Women pregnancy problem
Pregnancy Complications | Maternal and Infant Health
The following are some common conditions that can happen before, during, or after pregnancy. You can help prevent and manage them by seeing a health care provider regularly before, during, and after your pregnancy.
Anemia
Anemia is having lower than the normal number of healthy red blood cells. People with anemia may feel tired and weak. You are more likely to get iron-deficiency anemia during pregnancy because your body needs more iron than normal. Your health care provider will check your number of red blood cells during your pregnancy. Treating the underlying cause of the anemia, if possible, can help restore the number of healthy red blood cells. Your provider may also recommend you take iron and/or folic acid supplements to help prevent and manage anemia.
Anxiety
Anxiety disorders are common before, during, and after pregnancy. If you have an anxiety disorder, you may struggle with uncontrollable feelings of anxiety, nervousness, fear, worry, and/or panic. These feelings can be intense and may last a long time. They can also interfere with relationships and daily activities, such as work or school. Anxiety disorders often occur with depression. Getting treatment for anxiety before, during, and after pregnancy is important. Talk to your health care provider as soon as possible if you think you have an anxiety disorder.
Depression
Everyone feels sad sometimes, but these feelings usually pass in a few days. Depression interferes with daily life and may last for weeks or months at a time. Some people have depression before, during, or after pregnancy. Symptoms of depression include:
- Lasting sad, anxious, or “empty” mood.
- Feelings of hopelessness or pessimism.
- Loss of energy.
- Trouble falling asleep or sleeping too much.
- Overeating or loss of appetite.
- Feelings of irritability or restlessness.
- Problems concentrating, recalling details, and making decisions.

- Feelings of guilt, worthlessness, or helplessness.
- Suicidal thoughts or suicide attempts.
If you have many of these symptoms together, and they last more than 2 weeks, you may have depression. Depression during pregnancy can make it hard for you to care for yourself and your pregnancy. Having depression before or during pregnancy is also a risk factor for postpartum depression, which is depression that occurs after pregnancy. Getting treatment is important for both mother and baby. Talk to your health care provider as soon as possible if you think you have depression. If you have thoughts of harming yourself or your baby, seek medical care immediately. More information is available at Depression During and After Pregnancy.
Top of Page
Diabetes
Diabetes is a disease that affects how your body turns food into energy. There are three main types of diabetes: type 1, type 2, and gestational diabetes. For pregnant people with type 1 or type 2 diabetes, high blood sugar around the time of conception increases the risk of birth defects, stillbirth, and preterm birth. Among people with any type of diabetes, high blood sugar throughout pregnancy can also increase the risk of preeclampsia, cesarean delivery, and the baby being born too large. To manage your diabetes, see your doctor as recommended, monitor your blood sugar levels, follow a good nutrition plan developed with your provider or dietician, be physically active, and take insulin, if directed. Managing diabetes can help you have a healthy pregnancy. If you have diabetes before pregnancy or develop it during pregnancy, it’s important to continue seeing your health care provider after pregnancy to monitor your blood sugar and overall health.
Among people with any type of diabetes, high blood sugar throughout pregnancy can also increase the risk of preeclampsia, cesarean delivery, and the baby being born too large. To manage your diabetes, see your doctor as recommended, monitor your blood sugar levels, follow a good nutrition plan developed with your provider or dietician, be physically active, and take insulin, if directed. Managing diabetes can help you have a healthy pregnancy. If you have diabetes before pregnancy or develop it during pregnancy, it’s important to continue seeing your health care provider after pregnancy to monitor your blood sugar and overall health.
Top of Page
Heart Conditions
Heart conditions, such as coronary artery disease, heart attack, cardiomyopathy, and congenital heart defects, impact the heart and blood vessels. Making healthy food choices, limiting your alcohol intake, quitting smoking if you smoke, and managing any other chronic conditions can help reduce your risk for many heart conditions.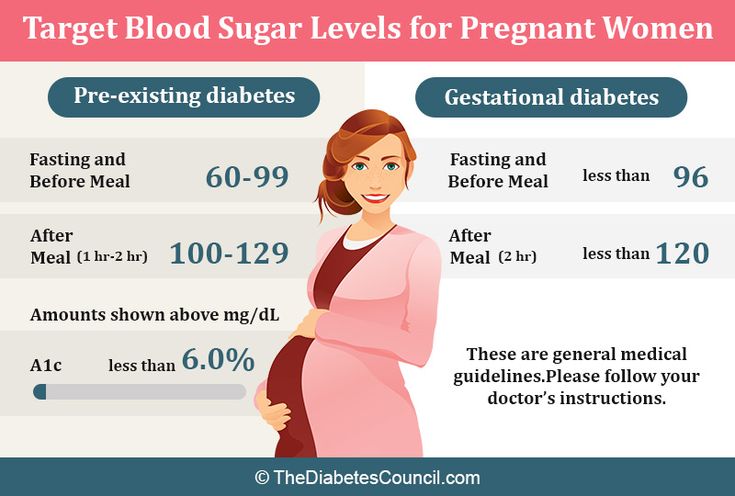 Not everyone has symptoms, but you may feel neck, jaw, chest, belly, or back pain if you have a heart condition. Many people with heart conditions have healthy, uneventful pregnancies, but pregnancy can put stress on the heart of people with some types of heart conditions. Having a heart condition may increase the risk of severe illness and death during and after pregnancy.
