal. This complication affects about 1 in 300 births (1).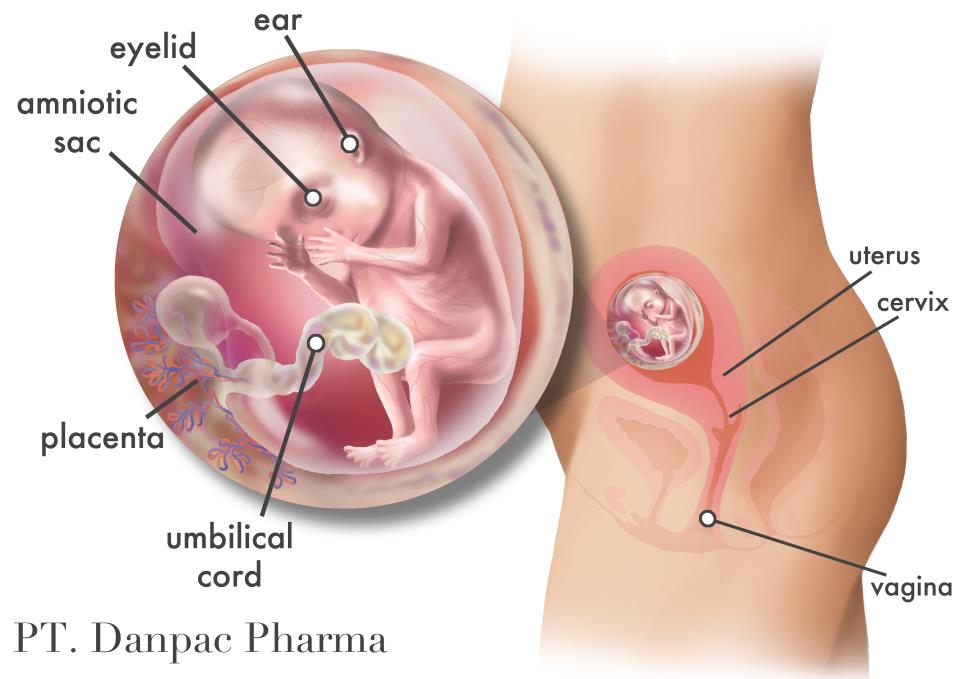 The baby can put pressure on the cord as he passes through the cervix and vagina during labor and delivery. Pressure on the cord reduces or cuts off blood flow from the placenta to the baby, decreasing the baby's oxygen supply. Umbilical cord prolapse can result in stillbirth unless the baby is delivered promptly, usually by cesarean section.
The baby can put pressure on the cord as he passes through the cervix and vagina during labor and delivery. Pressure on the cord reduces or cuts off blood flow from the placenta to the baby, decreasing the baby's oxygen supply. Umbilical cord prolapse can result in stillbirth unless the baby is delivered promptly, usually by cesarean section.
If the woman's membranes rupture and she feels something in her vagina, she should go to the hospital immediately or, in the United States, call 911. A health care provider may suspect umbilical cord prolapse if the bay develops heart rate abnormalities after the membranes have ruptured. The provider can confirm a cord prolapse by doing a pelvic examination. Cord prolapse is an emergency. Pressure on the cord must be relieved immediately by lifting the presenting fetal part away from the cord while preparing the woman for prompt cesarean delivery.
The risk of umbilical cord prolapse increases if:
- The baby is in a breech (foot-first) position.
- The woman is in preterm labor.
- The umbilical cord is too long.
- There is too much amniotic fluid.
- The provider ruptures the membranes to start or speed up labor.
- The woman is delivering twins vaginally. The second twin is more commonly affected.
What is vasa previa?
Vasa previa occurs when one or more blood vessels from the umbilical cord or placenta cross the cervix underneath the baby. The blood vessels, unprotected by the Wharton's jelly in the umbilical cord or the tissue in the placenta, sometimes tear when the cervix dilates or the membranes rupture. This can result in life-threatening bleeding in the baby. Even if the blood vessels do not tear, the baby may suffer from lack of oxygen due to pressure on the blood vessels. Vasa previa occurs in 1 in 2,500 births (4).
When vasa previa is diagnosed unexpectedly at delivery, more than half of affected babies are stillborn (4).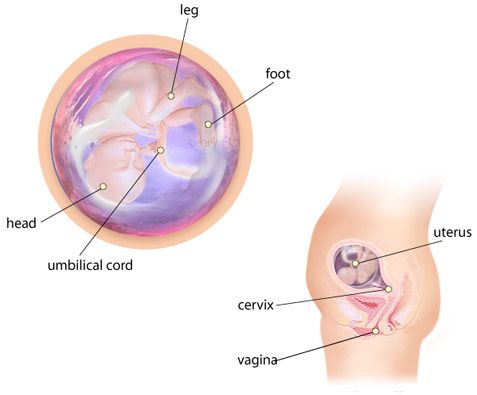 However, when vasa previa is diagnosed by ultrasound earlier in pregnancy, fetal deaths generally can be prevented by delivering the baby by cesarean section at about 35 weeks of gestation (4).
However, when vasa previa is diagnosed by ultrasound earlier in pregnancy, fetal deaths generally can be prevented by delivering the baby by cesarean section at about 35 weeks of gestation (4).
Pregnant women with vasa previa sometimes have painless vaginal bleeding in the second or third trimester. A pregnant woman who experiences vaginal bleeding should always report it to her health care provider so that the cause can be determined and any necessary steps taken to protect the baby.
A pregnant woman may be at increased risk for vasa previa if she:
- Has a velamentous insertion of the cord (the umbilical cord inserts abnormally into the fetal membranes, instead of the center of the placenta)
- Has placenta previa (a low-lying placenta that covers part or all of the cervix) or certain other placental abnormalities
- Is expecting more than one baby
What is nuchal cord?
