Food sensitivity during pregnancy
Can I Develop New Food Allergies Because Of Pregnancy?
By Kirstie Marie Landry
Share Tweet Share Share Share Email
As the body goes through many changes, some women may develop new food allergies during pregnancy.
via Public Domain FilesAllergies are something that can have an impact on anyone. Furthermore, there are a lot of things that parents (and those who plan to be parents soon) need to know about them. Allergies are one of the things that can make having a new baby a scary thing since it's hard to tell if they are allergic to anything before they have a reaction to it. But there are some myths about allergies. According to readysetfood.com, one myth is that pregnant women can keep their babies from being allergic to certain foods if they avoid those foods themselves. Ladies should also know whether or not they can get new food allergies while they are pregnant, since that can be scary. Here's what they should know about pregnancy and food allergies.
It Is Likely
via PeakpxPregnancy is something that comes along with a lot of changes. It changes a woman's body, as well as her overall lifestyle and other things. One of the things that it can also change is the way she reacts to certain things, which means that she could suddenly start having allergic reactions to things that never seemed to bother her much before. According to mybabymanual.co.uk, pregnancy can definitely change the foods that women can tolerate. This might be alarming to moms-to-be, and they'll likely wonder if their baby will be harmed by them having an allergic reaction to certain things. But they should know that their reactions to foods that they cannot tolerate usually will not cause much danger for the little ones that they're carrying.
There Is A Myth About This
There are many interesting myths about certain things, one of which is pregnancy. There are a lot of old wives' tales that focus on pregnant women and their unborn little boys and girls. Furthermore, some of those myths have a lot to do with what a woman eats when she is pregnant and how it may or may not affect her growing baby.
Furthermore, some of those myths have a lot to do with what a woman eats when she is pregnant and how it may or may not affect her growing baby.
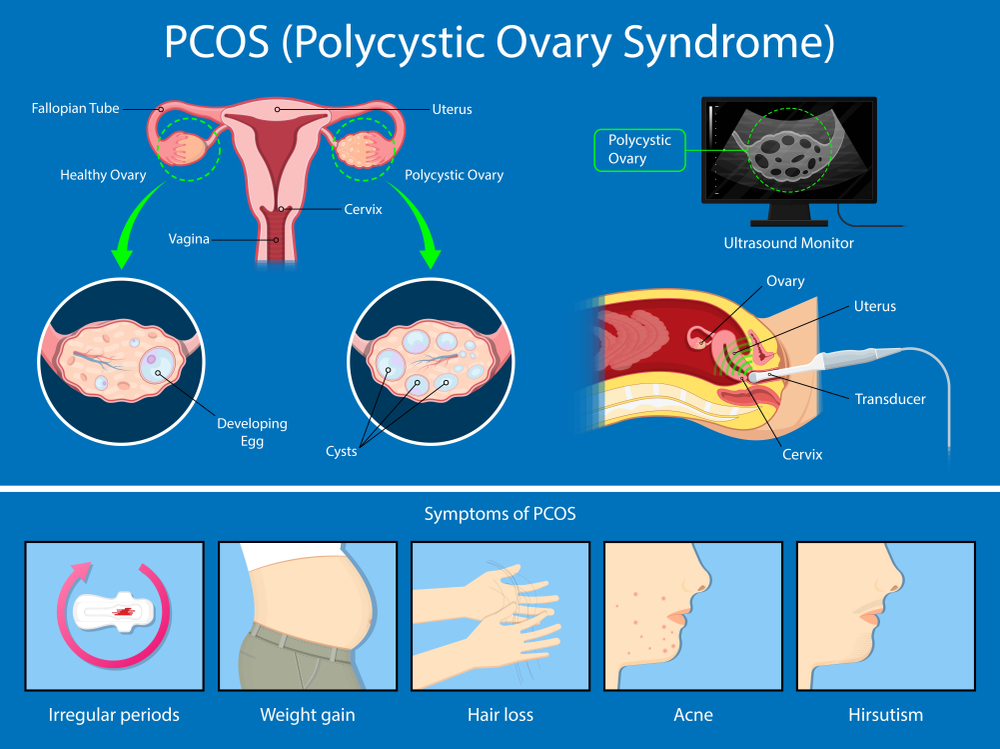
RELATED: Can I Get Pregnant Naturally With PCOS?