Not everyone has symptoms, but you may feel neck, jaw, chest, belly, or back pain if you have a heart condition. Many people with heart conditions have healthy, uneventful pregnancies, but pregnancy can put stress on the heart of people with some types of heart conditions. Having a heart condition may increase the risk of severe illness and death during and after pregnancy.
If you have a heart condition, it’s important to see your health care provider, ideally before pregnancy or as soon as possible after becoming pregnant. During your first prenatal care visit, let your provider know if you have a heart condition. If you are diagnosed with a heart condition during pregnancy, you may also need to be monitored by your provider earlier or more often after pregnancy. More information can be found at Heart Health and Pregnancy.
You may be at increased risk for other heart conditions in the future if you have some heart conditions, preeclampsia, or gestational diabetes during or shortly after pregnancy.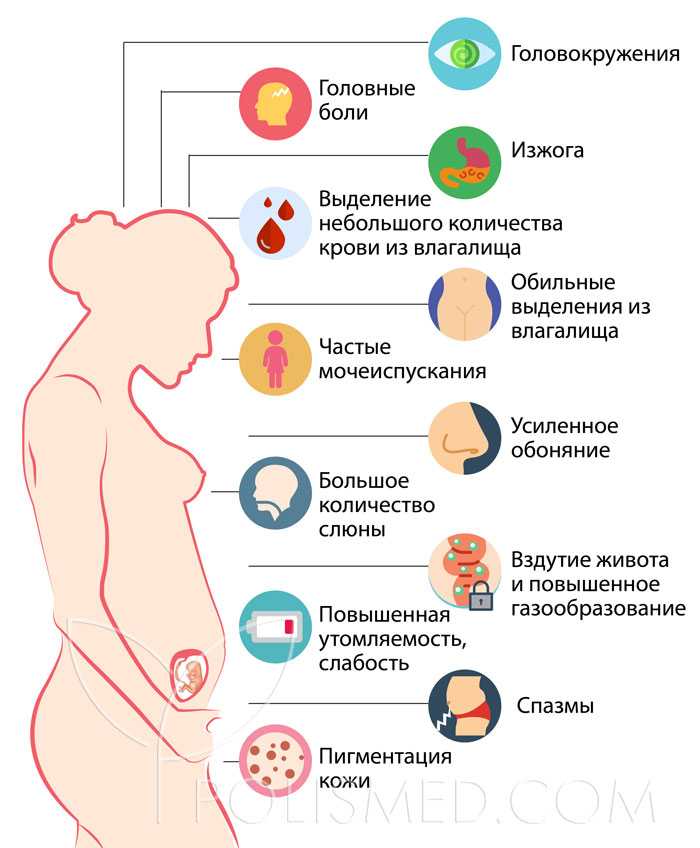 Work with your health care provider to monitor your risk or manage your heart condition before, during, and after pregnancy.
Work with your health care provider to monitor your risk or manage your heart condition before, during, and after pregnancy.
Top of Page
High Blood Pressure (Hypertension)
High blood pressure is a common heart condition occurring when your blood pressure is higher than normal. Chronic hypertension means having high blood pressure before you get pregnant or before 20 weeks of pregnancy. Gestational hypertension is high blood pressure that first occurs after 20 weeks of pregnancy. Preeclampsia happens if you previously had normal blood pressure and suddenly develop high blood pressure and protein in your urine or other problems after 20 weeks of pregnancy. If you have chronic hypertension, you can also get preeclampsia.
High blood pressure increases the risk of preterm delivery, and low birth weight, plus more serious issues such as eclampsia, stroke, and placental abruption (the placenta separating from the wall of the uterus). High blood pressure may be prevented and is treatable. These 7 strategies to live a heart-healthy lifestyle, plus at-home self-measured blood pressure monitoring with support from your health care provider, can help you manage your high blood pressure. If you are at high risk for preeclampsia, your provider may recommend low-dose aspirin after 12 weeks of pregnancy. Learn more about High Blood Pressure and Pregnancy.
These 7 strategies to live a heart-healthy lifestyle, plus at-home self-measured blood pressure monitoring with support from your health care provider, can help you manage your high blood pressure. If you are at high risk for preeclampsia, your provider may recommend low-dose aspirin after 12 weeks of pregnancy. Learn more about High Blood Pressure and Pregnancy.
Top of Page
Hyperemesis Gravidarum
Many pregnant people have some nausea or vomiting, or “morning sickness,” especially in the first 3 months of pregnancy. Hyperemesis gravidarum, however, is more extreme than “morning sickness.” It refers to persistent nausea and vomiting during pregnancy. This can lead to weight loss and dehydration and may require intensive treatment. If you are concerned about your symptoms, call your health care provider. If you have severe nausea (e.g., you are unable to drink for more than 8 hours or eat for more than 24 hours), seek medical care immediately.