About 25 percent of babies are born with a nuchal cord (the umbilical cord wrapped around the baby's neck) (1).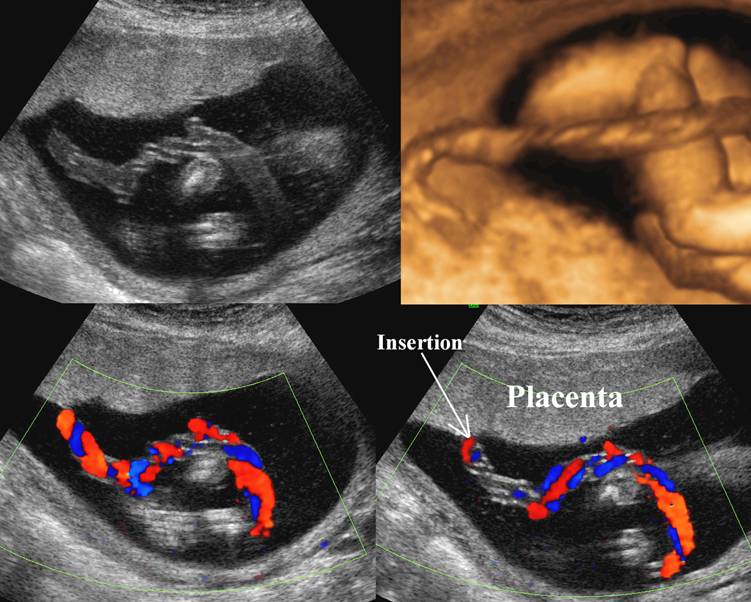 A nuchal cord, also called nuchal loops, rarely causes any problems. Babies with a nuchal cord are generally healthy.
A nuchal cord, also called nuchal loops, rarely causes any problems. Babies with a nuchal cord are generally healthy.
Sometimes fetal monitoring shows heart rate abnormalities during labor and delivery in babies with a nuchal cord. This may reflect pressure on the cord. However, the pressure is rarely serious enough to cause death or any lasting problems, although occasionally a cesarean delivery may be needed.
Less frequently, the umbilical cord becomes wrapped around other parts of the baby's body, such as a foot or hand. Generally, this doesn't harm the baby.
What are umbilical cord knots?
About 1 percent of babies are born with one or more knots in the umbilical cord (1). Some knots form during delivery when a baby with a nuchal cord is pulled through the loop. Others form during pregnancy when the baby moves around. Knots occur most often when the umbilical cord is too long and in identical-twin pregnancies. Identical twins share a single amniotic sac, and the babies' cords can become entangled.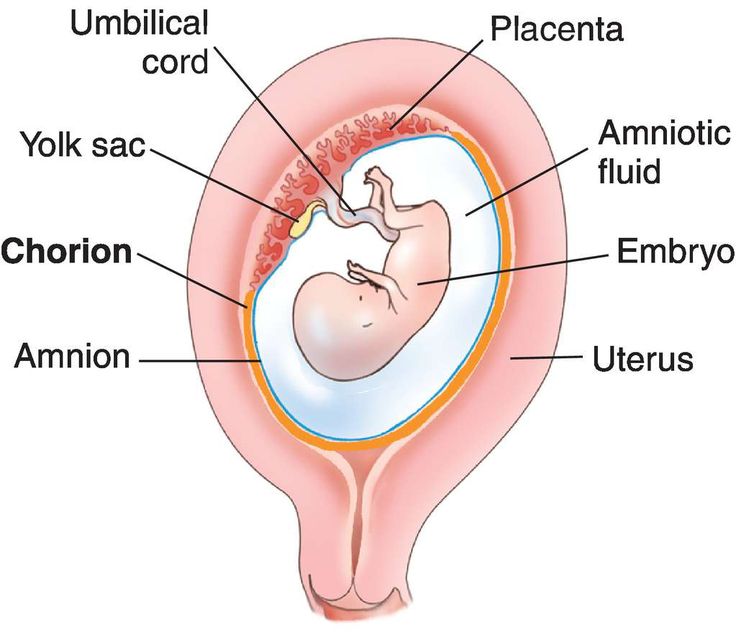
As long as the knot remains loose, it generally does not harm the baby. However, sometimes the knot or knots can be pulled tight, cutting off the baby's oxygen supply. Cord knots result in miscarriage or stillbirth in 5 percent of cases (1). During labor and delivery, a tightening knot can cause the baby to have heart rate abnormalities that are detected by fetal monitoring. In some cases, a cesarean delivery may be necessary.
What is an umbilical cord cyst?
Umbilical cord cysts are outpockets in the cord. They are found in about 3 percent of pregnancies (2).
There are true and false cysts:
- True cysts are lined with cells and generally contain remnants of early embryonic structures.
- False cysts are fluid-filled sacs that can be related to a swelling of the Wharton's jelly.
Studies suggest that both types of cysts are sometimes associated with birth defects, including chromosomal abnormalities and kidney and abdominal defects (2).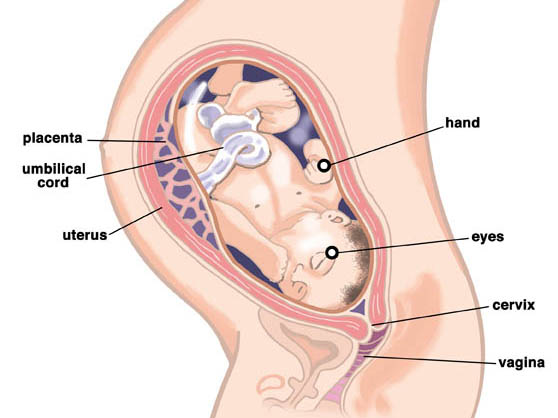 When a cord cyst is found during an ultrasound, the provider may recommend additional tests, such as amniocentesis and a detailed ultrasound, to diagnose or rule out birth defects.