For example, there is one myth that claims that women who have food allergies before they are pregnant will be able to handle the food that they are allergic to without any issues when they are pregnant. But the problem is that this is not true. If a woman has already been diagnosed with a food allergy prior to becoming pregnant, she should not consume the food that she is allergic to while carrying the baby. Her allergy is still likely to exist, and this can be dangerous.
Sometimes It Remains The Same
Pregnancy tends to change a lot about women, and it can even impact the physical reactions their bodies have to certain things. But that is not always the case. According to foodallergycanada.ca, there are times when women might not see any changes to their allergies at all when they are carrying a baby. Some women have had their symptoms to foods that they are allergic to remain the same while pregnant. This is something ladies should know if they have food allergies.
Some women have had their symptoms to foods that they are allergic to remain the same while pregnant. This is something ladies should know if they have food allergies.
It's Not Always Hereditary
Genetics are very important, as they can play a key role in whether or not a person ends up having a serious illness at some point in their life. This is something that causes some women to worry a bit since it is possible for them or the baby's father to pass certain unfortunate things down to their children. But the good thing about food allergies is that they are not always passed down from a parent to their child. This means that women who have some serious allergies to certain foods might not pass their allergies down to their unborn children.
Some Things Can Cause Kids To Have Allergies
via Health.milPregnant women tend to worry a lot about their own food allergies and whether or not their baby will have them when he or she is born. But, they should also know that there are some things that can put a child at risk for developing allergies in general. According to healthline.com, it is possible that children who were not born vaginally could end up having a higher chance of developing some kind of allergy than those who were not. However, it does seem as though breastfeeding can be helpful in that situation, so that is something ladies might want to keep in mind.
According to healthline.com, it is possible that children who were not born vaginally could end up having a higher chance of developing some kind of allergy than those who were not. However, it does seem as though breastfeeding can be helpful in that situation, so that is something ladies might want to keep in mind.
Talk To Your Doctor
Naturally, if a woman already has known food allergies by the time she becomes pregnant, she will wonder whether or not her allergies are going to affect the health of her growing baby. But even if women have already been diagnosed with some kind of allergy (not just one that is related to food), it is possible for them to have a safe pregnancy. According to whattoexpect.com, they just need to communicate with their doctors. In addition, they should also consult their doctors before taking any medications. This is one of the many things women should know about allergies.
READ NEXT: Can I Get Pregnant With Asherman's Syndrome?
Sources: Ready. Set. Food!, My Baby Manuel, Food Allergy Canada, Healthline, What To Expect
Set. Food!, My Baby Manuel, Food Allergy Canada, Healthline, What To Expect
Mom’s Diet in Pregnancy Can Affect Child’s Allergies
By The Healthline Editorial Team on November 8, 2019
Share on PinterestResearchers recommend pregnant women eat a healthy, well-rounded diet. Getty Images- Researchers are learning more about how a pregnant woman’s diet can affect the chance of her child developing allergies.
- Additionally, researchers have found that cesarean delivery may increase the risk of allergies in infants, compared to vaginal delivery.
- Researchers say women should try to eat a well-rounded diet and stay healthy but not be overly worried about the risks.
Experts have long known that when a woman is pregnant, what she eats and what she’s exposed to can have an effect on the fetus.
Now, they’re learning how a pregnant woman’s diet, and even how she delivers her child, could affect the infant’s risk of developing allergies.