Top of Page
Infections
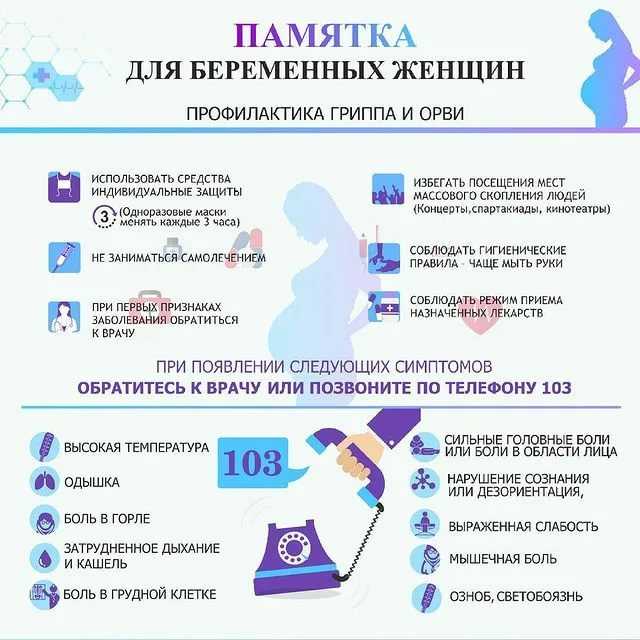
Infections can complicate pregnancy and may have serious consequences. Being screened and treated for infections, such as HIV and other sexually transmitted infections (STIs) and getting recommended vaccines can prevent many bad outcomes. Easy steps, including hand washing and avoiding certain foods, can also help protect you from some infections. Your health care provider can help you stay up to date with your vaccines. To learn more about different infections and how to protect your health, visit the following CDC pages:
Being screened and treated for infections, such as HIV and other sexually transmitted infections (STIs) and getting recommended vaccines can prevent many bad outcomes. Easy steps, including hand washing and avoiding certain foods, can also help protect you from some infections. Your health care provider can help you stay up to date with your vaccines. To learn more about different infections and how to protect your health, visit the following CDC pages:
- Pregnancy and HIV, Viral Hepatitis, STI & TB Prevention
- Vaccines During Pregnancy FAQs
- COVID-19 Vaccines While Pregnant and Breastfeeding
- Food Safety During Pregnancy
- 10 Tips for Preventing Infections Before and During Pregnancy
One common bacterial infection during pregnancy is a urinary tract infection (UTI). Your health care provider will likely test your urine early in pregnancy to see if you have a UTI and treat you with antibiotics, if necessary. Treatment will make it better, often in 1 or 2 days. Although not everyone with a UTI has symptoms, you may have a UTI if you have:
Although not everyone with a UTI has symptoms, you may have a UTI if you have:
- Pain or burning when you pee.
- Fever, tiredness, or shakiness.
- An urge to pee often.
- Pressure in your lower belly.
- Pee that smells bad or looks cloudy or reddish.
- Nausea or back pain.
Top of Page
Weight
Starting pregnancy at a healthy weight can help reduce the risk of preeclampsia, gestational diabetes, stillbirth, and cesarean delivery. If you are underweight [PDF – 1 MB] or overweight, talk to your health care provider about ways to reach and maintain a healthy weight before you get pregnant. Gaining a healthy amount of weight during pregnancy is also important for your health during and after pregnancy. Learn about pregnancy weight gain recommendations and steps to help you meet your pregnancy weight gain goal.
4 Common Pregnancy Complications | Johns Hopkins Medicine
When you find out you’re pregnant, your thoughts and emotions may go into overdrive.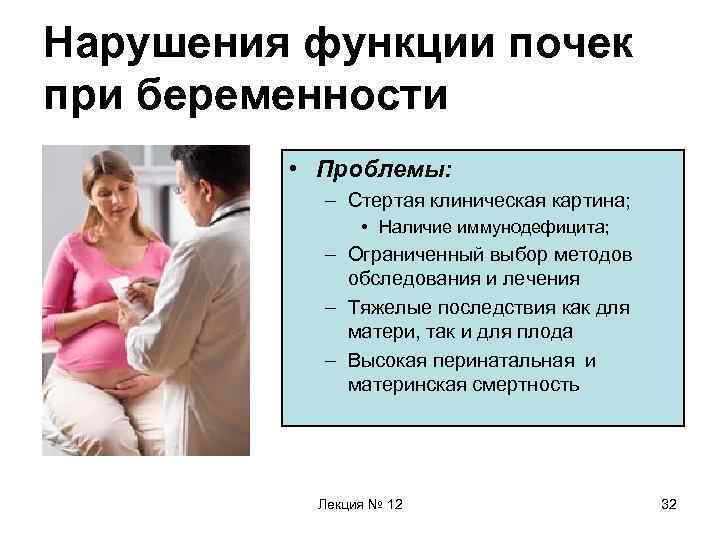 You might be as excited about this new person you will bring into the world as you are terrified that something may go wrong.
You might be as excited about this new person you will bring into the world as you are terrified that something may go wrong.
