How to administer cpr on a child
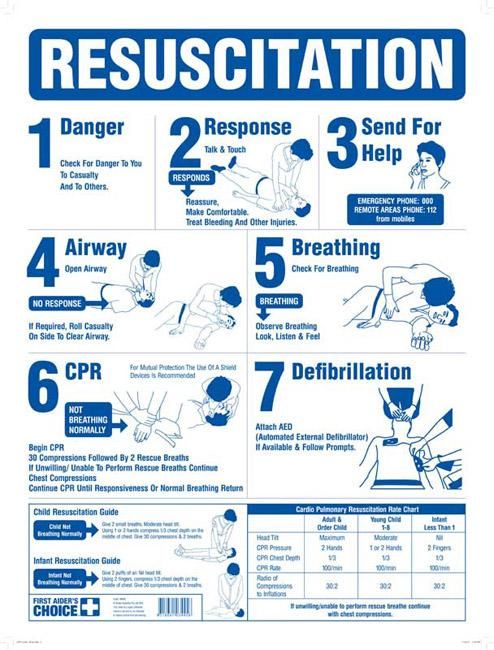
How to resuscitate a child
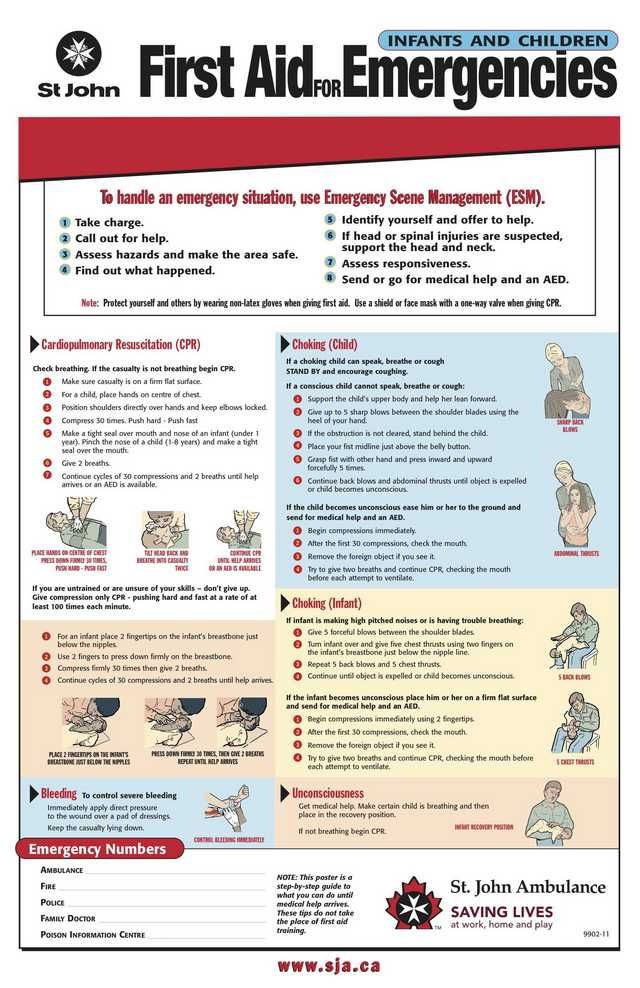
This page provides the full detailed cardiopulmonary resuscitation (CPR) sequence for infants (babies under 1 year old) and children.
It's highly recommended that every parent or carer goes on a first aid course, as it makes this process much easier to understand and remember.
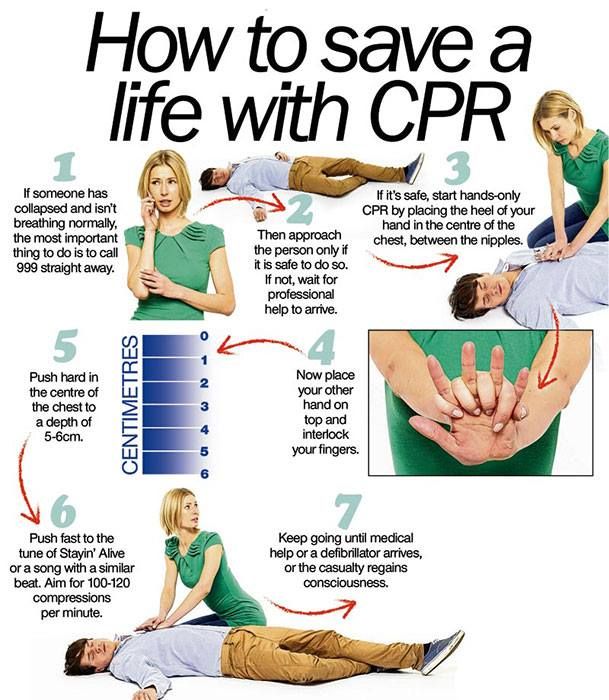
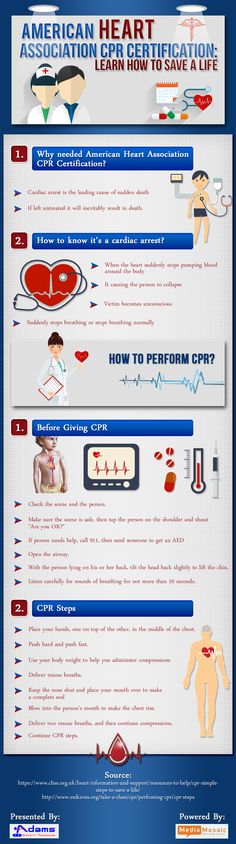
If a baby or child is unresponsive and not breathing normally, call 999 and start CPR straight away.
When you call 999 for an ambulance, you should be given basic life-saving instructions over the phone, including advice about CPR.
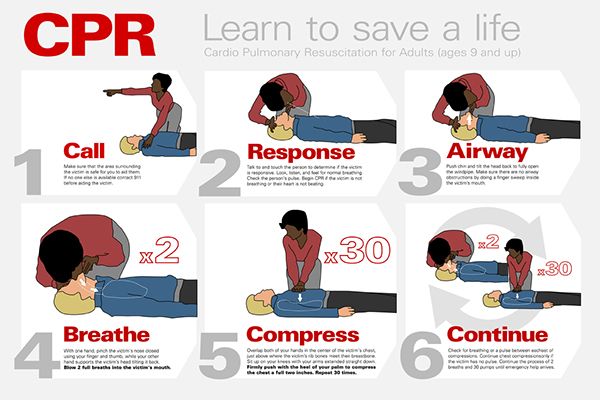
Child and baby CPR steps
1. Ensure the area is safe
- Check for hazards, such as electrical equipment or traffic.
2. Check your child's responsiveness
- Gently stimulate your child and ask loudly: "Are you alright?"
3a.
- Leave them in the position they were found in (provided they're not in danger).
- Check their condition and get help if needed.
- Reassess the situation regularly.
3b. If your child does not respond
- Call for help.
- Carefully turn the child on their back.
If the child is under 1 year old:
- Ensure the head is in a neutral position, with the head and neck in line.
- At the same time, with your fingertips under the point of your child's chin, lift the chin. Do not push on the soft tissues under the chin as this may block the airway.
If the child is over 1 year old:
- Open your child's airway by tilting the head and lifting the chin.