According to two new studies, how a woman eats while she’s pregnant, how she delivers, and how she feeds her baby can all have an impact on the child’s risk for developing allergies.
The research was presented at the American College of Allergy, Asthma, and Immunology (ACAAI) annual meeting.
The first study looked at data from more than 158,000 children. The researchers examined children with food allergy, eczema, asthma, and hay fever. Then, they looked at how the children were delivered and whether they were exclusively breastfed.
“We found vaginal delivery was associated with a reduced rate of development of allergic conditions,” Dr. David Hill, an allergist and lead author, said in a statement.
“While a mother can’t always control the way her baby is delivered, exclusive or supplemental breastfeeding may be helpful in reducing the rate of onset and overall burden of allergies in children,” Hill added.
The second study aimed to see if a link existed between how mothers ate during pregnancy, their history of allergic disease, and the child’s development of eczema and food allergy.
Carina Venter, PhD, RD, study presenter, tracked what 1,315 pregnant women ate during pregnancy, while noting their history of allergies.
Kids who were more likely to develop eczema and/or food allergies were born to mothers with poor diet diversity who had a history of allergic disease. In fact, 33 percent of children developed allergies by the age of 2 if their mothers had poor diet diversity and a history of allergic disease.
And 21 percent of children whose mothers ate a more varied diet while pregnant, regardless of whether or not they had a history of allergic disease, went on to develop eczema and/or food allergy by the time they were 2.
Pregnant women — especially those with allergies — need to be aware that their diet can affect their child’s chances of having eczema and/or food allergies, the authors reported.
Venter told Healthline that her study “really gives us an indication that everything may start in the womb.” She said it suggests that there may be dietary information that doctors could suggest to mothers in order to prevent food allergies or eczema in their children. More research, including a randomized controlled trial, would be needed to drive specific recommendations.
More research, including a randomized controlled trial, would be needed to drive specific recommendations.
“More information is definitely needed before a cause and effect relationship [between diet, delivery and/or infant feeding as it relates to allergy development] can be confirmed,” noted Dr. Jennifer Savitski, chair of the OB-GYN department at Cleveland Clinic Akron General.
Though the studies may be making headlines, the findings aren’t anything new, according to Stacey Galowitz, DO, an allergy specialist from New Jersey.
We still don’t know for certain how specific foods in the maternal diet, or lack thereof, have an impact on allergy development. We also don’t know what parts of a mother’s microbiome affect an infant’s immune development.
“A number of convincing studies have supported the concept of a critical window of exposure to allergens early in infancy — and perhaps even in prenatal life — in the prevention of allergic diseases,” she told Healthline.
Alterations in maternal diets during pregnancy have been suggested as a way to limit the development of allergies, asthma, and atopic dermatitis.
Currently, there aren’t specific recommendations to definitively prevent allergies in their unborn child. But most experts support maintaining a well-balanced diet throughout pregnancy and lactation, as specific restrictions of key allergens haven’t been shown to prevent the future development of allergic disease in children, Galowitz noted.
“At the moment, I advise women that there is no need to avoid food allergens during pregnancy, which is in line with current international guidelines. It is important to note that these guidelines do not actively recommend intake of food allergens,” Venter added. “All pregnant women should ideally consume a healthy, varied diet if possible.”
As for why C-sections may make some children more susceptible to allergic disorders, it goes back to the interruption in the transmission of the maternal microbiome and subsequently compromised intestinal microbiome that happens when an infant doesn’t pass through the birth canal, Galowitz said.
“This all goes back to our more global idea of the ‘hygiene hypothesis,’ or that the lack of early introduction of germs represses proper immune system development in infants/children,” she said.
C-sections aren’t typically recommended unless a doctor suggests the procedure, so it’s advised to try for a vaginal delivery if there are no indications requiring C-section, Galowitz said.
Women should keep in mind that the study doesn’t say that having a C-section or giving an infant formula will cause allergy issues.