Most pregnancies progress without incident. But approximately 8 percent of all pregnancies involve complications that, if left untreated, may harm the mother or the baby. While some complications relate to health problems that existed before pregnancy, others occur unexpectedly and are unavoidable.
It can be scary to hear that doctors have diagnosed a complication. You may be worried about your baby’s health and your own health. You may even feel panic that perhaps something you did (or didn’t do) caused this to happen. These feelings are completely normal. It may reassure you to know that nothing you did caused these complications. And beyond that —these complications are treatable. The best thing you can do for you and your baby is to get prenatal care from a provider you trust. With early detection and proper care, you increase the chances of keeping you and your baby healthy.
A Johns Hopkins obstetrician discusses some common pregnancy complications and how they can be managed.
Hyperemesis Gravidarum
What is it? While many pregnant women experience morning sickness (nausea, possibly with vomiting, generally in the morning hours) and other discomforts during pregnancy , women with hyperemesis gravidarum (HG) have morning sickness times 1,000. HG is severe nausea that results in significant weight loss and may require hospitalization. (Though it may not make you feel any better, know that if you have HG, you are in royal company — Her Royal Highness The Duchess of Cambridge, Kate Middleton, suffered from it.)
What are the symptoms? Women with HG have severe nausea and vomiting. The vomiting and reduced appetite leads to weight loss and dehydration. The major difference between HG and normal morning sickness is that HG results in a weight loss of 5 percent or more of your pre-pregnancy weight.
Who is at risk? Doctors do not yet fully understand HG, what causes it or who is more likely to experience it.
Can you prevent it? You cannot prevent HG, but you can take steps to control and manage it during your pregnancy. The most important thing you can do for you and your baby is to get regular prenatal care. HG can lead to not getting enough nutrients, which can be harmful to both you and your baby. However, with proper treatment, there are typically no long-term effects to either mom or child after the pregnancy.
How is it treated? If you have been diagnosed with HG, the priority is ensuring you have enough nutrients to keep you and your baby healthy. For some women, a diet of bland foods and fluids may be enough, while others may need to take medication to help relieve the nausea. In severe cases, you may need to be hospitalized to receive nutrients and fluids via intravenous (IV) line. You may feel down about having to be in the hospital during your pregnancy. But remember that you are just doing what you need to do to protect your and your baby’s health!
Many women start to feel better by the 20th week of pregnancy, while some continue to experience symptoms throughout the entire pregnancy.
What should I ask my doctor? If you’ve had HG in the past, talk to your doctor when you are thinking about getting pregnant again. It’s important to make sure you are physically, emotionally and psychologically ready to begin another pregnancy. If you had severe weight loss or other nutritional deficiencies, you’ll need to talk to your doctor about making sure you are healthy before getting pregnant.
Gestational Diabetes
What is it? Diabetes is a condition that prevents your body from breaking down sugar. Gestational diabetes mellitus (GDM) is a type of diabetes that occurs during pregnancy. One of the biggest risks of gestational diabetes is that your baby may grow much larger than normal, a condition called macrosomia. During delivery, a baby’s shoulders can get stuck. If the baby is thought to be too big for a safe vaginal delivery, your doctor will recommend a cesarean section .
What are the symptoms? Gestational diabetes has no outward signs or symptoms. Doctors screen for it between 24 and 28 weeks of pregnancy, or earlier in high-risk women such as those who are overweight or have a history of gestational diabetes.
Doctors screen for it between 24 and 28 weeks of pregnancy, or earlier in high-risk women such as those who are overweight or have a history of gestational diabetes.
Who is at risk? Risk factors for gestational diabetes include being overweight or having a history of GDM in previous pregnancies. If you are at high risk, your doctor will screen for GDM earlier than 24 weeks, typically in the first trimester.
Can you prevent it? Losing weight before pregnancy, sticking to a healthy diet and getting regular exercise can lower your risk of developing GDM.
How is it treated? You and your doctor should discuss how you can best control the GDM. Good old diet and exercise seem to be a good place to start. A very high percentage of gestational diabetes can be controlled by diet. Still, some women with GDM will need to take medications (pills or even insulin) to control blood sugar levels.
Exercise during pregnancy , even just walking 30 minutes a day, is also great for controlling blood sugar. It’s best to do something you enjoy so you’ll stick with it, but you should let your doctor know what type of exercise you are doing.
It’s best to do something you enjoy so you’ll stick with it, but you should let your doctor know what type of exercise you are doing.
What should I ask my doctor? If you’ve had GDM, you and your baby are both at risk of developing type 2 diabetes later in life. So talk to your doctor about steps you can take to reduce that risk.
Placenta Previa
What is it? While you are pregnant, the placenta provides your baby with oxygen and nutrients for proper development. The placenta normally attaches to the upper part of the uterus, but in placenta previa it either totally or partially covers the cervix (which is the opening between the uterus and vagina).
Who is at risk? You may be at higher risk if you have scarring on your uterus from previous pregnancies or from a uterine surgery, or if you have fibroids .