- To do this, place your hand on their forehead and gently tilt their head back.
- At the same time, with your fingertips under the point of your child's chin, lift the chin. Do not push on the soft tissues under the chin as this may block the airway.
If you think there may have been an injury to the neck, tilt the head carefully, a small amount at a time, until the airway is open. Opening the airway takes priority over a possible neck injury.
4. Check their breathing
Keeping the airway open, look, listen and feel for normal breathing by putting your face close to your child's face and looking along their chest.
- Look for chest movements.
- Listen at the child's nose and mouth for breathing sounds.
- Feel for air movement on your cheek.
Look, listen and feel for no more than 10 seconds before deciding that they're not breathing.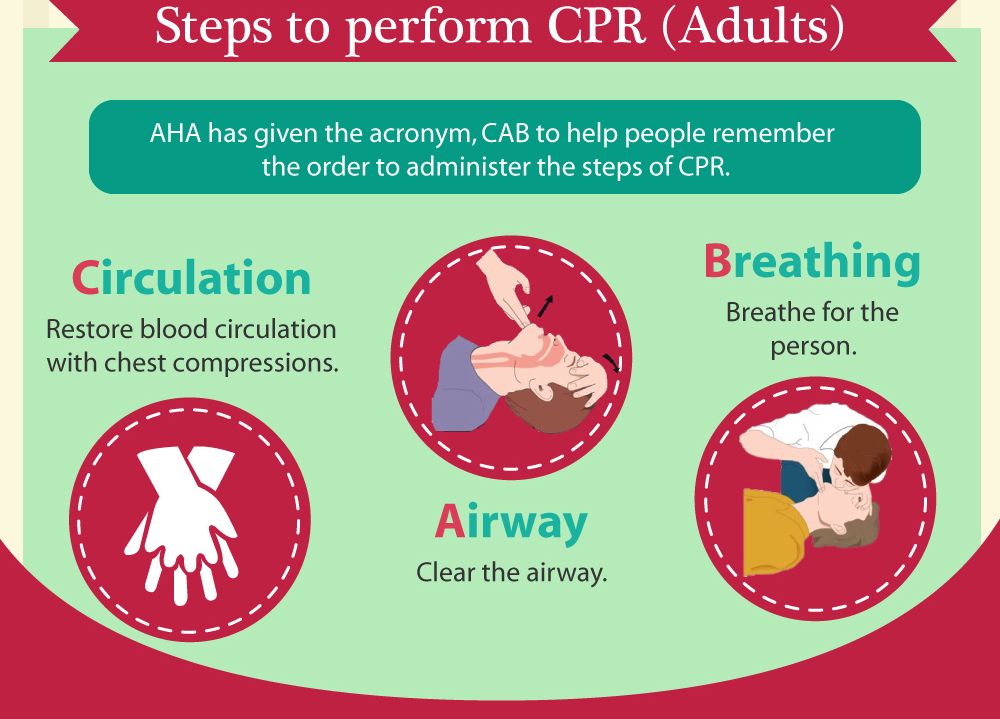 Gasping breaths should not be considered to be normal breathing.
Gasping breaths should not be considered to be normal breathing.
5a. If your child is breathing normally
- Turn them on their side.
- Check for continued breathing.
- Send or go for help – do not leave your child unless absolutely necessary.
5b. If your child is not breathing or is breathing infrequently and irregularly
- Carefully remove any obvious obstruction in the mouth.
- Give 5 initial rescue breaths (mouth-to-mouth resuscitation).
- While doing this, note any gag or cough response – this is a sign of life.
Rescue breaths for a baby under 1 year
- Ensure the head is in a neutral position and lift the chin.
- Take a breath, then cover your baby's mouth and nose with your mouth, making sure it's sealed.
 If you cannot cover both the mouth and nose at the same time, just seal either with your mouth. If you choose the nose, close the lips to stop air escaping.
If you cannot cover both the mouth and nose at the same time, just seal either with your mouth. If you choose the nose, close the lips to stop air escaping. - Blow a breath steadily into the baby's mouth and nose over 1 second. It should be sufficient to make the chest visibly rise.
- Keeping their head tilted and chin lifted, take your mouth away and watch for the chest to fall as air comes out.
- Take another breath and repeat this sequence 4 more times.
Rescue breaths for a child over 1 year
- Tilt the head and lift the chin.
- Close the soft part of their nose using the index finger and thumb of the hand that's on their forehead.
- Open their mouth a little, but keep the chin pointing upwards.
- Take a breath, then place your lips around their mouth, making sure it's sealed.

- Blow a breath steadily into their mouth over about 1 second, watching for the chest to rise.
- Keeping their head tilted and chin lifted, take your mouth away and watch for the chest to fall as air comes out.
- Take another breath and repeat this sequence 4 more times. Check that your child's chest rises and falls in the same way as if they were breathing normally.
5c. Obstructed airway
If you have difficulty achieving effective breathing in your child, the airway may be obstructed.
- Open the child's mouth and remove any visible obstruction. Do not poke your fingers or any object into the mouth.
- Ensure there's adequate head tilt and chin lift, but the neck is not overextended.
- Make up to 5 attempts to achieve effective breaths (enough to make the chest visibly rise).
 If this is still unsuccessful, move on to chest compressions combined with rescue breaths.
If this is still unsuccessful, move on to chest compressions combined with rescue breaths.
6. Assess the circulation (signs of life)
Look for signs of life. These include any movement, coughing, or normal breathing – not abnormal gasps or infrequent, irregular breaths.
Signs of life present
If there are definite signs of life:
- Continue rescue breathing until your child begins to breathe normally for themselves.
- Turn the child on their side into the recovery position and send for help.
- Continue to check for normal breathing and provide further rescue breaths if necessary.
No signs of life present
If there are no signs of life:
- Start chest compressions immediately.
- Combine chest compressions with rescue breaths, providing 2 breaths after every 30 compressions.
7. Chest compressions: general guidance
- To avoid compressing the stomach, find the point where the lowest ribs join in the middle, and then 1 finger's width above that. Compress the breastbone.
- Push down 4cm (for a baby or infant) or 5cm (a child), which is approximately one-third of the chest diameter.
- Release the pressure, then rapidly repeat at a rate of about 100-120 compressions a minute.
- After 30 compressions, tilt the head, lift the chin, and give 2 effective breaths.
- Continue compressions and breaths in a ratio of 2 breaths for every 30 compressions.
Although the rate of compressions will be 100-120 a minute, the actual number delivered will be fewer because of the pauses to give breaths.
The best method for compression varies slightly between infants and children.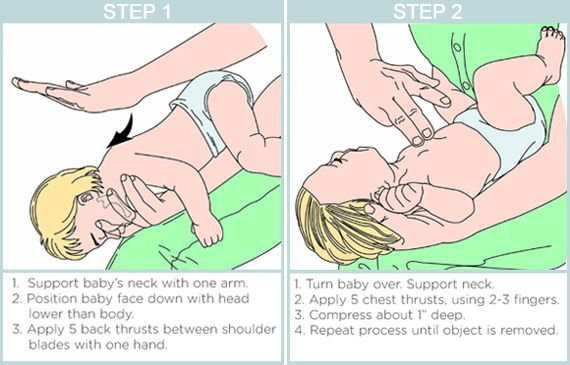
Chest compression in babies less than 1 year
- Do the compressions on the breastbone with the tips of 2 fingers, not the whole hand or with both hands.