When a cord cyst is found during an ultrasound, the provider may recommend additional tests, such as amniocentesis and a detailed ultrasound, to diagnose or rule out birth defects.
Does the March of Dimes support research on umbilical cord abnormalities?
The March of Dimes continues to support research aimed at preventing umbilical cord abnormalities and the complications they cause. One grantee is studying the development of blood vessels in the umbilical cord for insight into the causes of single umbilical artery and other cord abnormalities. The goals of this study are to:
- Develop a better understanding of the causes of birth defects
- Develop treatments to help prevent oxygen deprivation before and during delivery, which may contribute to cerebral palsy and other forms of brain damage
- Cruikshank, D.W. Breech, Other Malpresentations, and Umbilical Cord Complications, in: Scott, J.
R., et al. (eds.), Danforth's Obstetrics and Gynecology, 9th Edition. Philadelphia, Lippincott Williams and Wilkins, 2003, pages 381-395.
- Morgan, B.L.G. and Ross, M.G. Umbilical Cord Complications. emedicine.com, March 1, 2006.
- Gossett, D.R., et al. Antenatal Diagnosis of Single Umbilical Artery: Is Fetal Echocardiography Warranted? Obstetrics and Gynecology, volume 100, number 5, November 2002, pages 903-908.
- Oyelese, Y. and Smulian, J.C. Placenta Previa, Placenta Accreta, and Vasa Previa. Obstetrics and Gynecology, volume 107, number 4, April 2006, pages 927-941.
Last reviewed: February, 2008
Placenta and umbilical cord: what is important to know?
9 monthsHealth
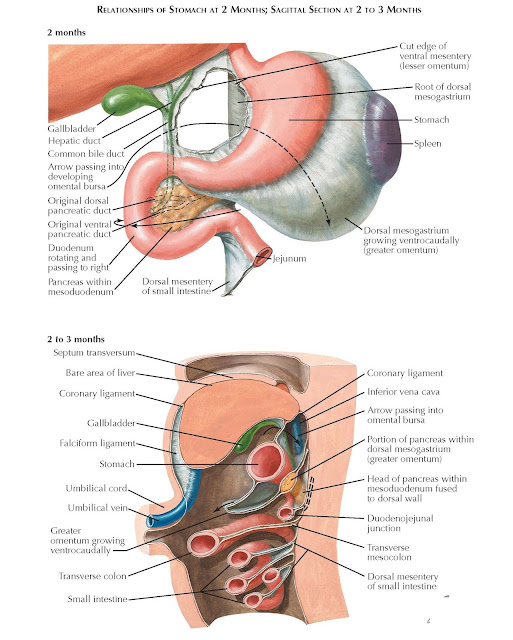
By the 12-14th week of pregnancy, the placenta and umbilical cord are finally formed - structures that exist only during pregnancy and perform the functions of exchange between mother and baby.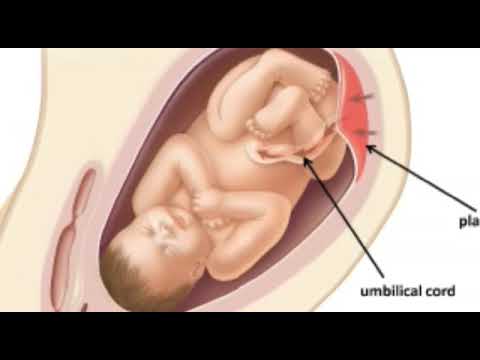 What are these temporary organs and how do they affect the development and condition of the baby?
What are these temporary organs and how do they affect the development and condition of the baby?
Placenta
Placenta (from Latin placenta – “pie, cake, pancake”) plays an invaluable role in the development of the fetus, ensuring its growth, development, nutrition, respiration and excretion of waste metabolic products, as well as protecting the fetus from all kinds of harmful impacts.
The placenta is a spongy oval or semicircular organ with a lobed structure. Each lobule of the placenta contains many small vessels. With a normal full-term pregnancy and a fetal weight of 3300-3400 g, the diameter of the placenta is from 15 to 25 cm, thickness 2-4 cm, weight 500 g.
Two systems of blood vessels converge in this organ: one of them (maternal) connects the placenta with the vessels of the uterus, the other (fetal) with the umbilical cord of the fetus. The baby's blood vessels come very close to the mother's, but the maternal and fetal blood streams never mix.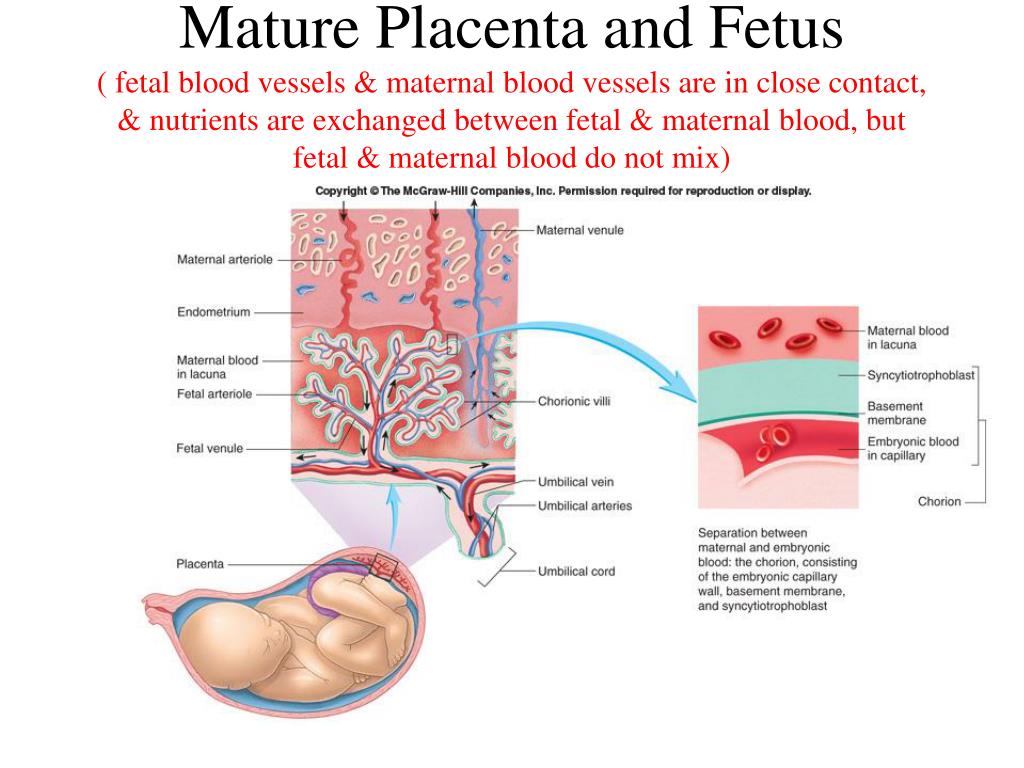 Between the two vascular systems there is a barrier membrane (one layer of cells) - the "customs and border service" of the placenta. Through it, the exchange of substances between mother and baby takes place: the maternal circulatory system brings oxygen and nutrients to the placenta and removes waste products and carbon dioxide from the placenta. The placental barrier allows the protective proteins (antibodies) of the mother to the child, ensuring its protection, and at the same time delays the cells of the woman's immune system that can cause a rejection reaction of the fetus, recognizing a foreign object in it. It is impenetrable to many harmful substances, viruses, bacteria. In addition, the placenta produces hormones that are important for successful pregnancy, and enzymes that destroy harmful substances.