“There are many reasons — both voluntary and nonvoluntary — that women deliver via C-section or choose to use formula, and they shouldn’t feel shamed for whatever they choose,” Galowitz added.
If a child shows early signs of an allergic disorder, such as having eczema, the parents should seek help from an allergist. Doing so early in life may help minimize the severity of allergies, Galowitz said.
Allergies in Pregnancy: Allergies in Pregnancy
Increased prevalence and use of cosmetics, synthetics, disinfectants, and changing food and human diets are contributing to the increase in allergies.
Allergic disease occurs when the body's immune system reacts to allergens when it comes into contact with them. Allergic diseases also include acute allergies.
Among people susceptible to acute allergosis, from 5 to 20% of cases are pregnant. Pregnant women are most susceptible to this disease between the ages of 18 and 24.
Allergies in pregnancy - effects on the baby
When allergies develop in pregnant women, they do not affect the fetus. This is due to the fact that immunocomplexes that react to an allergen that irritates the body cannot reach the fetus due to the placenta. Despite this, the fetus that is in the womb can be negatively affected by the disease due to three main reasons:
- When the mother's health condition changes.
- Medicines needed to treat when allergies occur during pregnancy may affect the reduction in uteroplacental blood flow. The process of supplying blood to the fetus is deteriorating.

- Drugs other than the above effects may have a bad effect on the fetus as a whole.
Treatment of allergies during pregnancy
Treatment should be started immediately, because only in this case the allergy will not have time to affect the fetus. Also, a very important task, which must be taken into account before starting treatment, is the maximum avoidance of harm that can be caused to an unborn child by drugs.
When prescribing a course of treatment, a doctor should take into account the fact that the number of pregnant women who have diseases of the internal organs, according to statistics, reaches 45%. In addition, the proportion of women taking medication during pregnancy ranges from 60% to 80%. The average number of medications a woman takes during the entire pregnancy process is 4 different types. And this is without taking into account various vitamin complexes, dietary supplements and minerals. That is why a pregnant woman should never engage in self-treatment after discovering the first signs of an allergy in herself. You must immediately go to an appointment with a doctor who will provide qualified assistance and prescribe the correct course of treatment, as harmless as possible to the fetus.
You must immediately go to an appointment with a doctor who will provide qualified assistance and prescribe the correct course of treatment, as harmless as possible to the fetus.
The search for an allergy medicine in pharmacies, if necessary, after a doctor's prescription, can be done on our portal. There is all the information about each of them, and it is also possible to compare their cost.
When contacting an allergist for a consultation, a woman, in order to correctly diagnose and identify the allergen, will be subject to a special examination. A similar test involves preparing a solution that is made from the irritants that are believed to have caused the allergy. After that, a similar solution is injected into the skin of a pregnant woman in a small amount. If she is allergic to one of the irritants present in the solution, the area around the injection site will become swollen.
Where to get skin tests for allergies, as well as a laboratory blood test, you can find on our website. Here you can choose a profitable and convenient location option for yourself.
Here you can choose a profitable and convenient location option for yourself.
There are three stages in the development of allergies during pregnancy. The first entry of the allergen into the body. Immunity cells recognize the "enemy" and mechanisms for the formation of antibodies begin to work in the body. Second allergen exposure. The body is again exposed to allergens. There are processes that stimulate the production of histamine, which causes allergic symptoms. Third stage. Vessels expand, tissue permeability increases. This results in swelling and inflammation. A strong vasodilation is also possible, causing a sharp drop in blood pressure, i.e. anaphylactic shock occurs.
The result is an acute allergic reaction.
Acute allergosis:
- allergic rhinitis. Complication of breathing through the nose, its congestion, the mucous membranes of the nose swell, and an abundant secretion of mucous secretion appears, sneezing and burning in the throat occur;
- urticaria.