What are the symptoms? The main symptom is vaginal bleeding that is not accompanied by cramping or other pain. Some women, however, do not experience any symptoms. Your doctor will confirm a diagnosis using an ultrasound or physical exam.
Some women, however, do not experience any symptoms. Your doctor will confirm a diagnosis using an ultrasound or physical exam.
Can you prevent it? There’s nothing you can do to prevent placenta previa. However, you can increase your and your baby’s health by getting regular prenatal care. If you are at high risk — because of a previous surgery, C-section or fibroids — make sure to tell your doctor. He or she may want to monitor you more closely during your pregnancy.
How is it treated? Placenta previa may result in bleeding during pregnancy. Some women have no bleeding, some have spotting and others may experience heavy bleeding. If the bleeding is heavy, you may need to stay in the hospital for a period of time. Women with placenta previa will require a C-section to deliver the baby, usually scheduled two to four weeks before their due date.
What should I ask my doctor? Always talk to your doctor if you notice any vaginal bleeding at any point during your pregnancy.
Preeclampsia
What is it? Preeclampsia is a condition that causes dangerously high blood pressure. It can be life-threatening if left untreated. Preeclampsia typically happens after 20 weeks of pregnancy, often in women who have no history of high blood pressure.
What are the symptoms? Symptoms of preeclampsia may include severe headache, vision changes and pain under the ribs. However, many women don’t feel symptoms right away. The first alert is usually when a woman comes in for a routine prenatal visit and has high blood pressure. In those cases, your doctor will test for things like kidney and liver function to determine whether it’s preeclampsia or just high blood pressure .
Who is at risk? Risk factors for preeclampsia include having a history of high blood pressure, being obese (having a body mass index, or BMI, greater than 30), age (teenage mothers and those over 40 are at higher risk) and being pregnant with multiples.
Can you prevent it? While you can’t prevent preeclampsia, staying healthy during pregnancy may help. If you have risk factors, experts recommend that you see your obstetrician either before you become pregnant or very early in your pregnancy, so you and your doctor can discuss ways that you can reduce your risk. For example, many women at risk for preeclampsia are prescribed a baby aspirin after the first trimester.
Regular prenatal visits are the best way to control preeclampsia. During those routine visits, your doctor will check your blood pressure. If it’s high, further tests can diagnose the condition so you can start getting the treatment you need.
How is it treated? The condition only goes away once the baby is born, so delivery is the best way to treat preeclampsia. However, delivering the baby too early can put the baby at risk for health problems. The decision about how to treat you will largely depend on how far along the pregnancy is. You may need to be hospitalized so your team can monitor you and your baby closely.
You may need to be hospitalized so your team can monitor you and your baby closely.
What should I ask my doctor? Your doctor will discuss the risks and benefits of delivering the baby early versus continuing the pregnancy and trying to manage the preeclampsia as long as possible through other methods. After delivery, the condition will go away, but you will be at greater risk for heart disease later in life. Talk to your doctor about what you can do to help reduce and manage those risks.
Pregnancy Complications: The Bottom Line
While these conditions may differ from one another, you may have noticed one common thread: Regular prenatal (even preconception) care is crucial. Women are encouraged to come in for a preconception consult to talk about what they can do to reduce their risks. Being healthy before pregnancy is the best thing you can do for your baby.
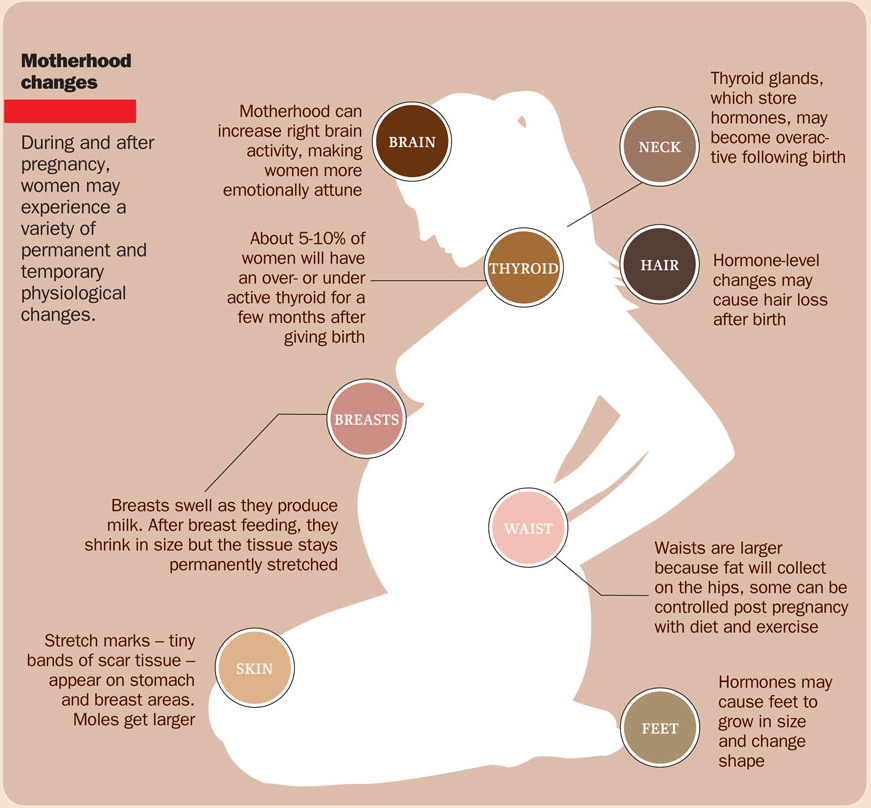
The SM-Clinic psychotherapist told how pregnancy affects the brain of a woman
Absent-mindedness, forgetfulness, tearfulness . .. It turns out that these "charms" of an interesting situation are almost impossible to control.