Between the two vascular systems there is a barrier membrane (one layer of cells) - the "customs and border service" of the placenta. Through it, the exchange of substances between mother and baby takes place: the maternal circulatory system brings oxygen and nutrients to the placenta and removes waste products and carbon dioxide from the placenta. The placental barrier allows the protective proteins (antibodies) of the mother to the child, ensuring its protection, and at the same time delays the cells of the woman's immune system that can cause a rejection reaction of the fetus, recognizing a foreign object in it. It is impenetrable to many harmful substances, viruses, bacteria. In addition, the placenta produces hormones that are important for successful pregnancy, and enzymes that destroy harmful substances.
Umbilical cord
From the fetal part of the placenta there are vessels that unite into larger ones, which eventually form the umbilical cord. The umbilical cord is a long cord (normally from 40 to 60 cm), up to 2 cm thick, consisting of connective tissue, inside of which there are two arteries and one vein.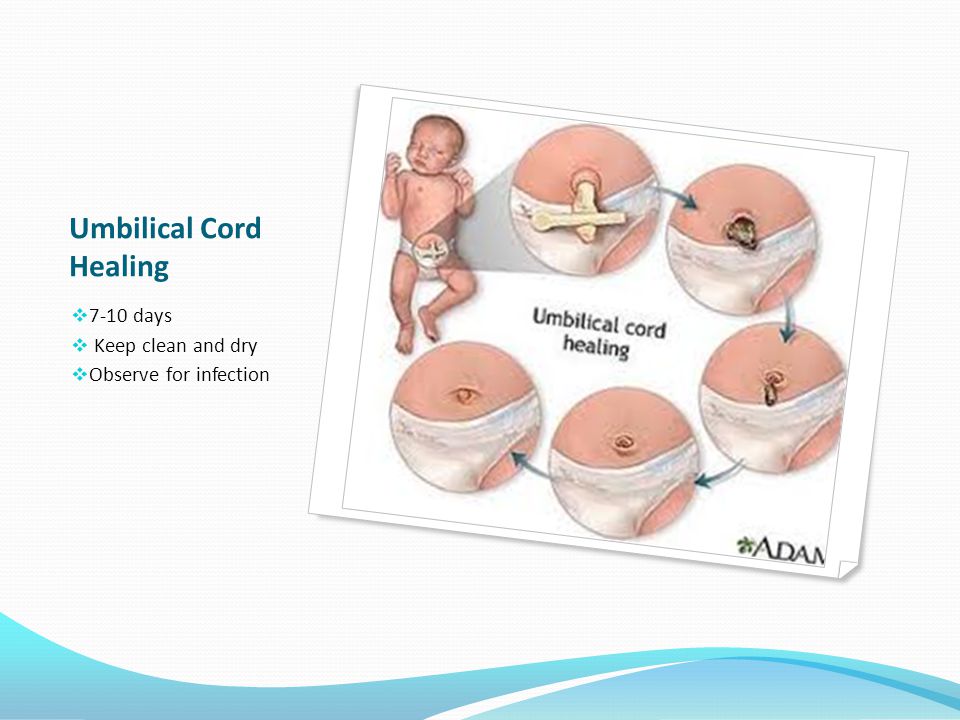 Despite the apparent discrepancy, the vessel called the venous carries arterial blood, while the two arterial vessels carry venous blood. These large vessels are surrounded by a special protective jelly-like substance - Wharton's jelly, which, due to its consistency, plays an important protective role - it protects the vessels from squeezing. The umbilical cord connects the placenta and the baby through the umbilical ring. The single umbilical vein that leaves the placenta enters the fetal abdomen through the umbilical ring and carries oxygenated blood, nutrients, and drugs that have passed the placental barrier. Through the arteries of the umbilical cord, the baby's blood flows back to the placenta, it carries waste products of decay and carbon dioxide. This is how fetal-placental blood flow occurs. After the birth of the baby, when the umbilical cord is cut, the connection between the blood circulation of the fetus and the blood flow of the mother stops, and only the navel reminds of their "blood" connection.