 Damage to a certain area of \u200b\u200bthe skin - the appearance of sharply defined blisters, accompanied by itching;
Damage to a certain area of \u200b\u200bthe skin - the appearance of sharply defined blisters, accompanied by itching; - redness, swelling, conjunctiva, itching of the eyes, lacrimation, narrowing of the palpebral fissure.
Severe allergy:
- generalized urticaria. Involvement of all areas of the skin with symptoms of simple urticaria;
- angioedema. Edema of the skin, mucous membranes, and subcutaneous tissue. Basically, in the area of lips, cheeks, forehead, eyelids, hands, feet. Swelling of the larynx. Swelling of the gastrointestinal mucosa, accompanied by pain;
- anaphylactic shock. Arterial hypotension. Loss of consciousness, respiratory failure, swelling of the respiratory tract, urticaria, itching.
Quincke's edema, urticaria and rhinitis are most common in pregnant women.
What causes allergic reactions? Conventionally, three stages can be distinguished in their development. When a mother has allergic reactions, the fetus does not show any signs of allergy, because specific immunocomplexes that react to an allergen-irritant are not able to penetrate the placenta. However, in spite of this, a child in the womb may be affected by allergies for the following reasons:
However, in spite of this, a child in the womb may be affected by allergies for the following reasons:
- the mother's condition changes due to the onset of the disease;
- the influence of certain drugs that can cause a decrease in uteroplacental blood flow, which ensures the life of the fetus;
- the negative effect of drugs directly on the fetus.
So how do you treat allergies in pregnant women? The most basic goal of treatment is the painless elimination of symptoms of pregnancy allergy without the risk of negative effects on the fetus. The reaction of the human body to taking various drugs largely depends on the general vitality, the type of therapy it undergoes, and the nature of the symptoms of the disease.
Pregnancy is a special, complex state of the body, because up to 45% of pregnant women can have diseases of the internal organs, and from 60 to 80% of expectant mothers who regularly take certain drugs in general. During the course of pregnancy, on average, according to surveys and observations, a woman can take up to four different medications, and this does not include vitamins, various nutritional supplements and minerals.
Habitual allergy pills, during pregnancy, for the most part, are contraindicated:
- Diphenhydramine taken late in pregnancy may cause uterine excitability or contractions when taken in doses greater than 50 mg;
- Terfenadine frequently causes weight loss in neonates;
- Astemizole has a strong toxic effect on the fetus;
- Suprastin (chloropyramine), cetirizine (Alleprtec), claritin (loratadine) and fexadine (fexofenadine) are acceptable during pregnancy, but only if the effect of treatment outweighs the potential risk to the child;
- Tavegil (clemastine) should never be used throughout pregnancy, except in cases of direct threat to the life of the pregnant woman;
- Pipolfen (piperacillin) is strongly discouraged during pregnancy and lactation.
If an allergy occurs in pregnant women for the first time, it is necessary to urgently contact an allergist. Separately, it is worth noting that during pregnancy, the primary task is to eliminate contact with the allergen, and not the symptoms of allergies.
To find out what may be an allergen in a particular case, a special examination is carried out.
What should be done in case of manifestation of OAS, and what drugs can be used:
- if the allergen is known, it must be eliminated immediately;
- consult a doctor;
- In the absence of the possibility of consulting a doctor, the following list of recommended drugs should be used.
1st generation of H2 blockers:
- Pipolfen (piperacillin) - not recommended during pregnancy or breastfeeding;
- Suprastin (chlorpyramidine) - can be prescribed only for acute allergic reactions during pregnancy;
- Allertec (cyterizine) - the drug can be taken in late pregnancy;
- Tavegil (clemastine) - during pregnancy is prescribed only in cases where an allergic reaction threatens the life of a pregnant woman, and for some reason there is no possibility of using other drugs. This is due to the negative effect of the drug on the fetus.