- The quality (depth) of chest compressions is very important. If the depth of 4cm cannot be achieved with the tips of 2 fingers, use the heel of 1 hand.
Chest compression in children over 1 year
- Place the heel of 1 hand over the lower third of the breastbone.
- Lift the fingers to ensure pressure is not applied over the ribs.
- Position yourself vertically above the chest and, with your arm straight, compress the breastbone so you push it down 5cm, which is approximately one-third of the chest diameter. The quality (depth) of chest compressions is very important.
- In larger children or if you're small, this may be done more easily by using both hands with the fingers interlocked, avoiding pressure on the ribs.
If you had no response to your call for help and you're alone, continue resuscitation for about 1 minute before trying to get help – for example, by calling 999.
8. Continue resuscitation until
- Your child shows signs of life – normal breathing, coughing, movement of arms or legs.
- Qualified help arrives.
Further information on first aid
- St John Ambulance: How to do baby CPR
- St John Ambulance: How to do CPR on a child
- British Red Cross: First aid training courses
Page last reviewed: 28 September 2022
Next review due: 28 September 2025
How to Perform Child and Baby CPR
Your browser's Javascript functionality is turned off. Please turn it on so that you can experience the full capabilities of this site.
Please turn it on so that you can experience the full capabilities of this site.
-
Although you hope you'll never use cardiopulmonary resuscitation (CPR) for a child or infant, it's important to know the steps so that you can help in the event of a cardiac or breathing emergency. And although you may have taken a class in child CPR, it's a good idea to keep the steps handy so that the information stays fresh in your memory. With our printable step-by-step guide, you can access the child and baby CPR steps anytime, anywhere. Simply print them up and place them in your car, your desk, your kitchen or with your other first aid supplies, then read over them from time to time to help maintain your skills.
Find a Class
Before Giving Child or Baby CPR
1
Check the scene for safety, form an initial impression, obtain consent from the parent or guardian, and use personal protective equipment (PPE)
2
If the child or baby appears unresponsive, check the child or baby for responsiveness (shout-tap-shout)
- For a child, shout to get the child’s attention, using the child’s name if you know it.
 If the child does not respond, tap the child’s shoulder and shout again while checking for breathing, life-threatening bleeding or another obvious life-threatening condition
If the child does not respond, tap the child’s shoulder and shout again while checking for breathing, life-threatening bleeding or another obvious life-threatening condition - For a baby, shout to get the baby’s attention, using the baby’s name if you know it. If the baby does not respond, tap the bottom of the baby’s foot and shout again while checking for breathing, life-threatening bleeding or another obvious life-threatening condition
- Check for no more than 10 seconds
3
If the child or baby does not respond and is not breathing or only gasping, CALL 9-1-1 and get equipment, or tell someone to do so
Performing Child & Baby CPR
1
Place the child or baby on their back on a firm, flat surface
- For a child, kneel beside the child
- For a baby, stand or kneel to the side of the baby, with your hips at a slight angle
2
Give 30 compressions
- For a child, place the heel of one hand in the center of the child’s chest, with your other hand on top and your fingers interlaced and off the child’s chest
- Position your shoulders directly over your hands and lock your elbows
- Keep your arms straight
- Push down hard and fast about 2 inches at a rate of 100 to 120 per minute
- Allow the chest to return to normal position after each compression
- For a small child, use a one-handed CPR technique
- Place the heel of one hand in the center of the child’s chest
- Push down hard and fast about 2 inches at a rate of 100 to 120 per minute
- For a baby, place both thumbs (side-by-side) on the center of the baby’s chest, just below the nipple line
- Use the other fingers to encircle the baby’s chest toward the back, providing support
- Using both thumbs at the same time, push hard down and fast about 1 ½ inches at a rate of 100 to 120 per minute
- Allow the chest to return to its normal position after each compression
- Alternatively, for a baby, use the two-finger technique
- Use two fingers placed parallel to the chest in the center of the chest
- For a baby, if you can’t reach the depth of 1 ½ inches, consider using the one-hand technique
3
Give 2 breaths
- For a child, open the airway to a slightly past-neutral position using the head-tilt/chin-lift technique
- For a baby, open the airway to a neutral position using the head-tilt/chin-lift technique
- Blow into the child or baby’s mouth for about 1 second
- Ensure each breath makes the chest rise
- Allow the air to exit before giving the next breath
- If the first breath does not cause the chest to rise, retilt the head and ensure a proper seal before giving the second breath.
 If the second breath does not make the chest rise, an object may be blocking the airway
If the second breath does not make the chest rise, an object may be blocking the airway
4
Continue giving sets of 30 chest compressions and 2 breaths until:
- You notice an obvious sign of life
- An AED is ready to use
- Another trained responder is available to take over compressions
- EMS personnel arrive and begin their care
- You are alone and too tired to continue
- The scene becomes unsafe
- You have performed approximately 2 minutes of CPR (5 sets of 30:2), you are alone and caring for baby, and you need to call 9-1-1
Be prepared for moments that matter by taking a CPR class and you could help save a life.
Find a Class
- For a child, shout to get the child’s attention, using the child’s name if you know it.
How to resuscitate a child: chest compressions and artificial respiration
The first minutes after an injury are the most important. If you immediately provide competent first aid, then the victim is more likely to live and live without consequences.
 But how can you help your child? How to resuscitate a child, how to perform artificial respiration and chest compressions? In relation to babies, there are some critical features, especially for children under 1 year old.
But how can you help your child? How to resuscitate a child, how to perform artificial respiration and chest compressions? In relation to babies, there are some critical features, especially for children under 1 year old. Updated:
- What you need to know about resuscitation of a child?
- Cardiopulmonary resuscitation of a child: what should be done?
Unfortunately, today little Ukrainians become victims of military battles taking place on the territory of Ukraine. And in these realities, we, adults, should know how to help a child in an emergency before the ambulance arrives, because it is the first minutes after the injury that are decisive - if you provide the right help, the child will be able to continue to lead a normal life after recovery.