.. It turns out that these "charms" of an interesting situation are almost impossible to control.
“Women are more dependent on hormones than men. It is with changes in the hormonal background that the cyclical mood and behavior are associated - the so-called hormonal swing. In the first phase of the cycle, the level of estrogen rises, as a result, the emotional background normalizes. In the middle of the cycle, their number drops sharply, and the level of progesterone, just like during pregnancy, grows. At the end of the cycle, the level of progesterone drops - the mood decreases, life loses its colors.
Thinking
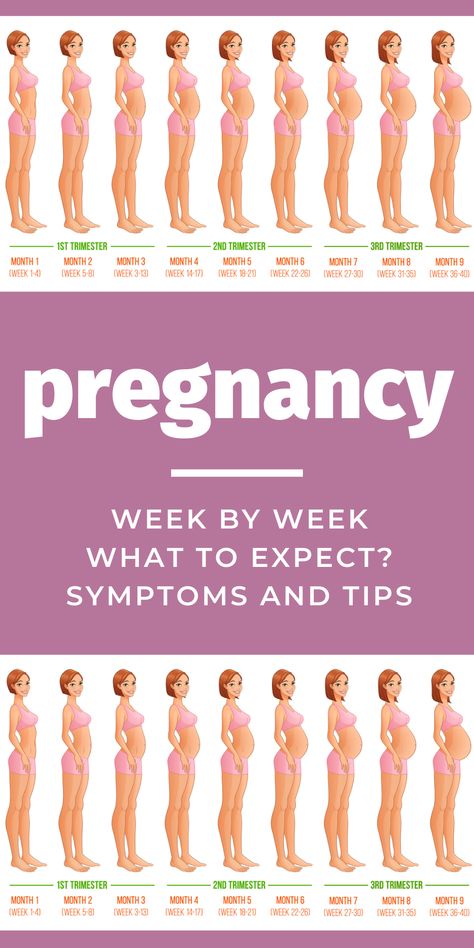
The body during the bearing of a baby suffers great stress, which is why the character and habits of a woman change. But not only! For many, it becomes a discovery that drowsiness, toxicosis and mood swings are far from all that awaits them. Chronic fatigue, inability to concentrate, memory lapses suddenly make themselves felt.
From the moment of conception, the level of progesterone increases. And the main reason for this is the emergence of a new hormone - the hormone of pregnancy (chorionic gonadotropin), which is produced by the placenta of the fetus. Already on the 6-8th day, he informs all organs and systems about the new state. It is progesterone, the concentration of which increases tenfold, that forms the dominant in the brain - the setting for the woman to perform the main function during this period - the continuation of life. And the endocrine and nervous systems are the first to be included in the restructuring process. Thanks to progesterone, pregnant women are focused solely on what is happening to them here and now.
The birth of a child is a double birth. A woman turns into a mother, and her way of thinking changes dramatically. The instincts of self-preservation, procreation, altruism and harmony, research, dominance, freedom and preservation of dignity come to the fore. However, not everyone is able to accept a new role for themselves. The reasons for this situation are different: from excessive demands on the expectant mother from relatives to her emotional immaturity. This is how neurotic disorders arise, accompanied even after childbirth by surges in pressure, insomnia, migraines.
The reasons for this situation are different: from excessive demands on the expectant mother from relatives to her emotional immaturity. This is how neurotic disorders arise, accompanied even after childbirth by surges in pressure, insomnia, migraines.
Psychic
In the first half of pregnancy, the processes of excitation in the nervous system prevail over the processes of inhibition. It is difficult to please an expectant mother: desires change five times a day, however, like mood. Husbands attribute everything to whims (well, of course, she wants more attention) and stock up on patience in the hope that this will end soon.
But not everything is clear! In nine months, more estrogen is produced in a woman's body than in her entire life, and the peak is reached in the third trimester. They stimulate the growth of the uterus, normalize vascular tone and blood pressure, promote childbirth. In addition, the function of the thyroid gland increases, as a result, the metabolism accelerates, the condition of the skin and hair improves. Adrenal function is also activated as a reaction to stress, which can cause pigmentation.
Adrenal function is also activated as a reaction to stress, which can cause pigmentation.
In the second half of pregnancy, inhibition processes in the nervous system dominate over excitation processes. During this period, emotions cease to go off scale, a woman becomes balanced and calm, even her voice becomes lower and more monotonous. At the same time, drowsiness appears, mental functions weaken, memory begins to fail.