2nd generation H2-histamine blockers:
Claritin (loratadine) - during pregnancy, the use is allowed only if the expected effect of the treatment outweighs the potential risk to the child. The drug can be used only in cases where the disease state of the mother threatens the fetus more than taking this drug. This risk in each case must be assessed by a doctor.
3rd generation H2-histamine blockers:
Fexadine (fexofenadine) - during pregnancy, you can use it only in cases where the expected positive effect of therapy outweighs the potential risk to the child.
Prevention of allergic disease during pregnancy
Prevention of allergies is important, as it will help to avoid allergic disease and the consequences of exposure to drugs for its treatment on the fetus. In order to prevent, it is necessary, first of all, to remove from the woman's food products that are characterized as highly allergic. This is primarily due to the fact that irritants most often enter through the gastrointestinal tract, and then penetrate to the fetus. Until about the 22nd week of intrauterine development in the fetus, the immune system completes its formation. It is after it becomes mature that hypersensitivity begins to develop. This means that after the 22nd week of pregnancy, a pregnant woman should review her diet and exclude from it foods that may be allergens for her.
Until about the 22nd week of intrauterine development in the fetus, the immune system completes its formation. It is after it becomes mature that hypersensitivity begins to develop. This means that after the 22nd week of pregnancy, a pregnant woman should review her diet and exclude from it foods that may be allergens for her.
Also, for the prevention of an allergic disease, one should not have much contact with recently appeared products from the field of cosmetics and household chemicals.
Expectant mothers who have ever been exposed to an allergic disease should completely exclude the possibility of contact with those allergens that have caused an allergic reaction at least once before. In addition, it is recommended not to have pets, to clean the house, preferably wet and daily, to carry out a complete house cleaning weekly, which should include airing rooms, vacuuming carpets and beating, drying pillows.
An important aspect of allergy prevention is fetal prevention. First of all, this is the restriction or refusal of the mother from highly allergenic foods. But since the child's immune system is not formed immediately, but only by the 22nd week of pregnancy, then, accordingly, the restriction in the use of highly allergenic foods makes sense from this period. Also, during the entire period of pregnancy, contact with household chemicals and new cosmetics should be limited.
First of all, this is the restriction or refusal of the mother from highly allergenic foods. But since the child's immune system is not formed immediately, but only by the 22nd week of pregnancy, then, accordingly, the restriction in the use of highly allergenic foods makes sense from this period. Also, during the entire period of pregnancy, contact with household chemicals and new cosmetics should be limited.
If the expectant mother has never had allergies before, then she can consume risky foods, in small quantities, and not every day, of course. Otherwise, you will have to abandon entire product groups.
Separately, it should be noted that smoking for a future mother during pregnancy and lactation is strictly prohibited, because it affects the development of the respiratory tract and lungs of the fetus, and can cause intrauterine growth retardation. It is also known that after smoking just one cigarette, a spasm of the uterus occurs, which leads to a violation of the supply of nutrients and oxygen to the fetus, and this can last 20-30 minutes. It is also worth refraining from having pets, vacuuming the room as often as possible, carrying out wet cleaning and knocking out and drying pillows weekly.
It is also worth refraining from having pets, vacuuming the room as often as possible, carrying out wet cleaning and knocking out and drying pillows weekly.
And of course, a pregnant woman needs to remember about a healthy lifestyle and the dangers of self-treatment and stress, because an unborn child requires no less care, and in some ways even more than a child who has already been born.
If the allergy nevertheless manifested itself and the doctor prescribed medication, you can search for medications through our website with catalogs of pharmacies in Kyiv.
Key nutrients needed during pregnancy
05/16/2019 The main nutrients needed during pregnancy.
You have probably heard about the importance of getting enough protein, iron, calcium, and folic acid during pregnancy. But the list doesn't end there - you need other important nutrients as well. Make sure you are getting enough of the most important nutrients listed below.