In this article, our medical experts tell you how to resuscitate a child, give artificial respiration and chest compressions before the arrival of an ambulance, because little patients have their own peculiarities.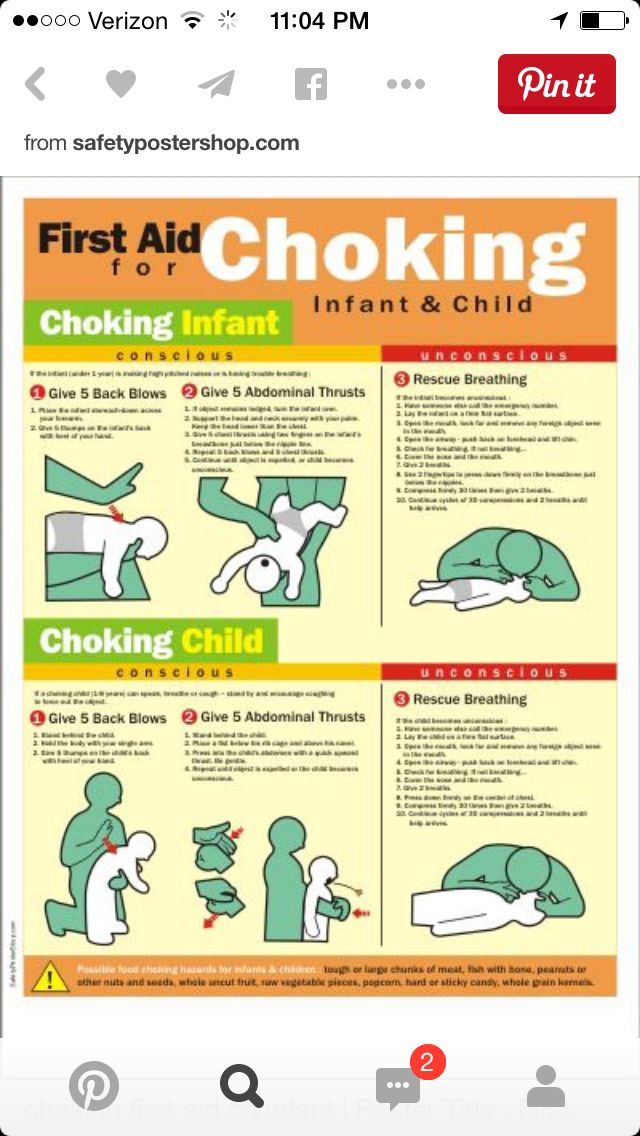
What you need to know about resuscitation of a child?
Emergency cardiopulmonary resuscitation is needed in various sudden situations, in particular in accidents.
Circulatory arrest leads to disruption of oxygen supply to all organ systems. The brain is most sensitive to hypoxia (lack of oxygen), in its tissues, first of all, when blood circulation stops, irreversible changes occur. This period can last 3-6 minutes maximum. For this reason, assistance must be provided in a timely, correct and fast manner.
Assessing the child's condition, first of all, it is necessary to check such parameters as:
- consciousness;
- breath;
- blood circulation.
Check the signs of consciousness in the child: does he answer the question addressed to him, does he react to touch? See if the child has any injuries or bleeding. If the child does not react, it is necessary to determine whether the child is breathing. Bring your ear to your child's mouth and nose. Is there breath on your cheek? Is the baby's chest moving?
Bring your ear to your child's mouth and nose. Is there breath on your cheek? Is the baby's chest moving?
If the child is unconscious but breathing, place the child in a stable lateral position to maintain a clear airway.
Position the child's arm on your side at a right angle to their body. Place the far hand of the child with the back of your hand on his opposite cheek, holding it with your hand. After that, bend the farthest leg of the child at the knee, place it resting on the foot, push the knee of this leg towards you and turn the child. After turning the child on its side, slightly tilt the head to open the airway and pull the leg lying on top closer to the stomach.
Cardiopulmonary resuscitation of a child: what should be done?
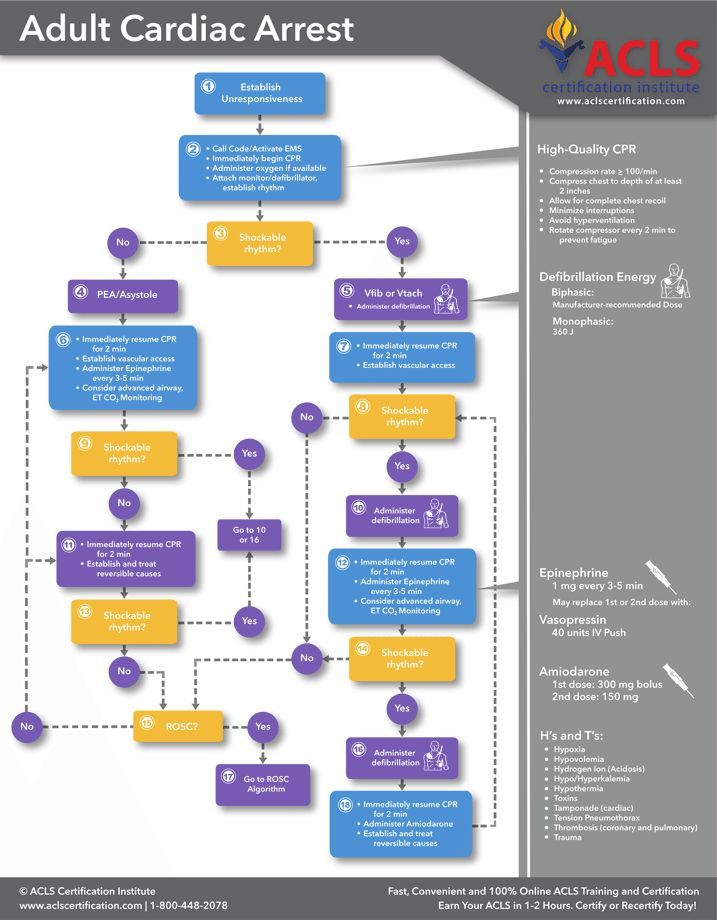
If the child is not responding and not breathing, urgently call an ambulance and perform cardiopulmonary resuscitation. Required:
- ensure airway patency;
- determine the pulse on the carotid artery;
- if the pulse is not detected - urgently perform chest compressions.

How to give artificial respiration to a child?
Lay the child on a hard surface on their back to ensure a good airway, then examine the airway. The oral cavity is freed from blood, vomit with a finger with a gauze swab, napkin or handkerchief.
The next step is to ensure the patency of the larynx. Place one hand on your forehead, tilt your head back and lift your chin. Remove your hand from your forehead and pinch the soft part of your nose. Before starting an indirect heart massage, five breaths (breaths) must be taken. These are short breaths and should not be longer than 1 second each.
Tilt your head, inhale and grasp the child's mouth.
Blow slowly and evenly into his mouth for one second until the chest rises.
The main criterion for the effectiveness and control of mechanical ventilation is chest excursion, the anterior wall of which should rise during inspiration and fall during expiration. Make sure that the chest rises.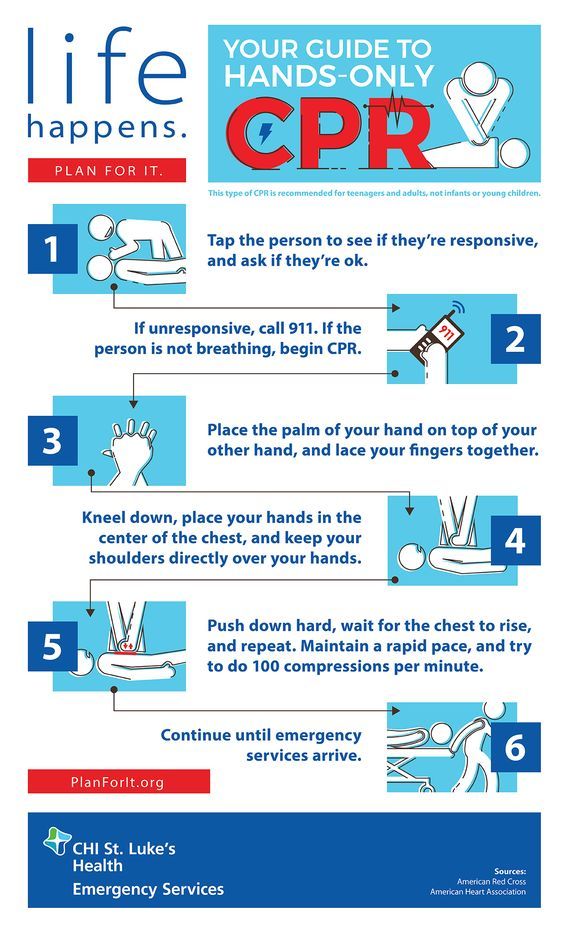 Watch your chest sink as the air comes out.