Despite the apparent discrepancy, the vessel called the venous carries arterial blood, while the two arterial vessels carry venous blood. These large vessels are surrounded by a special protective jelly-like substance - Wharton's jelly, which, due to its consistency, plays an important protective role - it protects the vessels from squeezing. The umbilical cord connects the placenta and the baby through the umbilical ring. The single umbilical vein that leaves the placenta enters the fetal abdomen through the umbilical ring and carries oxygenated blood, nutrients, and drugs that have passed the placental barrier. Through the arteries of the umbilical cord, the baby's blood flows back to the placenta, it carries waste products of decay and carbon dioxide. This is how fetal-placental blood flow occurs. After the birth of the baby, when the umbilical cord is cut, the connection between the blood circulation of the fetus and the blood flow of the mother stops, and only the navel reminds of their "blood" connection.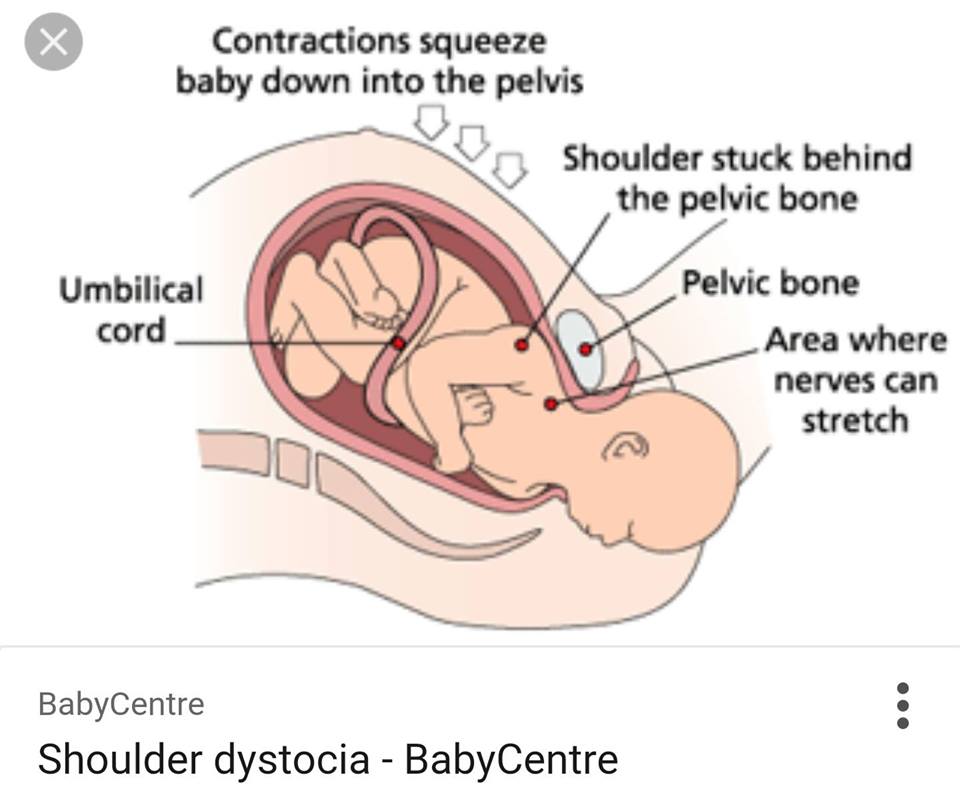
Disorders of the placenta
A change in the size (diameter and thickness) of the placenta, detected by ultrasound, does not always indicate that the pregnancy is unfavorable. Most often, such "deviations" are only an individual feature and do not affect the development of the fetus. Only significant deviations deserve attention.
Small placenta, or placental hypoplasia. Such a diagnosis is valid only with a significant decrease in the size of the placenta. The cause of this condition is most often genetic abnormalities, while the fetus often lags behind in development and has other malformations.
A thin placenta is considered to be a placenta with insufficient weight, but at the same time of normal size. Sometimes a thin placenta accompanies placental insufficiency and is therefore a risk factor for intrauterine growth retardation and serious problems in the neonatal period.
An increase in the thickness and size of the placenta can also be the result of an abnormal pregnancy.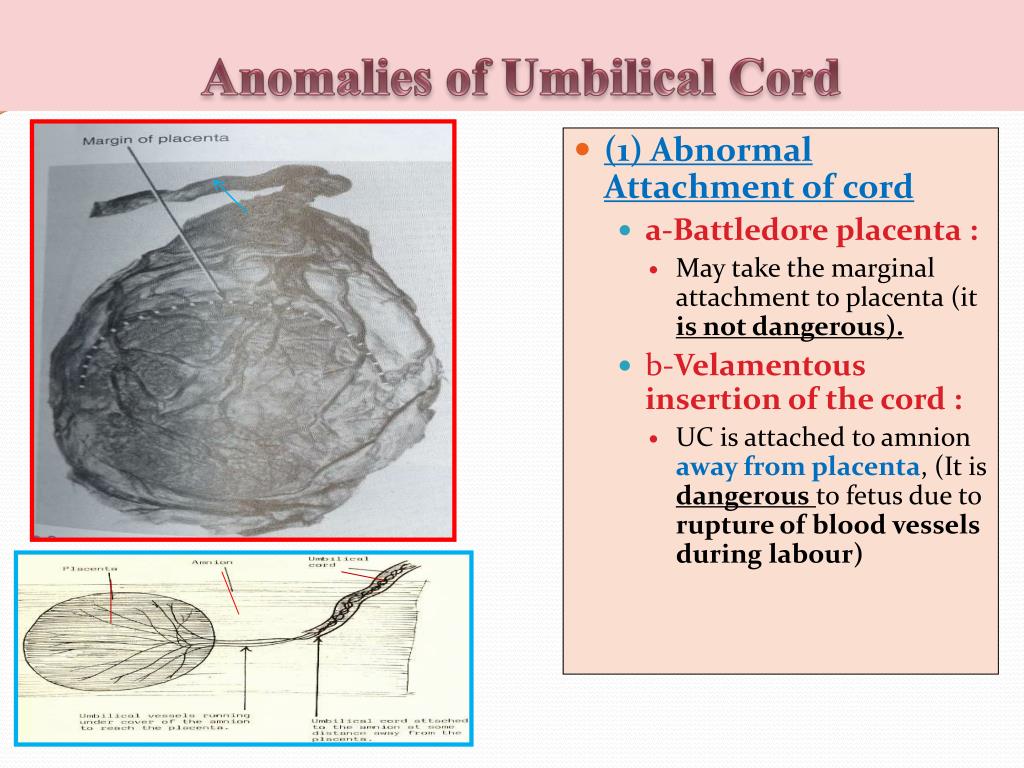 The most common cause of an increase in the size of the placenta is swelling of its villi due to inflammation ( placentitis or chorioamnionitis ). Chorioamnionitis can be caused by the penetration of microorganisms from the external genital organs into the placenta (with STIs: chlamydia, mycoplasmosis, herpes, gonorrhea) or with blood flow (with influenza, SARS, inflammation of the kidneys, toxoplasmosis, rubella). Placentitis is accompanied by dysfunction of the placenta (placental insufficiency) and intrauterine infection of the fetus.