Calcium
This microelement performs plastic and structural functions in the body - it participates in the formation of bone tissue; gives stability to cell membranes, takes part in the implementation of intercellular communications; necessary for normal excitability of nervous tissue and contractility of muscle fibers, is an activator of a number of enzymes and hormones, an essential component of the blood coagulation system; participates in the regulation of the permeability of cell membranes, promotes the excretion of salts of heavy metals and radionuclides from the body, and exhibits an antioxidant effect. A growing child receives the calcium he needs from his mother, therefore, in order to ensure the health of the bones and, in the future, the teeth of the child, as well as to maintain her bones and teeth, the mother needs to compensate for the calcium spent by proper nutrition. Also, getting enough calcium can help prevent high blood pressure during pregnancy.
A healthy pregnant woman should receive at least 1000 mg of calcium per day and no more than 2500 mg. The best food sources of calcium are yogurt, milk, fortified fruit juice, cheese (like cheddar), tofu, cottage cheese.
Choline
This is an important organic compound that is involved in various physiological processes - from maintaining the correct structure of cells to the functioning of the nervous system. Choline helps prevent the development of neural tube defects in a child and promotes brain development. Choline is involved in osteogenesis and may help prevent high blood pressure in a pregnant woman. A pregnant woman should receive from 450 to 3500 mg per day. Food sources of choline are eggs, cod, salmon, beef, broccoli.
Docosahexaenoic acid
Docosahexaenoic acid is one of the omega-3 polyunsaturated fatty acids. It helps to stimulate the development of the brain and vision in the child, and in the mother, it can reduce the risk of developing heart disease in the future. A pregnant woman should receive 300 mg of docosahexaenoic acid per day. Sources of PUFAs are fatty fish (salmon, catfish, tuna), seafood (blue crab), eggs.
A pregnant woman should receive 300 mg of docosahexaenoic acid per day. Sources of PUFAs are fatty fish (salmon, catfish, tuna), seafood (blue crab), eggs.
Folic acid
Folic acid is of particular importance for the processes of growth and development, it has a positive effect on fat metabolism in the liver, the metabolism of cholesterol and a number of vitamins. It helps protect the baby from developing neural tube defects (during the first 30 days of pregnancy) and prevents miscarriages and premature births. In pregnant women, folic acid prevents the development of anemia. A woman during pregnancy should receive 600 micrograms of folic acid daily. The best sources of folic acid in nature are lentils, spinach, rice, broccoli, orange juice.
Iodine
The trace element iodine enhances energy processes, increases immune protection. It is essential for the development of the brain and nervous system, preventing growth retardation, severe mental retardation and deafness. Also important in preventing miscarriage and stillbirth. For a future mother, iodine is important in terms of thyroid health. A healthy pregnant woman should receive at least 250 mcg (and no more than 1100 mcg) of iodine per day. Sources of iodine are iodized salt, cod, yogurt, cottage cheese, baked potatoes with skins.
Also important in preventing miscarriage and stillbirth. For a future mother, iodine is important in terms of thyroid health. A healthy pregnant woman should receive at least 250 mcg (and no more than 1100 mcg) of iodine per day. Sources of iodine are iodized salt, cod, yogurt, cottage cheese, baked potatoes with skins.
Iron
This trace element plays an important role in the body, the main function is the transport of oxygen to the tissues. It is also an important component of many body enzymes and supports immune function. This trace element helps prevent premature birth and prevents the development of anemia in pregnant women. In the diet of a pregnant woman, at least 27 mg (and not more than 45 mg) of iron should be present daily. Food sources of iron include whole grain cereals, canned white beans, beef, lamb, chicken, fruits and vegetables, and leafy greens.
Potassium
This micronutrient is important for expectant mothers, as it allows you to control blood pressure and maintain the correct fluid balance. Potassium may also help prevent kidney stones and bone loss with age. Most prenatal vitamins do not contain potassium, so it is very important to get this trace element from food. During pregnancy, it is recommended to consume 4700 mg of potassium per day. Sources of potassium are fruits and vegetables (bananas are especially rich in them), melon, potatoes, prunes, raisins, acorn squash, spinach, orange and tomato juices.