Watch your chest sink as the air comes out.
How to give chest compressions to a child?
In addition to ensuring an adequate supply of oxygen to the alveoli, cardiopulmonary bypass must be provided. For this purpose, indirect heart massage is used.
It is necessary to stand on the side of the child, the base of one palm is placed in the middle of the sternum, the second on top along the sternum. Then, with straight arms, without bending them at the elbow joint, it is necessary to press the chest to a depth of 4 cm or ⅓ of the sternum with a frequency of 100-120 per minute.
To prevent fracture of the ribs, the force must be concentrated only on the base of the palm, fingers should not press on the ribs. Hand pressure on the sternum is performed by the weight of the torso of the first aid participant.
Next, do 30 chest compressions, then 2 breaths. Continue compressions and breaths at a ratio of 2 breaths for every 30 compressions.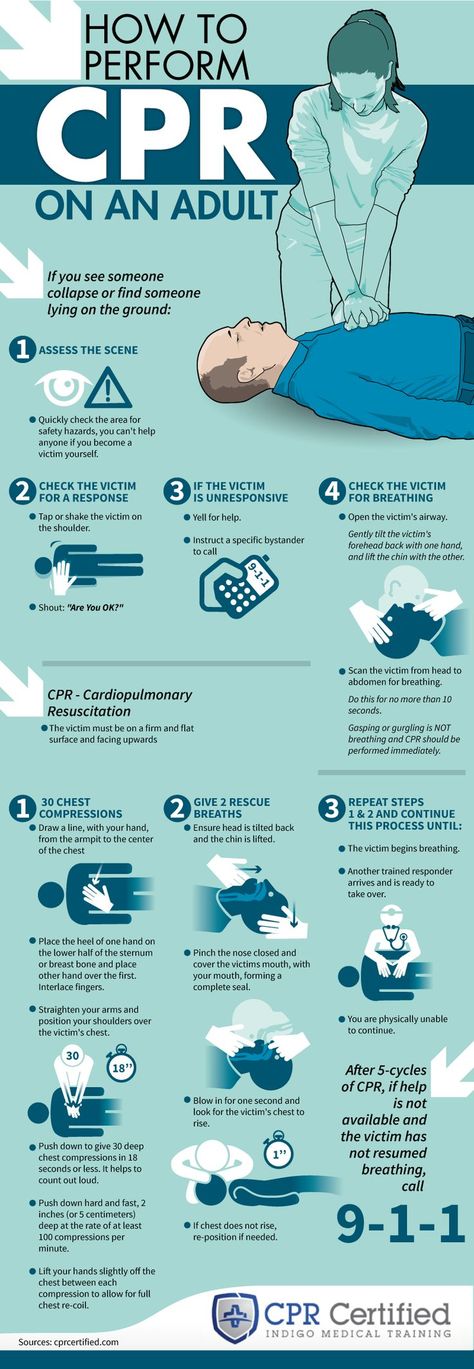
In children under 1 year of age , the procedure is different, it consists in pressing one or more index fingers on the sternum with a frequency of more than 100 beats per minute. If there are two rescuers, it is necessary to clasp the lower part of the sternum with the hands and compress with the tips of 2 thumbs.
The criteria for the effectiveness of chest compressions are:
the appearance of a pulse in the central peripheral arteries;
constriction of the pupils with the appearance of a reaction to light.
It should be remembered that long (more than 5-10 seconds) pauses should not be made during chest compressions.
If spontaneous breathing occurs before the arrival of medical personnel, place the child in a stable side position, control his breathing.
Also find out what should be in a first aid kit: a list of medicines and medical supplies for emergencies.
It is also important to know what to do before the ambulance arrives: how to provide first aid for burns, injuries, concussions and loss of consciousness.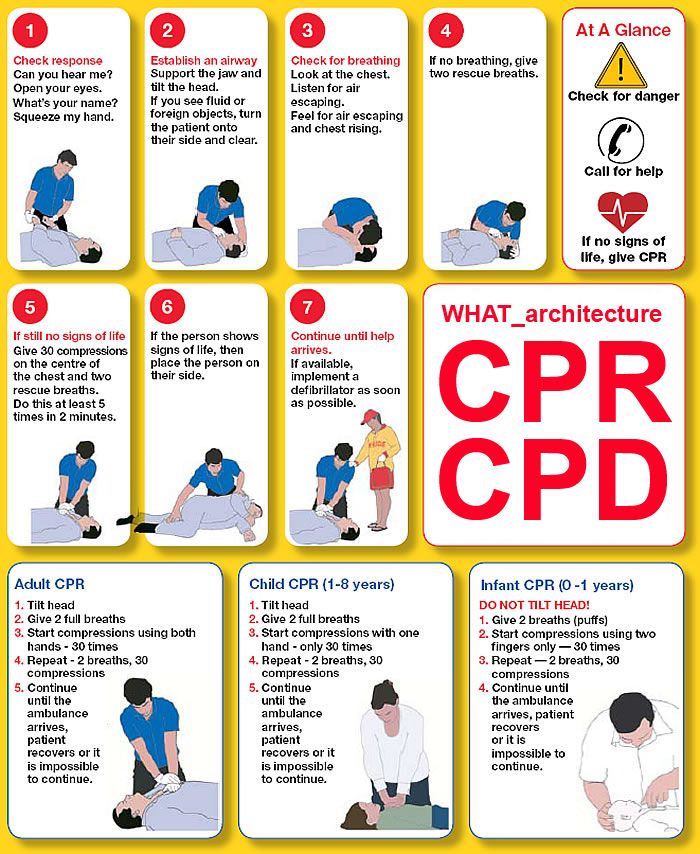
Learn more about health at apteka24.ua.
Sources
How to give CPR (mouth to mouth) to a baby or child / HSE
How to resuscitate a child / NHS
CPR for Children / WebMD
Child & Baby CPR / Red cross
Disclaimer
apteka24.ua provides comprehensive and reliable information on issues of medicine, health and well-being, however, the diagnosis and choice of treatment methods can only be made by your doctor! Self-medication may not be safe for your health. apteka24.ua is not responsible for possible negative consequences resulting from the use of information posted on the site by users of apteka24.ua.
CPR administration
© Copyrights Prenoxad Injection. 2014
Prescribing information | privacy policy
Please refer to Summary of Product Characteristics before prescribing.
Presentation: A 2ml pre-filled syringe containing Naloxone Hydrochloride 1mg/ml.
Indications: Prenoxad Injection is intended for emergency use in the home or other non-medical setting by appropriate individuals or in a health facility setting for the complete or partial reversal of respiratory depression induced by natural and synthetic opioids, including methadone, diamorphine (dicetylemorphine (INN)) and certain other opioids such as dextropropoxyphene and certain mixed agonist/antagonist analgesics: nalbuphine and pentazocine. Prenoxad Injection should be carried by persons at risk of such events. It may also be used for the diagnosis of suspected acute opioid overdose.