The most common cause of an increase in the size of the placenta is swelling of its villi due to inflammation ( placentitis or chorioamnionitis ). Chorioamnionitis can be caused by the penetration of microorganisms from the external genital organs into the placenta (with STIs: chlamydia, mycoplasmosis, herpes, gonorrhea) or with blood flow (with influenza, SARS, inflammation of the kidneys, toxoplasmosis, rubella). Placentitis is accompanied by dysfunction of the placenta (placental insufficiency) and intrauterine infection of the fetus.
Umbilical cord - norm and pathology
The umbilical cord is a spiral tube that connects the fetus to the placenta. Outside, the umbilical cord is covered with fetal membranes. It contains two arteries and one vein.
Arterial blood flows through the vein of the umbilical cord, carrying oxygen to the organs of the fetus. The umbilical arteries carry venous blood from the fetus to the placenta, this blood contains the metabolic products of the fetus.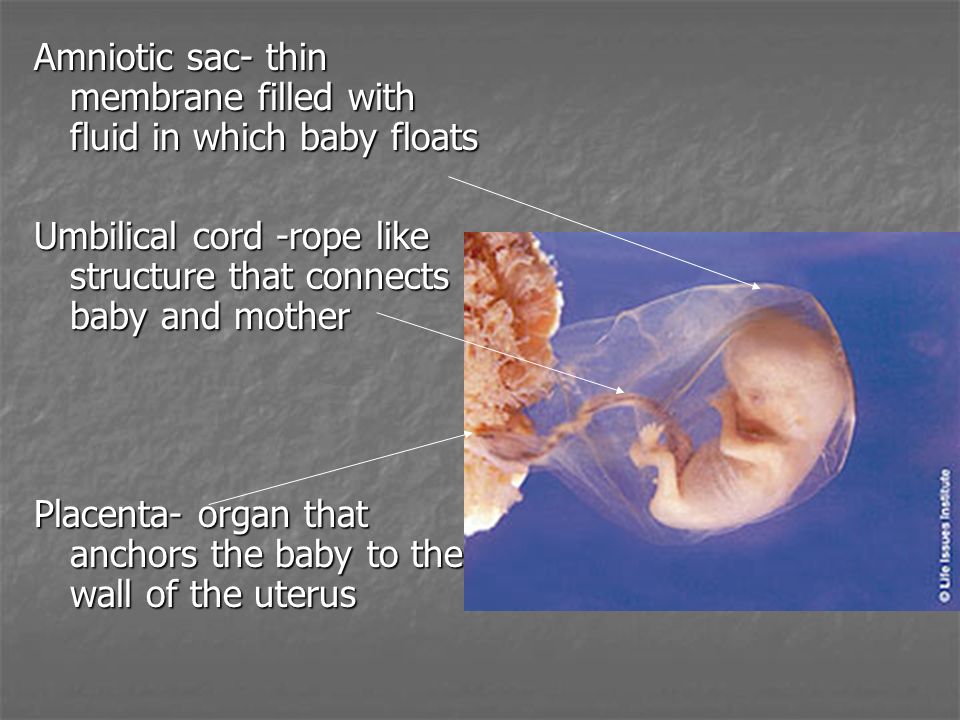 The vessels of the umbilical cord are in a special gelatinous substance that fixes them and protects them from injury, and also exchanges substances between the fetal blood and amniotic fluid. The umbilical cord begins to form from 2-3 weeks of pregnancy and grows with the baby. By the time of birth, its length is 45–60 cm (the length of the umbilical cord, on average, corresponds to the height of the child), and its diameter is 1.5–2 cm.
The vessels of the umbilical cord are in a special gelatinous substance that fixes them and protects them from injury, and also exchanges substances between the fetal blood and amniotic fluid. The umbilical cord begins to form from 2-3 weeks of pregnancy and grows with the baby. By the time of birth, its length is 45–60 cm (the length of the umbilical cord, on average, corresponds to the height of the child), and its diameter is 1.5–2 cm.
The umbilical cord can attach to the placenta in different ways. In some cases, attachment occurs in the center of the placenta (central attachment), in others - on the side (lateral attachment). Sometimes the umbilical cord is attached to the membranes, not reaching the placenta itself (shell attachment). In these cases, the vessels of the umbilical cord approach the placenta between the membranes. Such attachment of the placenta is a risk factor for the occurrence of fetal placental insufficiency.