Potassium may also help prevent kidney stones and bone loss with age. Most prenatal vitamins do not contain potassium, so it is very important to get this trace element from food. During pregnancy, it is recommended to consume 4700 mg of potassium per day. Sources of potassium are fruits and vegetables (bananas are especially rich in them), melon, potatoes, prunes, raisins, acorn squash, spinach, orange and tomato juices.
Riboflavin
One of the most important water-soluble vitamins (vitamin B2), coenzyme of many biochemical processes. It is involved in redox reactions in the body, is necessary for the formation of red blood cells, antibodies, for the regulation of growth and reproductive functions in the body. It is also essential for healthy skin, nails, growth, and overall health of the entire body, including thyroid function. During pregnancy, a woman needs 1.4 mg of riboflavin daily. Too much riboflavin can turn urine orange. Riboflavin is found in foods such as fortified cereals, skim milk, eggs, almonds, spinach, broccoli, chicken, salmon, and beef.
Vitamin B6
This vitamin is part of the enzyme system responsible for heme synthesis, supports the immune system, and helps in the production of protein for new cells. With its deficiency, irritability or lethargy and drowsiness, loss of appetite, nausea are observed. Pregnant women are advised to consume 1.9 mg per day. Unless your doctor prescribes vitamin B6 for you, do not take more than 100 mg per day. Vitamin B6 is found in foods such as fortified cereal, bananas, potatoes, chicken, salmon, spinach, hazelnuts, and vegetable juice.
Vitamin B12
This vitamin plays an important role in normal hematopoiesis (participates in the production of red blood cells) and the functioning of the nervous system. Stimulates growth, has a positive effect on fat metabolism in the liver, the state of the central and peripheral nervous system. During pregnancy, it is recommended to consume 2.6 micrograms of vitamin B12 daily. Shellfish, mussels, crabs, salmon, skim milk, beef, chicken and turkey are rich in vitamin B12.
Shellfish, mussels, crabs, salmon, skim milk, beef, chicken and turkey are rich in vitamin B12.
Vitamin C
Participates in redox reactions, stimulates growth, normalizes cholesterol metabolism, stimulates the activity of the endocrine glands, improves liver function, promotes iron absorption and normal hematopoiesis, increases the body's resistance to infections, chemical intoxication, overheating, cooling, oxygen starvation. During pregnancy, a woman should receive at least 85 mg and no more than 2000 mg daily. Fruits and vegetables are rich in vitamin C: sweet red and green peppers, melon, kiwi, strawberries, grapefruits, broccoli, oranges, tomatoes.
Vitamin D
Vitamin D helps absorb calcium from food and is involved in the formation and strengthening of bones and teeth. It also helps the muscles, nerves and immune system work properly.
For pregnant women, 600 IU or 15 micrograms is recommended daily. Do not exceed 4000 IU per day.
Do not exceed 4000 IU per day.
Our body produces vitamin D when exposed to the sun. But not everyone gets enough vitamin D this way, so it's important to get vitamin D from food as well. Vitamin D is found in salmon, tuna, beef liver, cheese, eggs, mushrooms, and fortified foods such as cereals, milk, and some fruit juices and soy drinks.
Zinc
This microelement plays an important role in the synthesis of protein and nucleic acids, regulates taste and smell sensitivity, protects the liver from chemical damage, is necessary for bone formation, and increases resistance to stress. It takes part in the formation of the child's brain. For an expectant mother, zinc is essential for cell growth and repair, as well as for energy production. Every day a woman needs to receive at least 11 mg and no more than 40 mg of zinc. Zinc is found in oysters (but don't eat raw oysters during pregnancy), crab, beef, pork, turkey, chickpeas, beans, nuts, and milk.