Dosage and Administration: : Prenoxad Injection may only be made available once the prescriber has assessed the suitability and competence of a client or representative to administer Naloxone in the appropriate circumstances. Prenoxad Injection is for administration by intramuscular injection.
Adults and the Elderly: Opioid overdosage (known or suspected).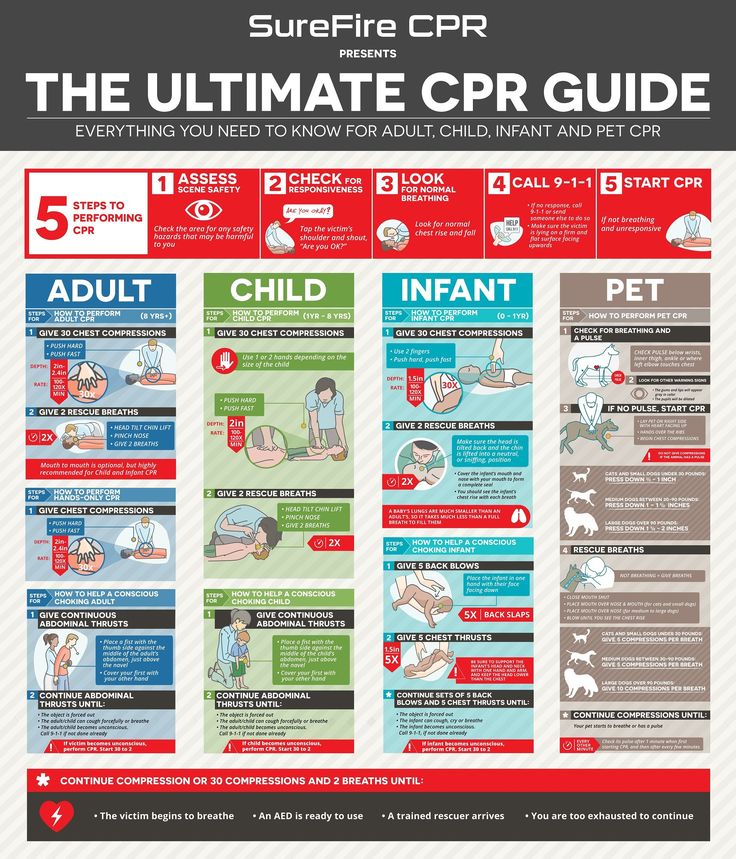 For Use by individuals in the community.
For Use by individuals in the community.
In patients where breathing does not appear to be normal. In patients where breathing does not appear to be normal administration of Prenoxad Injection should be preceded by calling emergency services and requesting an ambulance. Following this, 30 chest compressions and if possible 2 rescue breaths (Basic Life Support SINGLE CYCLE) should be given; 0.4ml Prenoxad Injection solution should then be administered by intramuscular injection into the outer thigh muscle or muscles of the upper arm, through clothing if necessary. A further 3 cycles of chest compressions and rescue breaths should then be given followed by administration of 0.4ml Prenoxad Injection. Three cycles of chest compression and rescue breaths should take approximately 2 minutes. This should be repeated until an ambulance arrives or the patient begins breathing normally / regains consciousness. The patient when breathing normally or has regained consciousness should be placed in the recovery position (lying on their side, mouth open pointing towards the ground) and observed continuously.
In patients were breathing is normal but the patient is unrousable or suspected to be unconscious. The patient should be placed in the recovery position. 0.4ml Prenoxad Injection solution should be administered by intramuscular injection into the outer thigh muscle or muscles of the upper arm, through clothing if necessary, and an ambulance should be called. 0.4ml Prenoxad Injection solution should then be administered every 2-3 minutes and continued until the ambulance arrives and or the patient regains consciousness.
Children and Neonates: The Prenoxad Injection presentation is not intended to be used for children in the home setting other than by an appropriately trained healthcare professional.
Contra-Indications: Known hypersensitivity to Naloxone or any of the ingredients.
Warnings And Precautions: Prenoxad Injection is intended as an emergency treatment and the patient should be advised to seek medical help immediately. It should be administered carefully to patients who have received large doses of opioids or to those physically dependent on opioids since too rapid reversal of opioid effects by Prenoxad may precipitate an acute withdrawal syndrome in such patients. Patients who have responded satisfactorily to Prenoxad should be kept under medical observation for at least 2 hours. Repeated doses of Prenoxad may be necessary since the duration of action of some opioids may exceed that of Prenoxad. Use with caution in patients with pre-existing cardiac, hepatic or renal disease and in those receiving medications with potential adverse cardiovascular effects e.g. hypotension, ventricular tachycardia or fibrillation and pulmonary oedema. Caution should be exercised and patients monitored when Prenoxad Injection is administered to these patients with renal insufficiency/failure or liver disease.
It should be administered carefully to patients who have received large doses of opioids or to those physically dependent on opioids since too rapid reversal of opioid effects by Prenoxad may precipitate an acute withdrawal syndrome in such patients. Patients who have responded satisfactorily to Prenoxad should be kept under medical observation for at least 2 hours. Repeated doses of Prenoxad may be necessary since the duration of action of some opioids may exceed that of Prenoxad. Use with caution in patients with pre-existing cardiac, hepatic or renal disease and in those receiving medications with potential adverse cardiovascular effects e.g. hypotension, ventricular tachycardia or fibrillation and pulmonary oedema. Caution should be exercised and patients monitored when Prenoxad Injection is administered to these patients with renal insufficiency/failure or liver disease.
Interactions: Administer carefully to opioid dependent patients including newborns of mother’s dependant or those suspected of having received large doses and observe for signs of acute withdrawal.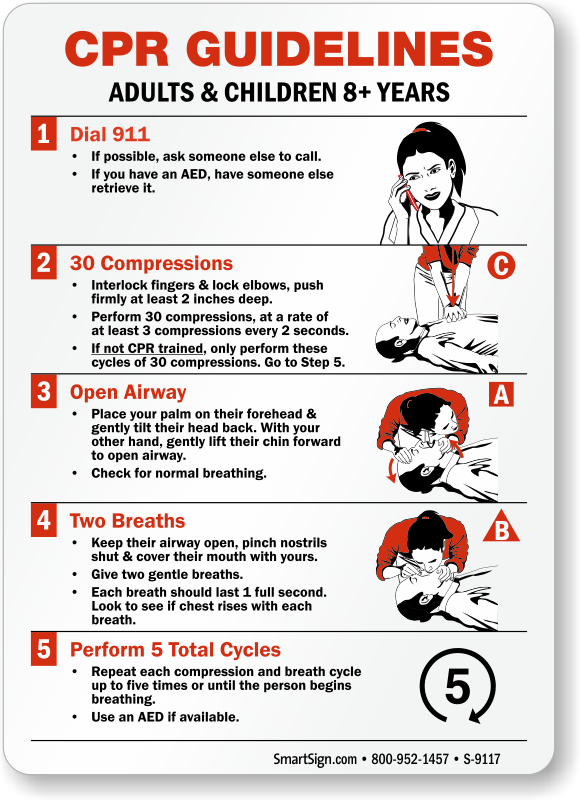
Pregnancy and Lactation: Prenoxad should be used with caution in pregnancy. The neonate must also be monitored for signs of opioid withdrawal. Naloxone may be administered during the second stage of labor to correct any respiratory depression due to opioid analgesics. It is not known whether Naloxone is excreted in human milk therefore use with caution in breastfeeding mothers.