The umbilical cord may also have features such as true and false nodes.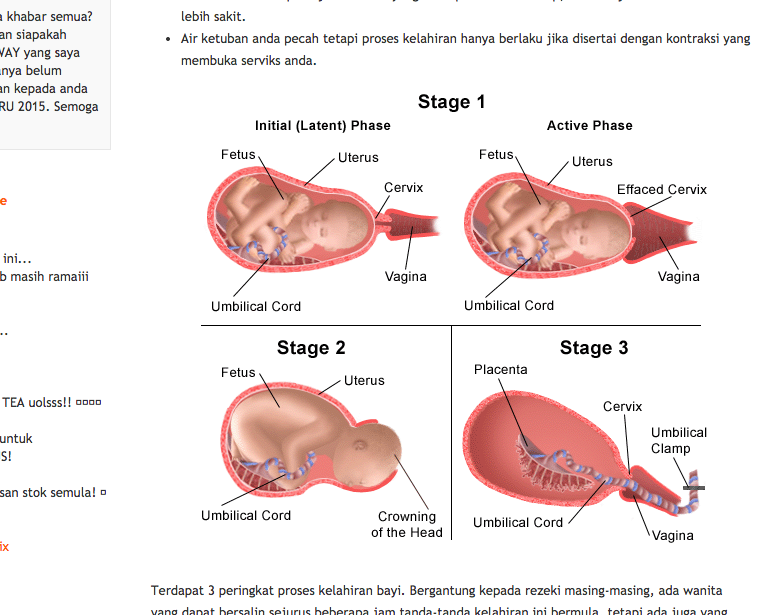 False nodes are local thickening of the umbilical cord due to varicose veins of the umbilical cord or accumulation of Wharton's jelly. They do not affect the development of the fetus and the process of childbirth. True umbilical cord knots form early in pregnancy, when the fetus is still small, allowing it to slip through the umbilical cord loop. True umbilical cord knots can affect the outcome of labor. When the umbilical cord is pulled, the knot is tightened, the flow and outflow of blood through the vessels stop. In this case, acute fetal hypoxia occurs.
False nodes are local thickening of the umbilical cord due to varicose veins of the umbilical cord or accumulation of Wharton's jelly. They do not affect the development of the fetus and the process of childbirth. True umbilical cord knots form early in pregnancy, when the fetus is still small, allowing it to slip through the umbilical cord loop. True umbilical cord knots can affect the outcome of labor. When the umbilical cord is pulled, the knot is tightened, the flow and outflow of blood through the vessels stop. In this case, acute fetal hypoxia occurs.
The pathology of the development of the umbilical cord is also a condition in which only one umbilical artery is formed instead of two; in some fetuses with one umbilical artery, various malformations are observed. The reason for this formation of the umbilical cord can be factors that cause fetal malformations - the so-called teratogenic factors (chemicals, certain drugs, ionizing radiation, genetic diseases of the parents).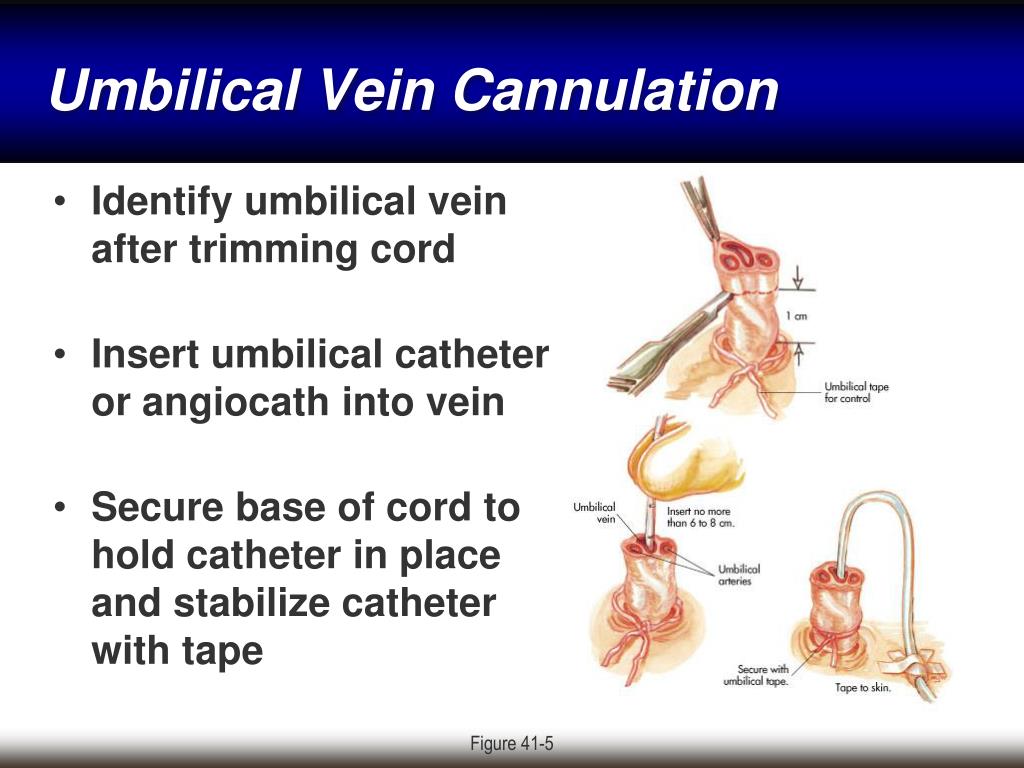
Some problems may arise in connection with the shortening of the umbilical cord. Shortening of the umbilical cord can be divided into absolute and relative. With an absolute shortening of the umbilical cord, the length of the umbilical cord is less than 45 cm. During pregnancy, this condition does not affect the development of the baby. During childbirth, both with relative and absolute shortness of the umbilical cord, due to its tension, the placenta can prematurely exfoliate, which the umbilical cord pulls along, which creates a direct threat to the life of the fetus.