Neurophysiologists have found that a woman's gray matter volume decreases by 6% during pregnancy. Thus, the problem of “cutting off the excess” is solved, which can make the work of other parts of the brain more efficient in terms of mastering the skills necessary for motherhood. Perhaps this process increases the productivity and specialization of certain parts of the brain. This helps the mother recognize the baby's needs and dangers.
Memory
Under the influence of the hormone oxytocin, labor begins. After childbirth, oxytocin triggers the maternal instinct and allows a woman to experience incredible tenderness for the baby. Progesterone drops to a minimum after childbirth, and young mothers go crazy with anxiety and anxiety. And also from the reproaches of the spouse, dissatisfied with the forgetfulness of his beloved. Yes, the new role overshadows the performance of tasks that are not related to the child. But this is a psychological problem.
After childbirth, oxytocin triggers the maternal instinct and allows a woman to experience incredible tenderness for the baby. Progesterone drops to a minimum after childbirth, and young mothers go crazy with anxiety and anxiety. And also from the reproaches of the spouse, dissatisfied with the forgetfulness of his beloved. Yes, the new role overshadows the performance of tasks that are not related to the child. But this is a psychological problem.
And there is another one - the restructuring of the hormonal background and its return to the "pre-pregnancy" norm. Plus the constant lack of sleep. Hence the distraction, the inability to concentrate. But don't panic! First, this is a temporary phenomenon. After childbirth, the size of the brain reaches its previous state within two years, and the emotional background also normalizes.
And secondly, changes in the brain occur in areas responsible for short-term memory. So you should not worry that after the birth the name of the betrothed will be forgotten. In addition, not all women experience such difficulties. It is believed that the less the child causes unrest to the mother (he is in good health, does not cry at night), the better her brain works. In addition, some studies prove that childbirth after 35 years (and this is not such a rarity) has a beneficial effect on brain cells.
In addition, not all women experience such difficulties. It is believed that the less the child causes unrest to the mother (he is in good health, does not cry at night), the better her brain works. In addition, some studies prove that childbirth after 35 years (and this is not such a rarity) has a beneficial effect on brain cells.
If there is a problem, you need:
- Get more sleep. During sleep, gray matter cells regenerate faster.
- Take vitamin complexes under medical supervision. Most often, women who have given birth experience a lack of iron, zinc, magnesium, B12, C, D.
- Train your brain: memorize, for example, the words of your favorite songs or solve crossword puzzles.
- Do not immerse yourself in negative information, move away from any sources of stress.
- More often to be in the fresh air.
- Include healthy foods in the menu: walnuts, black currants, broccoli, onions, tomatoes, apples, cocoa, red fish, sea kale.
 Be careful if you are a breastfeeding mother.
Be careful if you are a breastfeeding mother.
Published on the portal parents.ru
Pregnancy: A terrible word DANGER! Let's save ourselves!
Our today's conversation will touch upon recommendations for a pregnant woman who is faced with such a complication of pregnancy as a threatened miscarriage.
Pregnancy is a physiological process for the female body. If a woman is young (18-30 years old) and healthy, then, as a rule, pregnancy proceeds without complications. Recently, in the world and in our country, there has been a sharp deterioration in the health of women of reproductive age.
Complications of pregnancy for a better understanding of the reader can be divided into 3 groups (these are not standards).
- Firstly, the complications associated with the pregnancy itself, if it were not for this condition, then there would be no complication - the threat of abortion (the threat of premature birth).

- Secondly, these are complications associated with a disease (for example, rubella) that occurred during pregnancy.
- Thirdly, these are complications that arose in a woman who suffered from a particular disease before pregnancy (perhaps the first exacerbation of this disease is associated with pregnancy).
The most unpleasant psychological and physical complications are threatened miscarriage . If this happens in the early stages, then the term is used, the threat of termination of pregnancy ", if in the later stages (after 28 weeks), then " the threat of premature birth.
What to do if there is a threat of termination of pregnancy
In some countries, including Russia, it is customary to keep a pregnancy of any term; accordingly, if a woman notices spotting during pregnancy, then she immediately should see a doctor during the daytime or call the emergency team at night. But the question of the expediency of maintaining pregnancy with the onset of bleeding up to 12 weeks remains open, because. it is known that 70-80% of pregnancies terminated during this period are associated with chromosomal pathologies, sometimes incompatible with life. Those. It can be said that the body itself corrects its mistakes.
But the question of the expediency of maintaining pregnancy with the onset of bleeding up to 12 weeks remains open, because. it is known that 70-80% of pregnancies terminated during this period are associated with chromosomal pathologies, sometimes incompatible with life. Those. It can be said that the body itself corrects its mistakes.
Reasons for termination of pregnancy
Termination of pregnancy may also be associated with cervical incompetence . Those. its upper part may not be tightly closed, i.e. unable to play the role of a "castle". This condition can be caused by trauma during previous births or during abortions ( even if it was a single ). In this case, treatment is carried out in a hospital, and in the future, pregnancy is observed by an outpatient doctor. A woman can be stitched on the cervix if such a diagnosis is made at 16-20 weeks or a special retaining ring is placed if complaints appear later than this period. The suture or ring is removed at the time of the onset of labor, i.e. with the appearance of regular contractions or the outflow of amniotic fluid. However, this procedure can be performed two weeks before the expected date of birth.