Undesirable Effects: Common side effects include nausea, vomiting, dizziness, headache, ventricular tachycardia, hypotension and hypertension. Less common side effects: Tremor, sweating, arrhythmia, bradycardia, diarrhoea, dry mouth, hyperventilation, inflammation. Seizure tension, allergic recations, anaphylactic shock, fibrillation, cardiac arrest, erythema multiforme, fever, dyspnoea, runny nose, sneezing and yawning. Piloerection, weakness, shivering.
Product License Number: PL 12064/0125 Product License Holder: Aurum Pharmaceuticals Ltd, Bampton Road, Harold Hill, Romford, Essex RM3 8UG Basic NHS Price: £18.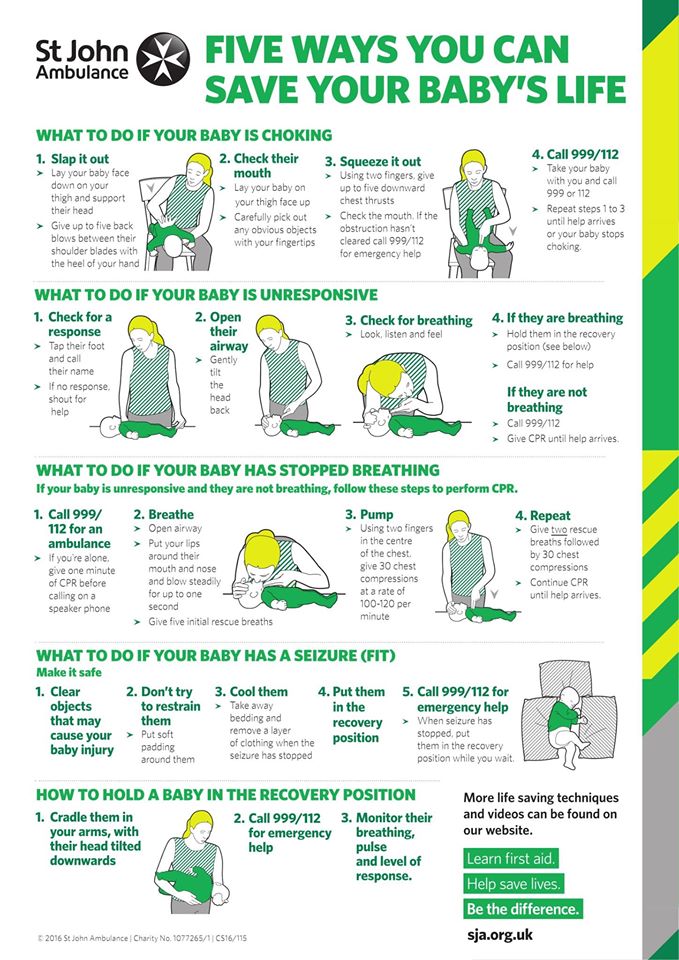 00 Legal Category: POM. Date of Preparation: April 2013
00 Legal Category: POM. Date of Preparation: April 2013
Reporting forms and information can be found at www.mhra.gov.uk/yellowcard. Adverse events should also be reported to Martindale Pharma Tel. 01277 266600 Fax 01708 382739e-mail [email protected]
Electronic Privacy Policy ("Privacy Policy")
Martindale Pharma ("We") is committed to protecting and respecting your right to privacy. In this section of the Privacy Policy, you will receive information about our procedures during the collection, use and disclosure of personally identifiable information that you may provide to us or that we may collect from you and which will then be processed by us. Please read the Privacy Policy section in its entirety before using or providing information on www.martindalepharma.co.uk ("this site"). This site is governed by UK law. Your use of this site requires your consent to be bound by this law and this Privacy Policy.
For the purposes of the UK Data Protection Act 1998, the Data Controller is Macarthys Laboratories Limited, branded as Martindale Pharma.
Active collection of information
This site may actively collect and process information collected from you by answering certain questions, as well as by contacting us directly via e-mail, job applications, questionnaires and / or feedback forms. Some of the information you provide may contain personally identifiable information (such as your email address). Please note that we may ask you for information when you report problems with this site. In addition, certain sections of this site may require you to provide information in order for you to effectively use said sections (eg newsletters, job applications) or participate in certain activities (eg promotions). In each case, you will be informed of what information is required, the purpose for which it is collected and what information is optional.
Passive collection of information
When you visit a website, certain information may be collected passively through a variety of technologies and means, including Internet Protocol (IP) and cookies.
Internet protocol
This website may use IP addresses. An IP address is a number assigned to your computer by your Internet service provider so that you can access the Internet. We use your IP address to analyze trends, track user movements, collect general demographic information for aggregate use and administer and improve the site.
Cookies
This site may use cookies to distinguish you from other users of this site. This helps us create a convenient environment for you when visiting this site and allows us to improve this site. A "cookie" is a piece of data stored on a user's hard drive that contains information about the user. Cookies allow the site to remember information about you and your preferences.
This site uses session cookies. "Session" cookies are temporary bits of information that are erased as soon as you close your web browser window or turn off your computer. Session cookies are used to improve website navigation and to collect aggregated statistical information. For example, session cookies allow a website to remember that a user has placed items in a shopping cart in an online store.
For example, session cookies allow a website to remember that a user has placed items in a shopping cart in an online store.
This site uses navigational data ("system logs" and "server logs") to manage the system, improve site content, market research purposes, and communicate information to visitors. You can change your browser settings so that cookies are not accepted. Please note that in this case, some functions of this site may not be available to you.
For more information about cookies and how to disable them, go to: http://www.allaboutcookies.org/ orhttp://www.ico.gov.uk/for_the_public/topic_specific_guides/online/cookies.aspx
Use of information
We use information about you to:
- to ensure that the content of this site is presented in the most effective way for you and your computer
- - to provide you with the requested information or information that we think may be of interest to you in cases where you have consented to such purposes;
- – to fulfill our obligations arising from entering into any contracts between you and us;
- - to allow you to participate in the interactive features of this service, if you agree to this;
- – notify you about changes to this service.

Recruitment
We understand the importance of maintaining the confidentiality of your personal information, skills and interests, and any other employment-related information you may provide when applying for a position with our company or an affiliate.
If we are considering you as a candidate for a position, your personal data may be shared with other companies acting on our behalf to provide employment screening services.
We will not release your personal information for six months and may contact you about future employment opportunities. You may leave our company holding information about you at any time by notifying us by email [email protected]. Please note that providing false information may result in the denial of a job application or the termination of any subsequent employment.