False shortening of the umbilical cord occurs when the umbilical cord is wrapped around the neck and torso of the fetus. The cause of umbilical cord entanglement may be its excessively long length (more than 70 cm), as well as increased fetal motor activity, which may be associated with chronic intrauterine fetal hypoxia. The causes of chronic lack of oxygen are different - these are maternal diseases, fetal diseases, and placental pathology.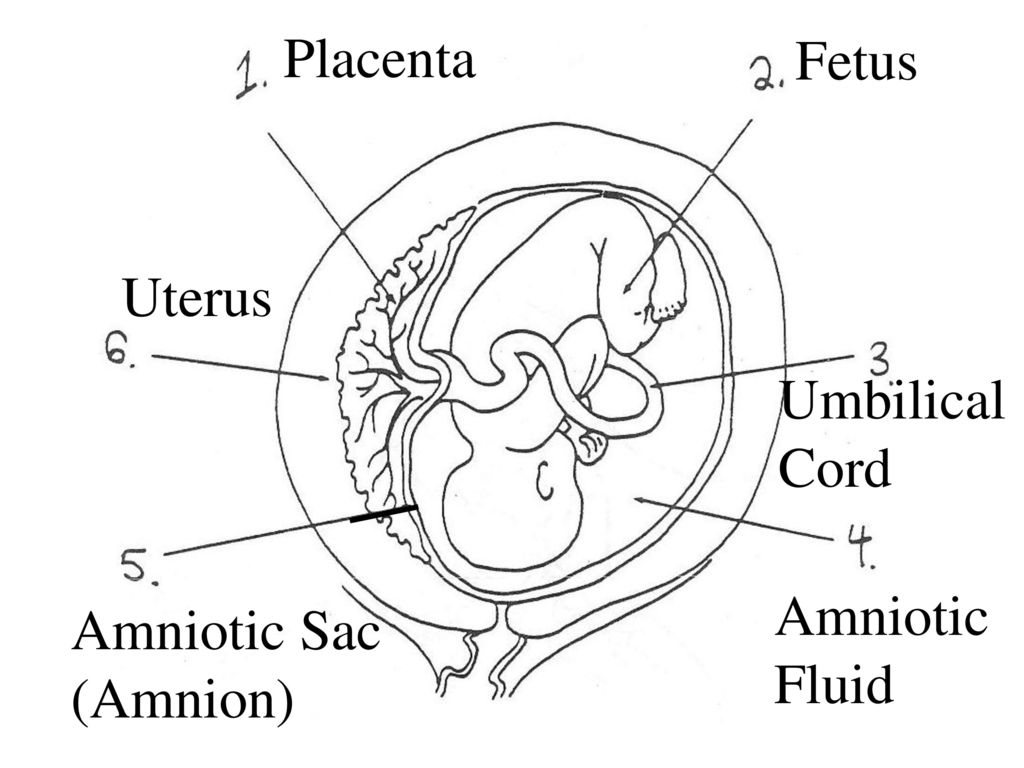 The entanglement of the umbilical cord can be single, double or even triple. During pregnancy, this condition usually does not affect the fetus, but problems can occur during childbirth. Tension or clamping of the vessels of the umbilical cord leads to disruption of blood flow.
The entanglement of the umbilical cord can be single, double or even triple. During pregnancy, this condition usually does not affect the fetus, but problems can occur during childbirth. Tension or clamping of the vessels of the umbilical cord leads to disruption of blood flow.
Conditions such as shortening of the umbilical cord (absolute and relative) and true knots of the umbilical cord during childbirth can lead to acute intrauterine fetal hypoxia. It is manifested by a change in the number of heartbeats. (The normal fetal heart rate is 120-160 beats per minute.) When acute intrauterine fetal hypoxia occurs, primordial feces (meconium) appears in the amniotic fluid, the water turns green. The appearance of all these symptoms requires emergency treatment. First of all, it is necessary to eliminate the cause of hypoxia, which is achieved by early delivery. The method of delivery depends on the period of labor and how far the presenting part of the fetus (head or pelvic end) has advanced along the birth canal.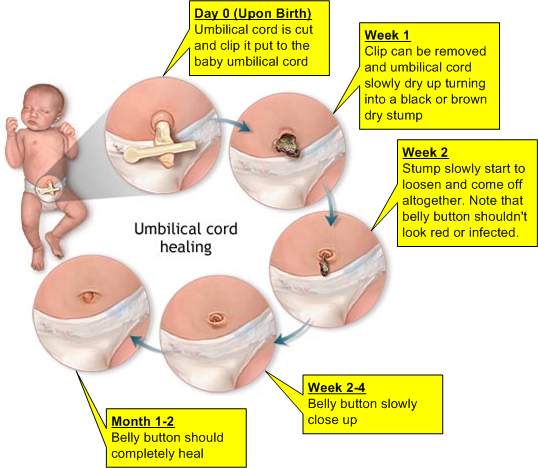 If acute hypoxia occurs during pregnancy or in the first stage of childbirth, the woman is given a caesarean section. In the second stage of labor, when the head or pelvic end is already close to the exit from the small pelvis, various obstetric aids are used to speed up the completion of the second stage of labor.
If acute hypoxia occurs during pregnancy or in the first stage of childbirth, the woman is given a caesarean section. In the second stage of labor, when the head or pelvic end is already close to the exit from the small pelvis, various obstetric aids are used to speed up the completion of the second stage of labor.
Fortunately, this condition does not occur often. Therefore, entanglement of the umbilical cord and knots of the umbilical cord are not an absolute indication for a planned caesarean section (it is impossible to diagnose the absolute shortness of the umbilical cord before delivery). These states are relative indications for surgery, i.e. caesarean section is done only in cases where, in addition to them, there are also other relative indications for surgery (the age of the woman is over 30 years old, mild forms of preeclampsia, etc.).
The only method that allows us to assume the pathology of the umbilical cord is an ultrasound scan. With the help of ultrasound, abnormalities of the umbilical cord can be detected, such as abnormal development of blood vessels (the only artery of the umbilical cord), true and false knots of the umbilical cord, entanglement of the umbilical cord.