The suture or ring is removed at the time of the onset of labor, i.e. with the appearance of regular contractions or the outflow of amniotic fluid. However, this procedure can be performed two weeks before the expected date of birth.
Termination of pregnancy may be associated with the hormonal status of a woman , therefore hormones play a leading role in the treatment of this complication. In order to clarify the diagnosis in the antenatal clinic, they can take the so-called “threat smear” (this is not a 100% confirmation of the diagnosis). Of course, hormones play one of the main roles in the regulation of pregnancy. The problem of treatment of miscarriage is very complex and multifaceted. I repeat that in our country it is customary to preserve early pregnancy. For this purpose, hormone therapy is used, based on the physiological and pathogenetic processes of the onset and development of pregnancy. A woman diagnosed with threatened miscarriage or threatened miscarriage is admitted to the hospital for appropriate therapy in severe condition, or may be observed on an outpatient basis and given hormonal therapy, as in inpatient treatment.
Symptoms of a threatened miscarriage
As for the threat of preterm labor, the first symptoms may not be spotting, but simply heavy discharge (sometimes a woman thinks that she has urinary incontinence). This may be a signal that the integrity of the fetal bladder is broken. Of course, in this case, you should immediately consult a doctor. If it is daytime, then a doctor of antenatal clinic is enough. At night, it is better to call an ambulance or get to the maternity hospital on your own.
In later pregnancy there may also be spotting . The reason for them may be a low-lying placenta and constant uterine contractions (uterine tone). It is the tone of the uterus that can cause placental abruption and, accordingly, bleeding. Contacting a doctor should be in the same mode as described above.
Special mention should be made of ectopic pregnancy . This condition can also be associated with the threat of termination, only the consequences of the termination of an ectopic pregnancy can adversely affect the woman's health. An ectopic pregnancy is a condition in which a fertilized egg attaches itself outside the uterine cavity. This place is most often tubes, but an ectopic pregnancy can also be found directly in the ovary or in the abdominal cavity. The diagnosis of "ectopic pregnancy" requires immediate surgical intervention. The scope of the operation and operative approach (cavitary or laparoscopic) can only be decided in a hospital setting and depends on many factors, including complications that have arisen at the time of admission to the hospital. Very often, an ectopic pregnancy occurs when there is a malfunction of the villi that are in the tubes and push the fertilized egg into the uterine cavity. It is impossible to predict this state. However, it can occur most often in chronic inflammatory diseases of the pelvic organs.
This condition can also be associated with the threat of termination, only the consequences of the termination of an ectopic pregnancy can adversely affect the woman's health. An ectopic pregnancy is a condition in which a fertilized egg attaches itself outside the uterine cavity. This place is most often tubes, but an ectopic pregnancy can also be found directly in the ovary or in the abdominal cavity. The diagnosis of "ectopic pregnancy" requires immediate surgical intervention. The scope of the operation and operative approach (cavitary or laparoscopic) can only be decided in a hospital setting and depends on many factors, including complications that have arisen at the time of admission to the hospital. Very often, an ectopic pregnancy occurs when there is a malfunction of the villi that are in the tubes and push the fertilized egg into the uterine cavity. It is impossible to predict this state. However, it can occur most often in chronic inflammatory diseases of the pelvic organs.
What to do in case of termination of pregnancy
If the pregnancy could not be maintained, then the question arises of the reasons for this situation. After what happened, an examination is necessary, which will include an examination of both spouses. It is necessary to obtain the results of a histological examination and consult a geneticist . A woman will be examined by a gynecologist for infections or hormonal disorders, a man needs to consult a urologist (andrologist) for the same examination.
Sometimes it is very difficult to find the cause, but this is not a reason to despair. Subsequent pregnancies can pass without complications, and the first unsuccessful attempt is quickly forgotten. With a successful examination , it is recommended to plan the next pregnancy in 4-6 months .
Everything that we have talked about should draw attention to the health of a pregnant woman and help her orient herself in the event of a particular situation. A desired pregnancy is a joyful state for a woman and her family. The task of the doctor is to prevent and, as far as possible, solve the problem with a positive result.
A desired pregnancy is a joyful state for a woman and her family. The task of the doctor is to prevent and, as far as possible, solve the problem with a positive result.
Doctors of the Fetal Medicine Center are one of the leading specialists in prenatal diagnostics, candidates of medical sciences, doctors of the highest categories with a narrow specialization and extensive experience in prenatal medicine.
All ultrasound examinations in the center are carried out according to the international standards of FMF (Fetal Medicine Foundation) and ISUOG (International Society for Ultrasound in Obstetrics and Gynecology).
Ultrasound doctors have international certificates from the Fetal Medicine Foundation (Fundamental Medicine, UK), which are are confirmed annually.
We take care of the most complex cases and, if necessary, it is possible to consult with specialists from King's College Hospital, King's College Hospital (London, UK).