Disclosure
We may disclose your personally identifiable information to other Martindale Pharma affiliates in countries outside the European Economic Area (EEA) where legislation offering protections similar to those provided by the UK Data Protection Act 1998 may not apply.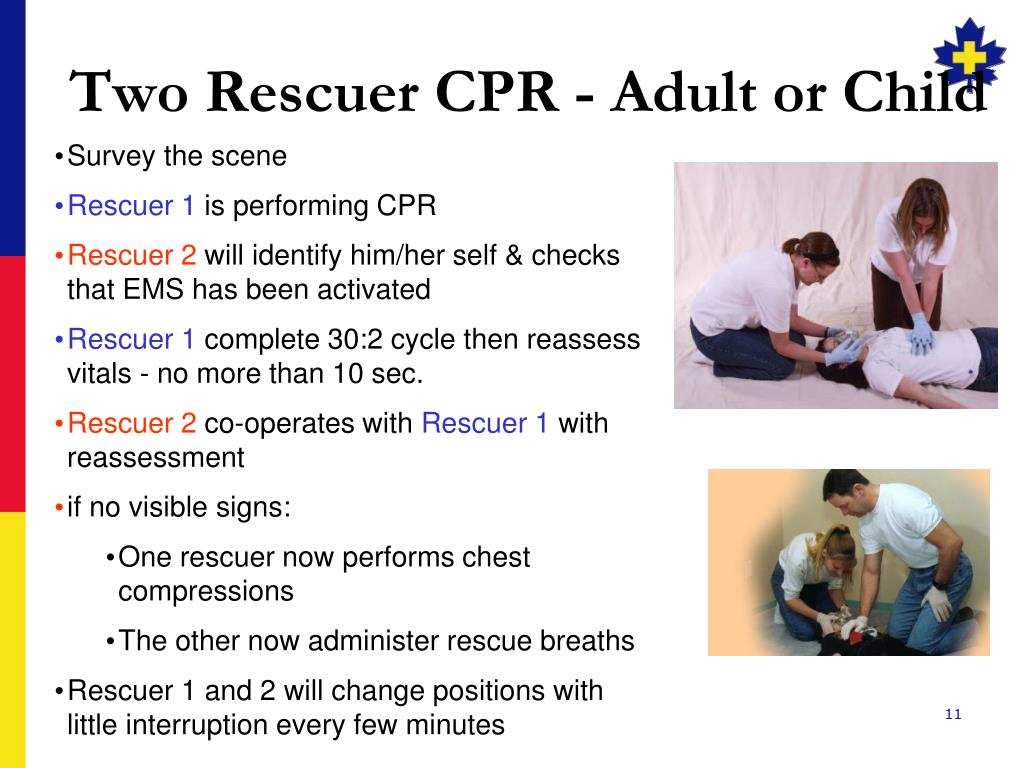 d. However, our affiliates agree to treat your information in accordance with this Privacy Policy. It may also be processed by personnel operating outside the EEA who work for us or for one of our suppliers. Such personnel may be involved in, among other things, the fulfillment of your order, the processing of your payment details, recruitment and the provision of support services. By providing personal data, you agree to their transfer, storage or processing. We will take all reasonable steps to ensure that your information is processed securely and in accordance with this Privacy Policy. In addition, we may disclose your personally identifiable information to a third party located in the UK and/or another country, but only
d. However, our affiliates agree to treat your information in accordance with this Privacy Policy. It may also be processed by personnel operating outside the EEA who work for us or for one of our suppliers. Such personnel may be involved in, among other things, the fulfillment of your order, the processing of your payment details, recruitment and the provision of support services. By providing personal data, you agree to their transfer, storage or processing. We will take all reasonable steps to ensure that your information is processed securely and in accordance with this Privacy Policy. In addition, we may disclose your personally identifiable information to a third party located in the UK and/or another country, but only
- contractors that we use to support our business activities (for example, order fulfillment services, technical support, delivery services, and financial institutions). In such a case, we will require the third party to consent to the treatment of your data in accordance with this Privacy Policy;
- in connection with the sale or purchase of any business or assets, assignment or other transfer of business to the company to which the information relates.
 In such a case, we will require the buyer to consent to the treatment of your data in accordance with this Privacy Policy;
In such a case, we will require the buyer to consent to the treatment of your data in accordance with this Privacy Policy;
if required by applicable law, court order or government regulation.
Any non-personally identifiable information obtained through this website will be used to its fullest extent.
Access, Correction and Storage
You can contact us at the contact details below to access, correct or update your personally identifiable information. We will take reasonable steps to update or correct the personally identifiable information we have that you have previously provided through this site. We will retain data that identifies you personally for a reasonable period of time (taking into account the purpose of collecting information from you).
Security
Although we do our best to protect your information, we cannot guarantee the security of your information transmitted to this site.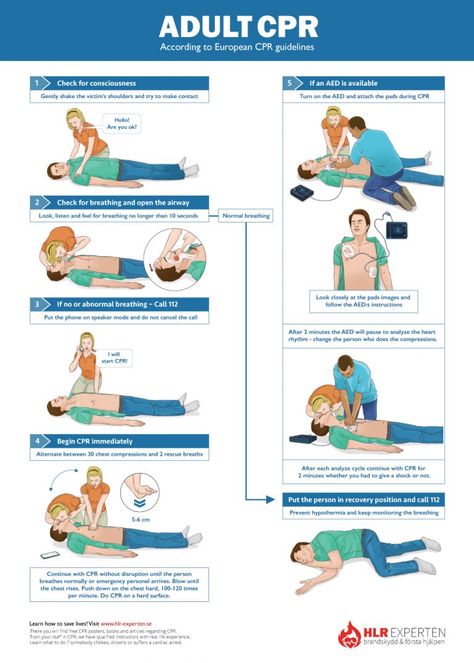 Any transmission of data is at your own risk. We take reasonable steps to protect your personally identifiable information while it is transmitted from your computer to this site and to protect it from loss, misuse and unauthorized access, disclosure, alteration or destruction. Please note that no data transmission over the Internet is 100% secure or error-free. In particular, email sent to or from this site may not be secure, and therefore you should take particular care when choosing the information you send us via email. Moreover, if you use passwords, identification numbers or other means of special access on this site, you are responsible for their safety.
Any transmission of data is at your own risk. We take reasonable steps to protect your personally identifiable information while it is transmitted from your computer to this site and to protect it from loss, misuse and unauthorized access, disclosure, alteration or destruction. Please note that no data transmission over the Internet is 100% secure or error-free. In particular, email sent to or from this site may not be secure, and therefore you should take particular care when choosing the information you send us via email. Moreover, if you use passwords, identification numbers or other means of special access on this site, you are responsible for their safety.
Links to other websites
This website contains links to other websites. Please note that we do not operate other websites and this Privacy Policy does not apply to those websites. We encourage users to be notified when they are leaving this site and we encourage you to read the privacy policy of each website that collects personally identifiable information.
Choice
Our users have the option to "opt-out" to the use of their information for purposes not directly related to this site when we request this information.
In the case of direct marketing, the user will be asked for consent (i.e. "consent to participate") before we process personally identifiable data for this purpose.
You can opt out of receiving marketing communications at any time. To do this, please contact us at [email protected]
Your consent
By using this site, you agree to this Privacy Policy. By providing information through this site, you consent to the collection, use and disclosure of that information in accordance with this Privacy Policy.
Children
This site is not intended for children under the age of 13. We do not knowingly collect information from site visitors in this age group.
Contact Details
If you have any questions, comments or concerns about this Privacy Policy or this site's information practices, please contact us at:
Martindale Pharma
IT Department
Hubert Road
Brentwood
Essex
CM14 4JY
Tel: 01277 266600
If you have any other questions please visit the Contact section.